-
Články
Top novinky
Reklama- Vzdělávání
- Časopisy
Top články
Nové číslo
- Témata
Top novinky
Reklama- Videa
- Podcasty
Nové podcasty
Reklama- Kariéra
Doporučené pozice
Reklama- Praxe
Top novinky
ReklamaImproving Newborn Survival in Low-Income Countries: Community-Based Approaches and Lessons from South Asia
article has not abstract
Published in the journal: . PLoS Med 7(4): e32767. doi:10.1371/journal.pmed.1000246
Category: Policy Forum
doi: https://doi.org/10.1371/journal.pmed.1000246Summary
article has not abstract
Summary Points
-
Reducing global neonatal mortality is crucial. In low-income countries, most births and deaths occur at home.
-
Obstacles to improving survival include: many newborn infants are invisible to health services; care-seeking for maternal and newborn ailments is limited; health workers are often not skilled and confident in caring for newborn infants; and there are inequalities across all these factors.
-
The best community-based approach is a combination of community mobilization and home visits by community-based workers. Both timing of visits and treatment interventions are critical.
-
It is not clear how community-based approaches should be balanced, and whether they are effective outside South Asia and when introduced into public sector systems. Operational challenges include integrating community-based activities into public health systems, and questions of how to achieve coverage at scale.
-
The possibility of partnership between the public and nongovernment sectors should be explored, particularly in terms of novel large-scale collaborations.
The Scale of the Problem
Until about twenty years ago, child survival meant the survival of children rather than newborn infants. With a steady worldwide decline in under-5 deaths—most of the lives saved being those of infants and children over the age of a month—the newborn period has come into focus as a relatively intransigent source of mortality. The “child survival revolution” increased child survival [1], but newborn infants went largely unnoticed. Neonatal mortality (0–28 d) now accounts for about two-thirds of global infant (0–1 y) mortality and about 3.8 million of the 8.8 million annual deaths of children under 5 [2]. Most of these deaths (98%) occur in low - and middle-income countries [3].
The last two decades have seen a rise in advocacy—a call for attention to the newborn infant along with her mother and siblings—and an incremental growth in the evidence for potential interventions [4]–[6]. Reducing neonatal mortality is both an ethical obligation and a prerequisite to achieving Millennium Development Goal 4, the target of which is a reduction in child mortality by two-thirds between 1990 and 2015. A 2008 report found only a quarter of relevant countries on track to reach this target [7].
Immediate Challenges
The main obstacles to improving newborn survival are that many babies are born at home without skilled attendance, care-seeking for maternal and newborn ailments is limited, health workers are often not skilled and confident in caring for newborn infants, and inequalities in all these factors are felt by those most in need.
Home Births and Limited Access to Care
In low-income settings, most babies are born at home and more than half of those who die do so at home. Three-quarters of neonatal deaths occur in the first week, and just under half in the first 24 h [3]. In South Asia and East and Southern Africa, only about 35% of births take place in institutions [8]. The newborn infant has traditionally occupied a transitional space between potential and actual personhood, and seclusion practices add to the likelihood that he or she will be invisible to health professionals. If care is sought, it is often in the traditional sector and beset by obstacles such as the notion that mother and baby are polluted, which may entail seclusion and cause delay in care-seeking. Access to allopathic (“Western” or biomedical) health services is limited by lack of facilities, human resources, equipment, and consumables.
There are four general ways of addressing this: improving the provision and quality of institutional health care, extending institutional care through community outreach, stimulating demand for appropriate health care and institutional delivery through community engagement and perhaps financial incentives, and changing ideas and behaviour by working with communities. These approaches are far from mutually exclusive and should be joined up [9].
Content of Health Care
The three commonest causes of neonatal deaths are infections (28%), complications of prematurity (30%), and intrapartum-related (“birth asphyxia”) (24%) [2]. Unfortunately, health workers may lack the skills and experience necessary to act appropriately. Basic resuscitation skills and knowledge may be limited, and there is a pervasive idea that intervention needs to be highly technical. This is not generally true. As early as 1905, Budin recommended resuscitation, warmth, early and frequent breastfeeding, keeping the baby with his or her mother, hygiene, and prompt recognition and treatment of illness [10]. Contemporary recommendations for “essential newborn care” follow this blueprint [11],[12]. The Lancet's series on neonatal survival suggested that between 41% and 72% of neonatal deaths could be averted if 16 simple, cost-effective interventions were delivered with universal coverage. Among these are adequate nutrition, improved hygiene, antenatal care, skilled birth attendance, emergency obstetric and newborn care, and postnatal visits for mothers and infants [13].
Inequity
Newborn survival increases with wealth. In India, for example, neonatal mortality is 56 per 1,000 in the poorest quintile, but 25 in the richest [14]. Such inequality is evident no matter how the population is segmented: by education, ethnicity, migrant status, or occupation [15]. In many countries, the responsibility to provide health care for poorer people falls on the public sector. As wealthier members of society move steadily towards private sector care, the burden of care for increasing numbers of poor people falls on already overstretched national public health systems.
What Is Meant by Community Intervention?
Figure 1 summarises both the components of health care that have been recommended to improve newborn survival and the range of delivery strategies that have been proposed, tested, or introduced. More detail can be found in a recent set of systematic reviews on intrapartum-related deaths [16]–[20]. Pregnancy is just one stage of a woman's life, and the figure reminds us that it may occur on a background of gender inequality. Inadequate education, nutrition, and care for childhood illness have short - and long-term effects that are not limited to women (although the burdens often fall on them, as do young age at marriage and conception, short birth intervals, and undesirably large families).
Fig. 1. Maternity as a life event, components of care with potential effects on newborn survival, and 11 possible delivery strategies. 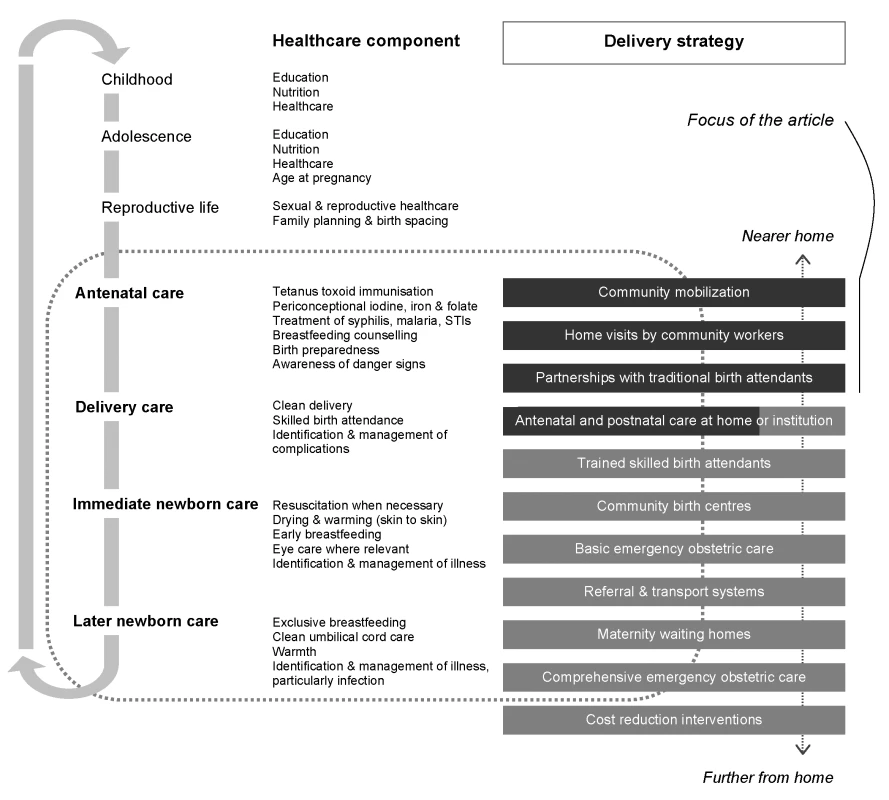
The figure locates intervention strategies in terms of their proximity to a woman's home. Some approaches deserve fuller comment than we can give here. Antenatal care is, and should remain, a feature of health care systems. It allows contact between women and health workers and strengthens the likelihood of birth preparedness and institutional delivery. It may identify certain remediable issues, and although its effectiveness in terms of general risk reduction is debated [21],[22], it can be delivered in the home. The same is true of postnatal care, and both phases of ambulatory care are included in community-based interventions. Training skilled birth attendants is central to current efforts to improve maternal outcomes and is included in health plans in many low-income countries. However, the rate of output is limited and unlikely to answer demand in the next 10 y [23]. Linked with this is the provision of skilled intrapartum care at primary health care centres, which is the focus of recommendations for maternal survival [24]. Both transport and referral remain problematic in many countries.
The issue is not only geographical movement between health care institutions but also realisation that a problem exists and communication and decision-making for referral. A maternity waiting home is a residence near a hospital to which women at risk move shortly before delivery or if complications arise [25]. The benefits have not been demonstrated conclusively, risk screening may be of limited use, and community acceptance varies, but waiting homes are an option in some settings and a strategy adopted in Cuba, for example. Cost reduction is an overarching means of stimulating demand for health services [26]. Strategies include the removal of user fees [27], conditional cash transfers for use of services [28], and insurance schemes.
All the potential approaches serve communities, but we will focus on the beginning of the sequence close to home (highlighted in Figure 1), in which the essential feature is not primarily institutional. We do so in response to a number of recent research programs—most of them successful and all of them originating in low-income countries—and the incorporation of their findings into national and international guidelines. It is true that community-driven approaches fall somewhat outside the prevailing health sector paradigm (in reality if not in principle), but they raise important questions about integration, which we will discuss later. Table 1 summarises published controlled trials in which the interventions under test included one or more of three broad strategies: community mobilization initiatives, programmes that involved home visits by community-based workers, and partnerships with traditional birth attendants (TBAs).
Tab. 1. Components of interventions and key features of controlled trials of community-based approaches to improve newborn survival. 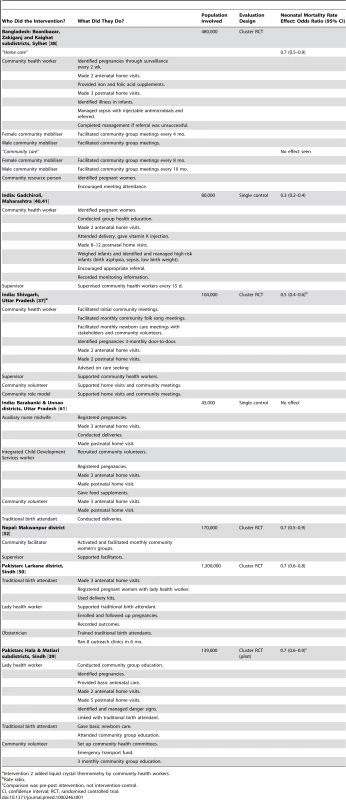
Intervention 2 added liquid crystal thermometry by community health workers. Community Mobilization
All the suggested approaches to improving newborn survival involve a degree of community mobilization. While general community development programmes may improve newborn survival, our experience in India and Nepal suggests that survival-focused interventions may reduce neonatal mortality rates even more efficiently. Here we emphasise programs in which work with communities to identify problems and solutions is a specific strategy to increase newborn survival. The idea that communities can develop insight into and solutions for their own problems has a long history and social and political implications [29],[30]. A stimulus for newborn survival initiatives came from Bolivia's Warmi program, which worked with rural Aymara women's groups to identify local opportunities and develop strategies to improve maternal and newborn health [31]. Groups moved through a cycle of discussions that encompassed sharing of experiences, internalising new information, prioritising, strategising, action, and evaluation. In a modified version of this process, in rural Nepal, a cluster randomised trial suggested that women's groups facilitated by a local female community worker—trained in facilitation techniques but without a health care background—could reduce neonatal mortality rates by about 30% [32]. There were behaviour changes in, for example, hygienic practices and care-seeking for problems, and also strategic initiatives such as maternal and child health funds and transport schemes. Seventy-five percent of groups remained active 18 mo after withdrawal of program support. The model is being tested with rural groups in Bangladesh [33], India [34], and Malawi [35] and in urban slums in India [36]. Group work, not necessarily confined to women, and with varying degrees of intensity, was also a feature of other successful programs [37],[38],[39].
Home Visits by Community Workers
Aside from the benefits of group-based discursive approaches, a growing number of programs have shown that targeted home visits by community-based workers can help reduce newborn mortality. The idea developed over some years in rural Maharashtra, India, where the nongovernment organisation (NGO), the Society for Education, Action and Research in Community Health (SEARCH) trained community health workers to conduct group health education, identify pregnant women and make antenatal care visits to their homes, attend delivery, give vitamin K injections, make several further postnatal home visits, identify and manage infants at risk from birth asphyxia, low birth weight and sepsis, and encourage appropriate referral. This seminal model gradually reduced neonatal mortality by 70% [40],[41].
Like most successful local initiatives, the SEARCH approach developed incrementally in the context of a commitment to community development and included a range of activities. The most prominent were regular visits to women and their newborn infants by a cadre of community-based women trained and remunerated by SEARCH. These local nongovernment workers were able to give advice and identify and treat neonatal problems, their skills extending to resuscitation and administration of intramuscular antibiotics. Since then, trials of home-based care have been conducted in North India [37], Bangladesh [38], and Pakistan [39] (summarised along with other key work in Table 1). Strategies differed in personnel and content. All the programs included community meetings, antenatal and postnatal home visits, and preventive advice. The Hala program included referral [39], as did the Projahnmo program, which also included curative care [35]. Strategies were also implemented by different cadres of workers. The Shivgarh strategy involved community health workers remunerated by the program and local volunteers [37]; the Projahnmo strategy involved NGO community health workers and mobilisers [38]; and the Hala strategy involved government Lady Health Workers, TBAs, and community volunteers.
Most of the programs showed improvements in care: increased uptake of antenatal care, some increase in institutional delivery (although this was not a primary feature of any program), and better performance on indicators of essential newborn care. Further evaluations are underway in South and Southeast Asia (Bangladesh, India, Nepal, Pakistan, and Vietnam) and sub-Saharan Africa (Ethiopia, Ghana, Malawi, Mali, Mozambique, South Africa, Tanzania, and Uganda), and WHO and UNICEF now recommend home visits in the first week of life by appropriately trained and supervised health workers [42].
Partnerships with Traditional Birth Attendants
About 60 million infants are delivered outside institutions annually, 23%–40% of them by TBAs [19], women who deliver babies in the community, with or without clinical training [43]. The idea of bringing TBAs into the allopathic fold by upgrading their skills and connecting them with health services has had a chequered history. Included in programs from the time of Alma Ata [44],[45], subsequent review led to the virtual abandonment of TBA training, or at least a modification of their role from care providers to link-workers [46],[47]. Recent reviews suggest that traditional attendants could have a role in increasing newborn survival [45],[48],[49], and a controlled trial in rural Pakistan found a 30% reduction in neonatal mortality when they were linked systematically with government community health workers and obstetric services [50]. There is also evidence that infants could be saved if TBAs had some skills in managing birth asphyxia, for example [51].
Five Things That We Need to Know
The Correct Balance of Supply and Demand Intervention
No attempt to address newborn deaths in the home will be successful if it does not reach the household and align with the aspirations of family members [52]–[54]. How much of the agenda should be community-driven, and how much should be predefined by health sector inputs, is still not clear. At one extreme, Nepal's Makwanpur trial worked through women's group discussions and the resulting interventions were left to community members to decide [32]. Maharashtra's SEARCH program involved a portfolio of interventions developed over several years (training of TBAs, home visits by community health workers, identification of illness, and administration of oral and parenteral antibiotics). Perceptions of the most important intervention differ according to the commentator. For some, the key issue was the provision of injectable antimicrobials by community-based workers (perhaps responsible for 30%–40% of the mortality reduction) [55]. For others, the essential transformation was due to the longevity of the program and the commitment of its cadres, driven by deeply held beliefs about community rights and action. Both must have played a part, and community group work has (rightly, we think) been included in all successful programs for newborn care. India's Shivgarh trial made community mobilization integral to the intervention, while in Bangladesh's Projahnmo trial, group activities were limited to visits made by female community mobilisers every 4 mo. The former trial showed an effect and the latter did not; integration and coverage seem to be important.
What Is Needed Outside South Asia
All the major trials of community interventions for newborn survival have so far been in South Asia. Their commonalities are more striking than their differences: rural setting, female literacy at around 40%, home delivery rates over 80%, skilled birth attendance below 15%, and public sector health care systems based on the primary health care model. Africa needs more attention, not least because the pattern of mortality may be different. Low birth weight—a key contributor to neonatal mortality in South Asia—is much less common in African countries, and post-neonatal mortality claims a greater share of under-5 deaths [56]. We hope that the operational research and trials underway in African countries, mentioned above, will answer some of the questions about whether strategies are both feasible and effective on another continent.
How to Fit Components into Systems
It is possible to think about community interventions in at least three ways: as a series of activities that need to be delivered (“package”), as a framework for delivery (“system”), or as a means of galvanising communities for change (“mobilization”). The 16 recommended newborn care practices are best seen as a package of activities, and there have been recent attempts to refine its content: antenatal care and birth preparedness, institutional delivery if possible, hygiene, early wiping and wrapping of the infant (but delayed bathing), early and exclusive breastfeeding, skin-to-skin contact between mother and infant, and recognition and appropriate treatment when danger signs appear [57]. What is required is integration of family, community, health system outreach and institutional care, and also of maternal, newborn, child, adolescent, and women's health care into a systemic continuum [8],[57]–[59]. Examining individual components is not the same as evaluating the effects of delivering them within complex systems. A recent review found no true effectiveness trials conducted at scale in health systems and few studies approximating complete packages; current evidence was “a weak foundation for guiding effective implementation of public health programmes addressing neonatal health,” and the reviewers called for new effectiveness trials tailored to local health needs and conducted at scale in developing countries [60].
Whether Workers Can Cope with the Intensity Demanded
Programs have worked so far with institutional cadres, community-based workers, and volunteers. In some cases the community-based workers were a new cadre [32],[37],[38],[40],[41], while in others they were drawn from existing public sector cadres [39],[50],[61]. As Table 1 shows, programs have usually involved more than one of these groups. Once a precedent is set—often a portfolio of activities—the options for less intensive approaches become questionable. Several of the model programs required at least two home visits during pregnancy, a visit on the day of birth, and at least three postnatal home visits [38],[39],[40],[41]. It is not clear how much pruning models would stand and still remain effective. Given the importance of the first days after birth to neonatal mortality, perhaps dropping the later postnatal visits would not compromise the outcomes [37],[50],[61]. In a recent joint statement, WHO and UNICEF recommend a minimum of two visits, in the first 24 h and on the third day [42].
Most programs involve an increased workload for community cadres and a substantial contribution from volunteers. While existing community-based health workers may achieve more job satisfaction from clearly delineated activities and support, increased workloads may be challenging, particularly because of the requirement for extensive field activities. Haines and colleagues have described problems in instituting focused tasks, adequate remuneration, training, and supervision in large-scale community health-worker programs [62]. Less than 15% of children born at home in five South Asian and sub-Saharan African countries were visited by a trained health worker within 3 d of birth. Speed of reaction and mobility might also be obstacles: a community health worker, perhaps living in a different village, must know about a woman's pregnancy or be informed of the birth and must then be willing and able to make repeated postnatal visits to check for warning signs in mother and baby and to treat or refer promptly. It is hard to know if this will happen, particularly since these activities have been part of the augmented surveillance systems for some trials [37],[38]. Villages are heterogeneous, and vulnerable marginalized groups may be less likely to be visited at home when programs expand beyond trial models with more rigorous supervision.
Coverage at Scale
Successful model programs need to be replicated, scaled up, and sustained. Although cost is usually a prime concern in this sort of discussion, it has not so far been a major obstacle. The interventions proposed are relatively inexpensive and could be integrated with existing systems [23],[58]. It is health systems integration that raises questions. Child survival is unequivocally important, and several countries have developed newborn care policies. Government partners are involved in operational research in Bangladesh, India, Indonesia, Nepal, Vietnam, Ethiopia, Malawi, Mali, Mozambique, Bolivia, and Guatemala (Saving Newborn Lives/Save the Children, personal communication). In Nepal, the NGO Mother and Infant Research Activities (MIRA) has embarked on a large trial in which NGO-employed facilitators of women's groups are replaced by existing female community health volunteers. SEARCH has supported two pilot scale-up programs, one mediated through NGOs at seven sites in Maharashtra (ANKUR) and one nested within the public health systems of five states (Indian Council of Medical Research field trial). The findings of the Shivgarh trial have been integrated into Uttar Pradesh's child survival program, and home-based newborn care has been included in both the Government of India's Reproductive and Child Health (RCH-II) strategy and the Integrated Management of Newborn and Child Illness.
Putting aside the issues of the content of programs and the continuum of care, the main challenge is to achieve the required levels of community mobilization and home visits by community-based workers. As with many public health interventions, it is the least accessible groups (geographically, socially, financially) who have the most problems and for whom outreach is most likely to be compromised if corners are cut. Only 13% of women who deliver at home in developing countries make a postnatal care visit [63]. The first priority is for community newborn survival interventions to be included in public sector health services. Here we face a tacit assumption that programs spearheaded by NGOs will not be viable or scalable; that the inertia of health systems will thwart efforts to build community linkages and generate enthusiasm and conscientiousness. Partnerships between the government and third (nongovernment) sectors could help. The success of NGOs in Bangladesh, for example, has been unprecedented in the country, with nationwide reach for organisations such as BRAC (www.brac.net) and private not-for-profit organisations such as the Diabetic Association of Bangladesh (www.dab-bd.org). Savings and credit initiatives have led to the creation and sustenance of thousands of community groups across Asia, many of them run by and for women. Cross-system linkage has been difficult, and one of the central agendas is to evaluate the possibilities of collaboration between sectors so that health care systems are integrated rather than parallel. Clearly, government needs to be involved in creating an enabling environment for such movements, perhaps only insofar as endorsement, but preferably through collaboration and policy. For example, India's National Rural Health Mission, which will work through community-based Accredited Social Health Activists (ASHAs), represents an opportunity for creative cross-sectoral partnership.
The Next Stage
There is little doubt that community interventions for newborn survival work in principle. In our opinion, the key questions are now more about the medium than the message: how effective simplified program designs might be, whether they are relevant in African contexts, whether they will be as effective as they appear, and how they could be rolled out and sustained. Research now needs to move from components to the operational realities of systems [60],[64]. Some major questions remain: the optimal population coverage of community-based workers, since coverage, we think, is crucial for success, and does require investment in community mobilization [65],[66], the requirements for selection of workers and their remuneration or compensation [41], and the right mix of existing and new cadres [12]. A particular challenge is how to integrate newborn and maternal survival interventions [67]. For governments the choice of approach should almost certainly focus on defining the roles and responsibilities of existing cadres in reaching out to women who deliver at home with an essential newborn care package. This is not simply a matter of training health workers, since it is the marginalised and hard to reach who are most at risk. Women's groups represent a valuable community resource that already exists in many areas and may have inbuilt sustainability. We see active involvement of individuals and communities as the key to achieving targeted coverage of poor and marginalized families to bring down neonatal mortality, and this is an opportunity for governments to facilitate community mobilization in partnership with civil society organisations.
Box. Five Things That We Need to Know
-
The correct balance of supply and demand intervention
-
What is needed outside South Asia
-
How to fit components into systems
-
Whether workers can cope with the intensity demanded
-
Coverage at scale
Zdroje
1. SchuftanC
1990 The Child Survival Revolution: a critique. Fam Pract 7 329 332
2. LawnJ
KerberK
Enweronu-LaryeaC
BatemanM
2009 Newborn survival in low resource settings - are we delivering? BJOG 116 Suppl 1 S49 S59
3. LawnJ
CousensS
ZupanJ
for the Lancet Neonatal Survival Steering Team 2005 4 million neonatal deaths: When? Where? Why? Lancet 365 891 900
4. Saving Newborn Lives 2001 State of the world's newborns. Washington DC Save the Children
5. DarmstadtG
LawnJ
CostelloA
2003 Advancing the state of the world's newborns. Bull World Health Organ 81 224 225
6. NNF 2004 The state of India's newborns. New Delhi & Washington DC National Neonatology Forum & Save The Children US
7. UNICEF 2008 Countdown to 2015: tracking progress in maternal, newborn and child survival. New York United Nations Children's Fund
8. UNICEF 2008 The state of the world's children 2009: maternal and newborn health. New York United Nations Children's Fund
9. KidneyE
WinterHR
KhanKS
GulmezogluAM
MeadsCA
2009 Systematic review of effect of community-level interventions to reduce maternal mortality. BMC Pregnancy Childbirth 9 2
10. BudinP
1907 The nursling. The feeding and hygiene of premature & full-term infants. Translation by WJ Maloney. London The Caxton Publishing Company
11. WHO 1996 Essential newborn care. Report of a technical working group (Trieste, 25–29 April 1994). WH0/FRH/MSM/96.13. Geneva World Health Organization, Division of Reproductive Health (Technical Support)
12. BhuttaZ
DarmstadtG
HasanB
HawsR
2005 Community-based interventions for improving perinatal and neonatal health outcomes in developing countries: a review of the evidence. Pediatrics 115 519 617
13. DarmstadtG
BhuttaZ
CousensS
AdamT
WalkerN
2005 Evidence-based, cost-effective interventions: how many newborn babies can we save? Lancet 365 977 988
14. Macro International Inc 2009 MEASURE DHS STATcompiler. Calverton, MD ICF Macro
15. HouwelingT
KunstA
2010 Socio-economic inequalities in childhood mortality in low and middle income countries: a review of the international evidence. Br Med Bull 93 7 26
16. LawnJ
LeeA
KinneyM
SibleyL
CarloW
2009 Two million intrapartum-related stillbirths and deaths: where, why, and what can be done? Int J Gynecol Obstet 107 S5 S19
17. WallS
LeeA
NiermeyerS
EnglishM
KeenanW
2009 Neonatal resuscitation in low-resource settings: what, who, and how to overcome challenges to scale up? Int J Gynecol Obstet 107 S47 S64
18. LeeA
LawnJ
CousensS
KumarV
OsrinD
2009 Linking families and facilities for care at birth: what works to avert intrapartum-related deaths? Int J Gynecol Obstet 107 S65 S88
19. DarmstadtG
LeeA
CousensS
SibleyL
BhuttaZ
2009 60 million non-facility births: who can deliver in community settings to reduce intrapartum-related deaths? Int J Gynecol Obstet 107 S89 S112
20. LawnJ
KinneyM
LeeA
ChopraM
DonnayF
2009 Reducing intrapartum-related deaths and disability: can the health system deliver? Int J Gynecol Obstet 107 S123 S142
21. CarroliG
RooneyC
VillarJ
2001 WHO programme to map the best reproductive health practices: how effective is antenatal care in preventing maternal mortality and serious morbidity? Paediatr Perinatal Epidemiol 15 Suppl 1 1 42
22. JaddoeV
2009 Antenatal education programmes: do they work? Lancet 374 863 864
23. KnippenbergR
LawnJ
DarmstadtG
BegkoyianG
FogstadH
2005 Systematic scaling up of neonatal care in countries. Lancet 365 1087 1098
24. CampbellO
GrahamW
2006 Strategies for reducing maternal mortality: getting on with what works. Lancet 368 1284 1299
25. WHO 1996 Maternity waiting homes: a review of experiences. Geneva World Health Organization
26. BorghiJ
EnsorT
SomanathanA
LissnerC
MillsA
2006 Mobilising financial resources for maternal health. Lancet 468 1457 1465
27. Korkor AnsahE
Narh-BanaS
AsiamahS
DzordzordziV
BianteyK
2009 Effect of removing direct payment for health care on utilisation and health outcomes in Ghanaian children: a randomised controlled trial. PLoS Med 6 e1000007 doi:10.1371/journal.pmed.1000007
28. LagardeM
HainesA
PalmerN
2007 Conditional cash transfers for improving uptake of health interventions in low - and middle-income countries: a systematic review. JAMA 298 1900 1910
29. FreireP
1995 Pedagogy of hope: reliving pedagogy of the oppressed. New York Continuum International Publishing Group
30. TaylorCE
1995 E.H. Christopherson Lecture: lessons for the United States from the worldwide Child Survival Revolution. Pediatrics 96 342 346
31. Howard-GrabmanL
SeoaneG
DavenportC
MotherCare and Save the Children 2002 The Warmi Project: a participatory approach to improve maternal and neonatal health, an implementor's manual. Westport John Snow International, Mothercare Project, Save the Children
32. ManandharD
OsrinD
ShresthaB
MeskoN
MorrisonJ
2004 Effect of a participatory intervention with women's groups on birth outcomes in Nepal: cluster randomized controlled trial. Lancet 364 970 979
33. BarnettS
AzadK
BaruaS
MridhaM
AbrarM
2006 Maternal and newborn-care practices during pregnancy, childbirth, and the postnatal period: a comparison in three rural districts in Bangladesh. J Health Popul Nutr 24 394 402
34. BarnettS
NairN
TripathyP
BorghiJ
RathS
2008 A prospective key informant surveillance system to measure maternal mortality - findings from indigenous populations in Jharkhand and Orissa. BMC Pregnancy and Childbirth 8
35. RosatoM
MwansamboC
KazembeP
PhiriT
SokoQ
2006 Women's groups' perceptions of maternal health issues in rural Malawi. Lancet 368 1180 1188
36. Shah MoreN
BapatU
DasS
PatilS
PorelM
2008 Cluster-randomised controlled trial of community mobilisation in Mumbai slums to improve care during pregnancy, delivery, postpartum and for the newborn. Trials 9 7
37. KumarV
MohantyS
KumarA
MisraR
SantoshamM
2008 Effect of community-based behaviour change management on neonatal mortality in Shivgarh, Uttar Pradesh, India: a cluster-randomised controlled trial. Lancet 372 1151 1162
38. BaquiAH
El-ArifeenS
DarmstadtGL
AhmedS
WilliamsEK
2008 Effect of community-based newborn-care intervention package implemented through two service-delivery strategies in Sylhet district, Bangladesh: a cluster-randomised controlled trial. Lancet 371 1936 1944
39. BhuttaZA
MemonZA
SoofiS
SalatMS
CousensS
2008 Implementing community-based perinatal care: results from a pilot study in rural Pakistan. Bull World Health Organ 86 452 459
40. BangA
BangR
BaituleS
ReddyM
DeshmukhM
1999 Effect of home-based neonatal care and management of sepsis on neonatal mortality: field trial in rural India. Lancet 354 1955 1961
41. BangAT
BangRA
ReddyHM
2005 Home-based neonatal care: summary and applications of the field trial in rural Gadchiroli, India (1993 to 2003). J Perinatol 25 Suppl 1 S108 S122
42. WHO, UNICEF 2009 WHO/UNICEF Joint Statement: home visits for the newborn child: a strategy to improve survival. WHO/FCH/CAH/09.02. Geneva and New York World Health Organization and United Nations Children's Fund
43. SibleyL
SipeT
KoblinskyM
2004 Does traditional birth attendant training improve referral of women with obstetric complications: a review of the evidence. Soc Sci Med 59 1757 1768
44. WHO 1992 Traditional birth attendants. a joint WHO/UNICEF/UNFPA statement. Geneva World Health Organization, United Nations Children's Fund, United Nations Fund for Populatino Activities
45. SibleyLM
SipeTA
2006 Transition to skilled birth attendance: is there a future role for trained traditional birth attendants? J Health Popul Nutr 24 472 478
46. MaineD
1990 Safe motherhood programs: options and issues. New York Center for Population and Family Health, Columbia University
47. WHO 2004 Beyond the numbers. Reviewing maternal deaths and complications to make pregnancy safer. Geneva Department of Reproductive Health and Research, World Health Organization
48. SibleyL
SipeT
2004 What can a meta-analysis tell us about traditional birth attendant training and pregnancy outcomes? Midwifery 20 51 60
49. SibleyLM
SipeTA
BrownCM
DialloMM
McNattK
2007 Traditional birth attendant training for improving health behaviours and pregnancy outcomes. Cochrane Database Syst Rev. CD005460 p
50. JokhioA
WinterH
ChengK
2005 An intervention involving traditional birth attendants and perinatal and maternal mortality in Pakistan. N Engl J Med 352 2091 2099
51. SinghalN
BhuttaZ
2008 Newborn resuscitation in resource-limited settings. Semin Fetal Neonatal Med 13 432 439
52. WinchP
AlamM
AktherA
AfrozD
AliN
2005 Local understandings of vulnerability and protection during the neonatal period in Sylhet district, Bangladesh: a qualitative study. Lancet 366 478 485
53. Neonatal Mortality Formative Research Working Group 2008 Developing community-based intervention strategies to save newborn lives: lessons learned from formative research in five countries. J Perinatol 28 Suppl 2 S2 S8
54. WaiswaP
KemigisaM
KiguliJ
NaikobaS
PariyoGW
2008 Acceptability of evidence-based neonatal care practices in rural Uganda - implications for programming. BMC Pregnancy Childbirth 8 21
55. BangAT
ReddyHM
DeshmukhMD
BaituleSB
BangRA
2005 Neonatal and infant mortality in the ten years (1993 to 2003) of the Gadchiroli field trial: effect of home-based neonatal care. J Perinatol 25 Suppl 1 S92 S107
56. LawnJ
CostelloA
MwansamboC
OsrinD
2007 Countdown to 2015: will the Millennium Development Goal for child survival be met? Arch Dis Child 92 551 556
57. KerberKJ
de Graft-JohnsonJE
BhuttaZA
OkongP
StarrsA
2007 Continuum of care for maternal, newborn, and child health: from slogan to service delivery. Lancet 370 1358 1369
58. DarmstadtGL
WalkerN
LawnJE
BhuttaZA
HawsRA
2008 Saving newborn lives in Asia and Africa: cost and impact of phased scale-up of interventions within the continuum of care. Health Policy Plan 23 101 117
59. BhuttaZ
AliS
CousensS
AliT
HaiderB
2008 Interventions to address maternal, newborn, and child survival: what difference can integrated primary health care strategies make? Lancet 372 972 989
60. HawsRA
ThomasAL
BhuttaZA
DarmstadtGL
2007 Impact of packaged interventions on neonatal health: a review of the evidence. Health Policy Plan 22 193 215
61. BaquiA
WilliamsEK
RosecransAM
AgrawalPK
AhmedS
2008 Impact of an integrated nutrition and health programme on neonatal mortality in rural northern India. Bull World Health Organ 86 796 804, A
62. HainesA
SandersD
LehmannU
RoweAK
LawnJE
2007 Achieving child survival goals: potential contribution of community health workers. Lancet 369 2121 2131
63. FortA
KothariM
AbderrahimN
2006 Postpartum care: levels and determinants in developing countries. Maryland Macro International Inc
64. CostelloA
FilippiV
KubbaT
HortonR
2007 Research challenges to improve maternal and child survival. Lancet 369 1240 1243
65. BryceJ
TerrerriN
VictoraC
MasonE
DaelmansB
2006 Countdown to 2015: tracking intervention coverage for child survival. Lancet 368 1067 1076
66. JohnsB
SigurbjornsdottirK
FogstadH
ZupanJ
MathaiM
2007 Estimated global resources needed to attain universal coverage of maternal and newborn health services. Bull World Health Organ 85 256 263
67. HofmeyrG
HawsR
BergstromS
LeeA
OkongP
2009 Obstetric care in low-resource settings: what, who, and how to overcome challenges to scale up? Int J Gynecol Obstet 107 S21 S45
Štítky
Interní lékařství
Článek Economic Appraisal of Ontario's Universal Influenza Immunization Program: A Cost-Utility AnalysisČlánek The Effect of Rural-to-Urban Migration on Obesity and Diabetes in India: A Cross-Sectional Study
Článek vyšel v časopisePLOS Medicine
Nejčtenější tento týden
2010 Číslo 4- Berberin: přírodní hypolipidemikum se slibnými výsledky
- Léčba bolesti u seniorů
- Příznivý vliv Armolipidu Plus na hladinu cholesterolu a zánětlivé parametry u pacientů s chronickým subklinickým zánětem
- Červená fermentovaná rýže účinně snižuje hladinu LDL cholesterolu jako vhodná alternativa ke statinové terapii
- Jak postupovat při výběru betablokátoru − doporučení z kardiologické praxe
-
Všechny články tohoto čísla
- Economic Appraisal of Ontario's Universal Influenza Immunization Program: A Cost-Utility Analysis
- The Effect of Rural-to-Urban Migration on Obesity and Diabetes in India: A Cross-Sectional Study
- Preoperative/Neoadjuvant Therapy in Pancreatic Cancer: A Systematic Review and Meta-analysis of Response and Resection Percentages
- Association between the 2008–09 Seasonal Influenza Vaccine and Pandemic H1N1 Illness during Spring–Summer 2009: Four Observational Studies from Canada
- China's Engagement with Global Health Diplomacy: Was SARS a Watershed?
- Laboratory Capacity Building in Asia for Infectious Disease Research: Experiences from the South East Asia Infectious Disease Clinical Research Network (SEAICRN)
- Mortality Measurement Matters: Improving Data Collection and Estimation Methods for Child and Adult Mortality
- Brazil and the Framework Convention on Tobacco Control: Global Health Diplomacy as Soft Power
- Health Diplomacy and the Enduring Relevance of Foreign Policy Interests
- Measuring Under-Five Mortality: Validation of New Low-Cost Methods
- What Can We Conclude from Death Registration? Improved Methods for Evaluating Completeness
- Improving Newborn Survival in Low-Income Countries: Community-Based Approaches and Lessons from South Asia
- Does Seasonal Influenza Vaccination Increase the Risk of Illness with the 2009 A/H1N1 Pandemic Virus?
- Measuring Adult Mortality Using Sibling Survival: A New Analytical Method and New Results for 44 Countries, 1974–2006
- Early Emergence of Ethnic Differences in Type 2 Diabetes Precursors in the UK: The Child Heart and Health Study in England (CHASE Study)
- Comparative Effectiveness Research: Challenges for Medical Journals
- Alternative Strategies to Reduce Maternal Mortality in India: A Cost-Effectiveness Analysis
- PLOS Medicine
- Archiv čísel
- Aktuální číslo
- Informace o časopisu
Nejčtenější v tomto čísle- Preoperative/Neoadjuvant Therapy in Pancreatic Cancer: A Systematic Review and Meta-analysis of Response and Resection Percentages
- Economic Appraisal of Ontario's Universal Influenza Immunization Program: A Cost-Utility Analysis
- China's Engagement with Global Health Diplomacy: Was SARS a Watershed?
- Laboratory Capacity Building in Asia for Infectious Disease Research: Experiences from the South East Asia Infectious Disease Clinical Research Network (SEAICRN)
Kurzy
Zvyšte si kvalifikaci online z pohodlí domova
Současné možnosti léčby obezity
nový kurzAutoři: MUDr. Martin Hrubý
Všechny kurzyPřihlášení#ADS_BOTTOM_SCRIPTS#Zapomenuté hesloZadejte e-mailovou adresu, se kterou jste vytvářel(a) účet, budou Vám na ni zaslány informace k nastavení nového hesla.
- Vzdělávání



