-
Články
Top novinky
Reklama- Vzdělávání
- Časopisy
Top články
Nové číslo
- Témata
Top novinky
Reklama- Videa
- Podcasty
Nové podcasty
Reklama- Kariéra
Doporučené pozice
Reklama- Praxe
Top novinky
ReklamaUsing Touchscreen Electronic Medical Record Systems to Support and Monitor National Scale-Up of Antiretroviral Therapy in Malawi
article has not abstract
Published in the journal: . PLoS Med 7(8): e32767. doi:10.1371/journal.pmed.1000319
Category: Health in Action
doi: https://doi.org/10.1371/journal.pmed.1000319Summary
article has not abstract
Background
The scale-up of antiretroviral therapy (ART) in sub-Saharan Africa is unprecedented. Effective monitoring and evaluation (M&E) systems are essential to track patient access to and retention on ART; to encourage feedback to improve clinic-based care; and to ensure rational drug forecasting and timely procurement to prevent drug stock-outs [1]. Complete and accurate data are a fundamental prerequisite for any M&E system.
Standardized tools for ART data collection were in use in all 297 public and private sector ART sites in Malawi by December 2009. Most sites use a paper-based system, consisting of treatment cards for each patient and one ART patient register per clinic. Their use in case-finding and treatment follow-up have been described previously [2]. Every quarter, ART clinic personnel perform a standardized patient cohort analysis that includes aggregation of case-finding details of patients registered during the previous quarter and since ART was first begun, as well as treatment outcomes for the cumulative cohort. The latter analysis requires a review of all treatment cards in order to update the clinic register and then a tally-score on current patient outcomes. “Primary outcomes” include alive on ART, died, stopped ART, transferred to another ART clinic, and lost to follow-up. Secondary outcomes for patients alive on ART include ART regimen, drug adherence, ART side effects, and current tuberculosis status. A rolling “cohort survival analysis” is also performed by counting primary outcomes of patients who registered during specified previous quarters [2].
By December 2009, 46 ART clinics in Malawi had each registered >2,000 patients and 11 of these had registered >5,000 patients [3]. At most of these high-burden clinics, nurses and medical record clerks can take up to 5 days to prepare the quarterly cohort report, sometimes closing the clinic in order to complete this task. While the quality of the quarterly case-finding data is usually good, the completeness and accuracy of primary outcome data are often compromised, and secondary outcome analyses are usually no longer feasible due to time constraints. These challenges are not limited to Malawi: a recent study conducted in 15 countries across Africa, South America, and Asia concluded that data quality at ART treatment sites is generally unsatisfactory [4]. Lack of access to evidence-based information remains a major barrier to improving healthcare in the developing world [5]–[7].
We believe that paper-based systems cannot work efficiently or accurately once large patient numbers are reached and that computerized systems are essential, a position supported by experienced practitioners in this field [8]. Furthermore, we believe that the traditional approach to M&E where the M&E process exists as a separate layer or “wrapper” around the clinical process has several shortcomings. Recognizing that M&E data and patient care data are essentially one [8], we advocate an approach that tightly couples M&E and patient care processes, recording data once at the point-of-care (POC).
Here, we describe the rationale and experience of using a touchscreen electronic medical record (EMR) system at the POC to monitor and support ART scale-up in Malawi. The EMR eliminates the process of manual updating of paper registers and data aggregation for cohort and survival analysis reports, and produces cohort reports at the touch of a button on the screen. We present a model, developed and refined in Malawi, that has the potential to improve data quality and clinical efficiency in low-resource settings by integrating EMR and M&E systems.
Start of ART EMR in Malawi
In 2005, a task force created by the Department for HIV and AIDS, Ministry of Health, Malawi (MoH), investigated the feasibility of introducing computers to capture patient data and produce cohort reports at ART clinics. Two EMR operational models were considered. The first (based on several systems used elsewhere in developing countries [9]–[15]) employed a dedicated clerk to enter patient information retrospectively from patient treatment cards into a single desktop computer. The second had computers in every clinic room, connected to a central server that stored the data. With the latter model, healthcare workers would use touchscreen computers to enter patient information during clinical encounters at POC. Based on experiences of using touchscreen systems in various domains in healthcare in Malawi since 2001 [15]–[24], the task force chose the second model and established core functionality requirements for the touchscreen POC system. Pilot implementation started at the ART clinic at Queen Elizabeth Central Hospital (QECH), Blantyre, in April 2006, funded by the Global AIDS Program of the Centers for Disease Control and Prevention in Malawi. The selection of QECH was based on both high patient burden resulting in failure to manually produce quarterly reports (see Figure 1) and ease of site access. Patient treatment cards and clinic registers were maintained until there was evidence that the EMR was working reliably, had been incorporated into daily use, and was institutionalized within the clinic.
Fig. 1. ART Clinic filing room at Queen Elizabeth Central Hospital. 
The man pictured in Figure 1 has given written informed consent (as outlined in the PLoS consent form) allowing the publication of his photograph. Image credit: Joep J. van Oosterhout. Engineering an EMR Solution
In creating the EMR, two guiding principles directed our design choices towards balancing the needs of system users equally with other stakeholder groups. First, the EMR must improve the work of the system user, in other words, “a person working in partnership with an information resource is ‘better’ than the same person [working] unassisted”, a proposed fundamental theorem in the field of biomedical informatics [25]. Second, the EMR must ease the work of the users in compelling ways by providing a value proposition for the user, an issue that receives insufficient attention in the development of EMR systems [26].
Early work in developing an EMR system in Kenya encountered four main barriers: 1) low computer literacy among the target user group, 2) lack of unique patient identifiers, 3) difficulty in maintaining clean and reliable electrical power, and 4) managing the transition from paper to an electronic medium [10]. These problems, cited by others working in resource-constrained settings, represent core challenges to be addressed. During early pilot work in Malawi, we approached each of these challenges using hardware and software innovations [23].
First, we addressed the issue of computer literacy among the target user group, as this had important design implications for both hardware and software. We focused on a touchscreen computer with a graphical user interface as a solution that was easy to learn and use [22].
Second, we realized that the absence of unique patient identifiers (IDs) was a significant barrier to maintaining continuity of care, a fundamental requirement in the management of life-long chronic illnesses such as HIV/AIDS, diabetes mellitus, and hypertension. We chose therefore to build and deploy a system for issuing patient ID numbers. The system was first piloted at the central hospital in Malawi's capital city in March 2001. It has issued more than 650,000 nationally unique patient IDs since going live (and more than 1,100,000 IDs nationally across six sites).
Third, we discounted the idea of using uninterruptible power supplies, as they provide an inadequate length of backup time to meet the demands of multi-hour blackouts common in low-income countries. We also rejected the idea of using a generator, as this requires logistical support for procuring and topping-up fuel that we believed to be unsustainable. We favored a centralized approach that would keep the entire “system” running that has the added advantage of requiring surge protection at a single location only, where the backup system is connected to the main electrical grid. We borrowed from the telecommunications industry, which has a long history of using 48 volts DC to reliably run electronic equipment without interruption. Our solution utilizes four locally available deep-cycle 12-volt batteries of the type used in solar power installations. To further extend the duration of backup power, we utilize low-power appliance-model hardware. A complete description of the power solution is given in Text S1.
Fourth, we addressed the transition from paper to an electronic system by adopting a POC approach. Paper-based data collection tools such as patient treatment cards were replaced with touchscreen clinical workstation (TCW) appliances. Recognizing that a “paperless” system was not yet feasible, we created a “paper-enhanced” system, where information such as patient visit summaries and medication prescriptions could be printed onto inexpensive adhesive labels and affixed to existing paper artifacts such as patient-kept health passports or patient discharge forms. To facilitate this transition, a newly formatted treatment card was created upon which labels documenting the clinic visit for each patient are affixed. A summary of these and other challenges and our solutions is provided in Text S2.
Software-related design decisions included a commitment to use open-source software and selecting programming languages that local software developers could quickly develop proficiency with (Text S3).
Use and Features of the EMR
At a typical ART clinic, healthcare workers interact with patients at multiple sequential locations or POC stages (registration, vital signs recording station, nurse review room, clinician review room, pharmacy). The software application is designed to support and enforce adherence to a standard workflow, but is sufficiently flexible to support multiple workflows (Text S4).
At each POC, healthcare workers use password-protected TCW appliances. The TCW comprises a low-power panel-PC-style touchscreen computer (no mouse or keyboard), augmented with a thermal label printer and barcode scanner. A description of the TCW and a rationale for the “information appliance” approach is provided in Text S5. Once logged in, healthcare workers initiate a session by scanning the barcoded label on the patient's health passport (Text S6). This starts the application at the correct stage for that patient.
The EMR guides the healthcare worker through a series of questions, one at a time, according to the Malawi ART guidelines. Touch-friendly screens are generated from standard HTML Web forms using the Touchscreen Toolkit (Text S7). While using the system, the healthcare worker has access to a limited past medical history through a patient dashboard and receives alerts (e.g., patient body mass index <18 – start nutritional support) and reminders (e.g., >6 months since previous CD4 lymphocyte count test). The system also performs clinical calculations (e.g., drug adherences) and facilitates medication prescribing and dispensing. Once the encounter is complete, a summary of the patient's visit is printed on an adhesive label and affixed in the patient's health passport (Text S6).
The system provides a complete set of automated reports for M&E, based on national requirements (Table 1). On-screen reports are “active”, allowing the user to tunnel down to a patient list from any indicator.
Tab. 1. Characteristics and Treatment Outcomes of ART Patients Registered at the Six EMR Sites in Malawi up to December 31, 2009. 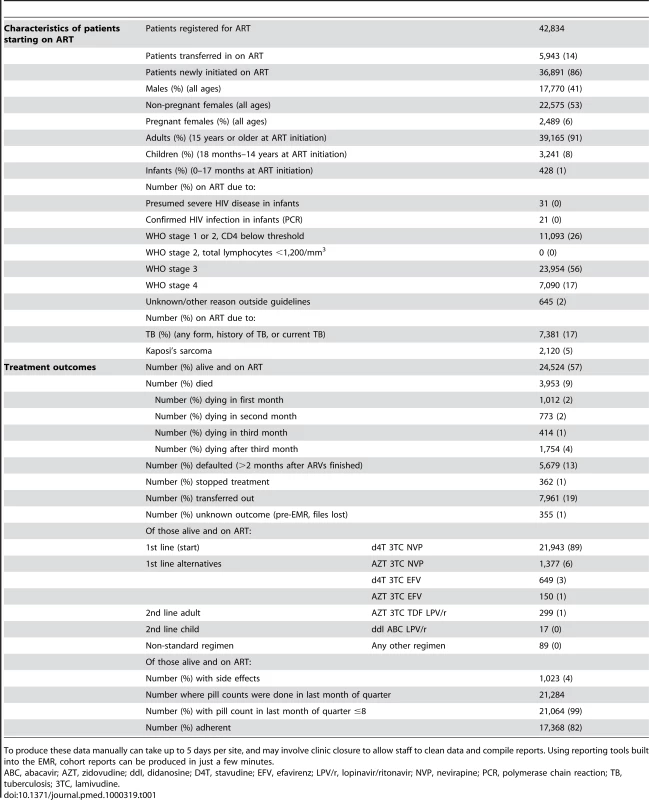
To produce these data manually can take up to 5 days per site, and may involve clinic closure to allow staff to clean data and compile reports. Using reporting tools built into the EMR, cohort reports can be produced in just a few minutes. We address the issue of scalability, localization, and customization of the EMR in Text S8. A list of the benefits afforded by the POC model is provided in Text S9.
Results
By December 2009, the EMR had been deployed at six ART sites in Malawi. Table 1 shows case finding and treatment outcome details of the 42,834 patients registered across the six sites.
In 2007, ten users at QECH were interviewed with a 25-question instrument to measure their impressions of the pilot EMR [27]. Seven (70%) of the users expressed a preference for the touchscreen over the paper system; two more (20%) had no preference. However, every respondent identified ongoing problems with the system that needed to be addressed and rectified as soon as possible. The detailed feedback from the survey was used in creating version 2 of the EMR. Version 2 was subsequently deployed at QECH.
In late 2007, version 2 of the EMR was piloted at two district hospitals (Dedza and Salima), and evaluated by the task force [28]. The evaluation concluded that the system met both patient care and programmatic monitoring objectives, and emphasized the importance of refining the approach of maintaining stable power, data communications, and user training. Based on the findings of this evaluation, the MoH endorsed the EMR for national use.
In 2008, a study comparing the accuracy of data captured at POC versus the same data entered retrospectively from treatment cards in the ART clinic at QECH showed that data were equally, or more, accurate when captured at POC in this setting [19],[20].
Lessons Learned in Rolling Out the EMR in Malawi
A number of valuable lessons have been learned that will inform future roll-out of the system at other high-burden sites. We aim to have at least 50,000 ART patients managed by the EMR system by December 2010.
Producing complete and accurate cohort reports has been challenging for several reasons. First, errors, inconsistencies, and incompleteness of data in paper records must be resolved prior to back-entry of data from patient treatment cards, a process required for cumulative cohort analysis after the EMR is deployed. Second, data entry errors are made at the POC. To address this, we introduced a system to improve data validation at the POC utilizing dynamically adjusted validity ranges. Here, users are warned when data values appear implausible, in addition to disallowing values entirely when completely out of range (Text S10). A data-cleaning module has been added to the system, enabling staff to systematically identify and amend inconsistent and incomplete records. Data cleaning is now carried out monthly, significantly improving data quality. Third, there were errors in reports due to incorrect software logic, e.g., cohort reports need to be censored on specific dates, ignoring all data collected after the censor date. Identifying and working through these complexities was not straightforward and took several iterations to resolve.
Validating the accuracy of EMR data remains challenging. The MoH supervision team observed that personnel operating a paper system for a long time were more inclined to trust paper records if inconsistencies with electronic reports were seen. To allow EMR data to be more easily accessible and provide users with tools for systematic checking, we added a module to allow staff and mentors to perform systematic reviews of patient records, view graphs displaying drug adherence levels, and produce tables showing inconsistent EMR use. Initial feedback by clinic staff and supervisors has been encouraging, emphasizing that provision of EMR monitoring tools is a key requirement for successful implementation.
Conclusions
Implementing a POC EMR has been more challenging than initially anticipated. Many of the technical difficulties have been addressed and resolved in the 8 years of ongoing system development in Malawi. However, the success of a POC system ultimately depends as much on a commitment from system users as on the technologies employed. Poor adherence to system use will result in incomplete data. Supervision is a necessary but insufficient requirement to ensure system use. Health workers will not adopt a system if they do not find sufficient value in it. Consequently, we believe that the primary challenge is to identify and address the value proposition for the user. This is an iterative process that requires a commitment to regular and ongoing dialog with the users if this paradigm shift to POC system use is to be sustainable. We believe that the experience gained, and infrastructure built, through successful deployment of the ART EMR will facilitate further roll-out to other high-burden ART sites in Malawi. We also see great potential for its adaptation and use for other chronic diseases such as tuberculosis, diabetes mellitus, and hypertension, preparing a foundation for a comprehensive electronic health record system.
Supporting Information
Zdroje
1. HarriesAD
SchoutenEJ
MakombeSD
LibambaE
NeufvilleHN
2007 Ensuring uninterrupted supplies of antiretroviral drugs in resource-poor settings: an example from Malawi. Bull World Health Organ 85 152 155
2. HarriesAD
GomaniP
TeckR
AscurraO
BakaliE
2004 Monitoring the response to antiretroviral therapy in resource-poor settings: the Malawi model. Trans R Soc Trop Med Hyg 98 695 701
3. HIV Department, Ministry of Health, Malawi 2010 Quarterly report on the antiretroviral treatment programme in Malawi with results up to 31st December, 2009 Lilongwe Ministry of Health, Malawi
4. ForesterM
BaileyC
BrinkhofM
GraberC
BoulleA
2008 Electronic medical record systems, data quality and loss to follow-up: survey of antiretroviral programmes in resource-limited settings. Bull World Health Organ 86 939 947
5. BoermaT
2005 WHO news. Getting the number right. Bull World Health Organ 83 567 568
6. GodleeF
Pakenham-WalshN
NcayiyanaD
CohenB
PackerA
2004 Can we achieve health information for all by 2015? Lancet 364 295 300
7. Abou-ZahrC
BoermaT
2005 Health information systems: the foundations of public health. Bull World Health Organ 83 578 583
8. TierneyWM
KanterSK
FraserHSF
BaileyC
2010 A toolkit for e-health partnerships in low-income nations. Health Aff 29 268 273
9. FraserHS
JazayeriD
NevilP
KaracaogluY
FarmerPE
2004 An information system and medical record to support HIV treatment in rural Haiti. BMJ 329 1142 1146
10. HannanTJ
RotichJK
OderoWW
MenyaD
EsamaiF
2000 The Mosoriot medical record system: design and initial implementation of an outpatient electronic record system in rural Kenya. Int J Med Inform 21 28
11. TassieJM
BalandineS
SzumilinE
Andrieux-MeyerI
BiotM
2002 FUCHIA: a free computer program for the monitoring of HIV/AIDS medical care at the population level [Abstract C11029]. XIV International AIDS Conference; 7–12 July 2002; Barcelona, Spain
12. JazayeriD
FarmerP
NevilP
MukherjeeJS
LeandreF
2003 An electronic medical record system to support HIV treatment in rural Haiti. AMIA Annu Symp Proc 878
13. MillbergJ
2003 Adapting an HIV/AIDS clinical information system for use in Kampala, Uganda. 44 45 In: Proceedings of the International Medical Informatics Association (IMIA) HELINA (HEaLth INformatics in Africa) Conference in Johannesburg, South Africa
14. SiikaAM
RotichJK
SimiyuCJ
KigothoEM
SmithFE
2005 An electronic medical record system for ambulatory care of HIV-infected patients in Kenya. Int J Med Inform 74 345 355
15. FraserHS
BiondichP
MoodleyD
ChoiS
MamlinBW
2005 Implementing electronic medical record systems in developing countries. Inform Prim Care 13 83 95
16. DouglasGP
KillamWP
HochgesangMS
DeulaRA
LimbeW
2005 Improving completeness, accuracy & timeliness of HIV voluntary counseling & testing client data in Malawi using touchscreen computers. AMIA Annu Symp Proc 2005 942
17. DouglasGP
DeulaRA
2003 Improving the completeness and accuracy of health information through the use of real-time data collection at the point of care. In: Proceedings of the International Medical Informatics Association (IMIA) HELINA (HEaLth INformatics in Africa) Conference in Johannesburg, South Africa
18. DouglasGP
DeulaRA
ConnorSE
2003 The Lilongwe Central Hospital Patient Management Information System: a success in computer-based order entry where one might least expect. AMIA Annu Symp Proc 2003 833
19. DouglasGP
2009 Engineering an EMR system in the developing world: necessity is the mother of invention [PhD dissertation] Pittsburgh (Pennsylvania) University of Pittsburgh
20. DouglasG
McKayM
BwanaliM
GadabuO
MumbaS
2008 A comparison of data captured at point of care versus data captured retrospectively. AMIA Annu Symp Proc 2008 934
21. WatersE
RafterJ
MagangaRT
FraserHSF
DouglasGP
2009 Integration of a touchscreen system for patient registration and primary care data collection with OpenMRS at Neno district hospital, Malawi. AMIA Annu Symp Proc 2009 107
22. LandisLewisZ
DouglasGP
MonacoV
2010 Touchscreen task efficiency and learnability in an electronic medical record at the point-of-care. Medinfo 2010 In press
23. McKayMV
DouglasGP
2008 Touchscreen clinical workstations at point-of-care: a paradigm shift in electronic medical record design for developing countries. 5th IET International Seminar on Appropriate Healthcare Technologies for Developing Countries; 21–22 May 2008; London, United Kingdom
24. WatersE
RafterJ
DouglasGP
BwanaliM
JazayeriD
2010 Experience implementing a point-of-care electronic medical record system for primary care in Malawi. Medinfo 2010 In press
25. FriedmanCP
2009 A “fundamental theorem” of biomedical informatics. J Am Med Inform Assoc 16 169 170
26. BallMJ
SilvaJS
BierstockS
DouglasJV
NorcioAF
2008 Failure to provide clinicians useful IT systems: opportunities to leapfrog current technologies. Methods Inf Med 47 4 7
27. Electronic Data Systems (EDS) Task Force 2007 Responses to the touchscreen system user survey: Queen Elizabeth Central Hospital. Internal report Malawi EDS Task Force, Department for HIV and AIDS, Ministry of Health
28. EDS Task Force 2008 Antiretroviral therapy electronic data system—evaluation & recommendations report Malawi EDS Task Force, Department for HIV and AIDS, Ministry of Health
Štítky
Interní lékařství
Článek vyšel v časopisePLOS Medicine
Nejčtenější tento týden
2010 Číslo 8- Berberin: přírodní hypolipidemikum se slibnými výsledky
- Léčba bolesti u seniorů
- Příznivý vliv Armolipidu Plus na hladinu cholesterolu a zánětlivé parametry u pacientů s chronickým subklinickým zánětem
- Červená fermentovaná rýže účinně snižuje hladinu LDL cholesterolu jako vhodná alternativa ke statinové terapii
- Jak postupovat při výběru betablokátoru − doporučení z kardiologické praxe
-
Všechny články tohoto čísla
- Reducing Malaria Transmission in Africa: A Model-Based Evaluation of Intervention Strategies
- Quantifying the Impoverishing Effects of Purchasing Medicines: A Cross-Country Comparison of the Affordability of Medicines in the Developing World
- Physical Activity Attenuates the Genetic Predisposition to Obesity in 20,000 Men and Women from EPIC-Norfolk Prospective Population Study
- Using Touchscreen Electronic Medical Record Systems to Support and Monitor National Scale-Up of Antiretroviral Therapy in Malawi
- Social Relationships Are Key to Health, and to Health Policy
- Assessing Strategy and Equity in the Elimination of Malaria
- Challenges in Developing Evidence-Based Recommendations Using the GRADE Approach: The Case of Mental, Neurological, and Substance Use Disorders
- Will Cardiovascular Disease Prevention Widen Health Inequalities?
- Moving from Data on Deaths to Public Health Policy in Agincourt, South Africa: Approaches to Analysing and Understanding Verbal Autopsy Findings
- Rapid Scaling Up of Insecticide-Treated Bed Net Coverage in Africa and Its Relationship with Development Assistance for Health: A Systematic Synthesis of Supply, Distribution, and Household Survey Data
- Ecology: A Prerequisite for Malaria Elimination and Eradication
- An Intervention to Reduce HIV Risk Behavior of Substance-Using Men Who Have Sex with Men: A Two-Group Randomized Trial with a Nonrandomized Third Group
- Impact of Community-Based Maternal Health Workers on Coverage of Essential Maternal Health Interventions among Internally Displaced Communities in Eastern Burma: The MOM Project
- The Costs and Underappreciated Consequences of Research Misconduct: A Case Study
- The Effect of Raltegravir Intensification on Low-level Residual Viremia in HIV-Infected Patients on Antiretroviral Therapy: A Randomized Controlled Trial
- Harnessing Health IT for Improved Cardiovascular Risk Management
- PLOS Medicine
- Archiv čísel
- Aktuální číslo
- Informace o časopisu
Nejčtenější v tomto čísle- Using Touchscreen Electronic Medical Record Systems to Support and Monitor National Scale-Up of Antiretroviral Therapy in Malawi
- Physical Activity Attenuates the Genetic Predisposition to Obesity in 20,000 Men and Women from EPIC-Norfolk Prospective Population Study
- Challenges in Developing Evidence-Based Recommendations Using the GRADE Approach: The Case of Mental, Neurological, and Substance Use Disorders
- Reducing Malaria Transmission in Africa: A Model-Based Evaluation of Intervention Strategies
Kurzy
Zvyšte si kvalifikaci online z pohodlí domova
Současné možnosti léčby obezity
nový kurzAutoři: MUDr. Martin Hrubý
Všechny kurzyPřihlášení#ADS_BOTTOM_SCRIPTS#Zapomenuté hesloZadejte e-mailovou adresu, se kterou jste vytvářel(a) účet, budou Vám na ni zaslány informace k nastavení nového hesla.
- Vzdělávání



