-
Články
Top novinky
Reklama- Vzdělávání
- Časopisy
Top články
Nové číslo
- Témata
Top novinky
Reklama- Videa
- Podcasty
Nové podcasty
Reklama- Kariéra
Doporučené pozice
Reklama- Praxe
Top novinky
ReklamaPerinatal mortality associated with induction of labour versus expectant management in nulliparous women aged 35 years or over: An English national cohort study
In a cohort study using English Hospital Episode Statistics (HES) data, Hannah E Knight and colleagues examine perinatal mortality and other birth outcomes in association with labour induction at 39, 40, and 41 weeks.
Published in the journal: . PLoS Med 14(11): e32767. doi:10.1371/journal.pmed.1002425
Category: Research Article
doi: https://doi.org/10.1371/journal.pmed.1002425Summary
In a cohort study using English Hospital Episode Statistics (HES) data, Hannah E Knight and colleagues examine perinatal mortality and other birth outcomes in association with labour induction at 39, 40, and 41 weeks.
Introduction
Across industrialised nations, the proportion of births to women aged ≥35 years is rising [1,2]. In England and Wales, births to women aged ≥35 years have increased from 6% of all births in 1975 to 21% in 2015 [3]. There has also been an increase in the number of babies born to first-time mothers aged ≥35 years, which in 2015 accounted for 14% of all first-time births and 5.4% of all births in England and Wales [4].
Older women are at increased risk of pregnancy complications, including gestational diabetes, placenta praevia, and postpartum haemorrhage [5,6], and experience higher rates of intervention during labour and delivery [5,7]. After controlling for comorbidities, the risk of antepartum stillbirth at term is higher among women aged ≥35 years than among younger women [8] and is higher still for nulliparous women aged ≥35 years [9]. Observational data indicate that induction of labour at or before term may be beneficial because the risk of perinatal death is at its lowest for births between 38 and 39 weeks of gestation [9]. However, current United Kingdom guidelines recommend that induction for prolonged gestation is offered to women between 41 to 42 weeks of gestation, when the risk of stillbirth is 2 to 3 per 1,000 deliveries [10].
A recent randomised controlled trial (RCT) has shown that among nulliparous women aged ≥35 years, elective induction of labour at 39 weeks of gestation had no significant effect on the rate of caesarean section and no adverse short-term effects on maternal or neonatal outcomes compared with expectant management [11], but the trial was underpowered to examine the effect of induction of labour on the risk of perinatal death. Well-conducted observational studies have found that induction of labour at term is associated with decreased perinatal mortality in the general pregnant population [12]; however, none has been sufficiently powered to examine the impact on this specific age group known to be at increased risk. We employed a large English routine dataset to determine the association between induction of labour at ≥39 weeks and the risk of perinatal death among nulliparous women aged ≥35 years.
Methods
We designed our methods to test the hypothesis that induction of labour at 39, 40, and 41 weeks reduced the risk of perinatal mortality among nulliparous women aged ≥35 years compared with expectant management (continuation of pregnancy to either spontaneous labour, induction of labour, or caesarean section at a later gestation).
Details of ethics approval
The study is exempt from UK National Research Ethics Service (NRES) approval because it involved the analysis of an existing dataset of anonymised data for service evaluation. Hospital Episode Statistics (HES) data were made available by NHS Digital (Copyright 2015, re-used with the permission of NHS Digital. All rights reserved.) Approvals for the use of anonymised HES data were obtained as part of the standard NHS Digital data access process.
Data source
We used the HES database to identify births in English National Health Service (NHS) hospitals. The HES database contains patient demographics, diagnostic and procedure information, and administrative data for each inpatient episode of care since 1997 [13]. A unique identifier enables studies to combine episodes of care that belong to the same patient.
In the HES database, for episodes related to childbirth, supplementary fields (the ‘maternity tail’) capture details including parity, birthweight, gestational age, onset of delivery, method of delivery, and birth outcome. Mothers’ delivery episodes were defined as records containing information about the mode of delivery in either the OPCS4 codes (R17–R25) or the maternity tail.
Diagnostic information is coded using the International Classification of Diseases, 10th Revision (ICD10) [14], and operative procedures are coded using the UK Office for Population Censuses and Surveys Classification, 4th Revision (OPCS4) [15]. The level of data completeness has improved over time [16,17] but varies across NHS hospitals: in 2014, data on onset of labour and gestational age were available in 85% and 82% of all delivery episodes, respectively [18].
Study population
We included all nulliparous women aged 35 to 50 years delivering at 39 weeks of gestation or beyond, between April 2009 and March 2014. We excluded multiple births; women with preexisting comorbidities (hypertension, diabetes, and cardiac or lung disease); births complicated by fetal malpresentation, abdominal pregnancy, and placenta praevia; and pregnancies resulting in perinatal deaths due to congenital abnormality. We excluded records that were missing birth status, delivery onset, or gestational age. We also performed data quality assessments at the individual hospital level and excluded hospitals with suspected poor-quality data for these key data items (S1 Appendix, Text A). The characteristics of women excluded on the basis of these assessments were compared with those of the study cohort. Limiting birth cohorts in this way to include only hospitals with high completeness of recording has been demonstrated to be a valid way of constructing cohorts from routine hospital data [16,17]. The mothers’ delivery records were linked to the hospital records of their babies using probabilistic linkage [19] to obtain data on perinatal outcomes using the babies' birth records (e.g., for in-hospital perinatal death) and any subsequent hospital inpatient or A&E records (e.g., emergency neonatal readmission within 28 days). Induction of labour was defined as either surgical induction by amniotomy; medical induction, including the administration of agents either orally, intravenously, or intravaginally; or a combination of surgical and medical induction.
Definitions of the induction and expectant management groups
For an observational study to appropriately examine the outcomes of induction of labour at different gestational ages, it is important to compare outcomes of women who have an induction of labour at a particular week of gestation (week n) with women who are expectantly managed, i.e., go on to deliver at a later gestation by any mode of onset, and not with women who labour spontaneously at the same gestation. There are 2 possible ways to define the expectant management group using observational data in which gestational age is recorded in weeks (see Stock et al. [12] for discussion):
women delivering at weeks >n
women delivering at weeks ≥n
For the primary analysis, we adopted the first approach, including women delivering at weeks >n following spontaneous or induced labour or prelabour caesarean. The robustness of this approach was then tested using a secondary analysis that used the alternative definition.
For each week of gestation examined, we excluded women if their labour was induced following an antepartum intrauterine death or prelabour rupture of membranes because, in both conditions, if labour does not begin spontaneously within 24 hours, the standard management is induction of labour [10]. However, we did not exclude women with these complications from the expectant management group if the event occurred after the week of gestation of induction in the induction group (at weeks >n). This followed a similar approach used in previous studies [12] and is supported by evidence that delays in the delivery of antepartum stillbirths or PROM are uncommon in UK hospitals [20]. Intrapartum stillbirths in all weeks ≥n were included in both groups.
Outcomes
We examined the following neonatal outcomes: stillbirth, in-hospital perinatal death, birth injury, shoulder dystocia, hypoxia in labour, meconium aspiration syndrome, neonatal seizures, and emergency readmission to hospital within 28 days of birth. In-hospital perinatal death was defined as stillbirth or in-hospital neonatal death within 7 days of birth. We also recorded the following maternal outcomes: emergency caesarean section, instrumental delivery, third or fourth degree perineal tear, and emergency readmission to hospital within 28 days of delivery. To calculate readmission rates, births that occurred in the last 28 days of the study period were excluded. Details of the definitions used are given in S1 Appendix, Table A.
Statistical analysis
All analyses were prespecified as described in the Methods section, with the exceptions of the exclusion of women with preexisting comorbidities and the use of Poisson rather than logistic regression. These modifications were made prior to the commencement of any statistical analyses; the rationale for each change is provided in S1 Appendix, Text B. We did not publish or pre-register a plan for this analysis.
We used proportions to summarise the distribution of pregnancy characteristics of induced and non-induced women and the chi-squared test for comparisons of variables between the groups. For each week of gestation, univariable and multivariable Poisson regression with robust standard errors was used to estimate the crude and adjusted effects of induction of labour compared with expectant management on each maternal and perinatal outcome. We chose not to use logistic regression because odds ratios overestimate the risk ratio for common outcomes [21]. The confounding variables included in all models were maternal age (years); ethnicity (white, Asian, black, other, or unknown); year of birth; baby’s sex (male or female); birthweight percentile according to UK 1990 fetal growth charts (<10th, 10th–90th, or >90th) [22]; and socioeconomic quintile according to the a Index of Multiple Deprivation (IMD) score, a measure that combines economic, social, and housing indicators [23]. The year of the birth was recorded as a linear variable to take into account changes in clinical practice over time. Estimates were adjusted for pregnancy-related conditions (pregnancy-induced hypertension, preeclampsia, or oedema; gestational diabetes; and fluid abnormalities) when these were found to have significant coefficients. No formal tests of interaction were done, and no adjustments were made for multiple comparisons. For both our primary and secondary analyses, we estimated the number of inductions of labour needed to prevent 1 perinatal death: number needed to treat (NNT) = 1/([induction of labour event risk]−[expectant management event risk]). All statistical tests were 2-sided, and the level of significance was set at P < 0.05. All analyses were performed in STATA version 14.1 (StataCorp, College Station, TX, United States).
Results
There were 77,327 women aged 35–50 years who met the inclusion criteria and gave birth in hospitals that passed the data quality assessments for key data items (Fig 1). Of these women, 25,583 (33.1%) were induced and 51,744 (66.9%) were not. Induction of labour rates among this group of women increased each year during the time period from 30.2% in 2009–2010 to 35.7% in the 2013–2014 cohort. Medical induction of labour was the principal method of induction throughout the time period (57.7% of inductions), with surgical and combined methods used less frequently (19.7% and 19.4% of inductions, respectively).
Fig. 1. Cohort selection flow chart. 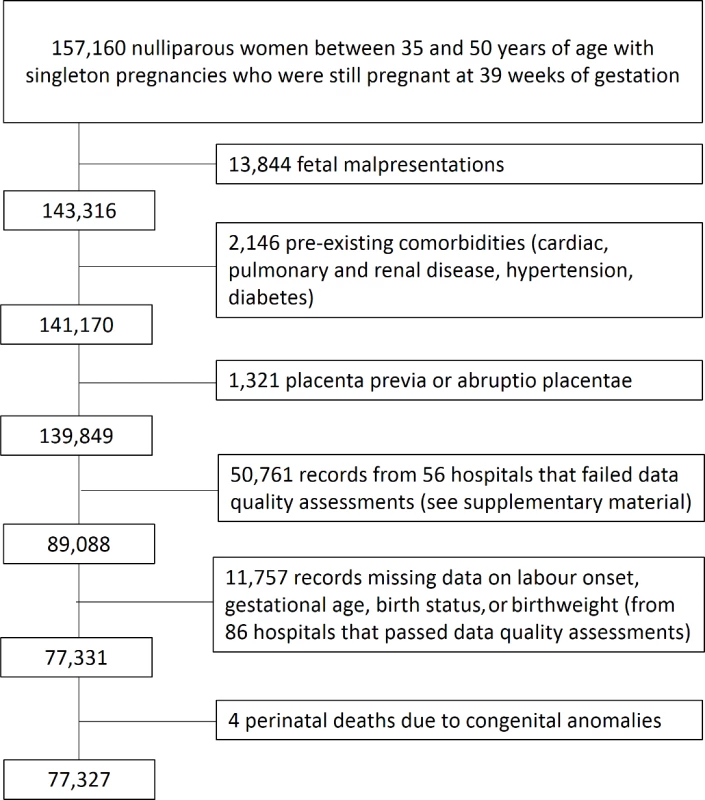
There were 50,761 eligible women who gave birth in hospitals that failed the data quality assessments for key data items required in the analysis, and these women were therefore not included in the study. The women included in the study shared similar characteristics to the excluded women who gave birth in hospitals with poor data quality (S1 Appendix, Table B). Hospitals that failed the data quality assessments were missing data on gestational age, birth status, and onset of labour in 40%, 25%, and 24% of records, respectively, compared with 11%, 10%, and 11% of records in hospitals that passed these assessments.
Women who had labour induced were more likely to be over 40 years old, of white ethnicity, and to deliver infants in less than the 10th centile for birthweight (Table 1). They were also more likely to have acquired complications of pregnancy. Fig 2 describes the composition of the cohorts used for the primary and secondary analyses.
Fig. 2. Composition of cohort by week of gestation. 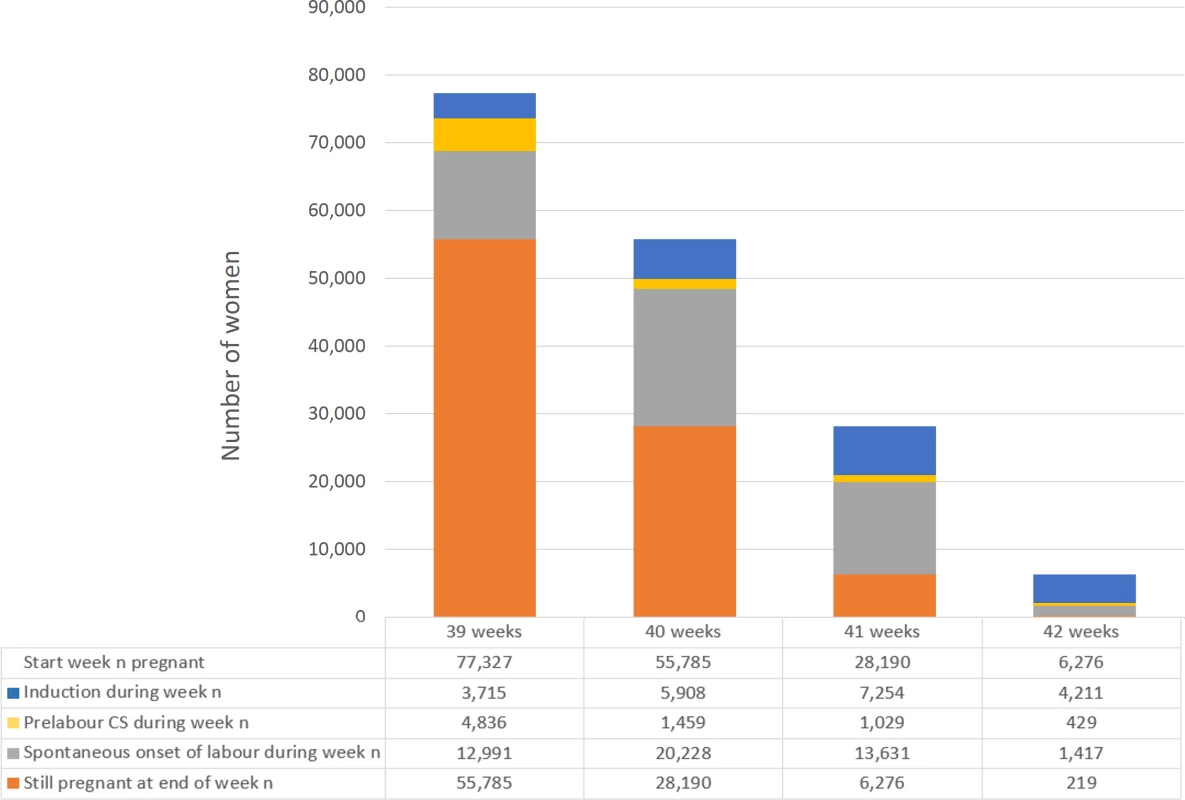
For each week of gestation (column), the primary analysis compares women who were induced at week n (blue column segment) with women who were expectantly managed, defined as those who delivered at weeks >n (orange column segment). The secondary analysis compares women who were induced at week n (blue column segment) with those who were expectantly managed according to the alternative definition, i.e., delivered at weeks ≥n (orange, grey, and yellow column segments). Abbreviation: CS, caesarean section. Tab. 1. Pregnancy characteristics of 77,327 women according to induction of labour. 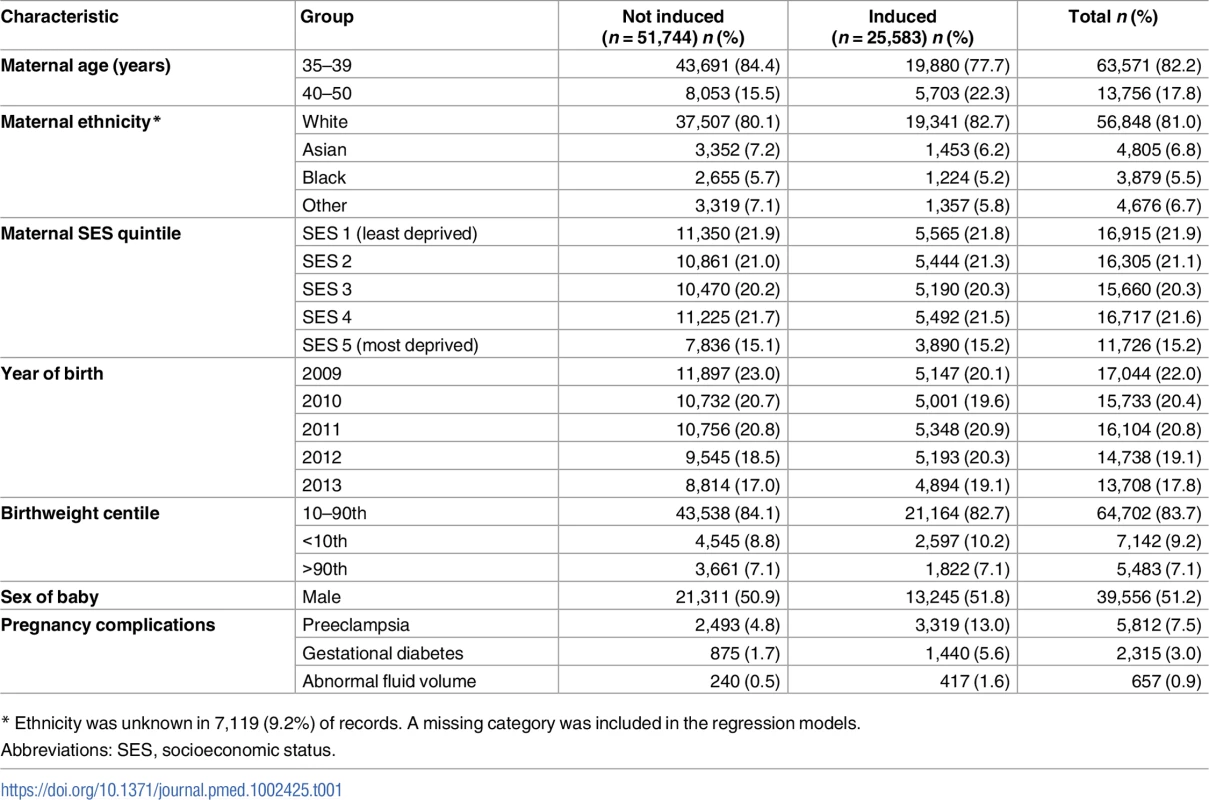
* Ethnicity was unknown in 7,119 (9.2%) of records. A missing category was included in the regression models. Perinatal mortality
Labour induction from 40 weeks onwards was associated with a significantly reduced rate of both in-hospital perinatal death and stillbirth when compared with expectant management (Fig 3).
Fig. 3. Perinatal outcomes after induction of labour compared with expectant management by week of gestation of induction of labour. 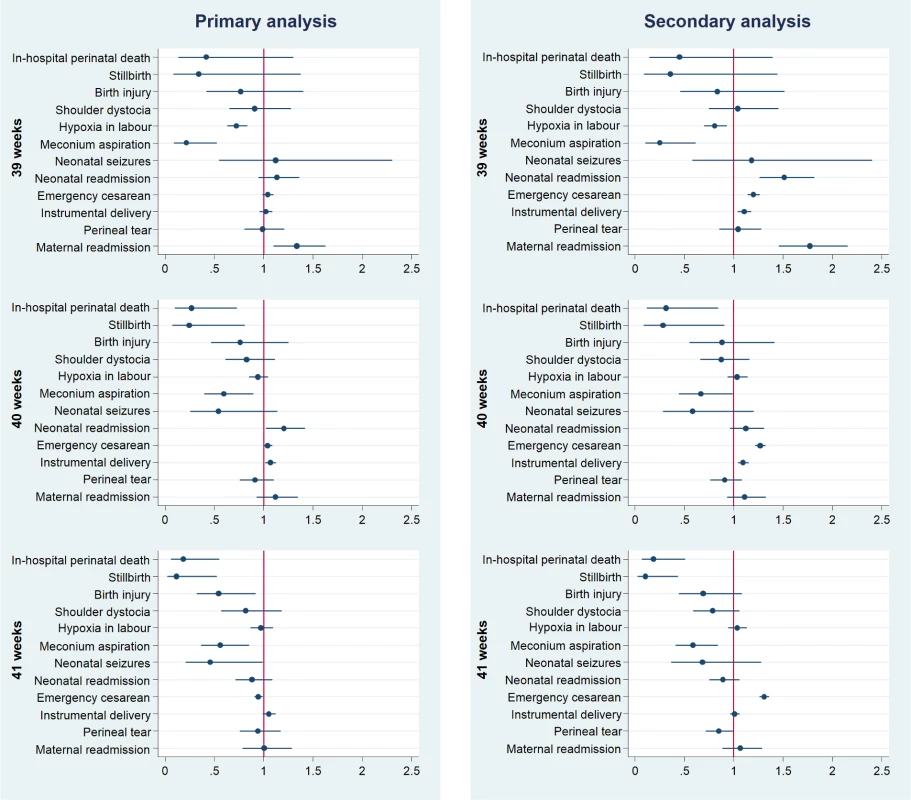
Outcomes have been adjusted for potential confounders. Full details and results of all models are presented in Table 2 and S1 Appendix, Table C. The horizontal axis represents adjusted relative risk, with a relative risk <1 favouring induction of labour. In the primary analysis, the adjusted risk ratio (adjRR) for in-hospital perinatal death associated with induction compared with expectant management was 0.33 (95% CI 0.13–0.80) at 40 weeks and 0.24 (95% CI 0.09–0.65) at 41 weeks (Table 2). However, there was no difference in the estimated adjRR for in-hospital perinatal death associated with induction at 39 weeks (0.37; 95% CI 0.12–1.15). Similar magnitudes of effect were observed for stillbirth, with an adjRR of 0.25 (95% CI 0.09–0.79) at 40 weeks and 0.18 (95% CI 0.05–0.65) at 41 weeks. The results of the secondary analysis were also consistent with those in the primary analysis for both outcomes (Fig 3 and S1 Appendix, Table C). The unadjusted risk ratios did not materially differ from the risk ratios adjusted for maternal characteristics (Table 2 and S1 Appendix, Table C).
Tab. 2. Perinatal outcomes after induction of labour compared with expectant management (primary analysis). 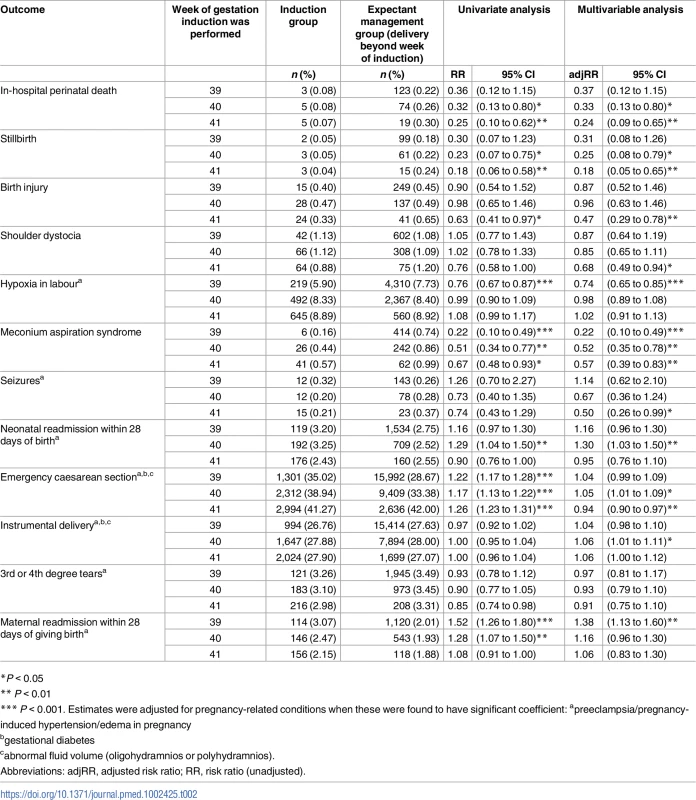
*P < 0.05 The NNT analysis indicated that 562 (95% CI 366–1,210) and 658 (95% CI 421–1,506) inductions of labour at 40 weeks would be required to prevent 1 perinatal death, for the primary and secondary analysis, respectively.
Perinatal morbidity
In the primary analysis, labour induction from 39 weeks onwards was associated with a significantly reduced rate of meconium aspiration syndrome, when compared with expectant management (Fig 3). Induction at 39 weeks was also significantly associated with reduced rates of hypoxia in labour (adjRR 0.74; 95% CI 0.65–0.85). However, this association was not significant at later weeks of gestation. Labour induction at 40 weeks was associated with higher rates of neonatal readmission to hospital within 28 days of birth (adjRR 1.30; 95% CI 1.03–1.50). Induction at 41 weeks was associated with reduced rates of birth injury (adjRR 0.47; 95% CI 0.29–0.78) and neonatal seizures (adjRR 0.50; 95% CI 0.26–0.99). No differences were found in the rates of shoulder dystocia in association with induction. Similar observations were seen in the secondary analysis, although the association with neonatal seizures was not replicated in secondary analysis (adjRR 0.67, 95% CI 0.38–1.16), and the association with higher neonatal readmission was seen at 39 as well as 40 weeks (Fig 3 and S1 Appendix, Table C).
Maternal outcomes
In the primary analysis, no differences in the rates of emergency caesarean section or instrumental delivery were found in association with induction at 39 weeks when compared with expectant management (Fig 3). Induction at 40 weeks was associated with a slightly increased risk of instrumental vaginal delivery (adjRR 1.06; 95% CI 1.01–1.11) and emergency caesarean delivery (adjRR 1.05; 95% CI 1.01–1.09). Induction at 41 weeks was associated with a slightly reduced risk of emergency caesarean section (adjRR 0.94; 95% CI 0.90–0.97) compared with expectant management. No differences were found in the rates of severe perineal tears in association with induction. Induction at 39 weeks was associated with higher risk of maternal readmission within 28 days of delivery (adjRR 1.38; 95% CI 1.13–1.60). In the secondary analysis, induction from 39 weeks onwards was associated with a 20%–30% increased rate of emergency caesarean section when compared with expectant management and a 10% increased rate of instrumental delivery at 39 and 40 weeks (S1 Appendix, Table C).
Discussion
The key finding of the present study is that induction of labour at 40 weeks of gestation was associated with a third of the risk of perinatal death compared with expectant management in a national cohort of nulliparous women aged ≥35 years. At this stage in pregnancy, the risk of perinatal death with expectant management was 26 per 10,000 pregnancies, whereas the risk among women induced at 40 weeks was 8 per 10,000 pregnancies. If these associations are causal, these data indicate that 562 (95% CI 366–1,210) inductions of labour would be required to prevent each perinatal death. Induction of labour was also associated with a significantly reduced risk of meconium aspiration syndrome.
A recent RCT has demonstrated no short-term adverse effect on the mother or infant of routine induction of labour at 39 weeks for women of advanced maternal age, and an associated economic evaluation has suggested that such a policy was associated with lower healthcare costs, principally through reduced rates of maternal readmission [24]. These findings could be taken together with those of the present study and used to support a policy of actively offering all women aged ≥35 years in their first pregnancy to have labour induced around their due date.
However, it could be argued that, because the data in this study are observational, the findings may be due to bias. We do not feel that this is a plausible explanation. First, the women being induced had higher proportions of risk factors, such as very advanced age and acquired complications of pregnancy. Second, we were able to adjust for these and other confounding factors in our statistical models, and this was without material effect. Third, while the risk adjustment models did not include all potential confounders, if there was an imbalance in their distribution across the 2 groups, it is likely that the confounders would be more prevalent in the induction group. Fourth, other well-conducted observational studies using other datasets have found similar effects on perinatal mortality, albeit not in this specific maternal age group [12].
The major cause of perinatal death at term is antepartum stillbirth. It is biologically plausible that stopping pregnancy at week 40 prevents the possibility of an antepartum stillbirth at 41 weeks. It may be argued that induction of labour in this context should only be widely recommended when these results are confirmed by an RCT, but the rarity of the outcome means a trial would be difficult. A sample size calculation based on the observed rates of perinatal death and effect size in the present study indicates that around 15,000 women would be required for a trial with 90% power to detect similarly large effects at 40 weeks of gestation. A well-funded multicentre RCT managed to recruit just over 600 such women [11], which is 4% of the required sample size.
In our primary analysis, we observed a 5% increase in the rate of emergency caesarean section and a 6% increase in the rate of operative vaginal delivery in the induction group. Although the 35/39 trial demonstrated no statistically significant association between induction and these outcomes, the point estimates for the effects in the present study are within the 95% CIs reported in the RCT [11]. Given the higher-risk nature of the women being induced, the adverse associations with induction of labour may be due to unmeasured confounders, as discussed above. These issues may be resolved by a larger-scale RCT of routine induction of labour in 6,000 nulliparous women aged ≥35 years, which is currently in progress [25]. However, that study will not be powered to detect a reduction in the risk of perinatal death, on the basis of the sample size calculation above.
The present study had a number of methodological strengths. The cohort is large and was drawn from an unselected population-based database which records the necessary data items for the appropriate comparison groups to be defined for this study. The use of a novel technique to link mothers’ and babies’ hospital records [19] enabled an examination of both maternal and perinatal outcomes, including morbidity as well as mortality. We were also able to follow up newborns after hospital discharge to examine emergency hospital readmission rates. A disadvantage of hospital administrative birth data is varying data quality between hospitals, which led to the records from some hospitals being excluded from this study. However, this approach has been demonstrated by others to be a valid way of constructing birth cohorts [16], and validation studies have found that the data are nationally representative for key variables, including sex, gestation, birth weight, maternal age, stillbirth, and multiple birth [19].
Despite the large sample size in the present study, it could be argued that because the number of observed perinatal deaths in the induced group is very small, under-recording of labour induction in the dataset could have a major impact on the results. However, since HES is used to guide the reimbursement of maternity care expenses and labour induction is recognised within the national pricing framework [26], we would expect hospitals not to overlook this procedure when coding. To reduce the risks associated with under - and over-coding of induction, we also excluded hospitals that appeared to have divergent coding practices from the analysis (S1 Appendix, Table A).
As with other studies using routine data to examine this issue, we addressed the limitation of gestational age being recorded in weeks rather than in days by testing the robustness of our primary definition of the expectant management group using a secondary analysis that used the alternative definition [12]. Nevertheless, we were not able to control for some important possible confounders, such as maternal obesity, nor to examine some important outcomes, such as postpartum haemorrhage. It is also possible that a small number of antepartum stillbirths were inappropriately included in the expectant management group in the case of delay between death and delivery following induction. Inclusion of these women in the expectant management group would overestimate the risk of perinatal death rate in this group. However, this bias is more likely to affect the results of our secondary analysis, and we found that the magnitude of effect was similar in both analyses.
In summary, our results suggest that among women aged ≥35 years, induction of labour at term is associated with a lower rate of perinatal mortality and morbidity. Hence, bringing forward the routine offer of induction of labour from the current recommendation of 41–42 weeks to 40 weeks of gestation in this group may reduce overall rates of perinatal death. It is, however, important to note the potential for downsides to a policy which would significantly increase the use of labour induction, and further studies should examine the impact of such a policy on resource utilisation and patient satisfaction.
Supporting Information
Zdroje
1. Australian Institute of Health and Welfare. Australia’s mothers and babies 2013—in brief. Perinatal statistics series no. 31. Canberra: AIHW, 2015.
2. Mathews T, Hamilton B. Mean age of mother, 1970–2000. National Vital Statistics Reports vol 50 no. 1. Hyattsville, Maryland: National Center for Health Statistics, 2002.
3. Office for National Statistics. Birth Summary Tables—England and Wales 2015 [cited 2017 3rd January]. Available from: https://www.ons.gov.uk/peoplepopulationandcommunity/birthsdeathsandmarriages/livebirths/datasets/birthsummarytables
4. Office for National Statistics. Births by parents' characteristics 2015 [cited 2017 3rd January]. Available from: https://www.ons.gov.uk/peoplepopulationandcommunity/birthsdeathsandmarriages/livebirths/datasets/birthsbyparentscharacteristics.
5. Jolly M, Sebire N, Harris J, Robinson S, Regan L. The risks associated with pregnancy in women aged 35 years or older. Hum Reprod. 2000;15(11):2433–7. 11056148.
6. Joseph KS, Allen AC, Dodds L, Turner LA, Scott H, Liston R. The perinatal effects of delayed childbearing. Obstet Gynecol. 2005;105(6):1410–8. doi: 10.1097/01.AOG.0000163256.83313.36 15932837.
7. Smith GC, Cordeaux Y, White IR, Pasupathy D, Missfelder-Lobos H, Pell JP, et al. The effect of delaying childbirth on primary cesarean section rates. PLoS Med. 2008;5(7):e144. doi: 10.1371/journal.pmed.0050144 18597550; PMCID: PMCPMC2443199.
8. Huang L, Sauve R, Birkett N, Fergusson D, van Walraven C. Maternal age and risk of stillbirth: a systematic review. CMAJ. 2008;178(2):165–72. doi: 10.1503/cmaj.070150 18195290; PMCID: PMCPMC2175002.
9. Smith GC. Life-table analysis of the risk of perinatal death at term and post term in singleton pregnancies. Am J Obstet Gynecol. 2001;184(3):489–96. doi: 10.1067/mob.2001.109735 11228508.
10. National Institute for Health and Clinical Excellence. Inducing labour. NICE guideline (CG70). 2008.
11. Walker KF, Bugg GJ, Macpherson M, McCormick C, Grace N, Wildsmith C, et al. Randomized Trial of Labor Induction in Women 35 Years of Age or Older. N Engl J Med. 2016;374(9):813–22. doi: 10.1056/NEJMoa1509117 26962902.
12. Stock SJ, Ferguson E, Duffy A, Ford I, Chalmers J, Norman JE. Outcomes of elective induction of labour compared with expectant management: population based study. BMJ. 2012;344:e2838. doi: 10.1136/bmj.e2838 22577197; PMCID: PMC3349781.
13. NHS Digital. Hospital Episode Statistics [cited 2017 3rd January]. Available from: http://content.digital.nhs.uk/hes.
14. World Health Organization. International Classification of Diseases, 10th edition (ICD-10). Available from: http://apps.who.int/classifications/icd10/browse/2016/en.
15. Mishanina E, Rogozinska E, Thatthi T, Uddin-Khan R, Khan KS, Meads C. Use of labour induction and risk of cesarean delivery: a systematic review and meta-analysis. CMAJ. 2014;186(9):665–73. doi: 10.1503/cmaj.130925 24778358; PMCID: PMC4049989.
16. Murray J, Saxena S, Modi N, Majeed A, Aylin P, Bottle A, et al. Quality of routine hospital birth records and the feasibility of their use for creating birth cohorts. J Public Health (Oxf). 2013;35(2):298–307. doi: 10.1093/pubmed/fds077 22967908.
17. Ghosh RE, Ashworth DC, Hansell AL, Garwood K, Elliott P, Toledano MB. Routinely collected English birth data sets: comparisons and recommendations for reproductive epidemiology. Arch Dis Child Fetal Neonatal Ed. 2016;101(5):F451–7. doi: 10.1136/archdischild-2015-309540 26837309.
18. NHS Digital. NHS Maternity Statistics—England, 2013–14 2015 [cited 2017 3rd January]. Available from: http://content.digital.nhs.uk/catalogue/PUB16725.
19. Harron K, Gilbert R, Cromwell D, van der Meulen J. Linking Data for Mothers and Babies in De-Identified Electronic Health Data. PLoS ONE. 2016;11(10):e0164667. doi: 10.1371/journal.pone.0164667 27764135; PMCID: PMCPMC5072610.
20. Smith GC. Sex, birth weight, and the risk of stillbirth in Scotland, 1980–1996. Am J Epidemiol. 2000;151(6):614–9. 10733043.
21. Knol MJ, Le Cessie S, Algra A, Vandenbroucke JP, Groenwold RH. Overestimation of risk ratios by odds ratios in trials and cohort studies: alternatives to logistic regression. CMAJ. 2012;184(8):895–9. doi: 10.1503/cmaj.101715 22158397; PMCID: PMCPMC3348192.
22. Freeman JV, Cole TJ, Chinn S, Jones PR, White EM, Preece MA. Cross sectional stature and weight reference curves for the UK, 1990. Arch Dis Child. 1995;73(1):17–24. 7639543; PMCID: PMCPMC1511167.
23. Department of Health. English indices of deprivation. Available from: https://www.gov.uk/government/collections/english-indices-of-deprivation.
24. Walker KF, Dritsaki M, Bugg G, Macpherson M, McCormick C, Grace N, et al. Labour induction near term for women aged 35 or over: an economic evaluation. BJOG. 2017. doi: 10.1111/1471-0528.14557 28075507.
25. Grobman WA. Induction of Labor and Cesarean Delivery. N Engl J Med. 2016;374(9):880–1. doi: 10.1056/NEJMe1516461 26962908.
26. National Casemix Office HaSCIC. HRG4 2015/16 Consultation Grouper. HRG4 Chapter Summaries. HSCIC, 2014.
Štítky
Interní lékařství
Článek Contemporary disengagement from antiretroviral therapy in Khayelitsha, South Africa: A cohort studyČlánek Bioequivalence of twice-daily oral tacrolimus in transplant recipients: More evidence for consensus?
Článek vyšel v časopisePLOS Medicine
Nejčtenější tento týden
2017 Číslo 11- Berberin: přírodní hypolipidemikum se slibnými výsledky
- Léčba bolesti u seniorů
- Příznivý vliv Armolipidu Plus na hladinu cholesterolu a zánětlivé parametry u pacientů s chronickým subklinickým zánětem
- Červená fermentovaná rýže účinně snižuje hladinu LDL cholesterolu jako vhodná alternativa ke statinové terapii
- Jak postupovat při výběru betablokátoru − doporučení z kardiologické praxe
-
Všechny články tohoto čísla
- Labour trafficking: Challenges and opportunities from an occupational health perspective
- The end of HIV: Still a very long way to go, but progress continues
- Contemporary disengagement from antiretroviral therapy in Khayelitsha, South Africa: A cohort study
- Bioequivalence of twice-daily oral tacrolimus in transplant recipients: More evidence for consensus?
- Treatment guidelines and early loss from care for people living with HIV in Cape Town, South Africa: A retrospective cohort study
- Perinatal mortality associated with induction of labour versus expectant management in nulliparous women aged 35 years or over: An English national cohort study
- Core Outcome Set-STAndards for Development: The COS-STAD recommendations
- Closing the gaps in the HIV care continuum
- Association between the 2012 Health and Social Care Act and specialist visits and hospitalisations in England: A controlled interrupted time series analysis
- HIV pre-exposure prophylaxis and early antiretroviral treatment among female sex workers in South Africa: Results from a prospective observational demonstration project
- Sexual exploitation of unaccompanied migrant and refugee boys in Greece: Approaches to prevention
- Child sex trafficking in the United States: Challenges for the healthcare provider
- The expanding epidemic of HIV-1 in the Russian Federation
- Cardiovascular disease (CVD) and chronic kidney disease (CKD) event rates in HIV-positive persons at high predicted CVD and CKD risk: A prospective analysis of the D:A:D observational study
- Validity of a minimally invasive autopsy for cause of death determination in maternal deaths in Mozambique: An observational study
- malERA: An updated research agenda for malaria elimination and eradication
- malERA: An updated research agenda for health systems and policy research in malaria elimination and eradication
- A combination intervention strategy to improve linkage to and retention in HIV care following diagnosis in Mozambique: A cluster-randomized study
- Bioequivalence between innovator and generic tacrolimus in liver and kidney transplant recipients: A randomized, crossover clinical trial
- malERA: An updated research agenda for basic science and enabling technologies in malaria elimination and eradication
- Human trafficking and exploitation: A global health concern
- Virological response and resistance among HIV-infected children receiving long-term antiretroviral therapy without virological monitoring in Uganda and Zimbabwe: Observational analyses within the randomised ARROW trial
- Postmenopausal hormone therapy and risk of stroke: A pooled analysis of data from population-based cohort studies
- Lansoprazole use and tuberculosis incidence in the United Kingdom Clinical Practice Research Datalink: A population based cohort
- malERA: An updated research agenda for insecticide and drug resistance in malaria elimination and eradication
- Safety, pharmacokinetics, and immunological activities of multiple intravenous or subcutaneous doses of an anti-HIV monoclonal antibody, VRC01, administered to HIV-uninfected adults: Results of a phase 1 randomized trial
- HIV prevalence and behavioral and psychosocial factors among transgender women and cisgender men who have sex with men in 8 African countries: A cross-sectional analysis
- Treatment eligibility and retention in clinical HIV care: A regression discontinuity study in South Africa
- malERA: An updated research agenda for characterising the reservoir and measuring transmission in malaria elimination and eradication
- Effectiveness of a combination strategy for linkage and retention in adult HIV care in Swaziland: The Link4Health cluster randomized trial
- The value of confirmatory testing in early infant HIV diagnosis programmes in South Africa: A cost-effectiveness analysis
- HIV self-testing among female sex workers in Zambia: A cluster randomized controlled trial
- The US President's Malaria Initiative, transmission and mortality: A modelling study
- Comparison of two cash transfer strategies to prevent catastrophic costs for poor tuberculosis-affected households in low- and middle-income countries: An economic modelling study
- Direct provision versus facility collection of HIV self-tests among female sex workers in Uganda: A cluster-randomized controlled health systems trial
- malERA: An updated research agenda for diagnostics, drugs, vaccines, and vector control in malaria elimination and eradication
- malERA: An updated research agenda for combination interventions and modelling in malaria elimination and eradication
- HIV-1 persistence following extremely early initiation of antiretroviral therapy (ART) during acute HIV-1 infection: An observational study
- Respondent-driven sampling for identification of HIV- and HCV-infected people who inject drugs and men who have sex with men in India: A cross-sectional, community-based analysis
- Extensive virologic and immunologic characterization in an HIV-infected individual following allogeneic stem cell transplant and analytic cessation of antiretroviral therapy: A case study
- Measuring success: The challenge of social protection in helping eliminate tuberculosis
- Prospects for passive immunity to prevent HIV infection
- Reaching global HIV/AIDS goals: What got us here, won't get us there
- Evidence-based restructuring of health and social care
- Extreme exploitation in Southeast Asia waters: Challenges in progressing towards universal health coverage for migrant workers
- PLOS Medicine
- Archiv čísel
- Aktuální číslo
- Informace o časopisu
Nejčtenější v tomto čísle- Postmenopausal hormone therapy and risk of stroke: A pooled analysis of data from population-based cohort studies
- Bioequivalence between innovator and generic tacrolimus in liver and kidney transplant recipients: A randomized, crossover clinical trial
- HIV pre-exposure prophylaxis and early antiretroviral treatment among female sex workers in South Africa: Results from a prospective observational demonstration project
- Bioequivalence of twice-daily oral tacrolimus in transplant recipients: More evidence for consensus?
Kurzy
Zvyšte si kvalifikaci online z pohodlí domova
Současné možnosti léčby obezity
nový kurzAutoři: MUDr. Martin Hrubý
Všechny kurzyPřihlášení#ADS_BOTTOM_SCRIPTS#Zapomenuté hesloZadejte e-mailovou adresu, se kterou jste vytvářel(a) účet, budou Vám na ni zaslány informace k nastavení nového hesla.
- Vzdělávání



