-
Články
Top novinky
Reklama- Vzdělávání
- Časopisy
Top články
Nové číslo
- Témata
Top novinky
Reklama- Videa
- Podcasty
Nové podcasty
Reklama- Kariéra
Doporučené pozice
Reklama- Praxe
Top novinky
ReklamaInflammatory Responses Associated with the Induction of Cerebral Malaria: Lessons from Experimental Murine Models
article has not abstract
Published in the journal: . PLoS Pathog 8(12): e32767. doi:10.1371/journal.ppat.1003045
Category: Pearls
doi: https://doi.org/10.1371/journal.ppat.1003045Summary
article has not abstract
Introduction
Malaria is one the most serious infectious diseases of humans, with ∼500 million clinical cases annually. Most cases of severe disease are caused by Plasmodium falciparum, which is endemic in sub-Saharan Africa and throughout the tropics. Severe malaria is associated with a range of disease syndromes including respiratory distress, metabolic acidosis, hypoglycaemia, renal failure, and cerebral malaria (CM) [1]. The blood stage of the parasite is entirely responsible for malaria-associated pathology. Mature forms of P. falciparum blood-stage express parasitic proteins (such as P. falciparum erythrocyte membrane protein 1) on the surface of the infected erythrocyte, which allow them to bind to vascular endothelial cells and avoid clearance in the spleen. This process called sequestration induces obstructions in the blood flow and is postulated to result in hypoxia and haemorrhages that appear to be associated with the development of organ-specific syndromes such CM and placental malaria [1]. Many disease-association studies indicate that in addition to parasite sequestration, inflammatory responses also contribute to severe disease [1]. High TNF, IFN-γ, and IL-1β levels have been associated with disease severity [1]. The role of inflammatory cytokines in severe malaria is not completely understood, but they are thought to contribute to disease by up-regulating the expression of adhesion molecules such as ICAM-1 involved in the binding of parasitised red blood cells (pRBCs) to the vascular endothelium. Although parasite sequestration is the most common feature of patients succumbing to CM, postmortem examination has also revealed intra - and peri-vascular pathology including the presence of leukocytes within brain blood vessels [2]. These findings suggested that sequestration of host leukocytes might also contribute to the pathogenesis of some CM cases. Interestingly, recent findings revealed that increased levels of several inflammatory chemokines including MIP-1α and MIP-1β [3] and CXCL10 or IP-10 are associated with increased risk of severe malaria [4], suggesting a role for leukocyte trafficking in the etiology of human disease.
Clearly, the analysis of intravascular inflammation predisposing to CM in humans is limited to the examination of post-mortem samples. Thus, murine malaria models constitute a valuable tool to obtain detailed mechanistic information, which cannot be deduced from human studies. Much useful evidence on the inflammatory processes (Figure 1) contributing to the induction of CM has been provided by the Plasmodium berghei ANKA model. This rodent infection has several features in common with human disease and is the best available model of severe malaria. Like in humans, pRBCs have been found to accumulate in brains of susceptible mice during infection. Numerous leukocytes are also present in brain blood vessels of these animals. This article summarizes the main lessons learnt from murine malaria studies and illustrates how emerging information on inflammatory pathways predisposing to disease might open new avenues for the development of therapeutic strategies to alleviate severe malaria.
Fig. 1. Inflammatory responses involved in the induction of ECM. 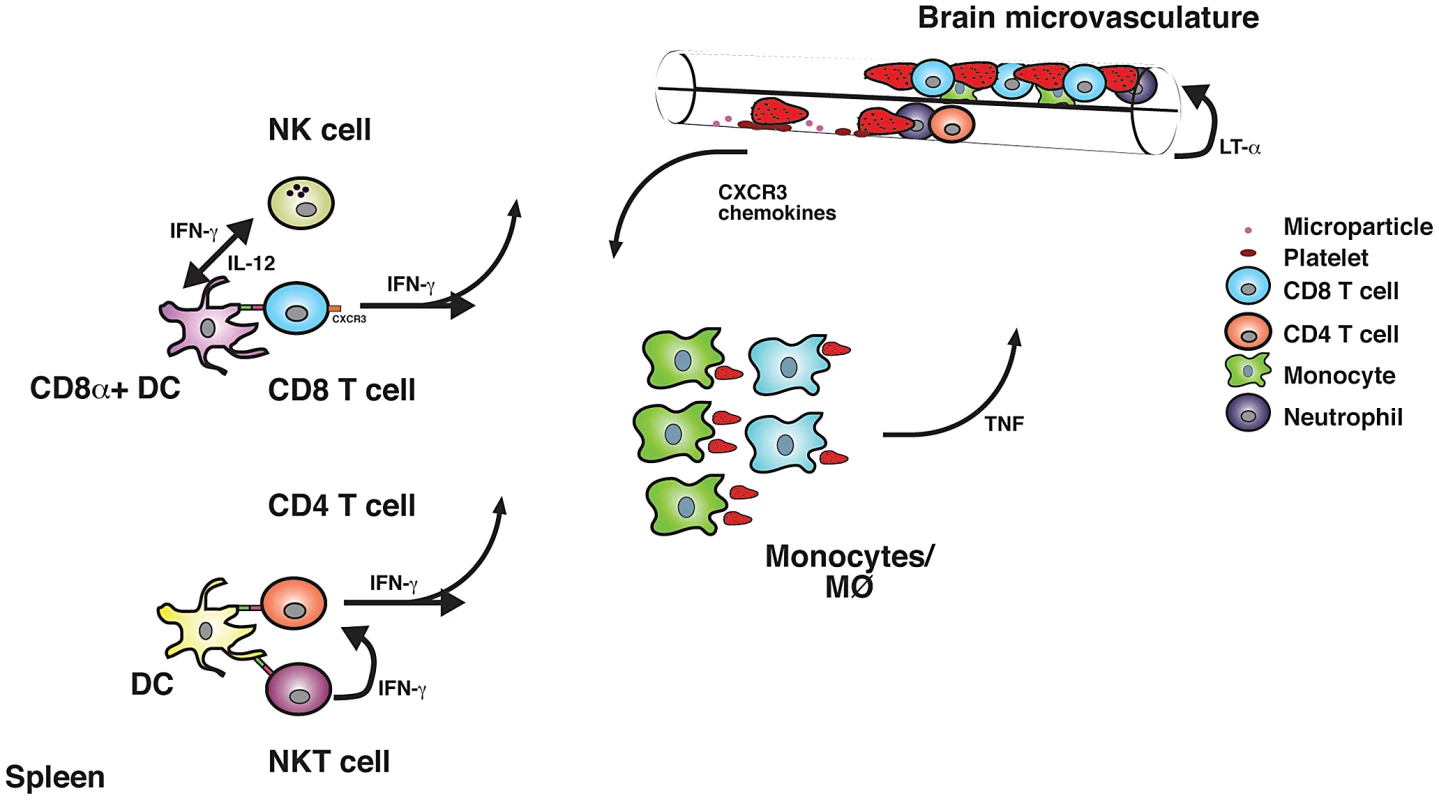
After phagocytosis of pRBC, conventional DCs in the spleen present malarial antigens to CD4+ and CD8+ T cells. CD8α+ DC is the main subset involved in the cross-presentation of parasite-expressed antigens to CD8+ T cells. NK cells enhance the capacity of CD8α+ DCs to prime naïve CD8+ T cells. In turn, DC-derived IL-12 is required for efficient NK cell responses to infection. IFN-γ secretion by CD1-restricted NKT cells appears to favour Th1 polarization. High IFN-γ levels contribute to the activation of macrophages/monocytes, which phagocytose pRBC and secrete other inflammatory cytokines such as TNF. Systemic pro-inflammatory cytokine responses and pRBC in brain blood vessels activate the vascular endothelium. This results in the release of MPs, which might enhance pRBC accumulation within brain blood vessels. Platelets might also contribute to this process. Activated endothelial cells release cytokines and chemotactic factors, which facilitate the recruitment of inflammatory cells. Neutrophils migrate to the brain and have been shown to contribute to disease induction. Activated CD8+ T cells and to a lesser extent CD4+ T cells up-regulate the expression of chemokine receptors such as CXCR3, which allows them to migrate to the inflamed organ. Sequestered pRBC and leukocytes impair cerebral blood flow, which might result in hypoxia. Cytotoxic molecules released by inflammatory leukocytes compromise the integrity of the blood brain barrier, which results in oedema and haemorrhages associated with the onset of severe disease. Systemic and Organ-Specific Inflammation Mediated by Leukocytes
Inflammatory responses mediated by cytokines such as TNF [5], IFN-γ [6], LT-α [7], and effector cells including CD4+T [8], CD8+T [9], [10], NKT [11], and NK cells [12] have been shown to contribute to the development of experimental CM (ECM). CBA and C57BL/6 mice, predisposed towards Type-1 responses, are susceptible to the ECM, whereas BALB/c mice are resistant. C57BL/6 and BALB/c mouse strains differ in the expression of molecules encoded by a genetic region called the Natural Killer Complex (NKC), and it has been shown that the differential expression of these receptors in CD1d-restricted NKT cells influences their immunological behaviour in response to malaria and accounts for the degree of susceptibility to ECM [11]. The expression of C57BL/6 NKC alleles, which is associated with disease severity, appears to favour enhanced IFN-γ responses to infection [11].
The role of T cells in the pathogenesis of ECM has been extensively investigated. Antibody depletion studies as well as infection of β2-microglobulin−/− mice demonstrated that CD8+ T cells contribute to the induction of ECM [8]. Cytotoxic CD8+ T cells have been found sequestered within brain blood vessels of P. berghei ANKA-infected mice [9], [10], and they appear to mediate CM via a perforin-dependent mechanism. The vast majority of inflammatory CD8+ T cells as well as CD4+ T cells and NK cells migrate to the brain of infected animals via a CXCR3-IP-10-dependent mechanism [13]–[15]. Brain-sequestered CD8+ T cells have been found to be specific for parasite-expressed model antigens [16]. Dendritic cells (DCs) are essential for the priming of T cell responses involved in the development of ECM [17]. Amongst these cells, CD8α+ conventional DCs are the main subset involved in the cross-presentation of parasite-expressed antigens to naïve CD8+ T cells [16].
CD4+ T cells have also been found in brain blood vessels of CM-affected mice [10]. They are not as abundant as CD8+ T cells, and it is not clear if they are parasite-specific or not. Nevertheless, in vivo depletion of CD4+ T cells with antibodies or genetic deletion of MHC class II molecules [8] also results in protection of susceptible mice from ECM. Recent work demonstrated that IFN-γ production by CD4+ T cells is required for the recruitment of CD8+ T cells to the brain of infected animals [18].
NK cells are important mediators of IFN-γ responses to malaria in humans and mice. Specific depletion of NK cells protects mice from P. berghei ANKA-mediated severe disease [12]. NK cells were shown to stimulate the recruitment of CXCR3+ T cells to the brain of malaria-infected mice in an IFN-γ-mediated manner [12]. More specifically, NK cells appear to stimulate the DC-mediated priming of naïve CD8+ T cells in response to P. berghei ANKA [19].
Cytokine-Dependent Activation of the Brain Vascular Endothelium
IFN-γ as well as members of the TNF superfamily such as LT-α and TNF [20] are produced in large amounts during infection and play important roles in the activation of the vascular endothelium. ICAM-1, VCAM-1, and P-selectin become highly up-regulated on brain vascular endothelial cells during the development of ECM [1]. Moreover, ICAM-1 - [21] and P-selectin - [22] deficient mice were found to be resistant to ECM. Leukocyte adhesion to the brain microvasculature was not inhibited in these animals. In contrast, the binding of platelets, which have been suggested to play a role in the development of CM in humans and mice, was substantially reduced in ICAM-1−/− and P-selectin−/− mice [23]. Whether genetic deletion of these adhesion molecules inhibits pRBC accumulation in the brain has not been investigated yet.
Cytokine-mediated activation of the vascular endothelium might also result in the release on microparticles (MPs). These submicron vesicles have been implicated in various neuroinflammatory conditions [24]. MPs were found in high numbers in patients with acute CM, they appear to increase the binding of pRBC to endothelial cells, and inhibition of their production in P. berghei ANKA-infected mice protects from the onset of the cerebral disease [24].
The Contribution of Inflammatory Responses to Parasite Tissue-Sequestration
Accumulation of pRBC within brain blood vessels has been detected in CM-affected mice [25]. Unlike P. falciparum, in which the ligands responsible for cytoadherance have been extensively investigated, the mechanism by which pRBC accumulate in the brain during rodent malaria is still unknown. P. berghei ANKA transgenic parasites expressing luciferase have been generated [26] and are a valuable resource to address this question. Bioluminescence in mice receiving a synchronous infection for 22–30 h has been detected in lungs, spleen, and adipose tissue but not brain [26]. Although these findings initially implied that brain sequestration was not required for cerebral pathology in this model, the results could not exclude the possibility that the short infection period used in the study was insufficient for appropriate induction of inflammatory responses and activation of the brain vasculature, which appear to be required for parasite brain accumulation. In support of that view, parasite sequestration could be readily detected after 6–7 days of infection with luciferase-expressing lines in brains of intracardially perfused mice [15]. Moreover, parasite biomass in the brain was found to be associated with increased risk of CM [15].
The contribution of inflammatory responses to pRBC accumulation in the brain has been recently investigated [27], [28]. Consistent with previous observations [15], parasite sequestration in various organs, including the brain, was found to be strongly associated with the onset of ECM. Furthermore, CD4+ T cells, CD8+ T cells, and the cytokines IFN-γ and LT-α appear to directly promote this process [27], [28].
Why Is It Useful to Have a Good Model of Severe Malaria?
There is an urgent need to develop adjunct therapies to improve the outcome of CM patients during treatment with antimalarial drugs. Good preclinical animal models provide a fast and cost-effective resource for assessment of new interventions. Although some interventions such as anti-TNF therapy that prevented ECM have not been effective in humans [29], other treatments such as L-arginine or NO administration appear to be protective in mice and humans [30], [31]. An important consideration that should be taken into account in the design of adjunctive therapies for severe malaria is that many inflammatory responses that contribute to disease are also involved in the control of parasite densities. Novel approaches such as inhibition of endothelial activation [32] and anti-chemokine therapies [15] are emerging as potential safe therapeutic alternatives, as they alleviate organ-specific inflammation without inducing a generalised immunosuppression of the host.
Zdroje
1. SchofieldL, GrauGE (2005) Immunological processes in malaria pathogenesis. Nat Rev Immunol 5 : 722–735.
2. TaylorTE, FuWJ, CarrRA, WhittenRO, MuellerJS, et al. (2004) Differentiating the pathologies of cerebral malaria by postmortem parasite counts. Nat Med 10 : 143–145.
3. OchielDO, AwandareGA, KellerCC, HittnerJB, KremsnerPG, et al. (2005) Differential regulation of beta-chemokines in children with Plasmodium falciparum malaria. Infect Immun 73 : 4190–4197.
4. ArmahHB, WilsonNO, SarfoBY, PowellMD, BondVC, et al. (2007) Cerebrospinal fluid and serum biomarkers of cerebral malaria mortality in Ghanaian children. Malar J 6 : 147.
5. GrauGE, FajardoLF, PiguetPF, AlletB, LambertPH, et al. (1987) Tumor necrosis factor (cachectin) as an essential mediator in murine cerebral malaria. Science 237 : 1210–1212.
6. GrauGE, HeremansH, PiguetPF, PointaireP, LambertPH, et al. (1989) Monoclonal antibody against interferon γ can prevent experimental cerebral malaria and its associated overproduction of tumor necrosis factor. Proc Natl Acad Sci USA 86 : 5572–5574.
7. EngwerdaCR, MynottTL, SawhneyS, De SouzaJB, BickleQD, et al. (2002) Locally up-regulated lymphotoxin alpha, not systemic tumor necrosis factor alpha, is the principle mediator of murine cerebral malaria. J Exp Med 195 : 1371–1377.
8. YanezDM, ManningDD, CooleyAJ, WeidanzWP, van der HeydeHC (1996) Participation of lymphocyte subpopulations in the pathogenesis of experimental murine cerebral malaria. J Immunol 157 : 1620–1624.
9. NitcheuJ, BonduelleO, CombadiereC, TefitM, SeilheanD, et al. (2003) Perforin-dependent brain-infiltrating cytotoxic CD8+ T lymphocytes mediate experimental cerebral malaria pathogenesis. J Immunol 170 : 2221–2228.
10. BelnoueE, KayibandaM, VigarioAM, DescheminJC, van RooijenN, et al. (2002) On the pathogenic role of brain-sequestered alphabeta CD8+ T cells in experimental cerebral malaria. J Immunol 169 : 6369–6375.
11. HansenDS, SiomosMA, BuckinghamL, ScalzoAA, SchofieldL (2003) Regulation of murine cerebral malaria pathogenesis by CD1d-restricted NKT cells and the natural killer complex. Immunity 18 : 391–402.
12. HansenDS, BernardNJ, NieCQ, SchofieldL (2007) NK cells stimulate recruitment of CXCR3+ T cells to the brain during Plasmodium berghei-mediated cerebral malaria. J Immunol 178 : 5779–5788.
13. CampanellaGS, TagerAM, El KhouryJK, ThomasSY, AbrazinskiTA, et al. (2008) Chemokine receptor CXCR3 and its ligands CXCL9 and CXCL10 are required for the development of murine cerebral malaria. Proc Natl Acad Sci U S A 105 : 4814–4819.
14. MiuJ, MitchellAJ, MullerM, CarterSL, MandersPM, et al. (2008) Chemokine gene expression during fatal murine cerebral malaria and protection due to CXCR3 deficiency. J Immunol 180 : 1217–1230.
15. NieCQ, BernardNJ, NormanMU, AmanteFH, LundieRJ, et al. (2009) IP-10-mediated T cell homing promotes cerebral inflammation over splenic immunity to malaria infection. PLoS Pathog 5: e1000369 doi: 10.1371/journal.ppat.1000369.
16. LundieRJ, de Koning-WardTF, DaveyGM, NieCQ, HansenDS, et al. (2008) Blood-stage Plasmodium infection induces CD8+ T lymphocytes to parasite-expressed antigens, largely regulated by CD8alpha+ dendritic cells. Proc Natl Acad Sci U S A 105 : 14509–14514.
17. deWalickS, AmanteFH, McSweeneyKA, RandallLM, StanleyAC, et al. (2007) Cutting edge: conventional dendritic cells are the critical APC required for the induction of experimental cerebral malaria. J Immunol 178 : 6033–6037.
18. Villegas-MendezA, GreigR, ShawTN, de SouzaJB, Gwyer FindlayE, et al. (2012) IFN-gamma-producing CD4+ T cells promote experimental cerebral malaria by modulating CD8+ T cell accumulation within the brain. J Immunol 189 : 968–979.
19. Ryg-Cornejo V, Nie CQ, Bernard NJ, Lundie RJ, Evans KJ, et al.. (2012) NK cells and conventional dendritic cells engage in reciprocal activation for the induction of inflammatory responses during Plasmodium berghei ANKA infection. Immunobiol E-pub ahead of print 23 May 2012. Available: dx.doi.org/10.1016/j.imbio.2012.05.018.
20. RandallLM, EngwerdaCR (2010) TNF family members and malaria: old observations, new insights and future directions. Exp Parasitol 126 : 326–331.
21. LiJ, ChangWL, SunG, ChenHL, SpecianRD, et al. (2003) Intercellular adhesion molecule 1 is important for the development of severe experimental malaria but is not required for leukocyte adhesion in the brain. J Investig Med 51 : 128–140.
22. CombesV, RosenkranzAR, RedardM, PizzolatoG, LepidiH, et al. (2004) Pathogenic role of P-selectin in experimental cerebral malaria: importance of the endothelial compartment. Am J Pathol 164 : 781–786.
23. SunG, ChangWL, LiJ, BerneySM, KimpelD, et al. (2003) Inhibition of platelet adherence to brain microvasculature protects against severe Plasmodium berghei malaria. Infect Immun 71 : 6553–6561.
24. CombesV, El-AssaadF, FailleD, JambouR, HuntNH, et al. (2010) Microvesiculation and cell interactions at the brain-endothelial interface in cerebral malaria pathogenesis. Prog Neurobiol 91 : 140–151.
25. HearnJ, RaymentN, LandonDN, KatzDR, de SouzaJB (2000) Immunopathology of cerebral malaria: morphological evidence of parasite sequestration in murine brain microvasculature. Infect Immun 68 : 5364–5376.
26. Franke-FayardB, JanseCJ, Cunha-RodriguesM, RamesarJ, BuscherP, et al. (2005) Murine malaria parasite sequestration: CD36 is the major receptor, but cerebral pathology is unlinked to sequestration. Proc Natl Acad Sci U S A 102 : 11468–11473.
27. AmanteFH, HaqueA, StanleyAC, Rivera FdeL, RandallLM, et al. (2010) Immune-mediated mechanisms of parasite tissue sequestration during experimental cerebral malaria. J Immunol 185 : 3632–3642.
28. ClaserC, MalleretB, GunSY, WongAY, ChangZW, et al. (2011) CD8+ T cells and IFN-gamma mediate the time-dependent accumulation of infected red blood cells in deep organs during experimental cerebral malaria. PLoS ONE 6: e18720 doi:10.1371/journal.pone.0018720.
29. van HensbroekMB, PalmerA, OnyiorahE, SchneiderG, JaffarS, et al. (1996) The effect of a monoclonal antibody to tumor necrosis factor on survival from childhood cerebral malaria. J Infect Dis 174 : 1091–1097.
30. GramagliaI, SobolewskiP, MeaysD, ContrerasR, NolanJP, et al. (2006) Low nitric oxide bioavailability contributes to the genesis of experimental cerebral malaria. Nat Med 12 : 1417–1422.
31. YeoTW, LampahDA, GitawatiR, TjitraE, KenangalemE, et al. (2008) Recovery of endothelial function in severe falciparum malaria: relationship with improvement in plasma L-arginine and blood lactate concentrations. J Infect Dis 198 : 602–608.
32. WassmerSC, CiancioloGJ, CombesV, GrauGE (2005) Inhibition of endothelial activation: a new way to treat cerebral malaria? PLoS Med 2: e245 doi:10.1371/journal.pmed.0020245.
Štítky
Hygiena a epidemiologie Infekční lékařství Laboratoř
Článek vyšel v časopisePLOS Pathogens
Nejčtenější tento týden
2012 Číslo 12- Jak souvisí postcovidový syndrom s poškozením mozku?
- Měli bychom postcovidový syndrom léčit antidepresivy?
- Farmakovigilanční studie perorálních antivirotik indikovaných v léčbě COVID-19
- 10 bodů k očkování proti COVID-19: stanovisko České společnosti alergologie a klinické imunologie ČLS JEP
-
Všechny články tohoto čísla
- Virus-Encoded microRNAs: An Overview and a Look to the Future
- Reactive Oxygen Species Production and Survivorship in with Artificial Infection Types
- Zinc Exploitation by Pathogenic Fungi
- Attenuated Typhimurium Lacking the Pathogenicity Island-2 Type 3 Secretion System Grow to High Bacterial Numbers inside Phagocytes in Mice
- The Polyfunctionality of Human Memory CD8+ T Cells Elicited by Acute and Chronic Virus Infections Is Not Influenced by Age
- How the Fly Balances Its Ability to Combat Different Pathogens
- MiniCD4 Microbicide Prevents HIV Infection of Human Mucosal Explants and Vaginal Transmission of SHIV in Cynomolgus Macaques
- Bidirectional Transfer of RNAi between Honey Bee and : Gene Silencing Reduces Population
- Global Gene Transcriptome Analysis in Vaccinated Cattle Revealed a Dominant Role of IL-22 for Protection against Bovine Tuberculosis
- Morphogenesis in Fungal Pathogenicity: Shape, Size, and Surface
- Inflammatory Responses Associated with the Induction of Cerebral Malaria: Lessons from Experimental Murine Models
- News from the Fungal Front: Wall Proteome Dynamics and Host–Pathogen Interplay
- Blood Flukes Exploit Peyer's Patch Lymphoid Tissue to Facilitate Transmission from the Mammalian Host
- Parallels in Intercellular Communication in Oomycete and Fungal Pathogens of Plants and Humans
- Influenza Human Monoclonal Antibody 1F1 Interacts with Three Major Antigenic Sites and Residues Mediating Human Receptor Specificity in H1N1 Viruses
- PLOS Pathogens
- Archiv čísel
- Aktuální číslo
- Informace o časopisu
Nejčtenější v tomto čísle- Influenza Human Monoclonal Antibody 1F1 Interacts with Three Major Antigenic Sites and Residues Mediating Human Receptor Specificity in H1N1 Viruses
- Parallels in Intercellular Communication in Oomycete and Fungal Pathogens of Plants and Humans
- Virus-Encoded microRNAs: An Overview and a Look to the Future
- Reactive Oxygen Species Production and Survivorship in with Artificial Infection Types
Kurzy
Zvyšte si kvalifikaci online z pohodlí domova
Současné možnosti léčby obezity
nový kurzAutoři: MUDr. Martin Hrubý
Všechny kurzyPřihlášení#ADS_BOTTOM_SCRIPTS#Zapomenuté hesloZadejte e-mailovou adresu, se kterou jste vytvářel(a) účet, budou Vám na ni zaslány informace k nastavení nového hesla.
- Vzdělávání



