-
Články
Top novinky
Reklama- Vzdělávání
- Časopisy
Top články
Nové číslo
- Témata
Top novinky
Reklama- Videa
- Podcasty
Nové podcasty
Reklama- Kariéra
Doporučené pozice
Reklama- Praxe
Top novinky
ReklamaIlluminating Fungal Infections with Bioluminescence
article has not abstract
Published in the journal: . PLoS Pathog 10(7): e32767. doi:10.1371/journal.ppat.1004179
Category: Pearls
doi: https://doi.org/10.1371/journal.ppat.1004179Summary
article has not abstract
What Is Bioluminescence Imaging (BLI)?
BLI is a powerful biophotonic imaging technology that allows in vivo visualization of temporal and spatial progression of infections in living organisms. BLI relies on the detection of visible light arising from an enzymatic reaction of oxidation known as bioluminescence. Originally, bioluminescence referred to the light emission of living organisms (e.g., bacteria, fungi, fish, insects, algae, and squid), which results from the oxidation of organic substrates mediated by catalysts named luciferases (Figure 1A) [1]. This fascinating natural phenomenon has been thus diverted to create bioluminescent microorganisms that are currently used in BLI as bioreporters. BLI has the advantages of being highly sensitive with excellent signal-to-noise ratios, and being non-invasive and nontoxic for animals. Such an approach has been applied in the past two decades to study the fate of tumor cells in various therapeutic settings and of several infectious agents including bacteria, viruses, parasitic protozoa, and, more recently, opportunistic fungi [2].
Fig. 1. Development and optimization of bioreporters for fungal infection BLI. 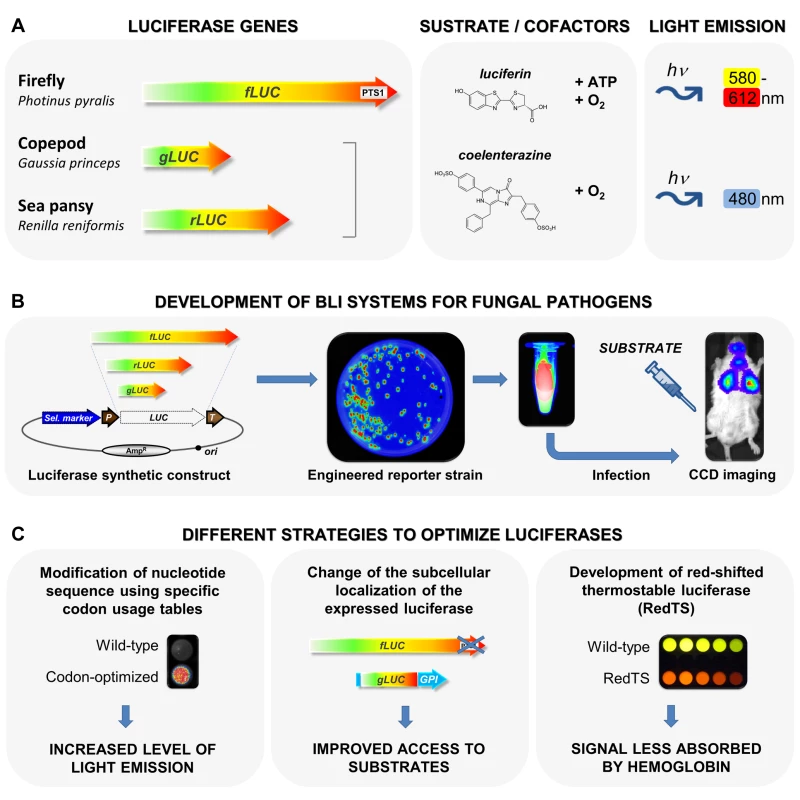
(A) The three luciferase-encoding genes used in Aspergillus and Candida species. The firefly (Photinus pyralis) fLUC gene encoding a luciferase (Fluc), which converts the substrate luciferin to oxy-luciferin in an ATP-dependent manner, the sea pansy (Renilla reniformis) rLUC and the copepod Gaussia (Gaussia princeps) gLUC, which both encode luciferases (Rluc and Gluc, respectively) that produce light emission from the substrate coelenterazine. All luciferases require oxygen for activity. (B) Schematic presentation of the different steps of the construction of fungal bioreporters and their use in BLI. A fungal strain is first genetically modified to stably express a luciferase gene as a reporter. Luciferase-expressing cells are used for animal infection and the substrate, luciferin or coelenterazine, is extemporaneously administered. Finally, light emitted from reporter cells is externally monitored in real time, using sensitive photon detectors based on cooled or intensified charge coupled devices (CCD). (C) Compilation of various strategies to optimize luciferases used in fungal infection BLI. This includes the adaptation of luciferase nucleotide sequences to the fungal host using specific codon usage tables (left panel), the change of the subcellular localization of the expressed luciferase either by removing (PTS1 of firefly luciferase) or by adding (GPI anchor for Gaussia luciferase) targeting sequences (middle panel), and the generation of red-shifted/thermostable firefly luciferases through enzyme redesign (right panel). In practice, an infectious agent is first genetically modified to stably express a luciferase gene (LUC) as a reporter (Figure 1A). Luciferase-expressing cells are then injected into animals and the substrate, luciferin or coelenterazine, is extemporaneously administered (Figure 1B). For bacterial bioreporters, substrate application is not required since prokaryotic lux operons include genes encoding luciferase and enzymes for substrate synthesis (long-chain aliphatic aldehyde). However, the bacterial luciferase dependence on FMNH2 as a co-substrate makes it less suitable for eukaryotic cells. Finally, regardless of the luciferase system used, light emitted from reporter cells is externally monitored in real time, using sensitive photon detectors based on cooled or intensified charge coupled devices (CCD) [3]. Thus, the special charm of the system results from repeated monitoring of individual animals at different time points.
What Were (Are) the Hurdles to Overcome in the Development of Fungal Infection BLI Models?
The development of BLI strategies for monitoring infections requires the construction of luciferase-expressing microorganisms that fit the special needs of subsequent experiments. To date, three different luciferase genes have been applied to infection studies on yeast and mold: (i) the firefly (Photinus pyralis) fLUC gene encoding a luciferase (Fluc), which converts the substrate luciferin to oxy-luciferin in an ATP-dependent manner, and (ii) the sea pansy (Renilla reniformis) rLUC and (iii) the copepod Gaussia (Gaussia princeps) gLUC, which both encode coelenterazine dependent luciferases (Rluc and Gluc, respectively) (Figure 1A) [2].
For a long time, the use of luciferase reporters in pathogenic fungi has been restricted to gene regulation studies [4]. However, recent technological advances aimed at developing BLI for fungal infections gave a new lease of life to these brilliant reporters. Indeed, a number of shackles have been released that were holding us back from obtaining robust fungal bioreporters (Figure 1C). For instance, efforts have been made to select strong promoters that provide high luciferase expression levels. Moreover, synthetic optimized luciferase sequences have improved light emission from bioluminescent strains (Figure 1C). In particular, the natural subcellular localizations of the Fluc, Gluc and Rluc proteins constituted real hurdles in pioneering works. The last three amino acids, SKL, of the wild-type firefly luciferase correspond to a strong type 1 peroxisomal targeting sequence (PTS1) (Figure 1A). It is now well established that this peroxisomal localization limits the access to the substrate luciferin, resulting in low light emission. As a consequence, PTS1 was removed from the firefly luciferase to design some of the currently available fungal infection BLI models (Figure 1C) [5]. Additionally, species-specific codon-optimization significantly increases luciferase translation efficiency (Figure 1C). Thus, synthetic optimization not only improves reporter strains from filamentous fungi, but appears to be of special importance to Candida albicans, which adopted an unconventional genetic code [6]–[10].
Recently, a breakthrough was also achieved via the rational optimization of some Gaussia luciferase-based BLI models. Basically, the Gaussia luciferase catalyzes an ATP-independent light emission and is naturally secreted from eukaryotic cells [11]. While uptake of the substrate coelenterazine by C. albicans cells is limited [7], its uncontrolled secretion may lead to increased background signals, reducing the sensitivity of the system as shown through in vivo monitoring of T cell recruitment in the murine setting [12]. The addition of a glycosylphosphatidylinositol (GPI) (Figure 1C) anchor to the Gaussia luciferase allowed a cell surface exposure of the enzyme that potentiates access to the substrate coelenterazine and promotes a focalization of strong photonic emissions from infected sites. This advance now represents the spearhead of powerful Gaussia luciferase-based BLI currently available for fungal infections [7], [8].
What Are the Currently Available BLI Systems for Pathogenic Fungi?
During the last decade, many efforts have been made to develop pioneering models of BLI for the most common opportunistic fungal infections such as candidiasis and aspergillosis.
The first BLI model of fungal infection was obtained for vulvo-vaginal candidiasis using a C. albicans strain that constitutively expressed a codon-modified version of the firefly luciferase as a bioreporter [13]. This system was sufficiently sensitive enough to detect bioluminescent C. albicans in the vaginal lumen of infected mice when the substrate luciferin was applied to the genital tract [13]. However, this approach failed to detect deep-seated systemic candidiasis. This failure might be largely attributed to the peroxisomal localization of the expressed luciferase, but restricted luciferin substrate permeability of C. albicans hyphae formed during infection has also been proposed. Both problems are now circumvented by using the cell surface–anchored Gaussia luciferase described above [7]. Unfortunately, this Candida bioluminescent strain does not appear to be a convenient reporter for imaging deep-seated C. albicans organ infections, because Gaussia luciferase emits light at 480 nm (Figure 1A), which is strongly absorbed by hemoglobin. Thus, this excellent model is mainly restricted to use in BLI of various superficial candidiasis models [14], [15].
However, studies on filamentous fungi have indicated that, in principle, hyphae are not completely impermeable to the firefly substrate luciferin, because pioneering BLI models for aspergillosis have successfully been applied. Initially, an Aspergillus fumigatus strain expressing a cytosolic-localized version of the firefly luciferase was used for monitoring of invasive aspergillosis [16] and the sensitivity of this system was significantly enhanced by a complete codon-adaptation of the firefly luciferase gene to the codon usage in A. fumigatus [10]. Recently, an A. fumigatus bioreporter expressing a cell wall–anchored version of the Gaussia luciferase was generated. Targeting of the luciferase into the secretory pathway and cell surface exposure of the enzyme were mediated by the incorporation of two additional secretion signals and a GPI-anchoring peptide in the Gaussia luciferase sequence. Similar to C. albicans, this BLI system is perfectly suited for sensitive detection of the fungal pathogen during cutaneous aspergillosis development in mice, but also failed in monitoring of deep-seated infections [8].
Finally, latest advances in BLI of deep-seated candidiasis look promising. With the above-mentioned knowledge, a completely synthetic firefly luciferase adapted to the codon usage of highly expressed C. albicans genes and lacking the PTS1 has been constructed and used to generate a new C. albicans bioreporter. First analyses in a murine infection model for disseminated candidiasis allowed successful monitoring of kidney infections with an excellent correlation between light intensity and fungal burden. Furthermore, cryptic host niches were detected that would have been overseen with conventional techniques (M. Brock, unpublished data, manuscript in revision). Thus, complete adaptation of luciferases to the respective fungal host appears essential for maximum sensitivity of the reporter system.
What Can Be Monitored Using Fungal Infection BLI Models?
The primary vocation of BLI for pathogenic fungal agents is to offer the possibility to follow with extreme accuracy, in real-time and in a non-invasive manner, the proliferation of microorganisms within intact living animals (Figure 1B).
From an ethical point of view, BLI thus allows a significant reduction in the number of animals required for such investigations (compared to traditional analyses performed post mortem), since multiple imaging of the same animal throughout an experiment can be easily carried out. As described above, the currently available fungal BLI infection models include cutaneous, subcutaneous, vaginal, oropharyngeal, and invasive candidiasis caused by C. albicans [7], [13], [17], [18], as well as invasive and cutaneous aspergillosis due to A. fumigatus [8], [16]. In addition to the spatial and temporal visualization of the infectious Candida or Aspergillus reporters, BLI now offers the possibility to study a wide range of other host–pathogen interactions, such as biofilm formation [19], [20] or interactions related to the host immune response [21], [22]. Furthermore, BLI opens a new window in monitoring antifungal drug efficacy in different organs during therapy of candidiasis [7], [13], [23] and aspergillosis [10]. Finally, BLI also represents an unprecedented, powerful approach to assist the development of new vaccines against fungal infections [24].
What Are the Future Challenges for Fungal Infection BLI?
Although recent advances clearly demonstrate the potential of BLI for monitoring cutaneous, subcutaneous, mucosal, and invasive mycosis, the available systems still suffer from major limitations, which have to be overcome to further expand their field of use.
All luciferases essentially require at least small amounts of oxygen (Figure 1A), which may be withdrawn locally by induced immune response in infected niches [5]. This remains a crucial bottleneck that may only be solved by a yet-undiscovered new class of luciferases that generate light independently of oxidation reactions. In addition, although cell surface–exposed Gaussia luciferase offers several advantages (small length, facilitated access to the substrate) compared to the large and ATP-hungry firefly luciferase (Figure 1A), its cognate substrate coelenterazine easily undergoes autoxidation (background signal), has a body site distribution that is strongly dependent on the application route (hidden infected sites), and a light emission at a wavelength (Figure 1A) strongly absorbed by hemoglobin (reduction of the signal) [5]. Thus, Gaussia luciferase currently only allows visualization of superficial infections. For these reasons, whereas significant progress was made in recent years to develop pioneering bioluminescent systems to monitor fungal infections, solving the equation concerning the improvement of BLI for deep fungal infections seems difficult and, therefore, represents a strong issue to take up. In this way, red-shifted coelenterazine analogues for Gaussia luciferase, as well as red-shifted and thermostable firefly luciferases [25] generated through enzyme redesign (Figure 1C), may enhance sensitivity of BLI, overcoming some of the current drawbacks. At the same time, the adaptation of BLI to other important fungal pathogens (as illustrated recently with Aspergillus terreus [9]), such as emerging non-albicans Candida species, dimorphic fungi, Cryptococcus, Fusarium, and zygomycetes, will certainly become a main challenge in the field.
Zdroje
1. GreerLF3rd, SzalayAA (2002) Imaging of light emission from the expression of luciferases in living cells and organisms: a review. Luminescence 17 : 43–74 doi:10.1002/bio.676
2. AndreuN, ZelmerA, WilesS (2011) Noninvasive biophotonic imaging for studies of infectious disease. FEMS Microbiol Rev 35 : 360–394 doi:10.1111/j.1574-6976.2010.00252
3. RiceBW, CableMD, NelsonMB (2001) In vivo imaging of light-emitting probes. J Biomed Opt 6 : 432–440 doi:10.1117/1.1413210
4. SollDR, SrikanthaT (1998) Reporters for the analysis of gene regulation in fungi pathogenic to man. Curr Opin Microbiol 1 : 400–405 Doi:10.1016/S1369-5274(98)80056-8
5. BrockM (2012) Application of bioluminescence imaging for in vivo monitoring of fungal infections. Int J Microbiol 2012 : 956794 doi:10.1155/2012/956794
6. DoyleTC, NawotkaKA, PurchioAF, AkinAR, FrancisKP, et al. (2006) Expression of firefly luciferase in Candida albicans and its use in the selection of stable transformants. Microb Pathog 40 : 69–81 doi:10.1016/j.micpath.2005.11.002
7. EnjalbertB, RachiniA, VediyappanG, PietrellaD, SpaccapeloR, et al. (2009) A multifunctional, synthetic Gaussia princeps luciferase reporter for live imaging of Candida albicans infections. Infect Immun 77 : 4847–4858 doi:10.1128/IAI.00223-09
8. DonatS, HasenbergM, SchäferT, OhlsenK, GunzerM, et al. (2012) Surface display of Gaussia princeps luciferase allows sensitive fungal pathogen detection during cutaneous aspergillosis. Virulence 3 : 51–61 doi:10.4161/viru.3.1.18799
9. SlesionaS, Ibrahim-GranetO, OliasP, BrockM, JacobsenID (2012) Murine infection models for Aspergillus terreus pulmonary aspergillosis reveal long-term persistence of conidia and liver degeneration. J Infect Dis 205 : 1268–1277 doi:10.1093/infdis/jis193
10. GaligerC, BrockM, JouvionG, SaversA, ParlatoM, et al. (2013) Assessment of efficacy of antifungals against Aspergillus fumigatus: value of real-time bioluminescence imaging. Antimicrob Agents Chemother 57 : 3046–3059 doi:10.1128/AAC.01660-12
11. PichlerA, PriorJL, Piwnica-WormsD (2004) Imaging reversal of multidrug resistance in living mice with bioluminescence: MDR1 P-glycoprotein transports coelenterazine. Proc Natl Acad Sci U S A 101 : 1702–1707 doi:10.1073/pnas.0304326101
12. SantosEB, YehR, LeeJ, NikhaminY, PunzalanB, et al. (2009) Sensitive in vivo imaging of T cells using a membrane-bound Gaussia princeps luciferase. Nat Med 15 : 338–344 doi:10.1038/nm.1930
13. DoyleTC, NawotkaKA, KawaharaCB, FrancisKP, ContagPR (2006) Visualizing fungal infections in living mice using bioluminescent pathogenic Candida albicans strains transformed with the firefly luciferase gene. Microb Pathog 40 : 82–90 doi:10.1016/j.micpath.2005.11.003
14. d'EnfertC, VecchiarelliA, BrownAJ (2010) Bioluminescent fungi for real-time monitoring of fungal infections. Virulence 1 : 174–176 doi:10.4161/viru.1.3.11119
15. VecchiarelliA, d'EnfertC (2012) Shedding natural light on fungal infections. Virulence 3 : 15–17 doi:10.4161/viru.3.1.19247
16. BrockM, JouvionG, Droin-BergèreS, DussurgetO, NicolaMA, et al. (2008) Bioluminescent Aspergillus fumigatus, a new tool for drug efficiency testing and in vivo monitoring of invasive aspergillosis. Appl Environ Microbiol 74 : 7023–7035 doi:10.1128/AEM.01288-08
17. PietrellaD, EnjalbertB, ZeidlerU, ZnaidiS, RachiniA, et al. (2012) A luciferase reporter for gene expression studies and dynamic imaging of superficial Candida albicans infections. Methods Mol Biol 845 : 537–546 doi:10.1007/978-1-61779-539-8_39
18. MosciP, PericoliniE, GabrielliE, KennoS, PeritoS, et al. (2013) A novel bioluminescence mouse model for monitoring oropharyngeal candidiasis in mice. Virulence 4 : 250–254 doi:10.1186/1471-2180-10-105
19. Vande VeldeG, KucharíkováS, SchrevensS, HimmelreichU, Van DijckP (2013) Towards non-invasive monitoring of pathogen-host interactions during Candida albicans biofilm formation using in vivo bioluminescence. Cell Microbiol 16 : 115–130 doi:10.1111/cmi.12184
20. Vande VeldeG, KucharíkováS, Van DijckP, HimmelreichU (2014) Bioluminescence imaging of fungal biofilm development in live animals. Methods Mol Biol 1098 : 153–167 doi:10.1007/978-1-62703-718-1_13
21. Ibrahim-GranetO, JouvionG, HohlTM, Droin-BergèreS, PhilippartF, et al. (2010) In vivo bioluminescence imaging and histopathopathologic analysis reveal distinct roles for resident and recruited immune effector cells in defense against invasive aspergillosis. BMC Microbiol 10 : 105 doi:10.1186/1471-2180-10-105
22. JouvionG, BrockM, Droin-BergèreS, Ibrahim-GranetO (2012) Duality of liver and kidney lesions after systemic infection of immunosuppressed and immunocompetent mice with Aspergillus fumigatus. Virulence 3 : 43–50 doi:10.4161/viru.3.1.18654
23. PietrellaD, AngiolellaL, VavalaE, RachiniA, MondelloF, et al. (2011) Beneficial effect of Mentha suaveolens essential oil in the treatment of vaginal candidiasis assessed by real-time monitoring of infection. BMC Complement Altern Med 11 : 18 doi:10.1186/1472-6882-11-18
24. PietrellaD, RachiniA, TorosantucciA, ChianiP, BrownAJ, et al. (2010) A beta-glucan-conjugate vaccine and anti-beta-glucan antibodies are effective against murine vaginal candidiasis as assessed by a novel in vivo imaging technique. Vaccine 28 : 1717–1725 doi:10.1016/j.vaccine
25. BranchiniBR, AblamskyDM, DavisAL, SouthworthTL, ButlerB, et al. (2010) Red-emitting luciferases for bioluminescence reporter and imaging applications. Anal Biochem 396 : 290–297 doi:10.1016/j.ab.2009.09.009
Štítky
Hygiena a epidemiologie Infekční lékařství Laboratoř
Článek Molecular and Cellular Mechanisms of KSHV Oncogenesis of Kaposi's Sarcoma Associated with HIV/AIDSČlánek The Semen Microbiome and Its Relationship with Local Immunology and Viral Load in HIV InfectionČlánek Peptidoglycan Recognition Proteins Kill Bacteria by Inducing Oxidative, Thiol, and Metal Stress
Článek vyšel v časopisePLOS Pathogens
Nejčtenější tento týden
2014 Číslo 7- Jak souvisí postcovidový syndrom s poškozením mozku?
- Měli bychom postcovidový syndrom léčit antidepresivy?
- Farmakovigilanční studie perorálních antivirotik indikovaných v léčbě COVID-19
- 10 bodů k očkování proti COVID-19: stanovisko České společnosti alergologie a klinické imunologie ČLS JEP
-
Všechny články tohoto čísla
- Bacteriophages as Vehicles for Antibiotic Resistance Genes in the Environment
- Helminth Infections, Type-2 Immune Response, and Metabolic Syndrome
- Defensins and Viral Infection: Dispelling Common Misconceptions
- Holobiont–Holobiont Interactions: Redefining Host–Parasite Interactions
- The Wide World of Ribosomally Encoded Bacterial Peptides
- Microbial Egress: A Hitchhiker's Guide to Freedom
- Molecular and Cellular Mechanisms of KSHV Oncogenesis of Kaposi's Sarcoma Associated with HIV/AIDS
- HIV-1 Capture and Transmission by Dendritic Cells: The Role of Viral Glycolipids and the Cellular Receptor Siglec-1
- Tetherin Can Restrict Cell-Free and Cell-Cell Transmission of HIV from Primary Macrophages to T Cells
- The Frustrated Host Response to Is Bypassed by MyD88-Dependent Translation of Pro-inflammatory Cytokines
- Larger Mammalian Body Size Leads to Lower Retroviral Activity
- The Semen Microbiome and Its Relationship with Local Immunology and Viral Load in HIV Infection
- Lytic Gene Expression Is Frequent in HSV-1 Latent Infection and Correlates with the Engagement of a Cell-Intrinsic Transcriptional Response
- Phase Variation of Poly-N-Acetylglucosamine Expression in
- A Screen of Mutants Reveals Important Roles for Dot/Icm Effectors and Host Autophagy in Vacuole Biogenesis
- Structure of the Trehalose-6-phosphate Phosphatase from Reveals Key Design Principles for Anthelmintic Drugs
- The Impact of Juvenile Coxsackievirus Infection on Cardiac Progenitor Cells and Postnatal Heart Development
- Vertical Transmission Selects for Reduced Virulence in a Plant Virus and for Increased Resistance in the Host
- Characterization of the Largest Effector Gene Cluster of
- Novel Drosophila Viruses Encode Host-Specific Suppressors of RNAi
- Pto Kinase Binds Two Domains of AvrPtoB and Its Proximity to the Effector E3 Ligase Determines if It Evades Degradation and Activates Plant Immunity
- Genetic Analysis of Tropism Using a Naturally Attenuated Cutaneous Strain
- Plasmacytoid Dendritic Cells Suppress HIV-1 Replication but Contribute to HIV-1 Induced Immunopathogenesis in Humanized Mice
- A Novel Mouse Model of Gastroenteritis Reveals Key Pro-inflammatory and Tissue Protective Roles for Toll-like Receptor Signaling during Infection
- Pathogenicity of Is Expressed by Regulating Metabolic Thresholds of the Host Macrophage
- BCKDH: The Missing Link in Apicomplexan Mitochondrial Metabolism Is Required for Full Virulence of and
- Independent Bottlenecks Characterize Colonization of Systemic Compartments and Gut Lymphoid Tissue by
- Peptidoglycan Recognition Proteins Kill Bacteria by Inducing Oxidative, Thiol, and Metal Stress
- G3BP1, G3BP2 and CAPRIN1 Are Required for Translation of Interferon Stimulated mRNAs and Are Targeted by a Dengue Virus Non-coding RNA
- Cytolethal Distending Toxins Require Components of the ER-Associated Degradation Pathway for Host Cell Entry
- The Machinery at Endoplasmic Reticulum-Plasma Membrane Contact Sites Contributes to Spatial Regulation of Multiple Effector Proteins
- Arabidopsis LIP5, a Positive Regulator of Multivesicular Body Biogenesis, Is a Critical Target of Pathogen-Responsive MAPK Cascade in Plant Basal Defense
- Plant Surface Cues Prime for Biotrophic Development
- Real-Time Imaging Reveals the Dynamics of Leukocyte Behaviour during Experimental Cerebral Malaria Pathogenesis
- The CD27L and CTP1L Endolysins Targeting Contain a Built-in Trigger and Release Factor
- cGMP and NHR Signaling Co-regulate Expression of Insulin-Like Peptides and Developmental Activation of Infective Larvae in
- Systemic Hematogenous Maintenance of Memory Inflation by MCMV Infection
- Strain-Specific Variation of the Decorin-Binding Adhesin DbpA Influences the Tissue Tropism of the Lyme Disease Spirochete
- Distinct Lipid A Moieties Contribute to Pathogen-Induced Site-Specific Vascular Inflammation
- Serovar Typhi Conceals the Invasion-Associated Type Three Secretion System from the Innate Immune System by Gene Regulation
- LANA Binds to Multiple Active Viral and Cellular Promoters and Associates with the H3K4Methyltransferase hSET1 Complex
- A Molecularly Cloned, Live-Attenuated Japanese Encephalitis Vaccine SA-14-2 Virus: A Conserved Single Amino Acid in the Hairpin of the Viral E Glycoprotein Determines Neurovirulence in Mice
- Illuminating Fungal Infections with Bioluminescence
- Comparative Genomics of Plant Fungal Pathogens: The - Paradigm
- Motility and Chemotaxis Mediate the Preferential Colonization of Gastric Injury Sites by
- Widespread Sequence Variations in VAMP1 across Vertebrates Suggest a Potential Selective Pressure from Botulinum Neurotoxins
- An Immunity-Triggering Effector from the Barley Smut Fungus Resides in an Ustilaginaceae-Specific Cluster Bearing Signs of Transposable Element-Assisted Evolution
- Establishment of Murine Gammaherpesvirus Latency in B Cells Is Not a Stochastic Event
- Oncogenic Herpesvirus KSHV Hijacks BMP-Smad1-Id Signaling to Promote Tumorigenesis
- Human APOBEC3 Induced Mutation of Human Immunodeficiency Virus Type-1 Contributes to Adaptation and Evolution in Natural Infection
- Innate Immune Responses and Rapid Control of Inflammation in African Green Monkeys Treated or Not with Interferon-Alpha during Primary SIVagm Infection
- Chitin-Degrading Protein CBP49 Is a Key Virulence Factor in American Foulbrood of Honey Bees
- Influenza A Virus Host Shutoff Disables Antiviral Stress-Induced Translation Arrest
- Nsp9 and Nsp10 Contribute to the Fatal Virulence of Highly Pathogenic Porcine Reproductive and Respiratory Syndrome Virus Emerging in China
- Pulmonary Infection with Hypervirulent Mycobacteria Reveals a Crucial Role for the P2X7 Receptor in Aggressive Forms of Tuberculosis
- Syk Signaling in Dendritic Cells Orchestrates Innate Resistance to Systemic Fungal Infection
- A Repetitive DNA Element Regulates Expression of the Sialic Acid Binding Adhesin by a Rheostat-like Mechanism
- T-bet and Eomes Are Differentially Linked to the Exhausted Phenotype of CD8+ T Cells in HIV Infection
- Israeli Acute Paralysis Virus: Epidemiology, Pathogenesis and Implications for Honey Bee Health
- Influence of ND10 Components on Epigenetic Determinants of Early KSHV Latency Establishment
- Antibody to gp41 MPER Alters Functional Properties of HIV-1 Env without Complete Neutralization
- PLOS Pathogens
- Archiv čísel
- Aktuální číslo
- Informace o časopisu
Nejčtenější v tomto čísle- Molecular and Cellular Mechanisms of KSHV Oncogenesis of Kaposi's Sarcoma Associated with HIV/AIDS
- Holobiont–Holobiont Interactions: Redefining Host–Parasite Interactions
- BCKDH: The Missing Link in Apicomplexan Mitochondrial Metabolism Is Required for Full Virulence of and
- Helminth Infections, Type-2 Immune Response, and Metabolic Syndrome
Kurzy
Zvyšte si kvalifikaci online z pohodlí domova
Současné možnosti léčby obezity
nový kurzAutoři: MUDr. Martin Hrubý
Všechny kurzyPřihlášení#ADS_BOTTOM_SCRIPTS#Zapomenuté hesloZadejte e-mailovou adresu, se kterou jste vytvářel(a) účet, budou Vám na ni zaslány informace k nastavení nového hesla.
- Vzdělávání



