-
Články
Top novinky
Reklama- Vzdělávání
- Časopisy
Top články
Nové číslo
- Témata
Top novinky
Reklama- Videa
- Podcasty
Nové podcasty
Reklama- Kariéra
Doporučené pozice
Reklama- Praxe
Top novinky
ReklamaFungal Immune Evasion in a Model Host–Pathogen Interaction: Versus Macrophages
article has not abstract
Published in the journal: . PLoS Pathog 9(11): e32767. doi:10.1371/journal.ppat.1003741
Category: Pearls
doi: https://doi.org/10.1371/journal.ppat.1003741Summary
article has not abstract
The innate immune system is the primary line of defense against systemic fungal infections. As a result, the interaction between Candida albicans, the most important fungal pathogen in the developed world, and innate immune phagocytes has received significant attention as a key infection determinant, revealing complex transcriptional and developmental responses in both cell types. The availability of easily propagated macrophage-like cell lines and the remarkable morphological switch that occurs in phagocytosed C. albicans cells have made this an important model of host–pathogen interactions. Several lines of evidence have emerged that C. albicans actively resists recognition by the immune system and inhibits some of the classical antimicrobial responses. This Pearl will discuss recent findings in Candida–macrophage interactions.
Immune Recognition: A Taste of Something Sweet
Innate immune phagocytes, including macrophages, recognize C. albicans and other fungal pathogens via Pathogen Associated Molecular Patterns (PAMPs); the most important of these are the cell wall carbohydrates: mannan (as mannosylated proteins), β-glucan, and chitin, a minor component. The structure of these polysaccharides and the receptors to which they bind has been discussed in depth elsewhere [1], [2]. In C. albicans yeast cells, the β-glucan layer is obscured by the outer mannoproteins and largely inaccessible to the immune system [3]. To oversimplify, a greater proinflammatory response results from alterations that increase exposure of the inner β-glucans, including hypoxia [4], antifungal drugs [3], and inhibition of glycerophosphatidylinositol (GPI)-anchoring of the mannoproteins in the wall [5]. Some strain-specific differences in β-glucan–based recognition by the Dectin-1 receptor are apparent only in vivo but affect the outcome of the infection [4]; one could speculate that this represents active regulation of cell wall structure in vivo.
Deposition of complement proteins on the cell surface is both microbicidal and immunostimulatory. The C. albicans cell surface binds numerous negative regulators of the complement cascade to inhibit complement activation: Pra1 (pH-Regulated Antigen) binds plasminogen, Factor H, FHL-1, and C4B, all in active forms [6], [7]. At least eight proteins bind plasminogen to the C. albicans surface [8], and complement factors are substrates of the Secreted Aspartyl Protease family [9]. The sum of these activities is to reduce immune recognition of the fungal cell.
Stress Responses: Pleading Self-Defense
C. albicans is resistant to macrophage-associated stresses, including reactive oxygen and nitrogen species (ROS/RNS). C. albicans encodes a catalase and six superoxide dismutases; unusually, three Sod enzymes (Sod4-6) are secreted and detoxify extracellular ROS produced by macrophages [10]. The single catalase (Cat1) does not have a signal sequence but has also been identified on the cell surface [8]. Thus, C. albicans blunts the antimicrobial respiratory burst before it can cause intracellular damage. Anti-RNS defenses are intracellular in the form of three flavohemoglobin enzymes (Yhb1, Yhb4, Yhb5); deletion of YHB1 renders cells hypersensitive to NO in vitro [11]. There is also evidence that a variety of fungi, including C. albicans, can inhibit NO production from macrophages, but no mechanism has been identified (see [12]).
A discrepancy exists, however, between in vitro and in vivo stress phenotypes. Mutation of the ROS-responsive Cap1 transcription factor confers profound sensitivity to oxidants and failure to filament within macrophages [13], [14]. Cap1 regulates catalase expression [15], as does the MAP kinase Hog1; both cat1Δ and hog1Δ have profound virulence defects in mice [16], [17]. Yet the cap1Δ mutant is fully virulent [18], suggesting additional Hog1 - and Cap1-independent regulatory mechanisms, as proposed [19]. Similarly, mutation of Yhb1 has only mild effects on virulence, suggesting roles for other anti-NO mechanisms in vivo [11].
Nutritional Stress: The South Beach Diet
C. albicans cells phagocytosed by macrophages switch to a gluconeogenic growth mode [20]. The starvation-like response is specific to carbon metabolism and mutation of genes encoding key steps of gluconeogenesis; the glyoxylate cycle and β-oxidation of fatty acids attenuate virulence to a greater or lesser degree [21], [22]. Single cell GFP reporters confirm induction of genes such as phosphoenolpyruvate carboxykinase (PCK1) and isocitrate lyase (ICL1) in macrophages and in tissues [21]. The regulatory networks that control expression of these genes differ markedly from the S. cerevisiae paradigms [23].
What carbon sources are most relevant in vivo? Some host niches are clearly glucose-deficient. Lactate, produced by tissues and by bacteria in the gut, is one potential carbon source. Fungi generally prefer glucose to the exclusion of any other carbon sources, but C. albicans cells metabolize glucose and lactate concurrently in at least some circumstances [24]. Cells grown on lactate have an altered cell wall; are more resistant to osmotic, envelope, and antifungal stresses; and are more adherent [25]. Lactate-grown cells elicit lower levels of proinflammatory cytokines from monocytic cells but, once phagoctyosed, actually do more damage to macrophages [26]. Thus, exposure to nonpreferred carbon sources benefits C. albicans in its interactions with macrophages. It is likely that this flexible organism finds and uses multiple carbon sources within the host.
We have proposed that amino acids are another relevant in vivo nutrient [27]. Phagocytosed cells induce the entire arginine biosynthetic pathway but no other amino acid synthetic genes [20], [28]. Surprisingly, expression results from exposure to moderate concentrations of ROS, rather than a lack of arginine. Induction is not seen when phagocytosed by ROS-deficient macrophages lacking the gp91 subunit of the phagocyte oxidase [28]. The significance of this connection between nutrients and oxidative stress is not clear.
Intracellular Trafficking: Losing One's Way
We are beginning to understand the molecular interactions at the interface between host and pathogen cells that lead to endocytosis and the activation of responses in both cells. In contrast, the intracellular fate of C. albicans once phagocytosed remains a mystery. Early investigations came to contradictory conclusions about whether phagosome–lysosome fusion occurred, depending on the approach used. A more recent analysis using markers along the endocytic pathway during phagosome maturation demonstrated that intracellular trafficking of C. albicans is aberrant, but a definitive mapping of these events was obscured by heterogeneity in postendocytic events [29]. Relative to heat-killed controls, phagosomes with live C. albicans cells were associated with less filamentous actin and acquired late endosomal markers less robustly, including LAMP-1 and the vATPase proton pump. Even transient colocalization with late endosomal makers was rapidly lost and, in phagosomes containing filamentation-competent cells, replaced with elements normally associated with the ER membrane, such as calnexin. Live C. albicans appears to inhibit both lysosomal acidification and NO release [29]. We have also identified macrophage-like conditions in which C. albicans releases ammonia derived from amino acid degradation to raise extracellular pH [27], potentially synergizing with the vATPase defect to block acidification. On top of this, some phagocytosed C. albicans cells escape macrophages through a non-lytic route [30]; the underlying mechanisms, again, are not understood.
The take-home message is that the intracellular fate of live C. albicans differs markedly from that of killed cells, implying an active modulation by the fungal cell. At least some filamentous cells escape the normal phagocytic pathway to an “ER-like” compartment. Further study, particularly with more refined temporal resolution to reduce heterogeneity, is clearly needed to understand the intracellular fate of this organism.
Morphogenesis: The Shape of What's to Come
Morphological differentiation is a central theme of fungal pathogenesis, from the multicellular development of Aspergillus species to the hyphal-to-yeast transition in the host of the dimorphic fungi, such as Histoplasma and Coccidioides. C. albicans yeast cells germinate within the macrophage, forming hyphae that penetrate and kill the phagocyte, a remarkable aspect of this interaction (Figure 1). Yeast, hyphae, and pseudohyphae can be seen simultaneously in tissues, and this reversible switch is a core virulence trait, as mutants locked in one form are avirulent [31], [32]. The regulation of hyphal morphogenesis is extremely complex, with multiple inducing signals, including neutral pH, elevated CO2, serum, physiological temperatures, and N-acetylglucosamine, feeding into signaling pathways that culminate in dozens of transcription factors (reviewed in [33]).
Fig. 1. Morphogenesis of C. albicans within macrophages. 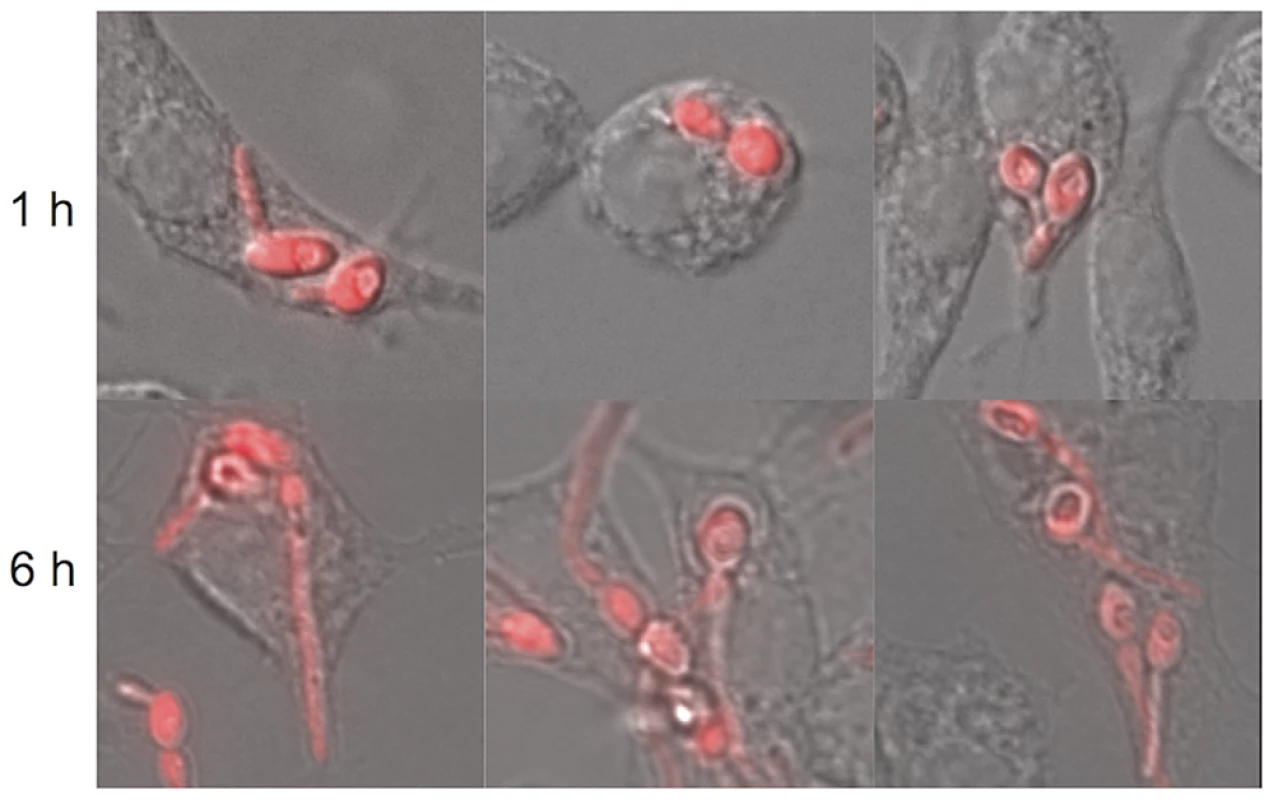
C. albicans cells constitutively expressing yCherry were incubated for one hour (top) or six hours (bottom). Germination is apparent early and has disrupted macrophage structures by the later time point. It is not clear why C. albicans switches to the hyphal form within the macrophage. The intracellular environment should be acidic and carbon-poor, which are conditions inhibitory to filamentous growth. The aberrant trafficking discussed above may put C. albicans in more conducive conditions, but what actually induces the transition is unknown. Two possibilities impinge on amino acid metabolism: Mutants lacking arg4Δ form hyphae less well than wild-type strains within macrophages, and it has been proposed that C. albicans cells synthesize and then degrade arginine for the purpose of generating CO2 [34], which is consistent with our demonstration that this pathway is induced [28]. More broadly, catabolism of amino acids as a carbon source in vitro releases ammonia as a byproduct, resulting in a dramatic rise in the extracellular pH, and we proposed that this occurs when in the macrophage [27]. ROS may also induce the hyphal switch, as cap1Δ mutants fail to filament after phagocytosis [14]. Either or both of these phenomena could create hyphal-inducing conditions in the macrophage.
In summary, the C. albicans–macrophage model is a dynamic interaction in which this opportunistic pathogen employs multiple avenues to blunt the antimicrobial activity of the phagocyte by inhibiting recognition, trafficking, and effector release (Figure 2), while overcoming several important stresses. While much is left to learn, this is an important model system for understanding host–pathogen interactions.
Fig. 2. Immunomodulatory activities of C. albicans. 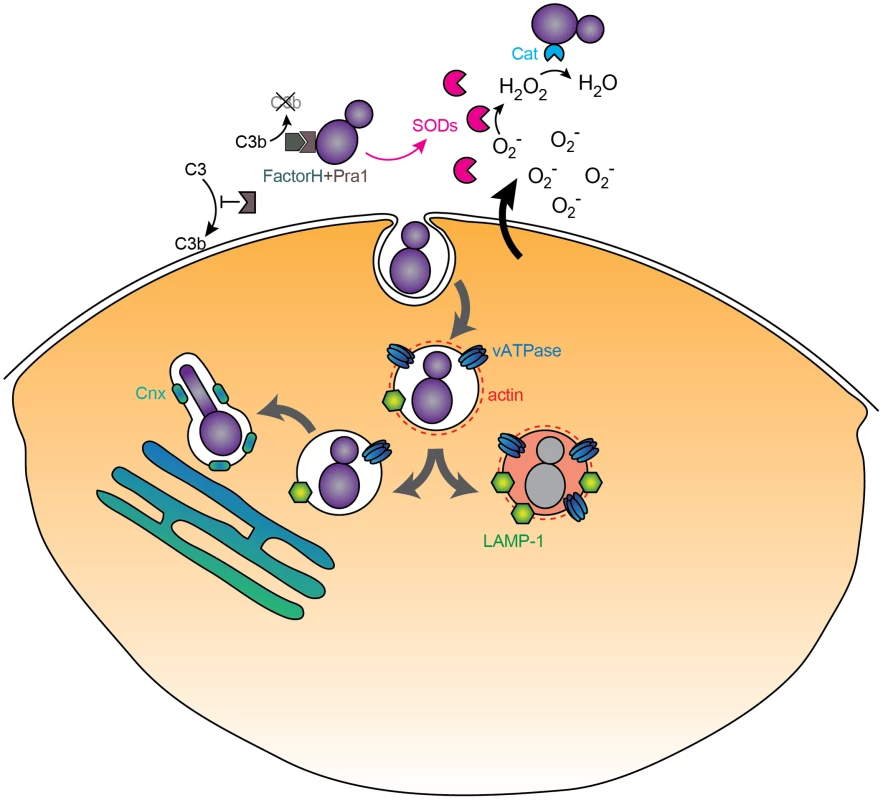
Extracellular C. albicans inhibits complement deposition and detoxifies ROS via secreted mediators (SODs, catalase, Pra1), while phagocytosed cells proceed along an altered trafficking pathway to end up in an ER-associated compartment characterized by the membrane calnexin (Cnx) and a loss of LAMP-1, peripheral actin, and vATPase.
Zdroje
1. NeteaMG, BrownGD, KullbergBJ, GowNA (2008) An integrated model of the recognition of Candida albicans by the innate immune system. Nat Rev Microbiol 6 : 67–78.
2. Perez-GarciaLA, Diaz-JimenezDF, Lopez-EsparzaA, Mora-MontesHM (2011) Role of cell wall polysaccharides during recongition of Candida albicans by the innate immune system. J Glycobiology 1 : 102.
3. WheelerRT, FinkGR (2006) A drug-sensitive genetic network masks fungi from the immune system. PLoS Pathog 2: e35.
4. MarakalalaMJ, VautierS, PotrykusJ, WalkerLA, ShepardsonKM, et al. (2013) Differential adaptation of Candida albicans in vivo modulates immune recognition by dectin-1. PLoS Pathog 9: e1003315 doi:10.1371/journal.ppat.1003315
5. McLellanCA, WhitesellL, KingOD, LancasterAK, MazitschekR, et al. (2012) Inhibiting GPI anchor biosynthesis in fungi stresses the endoplasmic reticulum and enhances immunogenicity. ACS Chem Biol 7 : 1520–1528.
6. LuoS, BlomAM, RuppS, HiplerUC, HubeB, et al. (2011) The pH-regulated antigen 1 of Candida albicans binds the human complement inhibitor C4b-binding protein and mediates fungal complement evasion. J Biol Chem 286 : 8021–8029.
7. LuoS, PoltermannS, KunertA, RuppS, ZipfelPF (2009) Immune evasion of the human pathogenic yeast Candida albicans: Pra1 is a Factor H, FHL-1 and plasminogen binding surface protein. Mol Immunol 47 : 541–550.
8. CroweJD, SievwrightIK, AuldGC, MooreNR, GowNA, et al. (2003) Candida albicans binds human plasminogen: identification of eight plasminogen-binding proteins. Mol Microbiol 47 : 1637–1651.
9. GroppK, SchildL, SchindlerS, HubeB, ZipfelPF, et al. (2009) The yeast Candida albicans evades human complement attack by secretion of aspartic proteases. Mol Immunol 47 : 465–475.
10. FrohnerIE, BourgeoisC, YatsykK, MajerO, KuchlerK (2009) Candida albicans cell surface superoxide dismutases degrade host-derived reactive oxygen species to escape innate immune surveillance. Mol Microbiol 71 : 240–252.
11. UllmannBD, MyersH, ChiranandW, LazzellAL, ZhaoQ, et al. (2004) Inducible defense mechanism against nitric oxide in Candida albicans. Eukaryot Cell 3 : 715–723.
12. ColletteJR, LorenzMC (2011) Mechanisms of immune evasion in fungal pathogens. Curr Opin Microbiol 14 : 668–675.
13. AlarcoAM, RaymondM (1999) The bZip transcription factor Cap1p is involved in multidrug resistance and oxidative stress response in Candida albicans. J Bacteriol 181 : 700–708.
14. PattersonMJ, McKenzieCG, SmithDA, da Silva DantasA, SherstonS, et al. (2013) Ybp1 and Gpx3 Signaling in Candida albicans Govern Hydrogen Peroxide-Induced Oxidation of the Cap1 Transcription Factor and Macrophage Escape. Antioxid Redox Signal E-pub ahead of print. doi:10.1089/ars.2013.5199
15. ZnaidiS, BarkerKS, WeberS, AlarcoAM, LiuTT, et al. (2009) Identification of the Candida albicans Cap1p regulon. Eukaryot Cell 8 : 806–820.
16. Alonso-MongeR, Navarro-GarciaF, MoleroG, Diez-OrejasR, GustinM, et al. (1999) Role of the mitogen-activated protein kinase Hog1p in morphogenesis and virulence of Candida albicans. J Bacteriol 181 : 3058–3068.
17. WysongDR, ChristinL, SugarAM, RobbinsPW, DiamondRD (1998) Cloning and sequencing of a Candida albicans catalase gene and effects of disruption of this gene. Infect Immun 66 : 1953–1961.
18. JainC, PastorK, GonzalezAY, LorenzMC, RaoRP (2013) The role of Candida albicans AP-1 protein against host derived ROS in in vivo models of infection. Virulence 4 : 67–76.
19. Gonzalez-ParragaP, Alonso-MongeR, PlaJ, ArguellesJC (2010) Adaptive tolerance to oxidative stress and the induction of antioxidant enzymatic activities in Candida albicans are independent of the Hog1 and Cap1-mediated pathways. FEMS Yeast Res 10 : 747–756.
20. LorenzMC, BenderJA, FinkGR (2004) Transcriptional response of Candida albicans upon internalization by macrophages. Eukaryot Cell 3 : 1076–1087.
21. BarelleCJ, PriestCL, MaccallumDM, GowNA, OddsFC, et al. (2006) Niche-specific regulation of central metabolic pathways in a fungal pathogen. Cell Microbiol 8 : 961–971.
22. PiekarskaK, MolE, van den BergM, HardyG, van den BurgJ, et al. (2006) Peroxisomal fatty acid β-oxidation is not essential for virulence of Candida albicans. Eukaryot Cell 5 : 1847–1856.
23. RamirezMA, LorenzMC (2009) The transcription factor homolog CTF1 regulates {beta}-oxidation in Candida albicans. Eukaryot Cell 8 : 1604–1614.
24. SandaiD, YinZ, SelwayL, SteadD, WalkerJ, et al. (2012) The evolutionary rewiring of ubiquitination targets has reprogrammed the regulation of carbon assimilation in the pathogenic yeast Candida albicans. MBio 3: e00495–12.
25. EneIV, AdyaAK, WehmeierS, BrandAC, MacCallumDM, et al. (2012) Host carbon sources modulate cell wall architecture, drug resistance and virulence in a fungal pathogen. Cell Microbiol 14 : 1319–1335.
26. EneIV, ChengSC, NeteaMG, BrownAJ (2013) Growth of Candida albicans cells on the physiologically relevant carbon source lactate affects their recognition and phagocytosis by immune cells. Infect Immun 81 : 238–248.
27. VylkovaS, CarmanAJ, DanhofHA, ColletteJR, ZhouH, et al. (2011) The Fungal Pathogen Candida albicans Autoinduces Hyphal Morphogenesis by Raising Extracellular pH. MBio 2: e00055–11.
28. Jimenez-LopezC, ColletteJR, BrothersKM, ShepardsonKM, CramerRA, et al. (2013) Candida albicans induces arginine biosynthetic genes in response to host-derived reactive oxygen species. Eukaryot Cell 12 : 91–100.
29. Fernandez-ArenasE, CabezonV, BermejoC, ArroyoJ, NombelaC, et al. (2007) Integrated proteomics and genomics strategies bring new insight into Candida albicans response upon macrophage interaction. Mol Cell Proteomics 6 : 460–478.
30. BainJM, LewisLE, OkaiB, QuinnJ, GowNA, et al. (2012) Non-lytic expulsion/exocytosis of Candida albicans from macrophages. Fungal Genet Biol 49 : 677–678.
31. LoHJ, KohlerJR, DiDomenicoB, LoebenbergD, CacciapuotiA, et al. (1997) Nonfilamentous C. albicans mutants are avirulent. Cell 90 : 939–949.
32. SavilleSP, LazzellAL, MonteagudoC, Lopez-RibotJL (2003) Engineered control of cell morphology in vivo reveals distinct roles for yeast and filamentous forms of Candida albicans during infection. Eukaryot Cell 2 : 1053–1060.
33. BiswasS, Van DijckP, DattaA (2007) Environmental sensing and signal transduction pathways regulating morphopathogenic determinants of Candida albicans. Microbiol Mol Biol Rev 71 : 348–376.
34. GhoshS, NavarathnaDH, RobertsDD, CooperJT, AtkinAL, et al. (2009) Arginine-induced germ tube formation in Candida albicans is essential for escape from murine macrophage line RAW 264.7. Infect Immun 77 : 1596–1605.
Štítky
Hygiena a epidemiologie Infekční lékařství Laboratoř
Článek vyšel v časopisePLOS Pathogens
Nejčtenější tento týden
2013 Číslo 11- Jak souvisí postcovidový syndrom s poškozením mozku?
- Měli bychom postcovidový syndrom léčit antidepresivy?
- Farmakovigilanční studie perorálních antivirotik indikovaných v léčbě COVID-19
- 10 bodů k očkování proti COVID-19: stanovisko České společnosti alergologie a klinické imunologie ČLS JEP
-
Všechny články tohoto čísla
- Baculoviruses: Sophisticated Pathogens of Insects
- How Do Viruses Avoid Inhibition by Endogenous Cellular MicroRNAs?
- The Regulation of Trypanosome Gene Expression by RNA-Binding Proteins
- DNA Damage Repair and Bacterial Pathogens
- Disease to Dirt: The Biology of Microbial Amyloids
- Fungal Immune Evasion in a Model Host–Pathogen Interaction: Versus Macrophages
- Infectious Prions Accumulate to High Levels in Non Proliferative C2C12 Myotubes
- The Biology and Taxonomy of Head and Body Lice—Implications for Louse-Borne Disease Prevention
- Antibodies Trap Tissue Migrating Helminth Larvae and Prevent Tissue Damage by Driving IL-4Rα-Independent Alternative Differentiation of Macrophages
- The Effects of Somatic Hypermutation on Neutralization and Binding in the PGT121 Family of Broadly Neutralizing HIV Antibodies
- Natural Selection Promotes Antigenic Evolvability
- Type I Interferon Protects against Pneumococcal Invasive Disease by Inhibiting Bacterial Transmigration across the Lung
- Mode of Parainfluenza Virus Transmission Determines the Dynamics of Primary Infection and Protection from Reinfection
- Type I and Type III Interferons Drive Redundant Amplification Loops to Induce a Transcriptional Signature in Influenza-Infected Airway Epithelia
- Unraveling a Three-Step Spatiotemporal Mechanism of Triggering of Receptor-Induced Nipah Virus Fusion and Cell Entry
- A Novel Membrane Sensor Controls the Localization and ArfGEF Activity of Bacterial RalF
- Macrophage and T Cell Produced IL-10 Promotes Viral Chronicity
- Global Rescue of Defects in HIV-1 Envelope Glycoprotein Incorporation: Implications for Matrix Structure
- Turning Defense into Offense: Defensin Mimetics as Novel Antibiotics Targeting Lipid II
- The Neonatal Fc Receptor (FcRn) Enhances Human Immunodeficiency Virus Type 1 (HIV-1) Transcytosis across Epithelial Cells
- Brd4 Is Displaced from HPV Replication Factories as They Expand and Amplify Viral DNA
- A Viral Genome Landscape of RNA Polyadenylation from KSHV Latent to Lytic Infection
- The Cytotoxic Necrotizing Factor of (CNF) Enhances Inflammation and Yop Delivery during Infection by Activation of Rho GTPases
- The Inflammatory Kinase MAP4K4 Promotes Reactivation of Kaposi's Sarcoma Herpesvirus and Enhances the Invasiveness of Infected Endothelial Cells
- Conservative Sex and the Benefits of Transformation in
- Microbial Endocrinology in the Microbiome-Gut-Brain Axis: How Bacterial Production and Utilization of Neurochemicals Influence Behavior
- Colonization Resistance: Battle of the Bugs or Ménage à Trois with the Host?
- Intracellular Interferons in Fish: A Unique Means to Combat Viral Infection
- SPOC1-Mediated Antiviral Host Cell Response Is Antagonized Early in Human Adenovirus Type 5 Infection
- Involvement of the Cellular Phosphatase DUSP1 in Vaccinia Virus Infection
- Killer Bee Molecules: Antimicrobial Peptides as Effector Molecules to Target Sporogonic Stages of
- A Unique SUMO-2-Interacting Motif within LANA Is Essential for KSHV Latency
- A Role for Host Activation-Induced Cytidine Deaminase in Innate Immune Defense against KSHV
- Haploid Genetic Screens Identify an Essential Role for PLP2 in the Downregulation of Novel Plasma Membrane Targets by Viral E3 Ubiquitin Ligases
- A Small Molecule Glycosaminoglycan Mimetic Blocks Invasion of the Mosquito Midgut
- Identification of the Adenovirus E4orf4 Protein Binding Site on the B55α and Cdc55 Regulatory Subunits of PP2A: Implications for PP2A Function, Tumor Cell Killing and Viral Replication
- Can Non-lytic CD8+ T Cells Drive HIV-1 Escape?
- Deletion of the α-(1,3)-Glucan Synthase Genes Induces a Restructuring of the Conidial Cell Wall Responsible for the Avirulence of
- PLOS Pathogens
- Archiv čísel
- Aktuální číslo
- Informace o časopisu
Nejčtenější v tomto čísle- Baculoviruses: Sophisticated Pathogens of Insects
- Identification of the Adenovirus E4orf4 Protein Binding Site on the B55α and Cdc55 Regulatory Subunits of PP2A: Implications for PP2A Function, Tumor Cell Killing and Viral Replication
- A Unique SUMO-2-Interacting Motif within LANA Is Essential for KSHV Latency
- Natural Selection Promotes Antigenic Evolvability
Kurzy
Zvyšte si kvalifikaci online z pohodlí domova
Současné možnosti léčby obezity
nový kurzAutoři: MUDr. Martin Hrubý
Všechny kurzyPřihlášení#ADS_BOTTOM_SCRIPTS#Zapomenuté hesloZadejte e-mailovou adresu, se kterou jste vytvářel(a) účet, budou Vám na ni zaslány informace k nastavení nového hesla.
- Vzdělávání



