-
Články
Top novinky
Reklama- Vzdělávání
- Časopisy
Top články
Nové číslo
- Témata
Top novinky
Reklama- Videa
- Podcasty
Nové podcasty
Reklama- Kariéra
Doporučené pozice
Reklama- Praxe
Top novinky
ReklamaAttenuation of Tick-Borne Encephalitis Virus Using Large-Scale Random Codon Re-encoding
The arbovirus Tick-borne encephalitis virus (TBEV; genus Flavivirus) is transmitted by ticks of the Ixodes genus. TBEV causes febrile illness and encephalitis in humans in forested regions of Europe and Asia. The incidence of TBE is increasing across Central and Eastern European countries despite the availability of several licensed inactivated vaccines and appropriate vaccination programmes. Large-scale codon re-encoding, a recently developed attenuation method that modifies viral RNA nucleotide composition of large coding regions without alteration of the encoded proteins, has been successfully applied to a variety of RNA viruses. In contrast with previous empirical methods of generating live attenuated vaccines, large-scale codon re-encoding facilitates rapid generation of vaccine candidates using reverse genetics methods, by direct control of the attenuation phenotype. Additional benefits include reduced costs and induction of long-term immunity. Here, we have applied the large-scale codon re-encoding method to the TBEV to demonstrate the principle of developing a live attenuated virus vaccine which protects mice against subsequent infection with the wild type virulent virus. This study therefore illustrates that codon re-encoding is potentially an easily derived and effective method of producing live attenuated vaccine candidates against positive-stranded RNA viruses.
Published in the journal: . PLoS Pathog 11(3): e32767. doi:10.1371/journal.ppat.1004738
Category: Research Article
doi: https://doi.org/10.1371/journal.ppat.1004738Summary
The arbovirus Tick-borne encephalitis virus (TBEV; genus Flavivirus) is transmitted by ticks of the Ixodes genus. TBEV causes febrile illness and encephalitis in humans in forested regions of Europe and Asia. The incidence of TBE is increasing across Central and Eastern European countries despite the availability of several licensed inactivated vaccines and appropriate vaccination programmes. Large-scale codon re-encoding, a recently developed attenuation method that modifies viral RNA nucleotide composition of large coding regions without alteration of the encoded proteins, has been successfully applied to a variety of RNA viruses. In contrast with previous empirical methods of generating live attenuated vaccines, large-scale codon re-encoding facilitates rapid generation of vaccine candidates using reverse genetics methods, by direct control of the attenuation phenotype. Additional benefits include reduced costs and induction of long-term immunity. Here, we have applied the large-scale codon re-encoding method to the TBEV to demonstrate the principle of developing a live attenuated virus vaccine which protects mice against subsequent infection with the wild type virulent virus. This study therefore illustrates that codon re-encoding is potentially an easily derived and effective method of producing live attenuated vaccine candidates against positive-stranded RNA viruses.
Introduction
The genus Flavivirus (family Flaviviridae) includes important human pathogens such as yellow fever virus (YFV), dengue virus (DENV), Japanese encephalitis virus (JEV), West Nile virus and tick-borne encephalitis virus (TBEV). Flaviviruses are enveloped, single-stranded positive-sense RNA viruses with virions, close to 50nm in diameter, and a viral genome of ca. 11 kb which includes a unique open reading frame (ORF) encoding structural (C-prM-E) and non-structural proteins (NS1–2A-2B-3–4A-4B-5) [1,2]. Some mosquito-borne flaviviruses also harbour sequences that induce a proportion of translating ribosomes to shift-1 nt and continue translating in the new reading frame to produce a ‘transframe’ fusion protein [3,4]. Most flaviviruses are arboviruses and are therefore maintained in nature by circulating between haematophagous arthropod vectors and vertebrate hosts. Arthropod-borne flaviviruses are sub-divided into two major groups: the tick-borne and mosquito-borne flaviviruses (TBFVs and MBFVs respectively) [1,2,5]. TBFVs include a heterogeneous group called seabird tick-borne flavivirus group (S-TBFV) [6] and the mammalian tick-borne flavivirus group (M-TBFV), with all known pathogenic TBFVs causing febrile illness, encephalitis and/or haemorrhagic fever in humans. In the latter group, TBEVs are recognised in 25 European and 7 Asian countries and transmitted by Ixodes species ticks [7]. The TBEVs are subdivided into three sub-types, namely Siberian, Western European and Far Eastern viruses [8,9], the latter being responsible for the most severe forms of central nervous system (CNS) disorders associated with high fatality rates (5–20%) [10]. Despite the availability of several licensed inactivated vaccines and vaccination programmes [1,11], the incidence of TBEV infections is increasing across much of Central and Eastern European countries, currently with an estimated 9,000 cases per year [12,13,14].
Live attenuated vaccines provide effective and affordable protection against major flaviviral infections. One dose of the widely used 17D YF vaccine used since 1937, provides long-lasting immunity [15]. The live attenuated JE vaccine (strain SA-14–14–2) has been successfully used in China with over 100 million children vaccinated [16]. Attenuated strains of virus have been obtained in the past using empirical methods such as serial passage of wild-type (WT) viruses in cell cultures and/or chicken embryos. Whilst several hundred million yellow fever vaccine doses have been administered, and proven to be safe and highly efficacious [16,17], the attenuation mechanism is associated with a number of non-synonymous mutations (31 in the case of the 17D-204 YF vaccine strain when compared with the WT Asibi virus). These modifications can occasionally generate new biological properties, e.g., a neurovirulent phenotype for YF 17D in contrast to the viscerotropic phenotype of WT yellow fever viruses. New approaches to resolve such problems are required.
Large-scale codon re-encoding is a recently developed method with which to attenuate virus by introducing a large number of slightly deleterious synonymous mutations into the protein coding region of the viral genomic RNA without alteration of the encoded proteins. Genomic re-encoding has been successfully applied to a variety of RNA viruses: poliovirus, influenza A virus, chikungunya virus, human respiratory syncytial virus, human immunodeficiency virus, Japanese encephalitis virus and porcine reproductive and respiratory syndrome virus [18,19,20,21,22,23,24,25,26,27]. In each of these examples, re-encoding modulated virus fitness thus generating potential vaccine candidates with antigenically indistinguishable proteins, therefore alleviating the generation of novel and therefore undesirable biological properties. To date, most published studies have utilised specific re-encoding approaches, including codon deoptimisation, codon-pair deoptimisation or increase of CpG/UpA dinucleotide frequency. The choice of these methods is based on the assumption that global modification of the viral genome induces attenuation because synonymous sites have been shaped by genome-wide mutational processes during virus evolution [28]. However, a random re-encoding approach, previously applied in cellulo to the chikungunya virus, also produced an attenuated phenotype without modifying the global properties of the viral genome, thus underlining the role of local constraints that also shape synonymous sites such as secondary structures or interactions between viral RNA and capsid proteins [27,29,30,31]. Therefore, whilst the efficacy of re-encoding methods for attenuating RNA viruses has been widely demonstrated, the precise—and presumably multiple - mechanisms and their respective contributions to attenuation remain to be analysed in more detail. In cellulo experiments showed, for poliovirus, chikungunya virus and bacterial virus T7, that the phenotype of the re-encoded viruses was stable, and that the evolutionary response to re-encoding was compensatory in nature, with very few reversion mutations [22,27,32].
In the present study, we have applied the random large-scale codon re-encoding method to the TBEV Oshima 5–10 strain, isolated in Japan in 1995 [33]. This strain belongs to the Far Eastern TBEV subtype which is characteristically highly neurovirulent for mice [34,35]. Our studies demonstrate that this re-encoded TBEV Oshima 5–10 strain exhibited an attenuated phenotype in vivo and induced robust protective immunity in mice subsequently infected with the WT virus.
Results
An infectious clone derived from the wild-type Oshima 5–10 TBEV strain was constructed using reverse genetics methods (see the Materials and Methods section for more details). This infectious clone was recovered from cell cultures and designated “WT_IC virus”. In addition, a re-encoded “NS5_Reenc_IC virus” was derived from WT_IC virus by substituting a cassette of approximately 1.4kb, in the corresponding NS5 coding region, with the re-encoded counterpart (Fig. 1). We have chosen to introduce mutations into the NS5 coding region because the first re-encoded cassette introduced into the Chikungunya virus, as described in our previous work [27], was located in the nsP4 coding region which also encoded the viral RNA dependent RNA polymerase. This enabled comparisons, in cellulo and in vivo, of the biological properties of the WT and re-encoded viruses.
Fig. 1. Schematic representation of the cloning vector pTBEV-32.11 ic (WT_IC). 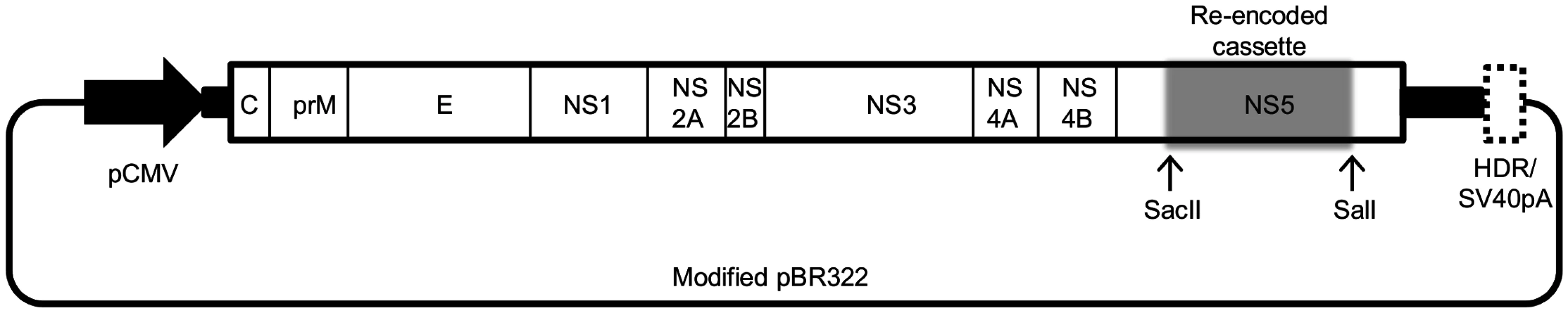
Coding (white rectangles) and non-coding (black rectangles) regions which represent the complete genome of the TBEV WT_IC were flanked in 5′ and 3′ by the pCMV and the HDR/SV40pA, and inserted into a modified pBR322 plasmid. The re-encoded cassette is represented by a grey rectangle flanked by the restriction sites SacII and SalI. In silico analysis
A total of 273 synonymous mutations, located between positions 8,619 and 10,019 (with reference to the complete genome sequence, GenBank accession number KF623542), was introduced in the specified NS5 coding region using a random distribution algorithm with restrictions [27] (Table 1). The codon usage (measured using the effective number of codons; eNC) and G+C% of the NS5_Reenc_IC virus was slightly modified compared with that of the WT_IC virus: 53.96 vs 55.46 and 54.3% vs 53.8%, respectively (Table 1). When compared with 85 TBEV and 56 other TBFV complete ORF sequences retrieved from GenBank, the eNC value of the NS5_Reenc_IC virus was higher than the maximum eNC value of TBEV sequences but fell within the extreme values of all available TBFV sequences. On the other hand, the G+C% value of NS5_Reenc_IC virus fell within the extreme values of TBEV sequences.
Tab. 1. Genetic characteristics of the complete coding regions of WT_IC and NS5_Reenc_IC viruses, and of 85 other tick-borne encephalitis viruses (TBEV) and 56 other tick-borne flaviviruses (TBFV). 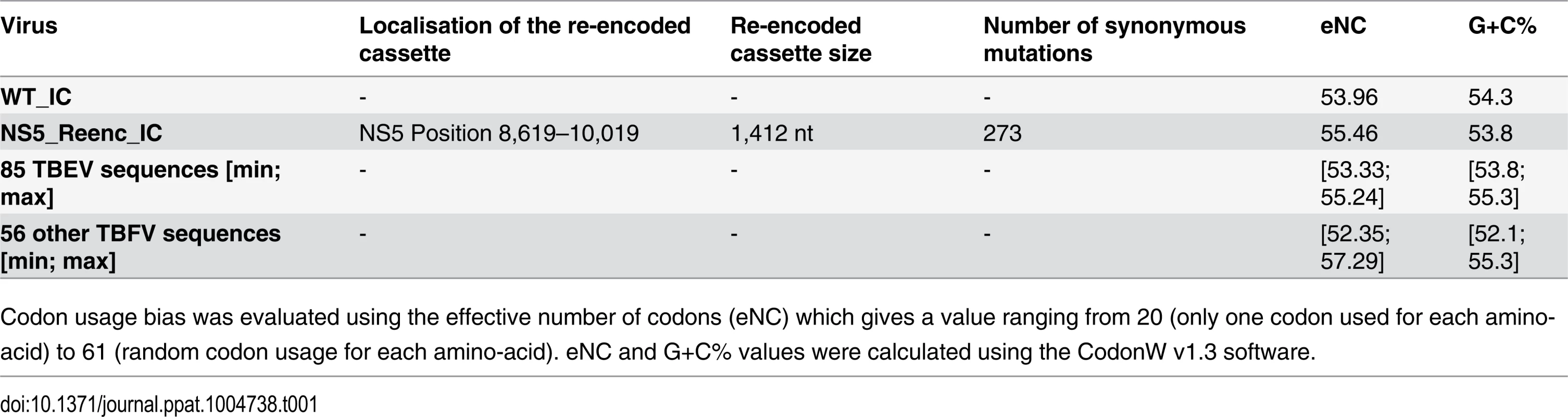
Codon usage bias was evaluated using the effective number of codons (eNC) which gives a value ranging from 20 (only one codon used for each amino-acid) to 61 (random codon usage for each amino-acid). eNC and G+C% values were calculated using the CodonW v1.3 software. In cellulo replicative fitness
WT_IC and NS5_Reenc_IC viruses were recovered following transfection of the corresponding infectious clones in BHK21 cells. These two viruses were then passaged once on BHK21 cells and their replicative fitness was subsequently studied.
Growth kinetics
Growth kinetics in BHK21 cells of both viruses were compared at high (200) and low (0.5) multiplicity of infection (moi). Infectious cell supernatant was harvested at 2, 5, 10, 15, 23, 31 and 48 hours post-infection. The infectious titre in each sample was estimated using a TCID50 assay. Regardless of the initial moi, growth kinetics of WT_IC and NS5_Reenc_IC viruses were essentially similar (Fig. 2A-B).
Fig. 2. In cellulo replicative fitness of WT_IC and NS5_Reenc_IC viruses in BHK21 cells. 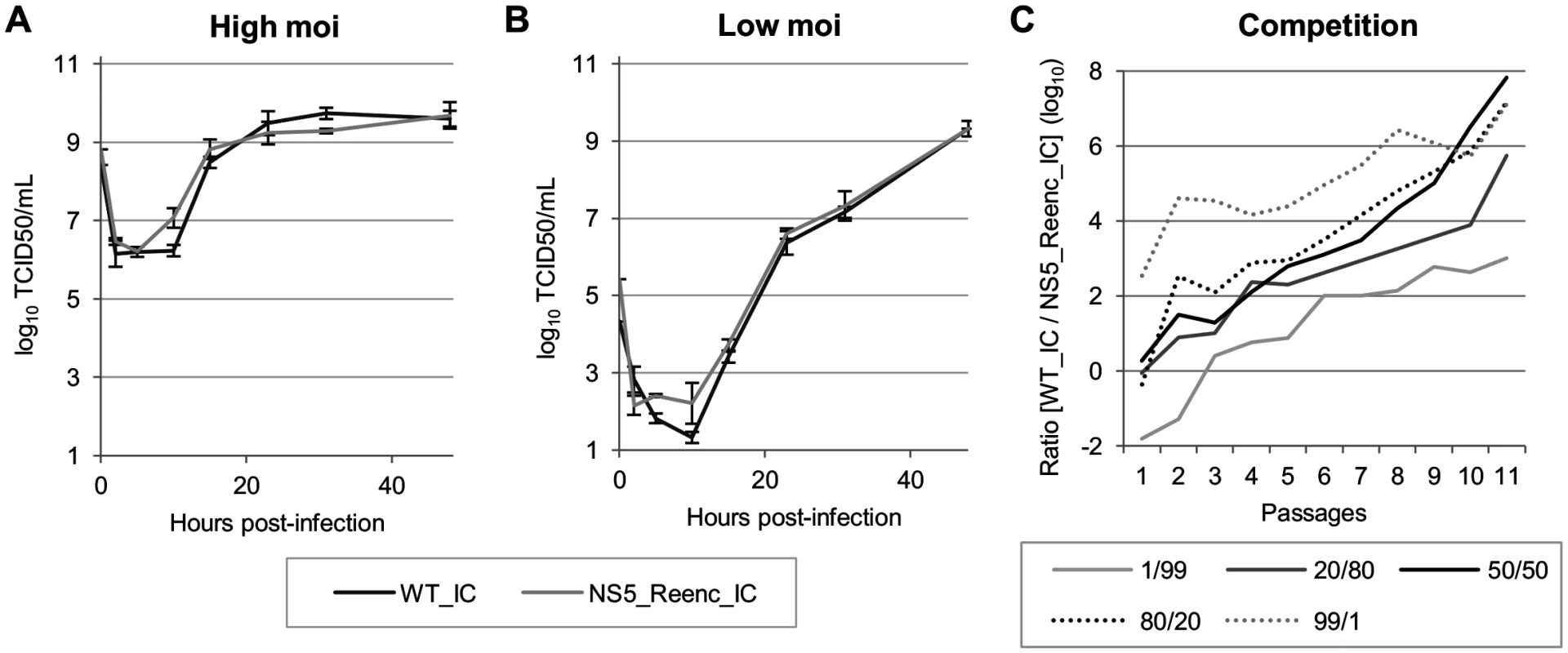
Results of growth kinetics curves performed at high (200) (A) or low (0.5) (B) initial moi (Results are expressed as mean/standard deviation values). Results of competition experiments (C) performed using five initial TCID50 ratios (WT_IC/NS5_Reenc_IC: 1/99, 20/80, 50/50, 80/20, 99/1). Two qRT-PCR assays, specific for WT_IC or NS5_Reenc_IC virus, enabled to monitor the evolution of the proportion of each virus along 11 passages. In cellulo competition experiments
Competition experiments can provide sensitive comparisons of the replicative fitness of two viruses [27]. Using the method described previously for chikungunya virus [27], five initial TCID50 ratios (WT_IC/NS5_Reenc_IC virus: 1/99, 20/80, 50/50, 80/20, 99/1) and a combined moi of 0.5 were used to infect BHK21 cells. Infectious cell supernatants were then passaged 11 times in BHK21 cells. Two specific quantitative RT-PCR techniques (each specifically detecting one of the competing viruses) were used to determine the proportion of each viral genome in cell supernatants at each passage (expressed as log10 in Fig. 2C). These competition experiments showed that WT_IC virus was fitter than NS5_Reenc_IC virus when the initial TCID50 ratios were compared. Indeed, by the 11th passage, the WT_IC/NS5_Reenc_IC ratio had increased by at least 10,000 fold.
In vivo experiments
The laboratory mouse model has been the primary global choice with which to study the CNS pathology induced by TBEVs. Pathologic changes in mouse brains as well as clinical signs are similar of those observed in humans [35,36,37]. In agreement with previous findings, virus recovered from infectious clones displayed lower mortality than the original cell culture derived Oshima 5–10 strain which induces high mortality in mice following intra-peritoneal inoculation [34]. Therefore, mortality was not used as a comparative criterion: we only observed late and low mortality rates when the mice were inoculated with the lower dose of TBEV (Fig. 3). It should also be noted that TBEVS are known to infect small rodents chronically/persistently as suggested by field studies [38,39].
Fig. 3. Time distribution of the proportion of mice with at least one symptom, with a weight loss of more than 6% and with virus detected in the serum or in the brain by qRT-PCR. 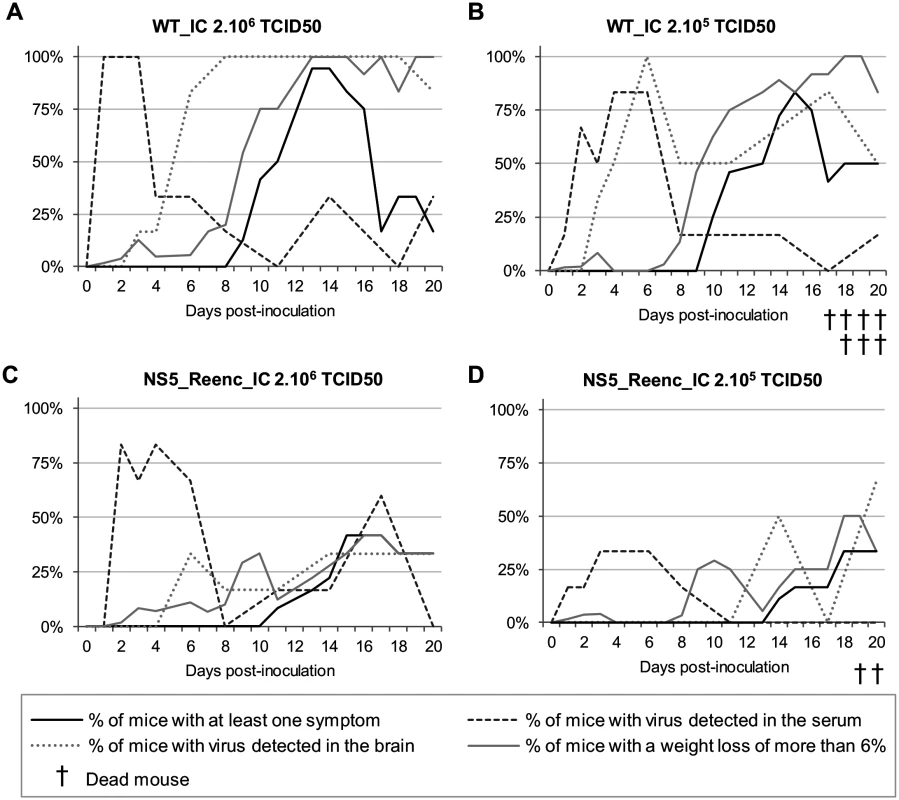
Mice were inoculated with 2.106 TCID50 of WT_IC virus (A), 2.105 TCID50 of WT_IC virus (B), 2.106 TCID50 of NS5_Reenc_IC virus (C) or 2.105 TCID50 of NS5_Reenc_IC virus (D). Five-week-old C57Bl/6J female mice were inoculated intra-peritoneally with 200μL containing 2.105 TCID50 [low dose] or 2.106 TCID50 [high dose] of virus. Clinical monitoring included (i) the clinical manifestation of the disease (shivering, humpback, dirty eyes, weak paws, hemiplegia or tetraplegia) and (ii) the body weight curve (a weight loss of more than 6% of the initial weight was chosen as a disease recognition criterion, as described in S1 Fig in S1 Text). Periodically, groups of mice were sacrificed to conduct virological investigations. A close relationship between viral load values determined using either quantitative RT-PCR (qRT-PCR) or the TCID50 method was observed. Consequently, the virological follow-up of sera and brains was performed using qRT-PCR (S2A and S2B Fig in S1 Text). Sera were also used for viral serological analysis by ELISA and virus neutralisation assays.
Comparative study of pathogenicity
Four groups of 60 mice were inoculated with two doses (2.105[low-dose] or 2.106[high-dose] TCID50) of either WT_IC virus or NS5_Reenc_IC virus. A control group of 16 mice was inoculated with PBS. Mice were weighed daily and monitored for the appearance of symptoms during the 20 day period of observation. Six mice per group were periodically euthanized to perform virus detection in sera and brains (at day 1, 2, 3, 4, 6, 8, 11, 14, 17 and 20 post-inoculation (p.i.)).
The proportion of viraemic animals was not significantly different between the high-dose and low-dose WT groups (Fig. 3A-3B), or between the high-dose re-encoded (Fig. 3C) and WT groups (Fig. 3A-3B). By contrast, it was significantly lower in the low-dose re-encoded group (Fig. 3D) compared with either the high-dose re-encoded (Fig. 3C) (p = 0.012, Fisher exact test) or WT groups of mice (Fig. 3A and 3B) (p<0.001, Fisher exact test). In all groups, the highest proportion of viraemic animals was observed 3 to 7 days p.i. Viral RNA yields found in sera were heterogeneous and no significant difference was found in term of inoculation dose or strain of virus (WT_IC or NS5_Reenc_IC viruses) inoculated (Fig. 4A-4D). In the WT-infected mice the peak period for detection of virus in the brain (neuroinvasion) always followed the peak viraemic titres, and preceded the appearance of encephalitic symptoms (see Fig. 3A-3B). In the groups infected by re-encoded virus, the kinetics of these parameters was atypical. Both weight loss and encephalitic symptoms were significantly less frequent than in the WT groups, regardless of the inoculation dose (Mandel-Cox’s Logrank test: p<0.0001 and p = 0.004 for mice infected with low and high doses, respectively; see Kaplan-Meier analysis in Fig. 5). The proportion of animals with virus in the brain (neuroinvasion) was significantly higher in WT-infected mice compared with re-encoded virus-infected mice, regardless of the dose used (Fisher exact test: p<0.0001 for both low - and high-dose groups, respectively; see Fig. 3). Viral RNA yields found in brains were heterogeneous and no significant difference was found in term of inoculation dose or strain of virus (WT_IC or NS5_Reenc_IC viruses) inoculated (Fig. 4E-4H).
Fig. 4. Viral RNA yields in sera (A-D) and brains (E-H). 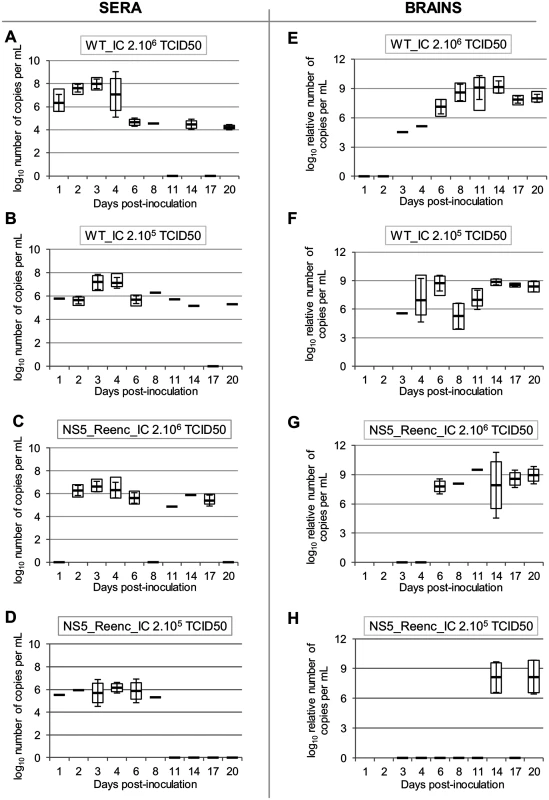
The virus and the dose used are indicated in each graphic. Viral RNA yields are expressed as log10 number of copies per mL (sera) or log10 relative number of copies per mL (brains) (values were normalized using the housekeeping gene HMBS as seen in the Materials and Methods section). White squares represent minimal and maximal values. Black lines and error bars represent mean values +/- standard deviation. A black line with a value of zero means that all samples were negative. Fig. 5. Kaplan-Meier survival analysis using as criteria, a weight loss of more than 6% (A) and appearance of at least one symptom (B). 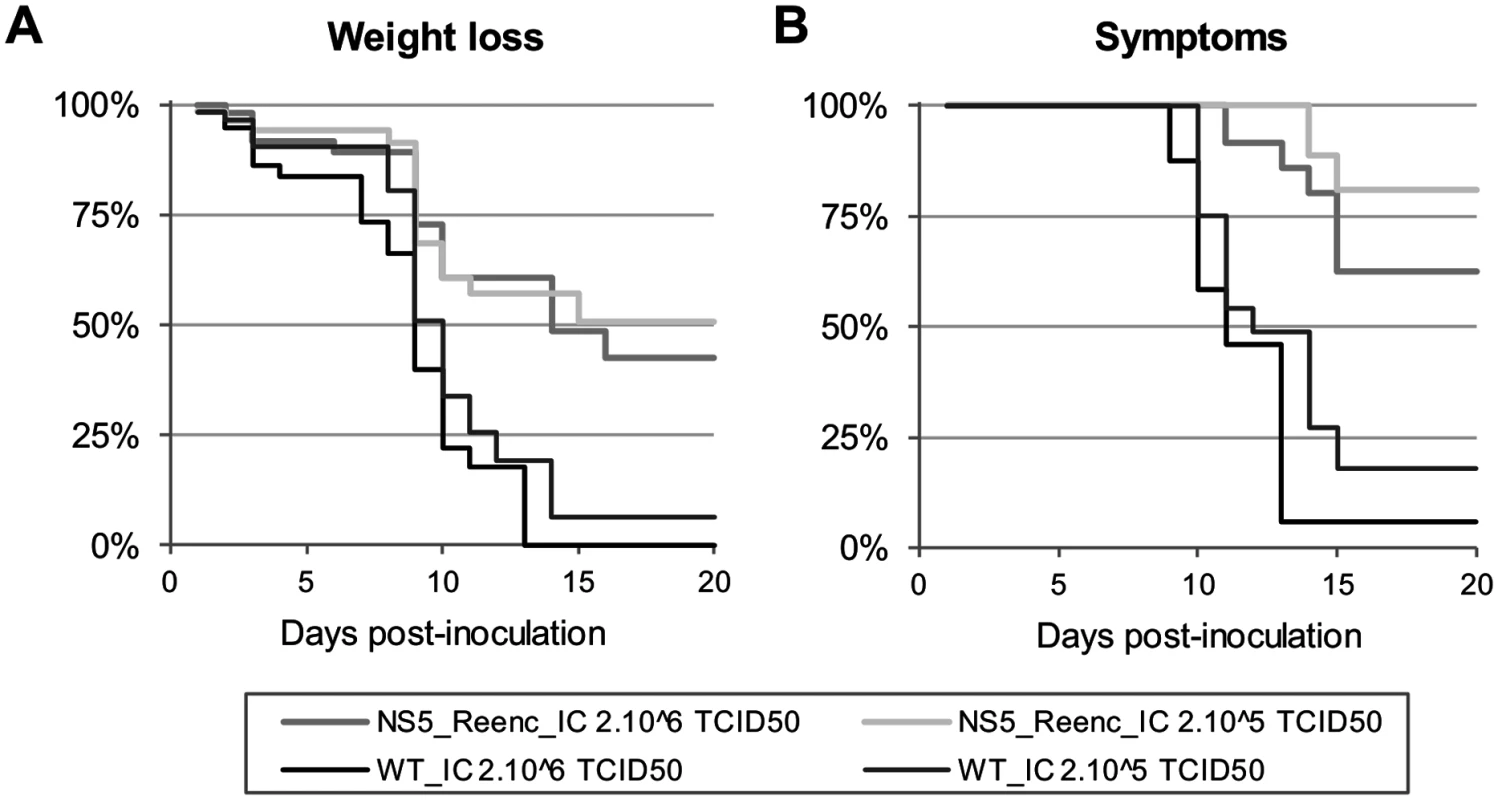
Serological investigations
Five groups of 4 mice were inoculated with either a low - or high-dose of WT_IC virus or NS5_Reenc_IC virus. A control group of non-infected mice was included. Forty three days after infection, the serum of each mouse was tested for the presence of antibodies to TBEV (only 3 mice were tested for the WT_IC 2.106 TCID50 group because one mouse died). TBEV-specific immunoglobulin G (IgG) antibodies were detected using a commercial diagnostic ELISA kit. High antibody titres were detected in mice infected by both the WT and the re-encoded viruses. Mice in the control group were negative (Student’s t-test; p<0.0001) (Fig. 6A). Sero-neutralisation tests were performed on the mouse sera representing mice inoculated with 2.106 TCID50 of virus. Neutralising antibodies were detected in all mice, but not in mice from the control group (Fig. 6B).
Fig. 6. Results of TBEV serology at day 43 post-inoculation. 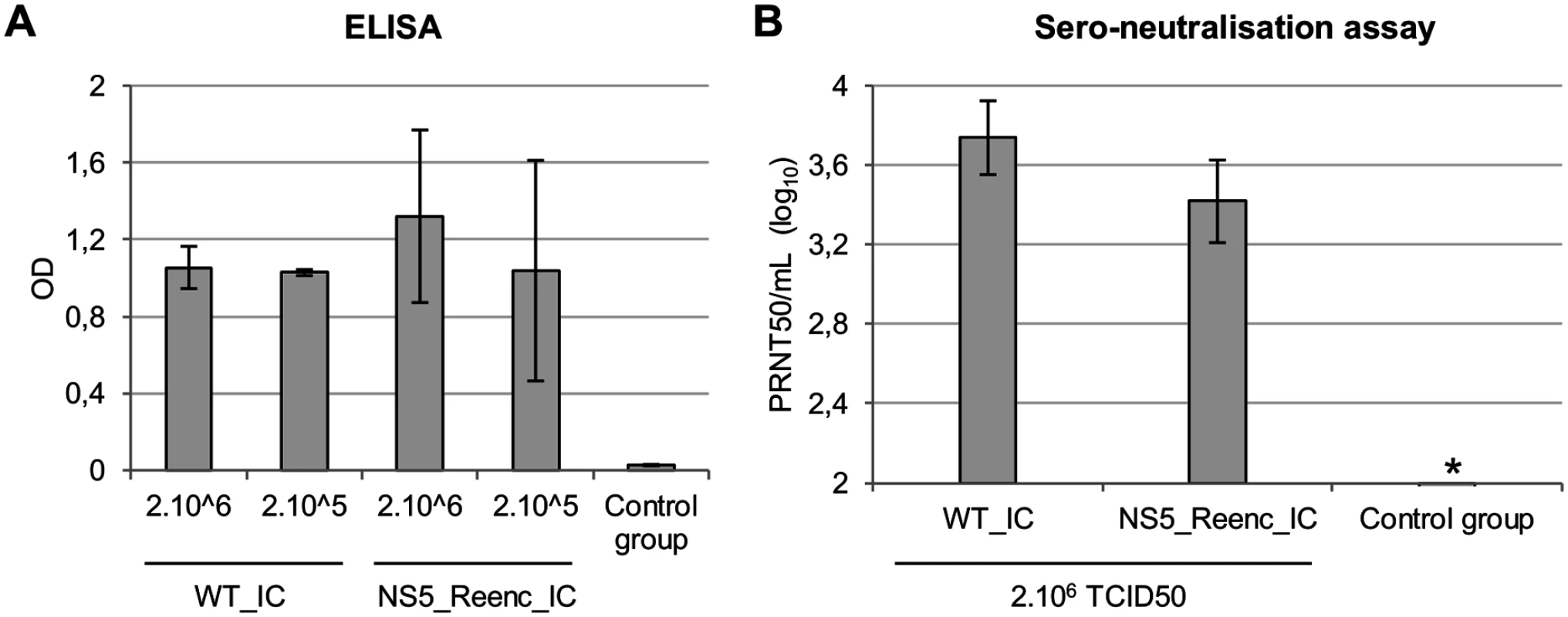
ELISA tests (A) and Sero-neutralisation tests (B). Results are expressed in the graphs as mean/standard deviation values for each group of mice. * all the sera of the control group tested were negative (all the samples were under the detection threshold of the method (2.25 PRNT50/mL)). Challenge experiments
Forty days after the inoculation of two groups of mice with the NS5_Reenc_IC virus and two groups of mice with the WT_IC virus (at both high and low doses for both viruses), 8 mice per group were challenged with 2.106 TCID50 of WT_IC virus, and the protection was evaluated by determining for each group the proportion of mice (i) viraemic at day 2 post-challenge, (ii) with brains positive for the presence of TBEV at day 12 post-challenge and (iii) with a weight loss of more than 6% of the weight at days 11 and 12 post-challenge. Two control groups of mice were used: one group of 8 mice inoculated with PBS and then challenged with virus as described above (mock group), and one group of 4 mice inoculated and challenged with PBS (used to normalise the weight of the mice).
Protection was 100% effective in terms of viraemia, for challenged mice immunised with the NS5_Reenc_IC virus or the WT_IC virus (both doses). In contrast, all mice in the mock group were viraemic (0/4 versus 4/4; Fisher’s exact test; p = 0.03 for each dose). Amongst all the weighing realised at days 11 and 12 post-challenge (S4 Table in S1 Text), only one showed a weight loss of more than 6% amongst mice immunised with the NS5_Reenc_IC virus (one mouse initially vaccinated with 2.105 TCID50 of NS5_Reenc_IC virus, at day 12 post-challenge, not at day 11 post-challenge). We found similar results with the challenged mice previously inoculated with the WT_IC virus: only one mouse inoculated with 2.105 TCID50 of WT_IC virus was below the detection threshold, only at day 12 post-challenge. In contrast, 87.5% of the weighing realised with the mice of the mock group were under this threshold (Fisher’s exact test; p≤0.01 when compared separately for each initial inoculation dose).
Surprisingly, we detected viral RNA in the brains of 100% of the challenged mice previously inoculated with the WT_IC virus and 100% of mice of the mock group. Viral RNA yields found in brains ranged from 103.7 to 106.8 relative number of copies per mL and no significant difference was found between the different groups of mice. We also detected viral RNA in the brains of 25% (1/4) and 75% (3/4) respectively of the challenged mice previously vaccinated with high and low doses of NS5_Reenc_IC virus. To determine whether or not the detected virus was the result of persistence in the brain, we quantified viral RNA yields with our two specific quantitative RT-PCR assays that were used previously in competition experiments (see above). For the challenged mice previously infected by the NS5_Reenc_IC virus, we found that the viral RNA present in the brain at day 12 post-challenge was exclusively the NS5_Reenc_IC virus but we failed to isolate the virus from these brain samples. Therefore, we obtained a protection of 100% in terms of neuroinvasion by the virus used for the protection experiments (0/4 versus 4/4; Fisher’s exact test; p = 0.03). However, for the mice vaccinated with the WT_IC virus, because the same virus was used to infect and challenge these mice, we could not draw valid conclusions in this instance.
In vivo competition experiments
In cellulo competition experiments had shown that WT_IC virus had a higher replicative fitness than NS5_Reenc_IC virus (see above). We therefore conducted in vivo competition experiments to determine whether or not the loss of replicative fitness due to re-encoding had an impact on viraemia and viral yields in the brain. Two initial TCID50 ratios (WT_IC/NS5_Reenc_IC virus: 10/90, 50/50—total dose: 2.106 TCID50) were used to inoculate two groups of six mice. At days 3 and 5 p.i., one group of mice per initial TCID50 ratio was sacrificed and the relative proportions of each viral genome in sera and brains was estimated using RT-PCR as reported in the earlier example of in cellulo competition assays (expressed as log10 in Fig. 7).
Fig. 7. Results of in vivo competition experiments. 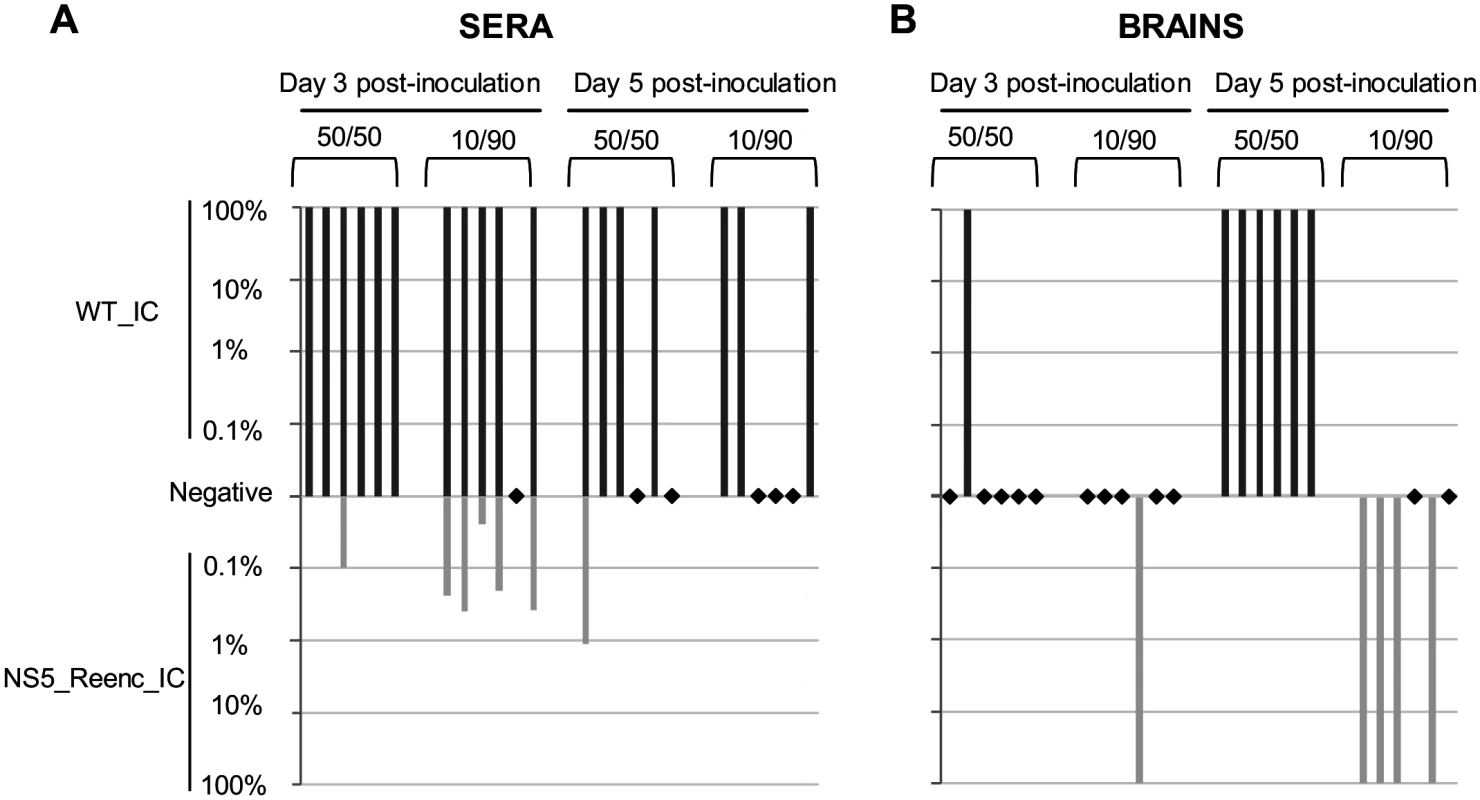
Competitions were performed using two initial PFU ratios (WT_IC/NS5_Reenc_IC virus: 50/50 or 10/90). Two qRT-PCR assays, specific for WT_IC or NS5_Reenc_IC virus enabled to quantify the proportion of each virus in the viral population in sera (A) and in brains (B). Dark and light grey rectangles represent the percentage of WT_IC and NS5_Reenc_IC virus in each sample (percentages are represented using a log10 scale). Black diamonds represent samples for which qRT-PCR were negative for WT_IC and NS5_Reenc_IC detection. In sera, regardless of the composition of the initial inoculum, the WT virus was the most represented in the viral population at days 3 and 5 p.i. (Fig. 7A). However, the results in brains were different: in all samples, only one of the 2 viruses was identified. The composition of the initial mixed inocula determined which virus was identified: the WT virus was recovered when the WT_IC/NS5_Reenc_IC ratio was 50/50 but the NS5_Reenc_IC virus was recovered when this ratio was 10/90 (Fig. 7B). The significance of these results is discussed further below.
Discussion
We have evaluated in cellulo and in vivo the effect of genomic large-scale random re-encoding on TBEV), a pathogenic TBFV that causes febrile illness and encephalitis in humans. Encephalitic flavivirus infections provoke CNS pathology which can be correlated with the observed morbidity and mortality: viruses replicating in the CNS induce direct neuronal damage causing severe CNS dysfunction often involving long-term neurological sequelae in non-fatal cases [36,40,41]. In addition, it has been demonstrated that host immune response is a critical determinant of clinical outcome [36,42,43,44,45].
Here, an infectious clone of a neurovirulent strain of TBEV (Far Eastern subtype) was used to perform in vivo studies in a mouse model that faithfully mirrors many aspects of the infection in humans. Our experiments showed that decreased replicative fitness (as determined by in cellulo competition assays and in vivo viraemia measurement) was associated with reduced neuroinvasiveness as previously described [46]. In vivo competition experiments shed further light on the mechanisms of pathogenesis: when a 50/50 (WT/Reenc) TCID50 initial ratio was used, as expected, the wild-type virus rapidly out-paced the re-encoded virus in blood and was the only virus detected in mouse brains. However, when a 10/90 (WT/Reenc) TCID50 initial ratio was used, the re-encoded virus was the only one detected in brain, suggesting an early and selective neuroinvasion process: only the majority virus present in blood during the first hours of the viraemia invades the central nervous system. Of course, more experiments are needed to confirm these findings and the potential role of viral interferences have to be assessed [47,48].
In this model, TBEV infection is frequently associated with asymptomatic persistence of the virus in mouse brain as previously described [38,39] and confirmed by our experiments (we detected viral RNA of the re-encoded virus but failed to isolate the virus). Previous reports of virus reactivation, years after the initial infection, suggest that this specific phenomenon might also occur in humans [49].
The main objectives of this study were (i) to analyse the effect of genome random re-encoding on the fitness and clinical phenotype of a virulent TBEV strain and (ii) to perform a complete set of in vivo experiments including immunisation with a re-encoded virus and follow-up challenge experiments with an infectious wild-type virus. It has previously been demonstrated that large-scale re-encoding generates attenuated viruses and the studies support the proposal that relative degree of attenuation or replicative fitness can be regulated by modulating the number of introduced synonymous mutations [18,19,20,21,22,23,24,25,26,27]. Indeed, a re-encoded strain of influenza A virus that displayed limited fitness in cellulo was highly attenuated when tested in a mouse model and showed potential for use as a vaccine candidate [25]. Similarly, re-encoding a 1.4 kb region of the CHIKV genome by introducing 300 random synonymous mutations was associated with only limited in cellulo attenuation [27]. Therefore, we hypothesised that appropriate re-encoding of a TBEV strain might result in limited fitness reduction in cellulo and thus provide a relevant candidate to study the relative degree of in vivo attenuation. Accordingly, we introduced 273 random synonymous mutations in the NS5 gene of a neurovirulent strain of TBEV (Oshima, Far Eastern subtype), with limited modification of G+C content or codon bias of the genome. This re-encoding protocol produced a virus variant that displayed no fitness difference when growth kinetics were compared with WT TBEV in mammalian cell cultures. However, more sensitive in cellulo competition experiments revealed that the replicative fitness of the wild-type virus was indeed higher than that of the re-encoded virus. Moreover, in vivo experiments in immunocompetent mice fully validated our starting hypothesis: the re-encoded virus could reproduce efficiently in mice but in competition experiments the wild-type virus had a significantly higher fitness. In vivo experiments also revealed the attenuated characteristics of the re-encoded virus, namely reduced neurovirulence in terms of weight loss and appearance of neurological symptoms and reduced neuroinvasiveness (i.e. lower proportion of mice with virus in the brain). It can therefore be concluded that the re-encoding process, although restricted to the NS5 gene, decreased the pathogenicity and led to the production of an attenuated phenotype of the normally highly virulent strain of TBEV.
Concerning the mouse protection experiments, the results showed that, at 40 days post-infection, neutralising antibodies were produced by 100% of mice, i.e. infected by either the wild-type or the re-encoded virus. Moreover, no significant differences in antibody titres were observed between mice infected with either virus. Thus, mice “immunised” by the re-encoded virus were likely to have been protected against subsequent TBEV infection. This was verified at 40 days post-infection by challenging the “immunised” mice using a high dose of intraperitoneally administered wild-type virus. Protection was effective in terms of viraemia, neurovirulence and neuroinvasion. Likewise, inoculation of CD155 tg mice with re-encoded strains of poliovirus induced the production of neutralising antibodies and protects the mice against a subsequent challenge with a lethal dose of virus [24].
The results provide a robust proof of concept: large-scale random re-encoding can be used to produce in vivo attenuated strains of TBEV and infection of mice by re-encoded viruses can induce neutralising and protective immune responses against challenge with virulent homologous viruses. This represents evidence that a positive-stranded randomly re-encoded RNA virus could be developed and trialled as a potential vaccine to protect humans and/or animals against viral pathogens.
Many current virus vaccines were derived empirically and carry an inherent risk of vaccine-associated complications. Our findings open up new perspectives for the development of new-generation custom-designed re-encoded live-attenuated vaccines which are potentially safe, induce high levels of protective immunity and are relatively easy to produce.
The use of a highly neurovirulent strain of TBEV in our experimental model enabled us to identify the in vivo modification of the clinical picture provided by genome re-encoding. The results strongly suggest that re-encoding could be used in the future for attenuation of highly pathogenic viral species. However, it would be wiser and more practical in the specific case of TBEV, to develop a live attenuated re-encoded vaccine using a strain known to have a naturally lower association with neurovirulence and by inserting additional synonymous mutations in coding regions with a view to reducing the encephalitic potential of the virus and thus produce a potentially safer vaccine candidate. Whilst effective inactivated vaccines are available to prevent TBEV infections, the use of a live attenuated vaccine may have specific advantages, e.g. long-term protection and reduced costs [50].
Materials and Methods
Cells and animals
Baby hamster kidney BHK21 (BHK21) cells (ATCC, number CCL10) and mouse (L929) cells (ATCC, number CCL1) were grown at 37°C with 5% CO2 in Minimum Essential Medium with 7% fetal calf serum (Life Technologies) and 1% Penicillin/Streptomycin (5000U/mL and 5000μg/mL; Life Technologies). Five-week-old C57Bl/6J mice females were provided by Charles River laboratories.
Ethics statement
Animal protocols were reviewed and approved by the ethics committee “Comité d’éthique en expérimentation animale de Marseille—C2EA—14” (protocol number 2504). All animal experiments were performed in compliance with French national guidelines and in accordance with the European legislation covering the use of animals for scientific purposes (Directive 210/63/EU).
In silico re-encoding method
A cassette of 1,412 bp located in the NS5 coding region was randomly re-encoded as described previously for chikungunya virus [27]. Briefly, a computer programme was used to randomly attribute nucleotide codons based on their corresponding amino acid sequence: for example, the amino acid proline was randomly replaced by CCT, CCC, CCA or CCG. The number and the position of rare codons in primate genomes [51] (i.e. CGU, CGC, CGA, CGG, UCG, CCG, GCG, ACG), and unique restriction sites were conserved (S1 Note in S1 Text).
Construction of TBEV infectious clones (ICs)
We modified a previously described IC of the Oshima 5–10 strain [34] (GenBank accession number of the parent virus: AB062063) by adding 9 synonymous mutations along the genome to increase the number of unique restriction sites, by replacing the SP6 promoter by a promoter CMV (pCMV) in 5′, by adding in 3′ of the complete viral genome the sequence of the hepatitis delta ribozyme followed by the simian virus 40 polyadenylation signal (HDR/SV40pA). The origin of replication was replaced by a modified pBR322. This IC was designated Cloning vector pTBEV-32.11 ic (GenBank accession number KF623542) and was considered as WT (Fig. 1). The re-encoded cassette (see above) was synthesized de novo by GenScript and inserted into the WT IC by digestion (SacII/SalI; New England Biolabs) (Fig. 1), gel purification of digestion products (Qiagen), ligation (T4 DNA ligase; Life Technologies) and transformation into electrocompetent STBL4 cells (Life Technologies). Before their transfection, both ICs were purified (0.22μm filtration) and their genome integrity was verified using a restriction map and complete sequencing.
Sequence analysis
Complete open reading frames of TBEV (n = 85) and other TBFV (n = 56) were manually extracted from GenBank (S2 and S3 Tables in S1 Text). G+C% and effective number of codons (eNC) were calculated using Codon W v1.3 software [52,53].
Recovery of infectious viruses and stock production
ICs were transfected into a 12.5cm2 culture flask containing sub-confluent BHK21 cells (FuGENE 6 transfection reagent; Roche). After incubation for 6 hours, cells were washed twice with Hank’s Balanced Salt Solution (HBSS, Life Technologies) and incubated until appearance of complete cytopathic effect (CPE). Cell supernatant medium was harvested, clarified by centrifugation and stored at -80°C. Each virus was then passaged in BHK21 cells at a calculated moi of 0.5 in a 175cm2 culture flask: after adsorption of the virus for 2 hours, the cells were washed twice (HBSS) and 50mL of medium was added and the flasks were incubated at 37°C for 72 hours. Cell supernatant media were harvested, clarified by centrifugation, aliquoted, stored at -80°C and used to perform in cellulo experiments. A similar experimental procedure was also carried out using L929 cells and the resulting cell supernatant medium was aliquoted, stored and used to perform the in vivo experiments. The integrity of the genome of all the viruses produced to perform in cellulo and in vivo experiments was verified using sequencing methods (Sanger methods).
Virus replication kinetics
A calculated moi of 200 or 0.5 was used to infect a 25cm2 culture flask of confluent BHK21 cells. Cells were washed twice (HBSS) 30 minutes after the infection and 7mL of medium was added. 800μL of cell supernatants were sampled just before the washes and at 2, 5, 10, 15, 23, 31 and 48 hours post-infection. They were clarified by centrifugation, aliquoted and stored at −80°C. They were then analyzed using a TCID50 assay (see below).
In cellulo competition experiments
As described previously for chikungunya virus WT_IC virus was competed with NS5_Reenc_IC virus [27]: five initial TCID50 ratios (WT_IC/NS5_Reenc_IC virus: 1/99, 20/80, 50/50, 80/20, 99/1) were used to infect a 25cm2 culture flask of confluent BHK21 cells at a calculated moi of 0.5. Cells were washed twice with HBSS and then incubated for 48h after addition of 7mL of medium. Recovered infectious cell supernatant was then sequentially passaged 10 times in the same manner with the clarified cell supernatant medium from the previous passage. At each passage, a calculated moi of 1 was used. Aliquots of cell supernatant from each passage were clarified by centrifugation and stored at -80°C. Viral RNA was extracted from clarified culture supernatant medium using the EZ1 Virus Mini Kit v2 on the EZ1 Biorobot (both from Qiagen). Using two specific quantitative real time RT-PCR assays targeting the re-encoded NS5 coding region (see the quantitative real time RT_PCR assays section for more details), the amount of viral RNA was assessed for each virus (WT_IC and NS5_Reenc_IC) and the ratio of the two values (WT_IC/NS5_Reenc_IC) was calculated.
In vivo experiments
Five-weeks-old C57Bl/6J female mice were intra-peritoneally inoculated with 200μL containing 2.105 TCID50 or 2.106 TCID50 of virus. In some experiments (see details in the results section), a control group of mice was used (they were intra-peritoneally inoculated with 200μL of PBS). The clinical course of the viral infection was monitored by following (i) the clinical manifestation of the disease (shivering, humpback, dirty eyes, hemi - or tetra-paresia, hemiplegia or tetraplegia) and (ii) the weight of the mice. Weights were normalized with the average weight of mice of control group; the normalized weight was expressed as percentage of initial weight and calculated as follows: (% of initial weight: weight/weight at the day of the inoculation or challenge)–(mean of the % of the initial weight for control mice) +100. Brains and blood were sampled from sacrificed mice. Blood was collected by intracardiac puncture. After centrifugation, serum was aliquoted and stored at -80°C. Nucleic acid extraction using 50μL of serum previously inactivated with 50μL of AVL buffer (Qiagen) and spiked with 10μL of MS2 bacteriophage (internal control) was performed using the EZ1 Virus Mini Kit v2 on the EZ1 Biorobot (both from Qiagen). Brains were collected in 1mL of PBS with a tungsten bead and ground using a TissueLyser (Qiagen) for 3min at 30cycles/s. The brain suspensions were homogenized with NucleoSpin filters (Macherey-Nagel). The collected filtrate was then aliquoted and stored at -80°C. Virus TCID50 assays were performed using these filtrates. Nucleic acid extraction using 30μL of filtrate, 270μL of RLT buffer (Qiagen) and 10μL of MS2 bacteriophage (internal control) was performed using the EZ1 RNA Tissue Mini Kit on the EZ1 Biorobot (both from Qiagen).
Virus isolation using brain samples
100μL of the filtrates collected from brain suspensions (see above) were used to inoculate a 12.5cm2 culture flask of confluent BHK21 cells containing 400μ of medium. After incubation for 2 hours, 2.5mL of medium was added and cells were incubated 5 days. A blind passage was then realised using a 25cm2 culture flask of confluent BHK21 cells. 2mL of clarified cell supernatant diluted 1 : 3 was used to inoculate the cells. After incubation for 2 hours, cells were washed once with HBSS and incubated 5 days. Virus replication was demonstrated using detection of viral genomes in cell supernatant using qRT-PCR assay and detection of cytopathic effect (CPE).
Quantitative real-time RT-PCR assays
All quantitative real-time PCR (qRT-PCR) assays were performed with SuperScript III Platinium One-Step qRT-PCR kit. The mix content for a final volume of 25μL per sample, was as follows: a standard quantity of 2x of PCR Mastermix and Enzymes, both primers (final concentration: 0.4μM), probe (final concentration: 0.1μM) and 4μL of extracted nucleic acids. qRT-PCR were performed on CFX96 Real-Time System/C1000 Touch Thermal Cycler (Biorad) with the following conditions: 15min at 50°C, 2min at 95°C, then 45 times 15sec at 95°C and 40sec at 60°C, data collection occurring during this last step. Primers and probe sequences are detailed in S1 Table in S1 Text. All sera and brain samples from mice were spiked with MS2 bacteriophage (internal control) prior nucleic acid extraction and a MS2-specific qRT-PCR was performed to monitor the extraction, reverse transcription, and amplification steps as previously described [54]. A universal qRT-PCR assay was used to detect the genomic RNA of all TBEVs (nucleotide position 10,236 to 10,337). The amount of viral RNA was calculated using synthetic RNA transcript for this universal assay. Results from mouse brains were normalized using amplification (qRT-PCR) of the housekeeping gene HMBS as described previously [55]. Two specific qRT-PCR assays were also used to specifically detect either WT_IC viruses or NS5_Reenc_IC viruses (nucleotide position 8,819 to 8,933). Nucleic acids from cell supernatant media of cultured WT_IC virus or NS5_Reenc_IC virus were used as standard for these specific assays. Values for the quantity of viral RNA of each standard used for both specific assays were calculated using the universal assay.
Tissue-culture infectious dose 50 (TCID50) assay
For each determination, a 96-well plate culture of confluent BHK21 cells was inoculated with 150μL/well of serial 10-fold dilutions of clarified (centrifugation) cell supernatant medium, mouse sera or mouse brain filtrates: each dilution was repeated 6 times. The plates were incubated for 7 days and read for absence or presence of CPE in each well. Determination of the TCID50/mL was performed using the method of Reed and Muench [56].
ELISA test
Sera were incubated for 30min at 56°C prior to viral serology. TBEV-specific immunoglobulin G (IgG) antibodies were detected using the Anti-TBE Virus ELISA (IgG) kit (Euroimmun). Sera were diluted 1 : 64 and then 1 : 101 prior to the first incubation using the Sample Buffer of the kit. Goat anti-mouse IgG antibodies (Invitrogen) diluted 1 : 2000 in BSA 0.7% (KPL) as secondary antibodies were used. Plates were read using the Sunrise reader (Tecan) at a wavelength of 450nm.
Serum neutralisation assay
Sera were incubated for 30min at 56°C prior to viral serology. For each serum, a 96-well plate culture of confluent BHK21 cells was inoculated with 50μL/well of WT_IC virus (final calculated moi: 0.001) and 50μL/well of a serial 2-fold dilution (first dilution at 1 : 40) of serum. Each row included 5 wells of serum dilution, a positive control (virus only) and a negative control with neither virus nor serum. The plates were incubated for 7 days and read for the absence or presence of a CPE in each well. The 50% plaque reduction neutralization titre (PRNT50/mL) was determined using the method of Reed and Muench [56].
Statistical analysis
Kaplan-Meier survival analysis with Mandel-Cox’s Logrank tests, Student’s t tests and Fisher’s exact tests were performed using SPSS software package (IBM). p values below 0.05 were considered significant.
Supporting Information
Zdroje
1. Gould EA, Solomon T (2008) Pathogenic flaviviruses. Lancet 371 : 500–509. doi: 10.1016/S0140-6736(08)60238-X 18262042
2. Gubler DJ (2012) Flaviviruses: Past, Present and Future. Molecular Virology and Control of Flaviviruses: 1–7.
3. Firth AE, Brierley I (2012) Non-canonical translation in RNA viruses. J Gen Virol 93 : 1385–1409. doi: 10.1099/vir.0.042499-0 22535777
4. Firth AE, Atkins JF (2009) A conserved predicted pseudoknot in the NS2A-encoding sequence of West Nile and Japanese encephalitis flaviviruses suggests NS1′ may derive from ribosomal frameshifting. Virol J 6 : 14. doi: 10.1186/1743-422X-6-14 19196463
5. Cook S, Holmes EC (2006) A multigene analysis of the phylogenetic relationships among the flaviviruses (Family: Flaviviridae) and the evolution of vector transmission. Arch Virol 151 : 309–325. 16172840
6. Grard G, Moureau G, Charrel RN, Lemasson JJ, Gonzalez JP, et al. (2007) Genetic characterization of tick-borne flaviviruses: new insights into evolution, pathogenetic determinants and taxonomy. Virology 361 : 80–92. 17169393
7. Charrel RN, Attoui H, Butenko AM, Clegg JC, Deubel V, et al. (2004) Tick-borne virus diseases of human interest in Europe. Clin Microbiol Infect 10 : 1040–1055. 15606630
8. Ecker M, Allison SL, Meixner T, Heinz FX (1999) Sequence analysis and genetic classification of tick-borne encephalitis viruses from Europe and Asia. J Gen Virol 80 (Pt 1): 179–185. 9934700
9. Gritsun TS, Lashkevich VA, Gould EA (2003) Tick-borne encephalitis. Antiviral Res 57 : 129–146. 12615309
10. Korenberg EI, Kovalevskii YV (1999) Main features of tick-borne encephalitis eco-epidemiology in Russia. Zentralbl Bakteriol 289 : 525–539. 10652719
11. Lehrer AT, Holbrook MR (2011) Tick-borne Encephalitis Vaccines. J Bioterror Biodef 2011 : 3. 23997980
12. Lundkvist A, Wallensten A, Vene S, Hjertqvist M (2011) Tick-borne encephalitis increasing in Sweden, 2011. Euro Surveill 16.
13. Suss J (2008) Tick-borne encephalitis in Europe and beyond—the epidemiological situation as of 2007. Euro Surveill 13.
14. Kollaritsch H, Chmelik V, Dontsenko I, Grzeszczuk A, Kondrusik M, et al. (2011) The current perspective on tick-borne encephalitis awareness and prevention in six Central and Eastern European countries: report from a meeting of experts convened to discuss TBE in their region. Vaccine 29 : 4556–4564. doi: 10.1016/j.vaccine.2011.04.061 21549781
15. Heinz FX, Stiasny K (2012) Flaviviruses and flavivirus vaccines. Vaccine 30 : 4301–4306. doi: 10.1016/j.vaccine.2011.09.114 22682286
16. Barrett AD (2001) Current status of flavivirus vaccines. Ann N Y Acad Sci 951 : 262–271. 11797783
17. Kitchener S (2004) Viscerotropic and neurotropic disease following vaccination with the 17D yellow fever vaccine, ARILVAX. Vaccine 22 : 2103–2105. 15149765
18. Meng J, Lee S, Hotard AL, Moore ML (2014) Refining the Balance of Attenuation and Immunogenicity of Respiratory Syncytial Virus by Targeted Codon Deoptimization of Virulence Genes. MBio 5.
19. Le Nouen C, Brock LG, Luongo C, McCarty T, Yang L, et al. (2014) Attenuation of human respiratory syncytial virus by genome-scale codon-pair deoptimization. Proc Natl Acad Sci U S A 111 : 13169–13174. doi: 10.1073/pnas.1411290111 25157129
20. Ni YY, Zhao Z, Opriessnig T, Subramaniam S, Zhou L, et al. (2014) Computer-aided codon-pairs deoptimization of the major envelope GP5 gene attenuates porcine reproductive and respiratory syndrome virus. Virology 450–451 : 132–139.
21. Martrus G, Nevot M, Andres C, Clotet B, Martinez MA (2013) Changes in codon-pair bias of human immunodeficiency virus type 1 have profound effects on virus replication in cell culture. Retrovirology 10 : 78. doi: 10.1186/1742-4690-10-78 23885919
22. Burns CC, Shaw J, Campagnoli R, Jorba J, Vincent A, et al. (2006) Modulation of poliovirus replicative fitness in HeLa cells by deoptimization of synonymous codon usage in the capsid region. J Virol 80 : 3259–3272. 16537593
23. Mueller S, Papamichail D, Coleman JR, Skiena S, Wimmer E (2006) Reduction of the rate of poliovirus protein synthesis through large-scale codon deoptimization causes attenuation of viral virulence by lowering specific infectivity. J Virol 80 : 9687–9696. 16973573
24. Coleman JR, Papamichail D, Skiena S, Futcher B, Wimmer E, et al. (2008) Virus attenuation by genome-scale changes in codon pair bias. Science 320 : 1784–1787. doi: 10.1126/science.1155761 18583614
25. Mueller S, Coleman JR, Papamichail D, Ward CB, Nimnual A, et al. (2010) Live attenuated influenza virus vaccines by computer-aided rational design. Nat Biotechnol 28 : 723–726. doi: 10.1038/nbt.1636 20543832
26. Burns CC, Campagnoli R, Shaw J, Vincent A, Jorba J, et al. (2009) Genetic inactivation of poliovirus infectivity by increasing the frequencies of CpG and UpA dinucleotides within and across synonymous capsid region codons. J Virol 83 : 9957–9969. doi: 10.1128/JVI.00508-09 19605476
27. Nougairede A, De Fabritus L, Aubry F, Gould EA, Holmes EC, et al. (2013) Random codon re-encoding induces stable reduction of replicative fitness of Chikungunya virus in primate and mosquito cells. PLoS Pathog 9: e1003172. doi: 10.1371/journal.ppat.1003172 23436995
28. Chen SL, Lee W, Hottes AK, Shapiro L, McAdams HH (2004) Codon usage between genomes is constrained by genome-wide mutational processes. Proc Natl Acad Sci U S A 101 : 3480–3485. 14990797
29. Watts JM, Dang KK, Gorelick RJ, Leonard CW, Bess JW Jr., et al. (2009) Architecture and secondary structure of an entire HIV-1 RNA genome. Nature 460 : 711–716. doi: 10.1038/nature08237 19661910
30. Thurner C, Witwer C, Hofacker IL, Stadler PF (2004) Conserved RNA secondary structures in Flaviviridae genomes. J Gen Virol 85 : 1113–1124. 15105528
31. Jones CT, Ma L, Burgner JW, Groesch TD, Post CB, et al. (2003) Flavivirus capsid is a dimeric alpha-helical protein. J Virol 77 : 7143–7149. 12768036
32. Bull JJ, Molineux IJ, Wilke CO (2012) Slow fitness recovery in a codon-modified viral genome. Mol Biol Evol 29 : 2997–3004. 22532576
33. Takashima I, Morita K, Chiba M, Hayasaka D, Sato T, et al. (1997) A case of tick-borne encephalitis in Japan and isolation of the the virus. J Clin Microbiol 35 : 1943–1947. 9230360
34. Hayasaka D, Gritsun TS, Yoshii K, Ueki T, Goto A, et al. (2004) Amino acid changes responsible for attenuation of virus neurovirulence in an infectious cDNA clone of the Oshima strain of tick-borne encephalitis virus. J Gen Virol 85 : 1007–1018. 15039543
35. Tigabu B, Juelich T, Bertrand J, Holbrook MR (2009) Clinical evaluation of highly pathogenic tick-borne flavivirus infection in the mouse model. J Med Virol 81 : 1261–1269. doi: 10.1002/jmv.21524 19475605
36. Hayasaka D, Nagata N, Fujii Y, Hasegawa H, Sata T, et al. (2009) Mortality following peripheral infection with tick-borne encephalitis virus results from a combination of central nervous system pathology, systemic inflammatory and stress responses. Virology 390 : 139–150. doi: 10.1016/j.virol.2009.04.026 19467556
37. Kimura T, Sasaki M, Okumura M, Kim E, Sawa H (2010) Flavivirus encephalitis: pathological aspects of mouse and other animal models. Vet Pathol 47 : 806–818. doi: 10.1177/0300985810372507 20551474
38. Bakhvalova VN, Dobrotvorsky AK, Panov VV, Matveeva VA, Tkachev SE, et al. (2006) Natural tick-borne encephalitis virus infection among wild small mammals in the southeastern part of western Siberia, Russia. Vector Borne Zoonotic Dis 6 : 32–41. 16584325
39. Kozuch O, Gresikova M, Nosek J, Lichard M, Sekeyova M (1967) The role of small rodents and hedgehogs in a natural focus of tick-borne encephalitis. Bull World Health Organ 36 Suppl: 61–66. 5298543
40. Shrestha B, Gottlieb D, Diamond MS (2003) Infection and injury of neurons by West Nile encephalitis virus. J Virol 77 : 13203–13213. 14645577
41. Ruzek D, Vancova M, Tesarova M, Ahantarig A, Kopecky J, et al. (2009) Morphological changes in human neural cells following tick-borne encephalitis virus infection. J Gen Virol 90 : 1649–1658. doi: 10.1099/vir.0.010058-0 19264624
42. Tun MM, Aoki K, Senba M, Buerano CC, Shirai K, et al. (2014) Protective role of TNF-alpha, IL-10 and IL-2 in mice infected with the Oshima strain of Tick-borne encephalitis virus. Sci Rep 4 : 5344. doi: 10.1038/srep05344 24938868
43. Ruzek D, Salat J, Palus M, Gritsun TS, Gould EA, et al. (2009) CD8+ T-cells mediate immunopathology in tick-borne encephalitis. Virology 384 : 1–6. doi: 10.1016/j.virol.2008.11.023 19070884
44. King NJ, Getts DR, Getts MT, Rana S, Shrestha B, et al. (2007) Immunopathology of flavivirus infections. Immunol Cell Biol 85 : 33–42. 17146465
45. Hayasaka D, Shirai K, Aoki K, Nagata N, Simantini DS, et al. (2013) TNF-alpha acts as an immunoregulator in the mouse brain by reducing the incidence of severe disease following Japanese encephalitis virus infection. PLoS One 8: e71643. doi: 10.1371/journal.pone.0071643 23940775
46. Goto A, Hayasaka D, Yoshii K, Mizutani T, Kariwa H, et al. (2003) A BHK-21 cell culture-adapted tick-borne encephalitis virus mutant is attenuated for neuroinvasiveness. Vaccine 21 : 4043–4051. 12922141
47. Wagner RR (1960) Viral Interference. Some Considerations of Basic Mechanisms and Their Potential Relationship to Host Resistance. Bacteriol Rev 24 : 151–166. 16350163
48. Roux L, Simon AE, Holland JJ (1991) Effects of defective interfering viruses on virus replication and pathogenesis in vitro and in vivo. Adv Virus Res 40 : 181–211. 1957718
49. Gritsun TS, Frolova TV, Zhankov AI, Armesto M, Turner SL, et al. (2003) Characterization of a siberian virus isolated from a patient with progressive chronic tick-borne encephalitis. J Virol 77 : 25–36. 12477807
50. Coffin JM (2008) Attenuation by a thousand cuts. N Engl J Med 359 : 2283–2285. doi: 10.1056/NEJMcibr0805820 19020330
51. Zhang SP, Zubay G, Goldman E (1991) Low-usage codons in Escherichia coli, yeast, fruit fly and primates. Gene 105 : 61–72. 1937008
52. Zhou JH, Zhang J, Chen HT, Ma LN, Liu YS (2010) Analysis of synonymous codon usage in foot-and-mouth disease virus. Vet Res Commun 34 : 393–404. doi: 10.1007/s11259-010-9359-4 20425142
53. Peden J (1997) CodonW v1.3. Laboratory of Paul Sharp at the University of Nottingham.
54. Ninove L, Nougairede A, Gazin C, Thirion L, Delogu I, et al. (2011) RNA and DNA bacteriophages as molecular diagnosis controls in clinical virology: a comprehensive study of more than 45,000 routine PCR tests. PLoS One 6: e16142. doi: 10.1371/journal.pone.0016142 21347398
55. Ding S, Chi MM, Scull BP, Rigby R, Schwerbrock NM, et al. (2010) High-fat diet: bacteria interactions promote intestinal inflammation which precedes and correlates with obesity and insulin resistance in mouse. PLoS One 5: e12191. doi: 10.1371/journal.pone.0012191 20808947
56. Reed LJ, Muench H (1938) A simple method of estimating fifty per cent endpoints. Am J Hyg 27 : 493–497.
Štítky
Hygiena a epidemiologie Infekční lékařství Laboratoř
Článek A Phospholipase Is Involved in Disruption of the Liver Stage Parasitophorous Vacuole MembraneČlánek Host ESCRT Proteins Are Required for Bromovirus RNA Replication Compartment Assembly and FunctionČlánek Enhanced CD8 T Cell Responses through GITR-Mediated Costimulation Resolve Chronic Viral Infection
Článek vyšel v časopisePLOS Pathogens
Nejčtenější tento týden
2015 Číslo 3- Jak souvisí postcovidový syndrom s poškozením mozku?
- Měli bychom postcovidový syndrom léčit antidepresivy?
- Farmakovigilanční studie perorálních antivirotik indikovaných v léčbě COVID-19
- 10 bodů k očkování proti COVID-19: stanovisko České společnosti alergologie a klinické imunologie ČLS JEP
-
Všechny články tohoto čísla
- To Be or Not IIb: A Multi-Step Process for Epstein-Barr Virus Latency Establishment and Consequences for B Cell Tumorigenesis
- Is Antigenic Sin Always “Original?” Re-examining the Evidence Regarding Circulation of a Human H1 Influenza Virus Immediately Prior to the 1918 Spanish Flu
- The Great Escape: Pathogen Versus Host
- Coping with Stress and the Emergence of Multidrug Resistance in Fungi
- Catch Me If You Can: The Link between Autophagy and Viruses
- Bacterial Immune Evasion through Manipulation of Host Inhibitory Immune Signaling
- Evidence for Ubiquitin-Regulated Nuclear and Subnuclear Trafficking among Matrix Proteins
- BILBO1 Is a Scaffold Protein of the Flagellar Pocket Collar in the Pathogen
- Production of Anti-LPS IgM by B1a B Cells Depends on IL-1β and Is Protective against Lung Infection with LVS
- Virulence Regulation with Venus Flytrap Domains: Structure and Function of the Periplasmic Moiety of the Sensor-Kinase BvgS
- α-Hemolysin Counteracts the Anti-Virulence Innate Immune Response Triggered by the Rho GTPase Activating Toxin CNF1 during Bacteremia
- Induction of Interferon-Stimulated Genes by IRF3 Promotes Replication of
- Intracellular Growth Is Dependent on Tyrosine Catabolism in the Dimorphic Fungal Pathogen
- HCV Induces the Expression of Rubicon and UVRAG to Temporally Regulate the Maturation of Autophagosomes and Viral Replication
- Spatiotemporal Analysis of Hepatitis C Virus Infection
- Subgingival Microbial Communities in Leukocyte Adhesion Deficiency and Their Relationship with Local Immunopathology
- Interaction between the Type III Effector VopO and GEF-H1 Activates the RhoA-ROCK Pathway
- Attenuation of Tick-Borne Encephalitis Virus Using Large-Scale Random Codon Re-encoding
- Establishment of HSV1 Latency in Immunodeficient Mice Facilitates Efficient Reactivation
- XRN1 Stalling in the 5’ UTR of Hepatitis C Virus and Bovine Viral Diarrhea Virus Is Associated with Dysregulated Host mRNA Stability
- γδ T Cells Confer Protection against Murine Cytomegalovirus (MCMV)
- Rhadinovirus Host Entry by Co-operative Infection
- A Phospholipase Is Involved in Disruption of the Liver Stage Parasitophorous Vacuole Membrane
- Dermal Neutrophil, Macrophage and Dendritic Cell Responses to Transmitted by Fleas
- Elucidation of Sigma Factor-Associated Networks in Reveals a Modular Architecture with Limited and Function-Specific Crosstalk
- A Conserved NS3 Surface Patch Orchestrates NS2 Protease Stimulation, NS5A Hyperphosphorylation and HCV Genome Replication
- Host ESCRT Proteins Are Required for Bromovirus RNA Replication Compartment Assembly and Function
- Disruption of IL-21 Signaling Affects T Cell-B Cell Interactions and Abrogates Protective Humoral Immunity to Malaria
- Compartmentalized Replication of R5 T Cell-Tropic HIV-1 in the Central Nervous System Early in the Course of Infection
- Diminished Reovirus Capsid Stability Alters Disease Pathogenesis and Littermate Transmission
- Characterization of CD8 T Cell Differentiation following SIVΔnef Vaccination by Transcription Factor Expression Profiling
- Visualization of HIV-1 Interactions with Penile and Foreskin Epithelia: Clues for Female-to-Male HIV Transmission
- Sensing Cytosolic RpsL by Macrophages Induces Lysosomal Cell Death and Termination of Bacterial Infection
- PKCη/Rdx-driven Phosphorylation of PDK1: A Novel Mechanism Promoting Cancer Cell Survival and Permissiveness for Parvovirus-induced Lysis
- Metalloprotease NleC Suppresses Host NF-κB/Inflammatory Responses by Cleaving p65 and Interfering with the p65/RPS3 Interaction
- Immune Antibodies and Helminth Products Drive CXCR2-Dependent Macrophage-Myofibroblast Crosstalk to Promote Intestinal Repair
- Adenovirus Entry From the Apical Surface of Polarized Epithelia Is Facilitated by the Host Innate Immune Response
- The RNA Template Channel of the RNA-Dependent RNA Polymerase as a Target for Development of Antiviral Therapy of Multiple Genera within a Virus Family
- Neutrophils: Between Host Defence, Immune Modulation, and Tissue Injury
- CD169-Mediated Trafficking of HIV to Plasma Membrane Invaginations in Dendritic Cells Attenuates Efficacy of Anti-gp120 Broadly Neutralizing Antibodies
- Japanese Encephalitis Virus Nonstructural Protein NS5 Interacts with Mitochondrial Trifunctional Protein and Impairs Fatty Acid β-Oxidation
- Yip1A, a Novel Host Factor for the Activation of the IRE1 Pathway of the Unfolded Protein Response during Infection
- TRIM26 Negatively Regulates Interferon-β Production and Antiviral Response through Polyubiquitination and Degradation of Nuclear IRF3
- Parallel Epigenomic and Transcriptomic Responses to Viral Infection in Honey Bees ()
- A Crystal Structure of the Dengue Virus NS5 Protein Reveals a Novel Inter-domain Interface Essential for Protein Flexibility and Virus Replication
- Enhanced CD8 T Cell Responses through GITR-Mediated Costimulation Resolve Chronic Viral Infection
- Exome and Transcriptome Sequencing of Identifies a Locus That Confers Resistance to and Alters the Immune Response
- The Role of Misshapen NCK-related kinase (MINK), a Novel Ste20 Family Kinase, in the IRES-Mediated Protein Translation of Human Enterovirus 71
- Chitin Recognition via Chitotriosidase Promotes Pathologic Type-2 Helper T Cell Responses to Cryptococcal Infection
- Activates Both IL-1β and IL-1 Receptor Antagonist to Modulate Lung Inflammation during Pneumonic Plague
- Persistence of Transmitted HIV-1 Drug Resistance Mutations Associated with Fitness Costs and Viral Genetic Backgrounds
- An 18 kDa Scaffold Protein Is Critical for Biofilm Formation
- Early Virological and Immunological Events in Asymptomatic Epstein-Barr Virus Infection in African Children
- Human CD8 T-cells Recognizing Peptides from () Presented by HLA-E Have an Unorthodox Th2-like, Multifunctional, Inhibitory Phenotype and Represent a Novel Human T-cell Subset
- Decreased HIV-Specific T-Regulatory Responses Are Associated with Effective DC-Vaccine Induced Immunity
- RSV Vaccine-Enhanced Disease Is Orchestrated by the Combined Actions of Distinct CD4 T Cell Subsets
- Concerted Activity of IgG1 Antibodies and IL-4/IL-25-Dependent Effector Cells Trap Helminth Larvae in the Tissues following Vaccination with Defined Secreted Antigens, Providing Sterile Immunity to Challenge Infection
- Structure of the Low pH Conformation of Chandipura Virus G Reveals Important Features in the Evolution of the Vesiculovirus Glycoprotein
- PPM1A Regulates Antiviral Signaling by Antagonizing TBK1-Mediated STING Phosphorylation and Aggregation
- Lipidomic Analysis Links Mycobactin Synthase K to Iron Uptake and Virulence in .
- Roles and Programming of Arabidopsis ARGONAUTE Proteins during Infection
- Impact of Infection on Host Macrophage Nuclear Physiology and Nucleopore Complex Integrity
- The Impact of Host Diet on Titer in
- Antimicrobial-Induced DNA Damage and Genomic Instability in Microbial Pathogens
- Herpesviral G Protein-Coupled Receptors Activate NFAT to Induce Tumor Formation via Inhibiting the SERCA Calcium ATPase
- The Causes and Consequences of Changes in Virulence following Pathogen Host Shifts
- Small GTPase Rab21 Mediates Fibronectin Induced Actin Reorganization in : Implications in Pathogen Invasion
- Positive Role of Promyelocytic Leukemia Protein in Type I Interferon Response and Its Regulation by Human Cytomegalovirus
- NEDDylation Is Essential for Kaposi’s Sarcoma-Associated Herpesvirus Latency and Lytic Reactivation and Represents a Novel Anti-KSHV Target
- β-HPV 5 and 8 E6 Disrupt Homology Dependent Double Strand Break Repair by Attenuating BRCA1 and BRCA2 Expression and Foci Formation
- An O Antigen Capsule Modulates Bacterial Pathogenesis in
- Variable Processing and Cross-presentation of HIV by Dendritic Cells and Macrophages Shapes CTL Immunodominance and Immune Escape
- Probing the Metabolic Network in Bloodstream-Form Using Untargeted Metabolomics with Stable Isotope Labelled Glucose
- Adhesive Fiber Stratification in Uropathogenic Biofilms Unveils Oxygen-Mediated Control of Type 1 Pili
- Vaccinia Virus Protein Complex F12/E2 Interacts with Kinesin Light Chain Isoform 2 to Engage the Kinesin-1 Motor Complex
- Modulates Host Macrophage Mitochondrial Metabolism by Hijacking the SIRT1-AMPK Axis
- Human T-Cell Leukemia Virus Type 1 (HTLV-1) Tax Requires CADM1/TSLC1 for Inactivation of the NF-κB Inhibitor A20 and Constitutive NF-κB Signaling
- Suppression of RNAi by dsRNA-Degrading RNaseIII Enzymes of Viruses in Animals and Plants
- Spatiotemporal Regulation of a T4SS Substrate by the Metaeffector SidJ
- Antigenic Properties of the Human Immunodeficiency Virus Envelope Glycoprotein Gp120 on Virions Bound to Target Cells
- Dependence of Intracellular and Exosomal microRNAs on Viral Oncogene Expression in HPV-positive Tumor Cells
- Identification of a Peptide-Pheromone that Enhances Escape from Host Cell Vacuoles
- Impaired Systemic Tetrahydrobiopterin Bioavailability and Increased Dihydrobiopterin in Adult Falciparum Malaria: Association with Disease Severity, Impaired Microvascular Function and Increased Endothelial Activation
- Transgenic Expression of the Dicotyledonous Pattern Recognition Receptor EFR in Rice Leads to Ligand-Dependent Activation of Defense Responses
- Comprehensive Antigenic Map of a Cleaved Soluble HIV-1 Envelope Trimer
- Low Doses of Imatinib Induce Myelopoiesis and Enhance Host Anti-microbial Immunity
- Impaired Systemic Tetrahydrobiopterin Bioavailability and Increased Oxidized Biopterins in Pediatric Falciparum Malaria: Association with Disease Severity
- PLOS Pathogens
- Archiv čísel
- Aktuální číslo
- Informace o časopisu
Nejčtenější v tomto čísle- Bacterial Immune Evasion through Manipulation of Host Inhibitory Immune Signaling
- BILBO1 Is a Scaffold Protein of the Flagellar Pocket Collar in the Pathogen
- Antimicrobial-Induced DNA Damage and Genomic Instability in Microbial Pathogens
- Attenuation of Tick-Borne Encephalitis Virus Using Large-Scale Random Codon Re-encoding
Kurzy
Zvyšte si kvalifikaci online z pohodlí domova
Současné možnosti léčby obezity
nový kurzAutoři: MUDr. Martin Hrubý
Všechny kurzyPřihlášení#ADS_BOTTOM_SCRIPTS#Zapomenuté hesloZadejte e-mailovou adresu, se kterou jste vytvářel(a) účet, budou Vám na ni zaslány informace k nastavení nového hesla.
- Vzdělávání



