-
Články
Top novinky
Reklama- Vzdělávání
- Časopisy
Top články
Nové číslo
- Témata
Top novinky
Reklama- Videa
- Podcasty
Nové podcasty
Reklama- Kariéra
Doporučené pozice
Reklama- Praxe
Top novinky
ReklamaRare Copy Number Variants Are a Common Cause of Short Stature
Human growth has an estimated heritability of about 80%–90%. Nevertheless, the underlying cause of shortness of stature remains unknown in the majority of individuals. Genome-wide association studies (GWAS) showed that both common single nucleotide polymorphisms and copy number variants (CNVs) contribute to height variation under a polygenic model, although explaining only a small fraction of overall genetic variability in the general population. Under the hypothesis that severe forms of growth retardation might also be caused by major gene effects, we searched for rare CNVs in 200 families, 92 sporadic and 108 familial, with idiopathic short stature compared to 820 control individuals. Although similar in number, patients had overall significantly larger CNVs (p-value<1×10−7). In a gene-based analysis of all non-polymorphic CNVs>50 kb for gene function, tissue expression, and murine knock-out phenotypes, we identified 10 duplications and 10 deletions ranging in size from 109 kb to 14 Mb, of which 7 were de novo (p<0.03) and 13 inherited from the likewise affected parent but absent in controls. Patients with these likely disease causing 20 CNVs were smaller than the remaining group (p<0.01). Eleven (55%) of these CNVs either overlapped with known microaberration syndromes associated with short stature or contained GWAS loci for height. Haploinsufficiency (HI) score and further expression profiling suggested dosage sensitivity of major growth-related genes at these loci. Overall 10% of patients carried a disease-causing CNV indicating that, like in neurodevelopmental disorders, rare CNVs are a frequent cause of severe growth retardation.
Published in the journal: . PLoS Genet 9(3): e32767. doi:10.1371/journal.pgen.1003365
Category: Research Article
doi: https://doi.org/10.1371/journal.pgen.1003365Summary
Human growth has an estimated heritability of about 80%–90%. Nevertheless, the underlying cause of shortness of stature remains unknown in the majority of individuals. Genome-wide association studies (GWAS) showed that both common single nucleotide polymorphisms and copy number variants (CNVs) contribute to height variation under a polygenic model, although explaining only a small fraction of overall genetic variability in the general population. Under the hypothesis that severe forms of growth retardation might also be caused by major gene effects, we searched for rare CNVs in 200 families, 92 sporadic and 108 familial, with idiopathic short stature compared to 820 control individuals. Although similar in number, patients had overall significantly larger CNVs (p-value<1×10−7). In a gene-based analysis of all non-polymorphic CNVs>50 kb for gene function, tissue expression, and murine knock-out phenotypes, we identified 10 duplications and 10 deletions ranging in size from 109 kb to 14 Mb, of which 7 were de novo (p<0.03) and 13 inherited from the likewise affected parent but absent in controls. Patients with these likely disease causing 20 CNVs were smaller than the remaining group (p<0.01). Eleven (55%) of these CNVs either overlapped with known microaberration syndromes associated with short stature or contained GWAS loci for height. Haploinsufficiency (HI) score and further expression profiling suggested dosage sensitivity of major growth-related genes at these loci. Overall 10% of patients carried a disease-causing CNV indicating that, like in neurodevelopmental disorders, rare CNVs are a frequent cause of severe growth retardation.
Introduction
Human growth is a highly complex and multifactorial trait, with an estimated heritability of about 80–90% [1]. Since 3% of the general population present with a body height below -2 SD scores (SDS), shortness of stature is one of the common medical concerns in childhood. Uncovering the genetic basis of short stature is not only important for clinical diagnosis, prognosis and genetic counseling of affected individuals and their families, but is also a prerequisite for future development of therapeutic approaches.
In clinical terms, short stature is divided into non-syndromic and syndromic forms, the latter affecting additional distinctive organ systems like brain and heart. In both forms growth retardation can either be of intrauterine or postnatal onset. A disproportion between the limbs and trunk is usually attributed to dysfunctional bone maturation or differentiation. Elucidation of the genetic basis of skeletal dysplasias has highlighted central defects in extracellular proteins, metabolic pathways, signal transduction mechanisms, core proteins, oncogenes and genes processing RNA and DNA as underlying mechanisms of growth [2]–[4]. However, skeletal dysplasias are rare [5], and the most common known causes of short stature are a dysfunctional growth hormone pathway, deficiency of the transcription factor SHOX and Ullrich-Turner syndrome in women [6]–[8]. After excluding these known defects the underlying cause remains unknown in approximately 80% of patients [8]–[10].
Many studies of copy number variants (CNVs) in patients with neuropsychiatric conditions or multiple congenital anomalies showed that de novo or inherited CNVs are pathogenic in up to 20% of patients [11], [12]. With an intermediate length of 1 kb to several Mb they include both duplications and deletions and can affect single exons, one or several genes as well as regulatory sequences. Unraveling pathogenic CNVs by molecular karyotyping also provided new opportunities to identify the genetic basis of several monogenic human diseases [13]–[16].
In this report we present the results of copy number detection in a study group of 200 patients with idiopathic short stature. Based on our hypothesis of rare variants involved in the frequent phenotype of growth retardation, we provide evidence of underlying CNVs in 10% of these patients in a gene based approach. These CNVs encompass known microaberration syndrome regions as well as de novo or inherited regions not yet associated with short stature but containing GWAS loci for height.
Results/Discussion
We now recruited a group of 200 individuals and their families with idiopathic short stature seen in the genetic clinic of the Institute of Human Genetics at the University of Erlangen-Nuremberg to identify yet unknown genetic factors of growth retardation. Height adjusted SD scores were calculated on basis of the Prader Growth charts [17]. We included patients with a height standard deviation score (SDS) of below −2 based on population data or who are significantly below the expected target height for their family. Common causes of short stature such as growth hormone deficiency, Ullrich-Turner syndrome, and SHOX deficiency were excluded where applicable. All patients underwent detailed clinical and dysmorphological evaluation by one of the authors (C.T.T.) and were classified as non-specific for any known genetic aberration. Our study group included 131 patients with isolated short stature (Table 1). 69 individuals presented with additional features such as malformations or a dysmorphic facial gestalt. The mean height SDS was −2.75. 52 individuals showed severe growth retardation of prenatal onset. Patients with significant body disproportions indicating skeletal dysplasias were considered a distinct aetiological group and were not included in this study [4], [18]. Only patients with disproportionate short stature but without radiographic signs suggestive of skeletal dysplasias were retained. A borderline IQ in the range of learning disability was observed in 3%. As these individuals received regular education no specific developmental assessment was available. A control cohort used to exclude common copy number polymorphisms consisted of 820 individuals originating from the same Central European region with either exfoliation syndrome or psoriatic arthritis [19], both late onset disorders not associated with short stature. Copy number variants as a cause of these disorders were foremost excluded and not reported in the literature.
Tab. 1. Overview of the phenotypic characteristics of the patient group. 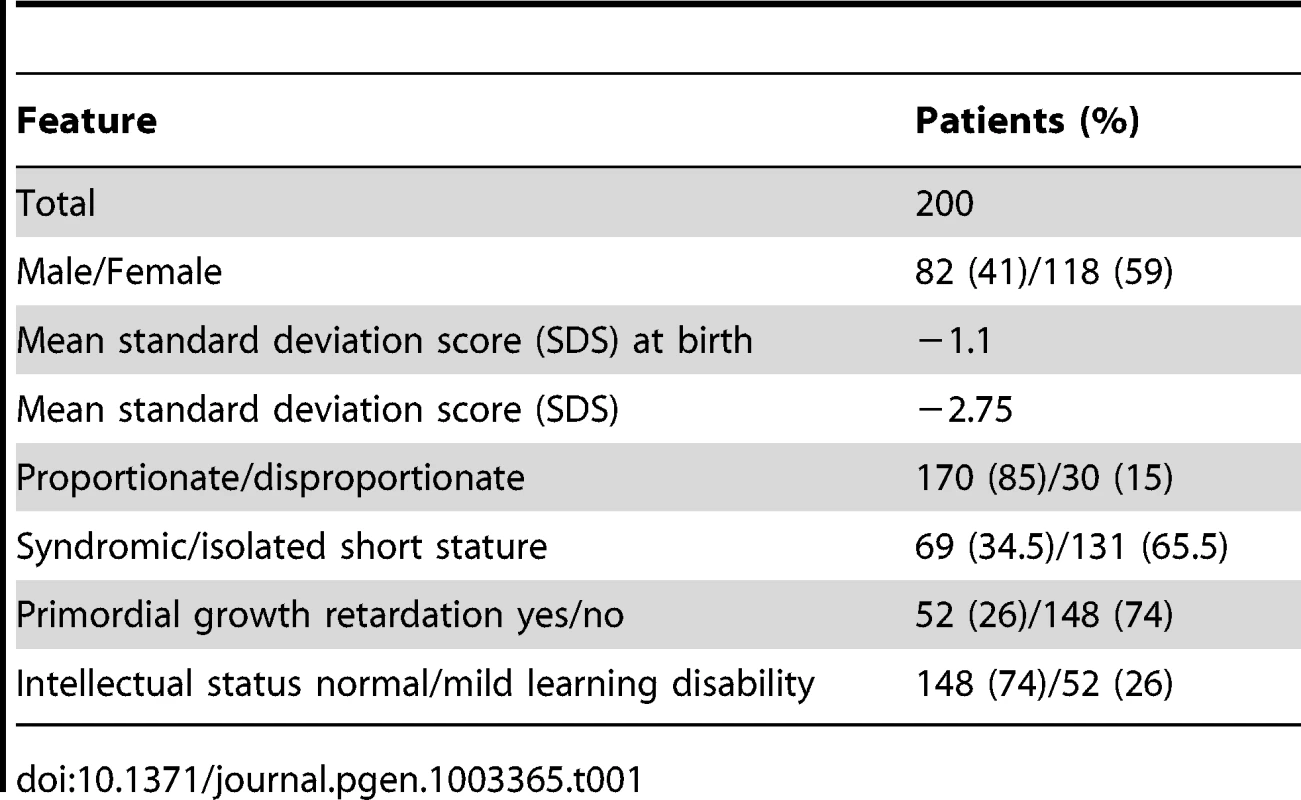
Molecular karyotyping of the 200 patient and the 820 control samples was performed using Genome-Wide Human SNP 6.0 or CytoScan HD arrays (Figure 1). All samples met in-house quality criteria. Overall, we detected 6,338 copy number changes with an average of 32 aberrations per affected individual (Figure 2). When comparing the size range of all observed CNVs in patients (6,338 CNVs) and controls (40,935 CNVs) we determined a size threshold at 99.2 kb (Figure 3A) and found a higher incidence of CNVs with a length of above 100 kb in affected individuals (p-value 1.188×10−7) (Figure 3B). To test for effects of common variants we performed a genome wide CNV association analysis calculating a permutation-based p-value across the CNVs of all individuals. As expected regarding the small cohort size, genome wide association at SNP level to the 20 loci where we identified rare variants was excluded (Figure S1).
Fig. 1. CNV discovery and characterization. 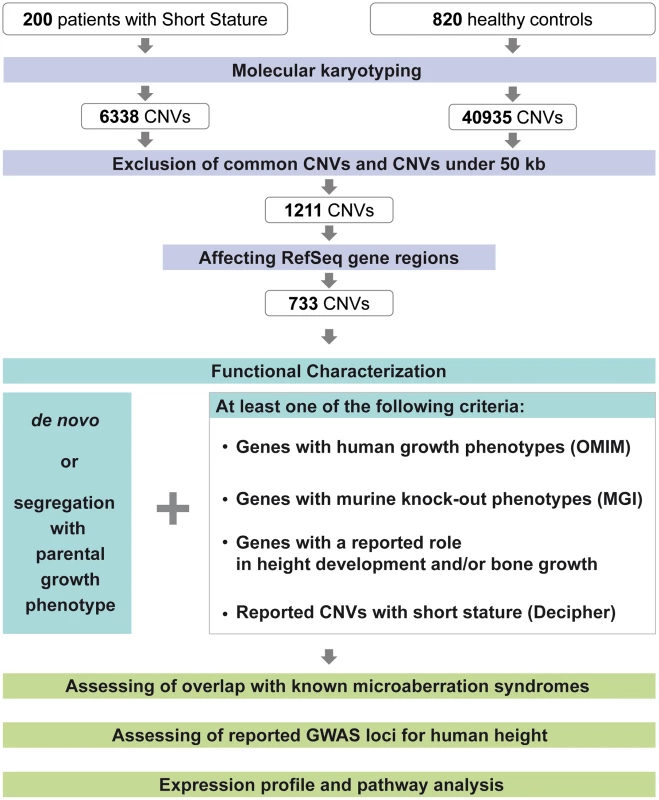
Molecular karyotyping was performed for 200 patients with short stature after thorough clinical evaluation and for 820 healthy control samples. Exclusion of common variants using the control samples and scoring CNVs above 50 kb resulted in an approx. reduction of 80% of the CNVs identified in the patient samples. 60.5% of these CNVs affect reference sequence gene regions. Functional characterization includes segregation analysis using parental arrays and/or MLPA as well as gene and CNV based evaluation. Fig. 2. Molecular karyotyping and MLPA confirmation of identified loci. 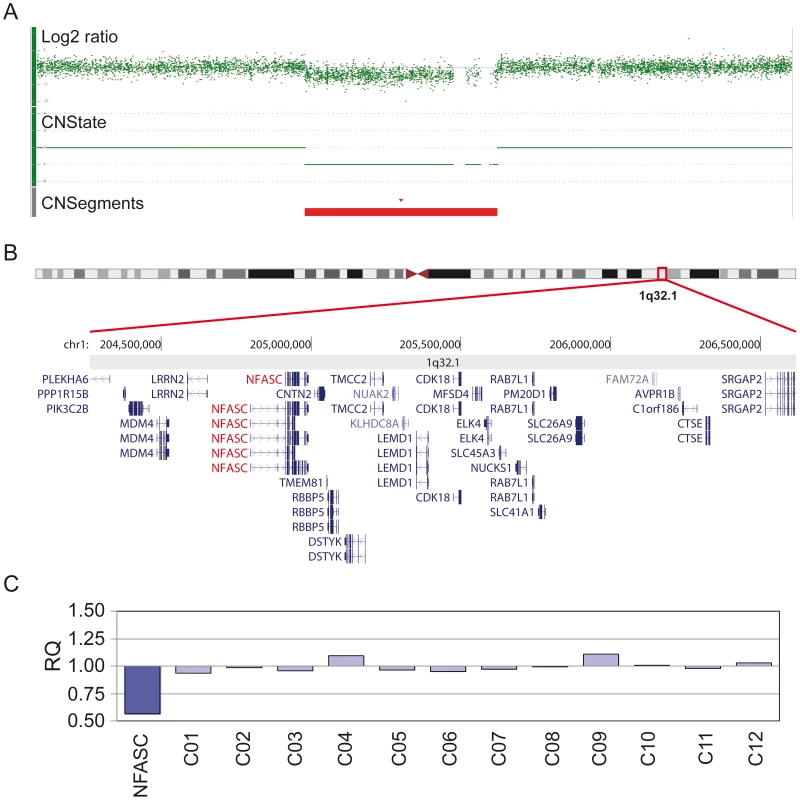
(A) Example representation of the copy number analysis of patient 1 using the Affymetrix Genotyping Console 3.0.2 software. The red bar shows the 2.2 Mb deletion region (CNSegments). (B) Graphical presentation of the deletion region including 33 candidate genes (modified from UCSC genome browser). (C) MLPA confirmation with a probe in the NFASC gene region. A relative quantity value (RQ) below 0.75 was considered as confirmation of a deletion, above 1.25 as confirmation of a duplication. Detailed data for the remaining patients is presented in the supporting information. Fig. 3. Higher incidence of CNVs with a length of above 100 kb in affected individuals. 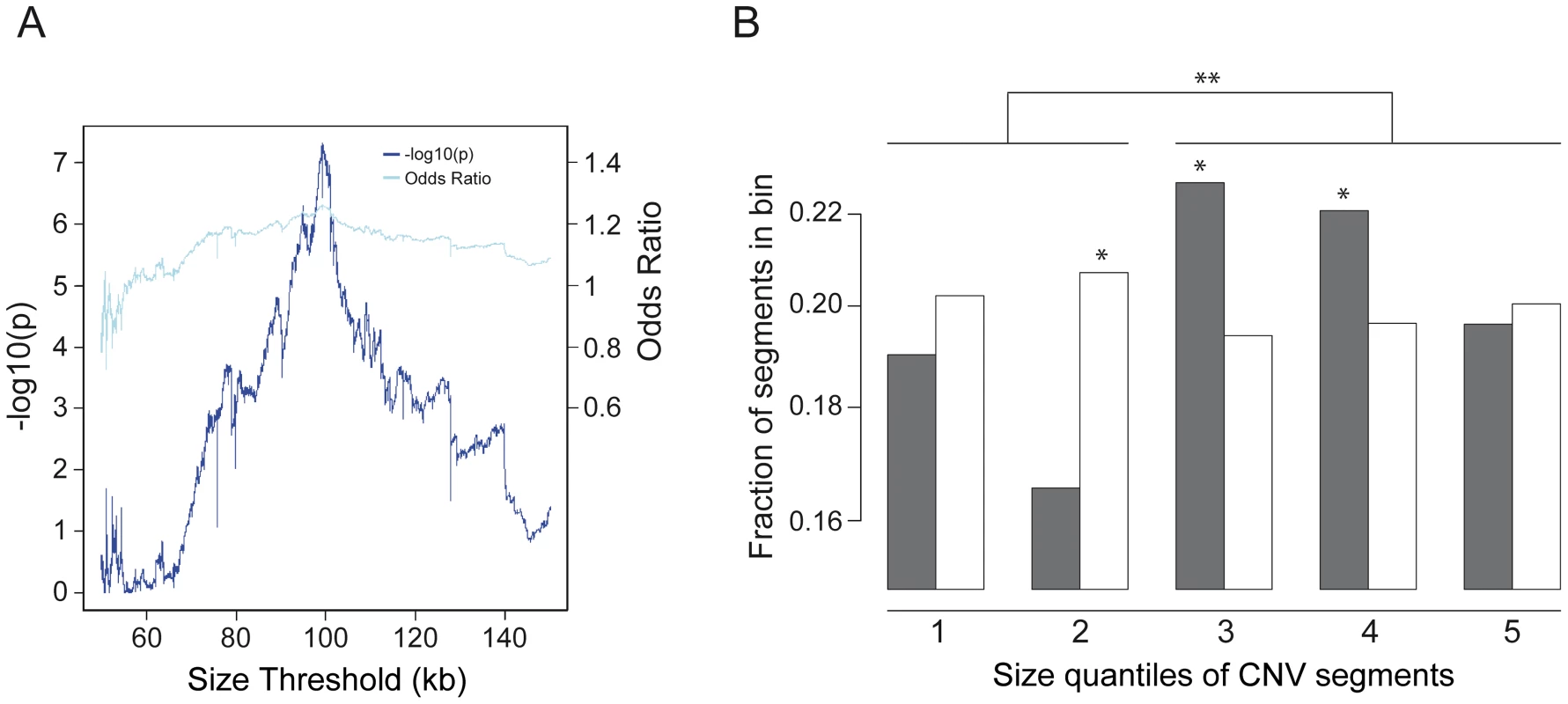
(A) Presentation of the Odds Ratio (light blue) and –log10(p-value) (dark blue) for determination of the size threshold of the number of CNVs in patients vs. controls. The Odds Ratio and the –log10(p-value) confirms a CNV size cut-off at 99.2 kb (OR 1.26 and p-value 4.98×10−8). (B) Fraction of copy numbers segments in cases (grey) vs. control (white) quintiles (* p<0.005). Quintile borders were Q1: 68.3 kb, Q2: 99.3 kb, Q3 149.6 kb, Q4 298.1 kb, and Q5: 72,571.3 kb. The y axis presents the fraction of CNVs inside the corresponding quintile bin. Significance levels are calculated using Fisher's exact test. The figure shows a shift towards segments above 100 kb in patients (** p-value 1.188×10−7). In an attempt to further investigate the variants under a “frequent disease - rare variant” – hypothesis to identify major gene effects we excluded frequent copy number polymorphisms by screening against 40,935 CNVs of the 820 control individuals (Figure 1). As we suspected low penetrance alleles to be also present in the control group, we only excluded CNVs with an overlap in CNV size of 95% in more than 15 control samples (approx. 2%). 1,211 aberrations >50 kb were retained. In a gene-centric approach we also excluded aberrations which only affected intronic or intergenic sequences. The remaining 733 CNVs were reviewed for gene content and familial segregation with the growth phenotype either by array analysis or by multiplex ligation-dependent probe amplification (MLPA; Table S1). We retained all CNVs that were either de novo in the sporadic cases or co-segregated with the phenotype in the familial cases. In addition both groups had to meet at least one of the following criteria: a) CNVs with previously described human growth phenotypes of the affected genes obtained from the OMIM database, b) Murine knock-out phenotypes of the Mouse Genome Informatics database (http://www.informatics.jax.org) including keywords like growth retardation and decreased body size (Table S2), c) genes with a possible role in height development and/or bone growth based on their reported function on cell cycle regulation, organization of the cytoskeleton, chromatin remodeling, cilia development and the involvement in important developmental pathways (Table S3), d) loci overlapping non-polymorphic, gene-containing aberrations of the Decipher database (http://decipher.sanger.ac.uk) with short stature as one of the described phenotypes.
Taken together all lines of evidence we identified a total of 20 likely pathogenic copy number changes, 10 deletions and 10 duplications, in 20 families (10% of the study group) (Table 2). It is striking that in the RefSeq exons covered by all 20 CNVs we found no overlapping control CNVs at all in 19 and just one control CNV overlapping some exons in the 5p15.33 CNV (Table S3). The size of these 20 CNVs ranged from 109 kb to 14 Mb. All 20 CNVs were independently confirmed by MLPA (Figure S2A–S2T). 7 aberrations (35%), 4 deletions and 3 duplications, were de novo (parental relationships confirmed) with an average size of 2,594 kb and an average of 30 genes. As we expected 6×10−3 de novo CNVs per haploid genome per generation in the healthy population [20], the identified number of de novo CNVs>50 kb in our patients was significantly higher than expected by chance further supporting pathogenicity of these variants (p-value 0.03, Fisher's exact test).
Tab. 2. Lines of Evidence. 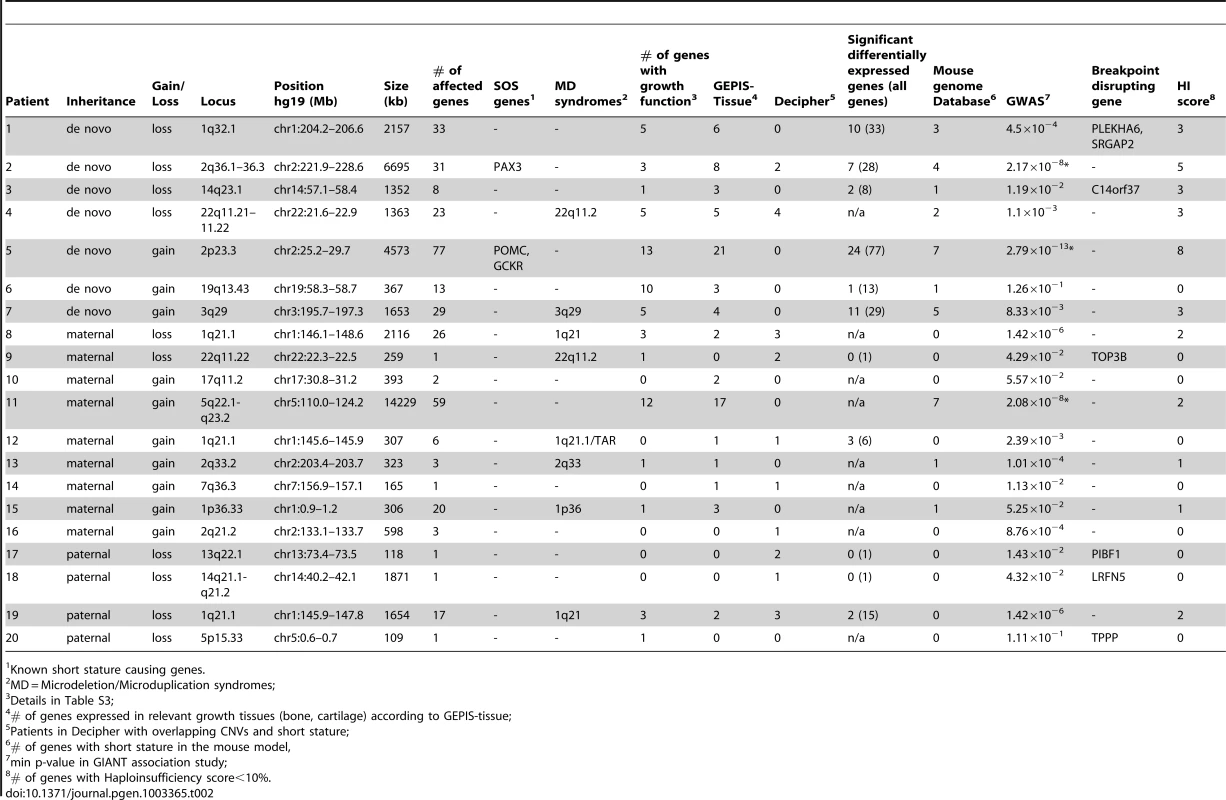
Known short stature causing genes. Unlike other entities with reduced reproductive fitness e.g. severe intellectual disability with a high rate of de novo CNVs [21], [22], we anticipated a higher rate of inherited CNVs in short stature as no reproductive disadvantage is known. This was confirmed by the identification of 13 inherited CNVs with an average CNV size of 1,727 kb and an average of 10 genes.
This group of 20 affected individuals with highly probable pathogenic CNVs consisted of 9 male and 11 female individuals (Table 3). Interestingly, the mean SD score for height was −3.34 and the SD score distribution of these 20 individuals was significantly lower when compared to the total study group (p-value 0.009; Wilcoxon test) (Figure 4). Thus, rare pathogenic CNVs are more likely identified in patients with severe short stature. No significant difference was observed in patients with CNVs with prenatal vs. postnatal onset, proportionate vs. disproportionate growth retardation, and syndromic vs. non-syndromic short stature (Table S4), but the number of affected cases in each group was small with limited statistical power. However, 40% of the 20 patients had a prenatal onset of short stature compared to 26% of the entire study group indicating central regulatory pathways of embryonic development to be disturbed by genes located in these CNVs.
Fig. 4. Height distribution of the study group. 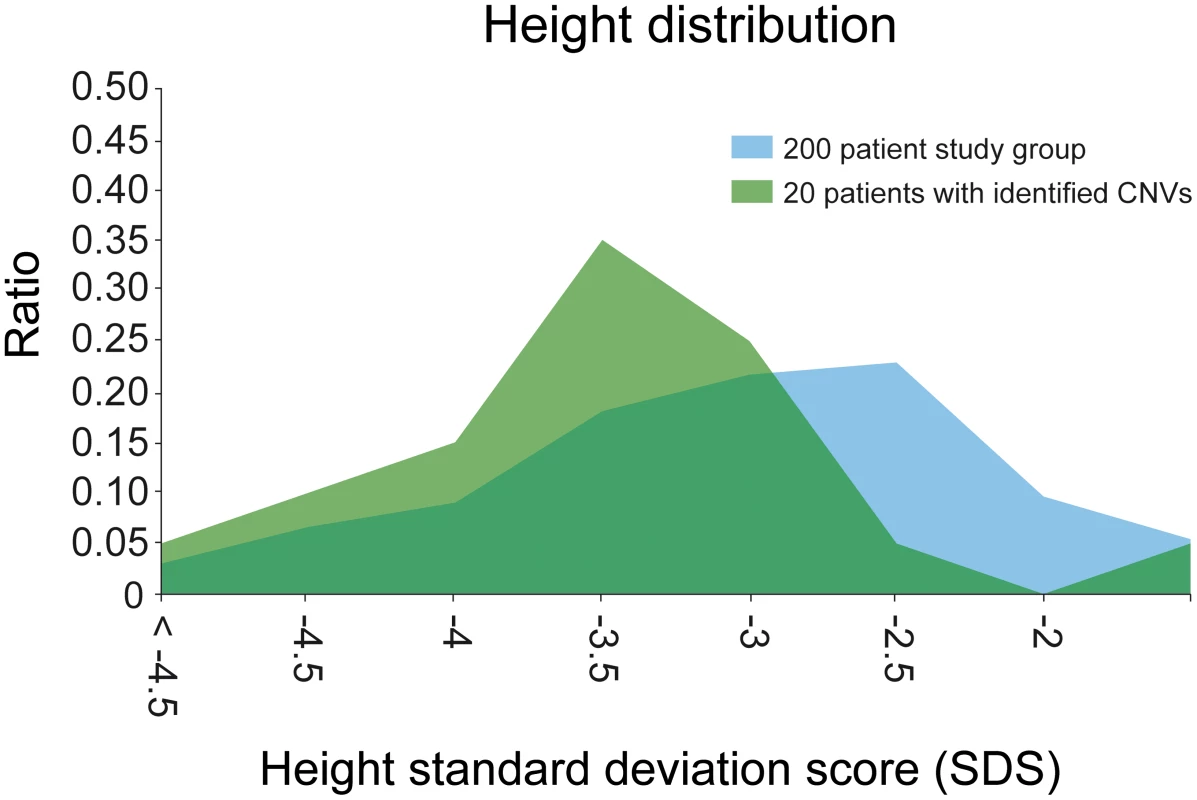
Height distribution (SDS) of all 200 patients (blue) compared to the 20 patients with identified CNVs (green). The mean SD score for height was −3.34. Patients with identified CNVs showed a significant difference in the SDS distribution (p-value 0.03). Tab. 3. Summary phenotype of patients with identified CNVs. 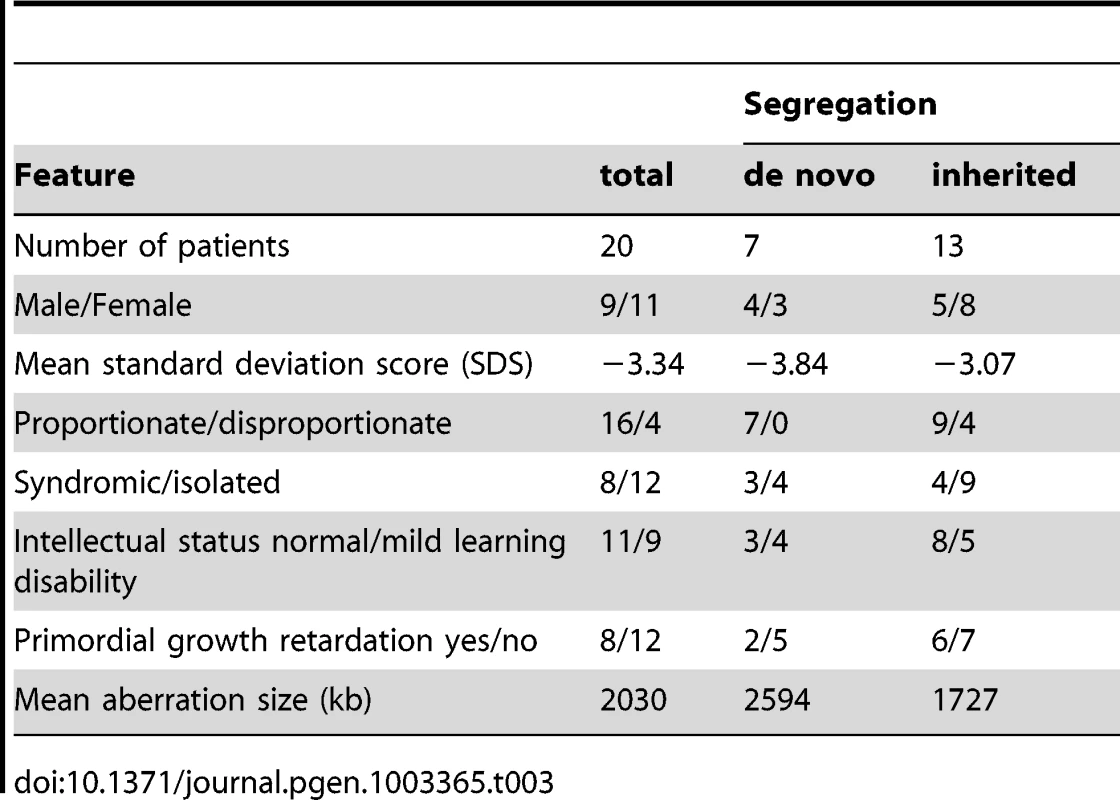
Eight patients had CNVs showing an overlap with 6 known microdeletion/duplication syndromes associated with short stature (Table 2). Two of these patients (patient 8 and 19) had large inherited deletions covering the complete 1q21.1 microdeletion region which is known for its phenotypic variability [23]. Short stature is present in about 25–50% of the patients [24]. Further commonly observed signs such as mild facial anomalies, microcephaly and developmental delay were also observed in our patients. The inherited 307 kb duplication of patient 12 included the distal end of the TAR syndrome susceptibility locus on 1q21.1 but without the recently reported RBM8A gene region [25]. A 1.6 Mb duplication overlapping the rare 3q29 microdeletion/duplication syndrome was found de novo in one patient with non syndromic idiopathic short stature (patient 7). Features of the 3q29 duplication syndrome have not been clearly determined, but failure to thrive has occasionally been reported [26]. We also found a 1,363 kb de novo deletion partially overlapping the classical and distal 22q11.22 microdeletion region of DiGeorge/Velo-cardio-facial syndrome [27]–[29] and a 259 kb inherited deletion within the distal part of 22q11.22 only (patient 4 and 9, respectively) [27]. Correspondingly, these two patients presented with short stature and some mild facial features, but no cardiac defects. Inherited duplications in patient 13 and 15 slightly overlapped the microdeletion regions 2q33 and 1p36 [30], [31]. Thus, the clinical presentation of these patients confirmed the broad variability of known microdeletion/duplication syndromes and might highlight potential candidate genes for the short stature phenotype in these entities.
Recent genome-wide association studies (GWAS) found common single nucleotide polymorphisms (SNPs) in at least 180 loci to be significantly associated with height variation in the general population. These associated loci accounted only for up to 10% of the phenotypic variation within the normal range of the Gaussian growth distribution [32]. We investigated if these loci might be located within our identified rare CNVs. Using LocusZoom [33] we compared position and gene content with the published genome wide association dataset of the GIANT consortium based on the CEU 1000genomes Nov 2010 imputation. To identify significant loci, we considered a Bonferroni corrected level of significance of 1.377×10−6 based on 36,316 SNPs from the GIANT dataset located in the 20 identified CNVs. Loci at 3 of our CNV regions reached this level of significance (variants with the best p-values respectively r2 values are shown in Figure S3A–S3T and Table S5). The loci with the best p-values were located in the 6.7 Mb deletion 2q36.1–36.3 (patient 2) (Figure 5), 4.5 Mb duplication 2p23.3 (patient 5), and 14.2 Mb duplication 5q22.1-q23.2 (patient 11). rs11125884 located in the promoter region of EFR2B (patient 5) even reached a level of genome wide significance based on SNP association (2.8×10−13). This number of 3 CNVs with significant associated SNP loci out of the 20 likely pathogenic CNVs was significantly higher than expected by chance (p-value<1×10−3). Our findings not only confirmed the significance of the published results of the genome wide association study but also suggest a possible functional link between common variants in growth variation and rare variants involved in severe growth retardation underlining a major gene effect in short stature.
Fig. 5. Genome-wide significant association of GWAS loci for height distribution in the 3 CNVs. 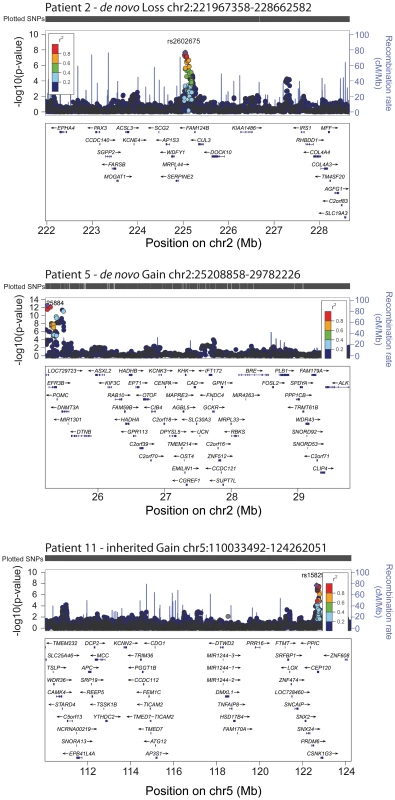
The values of r2 are based on the CEU 1000genomes Nov 2010 samples. The blue line and right-hand y axis represent recombination rates. The SNPs with the min p values are highlighted as purple diamond. The figures were created using LocusZoom (http://csg.sph.umich.edu/locuszoom/). A deletion or duplication of one gene or a subset of genes located in a CNV can lead to directly or indirectly impaired gene expression [34], [35]. To investigate whether this is the case for the 20 identified CNVs we performed expression profiling in 11 individuals where RNA from lymphocytes was available. Of the 188 genes contained in the CNVs 58 (31%) showed a significant differential gene expression in the direction of the respective CNV (Table S6). This number of differentially expressed genes we observed would be expected by chance only with a probability of less than 0.001 according to the binomial distribution, suggesting that these genes are dosage sensitive and the identified aberrations are leading to haploinsufficiency of these genes. To explore whether these 58 differentially expressed genes cluster in networks known to be involved in growth we performed pathway analyses using Ingenuity Pathway Analysis (IPA). This analysis identified networks involving cell death, cell cycle and DNA repair (Table S7) further supporting the pathogenicity of these CNVs.
In conclusion, we propose rare CNVs as a relatively common cause of short stature under a major gene effect model. These include duplications as well as deletions of more than 100 kb in a comparable frequency as observed in other entities e.g. intellectual disability [12], [36]. Our findings also provide strong evidence for a “rare variant – frequent disease” hypothesis for short stature.
Materials and Methods
Patient cohort
All individuals gave their consent to this study, which was approved by the Ethical Review Board of the Friedrich-Alexander University Erlangen-Nuremberg. Phenotypic data, medical history, and family history of 200 affected individuals with short stature and their family members were ascertained and compiled in a database. In all cases photographic documentation, pediatric and partially radiological evaluation was available. Height adjusted SD scores were calculated on the basis of the Prader Growth charts. A control cohort used to exclude common copy number polymorphisms consisted of 820 individuals originating from the same Central European region with either exfoliation syndrome or psoriatic arthritis. DNA and RNA of the affected individuals and DNA of their respective parents were obtained. DNA of cases and controls was extracted from blood samples using the same method and all necessary quality assessments during DNA sample and array preparation were attributed. Principal component analysis of the 200 affected and 820 control individuals demonstrated minor ethnic heterogeneity within both cases and controls caused by a residual amount of ethnic heterogeneity in both populations (Figure S4). This was comparable in both and considered not relevant for the identification of rare variants in contrast to the classical test of association not applied in this study.
Molecular karyotyping
Molecular karyotyping was performed using Genome-Wide Human SNP 6.0 and CytoScan HD arrays (Affymetrix, Santa Clara, USA). We calculated the genome wide copy number using the Genotyping Console 3.0.2 and the Chromosome Analysis Suite v1.2.2 software (Affymetrix, Santa Clara, USA). To exclude batch effects, all cases and controls were processed randomly. In-house quality criteria of a contrast QC value >0.4 and a MAPD value <0.4 were met by all 200 samples. Instead of the Affymetrix reference model file, our own reference file was created using 167 healthy control samples on the same platform with equal conditions. Copy number variants with a minimum of 10 kb and 5 affected markers (Genome-Wide Human SNP 6.0) or 20 affected markers (CytoScan HD array) were calculated. As CNV calling for the Y chromosome was not reliable, CNVs on the Y chromosome were excluded from further investigation.
At first a screening of all identified CNVs above 50 kb against an independent control cohort of 820 healthy control individuals excluded common copy number polymorphisms. 50 kb was the observed minimum resolution of the arrays where independent validation leads to reliable results. Accordingly, aberrations which showed a size overlap of more than 95% in more than 15 control samples were automatically excluded from further investigation. CNVs with less than 95% overlap in control samples but where all included genes are covered in CNVs of at least 15 control samples were also removed. As we aimed for rare variants all remaining CNVs were compared with CNVs annotated in the Database of Genomic Variants to exclude common variants which might not be covered by CNVs of our 820 control individuals. No additional CNVs were excluded in this step.
CNV validation
Multiplex ligation-dependent probe amplifications (MLPAs) were carried out using self-made MLPA kits with the SALSA MLPA Reagents kit and the P200 SALSA MLPA Reference kit according to the manufacturer's instructions (MRC Holland, Amsterdam, Netherlands). The reference kit includes control fragments and reference probes from 172 to 250 nucleotides. Corresponding to the affected copy number regions, MLPA probes were designed as described in the general guidelines of synthetic probe design by MRC Holland with the hg18 version of the human reference sequence (NCBI36, March 2006). For all oligonucleotides the RAW program was used to ensure a melting temperature of ≥70°C and a GC content of about 40–60%. The absence of annotated SNPs and a unique hybridization site was verified with the BLAT program. Including universal primer binding sites, the synthetic oligonucleotides product size was within a range of 100–136 bp. For the purpose of ligation all right probe oligos (RPOs) were 5′ phosphorylated (Thermo Fisher Scientific, Waltham, USA). 250 ng of genomic DNA were used to carry out the MLPA reaction. The PCR products were separated according to their length by capillary electrophoresis on an ABI PRISM 3100 Genetic Analyzer. The corresponding copy number of each locus was calculated by comparing the relative peak area of every patient to the mean peak area of at least 5 control individuals (probe ratios) in the MLPA module of the Sequence Pilot software (JSI medical systems GmbH, Kippenheim, Germany). Probe ratios under 75% indicated a deletion, whereas ratios over 125% confirmed duplications.
Furthermore, segregation of copy number changes in the families was confirmed by MLPA testing of the parental DNAs. CNVs inherited from unaffected parents were excluded from further investigation.
Association analysis
For the genome-wide copy number association analysis, pseudomarkers were defined at the endpoints of each CNV segment and the copy number status at this marker determined for each individual. Gains and Losses were separately evaluated in a permuted χ2 based test with 100,000 status permutations performed for each marker. Association analysis was performed with PLINK v. 1.07 [37] and visualized with GPGraphics [38].
Expression arrays
The PAXgene Blood RNA Kit by Qiagen was used to extract RNA from peripheral blood samples of the affected individuals. Available RNAs of 14 of the 20 affected individuals with proposed pathogenic CNVs were controlled for quantity and quality with an Agilent 2100 Bioanalyzer (Agilent, Santa Clara, USA). When quality standards were not passed, an additional purification was carried out using the “RNeasy Mini Kit” according to the manufacturer's instructions (Qiagen, Hilden, Germany). RNA of 3 individuals did not achieve the necessary quality requirements and were excluded from further analysis. Gene expression arrays of the remaining 11 affected individuals and 5 healthy controls were performed using the Affymetrix GeneChip Human Genome U133 Plus 2.0 Array. Expression data was analyzed with the PARTEK software (Partek Incorporated, St. Louis, USA). After GCRMA normalization, a one-way ANOVA analysis was performed to test for significant differences in gene expression levels.
Pathway analysis
Ingenuity Pathway Analysis (IPA) (Ingenuity Systems Inc., Redwood City, USA) was used to analyze potential functional relationships between affected genes of all 20 identified CNVs. A list of all affected genes (278 unique) as well as lists of all (60 unique), only deleted (21 unique), and only duplicated genes (39 unique) showing significant (p<0.05) differential expression of the 11 patients with expression array data available were analyzed. The fold change minimum was set to 1.25 (up regulation) and −1.33 (down regulation), respectively. After uploading the individual lists the software clustered genes according to their connectivity into molecular networks, common biological functions and canonical pathways. P-values and numerical scores were calculated to rank networks according to their degree of relevance in regards to the different gene lists. The calculated score is based on the hypergeometric distribution with the right-tailed Fisher's Exact Test. The score presents the negative log of the p-value.
GWAS comparison
We compared the position and gene content with the published genome wide association data of the GAINT consortium (CEU 1000genomes Nov 2010 sample imputation) using LocusZoom [32], [33]. Under the estimation of approx. 2000 copy number polymorphism of 50 kb or above in the human genome per individual we calculated a genome wide level of significance of 2.5×10−5.
Supporting Information
Zdroje
1. VisscherPM, HillWG, WrayNR (2008) Heritability in the genomics era–concepts and misconceptions. Nat Rev Genet 9 : 255266.
2. MendezH (1985) Introduction to the study of pre - and postnatal growth in humans: a review. Am J Med Genet 20 : 63–85.
3. Superti-FurgaA, BonafeL, RimoinDL (2001) Molecular-pathogenetic classification of genetic disorders of the skeleton. Am J Med Genet 106 : 282–293.
4. WarmanML, Cormier-DaireV, HallC, KrakowD, LachmanR, et al. (2011) Nosology and classification of genetic skeletal disorders: 2010 revision. Am J Med Genet A 155A: 943–968.
5. KallenB, KnudsenLB, MutchinickO, MastroiacovoP, LancasterP, et al. (1993) Monitoring dominant germ cell mutations using skeletal dysplasias registered in malformation registries: an international feasibility study. Int J Epidemiol 22 : 107–115.
6. RaoE, WeissB, FukamiM, RumpA, NieslerB, et al. (1997) Pseudoautosomal deletions encompassing a novel homeobox gene cause growth failure in idiopathic short stature and Turner syndrome. Nat Genet 16 : 54–63.
7. RappoldGA, FukamiM, NieslerB, SchillerS, ZumkellerW, et al. (2002) Deletions of the homeobox gene SHOX (short stature homeobox) are an important cause of growth failure in children with short stature. J Clin Endocrinol Metab 87 : 1402–1406.
8. SeaverLH, IronsM (2009) ACMG practice guideline: genetic evaluation of short stature. Genet Med 11 : 465–470.
9. VossLD, MulliganJ, BettsPR, WilkinTJ (1992) Poor growth in school entrants as an index of organic disease: the Wessex growth study. BMJ 305 : 1400–1402.
10. AhmedML, AllenAD, SharmaA, MacfarlaneJA, DungerDB (1993) Evaluation of a district growth screening programme: the Oxford Growth Study. Arch Dis Child 69 : 361–365.
11. CooperGM, CoeBP, GirirajanS, RosenfeldJA, VuTH, et al. (2011) A copy number variation morbidity map of developmental delay. Nat Genet 43 : 838–846.
12. MillerDT, AdamMP, AradhyaS, BieseckerLG, BrothmanAR, et al. (2010) Consensus statement: chromosomal microarray is a first-tier clinical diagnostic test for individuals with developmental disabilities or congenital anomalies. Am J Hum Genet 86 : 749–764.
13. ZweierC, PeippoMM, HoyerJ, SousaS, BottaniA, et al. (2007) Haploinsufficiency of TCF4 causes syndromal mental retardation with intermittent hyperventilation (Pitt-Hopkins syndrome). Am J Hum Genet 80 : 994–1001.
14. VissersLE, van RavenswaaijCM, AdmiraalR, HurstJA, de VriesBB, et al. (2004) Mutations in a new member of the chromodomain gene family cause CHARGE syndrome. Nat Genet 36 : 955–957.
15. KoolenDA, VissersLE, PfundtR, de LeeuwN, KnightSJ, et al. (2006) A new chromosome 17q21.31 microdeletion syndrome associated with a common inversion polymorphism. Nat Genet 38 : 999–1001.
16. SharpAJ, HansenS, SelzerRR, ChengZ, ReganR, et al. (2006) Discovery of previously unidentified genomic disorders from the duplication architecture of the human genome. Nat Genet 38 : 1038–1042.
17. PraderA (1981) [Normal growth and disorders of growth in children and adolescents (author's transl)]. Klin Wochenschr 59 : 977–984.
18. Superti-FurgaA, UngerS (2007) Nosology and classification of genetic skeletal disorders: 2006 revision. Am J Med Genet A 143 : 1–18.
19. HuffmeierU, UebeS, EkiciAB, BowesJ, GiardinaE, et al. (2010) Common variants at TRAF3IP2 are associated with susceptibility to psoriatic arthritis and psoriasis. Nat Genet 42 : 996–999.
20. ItsaraA, WuH, SmithJD, NickersonDA, RomieuI, et al. (2010) De novo rates and selection of large copy number variation. Genome Res 20 : 1469–1481.
21. VissersLE, de LigtJ, GilissenC, JanssenI, SteehouwerM, et al. (2010) A de novo paradigm for mental retardation. Nat Genet 42 : 1109–1112.
22. RauchA, WieczorekD, GrafE, WielandT, EndeleS, et al. (2012) Range of genetic mutations associated with severe non-syndromic sporadic intellectual disability: an exome sequencing study. Lancet 380 : 1674–82.
23. WillattL, CoxJ, BarberJ, CabanasED, CollinsA, et al. (2005) 3q29 microdeletion syndrome: clinical and molecular characterization of a new syndrome. Am J Hum Genet 77 : 154–160.
24. Brunetti-PierriN, BergJS, ScagliaF, BelmontJ, BacinoCA, et al. (2008) Recurrent reciprocal 1q21.1 deletions and duplications associated with microcephaly or macrocephaly and developmental and behavioral abnormalities. Nat Genet 40 : 1466–1471.
25. AlbersCA, PaulDS, SchulzeH, FresonK, StephensJC, et al. (2012) Compound inheritance of a low-frequency regulatory SNP and a rare null mutation in exon-junction complex subunit RBM8A causes TAR syndrome. Nat Genet 44 : 435–432, 435-439, S431-432.
26. LisiEC, HamoshA, DohenyKF, SquibbE, JacksonB, et al. (2008) 3q29 interstitial microduplication: a new syndrome in a three-generation family. Am J Med Genet A 146A: 601–609.
27. Ben-ShacharS, OuZ, ShawCA, BelmontJW, PatelMS, et al. (2008) 22q11.2 distal deletion: a recurrent genomic disorder distinct from DiGeorge syndrome and velocardiofacial syndrome. Am J Hum Genet 82 : 214–221.
28. WeinzimerSA, McDonald-McGinnDM, DriscollDA, EmanuelBS, ZackaiEH, et al. (1998) Growth hormone deficiency in patients with 22q11.2 deletion: expanding the phenotype. Pediatrics 101 : 929–932.
29. DigilioMC, MarinoB, CappaM, CambiasoP, GiannottiA, et al. (2001) Auxological evaluation in patients with DiGeorge/velocardiofacial syndrome (deletion 22q11.2 syndrome). Genet Med 3 : 30–33.
30. de RavelTJ, BalikovaI, ThiryP, VermeeschJR, FrijnsJP (2009) Another patient with a de novo deletion further delineates the 2q33.1 microdeletion syndrome. Eur J Med Genet 52 : 120–122.
31. SlavotinekA, ShafferLG, ShapiraSK (1999) Monosomy 1p36. J Med Genet 36 : 657–663.
32. Lango AllenH, EstradaK, LettreG, BerndtSI, WeedonMN, et al. (2010) Hundreds of variants clustered in genomic loci and biological pathways affect human height. Nature 467 : 832–838.
33. PruimRJ, WelchRP, SannaS, TeslovichTM, ChinesPS, et al. (2010) LocusZoom: regional visualization of genome-wide association scan results. Bioinformatics 26 : 2336–2337.
34. KleinjanDJ, van HeyningenV (1998) Position effect in human genetic disease. Hum Mol Genet 7 : 1611–1618.
35. DatheK, KjaerKW, BrehmA, MeineckeP, NurnbergP, et al. (2009) Duplications involving a conserved regulatory element downstream of BMP2 are associated with brachydactyly type A2. Am J Hum Genet 84 : 483–492.
36. GijsbersAC, LewJY, BoschCA, Schuurs-HoeijmakersJH, van HaeringenA, et al. (2009) A new diagnostic workflow for patients with mental retardation and/or multiple congenital abnormalities: test arrays first. Eur J Hum Genet 17 : 1394–1402.
37. PurcellS, NealeB, Todd-BrownK, ThomasL, FerreiraMA, et al. (2007) PLINK: a tool set for whole-genome association and population-based linkage analyses. Am J Hum Genet 81 : 559–575.
38. UebeS, PasuttoF, KrumbiegelM, SchanzeD, EkiciAB, et al. (2010) GPFrontend and GPGraphics: graphical analysis tools for genetic association studies. BMC Bioinformatics 11 : 472.
Štítky
Genetika Reprodukční medicína
Článek Ubiquitous Polygenicity of Human Complex Traits: Genome-Wide Analysis of 49 Traits in KoreansČlánek Alternative Splicing and Subfunctionalization Generates Functional Diversity in Fungal ProteomesČlánek RFX Transcription Factor DAF-19 Regulates 5-HT and Innate Immune Responses to Pathogenic Bacteria inČlánek Surveillance-Activated Defenses Block the ROS–Induced Mitochondrial Unfolded Protein ResponseČlánek Deficiency Reduces Adipose OXPHOS Capacity and Triggers Inflammation and Insulin Resistance in Mice
Článek vyšel v časopisePLOS Genetics
Nejčtenější tento týden
2013 Číslo 3
-
Všechny články tohoto čísla
- Power and Predictive Accuracy of Polygenic Risk Scores
- Rare Copy Number Variants Are a Common Cause of Short Stature
- Coordination of Flower Maturation by a Regulatory Circuit of Three MicroRNAs
- Ubiquitous Polygenicity of Human Complex Traits: Genome-Wide Analysis of 49 Traits in Koreans
- Genomic Evidence for Island Population Conversion Resolves Conflicting Theories of Polar Bear Evolution
- Mechanistic Insight into the Pathology of Polyalanine Expansion Disorders Revealed by a Mouse Model for X Linked Hypopituitarism
- Genome-Wide Association Study and Gene Expression Analysis Identifies as a Predictor of Response to Etanercept Therapy in Rheumatoid Arthritis
- Problem Solved: An Interview with Sir Edwin Southern
- Long Interspersed Element–1 (LINE-1): Passenger or Driver in Human Neoplasms?
- Mouse HFM1/Mer3 Is Required for Crossover Formation and Complete Synapsis of Homologous Chromosomes during Meiosis
- Alternative Splicing and Subfunctionalization Generates Functional Diversity in Fungal Proteomes
- A WRKY Transcription Factor Recruits the SYG1-Like Protein SHB1 to Activate Gene Expression and Seed Cavity Enlargement
- Microhomology-Mediated Mechanisms Underlie Non-Recurrent Disease-Causing Microdeletions of the Gene or Its Regulatory Domain
- Ancient Evolutionary Trade-Offs between Yeast Ploidy States
- Differential Evolutionary Fate of an Ancestral Primate Endogenous Retrovirus Envelope Gene, the EnvV , Captured for a Function in Placentation
- A Feed-Forward Loop Coupling Extracellular BMP Transport and Morphogenesis in Wing
- The Tomato Yellow Leaf Curl Virus Resistance Genes and Are Allelic and Code for DFDGD-Class RNA–Dependent RNA Polymerases
- The U-Box E3 Ubiquitin Ligase TUD1 Functions with a Heterotrimeric G α Subunit to Regulate Brassinosteroid-Mediated Growth in Rice
- Role of the DSC1 Channel in Regulating Neuronal Excitability in : Extending Nervous System Stability under Stress
- –Independent Phenotypic Switching in and a Dual Role for Wor1 in Regulating Switching and Filamentation
- Pax6 Regulates Gene Expression in the Vertebrate Lens through miR-204
- Blood-Informative Transcripts Define Nine Common Axes of Peripheral Blood Gene Expression
- Genetic Architecture of Skin and Eye Color in an African-European Admixed Population
- Fine Characterisation of a Recombination Hotspot at the Locus and Resolution of the Paradoxical Excess of Duplications over Deletions in the General Population
- Estrogen Mediated-Activation of miR-191/425 Cluster Modulates Tumorigenicity of Breast Cancer Cells Depending on Estrogen Receptor Status
- Complex Patterns of Genomic Admixture within Southern Africa
- Yap- and Cdc42-Dependent Nephrogenesis and Morphogenesis during Mouse Kidney Development
- Molecular Networks of Human Muscle Adaptation to Exercise and Age
- Alp/Enigma Family Proteins Cooperate in Z-Disc Formation and Myofibril Assembly
- Polycomb Group Gene Regulates Rice () Seed Development and Grain Filling via a Mechanism Distinct from
- RFX Transcription Factor DAF-19 Regulates 5-HT and Innate Immune Responses to Pathogenic Bacteria in
- Distinct Molecular Strategies for Hox-Mediated Limb Suppression in : From Cooperativity to Dispensability/Antagonism in TALE Partnership
- A Natural Polymorphism in rDNA Replication Origins Links Origin Activation with Calorie Restriction and Lifespan
- TDP2–Dependent Non-Homologous End-Joining Protects against Topoisomerase II–Induced DNA Breaks and Genome Instability in Cells and
- Recurrent Rearrangement during Adaptive Evolution in an Interspecific Yeast Hybrid Suggests a Model for Rapid Introgression
- Genome-Wide Association Study in Mutation Carriers Identifies Novel Loci Associated with Breast and Ovarian Cancer Risk
- Coincident Resection at Both Ends of Random, γ–Induced Double-Strand Breaks Requires MRX (MRN), Sae2 (Ctp1), and Mre11-Nuclease
- Identification of a -Specific Modifier Locus at 6p24 Related to Breast Cancer Risk
- A Novel Function for the Hox Gene in the Male Accessory Gland Regulates the Long-Term Female Post-Mating Response in
- Tdp2: A Means to Fixing the Ends
- A Novel Role for the RNA–Binding Protein FXR1P in Myoblasts Cell-Cycle Progression by Modulating mRNA Stability
- Association Mapping and the Genomic Consequences of Selection in Sunflower
- Histone Deacetylase 2 (HDAC2) Regulates Chromosome Segregation and Kinetochore Function via H4K16 Deacetylation during Oocyte Maturation in Mouse
- A Novel Mutation in the Upstream Open Reading Frame of the Gene Causes a MEN4 Phenotype
- Ataxin1L Is a Regulator of HSC Function Highlighting the Utility of Cross-Tissue Comparisons for Gene Discovery
- Human Spermatogenic Failure Purges Deleterious Mutation Load from the Autosomes and Both Sex Chromosomes, including the Gene
- A Conserved Upstream Motif Orchestrates Autonomous, Germline-Enriched Expression of piRNAs
- Statistical Analysis Reveals Co-Expression Patterns of Many Pairs of Genes in Yeast Are Jointly Regulated by Interacting Loci
- Matefin/SUN-1 Phosphorylation Is Part of a Surveillance Mechanism to Coordinate Chromosome Synapsis and Recombination with Meiotic Progression and Chromosome Movement
- A Role for the Malignant Brain Tumour (MBT) Domain Protein LIN-61 in DNA Double-Strand Break Repair by Homologous Recombination
- The Population and Evolutionary Dynamics of Phage and Bacteria with CRISPR–Mediated Immunity
- Long Noncoding RNA MALAT1 Controls Cell Cycle Progression by Regulating the Expression of Oncogenic Transcription Factor B-MYB
- Surveillance-Activated Defenses Block the ROS–Induced Mitochondrial Unfolded Protein Response
- DNA Topoisomerase III Localizes to Centromeres and Affects Centromeric CENP-A Levels in Fission Yeast
- Genome-Wide Control of RNA Polymerase II Activity by Cohesin
- Divergent Selection Drives Genetic Differentiation in an R2R3-MYB Transcription Factor That Contributes to Incipient Speciation in
- NODULE INCEPTION Directly Targets Subunit Genes to Regulate Essential Processes of Root Nodule Development in
- Spreading of a Prion Domain from Cell-to-Cell by Vesicular Transport in
- Deficiency in Origin Licensing Proteins Impairs Cilia Formation: Implications for the Aetiology of Meier-Gorlin Syndrome
- Deficiency Reduces Adipose OXPHOS Capacity and Triggers Inflammation and Insulin Resistance in Mice
- The Conserved SKN-1/Nrf2 Stress Response Pathway Regulates Synaptic Function in
- Functional Genomic Analysis of the Regulatory Network in
- Astakine 2—the Dark Knight Linking Melatonin to Circadian Regulation in Crustaceans
- CRL2 E3-Ligase Regulates Proliferation and Progression through Meiosis in the Germline
- Both the Caspase CSP-1 and a Caspase-Independent Pathway Promote Programmed Cell Death in Parallel to the Canonical Pathway for Apoptosis in
- PRMT4 Is a Novel Coactivator of c-Myb-Dependent Transcription in Haematopoietic Cell Lines
- A Copy Number Variant at the Locus Likely Confers Risk for Canine Squamous Cell Carcinoma of the Digit
- Evidence of Gene–Environment Interactions between Common Breast Cancer Susceptibility Loci and Established Environmental Risk Factors
- HIV Infection Disrupts the Sympatric Host–Pathogen Relationship in Human Tuberculosis
- Trans-Ethnic Fine-Mapping of Lipid Loci Identifies Population-Specific Signals and Allelic Heterogeneity That Increases the Trait Variance Explained
- A Gene Transfer Agent and a Dynamic Repertoire of Secretion Systems Hold the Keys to the Explosive Radiation of the Emerging Pathogen
- The Role of ATM in the Deficiency in Nonhomologous End-Joining near Telomeres in a Human Cancer Cell Line
- Dynamic Circadian Protein–Protein Interaction Networks Predict Temporal Organization of Cellular Functions
- Nuclear Myosin 1c Facilitates the Chromatin Modifications Required to Activate rRNA Gene Transcription and Cell Cycle Progression
- Robust Prediction of Expression Differences among Human Individuals Using Only Genotype Information
- A Single Cohesin Complex Performs Mitotic and Meiotic Functions in the Protist
- The Role of the Arabidopsis Exosome in siRNA–Independent Silencing of Heterochromatic Loci
- Elevated Expression of the Integrin-Associated Protein PINCH Suppresses the Defects of Muscle Hypercontraction Mutants
- Twist1 Controls a Cell-Specification Switch Governing Cell Fate Decisions within the Cardiac Neural Crest
- Genome-Wide Testing of Putative Functional Exonic Variants in Relationship with Breast and Prostate Cancer Risk in a Multiethnic Population
- Heteroduplex DNA Position Defines the Roles of the Sgs1, Srs2, and Mph1 Helicases in Promoting Distinct Recombination Outcomes
- PLOS Genetics
- Archiv čísel
- Aktuální číslo
- Informace o časopisu
Nejčtenější v tomto čísle- Fine Characterisation of a Recombination Hotspot at the Locus and Resolution of the Paradoxical Excess of Duplications over Deletions in the General Population
- Molecular Networks of Human Muscle Adaptation to Exercise and Age
- Recurrent Rearrangement during Adaptive Evolution in an Interspecific Yeast Hybrid Suggests a Model for Rapid Introgression
- Genome-Wide Association Study and Gene Expression Analysis Identifies as a Predictor of Response to Etanercept Therapy in Rheumatoid Arthritis
Kurzy
Zvyšte si kvalifikaci online z pohodlí domova
Současné možnosti léčby obezity
nový kurzAutoři: MUDr. Martin Hrubý
Všechny kurzyPřihlášení#ADS_BOTTOM_SCRIPTS#Zapomenuté hesloZadejte e-mailovou adresu, se kterou jste vytvářel(a) účet, budou Vám na ni zaslány informace k nastavení nového hesla.
- Vzdělávání



