-
Články
Top novinky
Reklama- Vzdělávání
- Časopisy
Top články
Nové číslo
- Témata
Top novinky
Reklama- Videa
- Podcasty
Nové podcasty
Reklama- Kariéra
Doporučené pozice
Reklama- Praxe
Top novinky
ReklamaWhy We Need Urban Health Equity Indicators: Integrating Science, Policy, and Community
article has not abstract
Published in the journal: . PLoS Med 9(8): e32767. doi:10.1371/journal.pmed.1001285
Category: Policy Forum
doi: https://doi.org/10.1371/journal.pmed.1001285Summary
article has not abstract
Summary Points
-
As the urban population of the planet increases and puts new stressors on infrastructure and institutions and exacerbates economic and social inequalities, public health and other disciplines must find new ways to address urban health equity.
-
Urban indicator processes focused on health equity can promote new modes of healthy urban governance, where the formal functions of government combine with science and social movements to define a healthy community and direct policy action.
-
An inter-related set of urban health equity indicators that capture the social determinants of health, including community assets, and track policy decisions, can help inform efforts to promote greater urban health equity.
-
Adaptive management, a strategy used globally by scientists, policy makers, and civil society groups to manage complex ecological resources, is a potential model for developing and implementing urban health equity indicators.
-
Urban health equity indicators are lacking and needed within cities of both the global north and south, but universal sets of indicators may be less useful than context-specific measures accountable to local needs.
Toward Healthier and More Equitable Cities
As the world urbanizes, global health challenges are increasingly concentrated in cities. Currently, over 80% of the population in Latin America already lives in cities. The African urban population is projected to double in the next decade and China has urbanized in thirty years at a rate it took Europe and North America a century [1]. Rapidly growing new cities and increasingly segregated older cities in the global north and south are contributing to health inequities. Urban planning and policies can influence population health by supporting or stymieing opportunities for employment, housing security, political participation, education, protection from environmental risks, access to primary health care, and a host of other social and physical determinants of well-being [2]. As the World Health Organization (WHO) and UN-HABITAT acknowledged in the 2010 report entitled “Hidden Cities: Unmasking and Overcoming Health Inequities in Urban Settings”, where in a city you live and how that city is governed can determine whether or not one benefits from city living [3].
Measuring the forces that contribute to urban health is one challenge for promoting more healthy and equitable cities. Burden of disease estimates have tended to focus on the whole world or specific geographic regions [4],[5]. These data can mask intra-city differences and global data may not be relevant to inform national or municipal policy making. Public health has developed metrics for single pathogenic exposures or risk factors, but these measures often ignore both community assets that promote health equity and the cumulative impacts on health from exposure to multiple urban environmental, economic, and social stressors [6],[7]. Recognizing these population health challenges, the United Nations (UN) Commission on Social Determinants of Health (2008) called for “health equity to become a marker of good government performance” ([8], p. 11) and for the UN to “adopt health equity as a core global development goal and use a social determinants of health indicators framework to monitor progress” ([8], p. 19). More recently, the 2011 World Social Determinants of Health Conference and the Pan-American Health Organization's Urban Health Strategy called for the development of new urban health equity indicators that track the drivers of health inequities across place and time, particularly within a city neighborhood [9] (Box S1). In this paper, we briefly outline an approach for promoting greater urban health equity through the drafting and monitoring of indicators. We draw examples from the cities of Richmond, California, and Nairobi, Kenya. More specifically, we argue that participatory indicator processes hold the potential to shape new healthy and equitable urban governance by:
-
integrating science with democratic decision making;
-
tracking policy decisions that shape the distribution of health outcomes; and
-
including protocols for ongoing monitoring and adjusting of measures over time.
Indicators for Health Promoting Policy Change
Ongoing measurement and evaluation is one critical aspect of moving toward more healthy and equitable cities because what we measure often matters for whether and how we act. Yet, the danger of indicator efforts is that they portray a too simplified picture of a complex reality and policy solutions may suffer the same defects. For example, indicators of single chemical exposures cannot produce policy-relevant knowledge about the environmental health consequences of multiple exposures. In a similar way, cross-sectional measures of single built and social environmental features of urban neighborhoods tend to ignore the cascading and relational effects of inequalities in urban areas. For example, in our own work in the slums of Nairobi, we have found that typical indicators that only measure population access to a toilet can misconstrue whether an ablution block is hygienic or safe. In Nairobi's slums, accessing a toilet may be controlled by a local cartel that might extort a high price for users, disproportionately impacting family income, while at the same time acting as a location for rape and sexual violence against women, particularly at night, when the toilet has no lighting or security, which in-turn might contribute to the spread of sexually transmitted diseases. Capturing the relationships between a physical or economic measure, the political decisions that shape the distribution of community resources, and how urban residents currently navigate urban inequities to stay healthy is central to our understanding of effective and meaningful urban health equity indictors.
The WHO defines an indicator as a variable with characteristics of quality, quantity, and time used to measure, directly or indirectly, changes in health and health-related situations [10]. In this paper, we use the term indicator to represent a construct often consisting of more than one measure, with a metric being the actual quantitative or qualitative data that is used to populate the indicator [11]. Our review of the vast health equity indicator literature suggests that indicators should do more than capture health outcomes, but also the determinants of health that often drive outcomes, including institutional practices and policy decisions made outside the health care and medical sectors. In addition, effective urban health equity indicators ought to highlight associations between determinants and health impacts, use data that are verifiable and easily accessible, and be shared in a clear and compelling way to a range of interested stakeholders [11],[12],[13],[14] (Table 1 and S1).
Tab. 1. Comparison of conventional and our approach to urban health equity indicators. 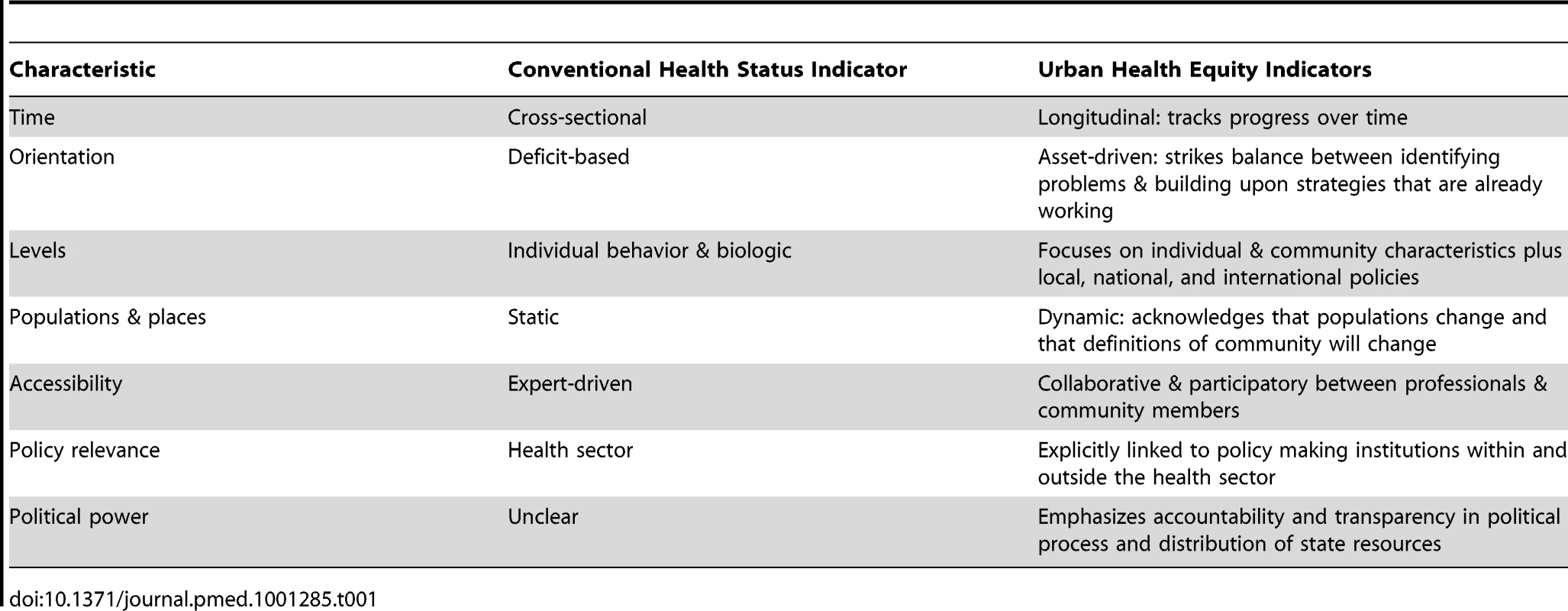
Indicators as Adaptive Urban Health Equity Governance
The complexity of cities and the variegated forces that contribute to (in)equity in urban neighborhoods demands that indicator development processes are similarly dynamic. The drafting, measuring, tracking, and reporting of indicators can be viewed not as a technical process for experts alone, but rather as an opportunity to develop new participatory science policy making, or what we call governance. Governance is not just government and the decisions of formal institutions, such as ministries of health, but also includes the norms, routines, and practices that help shape which issues get onto the health research and policy agenda, what evidence base is used to underwrite decisions, and which social actors are deemed expert enough to participate in these decisions [15]. In other words, governance processes can shape what issues are deemed important for promoting health equity and which institutions are responsible for action [16] (Box 1).
Box 1. How Indicators Act as a Form of Healthy Urban Governance
-
Identifying and framing what counts as a health policy issue.
-
Generating, or contributing to, the evidentiary standards that underwrite health equity issues.
-
Constituting some social actors as “experts”, by deciding who gets to participate in defining indicators.
-
Grappling with different knowledge claims as the weight and importance of indicators is debated.
-
Highlighting the importance of public accountability and transparency of data in the way indicators are reported and shared with various publics.
The UN-HABITAT Urban Indicators project recognizes the importance of governance measures for tracking urban equity. In order to measure governance, the UN project measures such things as the degree of decentralization in public decision making, voter participation, the number of participants in civil society organizations, and the public transparency and accountability of local government institutions [17]. Similarly, the World Health Organization's Urban Health Equity Assessment and Response Tool (HEART) also attempts to measure some aspects of governance related to health equity and includes indicators such as government spending on health and education, voter participation, percentage of population completing primary education, and the proportion of the population covered by health and other insurance [18]. These are important steps in acknowledging and capturing the role of politics and non–health care specific policy making in measuring and acting to promote greater health equity in cities.
We suggest that indicator processes themselves, not just the measures, can act as opportunities for crafting new healthy and equitable urban governance. While this is an emerging idea for city health management, ecologists and others have used an iterative governance process called adaptive management for decades to steward complex ecosystems, such as forests, wetlands, and fisheries [19]. Adaptive management acknowledges the failures of linear processes where narrow disciplinary scientists have aimed to develop complex models, predict long-term outcomes, and suggest one-time policy standards. Instead, adaptive management begins with an acknowledgement of the inherent complexity and uncertainty within systems, that this complexity demands an iterative, ongoing learning process among a range of expert stakeholders, and that policy interventions must be adjusted to reflect newly acquired knowledge [20]. Another difference between adaptive management and conventional science policy is that adaptive management does not postpone actions until definitive causality is known about a system, but rather emphasizes the importance of action in the face of uncertain science and couples decisions tightly to rigorous monitoring [21],[22].
The process of adaptive management is one where a broad group of stakeholders, from scientists to policy makers to users of a resource, work together to generate evidence, make decisions, monitor the progress of those decisions, and make ongoing adjustments to decisions as new information emerges from monitoring [20]. Gohlke and Portier call for greater capacity within public health institutions to adapt to new and emerging challenges, such as drug-resistant infections and climate change, and that the field and discipline is currently ill-suited for adaptive science-based research and practice [21]. Huang et al. also stress the importance of enhancing resources and training for the redesign of public health institutions to enhance the field's adaptive capacity [22]. Yet, few others in public health or urban planning have explored the potential of applying adaptive management to promote greater health equity in cities.
Urban Health Inequities in North and South
Drawing from our collaborative work on healthy urban governance and the drafting of health equity indicators in Richmond, California, and the Mathare Valley informal settlement in Nairobi, Kenya, we offer some brief examples of what an urban health equity adaptive management strategy might entail.
In Richmond, California, located in the San Francisco Bay Area, one-third of residents live at or below 200% of the federal poverty line, over 60% of the population is African-American, Latino, or Asian-American, one in seven people are unemployed, residents live with elevated concentrations of industrial and mobile source air pollution, and it is one of the most violent cities, measured by per-capita homicide rates, in the United States [23]. In Richmond, African-Americans have the highest rate of infant mortality, low-birth weight babies, and asthma hospitalizations in Contra Costa County, and residents of the Iron Triangle neighborhood, one of the poorest in the city, die on average 13 years earlier than their wealthier white neighbors [23].
The Mathare Valley is a sprawling informal settlement in Nairobi, where over 82% of residents rent dirt floor, sheet metal–walled, one-room shacks and 88% lack access to clean and reliable drinking water or a private, hygienic toilet [24] (Figure S1). According to a 2011 household survey conducted in Mathare, over two-thirds of residents experienced routine violence in the last year, over half live on environmentally risky slopes and flood-prone areas, and households spend, on average, 76% of their monthly income on food [24]. Child mortality in Nairobi's slums is 151 per 1,000 live births, compared to 62 per 1,000 in all of Nairobi and 113 in rural Kenya [25].
Recognizing these health inequities and the multiple factors contributing to them, actions to improve the physical, social, and economic environments are occurring in both Richmond and Mathare. In Richmond, community groups and the city government drafted a Health and Wellness Element—or a development and policy blueprint—as part of the city's General Plan Update. Community-based organizations also led their own processes to collect data for and draft health equity indicators [26],[27].
In Mathare, community groups are working to reduce violence, engage youth in employment activities, and build toilets and schools [28],[29]. One coalition includes Muungano wa Wanavijiji, the federation of the urban poor in Kenya, Slum Dwellers International (SDI), the University of Nairobi, and the University of California, Berkeley, who together are organizing residents to plan for physical and social improvements that include new water and sanitary infrastructure, housing and land rights, and environmental and health care services [30],[31]. The government of Kenya and the World Bank recently launched a national policy initiative aimed at improving living conditions and well-being in slums, called the Kenya Informal Settlements Improvement Programme (KISIP) [32].
Urban Health Equity Indicators in Practice
In Richmond, the indicator process emerged from ongoing community organizing and land use planning, and included community-based organizations and the city and county health department. Community priorities were highlighted through a process called “Measuring What Matters” where over ten different community-based organizations identified priority issues, chose indicators, collected and analyzed data, and published a comprehensive report that included quantitative and qualitative information [27]. At the same time, the city organized a participatory process to draft and implement the Health and Wellness Element, which included a set of goals and metrics aimed at promoting and monitoring progress on population health [33]. In order to track and monitor indicators on an ongoing basis, the Richmond Health Equity Partnership (http://richmondhealth.org) was established in 2012 and includes representatives from the city, county health department, school district, and a host of community-based organizations.
In Mathare, the nongovernmental organization Muungano Support Trust (MuST) has organized residents to survey themselves and document community assets and vulnerabilities in three waves starting in 2007 through 2012 [28],[31]. These data have been combined with spatial maps of community assets and hazards and used by MuST in community planning processes focused on specific projects, such as improving housing, water infrastructure, health care access, and community facilities [31]. In 2011, a comprehensive slum redevelopment plan focused on Mathare was drafted by residents, MuST, the University of Nairobi, and University of California, Berkeley, which includes indicators and a process for ongoing monitoring [31].
In both cases, we began by organizing community health priorities into three broad health equity categories: living conditions, economics and services, and political power and outcomes. Under each category, indicators were selected that constituted the elements of the category. For instance, under living conditions, housing, key utilities such as water, sanitation and food, the physical environment, community safety, and transportation were selected as representative indicator categories (Table 2).
Tab. 2. Examples of urban health equity indicators. 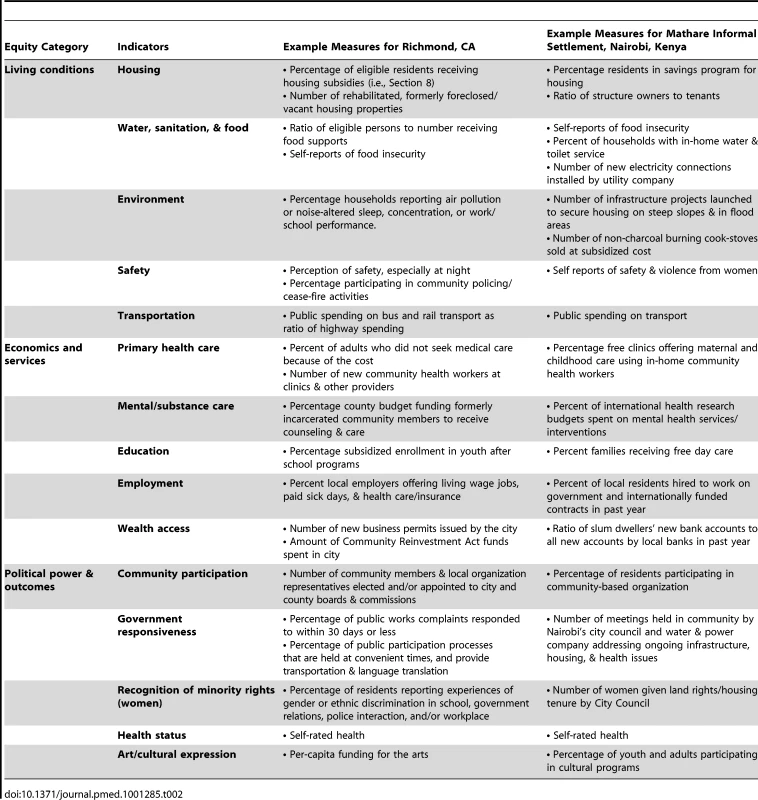
Importantly for public health practitioners, policy makers, and community residents, each indicator includes a health - and equity-based rationale that is referenced in the peer-reviewed literature. While a number of measures could populate each indicator, the participatory process selected one or two priority measures that were deemed representative of the larger equity issue being addressed and linked these to local or state policies that were understood by participants as potentially promoting greater health equity. The idea was to generate a set of measures that when combined could suggest whether or not the community was making progress toward greater health equity (Figure S2).
Limits of City Health Equity Indicators
All indicator efforts are limited in that they make judgments about selecting and highlighting certain data over others. These value judgments do not make indicator efforts unscientific or invalid, but rather demand that the processes for selection and the denial of data be explicit and transparent and, as we have suggested here, open to interpretation and re-evaluation. Another limitation of indicator efforts is whether they inspire action by different actors, from within and outside the health sector. Traditional indicators that measure morbidity and mortality tend to either place responsibility for improving health on the medical and public health communities or on vaguely identified institutions such as the economy, education, or built environment. The result is an overemphasis on medical and public health solutions while failing to articulate the specific institutions and policies that might need to change to promote greater health equity. While our examples from Richmond and Nairobi are in the early stages, we are witnessing non–health care specific sectors and institutions, from urban planning to legal and housing rights to violence prevention, re-framing their work as contributing to urban health equity.
Indicator projects can also be limited by a lack of available data and the costs of obtaining locally specific information. Very few cities in the global north or south collect data on the social determinants of health at the neighborhood scale and those that do rarely keep these data in one publically accessible location. However, advances in mobile information technology and the use of hand-held devices with built-in sensors are creating new opportunities for tracking and reporting different types of urban health equity data. In Toronto, Canada, the health ministry has created the Toronto Central Local Health Integration Network (LHIN), which aims to bring together multiple community actors and government agencies to improve health for the urban poor and tracks progress using indicators of equity [34]. In Rio de Janeiro, Brazil, the Center for Health Promotion is a network of over 150 civil society organizations working to promote health equity and, among other tasks, gathers data on the social determinants of health equity in Rio's favelas [35]. In Belo Horizonte, Brazil, an urban health observatory conducts participatory research and maintains data on population - and place-based health equity issues [36]. The Indian nongovernmental organization Urban Health Resource Centre (http://www.uhrc.in) works with the urban poor to improve health equity and helped shape India's National Urban Health Mission, which will document many determinants of health in cites [37]. In San Francisco, California, the public health department maintains a health equity–oriented publically available database called the Healthy Development Measurement Tool [38].
Conclusions
As urban health is increasingly recognized as a global health priority, new indicators accompanied by monitoring processes that can adapt and improve over time will be necessary to promote greater health equity. We have suggested here that indicator processes might be one important strategy to encourage new models of urban health governance in both the global north and south. Like any concept, more research and evaluation is necessary to understand the barriers and opportunities for turning our conceptual ideas into practice. Yet, lessons from other fields and emerging experiments around the world suggest that indicator processes can integrate science, policy, and community to promote greater urban health equity.
Supporting Information
Zdroje
1. World Bank (2011) Urban development data. Available: http://data.worldbank.org/topic/urban-development. Accessed 1 December 2011.
2. VlahovD, FreudenbergN, ProiettiF, OmpadD, QuinnA, et al. (2007) Urban as a determinant of health. J Urban Health 84(1):16–25.
3. World Health Organization/UN-HABITAT (2010) Hidden cities. Available: http://www.hiddencities.org/report.html. Accessed 8 July 2011.
4. MurrayCJ, LopezAD (1997) Mortality by cause for eight regions of the world: Global Burden of Disease Study. Lancet 349 : 1269–1276.
5. WurthweinR, GbangouA, SauerbornR, SchmidtCM (2001) Measuring the local burden of disease. A study of years of life lost in sub - Saharan Africa. Int J Epidemiol 30 : 501–508.
6. SteenlandK, ArmstrongB (2006) An overview of methods for calculating the burden of disease due to specific risk factors. Epidemiology 17 : 512–519.
7. HarphamT (2009) Urban health in developing countries: what do we know and where do we go? Health and Place 15 : 107–116.
8. Commission on Social Determinants of Health (CSDH) (2008) Closing the gap in a generation: health equity through action on the social determinants of health. Final Report of the Commission on Social Determinants of Health. Geneva, World Health Organization
9. World Health Organization (2011) Rio Political Declaration on Social Determinants of Health. World Conference on Social Determinants of Health. Available: http://www.who.int/sdhconference/declaration/en. Accessed 1 December 2011.
10. World Health Organization (2009) Indicator definitions. Available: http://www.who.int/whosis/indicators/en. Accessed 8 May 2011.
11. Flores LM, Davis R, Culross P (2007) Community health: a critical approach to addressing chronic diseases. Prev Chronic Disease 4(4): A108. Available: http://www.cdc.gov/pcd/issues/2007/oct/07_0080.htm. Accessed 14 June 2011.
12. O'NeillM, SimardP (2006) Choosing indicators to evaluate Healthy Cities projects: a political task? Health Promot Int 21(2):145–152.
13. Corburn J (2005) Street science: community knowledge and environmental health justice. Cambridge, MA: The MIT Press.
14. CumminsS, CurtisS, Diez-RouxAV, MacintyreS (2007) Understanding and representing ‘place’ in health research: a relational approach. Soc Sci Med 65 : 1825–1838.
15. BurrisS, HancockT, LinV, HerzogA (2007) Emerging strategies for healthy urban governance. J Urban Health 84(1):i54–i63.
16. Corburn J (2009) Toward the healthy city: people, places, and the politics of urban planning. Cambridge, MA: The MIT Press.
17. UN-HABITAT (2011) Urban indicators. Available: http://www.unhabitat.org/content.asp?typeid=19&catid=646&cid=8383. Accessed 11 November 2011.
18. Word Health Organization (WHO) (2010) Urban Health Equity Assessment and Response Tool (HEART). Available: http://www.who.int/kobe_centre/measuring/urbanheart/en/index.html. Accessed 3 October 2011.
19. Lee KN (1993) Compass and gyroscope: integrating science and politics for the environment. Washington, D.C.: Island Press.
20. National Research Council (2004) Adaptive management in water resources project planning. Panel on Adaptive Management for Resource Stewardship. Washington, DC: National Academies Press.
21. GohlkeJM, PortierCJ (2007) The forest for the trees: a systems approach to human health research. Environ Health Perspect 115(9):1261–1263.
22. HuangC, VaneckovaP, WangX, FitzGeraldG, GuoY, TongS (2011) Constraints and barriers to public health adaptation to climate change. Am J Prev Med 40(2):183–190.
23. Contra Costa Health Services (CCHS) (2010) Community health indicators for Contra Costa County. Available: http://cchealth.org/health_data/hospital_council/. Accessed 23 February 2011.
24. Muungano Support Trust (MuST) (2011) Mathare Valley community survey. University of Nairobi and University of California, Berkeley. Unpublished data. Available: http://muunganosupporttrust.wordpress.com/ and http://www.centreforurbaninnovations.com/. Accessed 13 December 2011.
25. Kenya National Bureau of Statistics (KNBS) (2010) Demographic Health Survey (DHS), 2003–2009, results. Nairobi, Kenya
26. CohenAK, LopezA, MalloyN, Morello-FroschR (2012) Our environment, our health: a community-based participatory environmental health survey in Richmond, CA. Health Educ Behav 39(2):198–209 doi:10.1177/1090198111412591.
27. Pacific Institute (2009) Measuring what matters: neighborhood research for economic and environmental health and justice in Richmond, North Richmond and San Pablo. Available: http://www.pacinst.org/reports/measuring_what_matters/index.htm Accessed 8 June 2011.
28. WeruJ (2004) Community federations and city upgrading: the work of Pamoja Trust and Muungano in Kenya. Environment and Urbanization 16(14):47–62.
29. KaranjaI (2010) An enumeration and mapping of informal settlements in Kisumu, Kenya, implemented by their inhabitants. Environment and Urbanization 22(1):217–239.
30. Slum Dwellers International (SDI) (2011) What is incrementalism, part 2: community-managed utilities in an informal settlement in Nairobi. Available: http://www.sdinet.org/blog/2011/05/23/what-is-incrementalism-part-2-/. Accessed 22 November 2011.
31. Muungano Support Trust (2011) The Mathare Zonal Plan. Available: http://muunganosupporttrust.wordpress.com/2011/10/28/the-mathare-zonal-plan/. Accessed 11 November 2011.
32. World Bank (2011) Kenya Informal Settlements Improvement Programme (KISIP). Available: http://web.worldbank.org/external/projects/main?Projectid=P113542&theSitePK=40941&piPK=73230&pagePK2=64283627&menuPK=228424. Accessed 3 December 2011.
33. City of Richmond (2011) Community Health and Wellness Element. Available: http://www.ci.richmond.ca.us/index.aspx?NID=2412. Accessed 25 April 2012.
34. Toronto Central Local Health Integration Network (LHIN) (2011) Toronto Central LHIN website. Available: http://www.torontocentrallhin.on.ca. Accessed 13 November 2011.
35. Centre for Health Promotion (CEDAPS) (2011) CEDAPS website. Available: http://www.cedaps.org.br. Accessed 12 October 2011.
36. Belo Horizonte Observatory for Urban Health (OSUBH) (2011) OSUBH website. Available: http://www.medicina.ufmg.br/osubh. Accessed 9 December 2011.
37. India Ministry of Health (2011) National Urban Health Mission. Available: http://mohfw.nic.in/NRHM/Documents/Urban_Health/UH_Framework_Final.pdf. Accessed 24 November 2011.
38. San Francisco Department of Public Health (2011) The Healthy Development Measurement Tool. Available: http://www.thehdmt.org. Accessed 22 September 2011.
Štítky
Interní lékařství
Článek Challenges for HIV Pre-Exposure Prophylaxis among Men Who Have Sex with Men in the United StatesČlánek Child Mortality Estimation: Accelerated Progress in Reducing Global Child Mortality, 1990–2010
Článek vyšel v časopisePLOS Medicine
Nejčtenější tento týden
2012 Číslo 8- Berberin: přírodní hypolipidemikum se slibnými výsledky
- Léčba bolesti u seniorů
- Příznivý vliv Armolipidu Plus na hladinu cholesterolu a zánětlivé parametry u pacientů s chronickým subklinickým zánětem
- Jak postupovat při výběru betablokátoru − doporučení z kardiologické praxe
- Červená fermentovaná rýže účinně snižuje hladinu LDL cholesterolu jako vhodná alternativa ke statinové terapii
-
Všechny články tohoto čísla
- Multidrug Resistant Pulmonary Tuberculosis Treatment Regimens and Patient Outcomes: An Individual Patient Data Meta-analysis of 9,153 Patients
- Challenges for HIV Pre-Exposure Prophylaxis among Men Who Have Sex with Men in the United States
- What Is the Relationship of Medical Humanitarian Organisations with Mining and Other Extractive Industries?
- Conflict of Interest Reporting by Authors Involved in Promotion of Off-Label Drug Use: An Analysis of Journal Disclosures
- Child Mortality Estimation: A Global Overview of Infant and Child Mortality Age Patterns in Light of New Empirical Data
- What Is the Optimal First Line Antiretroviral Therapy in Resource-Limited Settings?
- Educating Enough Competent Health Professionals: Advancing Educational Innovation at Muhimbili University of Health and Allied Sciences, Tanzania
- Developing and Costing Local Strategies to Improve Maternal and Child Health: The Investment Case Framework
- Child Mortality Estimation: Methods Used to Adjust for Bias due to AIDS in Estimating Trends in Under-Five Mortality
- Child Mortality Estimation: Appropriate Time Periods for Child Mortality Estimates from Full Birth Histories
- Child Mortality Estimation: Accelerated Progress in Reducing Global Child Mortality, 1990–2010
- Why We Need Urban Health Equity Indicators: Integrating Science, Policy, and Community
- Legal Disputes over Duties to Disclose Treatment Risks to Patients: A Review of Negligence Claims and Complaints in Australia
- An Alternative Framework for Analyzing Financial Protection in Health
- Child Mortality Estimation: A Comparison of UN IGME and IHME Estimates of Levels and Trends in Under-Five Mortality Rates and Deaths
- The Role of HIV-Related Stigma in Utilization of Skilled Childbirth Services in Rural Kenya: A Prospective Mixed-Methods Study
- Neonatal Mortality Risk Associated with Preterm Birth in East Africa, Adjusted by Weight for Gestational Age: Individual Participant Level Meta-Analysis
- Efficacy and Safety of Three Antiretroviral Regimens for Initial Treatment of HIV-1: A Randomized Clinical Trial in Diverse Multinational Settings
- The Air That We Breathe: Addressing the Risks of Global Urbanization on Health
- Effects of Intensive Blood Pressure Lowering on Cardiovascular and Renal Outcomes: A Systematic Review and Meta-Analysis
- Child Mortality Estimation: Estimating Sex Differences in Childhood Mortality since the 1970s
- Feasibility, Yield, and Cost of Active Tuberculosis Case Finding Linked to a Mobile HIV Service in Cape Town, South Africa: A Cross-sectional Study
- Diagnosing Severe Falciparum Malaria in Parasitaemic African Children: A Prospective Evaluation of Plasma HRP2 Measurement
- Child Mortality Estimation: Consistency of Under-Five Mortality Rate Estimates Using Full Birth Histories and Summary Birth Histories
- PLOS Medicine
- Archiv čísel
- Aktuální číslo
- Informace o časopisu
Nejčtenější v tomto čísle- Feasibility, Yield, and Cost of Active Tuberculosis Case Finding Linked to a Mobile HIV Service in Cape Town, South Africa: A Cross-sectional Study
- Multidrug Resistant Pulmonary Tuberculosis Treatment Regimens and Patient Outcomes: An Individual Patient Data Meta-analysis of 9,153 Patients
- Child Mortality Estimation: A Global Overview of Infant and Child Mortality Age Patterns in Light of New Empirical Data
- What Is the Optimal First Line Antiretroviral Therapy in Resource-Limited Settings?
Kurzy
Zvyšte si kvalifikaci online z pohodlí domova
Současné možnosti léčby obezity
nový kurzAutoři: MUDr. Martin Hrubý
Všechny kurzyPřihlášení#ADS_BOTTOM_SCRIPTS#Zapomenuté hesloZadejte e-mailovou adresu, se kterou jste vytvářel(a) účet, budou Vám na ni zaslány informace k nastavení nového hesla.
- Vzdělávání



