-
Články
Top novinky
Reklama- Vzdělávání
- Časopisy
Top články
Nové číslo
- Témata
Top novinky
Reklama- Videa
- Podcasty
Nové podcasty
Reklama- Kariéra
Doporučené pozice
Reklama- Praxe
Top novinky
ReklamaFungal Nail Infections (Onychomycosis): A Never-Ending Story?
article has not abstract
Published in the journal: . PLoS Pathog 10(6): e32767. doi:10.1371/journal.ppat.1004105
Category: Pearls
doi: https://doi.org/10.1371/journal.ppat.1004105Summary
article has not abstract
Is Onychomycosis Still a Problem?
The great majority of superficial fungal infections are caused by dermatophytes, which belong to one of three genera (Trichophyton, Epidermophyton, and Microsporum), with T. rubrum being the most prominent cause of nail infection (Figure 1). Table 1 summarizes the prevalence of various superficial fungal infections in different geographic areas [1]. Among superficial fungal infections, by far the most difficult to cure is toenail onychomycosis (Figure 2). The prevalence of onychomycosis has been reported to be as high as 23% across Europe [2] and 20% in East Asia [3]. In North America, the incidence of onychomycosis is up to 14% [4], with fungal infection responsible for 50% of all nail disease [5]. With millions of dollars being spent annually on oral and topical prescriptions, laser treatments, over-the-counter products, and home remedies, it is obvious that people are still bothered by their fungal toenail infections and are determined to get rid of them. Unfortunately, this is easier said than done. To successfully cure toenail onychomycosis requires long treatment duration that may extend to a full year. Even then, complete cure, defined as clinical cure (implying nail clearing) plus mycological cure (both negative microscopy and dermatophyte culture), is often unattainable.
Fig. 1. <i>Trichophyton rubrum</i> colony and microscopic appearance (40x). 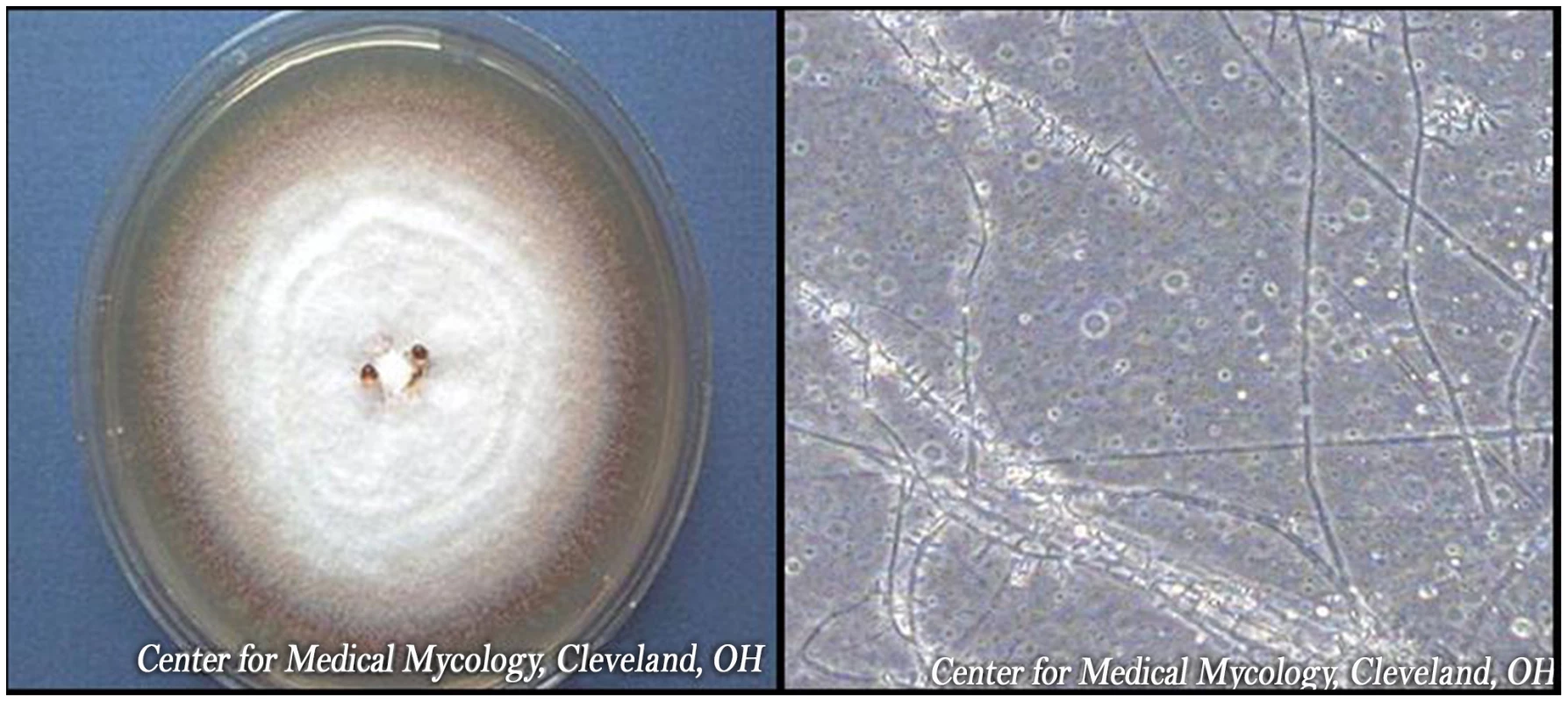
#obr:2#
#tab:1#
What Are the Risk Factors for Toenail Onychomycosis?
The most prevalent predisposing risk factor for developing onychomycosis is advanced age, which is reported to be 18.2% in patients 60–79 years of age, compared to 0.7% in patients younger than 19 years of age. Further, men are up to three times more likely to have onychomycosis than women, though the reasons for this gender difference are not clear [6]. Moreover, the low prevalence of infection in people whose spouses have onychomycosis compared to the prevalence among their children suggests a genetic risk factor [7]. Though extremely rare, one study reported four family members from seven unrelated groups with a common genetic trait (autosomal recessive CARD9 deficiency) who developed a dermatophyte infection of deep tissues that proved fatal [8].
Other risk factors include diabetes and conditions contributing to poor peripheral circulation [9]. In fact, onychomycosis may represent an important predictor for the development of diabetic foot syndrome and foot ulcers [10]. Patients who are immunosuppressed, such as those with HIV infection and those undergoing cancer therapy, are also predisposed to fungal nail infection [11]. There is at least one case report of a toenail infection caused by Fusarium (a non-dermatophyte fungus) that developed into a fatal systemic infection in a lymphoma patient following a bone marrow transplant [12].
Several nonclinical risk factors also affect a person's chance of developing fungal nail infections. Toenail onychomycosis is not prevalent in tropical climates, presumably because people in those areas are not in the habit of wearing occlusive footwear that create a warm, moist environment for the proliferation of fungi. Further, the spread of foot infections, including tinea pedis (athlete's foot), may occur in places such as shower stalls, bathrooms, or locker rooms where floor surfaces often are wet and people are barefoot [13]. Nail trauma will also increase the risk of fungal infection of the affected nail, especially in the geriatric population [11].
A recent study by our group utilized regression analysis to show that history of tinea pedis plus three clinical variables—onychomycosis, plantar scaling (a clinical sign of tinea pedis), and nail discoloration (a clinical sign of onychomycosis and generally indicative of severe nail infection) were statistically associated with spread of infection in households with multiple infected members (P≤.044) [14].
How Is Onychomycosis Treated?
Treatment of onychomycosis includes chemical or surgical removal of the infected nail, systemic or topical drugs, pulse therapy, or a combination thereof. Table 2 is a summary of oral and topical therapy regimens; as can be seen, the course of treatment for fingernail infections is shorter than for toenail infections. The treatment of onychomycosis has improved considerably over the past several decades, following the introduction of the oral antifungals terbinafine and itraconazole. However, these drugs may have side effects such as liver damage or drug interactions, which are particularly relevant in the elderly population [15]. Further, nail infections caused by non-dermatophyte organisms, such as Fusarium, are especially difficult to treat [16].
#tab:2#
Why Don't Topical Antifungals Work Better?
Unfortunately, currently available topical agents, such as amorolfine 5% and ciclopirox 8%, have low efficacy (approximately 5%–12%) [17], [18]. This low efficacy can mainly be attributed to the inability of the drug to penetrate through the nail plate to the nail bed where the infection resides [19]. Thickened nails, extensive involvement of the entire nail, lateral disease, and yellow spikes contribute to a poor response to topical treatment [11]. Figure 1 shows an example of distal subungual onychomycosis, trimmed to demonstrate nail thickening.
Further complicating the scenario is the fact that certain antifungals will bind to the nail plate and thus may not be available at the site of infection, which is the nail bed. For example, terbinafine has been shown to accumulate rapidly in the nail, reaching a maximum of 0.39 mg/g and persisting up to 2 months following the end of treatment [20]. In this regard, Ryder et al. developed an in vitro nail model that showed that the cidal action of terbinafine, when tested against an established dermatophyte infection in the presence of human nail, was in fact less effective than in conventional microdilution assays where no nail powder is present [21].
Many different approaches to solving the problem of nail penetration have been attempted recently. For example, there have been attempts to develop penetration enhancers to facilitate drug delivery through the nail plate, such as addition of dodecyl-2-N,N-dimethylaminopropionate hydrochloride (DDAIP HCl, trade name NexACT-88; NexMed) to terbinafine nail lacquer [19]. Another technique to enhance the penetration of nail lacquer was the incorporation of terbinafine into transfersome lipid vesicles, which are highly deformable and thus are able to pass through intercellular spaces [22]. Additionally, a novel small-molecule oxaborole antifungal (AN2690) has recently been developed that is designed for greater penetration through the nail plate [23]. However, to date, none of these topical products has been commercialized.
In this regard, approval of topical onychomycosis drugs by regulatory agencies may be negatively impacted by an overly stringent definition of complete cure, which includes nail clearing plus mycological cure (negative microscopy and culture). Review of data from several international clinical trials by Ghannoum et al. has suggested that reassessment of the definition of onychomycosis cure is critical [24]. In these trials, a high number of toenail samples collected from subjects at the end of clinical trials contained visible fungal hyphae that subsequently failed to grow upon culture. However, current technology does not differentiate between “live” and “dead” fungi, so even though these samples had to be reported as microscopy-positive, the infection may in fact have been cured. The authors propose that, for clinical trials of topical agents, the length of treatment should be extended to 18 months, followed by a longer washout period of 3–6 months before primary assessments to allow the removal of both residual drug in the nail and nonviable fungal cells. Therefore, the absence of clinical signs following an adequate wash out period, coupled with a negative culture, with or without negative microscopy, should be considered the definition of onychomycosis cure. These changes may enable more topical agents to be proven efficacious.
What's New in Onychomycosis Therapy?
Recent device-based therapies for onychomycosis include laser devices, photodynamic therapy, iontophoresis, and ultrasound. Laser treatment has been approved for cosmetic treatment only, but efficacy as a treatment to eradicate the fungal infection will have to be determined by additional randomized controlled trials [25]. There have been rare reports of onychomycosis cures following the use of phototherapy, which involves the irradiation of accumulated protoporphyrin within the fungal hyphae, leading to subsequent hyphal cell damage [26]. The ability of iontophoresis, or the use of electric current (0.5 mA/cm2) to facilitate the passage of drug through the nail plate, has been proven in studies with human cadaver nails, but relevant clinical studies remain to be conducted [27]. Finally, though ultrasound therapy has preliminarily demonstrated fungistatic activity against nail infections [28], the device itself seems overly complicated, with ultrasound transducers and drug delivery compartments needed above each toenail and the requirement for a computer software interface, making it a physician-office–only treatment and likely very expensive [29].
Why Do Patients So Often Relapse?
There are multiple factors that may contribute to the high rate of fungal nail infection recurrence. Patients with a genetic predisposition to onychomycosis, who are immunocompromised, or who have diabetes, are likely to experience relapse and may never achieve a permanent cure [11].
This may be due either to failure to eradicate the infecting fungus or to re-infection with a new fungal strain following subsequent exposure. Arthroconidia, which are chains of fungal conidia that are formed by breakage of the fungal hyphae, are considered to be the primary means of nail invasion. These arthroconidia, which have thicker cell walls than conidia formed in vitro, have been shown to be more resistant to antifungals and, thus, may remain in the nail bed as a reservoir for recurrent disease [30]. However, the incidence of innate resistance among dermatophytes is low. Our Center conducted in vitro susceptibility testing of 140 sequential isolates from subjects who failed treatment in an oral terbinafine clinical trial. In all cases, the minimum inhibitory concentrations (MICs) of terbinafine against each patient set were identical or within one tube dilution, implying no resistance development. The same results were obtained within each set with fluconazole, itraconazole, and griseofulvin (with the exception of one isolate having a 3-fold increase in the MIC). This further indicates that there was no crossresistance between antifungal agents [31]. This study showed that failure to cure the infected nails may be due to host/family factors.
Even in cases where the infecting fungus has been entirely eradicated by antifungal therapy, patients remain at risk for re-infection. As mentioned above, people are exposed to dermatophyte reservoirs in many of their day-to-day activities, including trips to the gym and increased travel. Common sense measures, such as not walking barefoot through public showers or hotel rooms, would help prevent unnecessary exposure. That being said, one of the most common routes of infection is within households. It has long been suspected that nail infections were spread by close contact with family members. However, it wasn't until recently that our group was able to employ molecular techniques to prove that persons within the same household were infected by the same strain of T. rubrum [14]. For those attempting to avoid re-infection, measures such as spraying their shoes with a topical antifungal spray or treating them with a commercial ultraviolet device [32] after each wearing would be prudent. Thus, a patient not only needs to treat the infection but also break the cycle of re-infection.
Zdroje
1. HavlickovaA, CzaikaVA, FriedrichM (2008) Epidemiological trends in skin mycoses worldwide. Mycoses 51 S4 : 2–15.
2. HanekeE, RoseeuwD (1999) The scope of onychomycosis: epidemiology and clinical features. Int J Dermatol 38 Suppl 2 : 7–12.
3. OgasawaraY (2003) Prevalence and patient's consciousness of tinea pedis and onychomycosis. Nihon Ishinkin Gakkai Zasshi 44 : 253–260.
4. GhannoumMA, HajjehRA, ScherR, KonnikovN, GuptaAK, et al. (2000) A large-scale North American study of fungal isolates from nails: the frequency of onychomycosis, fungal distribution, and antifungal susceptibility patterns. J Am Acad Dermatol 43 : 641–648.
5. ScherRK (1994) Onychomycosis is more than a cosmetic problem. Br J Dermatol 130 : 15.
6. GuptaAK, JainHC, LyndeCW, MacDonaldP, CooperEA, et al. (2000) Prevalence and epidemiology of onychomycosis in patients visiting physicians' offices: a multicenter Canadian survey of 15,000 patients. J Am Acad Dermatol 43 : 244–248.
7. FaergemannJ, CorreiaO, NowickiR, RoBI (2005) Genetic predisposition - understanding underlying mechanisms of onychomycosis. J Eur Acad Dermatol Venerol 19 : 17–19.
8. LanternierF, PathanS, VincentQB, LiuL, CypowyjS, etal (2013) Deep dermatophytosis and inherited CARD9 deficiency. N Engl J Med 369 : 1704–1714.
9. SaunteDM, HolgersenJB, HaedersdalM, StraussG, BitschM, et al. (2006) Prevalence of toe nail onychomycosis in diabetic patients. Acta Derm Venerol 86 : 425–428.
10. NenoffP, Ginter-HanselmayerG, TietzHJ (2012) Fungal nail infections - an update: Part 1 - Prevalence, epidemiology, predisposing conditions, and differential diagnosis. Hautarzt 63 : 30–38.
11. ScherRK, BaranR (2003) Onychomycosis in clinical practice: factors contributing to recurrence. Br J Dermatol 149 : 5–9.
12. ArreseJE, Pierard-FranchimontC, PierardGE (1996) Fatal hyalohyphomycosis following Fusarium onychomycosis in an immunocompromised patient. Am J Dermatopathol 18 : 196–198.
13. AlyR (1994) Ecology and epidemiology of dermatophyte infections. J Am Acad Dermatol 31: S21.
14. GhannoumMA, MukherjeePK, WarshawEM, EvansS, KormanNJ, et al. (2013) Molecular analysis of dermatophytes suggest spread of infection among household members. Cutis 91 : 237–246.
15. ElewskiB, TavakkolA (2005) Safety and tolerability of oral antifungal agents in the treatment of fungal nail disease: a proven reality. Ther Clin Risk Manag 1 : 299–306.
16. TostiA, PiracciniBM, LorenziS (2000) Onychomycosis caused by nondermatophyte molds: clinical features and response to treatment of 59 cases. J Am Acad Dermatol 42 : 217–224.
17. BlueCross BlueShield of Northeastern New York (2006 November 28) Drug Therapy Guidelines: Antifungal Agents Lamisil (terbinafine), Sporanox (itraconazole), Penlac (ciclopirox), Vfend (voriconazole). Drug P&T Newsletter.
18. LauharantaJ (1992) Comparative efficacy and safety of amorolfine nail lacquer 2% versus 5% once weekly. Clin Exp Dermatol 17 : 41–43.
19. GhannoumMA, LongL, PfisterWR (2009) Determination of the efficacy of terbinafine hydrochloride nail solution in the topical treatment of dermatophytosis in a guinea pig model. Mycoses 52 : 35–43.
20. FaergemannJ, ZehenderH, MilleriouxL (1994) Levels of terbinafine in plasma, stratum corneum, dermis-epidermis (without stratum corneum), sebum, hair and nails and after 250 mg terbinafine orally once daily for 7 and 14 days. Clin Exp Dermatol 19 : 121–126.
21. OsborneCS, LeitnerI, FavreB, RyderNS (2004) Antifungal drug response in an in vitro model of dermatophyte nail infection. Med Mycol 42 : 159–163.
22. GhannoumM, IshamN, HerbertJ, HenryW, YurdakulS (2011) Activity of TDT 067 (Terbinafine in Transfersome) against Agents of Onychomycosis, as Determined by Minimum Inhibitory and Fungicidal Concentrations. J Clin Microbiol 49 : 1716–1720.
23. AlleyMR, BakerSJ, BeutnerKR, PlattnerJ (2007) Recent progress on the topical therapy of onychomycosis. Expert Opin Investig Drugs 16 : 157–167.
24. GhannoumM, IshamN, CatalanoV (2013) A Second Look at Efficacy Criteria for Onychomycosis: Clinical and Mycological Cure. Br J Dermatol. E-pub ahead of print. doi:10.1111/bjd.12594
25. GuptaAK, SimpsonFC (2013) Laser therapy for onychomycosis. J Cutan Med Surg 17 : 301–307.
26. HarrisF, PierpointL (2012) Photodynamic therapy based on 5-aminolevulinic acid and its use as an antimicrobial agent. Med Res Rev 32 : 1292–1327.
27. Delgado-CharroMB (2012) Iontophoretic drug delivery across the nail. Expert Opin Drug Deliv 9 : 91–103.
28. SilvaJL, DoimoG, FariaDP (2011) The use of high frequency waves to treat onychomycosis: preliminary communication of three cases. An Bras Dermatol 86 : 598–600.
29. AbadiD, ZdericV (2011) Ultrasound-mediated nail drug delivery system. J Ultrasound Med 30 : 1723–1730.
30. YazdanparastSA, BartonRC (2006) Arthroconidia production in Trichophyton rubrum and a new ex vivo model of onychomycosis. J Med Microbiol 55 : 1577–1581.
31. BradleyM, LeidichS, IshamN, ElewskiB, GhannoumM (1999) Antifungal susceptibilities and genetic relatedness of serial Trichophyton rubrum isolates from patients with onychomycosis of the toenail. Mycoses 42 : 105–110.
32. GhannoumMA, IshamN, LongL (2012) Optimization of an infected shoe model for the evaluation of an ultraviolet shoe sanitizer device. J Am Podiatr Med Assoc 102 : 309–313.
Štítky
Hygiena a epidemiologie Infekční lékařství Laboratoř
Článek Recruitment of RED-SMU1 Complex by Influenza A Virus RNA Polymerase to Control Viral mRNA SplicingČlánek Systematic Phenotyping of a Large-Scale Deletion Collection Reveals Novel Antifungal Tolerance GenesČlánek The Contribution of Social Behaviour to the Transmission of Influenza A in a Human Population
Článek vyšel v časopisePLOS Pathogens
Nejčtenější tento týden
2014 Číslo 6- Jak souvisí postcovidový syndrom s poškozením mozku?
- Měli bychom postcovidový syndrom léčit antidepresivy?
- Farmakovigilanční studie perorálních antivirotik indikovaných v léčbě COVID-19
- 10 bodů k očkování proti COVID-19: stanovisko České společnosti alergologie a klinické imunologie ČLS JEP
-
Všechny články tohoto čísla
- Fungal Nail Infections (Onychomycosis): A Never-Ending Story?
- BdlA, DipA and Induced Dispersion Contribute to Acute Virulence and Chronic Persistence of
- Morphotype Transition and Sexual Reproduction Are Genetically Associated in a Ubiquitous Environmental Pathogen
- A Nucleic-Acid Hydrolyzing Single Chain Antibody Confers Resistance to DNA Virus Infection in HeLa Cells and C57BL/6 Mice
- HopW1 from Disrupts the Actin Cytoskeleton to Promote Virulence in Arabidopsis
- Ly6C Monocytes Become Alternatively Activated Macrophages in Schistosome Granulomas with Help from CD4+ Cells
- Recruitment of RED-SMU1 Complex by Influenza A Virus RNA Polymerase to Control Viral mRNA Splicing
- Contribution of Specific Residues of the β-Solenoid Fold to HET-s Prion Function, Amyloid Structure and Stability
- Antibody Responses to : Role in Pathogenesis and Diagnosis of Encephalitis?
- Discovery of a Novel Compound with Anti-Venezuelan Equine Encephalitis Virus Activity That Targets the Nonstructural Protein 2
- Activation of Focal Adhesion Kinase by Suppresses Autophagy via an Akt/mTOR Signaling Pathway and Promotes Bacterial Survival in Macrophages
- Crossing the Interspecies Barrier: Opening the Door to Zoonotic Pathogens
- Catching Fire: , Macrophages, and Pyroptosis
- IscR Is Essential for Type III Secretion and Virulence
- Selective Chemical Inhibition of Quorum Sensing in Promotes Host Defense with Minimal Impact on Resistance
- The Glycosylated Rv1860 Protein of Inhibits Dendritic Cell Mediated TH1 and TH17 Polarization of T Cells and Abrogates Protective Immunity Conferred by BCG
- A Genome-Wide Tethering Screen Reveals Novel Potential Post-Transcriptional Regulators in
- Structural Insights into SraP-Mediated Adhesion to Host Cells
- Human IGF1 Regulates Midgut Oxidative Stress and Epithelial Homeostasis to Balance Lifespan and resistance in
- Cycling Empirical Antibiotic Therapy in Hospitals: Meta-Analysis and Models
- Rab11 Regulates Trafficking of -sialidase to the Plasma Membrane through the Contractile Vacuole Complex of
- Mitogen and Stress Activated Kinases Act Co-operatively with CREB during the Induction of Human Cytomegalovirus Immediate-Early Gene Expression from Latency
- Profilin Promotes Recruitment of Ly6C CCR2 Inflammatory Monocytes That Can Confer Resistance to Bacterial Infection
- A Central Role for Carbon-Overflow Pathways in the Modulation of Bacterial Cell Death
- An Invertebrate Warburg Effect: A Shrimp Virus Achieves Successful Replication by Altering the Host Metabolome via the PI3K-Akt-mTOR Pathway
- The Highly Conserved Bacterial RNase YbeY Is Essential in , Playing a Critical Role in Virulence, Stress Regulation, and RNA Processing
- A Virulent Strain of Deformed Wing Virus (DWV) of Honeybees () Prevails after -Mediated, or , Transmission
- Systematic Phenotyping of a Large-Scale Deletion Collection Reveals Novel Antifungal Tolerance Genes
- Ubiquitin-Mediated Response to Microsporidia and Virus Infection in
- Preclinical Detection of Variant CJD and BSE Prions in Blood
- Toll-Like Receptor 8 Agonist and Bacteria Trigger Potent Activation of Innate Immune Cells in Human Liver
- Progressive Proximal-to-Distal Reduction in Expression of the Tight Junction Complex in Colonic Epithelium of Virally-Suppressed HIV+ Individuals
- The Triggering Receptor Expressed on Myeloid Cells 2 Inhibits Complement Component 1q Effector Mechanisms and Exerts Detrimental Effects during Pneumococcal Pneumonia
- Differential Activation of Acid Sphingomyelinase and Ceramide Release Determines Invasiveness of into Brain Endothelial Cells
- Forward Genetic Screening Identifies a Small Molecule That Blocks Growth by Inhibiting Both Host- and Parasite-Encoded Kinases
- Defining Immune Engagement Thresholds for Control of Virus-Driven Lymphoproliferation
- Growth Factor and Th2 Cytokine Signaling Pathways Converge at STAT6 to Promote Arginase Expression in Progressive Experimental Visceral Leishmaniasis
- Multimeric Assembly of Host-Pathogen Adhesion Complexes Involved in Apicomplexan Invasion
- Biogenesis of Influenza A Virus Hemagglutinin Cross-Protective Stem Epitopes
- Adequate Th2-Type Response Associates with Restricted Bacterial Growth in Latent Mycobacterial Infection of Zebrafish
- Protective Efficacy of Passive Immunization with Monoclonal Antibodies in Animal Models of H5N1 Highly Pathogenic Avian Influenza Virus Infection
- Fructose-Asparagine Is a Primary Nutrient during Growth of in the Inflamed Intestine
- The Calcium-Dependent Protein Kinase 3 of Influences Basal Calcium Levels and Functions beyond Egress as Revealed by Quantitative Phosphoproteome Analysis
- A Translocated Effector Required for Dissemination from Derma to Blood Safeguards Migratory Host Cells from Damage by Co-translocated Effectors
- Functional Characterization of a Novel Family of Acetylcholine-Gated Chloride Channels in
- Both α2,3- and α2,6-Linked Sialic Acids on O-Linked Glycoproteins Act as Functional Receptors for Porcine Sapovirus
- The Contribution of Social Behaviour to the Transmission of Influenza A in a Human Population
- MicroRNA-146a Provides Feedback Regulation of Lyme Arthritis but Not Carditis during Infection with
- Recombination in Enteroviruses Is a Biphasic Replicative Process Involving the Generation of Greater-than Genome Length ‘Imprecise’ Intermediates
- Cytoplasmic Viral RNA-Dependent RNA Polymerase Disrupts the Intracellular Splicing Machinery by Entering the Nucleus and Interfering with Prp8
- and Are Associated with Murine Susceptibility to Infection and Human Sepsis
- PLOS Pathogens
- Archiv čísel
- Aktuální číslo
- Informace o časopisu
Nejčtenější v tomto čísle- Fungal Nail Infections (Onychomycosis): A Never-Ending Story?
- Profilin Promotes Recruitment of Ly6C CCR2 Inflammatory Monocytes That Can Confer Resistance to Bacterial Infection
- Contribution of Specific Residues of the β-Solenoid Fold to HET-s Prion Function, Amyloid Structure and Stability
- The Highly Conserved Bacterial RNase YbeY Is Essential in , Playing a Critical Role in Virulence, Stress Regulation, and RNA Processing
Kurzy
Zvyšte si kvalifikaci online z pohodlí domova
Současné možnosti léčby obezity
nový kurzAutoři: MUDr. Martin Hrubý
Všechny kurzyPřihlášení#ADS_BOTTOM_SCRIPTS#Zapomenuté hesloZadejte e-mailovou adresu, se kterou jste vytvářel(a) účet, budou Vám na ni zaslány informace k nastavení nového hesla.
- Vzdělávání



