-
Články
Top novinky
Reklama- Vzdělávání
- Časopisy
Top články
Nové číslo
- Témata
Top novinky
Reklama- Videa
- Podcasty
Nové podcasty
Reklama- Kariéra
Doporučené pozice
Reklama- Praxe
Top novinky
ReklamaPostmenopausal hormone therapy and risk of stroke: A pooled analysis of data from population-based cohort studies
In a pooled analysis of data from 3 cohort studies, Karin Leander and colleagues examine the association between postmenopausal hormone therapy and risk of stroke.
Published in the journal: . PLoS Med 14(11): e32767. doi:10.1371/journal.pmed.1002445
Category: Research Article
doi: https://doi.org/10.1371/journal.pmed.1002445Summary
In a pooled analysis of data from 3 cohort studies, Karin Leander and colleagues examine the association between postmenopausal hormone therapy and risk of stroke.
Introduction
Postmenopausal hormone therapy (HT) is recognized as the most effective treatment currently available for menopausal symptoms [1,2]. Nevertheless, findings of a number of observational studies and randomized controlled trials (RCTs) of the influence of HT on stroke risk have been inconsistent [3–9]. A systematic review based on 10 RCTs concluded that oral HT in postmenopausal women increases the risk of stroke [10]. However, subanalyses of this review concluded that there was no strong evidence on risk of stroke according to the timing of initiation of HT [10]. There are recent indications of a favourable influence on subclinical atherosclerosis from HT initiated early, but not late, in relation to onset of menopause [11]; however, the clinical relevance for hard end points such as stroke remains to be determined [12]. The importance of early initiation of HT in relation to stroke risk was addressed in a limited number of previous studies [9,13,14], and the findings were inconsistent. Further, few studies have assessed the influence of HT use on the risk of haemorrhagic stroke, and results have been inconclusive because of the limited number of cases and because timing of HT initiation was not considered [15–18]. In addition, the pathophysiology of haemorrhagic stroke is different from that of the more common ischaemic stroke [19]. Therefore, it seems important to address these conditions separately.
The importance of the route of administration, type, active ingredient, and duration of HT for stroke risk is unclear [10]. To our knowledge, no previous studies have compared the different routes of administration (oral, transdermal, or vaginal) and active ingredients (conjugated equine oestrogens [CEEs] or oestradiol) in relation to stroke risk. Observational studies and RCTs that compared combined (oestrogen and a progestin) and oestrogen-only HT in relation to stroke risk have reported inconsistent results [9,20,21]. The optimal duration of HT from the perspective of stroke risk also remains to be determined [10].
We aimed to assess the association between HT and the risk of developing stroke, considering haemorrhagic stroke separately, while taking into account the timing of initiation of HT in relation to the onset of menopause, route of administration, type of HT, active ingredient, and duration. Our analysis is based on combined data from a large number of postmenopausal women in 5 population-based Swedish cohorts.
Methods
Study design
The Regional Ethical Review Board in Stockholm approved the study, performed in accordance with the principles expressed in the Declaration of Helsinki. Written informed consent was obtained from all study participants. This study is based on the Combined cohorts of menopausal women—Studies of register-based health outcomes in relation to hormonal drugs (COMPREHEND) collaborative effort initiated in 2011. Five cohorts included in COMPREHEND and with available data (from a questionnaire or interviews) on menopausal status, age at menopause onset, use of HT, and age at HT initiation were invited to collaborate in the present study, and all agreed. The cohorts are described below. Baseline investigations were performed between 1987 and 2002, a period during which HT was frequently prescribed.
Description of cohorts
The prospective, population-based Swedish Mammography Cohort (SMC) study was performed between 1 March 1987 and 14 December 1990. All women born during the period 1914–1948 and residing in Västmanland and Uppsala counties in central Sweden were invited to undergo a free mammography examination and complete a questionnaire to collect information about their height, weight, education, diet, and consumption of alcoholic beverages [22]. Of the 90,303 contacted women, a total of 66,651 (74%) completed the questionnaire. In September 1997, the 56,030 women who remained alive and resident in the study counties were sent a second questionnaire to update the original data and to collect further information about reproductive history, history of hypertension and diabetes mellitus and lifestyle factors (including smoking status); 39,227 (70%) of these women completed the second questionnaire [22].
The Northern Sweden Health and Disease Study (NSHDS) comprises 3 population-based subcohorts: the Mammary Screening Cohort (MSC), the Västerbotten Intervention Programme (VIP), and the Monitoring Trends and Determinants in Cardiovascular Disease (MONICA). The MSC was based on mammography screening (85% participation rate) and was initiated in 1995 for all women aged 50–69 years living in Västerbotten county. At screening (1995–2006), the women were also invited to participate in a study of several endemic diseases that included cardiovascular disease (CVD). Overall, 46% completed a questionnaire that was mainly concerning reproductive history; weight, height, and smoking status were also recorded. In the present study, the 27,708 participants in the MSC composed the core cohort, and 19,338 participants from the VIP and 1,053 from the MONICA subcohorts provided further data. A detailed description of the NHSDS has been reported [23].
In the Screening Across the Lifespan Twin (SALT), a substudy of the Swedish Twin Register, data were collected from 44,919 participants using computer-assisted telephone interviews. The SALT cohort consists of twin pairs (dizygotic and monozygotic) born up to 1958, identified from birth records. The interviews were conducted between 1998 and 2002 (73.6% participation rate). DNA analysis was used to determine zygosity for same-sex twins. The SALT study has been described previously [24].
The aim of the prospective, population-based Malmö Diet and Cancer study (MDCS) was to assess associations between cancer and lifestyle factors. The cohort comprises 17,035 women, 45–73 years of age, enrolled between 1991 and 1996 (born 1923–1950), with a participation rate of approximately 40%. Baseline examinations included anthropometric measures (e.g., body mass index), blood collection, a questionnaire to ascertain medications, sociodemographic characteristics, lifestyle, health status, and reproductive factors. Further details have been reported previously [25]. In contrast to the other cohorts, only a proportion (20%) of the women in the MDCS were asked to provide information that enabled the timing of HT initiation to be determined.
All women aged 50–59 years (born 1935–1945) and living in southern Sweden were invited to participate in a health survey as part of the Women’s Health in the Lund Area (WHILA). Between 2 December 1995 and 3 February 2000, a total of 6,916 participants (64% of the overall population of 10,766 women in 1995) underwent a physical examination and completed a questionnaire that included questions about health status, medications, sociodemographic characteristics, and alcohol consumption. Further details have been reported previously [26].
We excluded women with previous CVD, identified from the Swedish National Patient Register, as well as women who were not menopausal and those who were menopausal but reported an age at menopause outside the range of 40–59 years. After also excluding women for whom information on HT use was missing, a total of 88,914 were included in the study (S1 Fig) (i.e., 30,832, 20,108, 18,818, 13,700, and 5,456 from the SMC, NSHDS, SALT, MDCS, and WHILA cohorts, respectively).
Follow-up and definition of end points
Utilizing the Swedish National Patient Register and the Swedish Cause of Death Register, incident cases of stroke (ischaemic, haemorrhagic, or unspecified; International Classification of Diseases [ICD] codes ICD-9 430–434/436–438 and ICD-10 I60–I69) and of haemorrhagic stroke specifically (ICD-9 430–432 and ICD-10 I60–I62) during the follow-up period were identified. In addition, main diagnoses and the underlying causes of death were recorded. The end of follow-up varied between cohorts, from 31 December 2010 to 31 December 2013.
Classification of HT
Women who reported current or previous use of HT were categorized as ever users. Ever users who reported initiating HT within the previous 12 months were categorized as incident users. Early initiation and late HT initiation were defined using a 5-year cutoff as ≤5 and >5 years since menopause onset, respectively, or using a 10-year cutoff (≤10 and >10 years, respectively). The 5-year categorization and the 10-year categorization are the main categories used in previous literature. Therefore, we chose to use both. Considering that the category definitions are arbitrary, we also analysed the timing of initiation of HT as a continuous variable. For additional analyses of early HT initiation, women without available information about age at HT initiation and/or age at menopause onset were classified as early initiators based on their age at baseline: initiation of HT at ≤55 years for the 5-year cut-off and at ≤60 years for the 10-year cut-off.
HT was categorized as oestrogen-only or combined (oestrogen-progestin) HT. Women reporting the use of more than 1 HT medication were classified as users of combined HT if at least 1 of the medications was combined HT or 1 contained oestrogen alone and another contained progestin.
Oestradiol and CEEs were active ingredients of interest. All women who reported using both oestradiol and CEEs or neither of these medications (i.e., only other active ingredients) were excluded from the analysis that considered active ingredient.
Administration was considered to be oral if at least 1 of the medications was administered orally. In the absence of oral HT, administration was considered to be transdermal for at least 1 transdermally administered HT and vaginal in the absence of transdermal administration if 1 or more medications were vaginally administered. Vaginal HT could include creams, tablets, or rings.
The duration of use was classified, arbitrarily, as short (≤5 years) or long (>5 years).
The numbers of women in the various HT categories are shown in S1 Table, with information about data availability in each cohort.
Definition of covariates
Based on age at baseline, 5 categories were defined: <55, 55–59, 60–64, 65–69, and ≥70 years of age. Age at menopause onset was divided into 3 categories: 41–46, 47–52 and 53–58 years of age. The level of education was classified as primary school, high school, or university. Body mass index (weight divided by height squared) was classified as <25, 25–30, or >30 kg/m2. Smoking status was classified as never, former, or current smoker. Parity was categorized as 0–1, 2–3, or ≥4 children and physical activity as low, moderate, or high intensity. Alcohol consumption was classified as low, moderate, or high, and oral contraceptive use as never or ever use.
Dyslipidaemia was ascertained from self-reports at baseline of use of lipid-lowering medication and/or a diagnosis of dyslipidaemia, as well as from the Swedish National Patient Register (ICD-9 code 272; ICD-10 code E78 at admission before the baseline investigation). Diabetes was ascertained from self-reported information at baseline; women who reported treatment with oral medication for diabetes or insulin were categorized as having diabetes. In addition, diabetes was identified using the Swedish National Patient Register (ICD-9 code 250; ICD-10 codes E10–E14). Hypertension was identified from self-reports of use of antihypertensive medication and/or a diagnosis of hypertension and from the Swedish National Patient Register (ICD-9 codes 401–404; ICD-10 codes I10–I13). Anatomical therapeutic chemical classification (ATC) codes considered likely to have been prescribed as medication for hypertension were C02, C03, C07, C08, and C09. Family history of CVD was defined as having at least 1 first-degree relative (parent or sibling) who experienced a myocardial infarct or stroke below the age of 60 years. The sources used to identify dyslipidaemia, diabetes, and hypertension were available for all cohorts, except WHILA (in which the questionnaire did not ask for information on dyslipidaemia).
Statistical analysis
Information from the different cohorts was harmonized and mapped to a common set of variables. Stroke incidence and survival curves were compared between cohorts, before the pooling of data from individual participants in these cohorts, and were found to be fairly homogenous. Kaplan–Meier survival curves for the main exposure categories (early and late initiation and never use) were also plotted and found to be similar across cohorts; the early initiator category always had a better survival outcome (longer time free from a stroke event) than the never use category. The late initiator category sometimes had a better survival outcome than the never use category, but never a better survival outcome than the early initiator group. We considered that it was reasonable to combine the different cohorts, based on the population-based design of all 5 cohorts, the inclusion of women born during the same periods and therefore benefitting from the universal Swedish healthcare system, and the fact that the baseline investigations were all conducted at a time of a high HT prescription rate.
Participants contributed to time at risk from the date of the baseline investigation to the date of the first stroke (or haemorrhagic stroke where appropriate), the date of death from other causes, or the end of follow-up, whichever occurred first. Censored quantile regression, implemented using a Laplace regression [27] estimator, was applied to assess the potential associations between HT use and both incident stroke and haemorrhagic stroke, calculating the fifth percentile differences (PDs) and 95% confidence intervals (CIs). For the analysis of haemorrhagic stroke, the first PD was calculated instead. We calculated adjusted survival curves by estimating a grid of quantiles. The percentiles that could be reasonably estimated were selected based on the proportion of individuals with an event (i.e., those who were diagnosed with the disease) during the follow-up period; the proportions were 7.2% and 1.2% of the study population for stroke and haemorrhagic stroke, respectively. Estimating percentiles greater than the fifth for stroke and greater than the first for haemorrhagic stroke would require extrapolation beyond the range of observed data [28]. For analysis of the short-term risk of stroke associated with incident HT use, we also estimated the 0.5% PD, which roughly corresponds to the first 1.5 years of follow-up.
Laplace regression [27] is 1 of several techniques [29–31] for implementing censored quantile regression. It assumes that the outcome follows an asymmetric Laplace distribution but performs well under different data distributions. The technique provides robust estimates of the quantile regression coefficients [27,32].
For all analyses in the present study, the reference category was never users. The timing of HT initiation, as a continuous variable, was included in the regression models using restricted cubic splines with knots at the quartiles.
For several reasons, we decided to use Laplace regression rather than the more usual Cox regression. First, the hazard ratios (HRs) from Cox regression provide an overall estimate of relative risks based on assumptions of proportionality of hazards; in addition, less detailed information is available than from appropriately adjusted survival curves [33] such as estimates from Laplace regression [27,34]. Secondly, the use of survival curves enables better visualization of the results.
In order to calculate survival curves, a grid of percentiles (p1, p2, …) was estimated, and the estimated percentiles were plotted on the x-axis against the corresponding survival values given by (1 − p1), (1 − p2), …, on the y-axis. This approach is similar to creating Kaplan–Meier survival curves; however, an important difference is that estimates can be adjusted for covariates.
PDs are interpreted as follows. As an example, assuming that the fifth PD between groups A and B is 3 years, the survival curve of group A will take 3 years longer than that of group B to drop from 100% to 95%. In other words, the horizontal difference between the 2 curves, when survival is 95%, is 3 years (S2 Fig). In the results section, we referred generically to stroke-free period or haemorrhagic stroke-free period to indicate the percentiles or PDs. A PD point estimate of 0 corresponds to no difference in the disease-free period between the exposed and the reference group; thus, it is interpreted as a null result (corresponding to a HR of 1.0 had Cox regression been used).
We computed Kaplan–Meier curves describing the cumulative incidence of stroke and haemorrhagic stroke, respectively, cross stratifying by timing of HT initiation (using a 5-year cutoff) and each of the following variables: (1) age at baseline, (2) age at menopause onset, (3) level of education, (4) smoking status, (5) body mass index, (6) level of physical activity, (7) type of menopause, (8) parity, (9) use of oral contraceptives, (10) alcohol consumption, (11) presence of hypertension, (12) presence of dyslipidaemia, (13) presence of diabetes, (14) family history of CVD, and (15) cohort. Any marked differences between categories of these variables, as assessed visually, were further examined for potential confounding. The variables listed as 2–15 above were incorporated one at a time into crude models (adjusted only for age at baseline) for stroke and haemorrhagic stroke, respectively, separately modelling early and late HT initiation in relation to the outcome, to assess any substantial influence on the PD point estimates. The variables selected for inclusion in the final multivariable-adjusted model followed a prespecified criteria-based approach chosen on the basis of previous reports, visual inspection of the Kaplan–Meier curves, and any change ≥10% of the PD point estimates. Variables included in the final adjusted Laplace models were age at baseline, level of education, smoking status, body mass index, level of physical activity, and age at menopause onset.
A sensitivity analysis was conducted excluding 1 of each pair of twins in the SALT cohort to assess the robustness of the results. Of note, close relatives cannot be regarded as being sampled independently. In the case of monozygotic female twins as well as dizygotic twins who were both female, only 1 twin from each pair was included, randomly selected if both twins were either HT users or never users or otherwise the twin reporting HT use.
The Kaplan–Meier estimator was used to conduct further sensitivity analyses to examine whether stroke and haemorrhagic stroke associations varied between participants for whom detailed information on timing of HT initiation was or was not available. We also performed a complete case analysis, as a sensitivity analysis, to determine whether the exclusion of individuals due to missing values in the multivariable-adjusted final models is random.
All tests were 2-sided; a P value of 0.05 was considered statistically significant. Stata release 14 was used for all analyses. A prespecified analysis plan (S1 Text) was followed before first submission of the manuscript. After the peer-review process, a complete case analysis was added to address the issue of randomness of dropout due to missing data on covariates. Further, cohort as a covariate was added to the list of potential confounders evaluated (S2 Text).
This study is reported as per STROBE reporting guidelines (S1 STROBE Checklist).
Results
Overall, 6,371 of the 88,914 (7%) postmenopausal women experienced an incident stroke over a median follow-up of 14.3 years. Altogether, 1,080 (17%) of these events were haemorrhagic stroke. The characteristics of study participants by HT use categories are shown in Table 1.
Tab. 1. Baseline characteristics of the postmenopausal women included in the present study of the Combined cohorts of menopausal women—Studies of register-based health outcomes in relation to hormonal drugs (COMPREHEND) material. 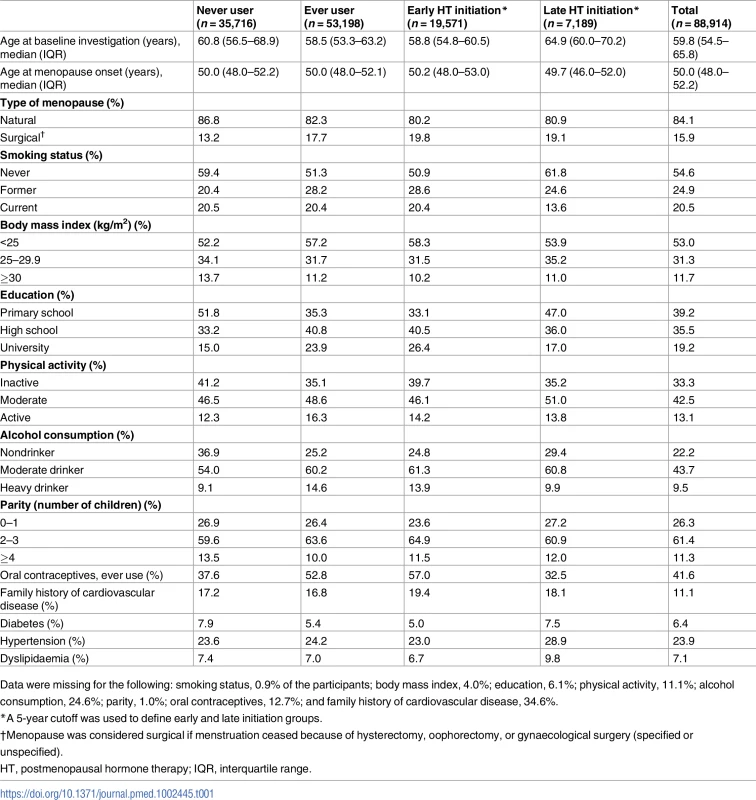
Data were missing for the following: smoking status, 0.9% of the participants; body mass index, 4.0%; education, 6.1%; physical activity, 11.1%; alcohol consumption, 24.6%; parity, 1.0%; oral contraceptives, 12.7%; and family history of cardiovascular disease, 34.6%. As shown in S2 Table, oestrogen-only HT and the vaginal route of administration, without taking into account timing of initiation, were associated with a longer stroke-free period than never use. Stroke and haemorrhagic stroke survival curves for route of administration are shown in S3 Fig. The remaining analyses presented in S2 Table show stroke-free or haemorrhagic stroke-free periods similar to those of never users or with wide CIs.
Results from analyses taking into account timing of HT initiation, employing the 5-year cutoff, are shown in Fig 1. The exact point estimate and confidence interval limits for each result are shown in S3 Table, which also includes results from analyses that employed the 10-year cutoff.
Fig. 1. 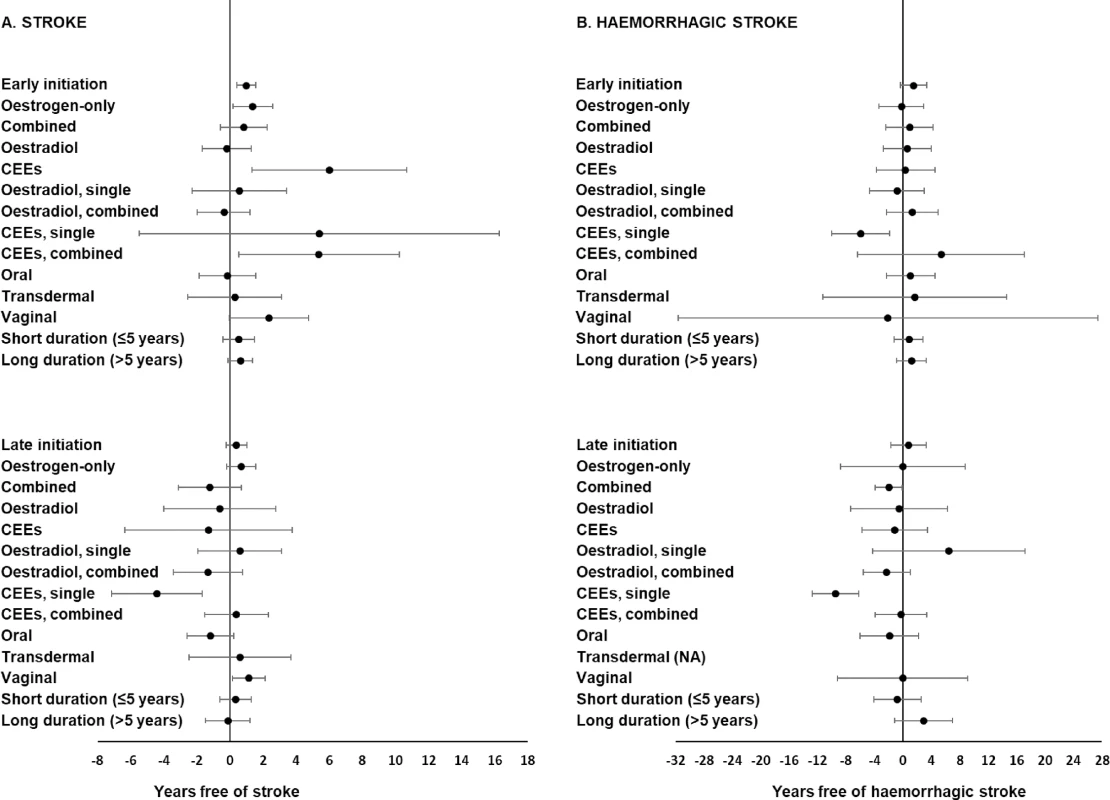
<b>Associations between multivariable-adjusted stroke-free (A) and haemorrhagic stroke-free (B) periods (percentile differences) and various categories of postmenopausal hormone therapy (HT) by timing of initiation using a 5-year cutoff.</b> The reference group is never use. The adjusted models included age at baseline, level of education (primary school, high school, or university), smoking status (never, former, or current), body mass index (<25, 25–29, or ≥30 kg/m<sup>2</sup>), level of physical activity (low, moderate, or high), and age at menopause onset (41–46, 47–52, or 53–58 years). The fifth and first percentile differences with 95% confidence intervals were calculated for stroke and haemorrhagic stroke, respectively. Note that the scale of the x-axis is different for stroke and haemorrhagic stroke. CEE, conjugated equine oestrogen; NA, not applicable, due to 0 haemorrhagic stroke cases among users of transdermal HT. Analyses of both the timing of initiation and the type of HT revealed that early initiation of oestrogen-only HT was associated with a longer stroke-free period (Fig 1A). When initiated late with regard to menopause onset, combined HT use was associated with a shorter stroke-free (Fig 1A) and haemorrhagic stroke-free (Fig 1B, S3 Table) period than never use, although this finding was not statistically significant for stroke, regardless use of the 5-year or the 10-year cutoff. All other associations related to both timing of initiation and type of HT for stroke and haemorrhagic stroke were null or inconclusive (Fig 1 and S3 Table).
Simultaneous consideration of the timing of HT initiation and the active ingredient revealed that, if initiated early, CEE therapy was associated with a longer stroke-free period compared with never use (Fig 1A). Other analyses of HT timing and active ingredient showed stroke-free and haemorrhagic stroke-free periods similar to those of the never user group (Fig 1 and S3 Table).
Simultaneously considering the timing of HT initiation, the type, and the active ingredient showed that users of combined CEEs, if initiated early, had a longer stroke-free period than never users (Fig 1A and S3 Table); corresponding findings for haemorrhagic stroke were inconclusive (Fig 1B and S3 Table). Users of early, single CEE therapy had a shorter haemorrhagic stroke-free (Fig 1B) period than never users; corresponding findings for stroke were observed, but only when using the 10-year cutoff (S3 Table). The late use of single CEE therapy was associated with shorter stroke-free (Fig 1A) and haemorrhagic stroke-free (Fig 1B) periods; a shorter haemorrhagic stroke-free period was also observed for late use of combined oestradiol, but only when the 10-year cut-off was used (S3 Table). All other analyses of timing of initiation, HT type, and active ingredient produced PDs similar to those of never users or PD values with wide CIs (Fig 1 and S3 Table).
Analyses of both the route of administration and the timing of HT initiation showed that vaginal HT, regardless of its timing of initiation, was associated with a longer stroke-free period, although results were not statistically significant for early initiation (Fig 1A and S3 Table). Early initiation of vaginal HT was associated with a longer haemorrhagic stroke-free period when the 10-year cutoff was used (S3 Table). Other analyses of the route and timing of HT showed stroke-free and haemorrhagic stroke-free periods similar to those of never users or point estimates with wide CIs (Fig 1 and S3 Table). Results for haemorrhagic stroke concerning transdermal HT when initiated late could not be produced due to 0 cases among the users of transdermal HT.
Analyses of both the duration and the timing of initiation of HT provided null results (Fig 1 and S3 Table).
Early HT initiation, using the 5-year cutoff, was associated with a significantly longer stroke-free (Fig 1 and Fig 2A) period, but not with a significantly longer haemorrhagic stroke-free (Fig 1 and Fig 2B) period, than never use, after multivariable adjustments. When considering timing as a continuous variable, the stroke-free and haemorrhagic stroke-free periods were maximal if HT was initiated approximately 0–5 years from the onset of menopause (Fig 3A and 3B).
Fig. 2. 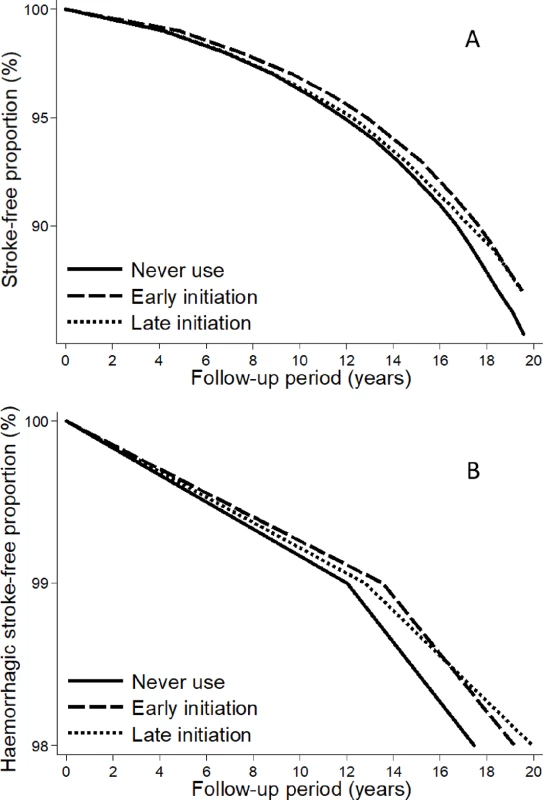
<b>Stroke (A) and haemorrhagic stroke (B) survival curves for early or late initiation, using the 5-year cutoff, of postmenopausal hormone therapy and never use.</b> The curves were computed using censored quantile regression adjusted for age at baseline, level of education, smoking status, body mass index, level of physical activity, and age at menopause onset. Fig. 3. 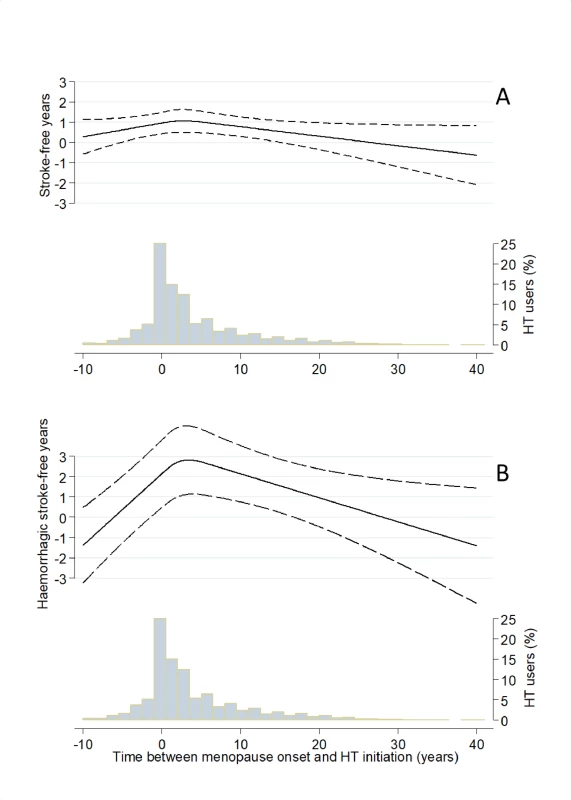
<b>Percentile difference (PD) between users and never users, modelled as a function of time of postmenopausal hormone therapy (HT) initiation using restricted cubic splines and adjusting for age at baseline, level of education, smoking status, body mass index, level of physical activity, and age at menopause onset: fifth PD of time-to-stroke (A) and first PD of time-to-haemorrhagic stroke (B</b>). Dashed lines represent pointwise 95% confidence intervals. The histograms illustrate the underlying distribution of timing of HT initiation. From (B), it can be seen that the PD between users and never users is at its maximum (about 3) when the time between menopause onset and HT initiation is approximately 5 years. The results from the complete cases analysis revealed no pronounced discrepancies between crude results based on complete versus noncomplete cases (S4 Table).
In a sensitivity analysis, women without detailed information on timing of HT initiation were allocated to the early initiator groups based on their age at baseline for both the 5-year and 10-year cutoffs. The results from analyses based on these groups (S5 Table) generally support the interpretations of the main results shown in S3 Table. However, for single CEE therapy in relation to haemorrhagic stroke, results from the sensitivity analysis were inconclusive.
A comparison of results from analyses restricted to women with detailed information on timing and from analyses without this restriction showed no clear differences in either stroke risk or haemorrhagic stroke risk.
Analyses of incident use of HT (based on the 0.5% PD) did not show signs of elevated short-term stroke risk regardless of the timing of initiation, type, active ingredient, and route of administration of HT (S6 Table).
The sensitivity analysis including twins selected from the SALT cohort provided similar results to those obtained in the total study population (S7 Table).
Discussion
In this population-based analysis of pooled individual participant data from more than 88,000 postmenopausal women, we observed no increased risk of stroke associated with HT when initiated <5 years since menopause onset. Overall, this finding persisted when the study outcome was restricted to haemorrhagic stroke. However, we observed increased risks of stroke and haemorrhagic stroke associated with late initiation of HT if it was administered with single CEE as the active ingredient. HT initiated late with regard to menopause onset and used in combination with a progestin was associated with an increased risk of haemorrhagic stroke only. Single CEE therapy was associated with an increased risk of haemorrhagic stroke regardless of timing of initiation.
Our finding that HT users had a similar stroke risk compared to never users is in agreement with the results from some observational studies [18], as well as from 2 RCTs: the Heart and Estrogen/Progestin Replacement Study (HERS) [3] and the Women's Estrogen for Stroke Trial (WEST) [4]. By contrast, the Nurses' Health Study (NHS) [20] and the Women's Health Initiative (WHI) [21,35] reported an increased risk of stroke, although neither timing of HT initiation nor regimens other than oral CEE therapy were considered. In all these studies—except WEST [4], in which a composite end point of ischaemic stroke and transient ischaemic attack was used—stroke was analysed as a composite end point of ischaemic stroke and haemorrhagic stroke.
Our findings on early HT initiation are not in agreement with those reported from a reanalysis of the NHS, where a positive association between HT (when initiated within 4 years from menopause onset) and stroke was observed: relative risk (RR) 1.29 (95% CI 1.06–1.58) and 1.22 (95% CI 0.95–1.55) for CEEs used as single and combined HT, respectively [14]. Reanalysis of the WHI [13] suggested that stroke risk did not depend on years since menopause at the time of HT initiation, but the results were not definite: HR 2.24 (95% CI 0.92–5.44) and 1.58 (95% CI 0.81–3.05) for oestrogen-only and combined HT, respectively, initiated within 10 years after the onset of menopause [13]. Our findings are in agreement with those from the Danish Osteoporosis Prevention Study (DOPS), in which women who had recently undergone menopause and were randomly assigned to receive combined treatment with oestradiol did not exhibit an increased risk of stroke (HR 0.77 [95% CI 0.35–1.70]) [9].
Our findings regarding late initiation of HT agree with results from the reanalysis of the NHS that showed an enhanced risk of stroke in association with CEEs as single therapy when initiated >10 years after menopause onset (RR 1.31 [95% CI 1.06–1.63]); the results regarding combined HT were not statistically significant (RR 1.18 [95% CI 0.87–1.60]) [14]. Reanalysis of the WHI indicated an enhanced risk of stroke in association with oestrogen-only (HR 1.47 [95% CI 0.92–2.35]) and combined CEEs (HR 1.12 [95% CI 0.76–1.64]) when initiated >10 years after the onset of menopause. Our finding that CEEs, but not oestradiol, were associated with an increased stroke risk in some analyses may reflect thrombotic effects exerted by CEEs [36,37]. In all of the aforementioned studies addressing the timing of HT initiation, women could not be precisely allocated into early and late HT initiation groups; allocation was based on age rather than detailed information on timing [10,13,14].
The majority of studies on HT and stroke risk have considered only oral administration [3,4,14,18,21]. However, among the different routes of administration, transdermal HT has been postulated as safer compared to oral HT with regard to stroke risk [38–41]. It was recently reported that oral oestrogen (odds ratio [OR] 1.58 [95% CI 1.01–2.49]), but not transdermal oestrogen (OR 0.83 [95% CI 0.56–1.24]), was associated with increased risk of ischaemic stroke [40]. In a register-based study that assessed vaginal HT, a reduced risk of death from stroke was reported [42]. To our knowledge, the present study is the first to investigate different routes of administration (oral, transdermal, and vaginal) while simultaneously considering the timing of HT initiation in relation to menopause onset.
Previous observational studies that analysed the association between oral HT and haemorrhagic stroke showed discrepant results [15–17,41]. To our knowledge, this is the first study to perform analyses considering the influence of the timing of HT initiation on the association between HT and haemorrhagic stroke. The reason for selecting haemorrhagic stroke as a separate end point was that stroke is a heterogeneous disease [43] with a complex pathogenesis [19]. Most previous studies analysed a stroke composite end point, probably due to an inability to analyse haemorrhagic stroke separately because of a limited number of clinical events. The results we observed for haemorrhagic stroke did not differ markedly from those for the composite end point, the latter mainly reflecting results for ischaemic stroke.
Strengths and limitations
The present prospective study has important advantages, including the use of national high-quality registers, which provides the opportunity to follow cohort participants over time essentially without loss to follow-up, as well as valid identification of incident stroke and haemorrhagic stroke [44]. The detailed and extensive data available from the cohort participants enabled comprehensive analysis and control of potential confounding factors, including 15 different variables, most of them commonly used in previous literature. The detailed information on the timing of HT initiation provided by more than 26,000 HT users is unique. The present study considered more aspects of HT (time of initiation, type of therapy, route of administration, active ingredient, and duration) than did most previous studies in this area. Our findings should be generalizable across different geographical regions considering our population-based design, the large sample size, and a high internal validity. Finally, the large sample size allowed us to use novel statistical modelling methods suitable for addressing our research questions, with the results reported in a manner that may be more intuitive to interpret than that of standard methods [27,28].
Because of the observational design of this study, the possibility of uncontrolled confounding cannot be ruled out. It is likely that women who used HT during the time period of our baseline investigations were in general more health conscious and had a higher socioeconomic position [45]. However, various lifestyle factors as well as body mass index and level of education were considered. Although the presence of missing data on covariates could have influenced the results, the missing proportions for the variables included in our final adjusted model only varied between 0.9% and 11.1%. Furthermore, complete case analyses revealed no signs of selection bias. Although the possibility of immortal time bias, related to the observational design of the study [46], cannot be completely excluded, our results from analysis restricted to incident use do not support such bias. We have no information regarding whether or not women switched from exposed to unexposed status after the baseline investigations. This is a limitation that may have influenced our results, most probably towards a dilution.
Another limitation of our study is that we did not have detailed information about either the HT dose or the type of progestin used in the combined therapy, both of which have been discussed regarding a potential effect on stroke risk [14,40]. It is possible that our results concerning CEE when initiated late in relation to menopause onset would have been less pronounced had a lower dose been used. The recommended HT dose used in Sweden at the time when the women in our study were treated was 0.625 mg/day for CEE, 1–2 mg/day for oral oestradiol, and 50–100 μg/day for transdermal oestradiol [47]. The progestins predominantly used in Sweden during this period were nortestosterones (e.g., norethisterone acetate, levonorgestrel, and dionegest), although pregnanes (e.g., medroxyprogesterone acetate) were also used. Considering that derivatives of norpregnane, the progestin found to be associated with increased risk of ischaemic stroke in a previous study [40], were not frequently used in our study [48], the type of progestin is unlikely to explain our observed association between combined HT and risk of haemorrhagic stroke.
Conclusion
HT was associated with a reduced or null risk of future stroke if initiated relatively soon after the onset of menopause, regardless of regimen (type, active ingredient, and route of administration) and duration. This finding was extended to haemorrhagic stroke, excepting use of CEEs as single therapy. However, when HT was initiated late with regard to menopause onset, an increased risk was observed for stroke and haemorrhagic stroke when CEEs were used as single therapy. Combined therapy initiated late was associated with increased risk of haemorrhagic stroke only.
Based on both our results and the available evidence from previous studies, we conclude that HT is not associated with increased stroke risk, if therapy is initiated soon after menopause onset. Our results suggest that the initiation of HT 0–5 years after menopause onset, as compared to never use, is associated with a decreased risk of stroke and haemorrhagic stroke.
Supporting Information
Zdroje
1. Manson JE, Kaunitz AM. Menopause Management—Getting Clinical Care Back on Track. N Engl J Med. 2016;374(9):803–6. Epub 2016/03/11. doi: 10.1056/NEJMp1514242 26962899.
2. Formoso G, Perrone E, Maltoni S, Balduzzi S, Wilkinson J, Basevi V, et al. Short-term and long-term effects of tibolone in postmenopausal women. The Cochrane database of systematic reviews. 2016;10:CD008536. doi: 10.1002/14651858.CD008536.pub3 27733017.
3. Simon JA, Hsia J, Cauley JA, Richards C, Harris F, Fong J, et al. Postmenopausal hormone therapy and risk of stroke: The Heart and Estrogen-progestin Replacement Study (HERS). Circulation. 2001;103(5):638–42. 11156873.
4. Viscoli CM, Brass LM, Kernan WN, Sarrel PM, Suissa S, Horwitz RI. A clinical trial of estrogen-replacement therapy after ischemic stroke. The New England journal of medicine. 2001;345(17):1243–9. doi: 10.1056/NEJMoa010534 11680444.
5. Grady D, Herrington D, Bittner V, Blumenthal R, Davidson M, Hlatky M, et al. Cardiovascular disease outcomes during 6.8 years of hormone therapy: Heart and Estrogen/progestin Replacement Study follow-up (HERS II). JAMA. 2002;288(1):49–57. Epub 2002/07/02. joc20521 [pii]. 12090862.
6. Rossouw JE, Anderson GL, Prentice RL, LaCroix AZ, Kooperberg C, Stefanick ML, et al. Risks and benefits of estrogen plus progestin in healthy postmenopausal women: principal results From the Women's Health Initiative randomized controlled trial. JAMA. 2002;288(3):321–33. Epub 2002/07/19. joc21036 [pii]. 12117397.
7. Anderson GL, Limacher M, Assaf AR, Bassford T, Beresford SA, Black H, et al. Effects of conjugated equine estrogen in postmenopausal women with hysterectomy: the Women's Health Initiative randomized controlled trial. JAMA. 2004;291(14):1701–12. Epub 2004/04/15. doi: 10.1001/jama.291.14.1701 291/14/1701 [pii]. 15082697.
8. Veerus P, Hovi SL, Fischer K, Rahu M, Hakama M, Hemminki E. Results from the Estonian postmenopausal hormone therapy trial [ISRCTN35338757]. Maturitas. 2006;55(2):162–73. Epub 2006/03/01. S0378-5122(06)00058-2 [pii]. doi: 10.1016/j.maturitas.2006.01.012 16504428.
9. Schierbeck LL, Rejnmark L, Tofteng CL, Stilgren L, Eiken P, Mosekilde L, et al. Effect of hormone replacement therapy on cardiovascular events in recently postmenopausal women: randomised trial. BMJ. 2012;345:e6409. Epub 2012/10/11. doi: 10.1136/bmj.e6409 bmj.e6409 [pii]. 23048011.
10. Boardman HM, Hartley L, Eisinga A, Main C, Roque i Figuls M, Bonfill Cosp X, et al. Hormone therapy for preventing cardiovascular disease in post-menopausal women. Cochrane Database Syst Rev. 2015;(3):CD002229. doi: 10.1002/14651858.CD002229.pub4 25754617.
11. Hodis HN, Mack WJ, Henderson VW, Shoupe D, Budoff MJ, Hwang-Levine J, et al. Vascular Effects of Early versus Late Postmenopausal Treatment with Estradiol. N Engl J Med. 2016;374(13):1221–31. doi: 10.1056/NEJMoa1505241 27028912; PubMed Central PMCID: PMCPMC4921205.
12. Keaney JF Jr., Solomon CG. Postmenopausal Hormone Therapy and Atherosclerosis—Time Is of the Essence. N Engl J Med. 2016;374(13):1279–80. Epub 2016/03/31. doi: 10.1056/NEJMe1602846 27028919.
13. Rossouw JE, Prentice RL, Manson JE, Wu L, Barad D, Barnabei VM, et al. Postmenopausal hormone therapy and risk of cardiovascular disease by age and years since menopause. JAMA. 2007;297(13):1465–77. doi: 10.1001/jama.297.13.1465 17405972.
14. Grodstein F, Manson JE, Stampfer MJ, Rexrode K. Postmenopausal hormone therapy and stroke: role of time since menopause and age at initiation of hormone therapy. Arch Intern Med. 2008;168(8):861–6. doi: 10.1001/archinte.168.8.861 18443262; PubMed Central PMCID: PMCPMC4001717.
15. Longstreth WT, Nelson LM, Koepsell TD, van Belle G. Subarachnoid hemorrhage and hormonal factors in women. A population-based case-control study. Ann Intern Med. 1994;121(3):168–73. 8017743.
16. Pedersen AT, Lidegaard O, Kreiner S, Ottesen B. Hormone replacement therapy and risk of non-fatal stroke. Lancet. 1997;350(9087):1277–83. doi: 10.1016/S0140-6736(97)06005-4 9357407.
17. Schairer C, Adami HO, Hoover R, Persson I. Cause-specific mortality in women receiving hormone replacement therapy. Epidemiology. 1997;8(1):59–65. 9116097.
18. Paganini-Hill A. Hormone replacement therapy and stroke: risk, protection or no effect? Maturitas. 2001;38(3):243–61. 11358642.
19. Sacco RL, Kasner SE, Broderick JP, Caplan LR, Connors JJ, Culebras A, et al. An updated definition of stroke for the 21st century: a statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2013;44(7):2064–89. doi: 10.1161/STR.0b013e318296aeca 23652265.
20. Grodstein F, Manson JE, Colditz GA, Willett WC, Speizer FE, Stampfer MJ. A prospective, observational study of postmenopausal hormone therapy and primary prevention of cardiovascular disease. Annals of internal medicine. 2000;133(12):933–41. 11119394.
21. Hendrix SL, Wassertheil-Smoller S, Johnson KC, Howard BV, Kooperberg C, Rossouw JE, et al. Effects of conjugated equine estrogen on stroke in the Women's Health Initiative. Circulation. 2006;113(20):2425–34. doi: 10.1161/CIRCULATIONAHA.105.594077 16702472.
22. Wolk A, Larsson SC, Johansson JE, Ekman P. Long-term fatty fish consumption and renal cell carcinoma incidence in women. JAMA. 2006;296(11):1371–6. doi: 10.1001/jama.296.11.1371 16985229.
23. Hallmans G, Agren A, Johansson G, Johansson A, Stegmayr B, Jansson JH, et al. Cardiovascular disease and diabetes in the Northern Sweden Health and Disease Study Cohort—evaluation of risk factors and their interactions. Scand J Public Health Suppl. 2003;61 : 18–24. doi: 10.1080/14034950310001432 14660243.
24. Lichtenstein P, De Faire U, Floderus B, Svartengren M, Svedberg P, Pedersen NL. The Swedish Twin Registry: a unique resource for clinical, epidemiological and genetic studies. J Intern Med. 2002;252(3):184–205. 12270000.
25. Manjer J, Carlsson S, Elmstahl S, Gullberg B, Janzon L, Lindstrom M, et al. The Malmo Diet and Cancer Study: representativity, cancer incidence and mortality in participants and non-participants. Eur J Cancer Prev. 2001;10(6):489–99. 11916347.
26. Samsioe G, Lidfeldt J, Nerbrand C, Nilsson P. The women's health in the Lund area (WHILA) study—an overview. Maturitas. 2010;65(1):37–45. doi: 10.1016/j.maturitas.2009.11.009 19962255.
27. Bottai M, Zhang J. Laplace regression with censored data. Biom J. 2010;52(4):487–503. doi: 10.1002/bimj.200900310 20680972.
28. Orsini N, Wolk A, Bottai M. Evaluating percentiles of survival. Epidemiology. 2012;23(5):770–1. doi: 10.1097/EDE.0b013e3182625eff 22872120.
29. Austin PC, Schull MJ. Quantile regression: a statistical tool for out-of-hospital research. Acad Emerg Med. 2003;10(7):789–97. 12837655.
30. Reich BJ, Bondell HD, Wang HJ. Flexible Bayesian quantile regression for independent and clustered data. Biostatistics. 2010;11(2):337–52. doi: 10.1093/biostatistics/kxp049 19948746.
31. Frumento P, Bottai M. Parametric modeling of quantile regression coefficient functions. Biometrics. 2016;72(1):74–84. doi: 10.1111/biom.12410 26394132.
32. Bottai M, Orsini N, Geraci M. A gradient search maximization algorithm for the asymmetric Laplace likelihood. J Stat Comput Sim. 2015;85(10):1919–25. doi: 10.1080/00949655.2014.908879 WOS:000352642500001.
33. Hernan MA. The hazards of hazard ratios. Epidemiology. 2010;21(1):13–5. doi: 10.1097/EDE.0b013e3181c1ea43 20010207; PubMed Central PMCID: PMCPMC3653612.
34. Bellavia A, Discacciati A, Bottai M, Wolk A, Orsini N. Using Laplace Regression to Model and Predict Percentiles of Age at Death When Age Is the Primary Time Scale. Am J Epidemiol. 2015;182(3):271–7. doi: 10.1093/aje/kwv033 26093508.
35. Wassertheil-Smoller S, Hendrix SL, Limacher M, Heiss G, Kooperberg C, Baird A, et al. Effect of estrogen plus progestin on stroke in postmenopausal women: the Women's Health Initiative: a randomized trial. Jama. 2003;289(20):2673–84. doi: 10.1001/jama.289.20.2673 12771114.
36. Smith NL, Blondon M, Wiggins KL, Harrington LB, van Hylckama Vlieg A, Floyd JS, et al. Lower risk of cardiovascular events in postmenopausal women taking oral estradiol compared with oral conjugated equine estrogens. JAMA Intern Med. 2014;174(1):25–31. doi: 10.1001/jamainternmed.2013.11074 24081194; PubMed Central PMCID: PMCPMC4636198.
37. Blondon M, van Hylckama Vlieg A, Wiggins KL, Harrington LB, McKnight B, Rice KM, et al. Differential associations of oral estradiol and conjugated equine estrogen with hemostatic biomarkers. J Thromb Haemost. 2014;12(6):879–86. doi: 10.1111/jth.12560 24628832; PubMed Central PMCID: PMCPMC5371691.
38. Lisabeth L, Bushnell C. Stroke risk in women: the role of menopause and hormone therapy. The Lancet Neurology. 2012;11(1):82–91. doi: 10.1016/S1474-4422(11)70269-1 22172623; PubMed Central PMCID: PMC3615462.
39. Renoux C, Dell'aniello S, Garbe E, Suissa S. Transdermal and oral hormone replacement therapy and the risk of stroke: a nested case-control study. Bmj. 2010;340:c2519. doi: 10.1136/bmj.c2519 20525678.
40. Canonico M, Carcaillon L, Plu-Bureau G, Oger E, Singh-Manoux A, Tubert-Bitter P, et al. Postmenopausal Hormone Therapy and Risk of Stroke: Impact of the Route of Estrogen Administration and Type of Progestogen. Stroke. 2016;47(7):1734–41. doi: 10.1161/STROKEAHA.116.013052 27256671; PubMed Central PMCID: PMCPMC4927222.
41. Sare GM, Gray LJ, Bath PM. Association between hormone replacement therapy and subsequent arterial and venous vascular events: a meta-analysis. Eur Heart J. 2008;29(16):2031–41. doi: 10.1093/eurheartj/ehn299 18599555; PubMed Central PMCID: PMCPMC2515884.
42. Mikkola TS, Tuomikoski P, Lyytinen H, Korhonen P, Hoti F, Vattulainen P, et al. Vaginal estradiol use and the risk for cardiovascular mortality. Human reproduction. 2016;31(4):804–9. doi: 10.1093/humrep/dew014 26874358.
43. Amarenco P, Bogousslavsky J, Caplan LR, Donnan GA, Hennerici MG. Classification of stroke subtypes. Cerebrovascular diseases. 2009;27(5):493–501. doi: 10.1159/000210432 19342825.
44. Ludvigsson JF, Almqvist C, Bonamy AK, Ljung R, Michaelsson K, Neovius M, et al. Registers of the Swedish total population and their use in medical research. European journal of epidemiology. 2016;31(2):125–36. doi: 10.1007/s10654-016-0117-y 26769609.
45. Ray WA. Evaluating medication effects outside of clinical trials: new-user designs. Am J Epidemiol. 2003;158(9):915–20. 14585769.
46. Hernan MA, Sauer BC, Hernandez-Diaz S, Platt R, Shrier I. Specifying a target trial prevents immortal time bias and other self-inflicted injuries in observational analyses. J Clin Epidemiol. 2016;79 : 70–5. doi: 10.1016/j.jclinepi.2016.04.014 27237061; PubMed Central PMCID: PMCPMC5124536.
47. Brandt C, Beermann B, Jansson-Delslind B. Information från läkemedelsverket: Medical Products Agency in Sweden; 2001. Available from: https://lakemedelsverket.se/upload/om-lakemedelsverket/publikationer/information-fran-lakemedelsverket/Info_fr_LV_2001-5.pdf
48. Stjernquist M. Nya amerikanska rekommendationer för hormonbehandling i klimakteriet: Läkartidningen; 2003. Available from: http://ww2.lakartidningen.se/old/content_0320/pdf/1790_1797.pdf
Štítky
Interní lékařství
Článek Contemporary disengagement from antiretroviral therapy in Khayelitsha, South Africa: A cohort studyČlánek Bioequivalence of twice-daily oral tacrolimus in transplant recipients: More evidence for consensus?
Článek vyšel v časopisePLOS Medicine
Nejčtenější tento týden
2017 Číslo 11- Berberin: přírodní hypolipidemikum se slibnými výsledky
- Léčba bolesti u seniorů
- Příznivý vliv Armolipidu Plus na hladinu cholesterolu a zánětlivé parametry u pacientů s chronickým subklinickým zánětem
- Jak postupovat při výběru betablokátoru − doporučení z kardiologické praxe
- Červená fermentovaná rýže účinně snižuje hladinu LDL cholesterolu jako vhodná alternativa ke statinové terapii
-
Všechny články tohoto čísla
- Labour trafficking: Challenges and opportunities from an occupational health perspective
- The end of HIV: Still a very long way to go, but progress continues
- Contemporary disengagement from antiretroviral therapy in Khayelitsha, South Africa: A cohort study
- Bioequivalence of twice-daily oral tacrolimus in transplant recipients: More evidence for consensus?
- Treatment guidelines and early loss from care for people living with HIV in Cape Town, South Africa: A retrospective cohort study
- Perinatal mortality associated with induction of labour versus expectant management in nulliparous women aged 35 years or over: An English national cohort study
- Core Outcome Set-STAndards for Development: The COS-STAD recommendations
- Closing the gaps in the HIV care continuum
- Association between the 2012 Health and Social Care Act and specialist visits and hospitalisations in England: A controlled interrupted time series analysis
- HIV pre-exposure prophylaxis and early antiretroviral treatment among female sex workers in South Africa: Results from a prospective observational demonstration project
- Sexual exploitation of unaccompanied migrant and refugee boys in Greece: Approaches to prevention
- Child sex trafficking in the United States: Challenges for the healthcare provider
- The expanding epidemic of HIV-1 in the Russian Federation
- Cardiovascular disease (CVD) and chronic kidney disease (CKD) event rates in HIV-positive persons at high predicted CVD and CKD risk: A prospective analysis of the D:A:D observational study
- Validity of a minimally invasive autopsy for cause of death determination in maternal deaths in Mozambique: An observational study
- malERA: An updated research agenda for malaria elimination and eradication
- malERA: An updated research agenda for health systems and policy research in malaria elimination and eradication
- A combination intervention strategy to improve linkage to and retention in HIV care following diagnosis in Mozambique: A cluster-randomized study
- Bioequivalence between innovator and generic tacrolimus in liver and kidney transplant recipients: A randomized, crossover clinical trial
- malERA: An updated research agenda for basic science and enabling technologies in malaria elimination and eradication
- Human trafficking and exploitation: A global health concern
- Virological response and resistance among HIV-infected children receiving long-term antiretroviral therapy without virological monitoring in Uganda and Zimbabwe: Observational analyses within the randomised ARROW trial
- Postmenopausal hormone therapy and risk of stroke: A pooled analysis of data from population-based cohort studies
- Lansoprazole use and tuberculosis incidence in the United Kingdom Clinical Practice Research Datalink: A population based cohort
- malERA: An updated research agenda for insecticide and drug resistance in malaria elimination and eradication
- Safety, pharmacokinetics, and immunological activities of multiple intravenous or subcutaneous doses of an anti-HIV monoclonal antibody, VRC01, administered to HIV-uninfected adults: Results of a phase 1 randomized trial
- HIV prevalence and behavioral and psychosocial factors among transgender women and cisgender men who have sex with men in 8 African countries: A cross-sectional analysis
- Treatment eligibility and retention in clinical HIV care: A regression discontinuity study in South Africa
- malERA: An updated research agenda for characterising the reservoir and measuring transmission in malaria elimination and eradication
- Effectiveness of a combination strategy for linkage and retention in adult HIV care in Swaziland: The Link4Health cluster randomized trial
- The value of confirmatory testing in early infant HIV diagnosis programmes in South Africa: A cost-effectiveness analysis
- HIV self-testing among female sex workers in Zambia: A cluster randomized controlled trial
- The US President's Malaria Initiative, transmission and mortality: A modelling study
- Comparison of two cash transfer strategies to prevent catastrophic costs for poor tuberculosis-affected households in low- and middle-income countries: An economic modelling study
- Direct provision versus facility collection of HIV self-tests among female sex workers in Uganda: A cluster-randomized controlled health systems trial
- malERA: An updated research agenda for diagnostics, drugs, vaccines, and vector control in malaria elimination and eradication
- malERA: An updated research agenda for combination interventions and modelling in malaria elimination and eradication
- HIV-1 persistence following extremely early initiation of antiretroviral therapy (ART) during acute HIV-1 infection: An observational study
- Respondent-driven sampling for identification of HIV- and HCV-infected people who inject drugs and men who have sex with men in India: A cross-sectional, community-based analysis
- Extensive virologic and immunologic characterization in an HIV-infected individual following allogeneic stem cell transplant and analytic cessation of antiretroviral therapy: A case study
- Measuring success: The challenge of social protection in helping eliminate tuberculosis
- Prospects for passive immunity to prevent HIV infection
- Reaching global HIV/AIDS goals: What got us here, won't get us there
- Evidence-based restructuring of health and social care
- Extreme exploitation in Southeast Asia waters: Challenges in progressing towards universal health coverage for migrant workers
- PLOS Medicine
- Archiv čísel
- Aktuální číslo
- Informace o časopisu
Nejčtenější v tomto čísle- Postmenopausal hormone therapy and risk of stroke: A pooled analysis of data from population-based cohort studies
- Bioequivalence between innovator and generic tacrolimus in liver and kidney transplant recipients: A randomized, crossover clinical trial
- HIV pre-exposure prophylaxis and early antiretroviral treatment among female sex workers in South Africa: Results from a prospective observational demonstration project
- Bioequivalence of twice-daily oral tacrolimus in transplant recipients: More evidence for consensus?
Kurzy
Zvyšte si kvalifikaci online z pohodlí domova
Současné možnosti léčby obezity
nový kurzAutoři: MUDr. Martin Hrubý
Všechny kurzyPřihlášení#ADS_BOTTOM_SCRIPTS#Zapomenuté hesloZadejte e-mailovou adresu, se kterou jste vytvářel(a) účet, budou Vám na ni zaslány informace k nastavení nového hesla.
- Vzdělávání



