-
Články
Top novinky
Reklama- Vzdělávání
- Časopisy
Top články
Nové číslo
- Témata
Top novinky
Reklama- Videa
- Podcasty
Nové podcasty
Reklama- Kariéra
Doporučené pozice
Reklama- Praxe
Top novinky
Reklama, , and the Human Mouth: A Sticky Situation
article has not abstract
Published in the journal: . PLoS Pathog 9(10): e32767. doi:10.1371/journal.ppat.1003616
Category: Pearls
doi: https://doi.org/10.1371/journal.ppat.1003616Summary
article has not abstract
Introduction
The human mouth with its diverse niches and ample supply of nutrients is undoubtedly conducive for the unrestricted formation of natural microbial biofilms. The oral microbial communities are some of the most complex microbial floras in the human body, consisting of more than 700 different bacterial species [1], [2]. Occurrence of disease results from disturbance of the equilibrium of this complex ecosystem, where population shifts lead to overrepresentation of pathogenic species which contribute to the onset and progression of the most common oral diseases, caries and periodontal disease [3]. Culture-independent molecular methods such as proteomics and 16S rRNA sequencing aiming to determine the bacterial diversity in the human oral cavity have demonstrated that in the supragingival plaque, S. mutans was the dominant species, with elevated levels of other streptococci including S. sanguinis, S. mitis, and S. salivarius in addition to lactobacilli and Veillonella. In contrast, the subgingival plaque was made up primarily of Gram-negative anaerobic bacteria such as Fusobacterium nucleatum, Porphyromonas gingivalis, and Prevotella intermedia which are known to be periodontal pathogens [3]–[5].
The dental tissues—enamel, dentin, and cementum—constitute the oral solid surfaces coated by a pellicle to which the microbial cells attach. The primary colonizers and secondary organisms stick to each other on the surface of teeth and generate a matrix of exopolysaccharide within which cells grow, forming a community with a collective physiology [6]. The resulting biofilm formed, known as dental plaque, subjects the teeth and gingival tissues to high concentrations of microbial metabolites which result in dental disease [2], [7]. The interactions between the various species in these mixed biofilms can be synergistic in that the presence of one microorganism generates a niche for other pathogenic microorganisms which can serve to facilitate the retention of organisms, an oral phenomenon known as coaggregation [3], [8]. The bacteria in the biofilm are always metabolically active which causes fluctuations in pH and loss of minerals from the tooth, ultimately resulting in dissolution of the dental hard tissues and formation of lesions known as dental caries [6], [9]. Interestingly, metabolic communications among oral bacteria may occur where the excretion of a metabolite by one organism is used as a nutrient by other organisms and breakdown of a substrate by enzymatic activity of one organism creates available substrates for different organisms [10], [11].
Dental Caries
Dental caries or tooth decay is among the most prevalent human diseases, second only to the common cold [12]. Caries is a chronic disease that progresses slowly and is characterized by localized and irreversible destruction of the tooth [13], [14]. Despite scientific advancements in cariology in the past 150 years, dental caries remains a serious issue worldwide, particularly in children where it is the primary source of tooth loss. In the United States, 42% of children of ages between 2 to 11 have had dental caries in their primary teeth, and in the adult population, dental caries and periodontal diseases affect 60–90% of individuals worldwide [13]. People with disabilities and lower socioeconomic status suffer from the highest prevalence and pathogenicity of dental caries. Caries results from the complex interactions among the microbial species adhering to the tooth surface, with dietary, salivary, and genetic influences. The metabolic microbial interactions that take place in the dental biofilm result in acid production and extracellular glucan formation which promote microbial attachment to teeth [6], [12], [13]. Ninety percent of carious lesions occur in the pits and fissures of permanent posterior teeth and molar teeth as the biofilm tends to stagnate and mature in these areas which are relatively protected from mechanical wear by the tongue, cheeks, and tooth brushing [6]. The recognition of acid as the central etiological agent in dental caries initiated a search for the causative microorganisms in the oral microbiota, and in the early 1960s, the bacterial species Streptococcus mutans (S. mutans) became the main focus of caries research, assumed to be the specific cariogen [15].
Streptococcus mutans: The Usual Suspect
Streptococcus mutans are Gram-positive bacteria that reside in the human mouth and, more specifically, in the multispecies biofilms on the surfaces of teeth [14]. Streptococcus mutans are major cariogenic organisms—the result of their ability to produce large quantities of glucans as well as acid, exceeding the salivary buffering capacities, which gives the bacteria an advantage to outcompete noncariogenic commensal species at low pH environments [9], [16]. This ability to survive in an acid environment by modulating sugar metabolic pathways coupled with irreversible binding to teeth is a key component to S. mutans pathogenesis. In the second stage of invasion, S. mutans coadhere or coaggregate with other microbial species, followed by proliferation and spread into other sites in the oral mucosa modulated by concerted action of genes and signaling molecules. In the final stage, the biofilm reaches a steady state which changes the equilibrium balance of the oral ecology; as a result, bacteria gain access into the deeper tissues and recesses in the gingival areas, ultimately causing dissolution of hydroxyapatite crystals in enamel and dentin which results in cavitation within the tooth [12], [17]. If not prevented, this cavitation provides an ecological niche where microorganisms form a protected biofilm, enabling caries to progress gradually [13]. Interestingly however, although it has been accepted for decades that S. mutans is the etiologic agent of dental caries, recent evidence indicates high prevalence for S. mutans in dental biofilms where the fungal pathogen Candida albicans (C. albicans) resides, suggesting that the interaction between these diverse species may mediate cariogenic development [18], [19].
Candida albicans: Partner in Crime?
Candida albicans is a commensal fungal species commonly colonizing human mucosal surfaces [20]. However, under conditions of immune dysfunction such as HIV infection, C. albicans can become opportunistic pathogens causing mucosal and disseminated infections. The ability of C. albicans to switch its morphology between yeast and hyphal forms contributes to its pathogenesis [20]. In the oral cavity, the coadhesion between C. albicans and oral bacteria is crucial for C. albicans colonization and persistence [21]. In addition to providing adhesion sites, the streptococci excrete lactate that can act as a carbon source for yeast growth, which in turn reduces oxygen tension to levels preferred by streptococci and provide growth stimulatory factors for the bacteria [21]. Increasing interest worldwide seems to focus on the role of C. albicans coaggregation with S. mutans during adherence to dental surfaces [18]. The hypothesis of the association between S. mutans and C. albicans is based on their mechanisms of virulence and biochemical characteristics as well as host factors that provide a buccal environment favoring the action of both microorganisms [17]–[19]. In fact, several in vitro studies have shown that C. albicans enhance the adherence of S. mutans, indicating a possible facilitation mechanism during their association where the yeast cells could be used by the bacteria as support for adherence [17], [19]. Scanning electron microscopic analysis of mixed species biofilms grown on human teeth and hydroxyapatite as substrata confirmed the strong coadherence between C. albicans and S. mutans to these surfaces and to each other, with S. mutans exhibiting high affinity to the C. albicans hyphae (Figures 1 and 2). More importantly, the yeast's potential to induce dental caries as a consequence of its pronounced ability to produce and tolerate acids was supported by a recent study by Klinke et al. [22], providing experimental evidence in vivo that C. albicans is capable of causing advanced occlusal caries in rats at a high rate. The findings from these in vitro and animal studies attributing a role for C. albicans in caries development and/or progression were solidified by data from a clinical study where the occurrence of caries in children was positively correlated with the frequency of oral candidal carriage [17]. Although still in its infancy, the research thus far strongly warrants that investigations on the microbiology of caries should include yeasts [22].
Fig. 1. Scanning electron micrographs of mature mixed biofilms of C. albicans and S. mutans grown on extracted human teeth, demonstrating the tight coadherence between C. albicans hyphae (red arrows) and S. mutans cells (blue arrows). 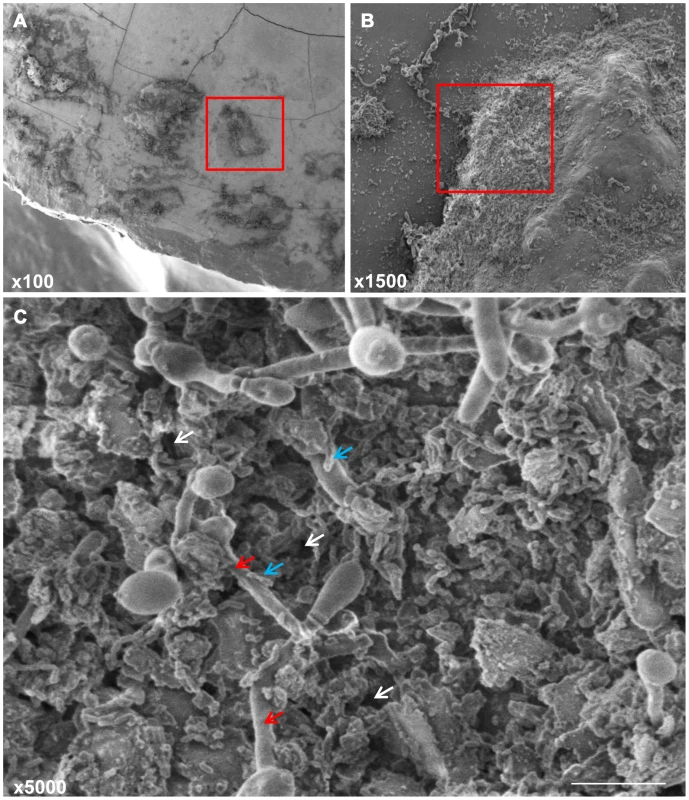
Microbial cells can be seen embedded in a matrix of extracellular polymeric substance with water channels (white arrows) through which liquid flows distributing nutrients and signaling molecules that facilitate communication between the cells. Bars 10 µm. Fig. 2. Scanning electron micrographs of mature mixed biofilms formed on discs of hydroxyapatite (a major component and essential ingredient of normal teeth), demonstrating the affinity of S. mutans to the hyphal elements of C. albicans. 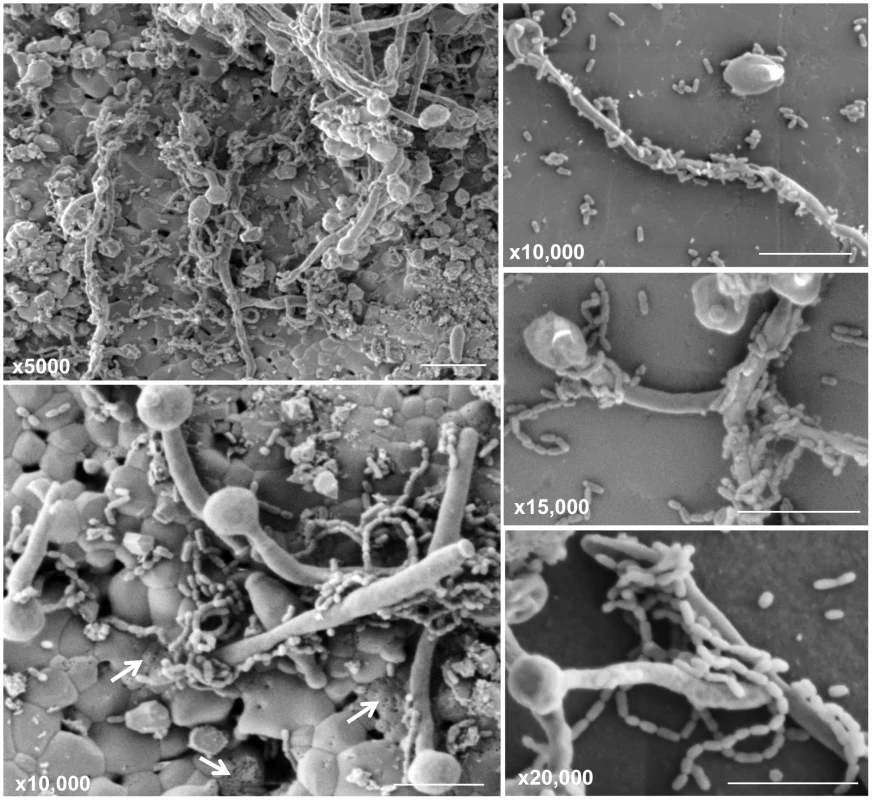
Bacterial cells are seen attached in chains as they adhere to and wrap around the hyphae. Perforations can be seen in the hydroxyapatite surface (white arrows), possibly the result of decalcification of the material due to the high acidic environment. Bars 10 µm. Therapy and Challenges
As teeth loss in both children and adults has become a financial burden worldwide, understanding the homeostatic synchrony between the resident microflora, thereby preventing biofilm-induced caries and improving the quality of life, has become crucial. Although regular removal of biofilm on the tooth and the incorporation of fluoride in toothpaste has been the mainstay of dental caries prevention, these practices offer incomplete protection and may not effectively address the infectious character of the disease [6], [16]. Unfortunately, designing effective therapies to treat caries has been a major challenge, particularly in terms of oral drug delivery systems that can penetrate the biofilm networks of the target location [12], [16]. Antimicrobial peptides such as the histatins are considered promising agents due to their broad-spectrum antimicrobial properties [23], [24]. However, several questions about the use of these molecules as a tool for microbial control remain unclear. The recent search for more effective antimicrobials has explored the potential use of nanotechnology to improve the physical and chemical properties of drugs where nanosystem formulations incorporating different agents can improve stability and antimicrobial activity [25]. Other studies investigated the use of active inhibitors of enzymes that make up the exopolysaccharide matrix, thereby affecting the cariogenic biofilm assembly. Data generated from these studies demonstrated that in combination with fluoride, the new antibiofilm compounds successfully inactivated exopolysaccharide accumulation and matrix development [16]. However, although promising, these compounds are yet to be justified in in vivo studies to further evaluate their applicability paving the direction toward clinical applications.
Conclusion and Future Directions
Microbial community interactions in health and caries pathogenesis are not well understood. It has been proposed that the translocation of oral bacteria to remote sites can lead to systemic diseases such as coronary artery disease [3]. Therefore, unraveling the basis of dental plaque development will ultimately contribute to both oral and overall health. To that end, using molecular techniques, current studies are focusing on identifying associations between oral bacteria and various oral and systemic diseases. Although in vitro studies can contribute to our understanding of the complex microbial associations and the dynamics of their interaction in the oral environment, the immunocompetence of the host and factors such as diet and oral hygiene play an important regulatory function. To better understand the impact of the interaction between C. albicans and S. mutans on caries development in a host, it is crucial to determine mechanistically precise details of adhesion and signaling under conditions of coexistence and to identify the molecular processes involved in the development of cariogenic biofilms in the host. By manipulation of adhesion interactions, it may be possible to develop new protocols to block adhesive reactions, impeding development of biofilm-related oral disease such as dental caries [9], [22], [26]. Therefore, the presence of C. albicans in the oral environment can now be considered an additional factor that needs to be taken into account in evaluating risks to caries [18]. To that end, future studies should focus on clinical studies and on designing animal model systems to study in vivo–grown polymicrobial biofilms, with the goal of developing novel therapeutic strategies to prevent dental caries through targeted actions.
Zdroje
1. DewhirstFE, ChenT, IzardJ, PasterBJ, TannerACR, et al. (2010) The human oral microbiome. J Bacteriol 192 : 5002–5017 doi: 10.1128/JB.00542-10
2. JenkinsonHF, LamontRJ (2005) Oral microbial communities in sickness and in health. Trends Microbiol 13 : 589–595.
3. KuboniwaM, TribbleGD, HendricksonEL, AmanoA, LamontRJ, et al. (2012) Insights into the virulence of oral biofilms: discoveries from proteomics. Expert Rev Proteomics 9 : 311–323.
4. PasterB, BochesSK, GalvinJL, EricsonRE, LauCN, et al. (2001) Bacterial diversity in human subgingival plaque. J Bacteriol 183 : 3770–3783.
5. GrossEL, BeallCJ, KutschSR, FirestoneND, LeysEJ, et al. (2012) Beyond Streptococcus mutans: dental caries onset linked to multiple species by 16S rRNA community analysis. PLoS ONE 7: e47722 doi:10.1371/journal.pone.0047722
6. KiddEAM, FejerskovO (2004) What constitutes dental caries? Histopathology of carious enamel and dentin related to the action of cariogenic biofilms. J Dent Res 83: C35–C38.
7. KolenbranderPE, AnsersonRX, BlehertDS, EglandPG, FosterJS, et al. (2002) Communication among oral bacteria. Microbiol Mol Biol Rev 66 : 486–505.
8. RickardAH, GilbertP, HighNJ, KolenbranderPE, HandleyPS (2003) Bacterial coaggregation: an integral process in the development of multi-species biofilms. Trends Microbiol 11 : 94–100.
9. LemosJA, QuiveyRGJr, KooH, AbranchesJ (2013) Streptococcus mutans: a new Gram-positive paradigm? Microbiology 159 : 436–45.
10. HojoK, NagaokaS, OhshimaT, MaedaN (2009) Bacterial interactions in dental biofilm development. J Dent Res 88 : 982–990.
11. KleinbergT (1999) Acids formed aerobically and anaerobically by pure and mixed cultures of oral bacteria from oxidizable sugar, organic acid and amino acid substrates. J Dent Res 78 : 211.
12. Isalm BKS, KhanAU (2007) Dental caries: from infection to prevention. Med Sci Monit 13: RA196–203.
13. RouabhiaM, ChmielewskiW (2012) Diseases associated with oral polymicrobial biofilms. Open Mycol J 6 : 27–32.
14. ZeroDTFM, Martinez-MierEA, Ferrera-ZandonaA, AndoM, Gonzalez-CabezasC, et al. (2009) The biology, prevention, diagnosis and treatment of dental caries. JADA 140 : 25S–34S.
15. KlinkeT, KneistS, de SoetJJ, KuhlischE, MauersbergerS, et al. (2009) Acid production by oral strains of Candida albicans and lactobacilli. Caries Res 43 : 83–91.
16. FalsettaML, KleinMI, LemosJA, SilvaBB, AgidiS, et al. (2012) Novel antibiofilm chemotherapy targets exoplysaccharide synthesis ad stress tolerance in Streptococcus mutans to modulate virulence expression in vivo. Antimicrob Agents Chemother 56 : 6201–6211.
17. RajaM, HannanA, AliK (2010) Association of oral candidal carriage with dental caries in children. Caries Res 44 : 272–276.
18. BarbieriDdS'AV, VicenteVA, FraizFC, LavorantiOJ, SvidzinskiTIE, et al. (2007) Analysis of the in vitro adherence of Streprococcus mutans and Candida albicans. Braz J Microbiol 38 : 624–663.
19. JaroszLM, DengDM, van der MeiHC, CrielaardW, KromBP (2009) Streptococcus mutans competence-stimulating peptide inhibits Candida albicans hypha formation. Eukaryotic Cell 8 : 1658–1664.
20. Calderone RA, editor (2012) Candida and Candidiasis. Washington: ASM Press.
21. Brogden KM, Guthmiller JM, editors (2008) Polymicrobial diseases. Washington: ASM Press.
22. KlinkeT, GuggenheimB, KlimmW, ThurnheerT (2011) Dental caries in rats associated with Candida albicans. Caries Res 45 : 100–106.
23. PetersBM, ShirtliffME, Jabra-RizkMA (2010) Antimicrobial peptides: primeval molecules or future drugs? PLoS Pathog 6: e1001067 doi:10.1371/journal.ppat.1001067
24. da SilvaBR, Nascimento-NetoLG, CarneiroVA, ArrudaFV, de AguilarAS, et al. (2012) Antimicrobial peptide control of pathogenic microorganisms of the oral cavity: a review of the literature. Peptides 36 : 315–321.
25. PupeCG, VillardiM, RodriguesCR, RochaHVA, MaiaLC, et al. (2011) Preparation and evaluation of antimicrobial activity of nanosystems for the control of oral pathogens Streptococcus mutans and Candida albicans. Int J Nanomedicine 6 : 2581–2590.
26. BowenW (2013) Rodent model in caries research. Odontology 101 : 9–14.
Štítky
Hygiena a epidemiologie Infekční lékařství Laboratoř
Článek vyšel v časopisePLOS Pathogens
Nejčtenější tento týden
2013 Číslo 10- Jak souvisí postcovidový syndrom s poškozením mozku?
- Měli bychom postcovidový syndrom léčit antidepresivy?
- Farmakovigilanční studie perorálních antivirotik indikovaných v léčbě COVID-19
- 10 bodů k očkování proti COVID-19: stanovisko České společnosti alergologie a klinické imunologie ČLS JEP
-
Všechny články tohoto čísla
- Are We There Yet? Recent Progress in the Molecular Diagnosis and Novel Antifungal Targeting of and Invasive Aspergillosis
- Fungal Iron Availability during Deep Seated Candidiasis Is Defined by a Complex Interplay Involving Systemic and Local Events
- Emergence of Azole-Resistant Strains due to Agricultural Azole Use Creates an Increasing Threat to Human Health
- Fungal Adenylyl Cyclase Acts As a Signal Sensor and Integrator and Plays a Central Role in Interaction with Bacteria
- Sensing of the Microbial Neighborhood by
- Antivirulence Therapy for Animal Production: Filling an Arsenal with Novel Weapons for Sustainable Disease Control
- The Cell Biology of : How to Teach Using Animations
- A Structure-Guided Mutation in the Major Capsid Protein Retargets BK Polyomavirus
- RNA Biology in Fungal Phytopathogens
- , , and the Human Mouth: A Sticky Situation
- The Gene Is Essential for Resistance to Human Serum in
- Unisexual Reproduction Drives Evolution of Eukaryotic Microbial Pathogens
- Bacterial Pathogens Activate a Common Inflammatory Pathway through IFNλ Regulation of PDCD4
- Bats and Viruses: Friend or Foe?
- Protein Trafficking through the Endosomal System Prepares Intracellular Parasites for a Home Invasion
- IL-22 Mediates Goblet Cell Hyperplasia and Worm Expulsion in Intestinal Helminth Infection
- B Cells Enhance Antigen-Specific CD4 T Cell Priming and Prevent Bacteria Dissemination following Genital Tract Infection
- Alternative Roles for CRISPR/Cas Systems in Bacterial Pathogenesis
- Chemicals, Climate, and Control: Increasing the Effectiveness of Malaria Vector Control Tools by Considering Relevant Temperatures
- Dengue Vaccines: Strongly Sought but Not a Reality Just Yet
- Feeding Uninvited Guests: mTOR and AMPK Set the Table for Intracellular Pathogens
- Driven Enforced Viral Replication in Dendritic Cells Contributes to Break of Immunological Tolerance in Autoimmune Diabetes
- IL-4Rα-Associated Antigen Processing by B Cells Promotes Immunity in Infection
- A Gammaherpesvirus Uses Alternative Splicing to Regulate Its Tropism and Its Sensitivity to Neutralization
- MicroRNA-155 Promotes Autophagy to Eliminate Intracellular Mycobacteria by Targeting Rheb
- Epigenetic Dominance of Prion Conformers
- MAIT Cells Detect and Efficiently Lyse Bacterially-Infected Epithelial Cells
- The Role of TcdB and TccC Subunits in Secretion of the Tcd Toxin Complex
- A Mechanism for the Inhibition of DNA-PK-Mediated DNA Sensing by a Virus
- PLOS Pathogens
- Archiv čísel
- Aktuální číslo
- Informace o časopisu
Nejčtenější v tomto čísle- Dengue Vaccines: Strongly Sought but Not a Reality Just Yet
- MicroRNA-155 Promotes Autophagy to Eliminate Intracellular Mycobacteria by Targeting Rheb
- Alternative Roles for CRISPR/Cas Systems in Bacterial Pathogenesis
- Feeding Uninvited Guests: mTOR and AMPK Set the Table for Intracellular Pathogens
Kurzy
Zvyšte si kvalifikaci online z pohodlí domova
Současné možnosti léčby obezity
nový kurzAutoři: MUDr. Martin Hrubý
Všechny kurzyPřihlášení#ADS_BOTTOM_SCRIPTS#Zapomenuté hesloZadejte e-mailovou adresu, se kterou jste vytvářel(a) účet, budou Vám na ni zaslány informace k nastavení nového hesla.
- Vzdělávání



