-
Články
Top novinky
Reklama- Vzdělávání
- Časopisy
Top články
Nové číslo
- Témata
Top novinky
Reklama- Videa
- Podcasty
Nové podcasty
Reklama- Kariéra
Doporučené pozice
Reklama- Praxe
Top novinky
ReklamaQuantifying the Impoverishing Effects of Purchasing Medicines: A Cross-Country Comparison of the Affordability of Medicines in the Developing World
Background:
Increasing attention is being paid to the affordability of medicines in low - and middle-income countries (LICs and MICs) where medicines are often highly priced in relation to income levels. The impoverishing effect of medicine purchases can be estimated by determining pre - and postpayment incomes, which are then compared to a poverty line. Here we estimate the impoverishing effects of four medicines in 16 LICs and MICs using the impoverishment method as a metric of affordability.Methods and Findings:
Affordability was assessed in terms of the proportion of the population being pushed below US$1.25 or US$2 per day poverty levels because of the purchase of medicines. The prices of salbutamol 100 mcg/dose inhaler, glibenclamide 5 mg cap/tab, atenolol 50 mg cap/tab, and amoxicillin 250 mg cap/tab were obtained from facility-based surveys undertaken using a standard measurement methodology. The World Bank's World Development Indicators provided household expenditure data and information on income distributions. In the countries studied, purchasing these medicines would impoverish large portions of the population (up to 86%). Originator brand products were less affordable than the lowest-priced generic equivalents. In the Philippines, for example, originator brand atenolol would push an additional 22% of the population below US$1.25 per day, whereas for the lowest priced generic equivalent this demographic shift is 7%. Given related prevalence figures, substantial numbers of people are affected by the unaffordability of medicines.Conclusions:
Comparing medicine prices to available income in LICs and MICs shows that medicine purchases by individuals in those countries could lead to the impoverishment of large numbers of people. Action is needed to improve medicine affordability, such as promoting the use of quality assured, low-priced generics, and establishing health insurance systems.
: Please see later in the article for the Editors' Summary
Published in the journal: . PLoS Med 7(8): e32767. doi:10.1371/journal.pmed.1000333
Category: Research Article
doi: https://doi.org/10.1371/journal.pmed.1000333Summary
Background:
Increasing attention is being paid to the affordability of medicines in low - and middle-income countries (LICs and MICs) where medicines are often highly priced in relation to income levels. The impoverishing effect of medicine purchases can be estimated by determining pre - and postpayment incomes, which are then compared to a poverty line. Here we estimate the impoverishing effects of four medicines in 16 LICs and MICs using the impoverishment method as a metric of affordability.Methods and Findings:
Affordability was assessed in terms of the proportion of the population being pushed below US$1.25 or US$2 per day poverty levels because of the purchase of medicines. The prices of salbutamol 100 mcg/dose inhaler, glibenclamide 5 mg cap/tab, atenolol 50 mg cap/tab, and amoxicillin 250 mg cap/tab were obtained from facility-based surveys undertaken using a standard measurement methodology. The World Bank's World Development Indicators provided household expenditure data and information on income distributions. In the countries studied, purchasing these medicines would impoverish large portions of the population (up to 86%). Originator brand products were less affordable than the lowest-priced generic equivalents. In the Philippines, for example, originator brand atenolol would push an additional 22% of the population below US$1.25 per day, whereas for the lowest priced generic equivalent this demographic shift is 7%. Given related prevalence figures, substantial numbers of people are affected by the unaffordability of medicines.Conclusions:
Comparing medicine prices to available income in LICs and MICs shows that medicine purchases by individuals in those countries could lead to the impoverishment of large numbers of people. Action is needed to improve medicine affordability, such as promoting the use of quality assured, low-priced generics, and establishing health insurance systems.
: Please see later in the article for the Editors' SummaryIntroduction
In developing countries the cost of medicines accounts for a relatively large portion of total healthcare costs [1]–[4]. As the majority of people in developing countries do not have health insurance [5] and medicines provided free through the public sector are often unavailable [4], medicines are often paid for out of pocket at the time of illness. Consequently, where medicine prices are high, people may be unable to procure them and therefore forego treatment or they may go into debt. For this reason, the World Health Organization (WHO) has designated affordable prices as a determinant of access to medicines (together with rational selection and use, sustainable financing, and reliable health and supply systems) [6]. In several international treaties, access to healthcare has been established as a right [7],[8]. States have a legal obligation to make essential medicines available to those who need them at an affordable cost. Determining the degree of affordability of medicines, especially in low - and middle-income countries (LICs and MICs), is an important, yet complex undertaking as affordability is a vague concept.
Medicine affordability has been investigated in terms of the days' wages that a country's lowest paid unskilled government worker (LPGW) needs to spend on a standard course of treatment [4],[9]. However, this metric is limited because it does not provide insight into the affordability of medicines for the often large sections of the population that earn less than the LPGW [4],[10]. Recently, Niëns et al. have proposed two alternative methods to gain insight into the affordability of medicines in the developing world [11]. A first method focuses on the catastrophic impact of expenditures on medicines, while the second approach consists of studying the impoverishing effect of these expenditures. Here we discuss the application of the latter approach and present the results of a cross-country analysis of the affordability of four medicines in 16 developing countries.
Methods
Our measurement of the affordability of medicines is based on the approach taken by Van Doorslaer et al. [3], who reassessed poverty estimates in 11 Asian countries after taking into account household expenditures on health care. The impoverishment approach has also been used in other fields of study such as housing affordability [12],[13] and health insurance [14].
The impoverishing effect of a medicine is defined in terms of the percentage of the population that would be pushed below an income level of US$1.25 or US$2 per day when having to purchase the medicine. Although different income levels have been used/proposed [3],[15], the US$1.25 and US$2 poverty lines were chosen because they are the most recent widely recognized poverty indicators as used by the World Bank [16]. Thus, the approach essentially compares households' daily per capita income before and after (the hypothetical) procurement of a medicine. If the prepayment income is above the US$1.25 (or US$2) poverty line and the postpayment income falls below these lines, purchasing the medicine impoverishes people. We used this method to generate “impoverishment rates,” which denote the percentage of the population that would become impoverished. The unaffordability of a medicine then refers to the percentage of the population that either already is or would fall below the poverty line when having to procure the medicine. First we consider the affordability of medicines in the total population at risk of becoming ill. We also indicate, using prevalence rates for the three chronic diseases, the expected number of patients actually affected.
Data
To conduct the first analysis, three types of data were required per country: medicine prices, aggregated income data, and information on the income distribution. In calculating expected numbers of patients affected, prevalence data are also required. Medicine prices were taken from standardized surveys using the WHO/Health Action International (HAI) price measurement methodology, which report median patient prices for a selection of commonly used medicines in the private sector, for both originator brand (OB) and lowest priced generic (LPG) products [17]. We focused on the private sector because the availability of essential medicines in the public sector is much lower [4]. In the countries studied here, therefore, many people will depend on the private sector for their medicines.
The World Bank's World Development Indicators (WDIs) provided Household Final Consumption Expenditure (HHFCE) data and information on income distribution [18]. Although WDIs have shortcomings (highlighted in the Discussion section), they have the advantage of being available for a wide range of countries. Moreover, in this context commonly used household surveys are often not available on a yearly basis and are not conducted in a standardized way, limiting the comparability of results across countries and over time [3],[19]. Here we use an affordability measure that can be quite easily applied in LICs and MICs where the use of more detailed household survey data may be limited.
HHFCE was selected as an aggregate income measure rather than gross domestic product (GDP) per capita as it better reflects households' resources [19], while GDP also includes consumption, gross investment, and net trade. Because the WDI did not provide any information on HHFCE for Nigeria and Yemen, the Economist Intelligence Unit (EIU) nominal private consumption figure was used for these countries [20]. For simplicity, we refer to “income” as measured by HHFCE or nominal private consumption. Apart from average income, the WDIs also provide some information on a country's income distribution by listing the proportion of total income earned in seven income groups; five income quintiles, with the poorest and richest quintiles split into deciles.
At the time of analysis, medicine price surveys were available for 53 countries. In large countries such as India and China, price surveys were carried out on a state or provincial level [4]. Because the WDIs do not provide state-level income distributions, HHFCE, and population figures, these countries were excluded from the current study. To ensure cross-country comparability, the analysis was limited to countries where income distributions (WDI data) were available from the year 2000 onwards. We used WDI income data from the same year as the WHO/HAI price data. Data on income distributions for the same year were used when possible, if not, the most recent income distribution data prior to the year of the price and income data were used.
Table 1 provides an overview of all countries and data used in this study. When discussing results, countries were grouped into LICs and MICs according to the 2008 World Bank's classification [21]. Sixteen countries were selected on the basis of the availability of WHO/HAI data. They are not representative of the developing world as a whole. However, as these countries vary substantially in terms of economic development, health care infrastructure, and medicine prices, they provide an interesting sample to study affordability of medicines.
Tab. 1. Overview of countries studied and years of data sources used. 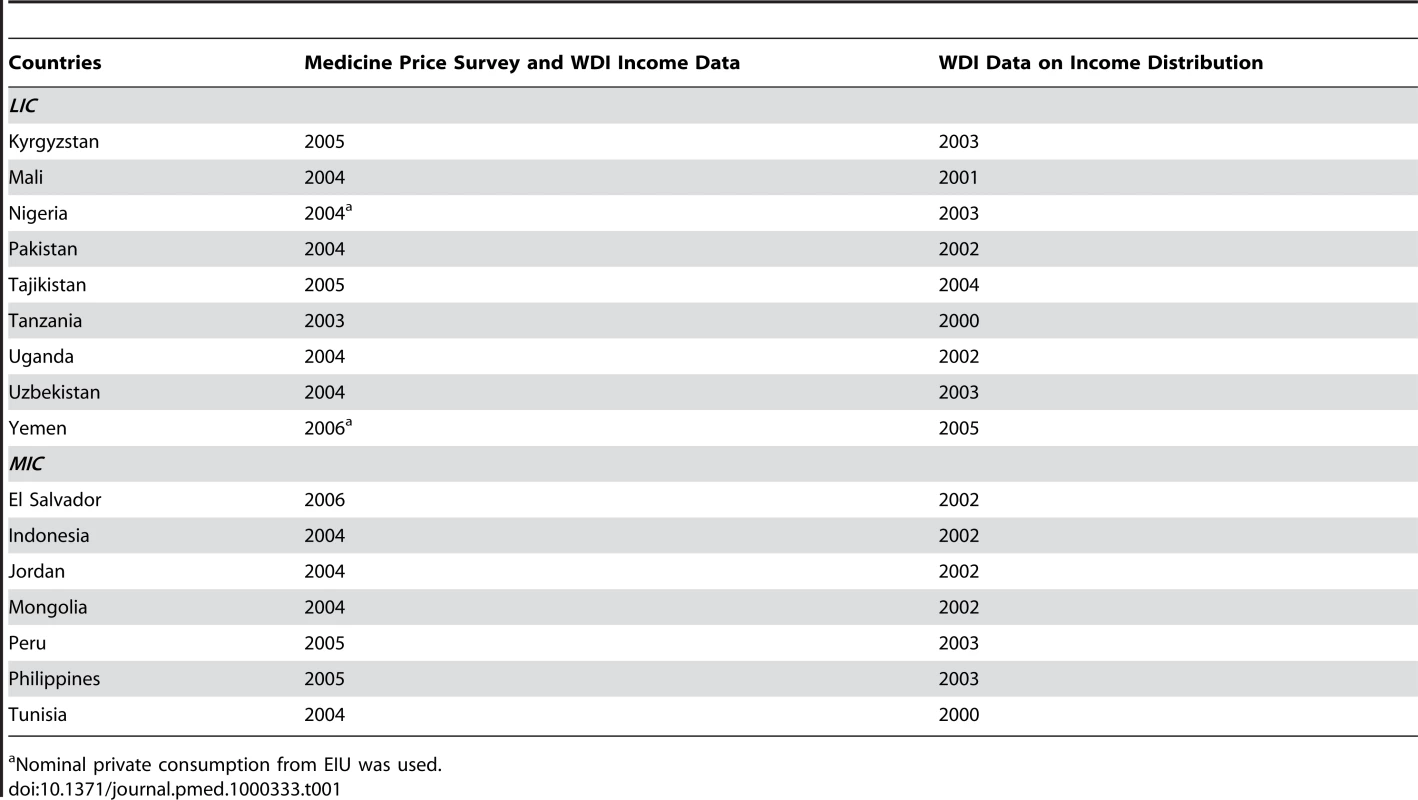
Nominal private consumption from EIU was used. We selected four medicines for which price data were available for the majority of countries and for which treatment regimens are relatively standard across countries. While these may not lead to results that are in a strict sense generalisable, they provide valuable insight into the affordability of common medicines in the selected countries. Table 2 lists the medicine, the ill health conditions for which these medicines are used, the total number of units per treatment course, and the treatment duration in days [17]. Three of the four study medicines are used to treat chronic conditions (asthma, diabetes, and hypertension). For each of these, we also calculated the expected numbers of patients becoming impoverished, using the prevalence data shown in Table S1. We could not do this for adult respiratory infection because of unavailability of comparable prevalence data.
Tab. 2. Description of studied medicines. 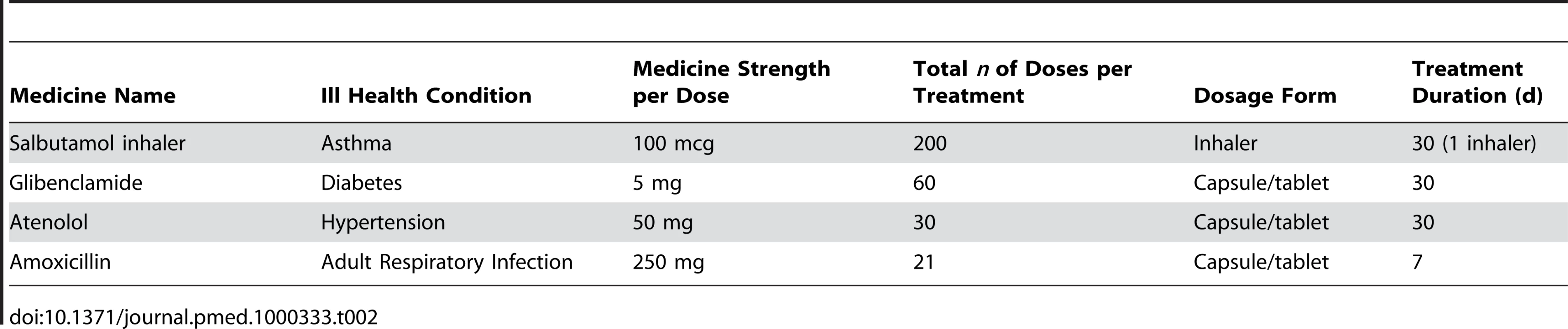
The emphasis on medicines for chronic disease is justified by the fact that these conditions require ongoing, usually lifelong expenditures, making it more difficult for households to use financing strategies like borrowing and selling assets [22]. Table 2 shows that the treatment duration for these medicines was set at 30 d to represent the monthly treatment costs. The affordability of one acute condition (adult respiratory infection) treated with a 7-d treatment course of amoxicillin was also studied. Recently, the WHO increased the guidelines for treatment of adult respiratory infection with amoxicillin to a daily regimen of three times 500 mg amoxicillin. This change implies that the affordability of this medicine is likely to be lower than reported here [23].
Calculation Methods
Our method of estimating the impoverishing effect of procuring medicines was based on the method used by Van Doorslaer et al. [3]. However, using aggregate data requires some simplifying assumptions about the income distribution across population groups. For a detailed discussion of the method used to calculate the impoverishing effect of medicines, we refer to Niëns et al. [11]. The basic idea is to compare poverty estimates before and after a (potential) purchase of the medicines listed in Table 1. Average per capita income within each income group is estimated by combining information on the proportion of total income earned across income groups with data on the HHFCE (as provided by the WDIs). As only data on average income in the different quintiles and deciles were available, we assumed linearity of the income distribution within these relevant groups in which the US$1.25 and US$2 poverty lines were located in calculating poverty and impoverishment. The proportion of the population that would earn less than US$1.25 or US$2 per day after buying a medicine but not before would therefore be impoverished because of purchasing medicines. The medicine is deemed affordable for the proportion of the population that would remain above the poverty line after having purchased it. We also estimated the actual number of patients with one of the three chronic illnesses for which the medicine is unaffordable. To make this estimation, we used prevalence rates from various data sources and again assume that the respective disease is evenly spread over the income distribution.
Because HHFCE is measured in current US$, we recalculated the US$1.25 and US$2 poverty lines to US$ values for the HAI/WHO survey year. HAI/WHO medicine prices were expressed in US$ for the same year.
Results
Table 3 presents the percentages of the population that are pushed below the poverty line owing to the purchasing of each of the four study medicines, both LPG and OB products.
Tab. 3. Percentage of the population below the poverty line before procurement of the medicines and the population drawn below the poverty line by expenditures on these medicines. 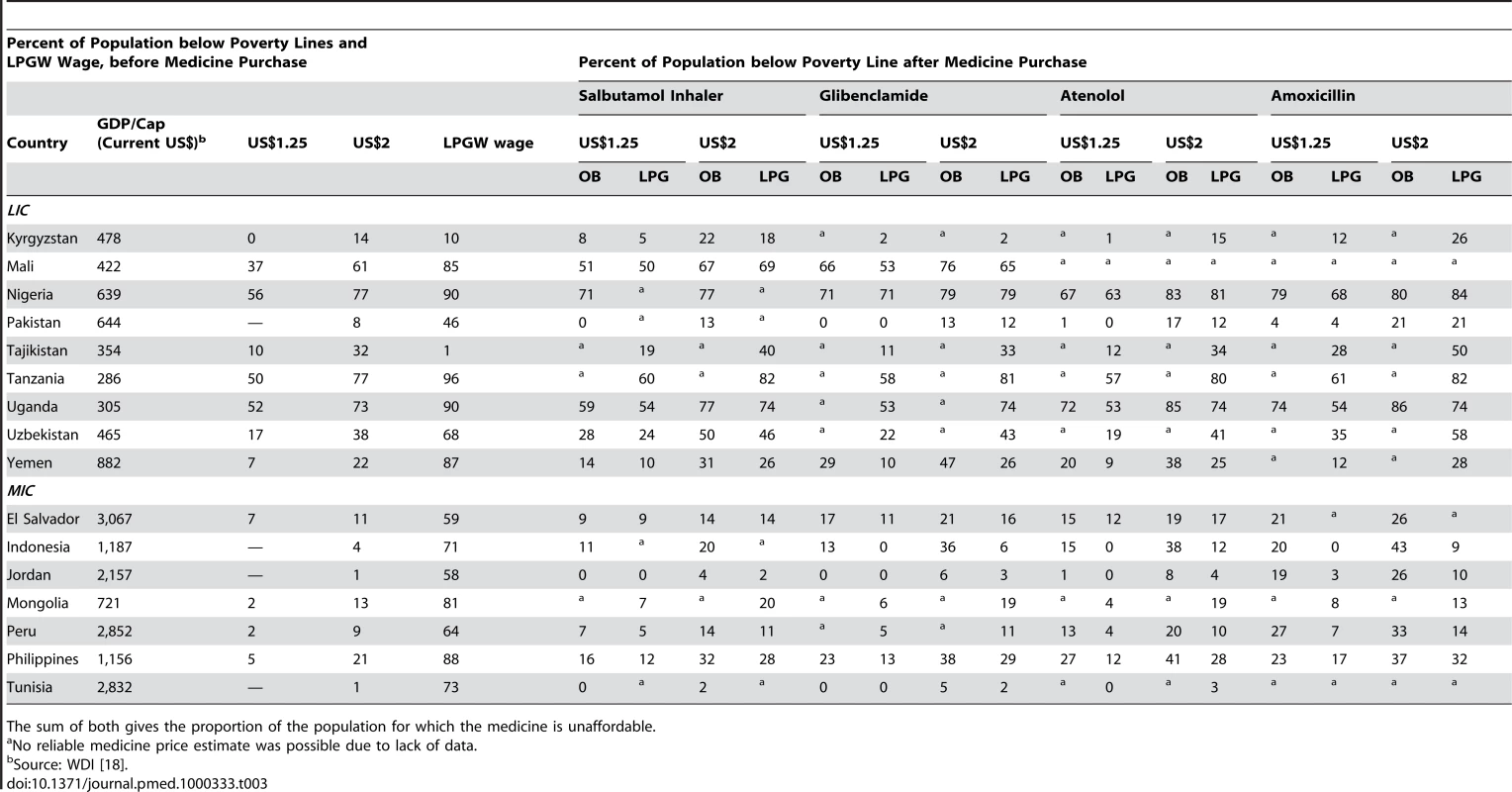
The sum of both gives the proportion of the population for which the medicine is unaffordable. For each country, Table 3 first highlights the proportion of the population already below the US$1.25 and US$2 poverty lines without purchasing these medicines. These poverty estimates correlate highly with the commonly used (household-survey based) estimates from the United Nations Development Program with Pearson correlation coefficients [24] equal to 0.90 for the proportion of the population below the US$1.25 poverty line, and 0.86 for the proportion below the US$2 poverty line. Table 3 also shows the proportion of the population earning less than the LPGW, which varies widely across countries; from only 1% in Tajikistan to 96% in Tanzania. This cross-country variability represents one of the limitations of the LPGW metric as used by the WHO/HAI methodology [9].
Comparing the proportion of the population below the US$1.25 and US$2 poverty lines before and after procurement of medicines gives insight into the impoverishing effect of medicine procurement. By adding the proportion of the population already living below the US$1.25 and US$2 poverty lines to the group that would fall below these poverty lines when procuring the medicines, we get the proportion of the population for which the four medicines are unaffordable.
The results in Table 3 illustrate that the impoverishing effect of medicines varies substantially between OB and LPG products. For example in Yemen, a LIC where 7% of the population lives on a prepayment income of less than US$1.25 a day, OB glibenclamide purchased in the private sector would impoverish an additional 22% of the population versus 3% for the LPG equivalent. In Nigeria, a LIC where 56% of the population lives below US$1.25 per day, purchasing amoxicillin from the private sector would impoverish an additional 23% if the OB is bought and 12% if buying the LPG.
Rather than showing proportions of the population, Table 4 presents both the absolute number of individuals that would be pushed into poverty owing to the cost of buying medicines from the private sector (“Impoverished” column) and the number of people for which medicines are unaffordable (“Unaffordable” column). Besides absolute figures, in Table 5 we present the relative change of the poverty estimates for the total population studied as well as for the patient population. So, if 40% of the population is initially above the poverty line, while only 30% would remain above after purchasing medicines, this proportion is 25% (10% out of 40% are impoverished). These numbers are listed for all four medicines, both OB and LPG. The total population of the 16 countries analyzed amounts to over 775 million people, of which approximately 126 million live on less than US$1.25 and 209 million on less than US$2 per day, respectively. Table 4 illustrates that across this set of 16 developing countries, for respectively almost one-fourth and two-fifths of the total population, essential medicines are unaffordable using the US$1.25 and US$2 poverty line.
Tab. 4. Absolute impoverishment and unaffordability estimates of medicines procured in the private sector for the total and chronic patient populations across 16 countries (rounded to millions). 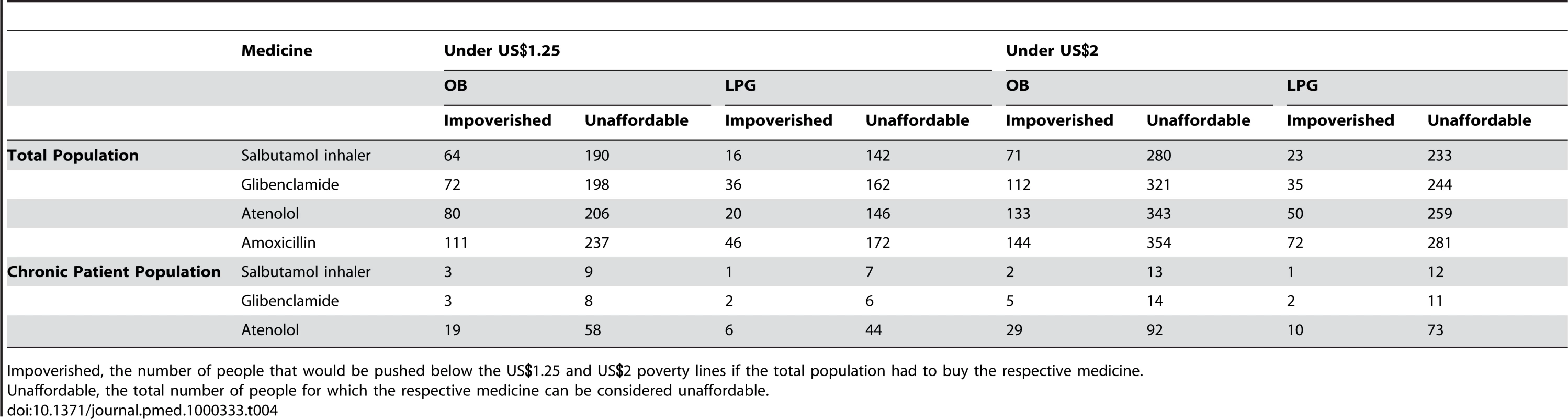
Impoverished, the number of people that would be pushed below the US.25 and US poverty lines if the total population had to buy the respective medicine. Tab. 5. The relative change of the poverty estimates (i.e., the impoverished population expressed as a proportion of the population initially above the poverty line). 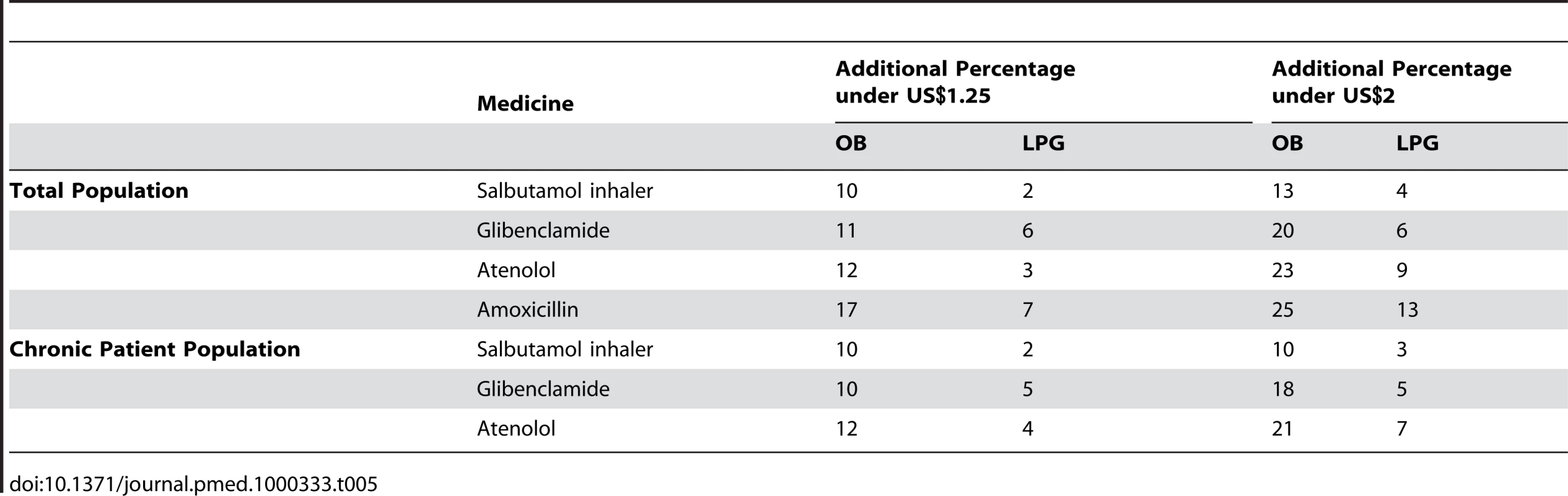
The upper half of Table 4 shows the proportions of the total population for which medicines would be unaffordable when having to procure them. The actual number of people affected by this unaffordability (in terms of experiencing the disease) depends on the prevalence of diseases as well. Therefore, the lower half of Table 4 also shows the expected absolute number of patients affected by the unaffordability of medicines using the prevalence rates listed in Table S1. As the prevalence rates of hypertension are substantially higher than those of asthma and diabetes, the impoverishing effect, and therefore also the unaffordability, of atenolol is substantially higher than that for the other medicines. In this approach, given the height and distribution of income, impoverishment is determined by both medicine prices and prevalence rates for the relevant diseases.
Discussion
The results illustrate that substantial proportions of the population would be pushed into poverty as a result of medicine procurement, implying that in many countries affordability of these treatments is low. In the private sector, LPGs were generally substantially more affordable than OB products. Thus, increasing the use of quality-assured generics could reduce the impoverishing effect of medicines. This use of generics, in turn, could bring about improvements in the health status of these populations by avoiding low compliance to recommended dosages or duration of treatment, resulting in problems such as sustained hypertension, elevated blood glucose levels, or the promotion of bacterial resistance due to too short courses of antibiotics.
Our calculation method has the advantage of allowing for comparisons of medicine-induced impoverishment across time and across countries using widely available aggregate data. The method, therefore, is useful and generalisable for studying the affordability of a wide range of goods and health care services. The use of such data also brings some limitations, which are discussed in further detail in Niëns et al. [11]. First, dividing HHFCE by total population to get an estimate of income per capita assumes that each household is the same size. However, poor households are generally larger than their richer counterparts [25]. This discrepancy causes the average income per capita to be overestimated in the lower income groups, making our affordability estimates rather conservative. Second, the assumption of linearity of the income distribution between income groups is also likely to lead to an overestimation of average incomes across the income distribution and therefore to a downward bias in our results. We also assumed a linear distribution of illness over the income distribution to calculate expected numbers of affected people. Although, in general, disease may be more prevalent in low income groups, which would imply conservative estimates of unaffordability, this also depends on the exact diseases studied. Moreover, it is clear that considering only medicine costs, for four medicines independently, merely demonstrates the larger problem of medicine and health care affordability. The treatment of chronic conditions often requires a combination of medicines and is therefore likely to be even more unaffordable than what is reported here [4]. For chronic asthma patients, for example, appropriate management of their disease requires use of both salbutamol and beclometasone inhalers for treatment and prevention [17]. Due to the lack of available price information on beclometasone inhalers (because of poor availability), it was not possible to include this medicine in the analysis. As such, the true affordability of asthma treatment is likely to be lower than reported in Tables 3 and 4. Having said this, the medicines studied in this paper are commonly used to treat ill health conditions from which considerable proportions of the population in the developing world suffer, as is also illustrated in Table S1 [26]. As such, low affordability of these medicines is likely to signal a more general problem of low affordability of medicines in LIC and MIC. Further, it should be noted that comparability of impoverishment rates for acute and chronic conditions may be limited. If people suffer from an adult respiratory infection, on average three times per year, and are able to shift resources over time, the impoverishment rates for amoxicillin should be interpreted with caution. Further research is needed on this issue, for example by calculating affordability for standardized time periods taking into account the relevant incidence rates of respiratory infections.
Notwithstanding these limitations, this study provides useful insights into the affordability of these four medicines in the developing world. When medicine prices are known, the methods used, as they rely on easily obtainable aggregated data, can be used to compare affordability of medicines across countries and over time. Clearly, medicines represent only a part of the costs associated with the management of an illness. Other costs, such as for diagnostics, physician consultations, transport costs to clinics, lost work time, etc., place an additional burden on household finances in developing countries. However, given the relatively large share of health care costs for medicines in developing countries [1]–[4], medicine affordability is likely to be an important determinant to access to treatment.
This study shows high medicine costs can push large groups of patients into poverty. These results call for action, both by governments, civil society organizations, and others, to make access to essential medicines a priority, and not only to ensure access to necessary medicines, but also as a component in the context of reducing poverty. Possible lines of action include developing, implementing, and enforcing sound national and international price policies. In the short term these policies could encompass, for example, restrictions on supply chain mark-ups, tax exemptions, and regulating prices for end-users. Promoting the use of quality-assured, low-cost generics, for example, through preferential registration procedures, is also an important strategy [4]. In the public sector, ensuring availability of essential medicines at little or no charge to the poor is critical. In the longer term, establishing health insurance systems with outpatient medicine benefits seems crucial to avoid poverty due to health shocks (and poor health due to poverty). Innovative approaches, such as using private distribution systems to supply subsidized medicines to chronic disease patients, should also be considered. For medicines that are still subject to patent restrictions, pharmaceutical companies should be encouraged to differentially price these products, as is the case with antiretrovirals [27]. Countries also have the option of using compulsory licensing to oblige patent holders to grant its use to the state or others [28], as was recently done by Thailand [29],[30].
When resources are limited, those in greatest need, such as people suffering from chronic disease who earn less than US$1.25 per day, should benefit from state and/or donor actions. The price in terms of health losses due to unaffordable medicines is something we cannot afford.
Supporting Information
Zdroje
1. World Health Organization 2000 Global comparative pharmaceutical expenditures with related reference information. Health Economics and Drugs EDM Series No. 3 Geneva World Health Organization
2. World Health Organization 2004 WHO medicines strategy 2004–2007 - countries at the core. Available: http://www.who.int/medicinedocs/collect/medicinedocs/pdf/s5416e/s5416e.pdf Accessed 28 April 2009
3. van DoorslaerE
O'DonnellO
Rannan-EliyaRP
SomanathanA
AdhikariSR
2006 Effect of payments for health care on poverty estimates in 11 countries in Asia: an analysis of household survey data. Lancet 368 1357 1364
4. CameronA
EwenM
Ross-DegnanD
BallD
LaingR
2009 Medicine prices, availability, and affordability in 36 developing and middle-income countries: a secondary analysis. Lancet 373 240 249
5. DrorDM
PrekerAS
JakabM
2002 The role of communities in combating social exclusion.
DrorDM
PrekerAS
Social reinsurance - a new approach to sustainable community health financing Washington (D.C.); Geneva The World Bank Group and the International Labour Office
6. World Health Organization 2008 Access to medicines. Available: http://www.who.int/trade/glossary/story002/en/ Accessed 22 April 2009
7. United Nations 1948 The universal declaration of human rights, article 25. Available: http://www.un.org/Overview/rights.html#a25. Accessed 22 April 2009
8. United Nations 1966 International covenant on economic, social and cultural rights, article 12. Geneva. Available: http://www.unhchr.ch/html/menu3/b/a_cescr.htm. Accessed 22 April 2009
9. World Health Organization, Health Action International 2008 Measuring medicine prices, availability, affordability and price components – 2nd edition Geneva World Health Organization
10. NiënsLM
BrouwerWB
2009 Better measures of affordability required. Lancet 373 1081 author reply 1081–1082
11. NiënsLM
Van de PoelE
CameronA
EwenM
LaingR
2009 Practical measurement of affordability: an application to medicines Rotterdam Institute of Health Policy and Management, Erasmus University Working Paper W2009.02
12. HancockKE
1993 ‘Can pay? won't pay?’ or economic principles of ‘Affordability’. Urban Stud 30 127 145
13. KuttyNK
2005 A new measure of housing affordability: estimates and analytical results. Hous Policy Debate 16 113 142
14. BundorfMK
PaulyMV
2006 Is health insurance affordable for the uninsured? J Health Econ 25 650 673
15. ChenS
RavallionM
2008 The developing world is poorer than we thought, but no less successful in the fight against poverty Washington (D.C.) Development Research Group, The World Bank Group
16. The World Bank Group. Available: http://go.worldbank.org/C9GR27WRJ0. Accessed 10 January 2010
17. Health Action International. Medicine prices. Available: http://www.haiweb.org/medicineprices/. Accessed 5 March 2009
18. The World Bank Group. World development indicators. Available: http://publications.worldbank.org/WDI/. Accessed 12 March 2009
19. O'DonnellO
van DoorslaerE
WagstaffA
LindelowM
2008 Analyzing health equity using household survey data – A guide to techniques and their implementation Washington (D.C.) The World Bank Group
20. The Economist. The economist intelligence unit. Available: http://www.eiu.com/. Accessed 2 April 2009
21. The World Bank Group. Country groups. Available: http://go.worldbank.org/D7SN0B8YU0. Accessed 16 March 2009
22. FloresG
KrishnakumarJ
O'DonnellO
van DoorslaerE
2008 Coping with health-care costs: implications for the measurement of catastrophic expenditures and poverty. Health Econ 17 1393 1412
23. World Health Organization 2008 WHO model formulary. Available: http://www.who.int/selection_medicines/list/WMF2008.pdf. Accessed 27 August 2009
24. United Nations Development Program 2008 Human development report 2007/2008. Available: http://hdr.undp.org/en/media/HDR_20072008_Tables.pdf. Accessed 19 February 2009
25. LiptonM
RavaillonM
1994 Povert and policy.
BehrmanJ
SrinivasanTN
Handbook of development economics Amsterdam: Elsevier
26. World Health Organization 2004 Global burden of disease - 2004 update. Available: http://www.who.int/healthinfo/global_burden_disease/2004_report_update/en/index.html. Accessed 12 February 2010
27. WaningB
KaplanW
KingAC
LawrenceDA
LeufkensHG
2009 Global strategies to reduce the price of antiretroviral medicines: evidence from transactional databases. Bull World Health Organ 87 520
28. World Health Organization 2006 Public health innovation and intellectual property rights. report of the commission on intellectual property rights, innovation, and public health Geneva World Health Organization
29. SeimL
2007 Thailand: government issues compulsory licences for HIV/AIDS drugs. HIV AIDS Policy Law Rev 12 28 29
30. FordN
WilsonD
Costa ChavesG
LotrowskaM
KijtiwatchakulK
2007 Sustaining access to antiretroviral therapy in the less-developed world: lessons from brazil and Thailand. AIDS (London) 21 S21 S29
Štítky
Interní lékařství
Článek vyšel v časopisePLOS Medicine
Nejčtenější tento týden
2010 Číslo 8- Berberin: přírodní hypolipidemikum se slibnými výsledky
- Léčba bolesti u seniorů
- Příznivý vliv Armolipidu Plus na hladinu cholesterolu a zánětlivé parametry u pacientů s chronickým subklinickým zánětem
- Červená fermentovaná rýže účinně snižuje hladinu LDL cholesterolu jako vhodná alternativa ke statinové terapii
- Jak postupovat při výběru betablokátoru − doporučení z kardiologické praxe
-
Všechny články tohoto čísla
- Reducing Malaria Transmission in Africa: A Model-Based Evaluation of Intervention Strategies
- Quantifying the Impoverishing Effects of Purchasing Medicines: A Cross-Country Comparison of the Affordability of Medicines in the Developing World
- Physical Activity Attenuates the Genetic Predisposition to Obesity in 20,000 Men and Women from EPIC-Norfolk Prospective Population Study
- Using Touchscreen Electronic Medical Record Systems to Support and Monitor National Scale-Up of Antiretroviral Therapy in Malawi
- Social Relationships Are Key to Health, and to Health Policy
- Assessing Strategy and Equity in the Elimination of Malaria
- Challenges in Developing Evidence-Based Recommendations Using the GRADE Approach: The Case of Mental, Neurological, and Substance Use Disorders
- Will Cardiovascular Disease Prevention Widen Health Inequalities?
- Moving from Data on Deaths to Public Health Policy in Agincourt, South Africa: Approaches to Analysing and Understanding Verbal Autopsy Findings
- Rapid Scaling Up of Insecticide-Treated Bed Net Coverage in Africa and Its Relationship with Development Assistance for Health: A Systematic Synthesis of Supply, Distribution, and Household Survey Data
- Ecology: A Prerequisite for Malaria Elimination and Eradication
- An Intervention to Reduce HIV Risk Behavior of Substance-Using Men Who Have Sex with Men: A Two-Group Randomized Trial with a Nonrandomized Third Group
- Impact of Community-Based Maternal Health Workers on Coverage of Essential Maternal Health Interventions among Internally Displaced Communities in Eastern Burma: The MOM Project
- The Costs and Underappreciated Consequences of Research Misconduct: A Case Study
- The Effect of Raltegravir Intensification on Low-level Residual Viremia in HIV-Infected Patients on Antiretroviral Therapy: A Randomized Controlled Trial
- Harnessing Health IT for Improved Cardiovascular Risk Management
- PLOS Medicine
- Archiv čísel
- Aktuální číslo
- Informace o časopisu
Nejčtenější v tomto čísle- Using Touchscreen Electronic Medical Record Systems to Support and Monitor National Scale-Up of Antiretroviral Therapy in Malawi
- Physical Activity Attenuates the Genetic Predisposition to Obesity in 20,000 Men and Women from EPIC-Norfolk Prospective Population Study
- Challenges in Developing Evidence-Based Recommendations Using the GRADE Approach: The Case of Mental, Neurological, and Substance Use Disorders
- Reducing Malaria Transmission in Africa: A Model-Based Evaluation of Intervention Strategies
Kurzy
Zvyšte si kvalifikaci online z pohodlí domova
Současné možnosti léčby obezity
nový kurzAutoři: MUDr. Martin Hrubý
Všechny kurzyPřihlášení#ADS_BOTTOM_SCRIPTS#Zapomenuté hesloZadejte e-mailovou adresu, se kterou jste vytvářel(a) účet, budou Vám na ni zaslány informace k nastavení nového hesla.
- Vzdělávání



