-
Články
Top novinky
Reklama- Vzdělávání
- Časopisy
Top články
Nové číslo
- Témata
Top novinky
Reklama- Videa
- Podcasty
Nové podcasty
Reklama- Kariéra
Doporučené pozice
Reklama- Praxe
Top novinky
ReklamaLong-Term Outcomes Associated with Traumatic Brain Injury in Childhood and Adolescence: A Nationwide Swedish Cohort Study of a Wide Range of Medical and Social Outcomes
In a population-wide observational cohort, Seena Fazel and colleagues use a sibling-matched design to examine the burden of long-term outcomes associated with traumatic brain injury.
Published in the journal: . PLoS Med 13(8): e32767. doi:10.1371/journal.pmed.1002103
Category: Research Article
doi: https://doi.org/10.1371/journal.pmed.1002103Summary
In a population-wide observational cohort, Seena Fazel and colleagues use a sibling-matched design to examine the burden of long-term outcomes associated with traumatic brain injury.
Introduction
The World Health Organization ranks traumatic brain injury (TBI) as the leading cause of both disability and mortality in individuals below the age of 45 y [1]. Conservative estimates from the United States indicate that TBI accounts for an annual combined average of approximately 848,000 hospital admissions and emergency room visits in individuals under the age of 25 y, the majority of which classified as concussions or mild TBI [2]. In England and Wales, it is estimated that between 462,200 and 700,000 children under 15 y of age attend emergency departments annually with head injury [3]. Similar findings have been reported in other high-income countries [4–6].
Epidemiological studies have consistently found higher rates of adverse outcomes in adults who have sustained a TBI when compared to the general population [7–16]. However, there is a lack of large-scale studies that have examined the potential long-term impact of TBI exposure during childhood and adolescence. Importantly, there is a gap in the literature identifying how injury characteristics (e.g., severity, recurrence, and developmental timing) might moderate such associations. Previous work suggests that TBI in children contributes to poorer measures of emotion perception and social interaction [17,18], employment, and quality of life [19,20]. Nevertheless, uncertainty remains as to how early TBI exposure is related to a broader set of specific medical and social functioning outcomes in adulthood [10,21,22], such as premature mortality, disability pension, and educational attainment. Some of this uncertainty is attributed to small and selected clinical samples, poor adjustments for confounding factors, and non-specific outcomes that measure global disabilities.
Therefore, we have used population-based registers of the entire Swedish population born between 1973 and 1982 to examine how exposure to a TBI from birth up to age 25 y is associated with functioning in adulthood. These datasets have allowed us to examine the extent to which injury severity and recurrent injuries predict a range of long-term outcomes. Injuries to the brain during developmentally sensitive periods may be particularly problematic [23,24]. We have also separately considered the associations between TBI experienced during different developmental stages during childhood and adolescence and the adverse functioning outcomes in adulthood. A unique feature of this study is the use of the sibling-comparison design [25]. This has been adopted in previous Swedish studies [8,16] and allows one to account for unobserved familial (e.g., genetic and environmental) confounders. This is important because previous research has demonstrated that indicators of medical and social functioning are considerably heritable [26–28]. By comparing differentially exposed siblings, we were able to account for an aggregate of their shared genetic and environmental risks, which allowed us to estimate more accurate estimates of the consequences of early TBI exposure.
Methods
Swedish Nationwide Registers
This study was approved by the Regional Research Ethics Committee in Stockholm (RRECiS; 2013/5 : 8). Statistics Sweden, an independent governmental agency, maintains a number of nationwide longitudinal registries with routinely gathered governmental agency data. A ten-digit civic registration number assigned to all Swedish residents enables them to merge all of these registers. Following the approval from the RRECiS, we were given access to anonymised data.
The Total Population/Multi-Generation Register (TPR/MGR; 1932–2014) linked all Swedish residents to their biological parents, allowing us to identify all biological full siblings. Emigration and mortality dates were derived from the Migration and the Causes of Death Registers (1973–2014), respectively. The National Patient Register provided data on inpatient care (based on International Classification of Diseases eighth, ninth, and tenth editions [ICD-8, ICD-9 and ICD-10] codes; 1973–2013) and outpatient care (ICD-10; 2001–2013). Parental criminal convictions were gathered from the National Crime Register, which includes all criminal convictions in lower general court in Sweden (1973–2013). Annual sociodemographic data were derived from the following census registers covering all Swedish residents who were alive at the end of each year: the Education Register (1985–2012), the Population and Housing Register (1985), and the Integrated Database for Labour Market Research (LISA; 1990–2012).
Sample
Our initial sample included all Swedish children born between 1973 and 1985 (n = 1,333,919). In the following order, we excluded those who could not be linked to both of their biological parents (n = 63,018), had died (n = 16,806) or had migrated (n = 95,327) before the age of 26 y, as well as those who lacked data on parental sociodemographic factors (n = 3,427) and adulthood outcome measures (n = 11,871). The final sample therefore consisted of 1,143,470 children with complete data, of which 683,860 had at least one biological full-sibling. We found no evidence of non-random selection effects in the excluded sample (S1 Text).
Measures
Definition of TBI
We defined an individual who had sought treatment for at least one episode of a concussion (mild TBI) or a moderate-to-severe TBI before 25 y of age as a TBI patient. The patients were diagnosed in specialist care according to ICD-criteria (see S1 Table). Mild TBI diagnoses recorded in the Swedish National Patient Register have demonstrated excellent validity (positive predictive value = 100%; negative predictive value = 99.8%) [29]. Similar results have also been found for unintentional injuries [30]. To examine the effects of injury severity, we also generated separate measures for mild TBI and moderate to severe TBI. Individuals who had sustained a mild and a moderate-to-severe TBI were only included in the omnibus TBI measure. We defined recurrence as two or more episodes of TBI. To avoid bias resulting from duplicate records of the same episode in the registries, we excluded episodes that had occurred within 15 d of one another.
We examined developmentally sensitive periods by stratifying the group of TBI patients according to their age at first injury using the same age categories as the US Centers for Disease Control and Prevention [2], namely 0–4 y, 5–9 y, 10–14 y, 15–19 y, and 20–24 y. To investigate whether our findings were specific to TBI or to a general proneness to injury, we additionally examined a group of individuals who had been through at least one episode of fall-related injury but who had not been diagnosed with a TBI in a sensitivity test.
Outcomes
Six outcome variables that assessed specific dimensions of both medical and social functioning were examined. The baseline of the study started during the year that the individuals turned 26 y of age and we followed them in the registers until they experienced the outcome, migrated, died, or exited the study (e.g., the end of 2012–2014 depending on the outcome of interest). “Disability pension” measured whether the individual was in receipt of disability pension (covering up to 65% of lost wages) due to permanent work incapacity [31]. “Psychiatric visit” or “psychiatric hospitalisation” measured whether the individual had visited an outpatient clinic or been admitted to inpatient care for any psychiatric diagnosis. “Premature mortality” indicated whether the individual had died before a maximum age of 41 y. “Low educational level” indicated that the highest achieved attainment did not meet secondary school qualifications as defined by the SUN2000 classification system [32], at the baseline of the follow-up (age 26 y). “Welfare recipiency” indicated whether the individual had received means-tested welfare benefits [33].
Covariates
The TPR provided information on sex, birth year (continuous), and birth order (first, second, third, and fourth or higher). Parental lifetime history of psychiatric morbidity and criminality were measured as binary variables, indicating whether either biological parent of the individuals had been diagnosed for any psychiatric disorder or convicted of a criminal offence. We measured parental sociodemographic factors in 1985. If the information was missing, we used the earliest available information up until 2012. “Family income” was defined as the disposable income, which includes both earnings and benefits, averaged across both biological parents. “Low parental education level” measured whether neither biological parent had achieved secondary school qualifications. “Maternal single status” indicated that the mother was not married.
Analytical Approach
We initially generated descriptive statistics to examine how sociodemographic characteristics were distributed across TBI exposure groups with varying degrees of injury severity.
We then estimated the magnitude of the associations between TBI and the functional outcomes of interest by fitting a series of logistic and Cox regression models that accommodated the binary and right-censored outcome distributions. A total of 42,132 individuals had emigrated and 5,494 individuals had died during the follow-up period and were right-censored. Time at risk was, therefore, explicitly accounted for in the Cox regression model. We will henceforth refer to the effect measures (e.g., odds and hazard ratios) as risk ratios. We gradually accounted for a number of measured covariates by fitting two separate models to the full sample (n = 1,143,470). In these analyses, we assumed that all individuals were unrelated to one another. In Model I, we only adjusted for sex, birth year, and birth order. Model II additionally adjusted for individual and parental educational level, parental lifetime history of psychiatric morbidity and criminality, family income, as well as maternal single status. In Model III, we further tested for the contribution of unobserved familial confounders by fitting a sibling-comparison model to the sibling subsample (n = 683,860) using fixed-effects estimators [34] of the statistical models described above, which stratified the estimates across clusters of biological parents.
The rationale for Model III was to compare risks of poor adulthood functioning in differentially exposed full-siblings (i.e., one sibling has sustained a TBI and the other one has not; n = 108,086) and thereby indirectly control for an aggregate of factors that make the siblings similar to one another (e.g., 50% of their co-segregating genes and their shared childhood environments). This implies that Model III indirectly accounted for all of the measured family-wide covariates (e.g., family income and maternal single status) in Model II, as they are constant between siblings. Under these assumptions, Model III isolated the residual effect of the association of interest, which is consistent with a causal inference [25]. The magnitude of familial confounding is measured as the relative attenuation of the within-family estimate compared to the unrelated population estimate [35]. We followed the STROBE guidelines for cohort studies (see S1 STROBE Checklist for details).
Sensitivity analyses
We re-fitted Models I–III to non-TBI fall-related injury to examine whether the findings were specific to TBI or to a general proneness to injury. To examine whether recurrent TBIs was a stronger risk factor than a single-episode TBI, we re-specified Models I–III so that we compared individuals who had sustained recurrent TBIs with those who had sustained a single TBI, rather than those who had not sustained any TBIs. By definition, this implies that Model III examined the relative risk differences between siblings that were differentially exposed to either recurrent TBIs and single TBI. We explored potential moderation effects by age at first TBI by re-fitting Models I–III to the five age category measures. To maximise statistical power in these analyses for premature mortality, we defined the baseline of the follow-up at the end of each exposure period (e.g., at ages 4, 9, 14, 19, and 24 y).
We were asked to conduct the following complementary sensitivity analyses during the peer review process: We tested whether our findings could be explained by any comorbid psychiatric and/or neurological conditions that had occurred at any time throughout the exposure period, up to the age of 25 y, by re-running Models I–III on a subsample that excluded individuals who met such criteria (n = 83,897). To explore time trends, we tested whether the birth year moderated the effects of TBI on the outcomes by adding an interaction term to Model III. We also considered whether the correlated nature of our outcome measures (correlation table presented in S2 Table) could impact on the presented findings by comparing the Model I estimates to equivalent estimates derived from a multivariate structural equation model (SEM), where all of the associations were tested jointly. In the SEM, we specified the right-censored outcome variables to be treated as Poisson distributed counts with offset variables, which allowed us to explicitly take time at risk into account. We also calculated population attributable fractions (PAF), or the relative share of the outcomes that could be attributed to TBI. Similar to the individual-level analyses described above, we gradually accounted for confounding factors using the Models I–III specifications.
We used Stata 14 MP [36] to fit the logistic regression (logit), conditional logistic regression (xtlogit, fe), Cox regression (stcox), stratified Cox regression (stcox, strata()), and multivariate SEM (gsem) models, as well as to estimate PAFs (punafcc) for Models I and II. We used the AF 0.1.1 package [37] in R 3.2.2 [38] to estimate PAFs for Model III.
Results
We identified 104,290 (9.1%) individuals that had sustained a TBI before age 25 y (Table 1). The overwhelming majority of these persons had suffered from mild TBIs (n = 80,676; 77.4%) and one in eight (n = 12,680; 12.2%) had experienced recurrent injuries. People with head injuries were, on average, more likely to be male and to have grown up in households characterised by a range of adverse psychosocial indicators (Table 1). Individuals who had sustained recurrent TBIs were, on average, approximately 2 y younger at their first injury than those who had sustained a single TBI (12.0 versus 13.8 y). Those who had sustained mild TBIs also tended to be younger at the time of their first injury than those who had sustained moderate to severe TBIs (12.2 versus 19.2 y).
Tab. 1. Sociodemographic characteristics for the sample (n = 1,143,470). 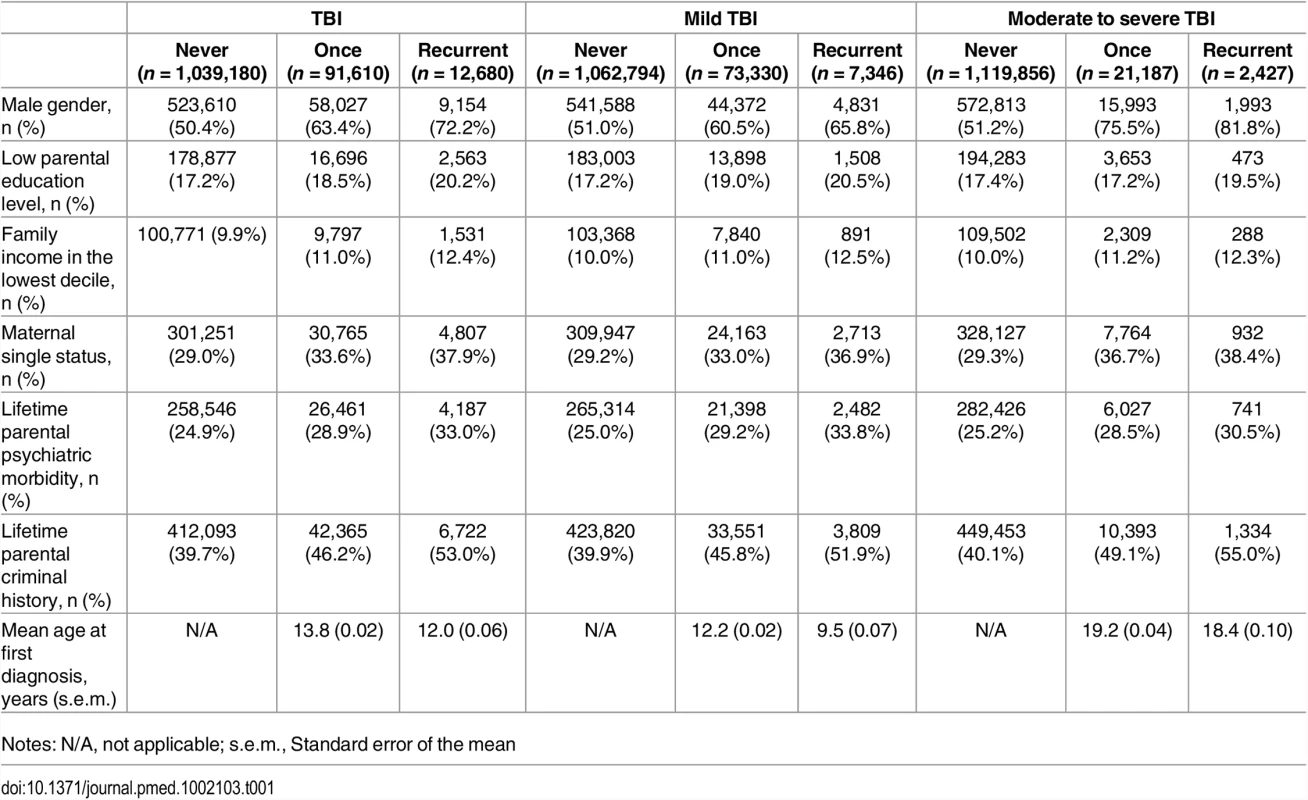
Notes: N/A, not applicable; s.e.m., Standard error of the mean TBI was associated with elevated risk of impaired adult functioning across all outcome measures (Fig 1; Table 1; complete list of absolute risks in S3 Table). Sustaining a TBI contributed to absolute risks of over 10% for specialist diagnoses of psychiatric disorders, low educational attainment, and welfare recipiency, and approximately 6% for disability pension. In terms of relative risks (Table 2), we found that the risk of disability pension increased by 76% (RR = 1.76; 95% CI: 1.71–1.82), which reduced to 49% (RR = 1.49; 1.38–1.60) when the comparison was made with unaffected siblings. The strongest association was found for psychiatric inpatient hospitalisation, for which the risk was doubled (RR = 1.95; 1.90–2.10). When compared to their unaffected siblings, TBI patients continued to be nearly 60% (RR = 1.57; 95% CI: 1.47–1.67) more likely to be hospitalised for any psychiatric disorder. Social functioning impairments were also more common in those who had sustained a TBI, being 60% more likely than unrelated controls (RR = 1.58; 1.55–1.61) and 28% more likely than their unaffected siblings (RR = 1.28; 1.23–1.33) to have attained a low level of education in adulthood. Similar results were observed for receiving welfare benefits. These findings could not be attributed to comorbid psychiatric and/or neurological conditions throughout the exposure period (S4 Table). Multivariate analyses taking the correlation between the outcomes into account were also commensurate with these findings (Table 3). Furthermore, we did not find any statistically significant (p < 0.05) moderation effects by birth year, thus suggesting that the effects of TBI on the outcomes did not change materially over time.
Fig. 1. Kaplan-Meier survival curves for all right-censored outcomes across TBI exposure before age 25 y. 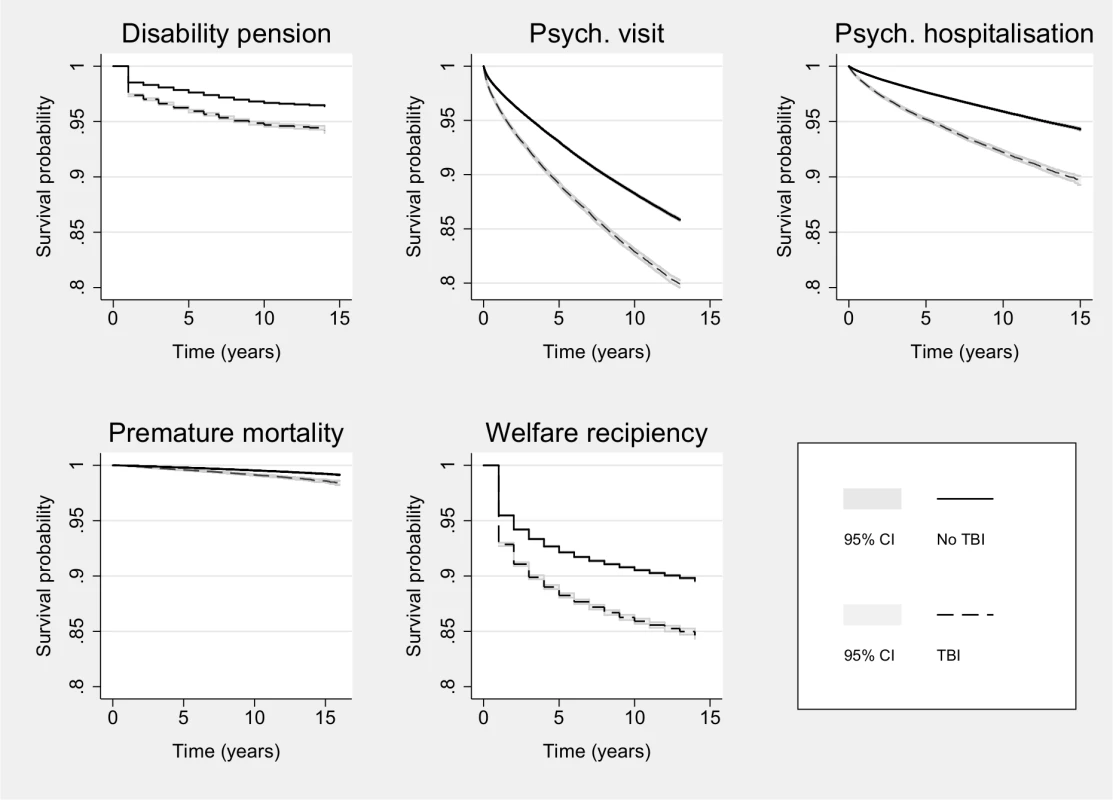
Tab. 2. Relative risks (RR) and corresponding 95% confidence intervals (CIs) for the associations between TBI before age 25 y and poor functioning in adulthood. 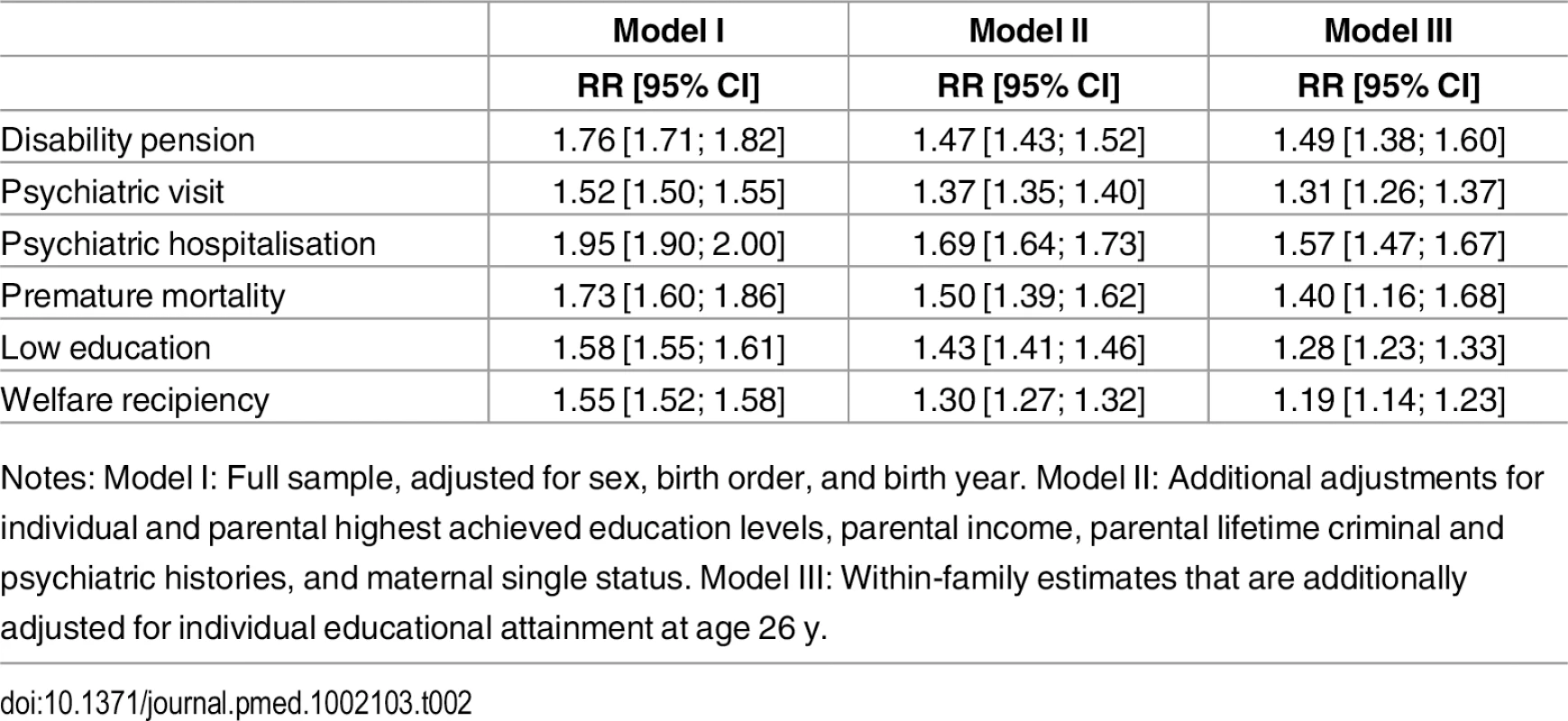
Notes: Model I: Full sample, adjusted for sex, birth order, and birth year. Model II: Additional adjustments for individual and parental highest achieved education levels, parental income, parental lifetime criminal and psychiatric histories, and maternal single status. Model III: Within-family estimates that are additionally adjusted for individual educational attainment at age 26 y. Tab. 3. Relative risks (RR) and corresponding 95% confidence intervals (CIs) for the associations between TBI before age 25 y and poor functioning in adulthood, assessed in univariate and multivariate models. 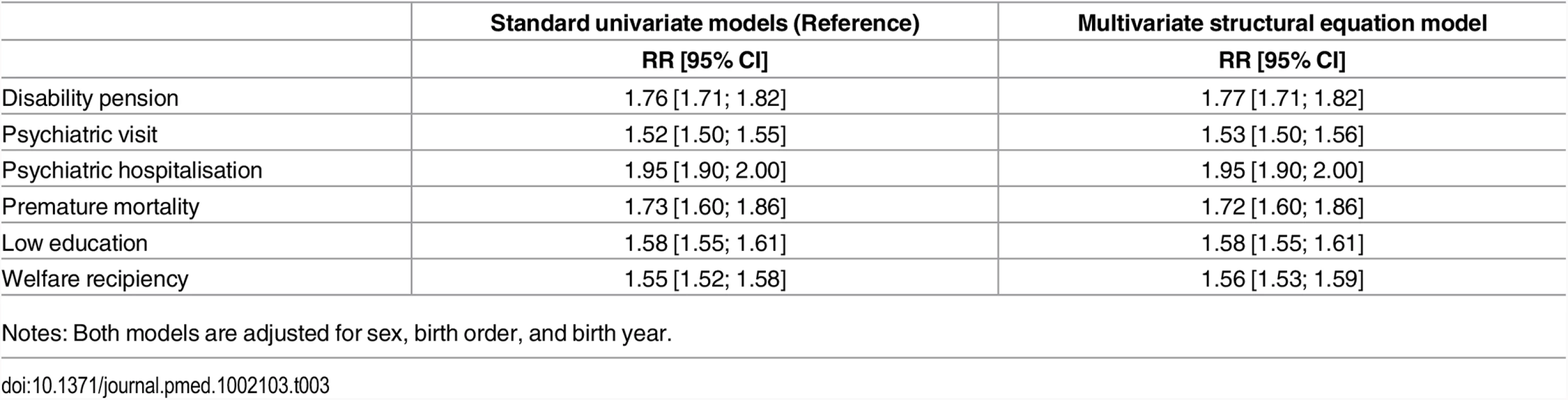
Notes: Both models are adjusted for sex, birth order, and birth year. We found that the crude population contributions of TBI explained approximately 4%–7% of the differences in the outcome measures (Table 4; Model I). These estimates were partially attenuated once familial confounders were accounted for (Model III) but remained statistically significant, explaining between 2%–6% of the population differences in the outcomes. The strongest population attributable risks were found for the severe outcomes, including psychiatric inpatient hospitalisation (PAF = 5.5%; 4.9%–6.1%), premature mortality (PAF = 4.7%; 2.9%–6.5%), and disability pension (PAF = 4.6%; 3.8%–5.3%).
Tab. 4. Population-attributable fractions, expressed as percentages, for TBI before age 25 y on poor functioning in adulthood. 
Notes: Model I: Full sample, adjusted for sex, birth order, and birth year; Model II: Additional adjustments for individual and parental highest achieved education levels, parental income, parental lifetime criminal and psychiatric histories, and maternal single status; Model III: Within-family estimates that are additionally adjusted for individual educational attainment at age 26 y. Individuals that had sustained non-TBI fall injuries were generally less likely than those who had sustained a TBI to have poor adulthood outcomes (Table 5). The differences were most noticeable for severe outcomes, such as disability pension, for which the risk increase for non-TBI patients compared to their unaffected siblings (RR = 1.01; 0.91–1.12) was less than the equivalent risk estimate for TBI patients (RR = 1.49; 1.38–1.60). We also found similar results for premature mortality.
Tab. 5. Relative risks (RR) and corresponding 95% confidence intervals (CIs) for the associations between non-TBI fall injuries, mild TBI and moderate to severe TBI up to age 25 y on adulthood poor functioning. 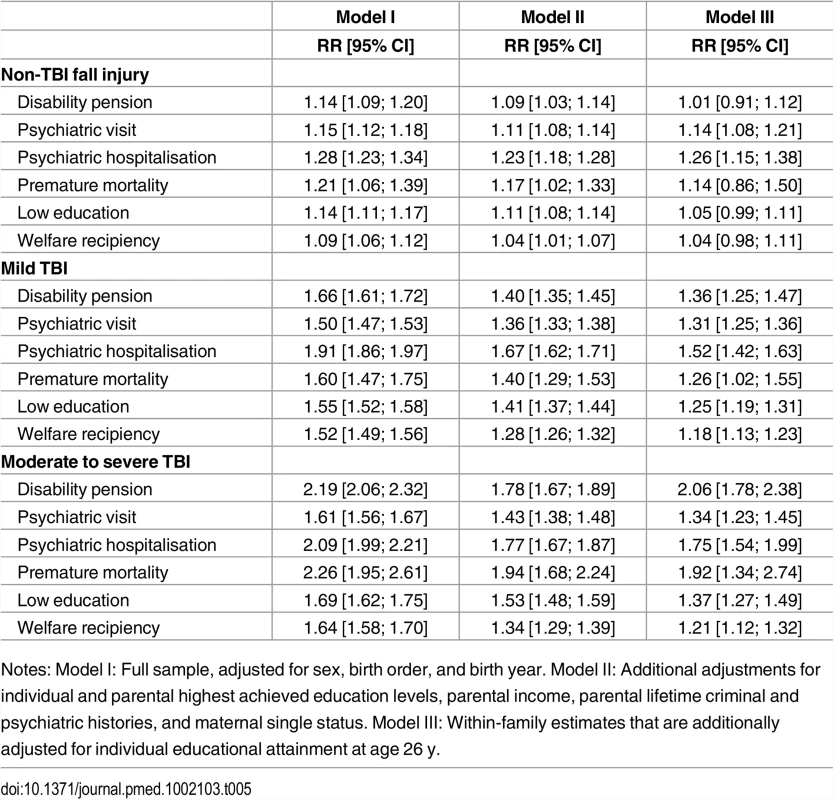
Notes: Model I: Full sample, adjusted for sex, birth order, and birth year. Model II: Additional adjustments for individual and parental highest achieved education levels, parental income, parental lifetime criminal and psychiatric histories, and maternal single status. Model III: Within-family estimates that are additionally adjusted for individual educational attainment at age 26 y. Stratifying the TBI exposure across injury severity (Table 5), we found that the estimates of mild TBI exposure were only slightly attenuated compared to the TBI estimates. Importantly, we observed that moderate-to-severe TBI was a stronger risk factor for all functioning outcomes. This was particularly evident in the case of premature mortality, for which moderate-to-severe TBI patients had an approximately 2-fold increase in risk compared to both unrelated controls (RR = 2.26; 1.95–2.61) and their unaffected siblings (RR = 1.92; 1.34–2.74). We found similar results for disability pension and psychiatric inpatient hospitalisation.
The risks of poor functioning in adulthood were substantially elevated across all outcomes in individuals who had suffered recurrent TBIs compared to those who had suffered a single TBI (Table 6). Recurrent TBI was, for instance, associated with a nearly 3-fold increase in risk of being in receipt of disability pension (RR = 2.58; 2.41–2.76) compared to unrelated controls that had sustained a single TBI and a 2-fold increase in risk compared to their siblings that had sustained a single TBI (RR = 2.22; 1.88–2.63). Similarly, we observed that the risks of psychiatric inpatient hospitalisation (RR = 1.84; 1.73–1.95) and premature mortality (RR = 2.11; 1.78–2.49) were doubled in individuals with recurrent injuries compared to those who had suffered a single TBI. These increases in risk persisted in the sibling-comparison models for both psychiatric inpatient hospitalisation (RR = 1.53; 1.31–1.79) and premature mortality (RR = 1.59; 1.02–2.49). Further stratification of the recurrence effects across injury severity revealed that individuals who had sustained multiple moderate to severe TBIs had a 6-fold increase in risk of being in receipt of disability pension (RR = 5.84; 5.17–6.60) when compared to population controls who were exposed to a single moderate-to-severe TBI, which persisted when further compared with their siblings who were similarly exposed to a single moderate-to-severe TBI (RR = 6.13; 4.18–8.99).
Tab. 6. Relative risks (RR) and corresponding 95% confidence intervals (CIs) for the associations between recurrent TBI compared to single-episode TBI, across injury severity, before age 25 y and poor functioning in adulthood. 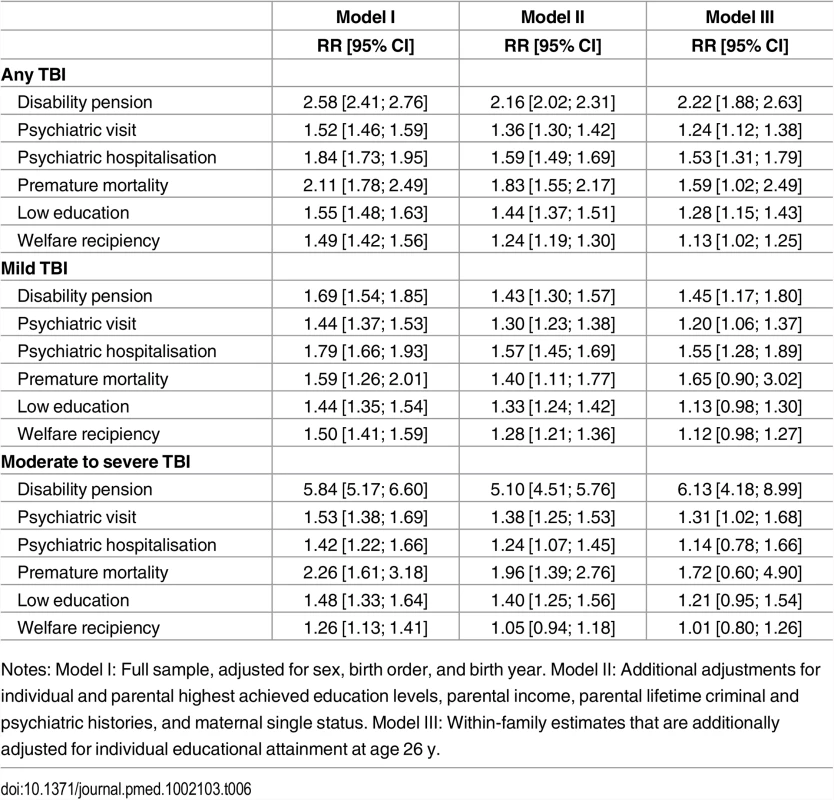
Notes: Model I: Full sample, adjusted for sex, birth order, and birth year. Model II: Additional adjustments for individual and parental highest achieved education levels, parental income, parental lifetime criminal and psychiatric histories, and maternal single status. Model III: Within-family estimates that are additionally adjusted for individual educational attainment at age 26 y. The age at first TBI was a very strong moderator of poor functioning in adulthood (Table 7; Model III findings in S5 Table). We observed a positive association between older age at first TBI and all outcomes, and in particular among those who sustained their first injury after the age of 15 y. The largest observed differences were found for psychiatric inpatient hospitalisation, for which the first TBI exposure between ages 0–4 y was associated with a 1.2 fold (RR = 1.24; 1.15–1.34) increased risk, while the equivalent estimate for ages 20–24 y was a 2.5-fold risk increase (RR = 2.47; 2.37–2.58). In complementary sensitivity analyses, we replicated these findings for mild TBI (S6 Table), which suggests that these findings could not be attributed to increased injury severity among those who sustained their first injury at an older age.
Tab. 7. Relative risks (RR) and corresponding 95% confidence intervals (CIs) for the associations between TBI and poor functioning in adulthood, across age-band at first injury. 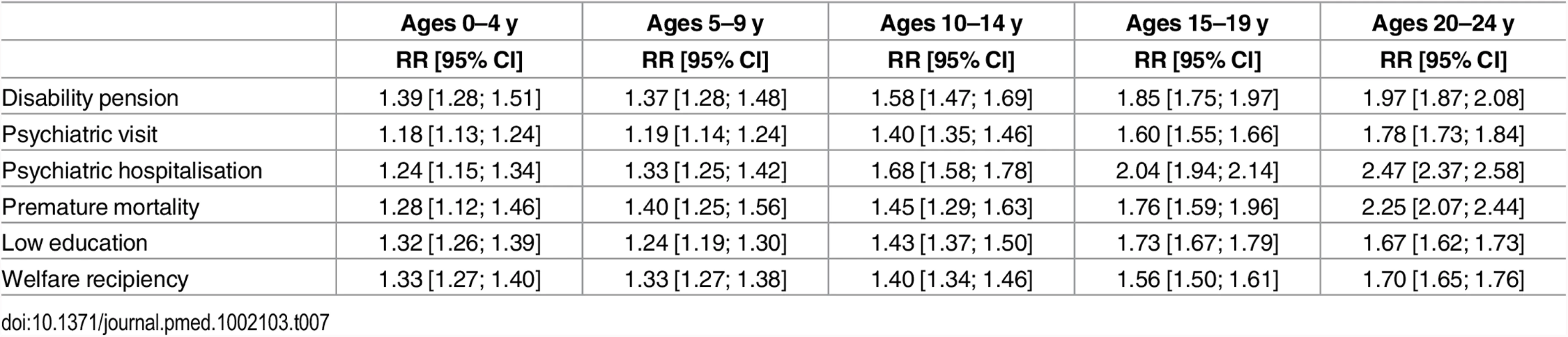
Discussion
In this population-based register study of over 1.1 million Swedish children, we examined the associations between TBI exposure, identified from inpatient and outpatient episodes, from birth up to age 25, and a range of adverse adult medical and social outcomes with public health implications. We followed the sample for up to 41 y, examined 683,860 siblings in addition to population controls, and the investigation was sufficiently powered to reliably explore the moderating effects of age categories at first injury. There were five principal findings. First, we found that being exposed to a mild TBI was associated with a range of adverse outcomes, including disability pension, psychiatric visits and inpatient hospitalisation, premature mortality, low educational attainment, and welfare recipiency. To provide more accurate estimates, we used unaffected siblings as comparisons, which demonstrated that although there was some familial confounding (shared genetic and childhood family environmental risks), we found that mild TBI was associated with 18%–52% increased risk of these outcomes. In particular, the risks were highest for psychiatric inpatient hospitalisation and disability pension.
Second, we found that greater injury severity was associated with poorer functioning outcomes. Compared to mild TBI, exposure to moderate-to-severe TBI increased the risk of disability pension by 106% and of psychiatric inpatient hospitalisation by 92% when compared to their unaffected siblings. Importantly, we observed smaller differences between the population and sibling-comparison estimates (Model I and III) in the case of moderate-to-severe TBI compared to mild TBI, which provides additional evidence for a potentially causal effect of more severe TBI on adverse outcomes.
The third main finding was that recurrent TBIs led to poorer outcomes than a single TBI. This was most noticeable for the likelihood of receiving disability pension, for which the risk increase between differentially exposed siblings was around 2-fold for recurrent TBIs compared to a single TBI. One in eleven (n = 1,139; 9.0%) individuals who sustained recurrent TBIs went on to receive a disability pension, which is 759 individuals more than we would have expected. This risk increase is associated with a substantial economic impact. The per person average cost of productivity loss for a single day of work absence in Sweden is estimated to be US$190 [39]. If we assume that these 759 individuals are absent from the labour market for a period of 30 y, this would roughly translate to a cumulative cost of US$1.3 million per person or US$987 million in total for productivity losses alone over the same time period. Generalising this to the US setting, with an annual 848,000 TBI patients under the age of 25 y [2], we would expect 34,600 of these individuals to be at risk for permanent labour market exclusion, equating to approximately US$1.1 trillion.
Fourth, we found that TBI accounted for between 2%–6% of the differences in the adverse outcomes following adjustments for familial confounders shared by differentially exposed siblings. These estimates are not insignificant. By way of comparison, the population attributable risk of severe mental illnesses on violent criminal convictions in Sweden has been estimated at 5% [40]. Importantly, as the examples presented above demonstrate, successful prevention efforts targeting high-risk individuals may have a notable impact on health care and other costs.
Fifth, we found that age at first head injury moderated the effects on long-term outcome. There was an age-related association in which older age at first head injury, and particularly after the age of 15 y, substantially increased the risks of all examined outcomes. In the case of premature mortality, we further minimised the risks of survival bias by initiating the follow-up period at the end of each exposure period. This approach thus allowed us to include individuals who had died before age 26. Although in need of replication, our findings are perhaps consistent with the hypothesis that neuroplasticity in early life may have long-term protective effects. These effects were most noticeable in relation to psychiatric hospitalisation for which the risk was substantially less among those who had sustained their first TBI between ages 0–4 y (RR = 1.24; 1.15–1.34) compared to those who had sustained their first injury between ages 20–24 y (RR = 2.47; 2.37–2.58). The neuroplasticity literature is currently mixed and inconclusive, largely due to similar methodological limitations as those outlined above [41–43]. Our robust findings, however, cannot be explained by differential injury levels, injury proneness across the examined age groups, survival bias, or familial selection factors. Importantly, our findings suggest that current clinical guidelines [3] should be revised to explicitly offer age-sensitive recommendations for follow-up interventions in childhood, adolescence, and early adulthood.
Two main findings—that TBI was associated with subsequent adverse adulthood outcomes, and the dose-response relationship with injury severity—are consistent with previous research [17–20,44], although these studies have mostly focused on small and selected samples that rely extensively on self-reported data either from (severely) injured patients or their caregivers; an approach subject to substantial bias [45]. Similar results have been reported in studies examining global disability indices [10], such as the extended Glasgow Outcome Scale (GOSE) [21]. Our third finding, on the effects of recurrent injuries, is broadly consistent with the emerging literature on the adverse consequences of sports and combat-related neurotrauma [7,9,11–14,46–49]. Although replication of this research is needed with larger samples of athletes and using research designs, such as comparisons with sibling controls, that account for confounding factors, our findings suggest that recurrent neurotrauma in any setting may be a causal risk factor for a wide range of social, cognitive, and medical adverse outcomes.
One of the implications of these findings is the importance of developing preventive interventions for early exposure to head injuries. In toddlers and preschoolers, these interventions should ideally be targeting improved parental supervision, as falling is the most common cause of TBI in this group. Prevention of sports-related concussions in older children could focus on changes to rules so that the risks of players colliding their heads with each other and with equipment (e.g., heading soccer balls or getting hit in the head by a racket, bat, or stick) [50] is reduced. A recent systematic review indicated that helmet use in most sports is generally associated with reduced risks for severe head injuries but not for concussions/mild TBI [51]. The development of safer helmets should also be prioritised as, for instance, recent evaluations of American football helmets report performance differences [52]. A further implication of the current study is that individuals who have suffered serious injuries should receive close follow-up interventions beyond medical care. This holds especially true if the injuries are recurrent or have occurred for the first time after the age of 20 y. The involvement of social services and work training opportunities may mitigate a potential downward social drift.
Our study has significant strengths that include (1) a very large sample size, enabling precise measures of associations between early TBI exposure and objectively defined indicators of medical and social functioning during adulthood to be defined; (2) the high quality of registers allowed selection bias to a minimum, as we were able to retain 86% of the targeted sample across 41 y of follow-up; and (3) the family-based research design allowed us to robustly test for the aggregated effects of all pre-injury and other selection characteristics shared within the family. Two limitations should be noted: We will have underestimated the prevalence of mild TBI. We used the National Patient Register, as adopted by previous studies [8,15,16], to ascertain TBI cases. This allowed comprehensive information on all individuals who sought medical treatment for their injuries, but will have underestimated milder forms of TBI, for example of the type prevalent in sports-related injuries [53–56]. This will not likely affect our main conclusions, as misclassifying head injured individuals as unaffected will have led to an underestimation of the presented associations, assuming that the effects of diagnosed and undiagnosed TBI on the outcomes are similar in magnitude. A co-twin design might better account for residual genetic confounds, but we were underpowered to do so, as it would require monozygotic twins that are discordant on head injuries, which would lead to considerably wider confidence intervals than traditional approaches [25].
The generalisability of our findings is an important consideration, and there is evidence that Sweden is similar to other high-income countries in terms of the key exposures and outcomes in this study. A recent systematic review [57] of annual TBI incidence rates for individuals up to age 20 y identified three studies from the US and New Zealand with a median estimate of 973 [range: 790–1,652] injuries per 100,000 population. We calculated equivalent estimates for Sweden between 2001 and 2009 and observed a median of 1,220 (range: 931–1,262) injuries per 100,000 population. Sweden’s employment rate (74.2%) was comparable to that of the United Kingdom (70.5%) and the US (67.3%) in 2013 [58]. The estimated life expectancy in Sweden is similar to that of other Organisation for Economic Co-operation and Development (OECD) countries [59], and a systematic review of the rates of mental disorders in Western European countries found no material country differences [60].
Children and adolescents who are exposed to TBI, even if the injuries appear to be relatively minor, have elevated risks to develop a wide range of medical and social problems during adulthood. The risks are substantially elevated as a function of injury severity, recurrence, and time of injury. These observations have potentially important implications for the way that paediatric TBI is currently clinically managed. Currently most children with significant head injuries receive no systematic long-term follow-up. An implication of our findings is that this should change. Services should consider how to routinely and systematically review these children on a regular basis to allow the subtle but important neurological, cognitive, and psychiatric consequences of TBI to be identified. Routinely tracking the progress of patients following significant TBI allows those with an altered developmental and educational trajectory to be identified and appropriate, age-sensitive interventions to be initiated. Detailed clinical studies on representative paediatric populations are needed to extend recent advances in the understanding of adult TBI pathophysiology, as this will inform the nature of key drivers for poor long-term outcome [61,62]. Effective prevention that minimises the risks of early exposure to TBI is required, and such efforts should benefit from large-scale epidemiological studies that identify potentially causal risk factors for the severity, recurrence, and developmental timing of TBI.
Supporting Information
Zdroje
1. World Health Organization. Neurological disorders: Public health challenges. Geneva, Switzerland 2006.
2. Faul M, Xu L, Wald M, Coronado VG. Traumatic brain injury in the United States: emergency department visits, hospitalizations and deaths 2002–2006. Atlanta, GA: Centers for Disease Control and Prevention, National Center for Injury Prevention and Control. 2010 : 2–70.
3. National Institute for Health and Care Excellence (NICE). Head injury: Triage, assessment, and early management of head injury in children, young people and adults. NICE clinical guideline 176. 2014.
4. Styrke J, Stålnacke B-M, Sojka P, Björnstig U. Traumatic brain injuries in a well-defined population: epidemiological aspects and severity. J Neurotrauma. 2007;24(9):1425–36. 17892405
5. McKinlay A, Grace R, Horwood L, Fergusson D, Ridder EM, MacFarlane M. Prevalence of traumatic brain injury among children, adolescents and young adults: prospective evidence from a birth cohort. Brain inj. 2008;22(2):175–81. doi: 10.1080/02699050801888824 18240046
6. Feigin VL, Theadom A, Barker-Collo S, Starkey NJ, McPherson K, Kahan M, et al. Incidence of traumatic brain injury in New Zealand: a population-based study. Lancet Neurol. 2013;12(1):53–64. doi: 10.1016/S1474-4422(12)70262-4 23177532
7. Guskiewicz KM, Marshall SW, Bailes J, McCrea M, Cantu RC, Randolph C, et al. Association between recurrent concussion and late-life cognitive impairment in retired professional football players. Neurosurgery. 2005;57(4):719–26. 16239884
8. Fazel S, Lichtenstein P, Grann M, Långström N. Risk of violent crime in individuals with epilepsy and traumatic brain injury: a 35-year Swedish population study. PLoS Med. 2011;8(12):e1001150. doi: 10.1371/journal.pmed.1001150 22215988
9. Daneshvar DH, Nowinski CJ, McKee AC, Cantu RC. The epidemiology of sport-related concussion. Clin Sports Med. 2011;30(1):1–17. doi: 10.1016/j.csm.2010.08.006 21074078
10. McMillan TM, Teasdale GM, Stewart E. Disability in young people and adults after head injury: 12–14 year follow-up of a prospective cohort. J Neurol Neurosurg Psychiatry. 2012;83(11):1086–91. doi: 10.1136/jnnp-2012-302746 22645256
11. McKee AC, Stein TD, Nowinski CJ, Stern RA, Daneshvar DH, Alvarez VE, et al. The spectrum of disease in chronic traumatic encephalopathy. Brain. Epub 2012 Dec 2. doi: 10.1093/brain/aws307
12. Kerr ZY, Marshall SW, Harding HP, Guskiewicz KM. Nine-year risk of depression diagnosis increases with increasing self-reported concussions in retired professional football players. Am J Sports Med. 2012;40(10):2206–12. 22922518
13. McKee AC, Robinson ME. Military-related traumatic brain injury and neurodegeneration. Alzheimers Dement. 2014;10(3):S242–S53. doi: 10.1016/j.jalz.2014.04.003 24924675
14. Pearce AJ, Hoy K, Rogers MA, Corp DT, Davies CB, Maller JJ, et al. Acute motor, neurocognitive and neurophysiological change following concussion injury in Australian amateur football. A prospective multimodal investigation. Journal of Science and Medicine in Sport. Epub 2014 Jul 24. doi: 10.1016/j.jsams.2014.07.010
15. Orlovska S, Pedersen MS, Benros ME, Mortensen PB, Agerbo E, Nordentoft M. Head injury as risk factor for psychiatric disorders: A nationwide register-based follow-up study of 113,906 persons with head injury. Am J Psychiat. 2014;171(4):463–9. doi: 10.1176/appi.ajp.2013.13020190 24322397
16. Fazel S, Wolf A, Pillas D, Lichtenstein P, Långström N. Suicide, fatal injuries, and other causes of premature mortality in patients with traumatic brain injury: A 41-year Swedish population study. JAMA Psychiatry. 2014;71(3):326–33. doi: 10.1001/jamapsychiatry.2013.3935 24430827
17. Ewing-Cobbs L, Prasad MR, Mendez D, Barnes MA, Swank P. Social interaction in young children with inflicted and accidental traumatic brain injury: relations with family resources and social outcomes. J Int Neuropsychol Soc. 2013;19(05):497–507.
18. Ryan NP, Anderson V, Godfrey C, Beauchamp MH, Coleman L, Eren S, et al. Predictors of very-long-term sociocognitive function after pediatric traumatic brain injury: evidence for the vulnerability of the immature “social brain”. J Neurotrauma. 2014;31(7):649–57. doi: 10.1089/neu.2013.3153 24147615
19. Anderson V, Brown S, Newitt H, Hoile H. Educational, Vocational, Psychosocial, and Quality‐of‐Life Outcomes for Adult Survivors of Childhood Traumatic Brain Injury. J Head Trauma Rehabil. 2009;24(5):303–12. doi: 10.1097/HTR.0b013e3181ada830 19858964
20. Anderson V, Brown S, Newitt H, Hoile H. Long-term outcome from childhood traumatic brain injury: intellectual ability, personality, and quality of life. Neuropsychology. 2011;25(2):176. doi: 10.1037/a0021217 21219074
21. Wilson JL, Pettigrew LE, Teasdale GM. Structured interviews for the Glasgow Outcome Scale and the extended Glasgow Outcome Scale: guidelines for their use. J Neurotrauma. 1998;15(8):573–85. 9726257
22. Gary KW, Wilson KB. Traumatic brain injury: Short, long, and very long-term vocational outcomes. Brain injury: Functional aspects, rehabilitation and prevention. Rejecka, Croatia: InTech; 2012. p. 175–98.
23. Lenroot RK, Giedd JN. Brain development in children and adolescents: insights from anatomical magnetic resonance imaging. Neurosci Biobehav Rev. 2006;30(6):718–29. 16887188
24. Paus T, Keshavan M, Giedd JN. Why do many psychiatric disorders emerge during adolescence? Nat Rev Neurosci. 2008;9(12):947–57. doi: 10.1038/nrn2513 19002191
25. D’Onofrio BM, Lahey BB, Turkheimer E, Lichtenstein P. Critical need for family-based, quasi-experimental designs in integrating genetic and social science research. Am J Public Health. 2013;103(S1):S46–S55.
26. Narusyte J, Ropponen A, Silventoinen K, Alexanderson K, Kaprio J, Samuelsson A, et al. Genetic liability to disability pension in women and men: a prospective population-based twin study. PLoS ONE. 2011;6(8):e23143. doi: 10.1371/journal.pone.0023143 21850258
27. Plomin R, Deary I. Genetics and intelligence differences: five special findings. Mol Psychiatry. 2014;20 : 98–108. doi: 10.1038/mp.2014.105 25224258
28. Polderman TJ, Benyamin B, de Leeuw CA, Sullivan PF, van Bochoven A, Visscher PM, et al. Meta-analysis of the heritability of human traits based on fifty years of twin studies. Nat Genet. 2015;47 : 702–9. doi: 10.1038/ng.3285 25985137
29. Nilsson AC, Spetz CL, Carsjo K, Nightingale R, Smedby B. Reliability of the hospital registry. The diagnostic data are better than their reputation. Lakartidningen. 1994;91 : 603–5.
30. Gedeborg R, Engquist H, Berglund L, Michaëlsson K. Identification of incident injuries in hospital discharge registers. Epidemiology. 2008 : 860–7. 18938655
31. Narusyte J, Ropponen A, Alexanderson K, Svedberg P. The role of familial factors in the associations between sickness absence and disability pension or mortality. Eur J Public Health. 2014;24(1):106–10. doi: 10.1093/eurpub/ckt039 23531525
32. Halldén K. The Swedish educational system and classifying education using the Isced-97. In: Schneider SL, editor. The International Standard Classification of Education (Isced-97): An evaluation of content and criterion validity in 15 European countries. Mannheim: MZES; 2008.
33. Sariaslan A, Larsson H, D'Onofrio BM, Långström N, Lichtenstein P. Childhood family income, adolescent violent criminality and substance misuse: quasi-experimental total population study. Br J Psychiatry. 2014;205 : 286–90. doi: 10.1192/bjp.bp.113.136200 25147371
34. Allison PD. Fixed effects regression models. Sage, Thousand Oaks; 2009.
35. Carlin JB, Gurrin LC, Sterne JA, Morley R, Dwyer T. Regression models for twin studies: a critical review. Int J Epidemiol. 2005;34(5):1089–99. 16087687
36. StataCorp. Stata Statistical Software: Release 14. College Station: StataCorp LP; 2015.
37. Dahlqwist E, Sjölander A. Model-based estimation of confounder-adjusted attributable fractions. R package AF 0.1.1. 2015. https://cran.r-project.org/web/packages/AF/index.html.
38. R Core Team. R: A Language and environment for statistical computing. Vienna, Austria: R Foundation for Statistical Computing; 2015.
39. von Knorring L, Åkerblad A-C, Bengtsson F, Carlsson Å, Ekselius L. Cost of depression: effect of adherence and treatment response. Eur Psychiatry. 2006;21(6):349–54. 16777385
40. Fazel S, Grann M. The population impact of severe mental illness on violent crime. Am J Psychiat. 2006;163(8):1397–403. 16877653
41. Anderson V, Godfrey C, Rosenfeld JV, Catroppa C. Predictors of cognitive function and recovery 10 years after traumatic brain injury in young children. Pediatrics. 2012;129(2):e254–e61. doi: 10.1542/peds.2011-0311 22271691
42. Crowe LM, Catroppa C, Babl FE, Anderson V. Intellectual, behavioral, and social outcomes of accidental traumatic brain injury in early childhood. Pediatrics. 2012;129(2):e262–e8. doi: 10.1542/peds.2011-0438 22271692
43. Nudo RJ. Recovery after brain injury: mechanisms and principles. Front Hum Neurosci. 2013;7.
44. Cancelliere C, Kristman VL, Cassidy JD, Hincapié CA, Côté P, Boyle E, et al. Systematic review of return to work after mild traumatic brain injury: results of the International Collaboration on Mild Traumatic Brain Injury Prognosis. Arch Phys Med Rehabil. 2014;95(3):S201–S9. doi: 10.1016/j.apmr.2013.10.010 24581906
45. Griffen J, Hanks R. Cognitive and behavioral outcomes from traumatic brain injury. Handbook on the neuropsychology of traumatic brain injury: Springer; 2014. p. 25–45.
46. Guskiewicz KM, Valovich McLeod TC. Pediatric sports-related concussion. PM&R. 2011;3(4):353–64.
47. Pearce AJ, Hoy K, Rogers MA, Corp DT, Maller JJ, Drury HG, et al. The long-term effects of sports concussion on retired Australian football players: A study using Transcranial Magnetic Stimulation. J Neurotrauma. 2014;31(13):1139–45. doi: 10.1089/neu.2013.3219 24579780
48. Spira JL, Lathan CE, Bleiberg J, Tsao JW. The impact of multiple concussions on emotional distress, post-concussive symptoms, and neurocognitive functioning in active duty United States marines independent of combat exposure or emotional distress. J Neurotrauma. 2014;31(22):1823–34. doi: 10.1089/neu.2014.3363 25003552
49. Guskiewicz K, Teel E, McCrea M. Concussion: key stakeholders and multidisciplinary participation in making sports safe. Neurosurgery. 2014;75:S113–S8. doi: 10.1227/NEU.0000000000000494 25232875
50. Marshall SW, Guskiewicz KM, Shankar V, McCrea M, Cantu RC. Epidemiology of sports-related concussion in seven US high school and collegiate sports. Inj Epidemiol. 2015;2(1):13.
51. Benson BW, McIntosh AS, Maddocks D, Herring SA, Raftery M, Dvořák J. What are the most effective risk-reduction strategies in sport concussion? Br J Sports Med. 2013;47(5):321–6. doi: 10.1136/bjsports-2013-092216 23479492
52. Rowson S, Duma SM, Greenwald RM, Beckwith JG, Chu JJ, Guskiewicz KM, et al. Can helmet design reduce the risk of concussion in football? Technical note. J Neurosurg. 2014;120(4):919–22. doi: 10.3171/2014.1.JNS13916 24484225
53. McCrea M, Hammeke T, Olsen G, Leo P, Guskiewicz K. Unreported concussion in high school football players: implications for prevention. Clin J Sport Med. 2004;14(1):13–7. 14712161
54. Halstead ME, Walter KD. Sport-related concussion in children and adolescents. Pediatrics. 2010;126(3):597–615. doi: 10.1542/peds.2010-2005 20805152
55. Williamson I, Goodman D. Converging evidence for the under-reporting of concussions in youth ice hockey. Br J Sports Med. 2006;40(2):128–32. 16431999
56. Llewellyn T, Burdette GT, Joyner AB, Buckley TA. Concussion reporting rates at the conclusion of an intercollegiate athletic career. Clin J Sport Med. 2014;24(1):76–9. doi: 10.1097/01.jsm.0000432853.77520.3d 24157468
57. Thurman DJ. The epidemiology of traumatic brain injury in children and youths: A review of research since 1990 [Epub ahead of print 14 Aug 2014]. J Child Neurol.
58. OECD. Society at a glance 2014. OECD Social Indicators. OECD Publishing, 2014.
59. OECD. Health at a glance 2010. OECD Publishing, 2010.
60. Wittchen H-U, Jacobi F, Rehm J, Gustavsson A, Svensson M, Jönsson B, et al. The size and burden of mental disorders and other disorders of the brain in Europe 2010. Eur Neuropsychopharmacol. 2011;21(9):655–79. doi: 10.1016/j.euroneuro.2011.07.018 21896369
61. Ramlackhansingh AF, Brooks DJ, Greenwood RJ, Bose SK, Turkheimer FE, Kinnunen KM, et al. Inflammation after trauma: microglial activation and traumatic brain injury. Ann Neurol. 2011;70(3):374–83. doi: 10.1002/ana.22455 21710619
62. Sharp DJ, Scott G, Leech R. Network dysfunction after traumatic brain injury. Nat Rev Neurol. 2014;10(3):156–66. doi: 10.1038/nrneurol.2014.15 24514870
Štítky
Interní lékařství
Článek vyšel v časopisePLOS Medicine
Nejčtenější tento týden
2016 Číslo 8- Berberin: přírodní hypolipidemikum se slibnými výsledky
- Příznivý vliv Armolipidu Plus na hladinu cholesterolu a zánětlivé parametry u pacientů s chronickým subklinickým zánětem
- Léčba bolesti u seniorů
- Jak postupovat při výběru betablokátoru − doporučení z kardiologické praxe
- Červená fermentovaná rýže účinně snižuje hladinu LDL cholesterolu jako vhodná alternativa ke statinové terapii
-
Všechny články tohoto čísla
- Dementia across the Lifespan and around the Globe—Pathophysiology, Prevention, Treatment, and Societal Impact: A Call for Papers
- Progress and Challenges in Scaling Up Laboratory Monitoring of HIV Treatment
- Facility-Based Delivery during the Ebola Virus Disease Epidemic in Rural Liberia: Analysis from a Cross-Sectional, Population-Based Household Survey
- Availability and Use of HIV Monitoring and Early Infant Diagnosis Technologies in WHO Member States in 2011–2013: Analysis of Annual Surveys at the Facility Level
- Duration of Adulthood Overweight, Obesity, and Cancer Risk in the Women’s Health Initiative: A Longitudinal Study from the United States
- Improving Clinical Risk Stratification at Diagnosis in Primary Prostate Cancer: A Prognostic Modelling Study
- Genetically Predicted Body Mass Index and Breast Cancer Risk: Mendelian Randomization Analyses of Data from 145,000 Women of European Descent
- Social Dancing and Incidence of Falls in Older Adults: A Cluster Randomised Controlled Trial
- Genetic and Environmental Risk for Chronic Pain and the Contribution of Risk Variants for Major Depressive Disorder: A Family-Based Mixed-Model Analysis
- Long-Term Outcomes Associated with Traumatic Brain Injury in Childhood and Adolescence: A Nationwide Swedish Cohort Study of a Wide Range of Medical and Social Outcomes
- On Risk Estimation versus Risk Stratification in Early Prostate Cancer
- Make Data Sharing Routine to Prepare for Public Health Emergencies
- Assessment of Adverse Events in Protocols, Clinical Study Reports, and Published Papers of Trials of Orlistat: A Document Analysis
- Concussions and Repercussions
- South Asia as a Reservoir for the Global Spread of Ciprofloxacin-Resistant : A Cross-Sectional Study
- Building from the HIV Response toward Universal Health Coverage
- Transitioning to Country Ownership of HIV Programs in Rwanda
- Accelerating the Uptake and Timing of Antiretroviral Therapy Initiation in Sub-Saharan Africa: An Operations Research Agenda
- Glycemic Control and the Risk of Tuberculosis: A Cohort Study
- Adjuvant Trastuzumab in HER2-Positive Early Breast Cancer by Age and Hormone Receptor Status: A Cost-Utility Analysis
- Uptake of Home-Based HIV Testing, Linkage to Care, and Community Attitudes about ART in Rural KwaZulu-Natal, South Africa: Descriptive Results from the First Phase of the ANRS 12249 TasP Cluster-Randomised Trial
- An Audit and Feedback Intervention for Reducing Antibiotic Prescribing in General Dental Practice: The RAPiD Cluster Randomised Controlled Trial
- Multidrug-Resistant Tuberculosis Treatment in North Korea: Is Scale-Up Possible?
- Associations between Mental Health and Ebola-Related Health Behaviors: A Regionally Representative Cross-sectional Survey in Post-conflict Sierra Leone
- Pancreatic Cancer Surgical Resection Margins: Molecular Assessment by Mass Spectrometry Imaging
- Integrated Delivery of Antiretroviral Treatment and Pre-exposure Prophylaxis to HIV-1–Serodiscordant Couples: A Prospective Implementation Study in Kenya and Uganda
- Measuring Burden of Unhealthy Behaviours Using a Multivariable Predictive Approach: Life Expectancy Lost in Canada Attributable to Smoking, Alcohol, Physical Inactivity, and Diet
- Comparison of Outcomes before and after Ohio's Law Mandating Use of the FDA-Approved Protocol for Medication Abortion: A Retrospective Cohort Study
- Core Outcomes for Colorectal Cancer Surgery: A Consensus Study
- Adverse Renal, Endocrine, Hepatic, and Metabolic Events during Maintenance Mood Stabilizer Treatment for Bipolar Disorder: A Population-Based Cohort Study
- PLOS Medicine
- Archiv čísel
- Aktuální číslo
- Informace o časopisu
Nejčtenější v tomto čísle- Glycemic Control and the Risk of Tuberculosis: A Cohort Study
- Transitioning to Country Ownership of HIV Programs in Rwanda
- Dementia across the Lifespan and around the Globe—Pathophysiology, Prevention, Treatment, and Societal Impact: A Call for Papers
- Social Dancing and Incidence of Falls in Older Adults: A Cluster Randomised Controlled Trial
Kurzy
Zvyšte si kvalifikaci online z pohodlí domova
Současné možnosti léčby obezity
nový kurzAutoři: MUDr. Martin Hrubý
Všechny kurzyPřihlášení#ADS_BOTTOM_SCRIPTS#Zapomenuté hesloZadejte e-mailovou adresu, se kterou jste vytvářel(a) účet, budou Vám na ni zaslány informace k nastavení nového hesla.
- Vzdělávání



