-
Články
Top novinky
Reklama- Vzdělávání
- Časopisy
Top články
Nové číslo
- Témata
Top novinky
Reklama- Videa
- Podcasty
Nové podcasty
Reklama- Kariéra
Doporučené pozice
Reklama- Praxe
Top novinky
ReklamaAssociations between Mental Health and Ebola-Related Health Behaviors: A Regionally Representative Cross-sectional Survey in Post-conflict Sierra Leone
Theresa Betancourt and colleagues examine the associations between mental health and Ebola-related health behaviors in post-conflict Sierra Leone.
Published in the journal: . PLoS Med 13(8): e32767. doi:10.1371/journal.pmed.1002073
Category: Research Article
doi: https://doi.org/10.1371/journal.pmed.1002073Summary
Theresa Betancourt and colleagues examine the associations between mental health and Ebola-related health behaviors in post-conflict Sierra Leone.
Introduction
In many post-conflict settings, years of protracted violence have left the populace exposed to war trauma and loss, which contribute to unmet mental health needs. A history of conflict in West Africa has destroyed health systems, undermined community relations, and reduced trust in state institutions, increasing risks for health crises and social unrest [1]. In Sierra Leone, the health system was decimated over the course of the 11-y civil war (1991–2002). An estimated 50,000 persons were killed, and over 20,000 children and adolescents were involved with armed groups [2]. In Sierra Leone today, health services remain underdeveloped, of poor quality, and fraught with barriers to accessing care [3]. Mental health and social services are nearly nonexistent [4].
Direct and indirect effects of war likely contributed to the ability of Ebola virus disease (EVD) to ravage the country in 2014–2015. This EVD outbreak in Sierra Leone is reported to have resulted in 8,704 confirmed cases (13,823 confirmed, probable, and suspected cases) and 3,589 confirmed deaths (3,955 confirmed, probable, and suspected deaths) [5] and laid bare the inadequacies of the health system, which was unable to manage the crisis at its peak. To prevent future EVD outbreaks in Sierra Leone, it is important to understand how unmet mental health and social service needs influence both EVD risk and health behaviors critical for EVD prevention.
Research has documented associations between war exposures, mental health problems, and impairments in functioning among survivors of trauma including war [6–11]. However, in the context of EVD in West Africa, associations between past trauma, ongoing mental health difficulties, and health behaviors remain unexplored. Drawing from theories examining adaptive coping to life stressors as well as research investigating disease risk behaviors in the context of HIV/AIDS [12–15], Fig 1 sets out a conceptual model whereby exposure to past trauma may affect both EVD risk behaviors and the uptake of prevention messaging and EVD prevention/health-promoting behaviors, and where this effect may be mediated by related mental health difficulties. Our hypotheses are grounded in previous research on mental health and the dynamics of infectious disease prevention. For instance, poor adherence to treatment for HIV/AIDS has been linked to depression as well as post-traumatic stress disorder (PTSD) and other anxiety disorders [16–20]. Similarly, we hypothesized that in the context of EVD, past trauma and depression would relate to poor problem-solving in the context of EVD. We theorized that PTSD and depression might contribute to hopelessness and a foreshortened sense of the future, which might increase the likelihood of risk behavior. Understanding the relationship between past war exposures, mental health, and EVD risk and EVD prevention behaviors might provide critical knowledge for EVD prevention in Sierra Leone and other post-conflict settings.
Fig. 1. Conceptual model for war exposures, mental health, and EVD-related behaviors. 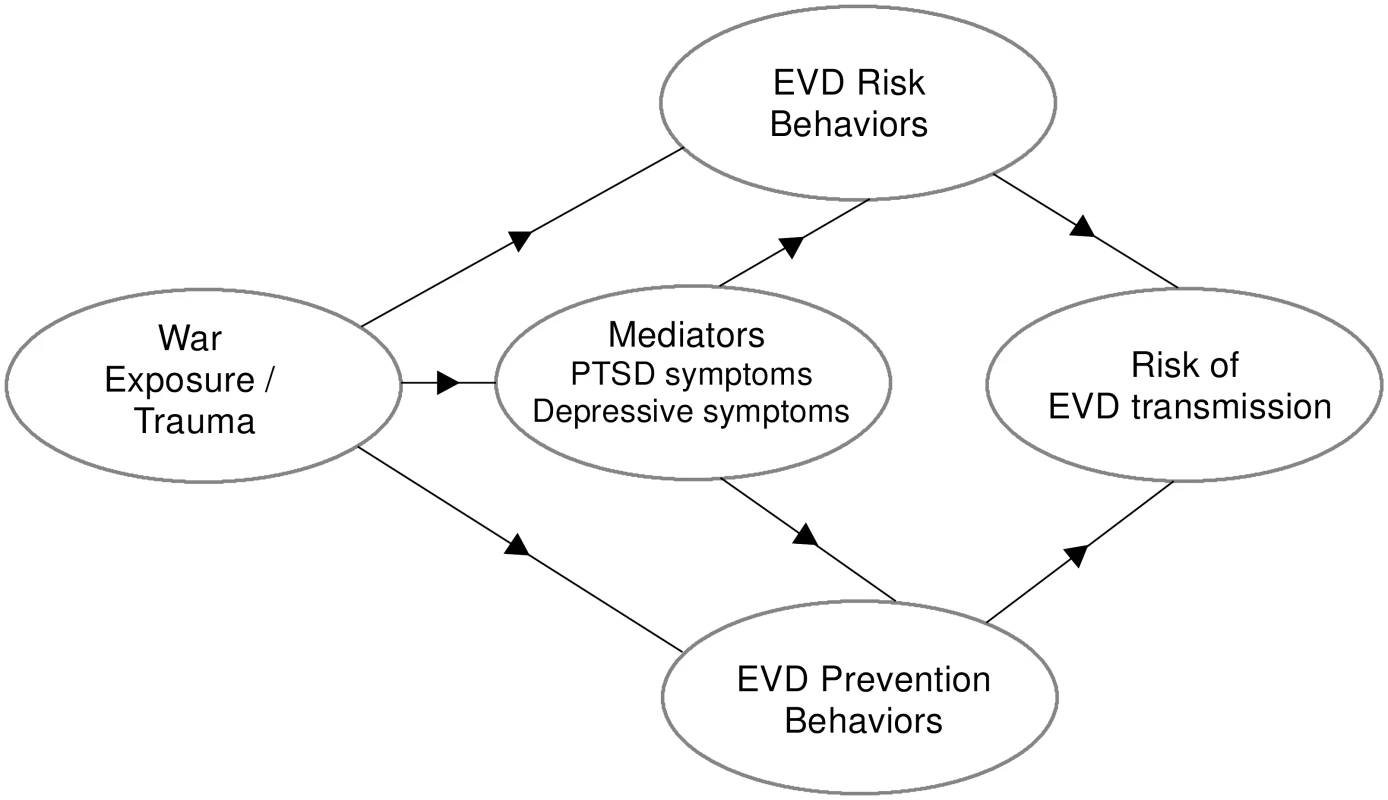
Methods
Institutional review board approval was obtained from the Harvard T. H. Chan School of Public Health (Protocol #15145, Approval #17) and the Sierra Leone Ministry of Health and Sanitation Ethics and Scientific Review Committee. With institutional review board approval, consent was obtained orally with a witness due to low literacy among participants. A local community advisory board, comprising community members and healthcare professionals, reviewed and advised the research.
This survey was conducted January–April 2015 in the Western Urban (including the capital, Freetown) and the Western Rural districts of Sierra Leone (Fig 2). These districts represent diversity in ethnic composition and degrees of war exposure and were the epicenter of EVD cases during the 2014–2015 outbreak, together accounting for over 40% of confirmed cases.
Fig. 2. Sampled districts (Western Urban and Western Rural) in Sierra Leone. 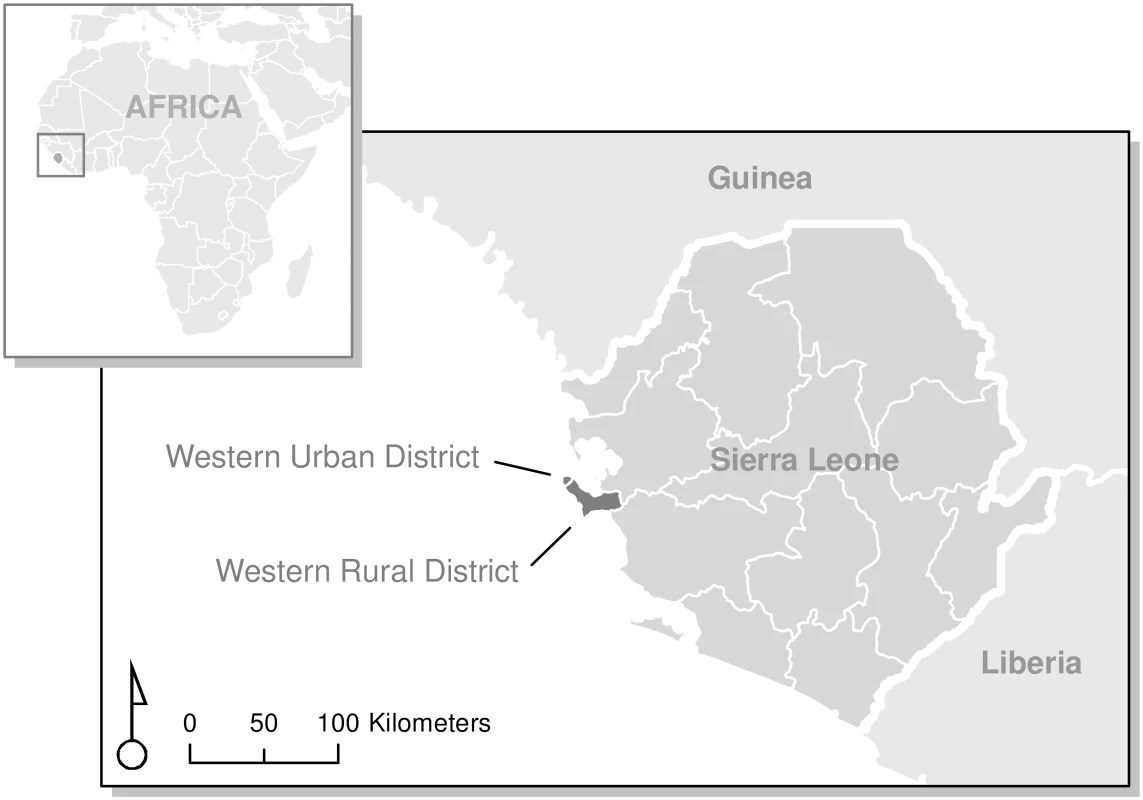
Map by the authors, based on 2012 global administrative areas in GADM, version 2.0 (http://www.gadm.org). Sample
The sampling population included adults 18 y and older living in the Western Urban and Western Rural districts, including Sierra Leone’s capital. Participants were selected using multistage cluster sampling. Census enumeration areas (EAs) were the primary sampling unit (see Fig 3). A list of EAs for the two districts and maps defining the EA boundaries were obtained from Statistics Sierra Leone [21]. Sixty-three EAs were randomly sampled from the list. Sixteen households within each EA were selected using random geographic sampling techniques. For each EA, a map was provided by Statistics Sierra Leone with a specified number of streets (2–5) indicated encompassing the EAs for the Sierra Leone 2004 Population and Housing Census. On those streets, the interviewers then selected a proportional sample of equally distanced households (with “household” defined as persons residing together). Each household was approached, and among adults who happened to be available on first contact, one was chosen at random from the household by alphabetizing first names in ascending order and choosing the first one. When a selected individual was unable or refused to participate, another individual within the selected household was randomly selected. After three attempts over the course of one day, if no household member was available, another household was selected using the same geographic randomization techniques.
Fig. 3. Sampling procedure. 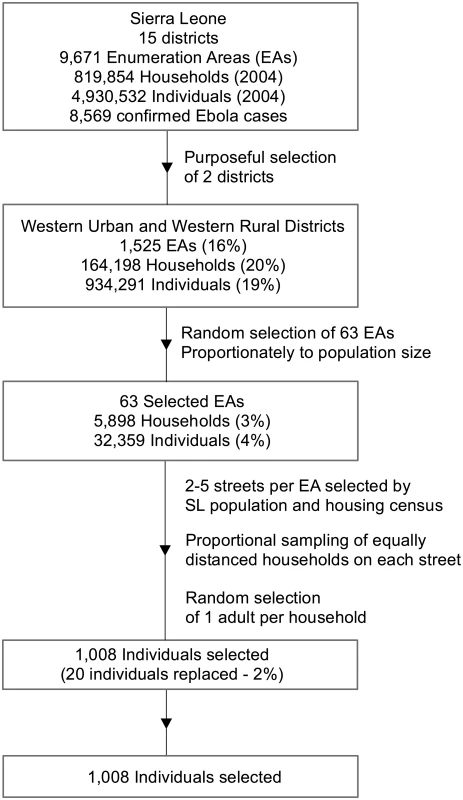
SL, Sierra Leone. Study Measures
The EVD risk behaviors outcome (Cronbach’s α = 0.84) was measured by 14 three-point items assessing likelihood (0 = very unlikely, 1 = somewhat likely, 2 = very likely) of engaging in certain behaviors if a family member or oneself experienced EVD-like symptoms (fever, fatigue, malaise and weakness, reddened eyes, joint and muscle pain, headache, nausea and vomiting). Such risk behaviors included waiting to see if the symptoms would go away, trying to treat the symptoms at home, and trying treatments such as hot salt water baths (see S1 Table for full list of risk behavior items). The EVD prevention behaviors outcome comprised a set of 16 items (α = 0.88) scored on a four-point frequency scale (0 = never, 1 = sometimes, 2 = often, 3 = always); EVD prevention behaviors included frequent hand washing, seeking EVD prevention information from a healthcare worker, and avoidance of large public events, public transport, and touching dead bodies, consistent with prevention messaging being used in Sierra Leone at the time of the study (see S2 Table for full list of prevention behavior items).
Independent variables (predictors) included an adapted version of the War Trauma Questionnaire, comprising 16 items, used in Liberia and the Democratic Republic of the Congo [22,23] to assess conflict-related experiences (eight items) and witnessing experiences (four items). Based on frequency of occurrence in the sample, item–total correlations, and internal consistency estimates, the 16 war exposure items in the original questionnaire were reduced to eight items addressing five victimization experiences (being forced to flee, having one’s home destroyed, being physically beaten, being forced to work or commit violence, being threatened with death) and three witnessing experiences (looting and destruction, beating or torture, killing of a household member). These were coded as 1 = occurrence or 0 = no occurrence and combined into one scale (α = 0.85). Anxiety and depression were assessed using a Krio (the lingua franca of Sierra Leone) adaptation of the Hopkins Symptom Checklist-25 (HSCL-25), scored on past week symptom intensity (1 = not at all, 2 = a little, 3 = quite a bit, 4 = extremely), previously adapted for Sierra Leone [24–26]. Both the depression (α = 0.91) and anxiety (α = 0.93) subscales had excellent internal consistency. To assess symptoms of PTSD, participants responded to 16 items (0 = no, 1 = yes) about the most distressing event they had ever experienced or witnessed, using the PTSD Symptom Scale–Interview adapted for use in Liberia (see S3 Table; α = 0.93) [27]. To assess personal EVD exposure, participants were asked five questions to determine whether a household member, a family member whom they did not live with, a friend, a neighbor, or someone in their community had been diagnosed with EVD over the past 12 mo (0 = no, 1 = yes).
Mental health scales used had been previously validated or used in Sierra Leone, Liberia, or other conflict-affected countries in sub-Saharan Africa [24–29]. All measures new to this setting were reviewed by local collaborators for face validity, examined item by item for local comprehension, and forward - and backward-translated following a standard protocol [30–32].
All continuous scales are averaged; thus, they are interpreted in terms of their original response scale.
Procedures
Local research assistants (eight women and seven men) were trained to administer the survey using Android tablets running Kobo Toolbox digital data collection software [33]. All research assistants received a 3-d training on survey administration and research ethics. Interviewers were assigned to same-sex participants. Interviews were conducted one-on-one in an outdoor setting (due to ongoing EVD outbreak) that provided privacy and confidentiality. Participants were given contact information to use if they had any questions and were offered a small gift of foodstuffs (value US$2) for agreeing to be interviewed. Risk of harm cases were referred to local mental health or social services for follow-up care (two cases were identified and referred).
Data Analysis Plan
All descriptive statistical analyses were conducted in STATA 13.0 SE [34]. Using HLM 7.0 [35], we estimated two-level hierarchical linear models (also called “multilevel” or “mixed” models) to accommodate the clustering of data into EAs and to prevent bias in estimation of standard errors. Because this was an equal allocation sampling design based on 16 households per EA, weights were applied based on the population of each EA to allow generalization to the Western Urban and Western Rural districts from which the EAs were sampled. Households in two EAs were undersampled because the EAs had been improperly identified (clerical error), so the remaining households were up-weighted so that those EAs would be properly represented in the sample. Furthermore, the households that had been misidentified were placed in their proper EAs, resulting in oversampling of those EAs; households in these EAs were, therefore, down-weighted to prevent overrepresentation in the weighted sample. Robust standard errors were used for all model interpretation.
In accordance with our conceptual model, multilevel models predicting EVD prevention behaviors and EVD risk behaviors were fit, containing the three mental health variables—anxiety, depression, and PTSD symptoms—as well as war exposures and EVD diagnosis of people in their family or community (details described above). To examine PTSD symptoms, anxiety, and depression as mediators of EVD risk and prevention behaviors, and to estimate the direct and indirect effects of war exposures, we fit multilevel models in which each of the outcomes (EVD prevention behaviors and EVD risk behaviors) was regressed on war exposures (with measures of personal exposure to EVD and anxiety as controls) and each of the mental health outcomes, and also models in which two of the mental health variables (PTSD symptoms and depression symptoms) were regressed on war exposures [36]. Because the temporal sequencing of EVD-related health behaviors and anxiety was less clear than that of the other two mental health variables, anxiety was not considered as a mediator. Mediation analyses assumed that the effect of the exposure and mediator on the outcome were unconfounded.
In order to make use of all available data (n = 1,008) and avoid possible bias associated with listwise missing value deletion, 20 multiply imputed datasets were created for the analyses, using all variables included in the analyses plus additional demographic variables (participant age, sex, marital status, education, and household wealth, based on household land and asset ownership) and participant report of daily hardships for the imputations. The number of missing values for a given variable can be determined by comparing the n for a given variable in Tables 1 and 2 (e.g., 979 for depression symptoms score) to 1,008, the total number of participants interviewed.
Tab. 1. Unweighted and weighted sociodemographic profile of participants. 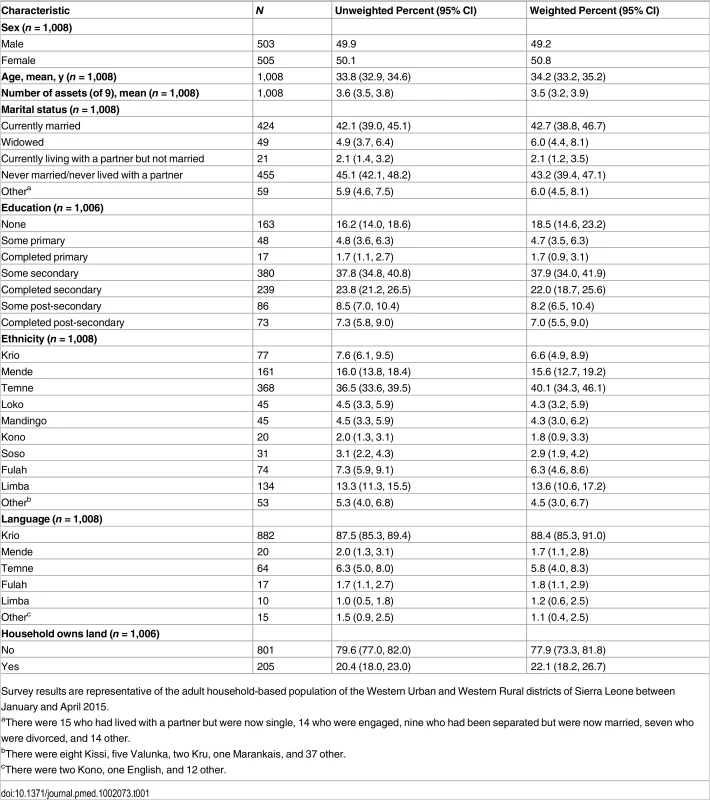
Survey results are representative of the adult household-based population of the Western Urban and Western Rural districts of Sierra Leone between January and April 2015. Tab. 2. Unweighted and weighted war exposures, mental health symptoms, personal exposure to EVD, and EVD-related health behavior outcomes. 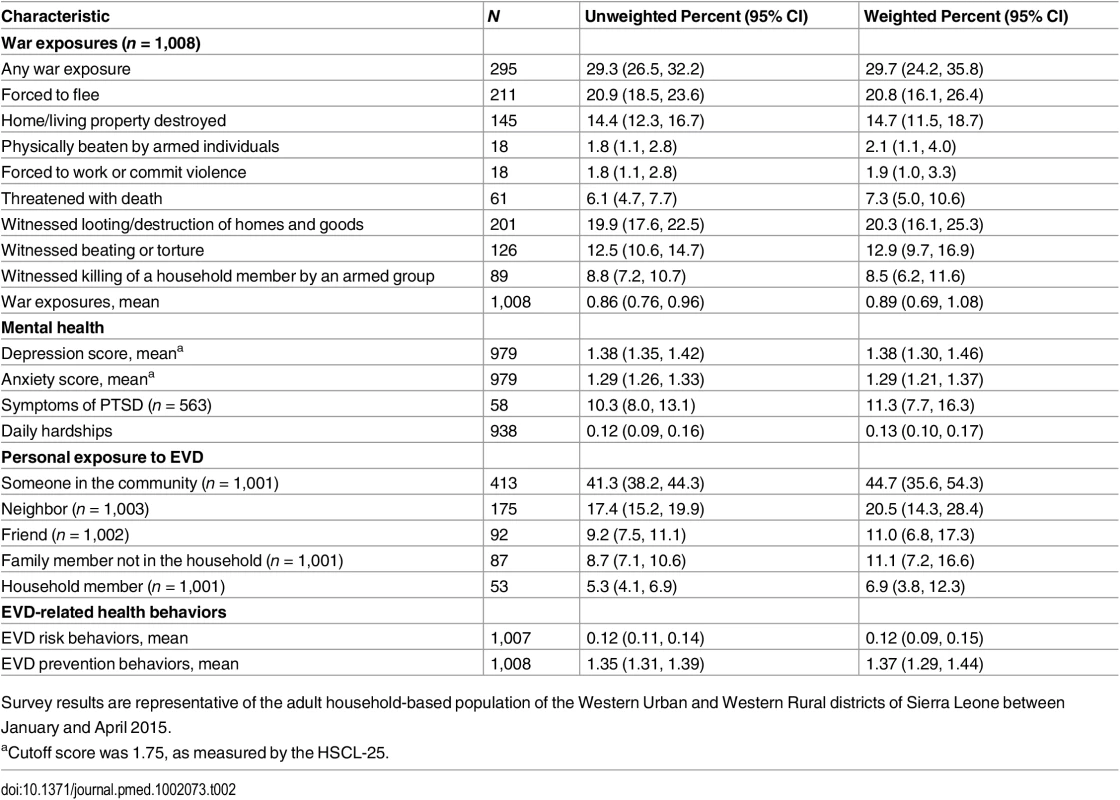
Survey results are representative of the adult household-based population of the Western Urban and Western Rural districts of Sierra Leone between January and April 2015. Results
Population-weighted estimates for the adult household-based population living in the Western Urban and Western Rural districts of Sierra Leone are presented in Table 1. The sample comprised 505 women (50.8%) and 503 men (49.2%). The mean age of participants was 34.2 y (95% CI 33.2, 35.2 y) and median age was 30 y, ranging from 18 to 84 y. Over 42% (42.7%; 95% CI 38.8%, 46.7%) of the participants reported being in a marital relationship or a partnership; an equal proportion (43.2%; 95% CI 39.4%, 47.1%) reported never being married or living with a partner. About a fifth of the participants reported no formal education (18.5%; 95% CI 14.6%, 23.2%) or incomplete primary schooling (4.7%; 95% CI 3.5%, 6.3%). The main ethnic groups were Temne (40.1%; 95% CI 34.3%, 46.1%), Mende (15.6%; 95% CI 12.7%, 19.2%), and Limba (13.6%; 95% CI 10.6%, 17.2%), and a majority of the participants (88.4%; 95% CI 85.3%, 91.0%) spoke Krio at home. Less than a quarter of participant households (22.1%; 95% CI 18.2%, 26.7%) owned their land, and out of a list of nine common assets, a mean of 3.5 (95% CI, 3.2, 3.9) assets was owned.
Thirty percent of participants (29.7%; 95% CI 24.2%, 35.8%) were exposed to at least one war-related event (Table 2), and the average number of war exposures was 0.88 (95% CI 0.69, 1.08). Of note, 20.8% (95% CI 16.1%, 26.4%) of the sample reported being forced to flee during the war, and 14.7% (95% CI 11.5%, 18.7%) had seen their homes/property destroyed. Just over 2% (2.1%; 95% CI 1.1%, 4.0%) of participants reported being beaten during the war, and 7.3% (95% CI 5.0%, 10.6%) of the sample had been threatened with death. Twenty percent of the sample (20.3%; 95% CI 16.1%, 25.3%) had witnessed looting/destruction of their home or belongings, 12.9% (95% CI 9.7%, 16.9%) had witnessed beating or torture of others, and 8.5% (95% CI 6.2%, 11.6%) had witnessed the killing of a household member by an armed group.
Levels of mental health problems were noteworthy. On the HSCL-25, the mean score was 1.38 (95% CI 1.30, 1.46) for the depression section and 1.29 (95% CI 1.21, 1.37) for the anxiety section. On the PTSD Symptom Scale, among those individuals who endorsed a traumatic war-related event or who chose to discuss a troubling event without describing it (n = 563), an estimated weighted prevalence in this sample for meeting the criteria of likely PTSD was 11.3% (95% CI 7.7%, 16.3%).
Close to half the participants reported having EVD cases in their community (44.7%; 95% CI 35.6%, 54.3%), and one in five reported cases among neighbors (20.5%; 95% CI 14.3%, 28.4%). Fewer reported cases among friends (11.0%; 95% CI 6.8%, 17.3%), family members outside the household (11.1%; 95% CI 7.2%, 16.6%), and household members (6.9%; 95% CI 3.8%, 12.3%).
Relationships between War Trauma and EVD Exposure, Mental Health, and EVD-Related Health Behaviors
Initial analyses showed that when personal EVD exposures were considered together, only EVD diagnosis of a friend showed a significant relationship with individual EVD prevention or risk behaviors; the other EVD exposures were thus dropped from all models for parsimony.
Relationships between war exposures, personal EVD exposure, mental health, and EVD-related health behaviors are displayed in Table 3. EVD risk behaviors were positively associated with depression symptom severity (b = 0.05; 95% CI 0.00, 0.10; p = 0.037) and PTSD symptom severity (b = 0.10; 95% CI 0.03, 0.17; p = 0.008) and inversely associated with war exposures (b = −0.09; 95% CI −0.17, −0.02; p = 0.036) and having a friend diagnosed with EVD (b = −0.04; 95% CI −0.08, −0.00; p = 0.036). Both PTSD (b = 0.47; 95% CI 0.31, 0.63; p < 0.001) and depression (b = 0.51; 95% CI 0.26, 0.76; p < 0.003) were associated with war exposures. The unstandardized coefficients are in terms of their original units as displayed in Table 2; for example, having a friend who had EVD is associated with an overall decrease in the risk behavior score of 0.04, which is about 17.6% of a standard deviation of that score. A decrease in the average response to the severity of depression scale of roughly 0.55 (a little more than halfway between responses on the Likert scale)—which corresponds to one standard deviation—results in an approximate 0.03 change in the outcome, which amounts to a 11.5% of a standard deviation change. Considering all variables in the model predicting EVD risk behaviors displayed in Table 3 and the additional steps to assess mediation, war exposures have an indirect positive effect on EVD risk behaviors through PTSD symptoms and depression; however, accounting for this effect, there is a negative direct effect of war exposures (i.e., tending to reduce EVD risk behaviors). Because the direct and indirect effects are in opposite directions, they act against each other and thus the total effects are closer to zero and not significant. Table 4 displays the direct, indirect, and total effects for depression and PTSD as mediators of war exposure’s effect on EVD risk and prevention behaviors.
Tab. 3. Estimated coefficients predicting EVD prevention and risk behaviors. 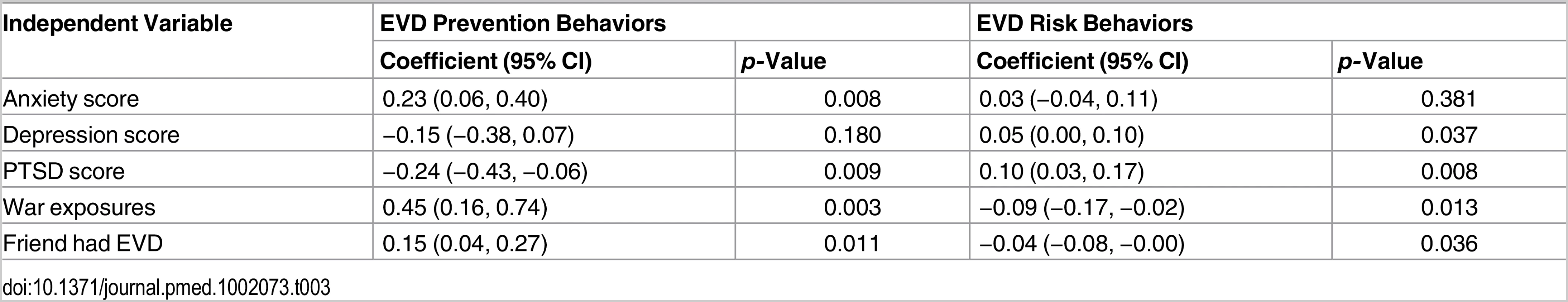
Tab. 4. Decomposition of effects of war exposures on EVD risk and prevention behaviors. 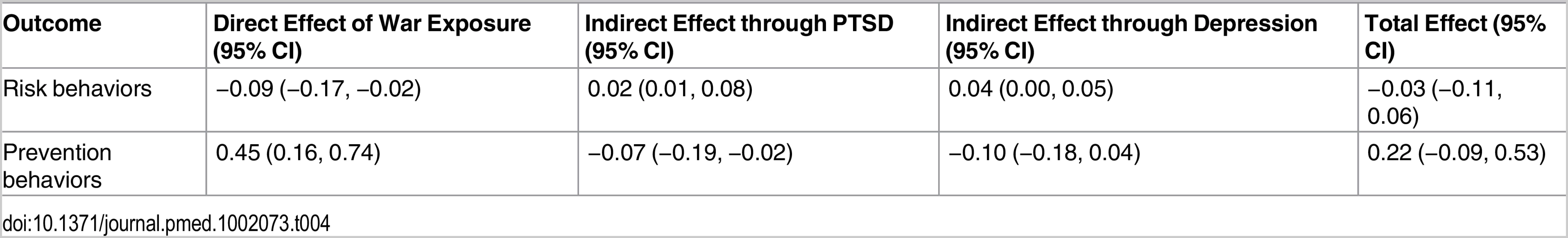
EVD prevention behaviors (Table 3) such as frequent hand washing and avoiding mass gatherings were associated with higher levels of anxiety (b = 0.23; 95% CI 0.06, 0.40; p = 0.008). Depression was not significantly associated with EVD prevention behaviors. Having a friend diagnosed with EVD (b = 0.15; 95% CI 0.04, 0.27; p = 0.011) and higher levels of war exposure (b = 0.45; 95% CI 0.16, 0.74; p = 0.003) were associated with greater EVD prevention behaviors, while PTSD symptoms were associated with fewer EVD prevention behaviors (b = −0.24; 95% CI −0.43, −0.06; p = 0.009). As above, the coefficients are in the original units of the scale. For example, having a friend diagnosed with EVD is related to an increase in the level of preventative behaviors of 0.15, which is about 24.6% of a standard deviation. A change in the response for anxiety symptoms, about one standard deviation, was related to an increase of about 0.13 on the preventative behavior scale, which is about 21.3% of a standard deviation. Similar to the effect seen above, war exposures had negative indirect effects on EVD prevention behaviors, but in the presence of mental health mediators, there was a positive direct effect of war exposures on preventative behaviors (Table 4).
Discussion
Consistent with our conceptual model, higher scores on measures of PTSD symptoms and depression were associated with higher EVD risk behaviors, and symptoms of PTSD were associated with lower levels of EVD prevention behaviors. In other words, chronic mental health difficulties associated with war trauma were associated with higher levels of risk behaviors in the context of the EVD epidemic. Furthermore, we showed that both PTSD and depression were in part associated with exposure to traumatic events during Sierra Leone’s civil war.
For both EVD prevention and EVD risk behaviors, the behaviors of participants were associated with EVD diagnosis of a friend, more so than with diagnosis of EVD among neighbors or other community members, suggesting that intimate knowledge of affected patients may be more important than geographic proximity in shaping one’s personal response to the epidemic.
After accounting for the association between war exposures and adverse mental health consequences, higher levels of exposure to war-related events were associated with EVD prevention behaviors; such a relationship might be indicative of individuals with higher levels of war exposure being persons with stronger survival skills or who have become more risk adverse.
Our results are consistent with relationships established between depression and PTSD in research on HIV risk behaviors [15]. As has been found in HIV research, in the presence of common mental health problems such as depression, good judgment was possibly distorted, leading to our finding that higher levels of depression symptoms were associated with higher levels of EVD risk behaviors. Traumatic stress reactions may also play a similar role whereby, in the presence of PTSD symptoms, the ability of the individual to attend to EVD prevention activities was less. However, higher levels of anxiety symptoms were associated with more EVD prevention behaviors such as hand washing and seeking out EVD information via healthcare workers, suggesting that anxious persons may maintain a higher level of vigilance or concern about the EVD epidemic or that vigilance may have raised anxiety in some individuals who were more actively taking precautions. It is also difficult to disentangle the relationship of anxiety to the EVD epidemic. It is possible that an unmeasured trait, such as vigilance, underlies both anxiety and preventive behaviors.
Study Limitations
Although this is, to our knowledge, the first study of its kind to examine the relationship between both past war exposure and mental health and present-day EVD-related health behaviors, limitations must be noted. Although we used randomly selected census EAs to derive a representative sample of households in the Western Area at the height of the epidemic, this sample is specific to Freetown and the Western Area and not representative of Sierra Leone’s other 13 districts. However, this sample is of relevance for understanding the dynamics related to EVD and mental health in other major capital cities in the EVD-affected countries of West Africa. The analyses may also be subject to some degree of confounding. In addition, the measures of our main outcomes as well as personal EVD exposure, war exposures, and mental health predictors rely on self-report, and therefore raise the possibility of common methods bias.
Conclusion
In post-conflict settings, high levels of unaddressed mental health problems are common and are associated with war exposure. Such mental health difficulties can in turn shape the uptake of sensitization campaigns and public health messages aimed at reducing EVD risk. The findings in this study indicate the need for greater attention to the role of PTSD, depression, and other common mental health problems in counteracting risks for EVD in post-conflict Sierra Leone and may have implications for other war-affected regions. More generally, the findings suggest that successful uptake of EVD prevention messages among individuals with poor mental health in post-conflict low - and middle-income countries requires specific and targeted approaches that take into account the nature of war traumas, the resulting behavioral implications, and the potentially re-traumatizing effect of communication around fear and death, which are exacerbated in the context of such crises but remain underaddressed. The EVD epidemic laid bare the weaknesses in Sierra Leone’s health services. The country’s highly underdeveloped mental health and social services system must be strengthened to respond to the reality of compounded adversity due to both war and the recent epidemic and to prevent future outbreaks [37].
Supporting Information
Zdroje
1. World Health Organization. Building back better: sustainable mental health care after emergencies. Geneva: World Health Organization; 2013.
2. Human Rights Watch. Youth poverty and blood: the lethal legacy of West Africa’s regional warriors. New York: Human Rights Watch; 2005.
3. World Health Organization. Mental health atlas 2011. Geneva: World Health Organization; 2011.
4. Shultz JM, Baingana F, Neria Y. The 2014 Ebola outbreak and mental health: current status and recommended response. JAMA. 2015;313 : 567–568. doi: 10.1001/jama.2014.17934 25532102
5. Sierra Leone Ministry of Health and Sanitation. Ebola virus disease—situation report. 2015 Apr 16. Freetown: Government of Sierra Leone; 2015.
6. Vinck P, Pham PN. Association of exposure to violence and potential traumatic events with self-reported physical and mental health status in the Central African Republic. JAMA. 2010;304 : 544–552. doi: 10.1001/jama.2010.1065 20682934
7. Newnham EA, Pearson RM, Stein A, Betancourt TS. Youth mental health after civil war: the importance of daily stressors. Br J Psychiatry. 2015;206 : 116–121. doi: 10.1192/bjp.bp.114.146324 25497299
8. Miller KE, Rasmussen A. War exposure, daily stressors, and mental health in conflict and post-conflict settings: bridging the divide between trauma-focused and psychosocial frameworks. Soc Sci Med. 2010;70 : 7–16. doi: 10.1016/j.socscimed.2009.09.029 19854552
9. Miller K, Omidian P, Rasmussen A, Yaqubi A, Daudzai H. Daily stressors, war experiences, and mental health in Afghanistan. Transcult Psychiatry. 2008;45 : 611–638. doi: 10.1177/1363461508100785 19091728
10. Derluyn I, Broekaert E, Schuyten G, De Temmerman E. Post-traumatic stress in former Ugandan child soldiers. Lancet. 2004;363 : 861–863. 15031032
11. Miller KE, Omidian P, Kulkarni M, Yaqubi A, Daudzai H, Rasmussen A. The validity and clinical utility of post-traumatic stress disorder in Afghanistan. Transcult Psychiatry. 2009;46 : 219–237. doi: 10.1177/1363461509105813 19541748
12. Sikkema K, Watt M, Drabkin A, Meade C, Hansen N, Pence B. Mental health treatment to reduce HIV transmission risk behavior: a positive prevention model. AIDS Behav. 2010;14 : 252–262. doi: 10.1007/s10461-009-9650-y 20013043
13. Lovejoy T, Heckman T, Sikkema K, Hansen N, Kochman A. Changes in sexual behavior of HIV-infected older adults enrolled in a clinical trial of standalone group psychotherapies targeting depression. AIDS Behav. 2015;19 : 1–8. doi: 10.1007/s10461-014-0746-7 24668254
14. Tsai A, Mimiaga M, Dilley J, Hammer G, Karasic D, Charlebois E, et al. Does effective depression treatment alone reduce secondary HIV transmission risk? Equivocal findings from a randomized controlled trial. AIDS Behav. 2013;17 : 2765–2772. doi: 10.1007/s10461-013-0600-3 23975476
15. Cavanaugh CE, Hansen NB, Sullivan TP. HIV sexual risk behavior among low-income women experiencing intimate partner violence: the role of posttraumatic stress disorder. AIDS Behav. 2010;14 : 318–327. doi: 10.1007/s10461-009-9623-1 19856093
16. Willie TC, Overstreet NM, Sullivan TP, Sikkema KJ, Hansen NB. Barriers to HIV medication adherence: examining distinct anxiety and depression symptoms among women living with HIV who experienced childhood sexual abuse. Behav Med. 2016;42 : 120–127. doi: 10.1080/08964289.2015.1045823 26010763
17. Whetten K, Shirey K, Pence BW, Yao J, Thielman N, Whetten R, et al. Trauma history and depression predict incomplete adherence to antiretroviral therapies in a low income country. PLoS ONE. 2013;8:e74771. doi: 10.1371/journal.pone.0074771 24124455
18. Peterson K, Togun T, Klis S, Menten J, Colebunders R. Depression and posttraumatic stress disorder among HIV-infected Gambians on antiretroviral therapy. AIDS Patient Care STDS. 2012;26 : 589–596. doi: 10.1089/apc.2012.0089 22989270
19. Panigrahi M, Swain TR, Mohanty S. Nonadherence to anti-HIV medication is associated with higher level of anxiety: experience from a tertiary care hospital of Odisha. Indian J Pharmacol. 2015;47 : 672–675. doi: 10.4103/0253-7613.169578 26729962
20. Adejumo O, Oladeji B, Akpa O, Malee K, Baiyewu O, Ogunniyi A, et al. Psychiatric disorders and adherence to antiretroviral therapy among a population of HIV-infected adults in Nigeria. Int J STD AIDS. 2015 Sep 18. doi: 10.1177/0956462415600582
21. Statistics Sierra Leone. Final results: 2004 population and housing census. 2006 Feb 23 [cited 15 Jun 2016]. http://www.sierra-leone.org/Census/ssl_final_results.pdf.
22. Pham PN, Vinck P, Kinkodi DK, Weinstein HM. Sense of coherence and its association with exposure to traumatic events, posttraumatic stress disorder, and depression in eastern Democratic Republic of Congo. J Trauma Stress. 2010;23 : 313–321. doi: 10.1002/jts.20527 20564363
23. Vinck P, Pham PN. Association of exposure to intimate-partner physical violence and potentially traumatic war-related events with mental health in Liberia. Soc Sci Med. 2013;77 : 41–49. doi: 10.1016/j.socscimed.2012.10.026 23219850
24. Bean T, Derluyn I, Eurelings-Bontekoe E, Broekaert E, Spinhoven P. Validation of the multiple language versions of the Hopkins Symptom Checklist-37 for refugee adolescents. Adolescence. 2007;42 : 51–71. 17536475
25. Betancourt TS, Borisova II, de la Soudière M, Williamson J. Sierra Leone’s child soldiers: war exposures and mental health problems by gender. J Adolesc Health. 2011;49 : 21–28. doi: 10.1016/j.jadohealth.2010.09.021 21700152
26. Derogatis LR, Lipman RS, Rickels K, Uhlenhuth EH, Covi L. The Hopkins Symptom Checklist (HSCL): a self-report symptom inventory. Behav Sci. 1974;19 : 1–15. 4808738
27. Johnson K, Asher J, Rosborough S, Raja A, Panjabi R, Beadling C, et al. Association of combatant status and sexual violence with health and mental health outcomes in postconflict Liberia. JAMA. 2008;300 : 676–690. doi: 10.1001/jama.300.6.676 18698066
28. Bolton P, Neugebauer R, Ndogoni L. Prevalence of depression in rural Rwanda based on symptom and functional criteria. J Nerv Ment Dis. 2002;190 : 631–637. 12357098
29. Betancourt TS, Brennan RT, Rubin-Smith J, Fitzmaurice GM, Gilman SE. Sierra Leone’s former child soldiers: a longitudinal study of risk, protective factors, and mental health. J Am Acad Child Adolesc Psychiatry. 2010;49 : 606–615. doi: 10.1016/j.jaac.2010.03.008 20494270
30. Van Ommeren M, Sharma B, Thapa S, Makaju R, Prasain D, Bhattarai R, et al. Preparing instruments for transcultural research: use of the translation monitoring form with Nepali-speaking Bhutanese refugees. Transcult Psychiatry. 1999;36 : 285.
31. Betancourt T, Scorza P, Meyers-Ohki S, Mushashi C, Kayiteshonga Y, Binagwaho A, et al. Validating the center for epidemiological studies depression scale for children in Rwanda. J Am Acad Child Adolesc Psychiatry. 2012;51 : 1284–1292. doi: 10.1016/j.jaac.2012.09.003 23200285
32. World Health Organization. Process of translation and adaptation of instruments. 2012 [cited 17 Apr 2015]. http://www.who.int/substance_abuse/research_tools/translation/en/.
33. Harvard Humanitarian Initiative. KoBo Toolbox 2.0. http://www.kobotoolbox.org/.
34. StataCorp. Stata statistical software: release 13.0. College Station (Texas): StataCorp; 2013.
35. Raudenbush SW, Bryk AS, Congdon RT Jr. HLM 7.0 for Windows. Skokie (Illinois): Scientific Software International; 2011.
36. MacKinnon DP. Introduction to statistical mediation analysis. New York: Lawrence Erlbaum; 2009.
37. Reardon S. Ebola’s mental health wounds linger in Africa. Nature. 2015;519 : 13–14. doi: 10.1038/519013a 25739606
Štítky
Interní lékařství
Článek vyšel v časopisePLOS Medicine
Nejčtenější tento týden
2016 Číslo 8- Berberin: přírodní hypolipidemikum se slibnými výsledky
- Léčba bolesti u seniorů
- Příznivý vliv Armolipidu Plus na hladinu cholesterolu a zánětlivé parametry u pacientů s chronickým subklinickým zánětem
- Jak postupovat při výběru betablokátoru − doporučení z kardiologické praxe
- Červená fermentovaná rýže účinně snižuje hladinu LDL cholesterolu jako vhodná alternativa ke statinové terapii
-
Všechny články tohoto čísla
- Dementia across the Lifespan and around the Globe—Pathophysiology, Prevention, Treatment, and Societal Impact: A Call for Papers
- Progress and Challenges in Scaling Up Laboratory Monitoring of HIV Treatment
- Facility-Based Delivery during the Ebola Virus Disease Epidemic in Rural Liberia: Analysis from a Cross-Sectional, Population-Based Household Survey
- Availability and Use of HIV Monitoring and Early Infant Diagnosis Technologies in WHO Member States in 2011–2013: Analysis of Annual Surveys at the Facility Level
- Duration of Adulthood Overweight, Obesity, and Cancer Risk in the Women’s Health Initiative: A Longitudinal Study from the United States
- Improving Clinical Risk Stratification at Diagnosis in Primary Prostate Cancer: A Prognostic Modelling Study
- Genetically Predicted Body Mass Index and Breast Cancer Risk: Mendelian Randomization Analyses of Data from 145,000 Women of European Descent
- Social Dancing and Incidence of Falls in Older Adults: A Cluster Randomised Controlled Trial
- Genetic and Environmental Risk for Chronic Pain and the Contribution of Risk Variants for Major Depressive Disorder: A Family-Based Mixed-Model Analysis
- Long-Term Outcomes Associated with Traumatic Brain Injury in Childhood and Adolescence: A Nationwide Swedish Cohort Study of a Wide Range of Medical and Social Outcomes
- On Risk Estimation versus Risk Stratification in Early Prostate Cancer
- Make Data Sharing Routine to Prepare for Public Health Emergencies
- Assessment of Adverse Events in Protocols, Clinical Study Reports, and Published Papers of Trials of Orlistat: A Document Analysis
- Concussions and Repercussions
- South Asia as a Reservoir for the Global Spread of Ciprofloxacin-Resistant : A Cross-Sectional Study
- Building from the HIV Response toward Universal Health Coverage
- Transitioning to Country Ownership of HIV Programs in Rwanda
- Accelerating the Uptake and Timing of Antiretroviral Therapy Initiation in Sub-Saharan Africa: An Operations Research Agenda
- Glycemic Control and the Risk of Tuberculosis: A Cohort Study
- Adjuvant Trastuzumab in HER2-Positive Early Breast Cancer by Age and Hormone Receptor Status: A Cost-Utility Analysis
- Uptake of Home-Based HIV Testing, Linkage to Care, and Community Attitudes about ART in Rural KwaZulu-Natal, South Africa: Descriptive Results from the First Phase of the ANRS 12249 TasP Cluster-Randomised Trial
- An Audit and Feedback Intervention for Reducing Antibiotic Prescribing in General Dental Practice: The RAPiD Cluster Randomised Controlled Trial
- Multidrug-Resistant Tuberculosis Treatment in North Korea: Is Scale-Up Possible?
- Associations between Mental Health and Ebola-Related Health Behaviors: A Regionally Representative Cross-sectional Survey in Post-conflict Sierra Leone
- Pancreatic Cancer Surgical Resection Margins: Molecular Assessment by Mass Spectrometry Imaging
- Integrated Delivery of Antiretroviral Treatment and Pre-exposure Prophylaxis to HIV-1–Serodiscordant Couples: A Prospective Implementation Study in Kenya and Uganda
- Measuring Burden of Unhealthy Behaviours Using a Multivariable Predictive Approach: Life Expectancy Lost in Canada Attributable to Smoking, Alcohol, Physical Inactivity, and Diet
- Comparison of Outcomes before and after Ohio's Law Mandating Use of the FDA-Approved Protocol for Medication Abortion: A Retrospective Cohort Study
- Core Outcomes for Colorectal Cancer Surgery: A Consensus Study
- Adverse Renal, Endocrine, Hepatic, and Metabolic Events during Maintenance Mood Stabilizer Treatment for Bipolar Disorder: A Population-Based Cohort Study
- PLOS Medicine
- Archiv čísel
- Aktuální číslo
- Informace o časopisu
Nejčtenější v tomto čísle- Glycemic Control and the Risk of Tuberculosis: A Cohort Study
- Transitioning to Country Ownership of HIV Programs in Rwanda
- Dementia across the Lifespan and around the Globe—Pathophysiology, Prevention, Treatment, and Societal Impact: A Call for Papers
- Social Dancing and Incidence of Falls in Older Adults: A Cluster Randomised Controlled Trial
Kurzy
Zvyšte si kvalifikaci online z pohodlí domova
Současné možnosti léčby obezity
nový kurzAutoři: MUDr. Martin Hrubý
Všechny kurzyPřihlášení#ADS_BOTTOM_SCRIPTS#Zapomenuté hesloZadejte e-mailovou adresu, se kterou jste vytvářel(a) účet, budou Vám na ni zaslány informace k nastavení nového hesla.
- Vzdělávání



