-
Články
Top novinky
Reklama- Vzdělávání
- Časopisy
Top články
Nové číslo
- Témata
Top novinky
Reklama- Videa
- Podcasty
Nové podcasty
Reklama- Kariéra
Doporučené pozice
Reklama- Praxe
Top novinky
ReklamaSerological Profiling of a Protein Microarray Reveals Permanent Host-Pathogen Interplay and Stage-Specific Responses during Candidemia
Candida albicans in the immunocompetent host is a benign member of the human microbiota. Though, when host physiology is disrupted, this commensal-host interaction can degenerate and lead to an opportunistic infection. Relatively little is known regarding the dynamics of C. albicans colonization and pathogenesis. We developed a C. albicans cell surface protein microarray to profile the immunoglobulin G response during commensal colonization and candidemia. The antibody response from the sera of patients with candidemia and our negative control groups indicate that the immunocompetent host exists in permanent host-pathogen interplay with commensal C. albicans. This report also identifies cell surface antigens that are specific to different phases (i.e. acute, early and mid convalescence) of candidemia. We identified a set of thirteen cell surface antigens capable of distinguishing acute candidemia from healthy individuals and uninfected hospital patients with commensal colonization. Interestingly, a large proportion of these cell surface antigens are involved in either oxidative stress or drug resistance. In addition, we identified 33 antigenic proteins that are enriched in convalescent sera of the candidemia patients. Intriguingly, we found within this subset an increase in antigens associated with heme-associated iron acquisition. These findings have important implications for the mechanisms of C. albicans colonization as well as the development of systemic infection.
Published in the journal: . PLoS Pathog 6(3): e32767. doi:10.1371/journal.ppat.1000827
Category: Research Article
doi: https://doi.org/10.1371/journal.ppat.1000827Summary
Candida albicans in the immunocompetent host is a benign member of the human microbiota. Though, when host physiology is disrupted, this commensal-host interaction can degenerate and lead to an opportunistic infection. Relatively little is known regarding the dynamics of C. albicans colonization and pathogenesis. We developed a C. albicans cell surface protein microarray to profile the immunoglobulin G response during commensal colonization and candidemia. The antibody response from the sera of patients with candidemia and our negative control groups indicate that the immunocompetent host exists in permanent host-pathogen interplay with commensal C. albicans. This report also identifies cell surface antigens that are specific to different phases (i.e. acute, early and mid convalescence) of candidemia. We identified a set of thirteen cell surface antigens capable of distinguishing acute candidemia from healthy individuals and uninfected hospital patients with commensal colonization. Interestingly, a large proportion of these cell surface antigens are involved in either oxidative stress or drug resistance. In addition, we identified 33 antigenic proteins that are enriched in convalescent sera of the candidemia patients. Intriguingly, we found within this subset an increase in antigens associated with heme-associated iron acquisition. These findings have important implications for the mechanisms of C. albicans colonization as well as the development of systemic infection.
Introduction
The yeast Candida albicans exists in a dichotomist relationship with the human host. C. albicans is frequently found as a commensal organism on the human skin, gastrointestinal (GI) tract and the vulvovaginal tract [1]. Close to 60% of healthy individuals carry C. albicans as a commensal in the oral cavity. Colonic and rectal colonization is even higher, ranging from 45% to 75% among patient groups. Alterations in the host immunity, physiology, or normal microflora rather than the acquisition of novel or hypervirulent factors associated with C. albicans, are suggested to lead to the development of candidiasis [2]. Both neutrophils and mucosal integrity of the GI tract, are critical in preventing hematogenously disseminated candidiasis [3]. The development of candidemia can begin with the translocation of C. albicans into the bloodstream from initial commensal GI colonization or the shedding from developing biofilms on indwelling catheters [4],[5]. Fungal cells that evade the host immune system can spread to deep organ systems leading to hematogenously disseminated candidiasis, which has an estimated mortality rate of 40%, even with the use of antifungal drugs [2].
Information on in vivo gene expression would provide insight into how C. albicans interacts with host cells during the transition from commensal colonization to an opportunistic pathogen in the immunocompromised host. However, in vivo transcription profiling of C. albicans during commensal colonization or candidemia is technically challenging [6]. Instead, several genome-wide transcriptional analyses of C. albicans responses to host cells have been performed using ex vivo and in vivo infection models. These include phagocytosis of C. albicans cells by neutrophils [7] and macrophages [8], exposure to human blood, plasma, and blood cells [9],[10], as well as invasion of perfused pig liver and reconstituted human epithelium [11],[12]. Genes that are associated with morphological changes, metabolic adaptation, and oxidative stress are the major responses of C. albicans to host cells identified in these studies. The changes in gene expression identified in these in vitro model systems possibly reflect tissue - or stage-specific expression during an infection in patients. Profiling of antibody responses during infection in patients offers an alternative approach that can overcome technical challenges of in vivo transcription profiling. An antibody-based approach has been used to identify C. albicans gene expression during thrush in individuals with HIV [13].
Currently the isolation of C. albicans from blood cultures is the standard method for the diagnosis of candidemia. Nevertheless, blood cultures may only become positive late in infection, and in one study up to 50% of all autopsy-proven cases of candidemia were reported as negative in blood cultures [14]. Thus, the ability to rapidly and easily diagnose candidiasis is urgently needed. An alternative approach to microbiological confirmation of C. albicans infection is serological diagnosis. An immunoproteomic approach using two-dimensional electrophoresis followed by quantitative Western blotting and mass spectrometry has been used to profile serologic response to peptides from cell surface extracts in candidemia [15]–[17]. A significant proportion of antigens identified were glycolytic enzymes and heat shock proteins. An antigenic multiplex consisting of the peptides Bgl2, Eno1, Pgk1, Met6, Gap1, and Fba1 provides 87% sensitivity and 74% specificity when distinguishing patients with candidemia from uninfected hospital patients [17]. However, this approach has several limitations; only the most abundant and soluble proteins can be resolved on the immunoblot, there is a lack of reproducibility of cell wall preparations, and most importantly, there is the inability to account for various stage - and tissue-specific gene expressions from the cultured cells. These limitations can be addressed by using a protein microarray to profile antibody responses [18]–[21].
To investigate the establishment of the humoral immunity during commensal sensitization, as well as the adaptive immune response to candidemia, we have developed a C. albicans cell surface protein microarray. Our rationale in developing a cell surface protein microarray is that the cell surface of C. albicans is the immediate target of the human immune system when C. albicans cells enter the bloodstream. Cell surface proteins play important roles in host interaction, and many of them are known virulence factors. In addition, a recent study showed that there is a significant expansion of cell wall, secreted and transporter gene families in pathogenic Candida species in comparison to non-pathogenic yeasts [22]. In this study, profiling of serological response on the protein microarray with sera from candidemia patients, blood-culture negative hospital patients and healthy individuals lead to the identification of serological signature specific for acute and convalescent stages of candidemia. Intriguingly, large proportions of the identified antigens are involved in oxidative stress, drug resistance and iron acquisition. Furthermore, strong IgG response to many proteins known to be induced and/or required for C. albicans invasion of epithelial and endothelial cells is observed in both candidemia patients and non-candidemia controls, including all healthy individuals. Our findings provide new insights into commensal colonization and pathogenesis of C. albicans, as well as the characterization of potential serodiagnostic antigens and vaccine candidates.
Results
Sera collection and study population
Hospital patient sera were collected from Shands Hospital at the University of Florida (UF) (SH-UF) from January 2004 to December 2006. We collected sera from 21 patients with candidemia where the etiological agent was C. albicans. The median time from the date of positive culture to serum collection was two days. The study population was classified by age, gender, underlying disease, portal of entry, antifungal received, and outcome of stay (Table S1). A subset of the candidemia patients was followed through acute infection (days 0–14) to early convalescent (week 4) and mid convalescent (week 12) infection. We also used sera from 12 hospital patients and 50 healthy individuals who had no evidence of candidiasis as our negative control groups.
C. albicans cell surface protein microarray construction and hybridization
C. albicans cell surface proteins were chosen for the protein microarray because they interact directly with the host and thus are likely important for colonization and infection, as well as likely targets for the host immune system. Furthermore, many of their protein expression levels are regulated in response to extracelluar signals, such as stress, nutrients, host factors, or changes in environment. Known antigenic proteins are also included as controls (Bgl2, Eno1, Pgk1, Gap1, Cdc19, Tkl1, Hsp90, and members of the Hsp70 family) [15],[17]. The collection contains 451 His - and HA-tagged peptides (Table S2) that represent 363 different proteins, since ORFs >3,000 bps were cloned into two or more segments. All tagged proteins were confirmed individually by western blot and again on the protein microarray.
We have used the C. albicans cell surface microarray to evaluate the antibody profile of patients with candidemia against healthy individuals and uninfected hospital patients to determine relevant cell surface antigens that correlate with infection. Arrays were probed with a collection of sera consisting of different stages of candidemia: acute, early convalescent (approximately 4 weeks after onset of infection) and mid convalescent (approximately 12 weeks after onset of infection), as well as uninfected hospital patients and healthy individuals. Figure S1 shows a representative image of the microarray hybridized with the serum of an acute candidemia patient. All hybridizations in this study were done under the same conditions and dilutions with protein microarrays printed from the same batch. Their serological reactivity is shown as a heatmap where the antigens are sorted by increasing normalized global mean intensity, with bright green having the weakest intensity, red being the strongest, and black in between (Figure S2). An examination of the IgG response to the entire C. albicans cell surface protein microarray showed that the mean global signal intensity was similar among different groups (data not shown), although antigenic profiles are not identical between individuals.
Characterization of an IgG response indicative of permanent host-pathogen interplay in commensal colonization
We were interested in determining the most seroprevalent antibodies in the acute candidemia patients and how their humoral response compared against the negative control groups. Antigens to the most seroprevalent antibodies were defined as serodominant antigens and characterized as having mean antigen reactivity 2-fold greater than the in vitro transcription/translation reaction mixture containing no vector. The top-forty serodominant antigens in the candidemia patients consisted of many previously characterized antigenic peptides such as Bgl2 [17], Tkl1 [15], Hwp1 [13],[23], Eft2 [15], and Cdc24 [13] (Table 1). Also among the top-forty serodominant antigens were many previously identified virulence-associated and/or hyphal-regulated proteins (eg. Int1, Hwp1, Als1, Als3, Als5, Ece1, Hyr1, Cdc24, and Utr2) (Table 1) [24]–[32]. Interestingly, this serological response of acute candidemia patients was shared with both uninfected hospital patients and healthy individuals. The mean signal intensity to the top-forty serodominant antigens was 8,825 in acute candidemia patients, 8,837 in uninfected hospital patients, and 10,790 in healthy individuals. A two-way hierarchical cluster analysis of the top-forty serodominant antigens shows that the serum specimens of both the positive and negative candidemia groups were randomly dispersed throughout the hierarchical tree (Figure 1A). To further confirm that the top-forty serodominant antigenic signatures are shared among acute candidemia patients, the uninfected hospital patients and healthy individuals, principal component analysis (PCA) was used to generate a three-dimensional projection of the data (Figure 1B, 1C and 1D). The PCA shows that a large proportion of both the positive and negative acute candidemia sera are clustered together. These analyses suggest that IgG levels to the top-forty serodominant antigens are similar in both the negative control groups and acute candidemia sera. Since many of the top-forty antigens are either important for or induced during the invasion of epithelial or endothelial cells [11],[33], their expression in healthy people, inferred from the presence of their antibodies, indicates the existence of a permanent host-pathogen interplay in immunocompetent individuals.
Fig. 1. Prevalence of the serodominant anti-C. albicans cell surface IgGs in the study population. 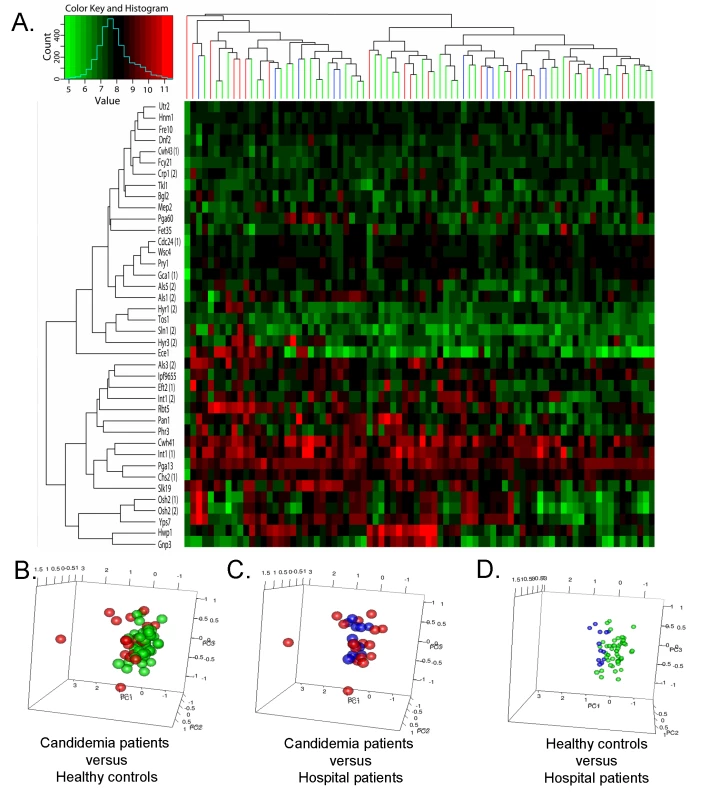
(A) Two-way hierarchical cluster of the top-forty serodominant antibodies (rows) and serum specimens (columns) from acute candidemia patients (n = 18) and negative controls groups (hospital patients (n = 12) and healthy individuals (n = 50)). The color scale ranks the antigens with red being the strongest, bright green the weakest, and black in between. (B, C & D) Principal component analyses of top-forty serodominant anti-C. albicans cell surface IgG antibody expression profiles between acute candidemia patients and each negative control group (hospital patients and health individuals). Each circle denotes the anti-C. albicans cell surface antibody profile of a single serum specimen. Samples are color coded as the following acute candidemia patients (red), healthy individuals (green), and hospital patients (blue). Tab. 1. The forty most serodominant antigens in acute candidemia patients. 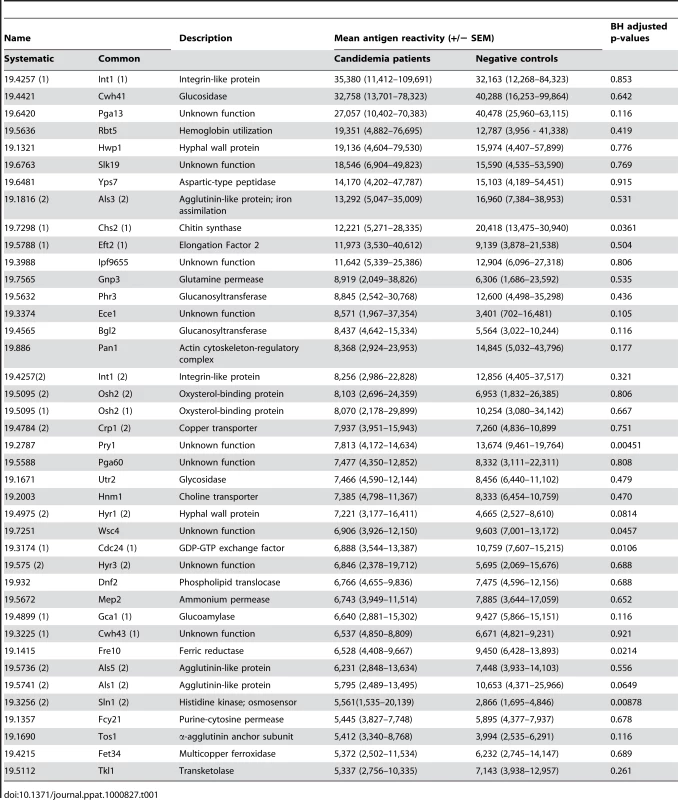
Identification of antigens correlative with the acute-stage of candidemia
To determine stage-specific biomarkers of acute candidemia, the normalized serological expression of acute candidemia patients were compared against the humoral reactivity of the uninfected hospital patients and healthy individuals. Serodiagnostic antigens were defined as having an IgG response significantly greater in acute candidemia patients (days 0–14) as compared to the negative control groups with Benjamini and Hochberg (BH) adjusted Cyber-T p-values <0.05. Thirteen antigens met this requirement (Table 2). Moreover, among the proteins identified as serodiagnostic markers, proteins involved in oxidative stress response appeared to be enriched over other functional categories. Sln1 and Nik1 are two out of three histidine kinases on the cell surface protein microarray and they are both identified as serodiagnostic antigens. Sln1 and Nik1 are sensors for the high-osmolarity glycerol (HOG) pathway, a mitogen-activated protein kinase cascade responsible for osmotic and oxidative stress adaptation in C. albicans [34],[35]. In addition, the expression levels of CDR4, RAS2, and ALS9 are up-regulated during oxidative stress [35]. Another functional group over-represented among the serodiagnostic antigens are transporters associated with drug resistance (Cdr1, Cdr4, and Yor1) [36].
Tab. 2. Antigenic biomarkers of the acute candidemia patients. 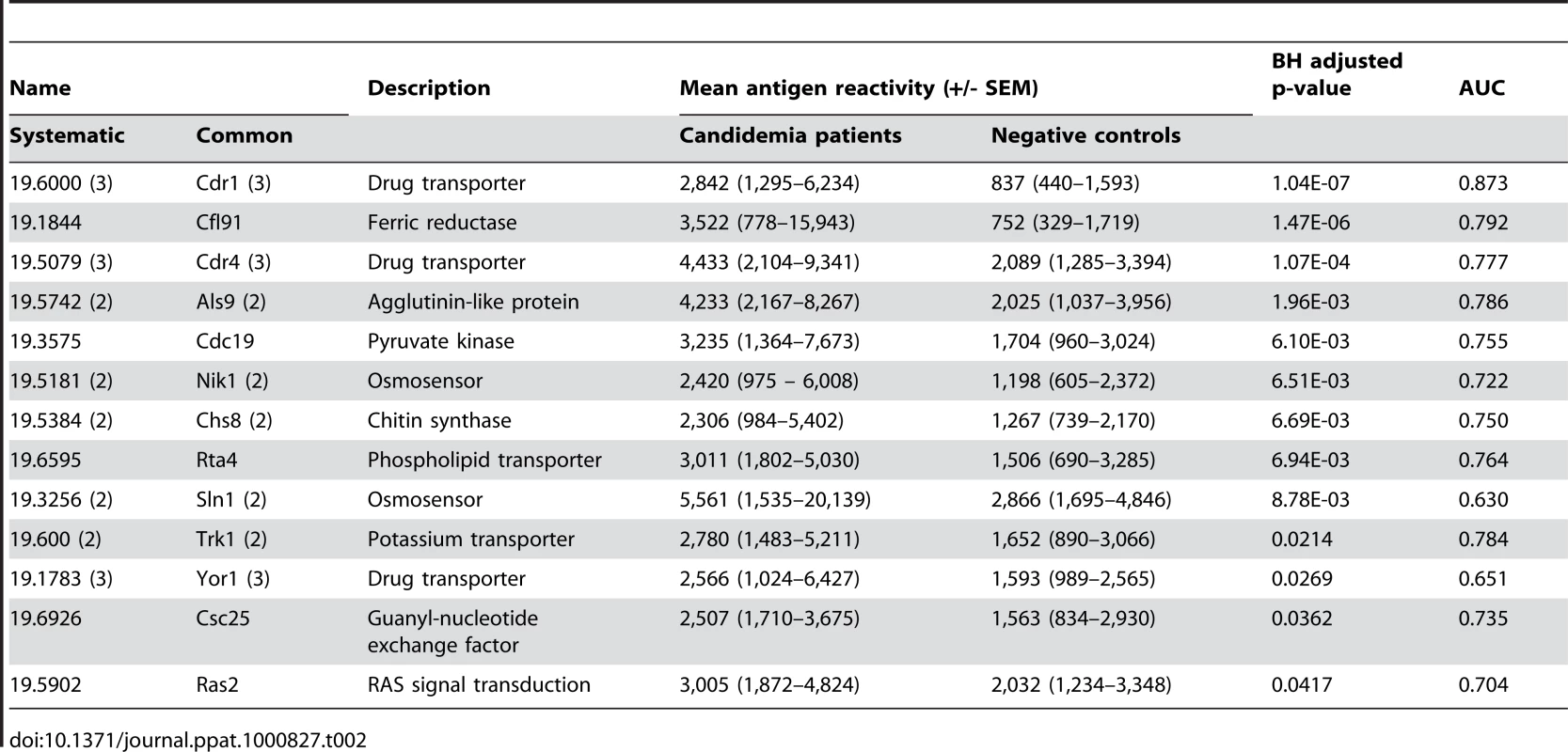
The 13-serodiagnostic antigens were also evaluated with a two-way hierarchical cluster analysis on candidemia positive and negative sera. Interestingly, the sera clustered into two distinct groups based on their responses to the 13 antigens (Figure 2A). Cluster I contained 10 candidemia sera and only one uninfected hospital patient. Cluster II contained all 50 healthy individuals, 11 of the 12 hospital patients, and 8 acute candidemia sera (Figure 2A). To further confirm that the antigenic signatures identified during the acute phase of candidemia differed from the negative control groups, PCA was used to create a three-dimensional projection of the data (Figure 2B, 2C, and 2D). In agreement with the two-way hierarchical cluster analysis, two distinct groups were observed (Figure 2B and 2C). Also, the PCA of the negative control groups showed individuals are clustered together with the exception of one outlying uninfected hospital patient found clustered with the acute candidemia patients (Figure 2C and 2D). These data provide further support of the antigenic signature of patients during the acute phase of candidemia. Multiple linear regression models determined that the antigenic profiles of acute candidemia patients were not related to various risk factors (i.e. age, gender, course of treatment, coexisting disease, and recovery/fatality) (data not shown). However, this determination is limited by the small sample size of our study.
Fig. 2. Discrimination of acute candidemia patients from the study population. 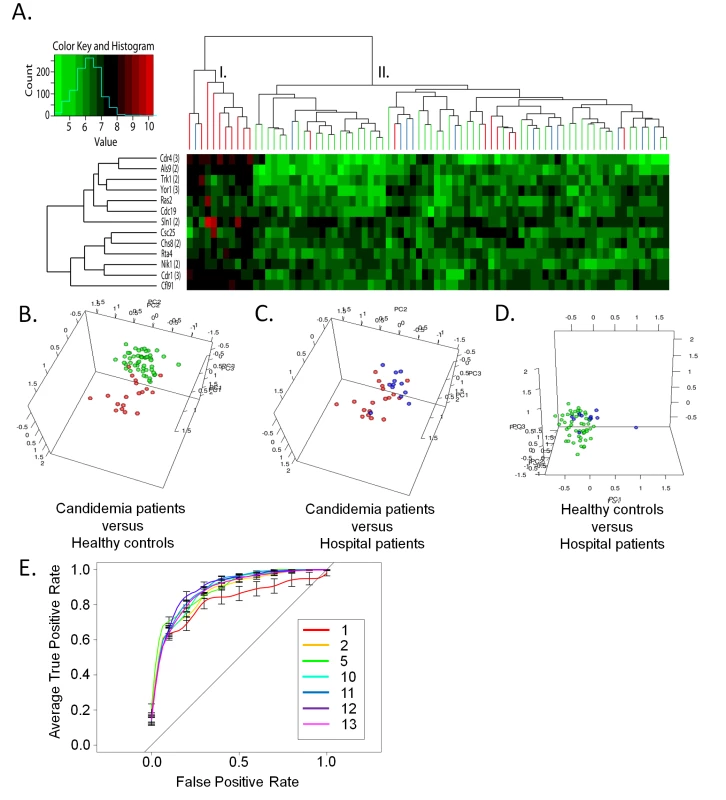
(A) Two-way hierarchical cluster analyses of the 13 differentially expressed anti-C. albicans cell surface antibodies in acute candidemia sera. The heatmap is organized with antigens, in rows, and acute candidemia patients (n = 18) and negative controls groups (hospital patients (n = 12) and healthy individuals (n = 50)) in columns. The colorized scale ranks the antigens with red being the strongest, bright green the weakest, and black in between. (B, C & D) Principal component analyses of serum anti-C. albicans cell surface IgG antibody expression profiles that discriminate between candidemia patients and each negative control group (hospital patients and health individuals). Each circle denotes the anti-C. albicans cell surface antibody profile of a single serum specimen. Samples are color coded as the following acute candidemia patients (red), healthy individuals (green), and hospital patients (blue). (E) The graph shows the ROC curves generated using different sets of acute serodiagnositc antigens. Multiple independent serodiagnostic antigens can dramatically improve the sensitivity and accuracy of serodiagnostic tests [37]. To establish a collection of antigens that could be used as a multiplex set to accurately distinguish candidemia cases from controls, we studied the discriminatory power of different sets of proteins using receiver operating characteristic (ROC) curves. First, ROC curves were generated for individual serodiagnostic antigens and the area under the ROC curves (AUC) for each antigen is listed in Table 2. The top-five cell surface proteins all have an AUC greater than 0.76, with CDR1 (3) (AUC 0.87, BH adjusted Cyber-T p-value <1.04e-7) giving the best single antigen discrimination (Table 2). The 13th antigen has an AUC of 0.630, which still exceeds the upper 95% confidence interval for random expectations for the AUC. To extend the analysis to combinations of antigens, we used kernel methods and support vector machines to build linear and nonlinear classifiers. As inputs to the classifier, we used the highest-ranking AUC antigens in combinations of 2, 5, 10, 11, 12 and 13 proteins and the results were validated with 10 runs of three-fold cross-validation (Figure 2E). Increasing the antigen number from 2 to 5, and 5 to 10 produced improvements in the classifier. But as the antigens increased to 13, a reduction in accuracy was observed. Using the ten most significant diagnostic antigens (in rank order: Cdr1 (3), Cfl91, Cdr4 (3), Als9 (2), Cdc19, Nik1 (2), Chs8 (2), Rta4, Sln1 (2), and Trk1 (2)), the classifier predicts 83% (95% CI, 76–89%) sensitivity, 72% (95% CI, 68–76%) specificity, and 74% (95% CI, 72–76%) accuracy in diagnosis of acute phase candidemia from the negative controls (healthy individuals and uninfected hospital patients) (Table 3).
Tab. 3. Test operating characteristics of the clinical biomarkers. 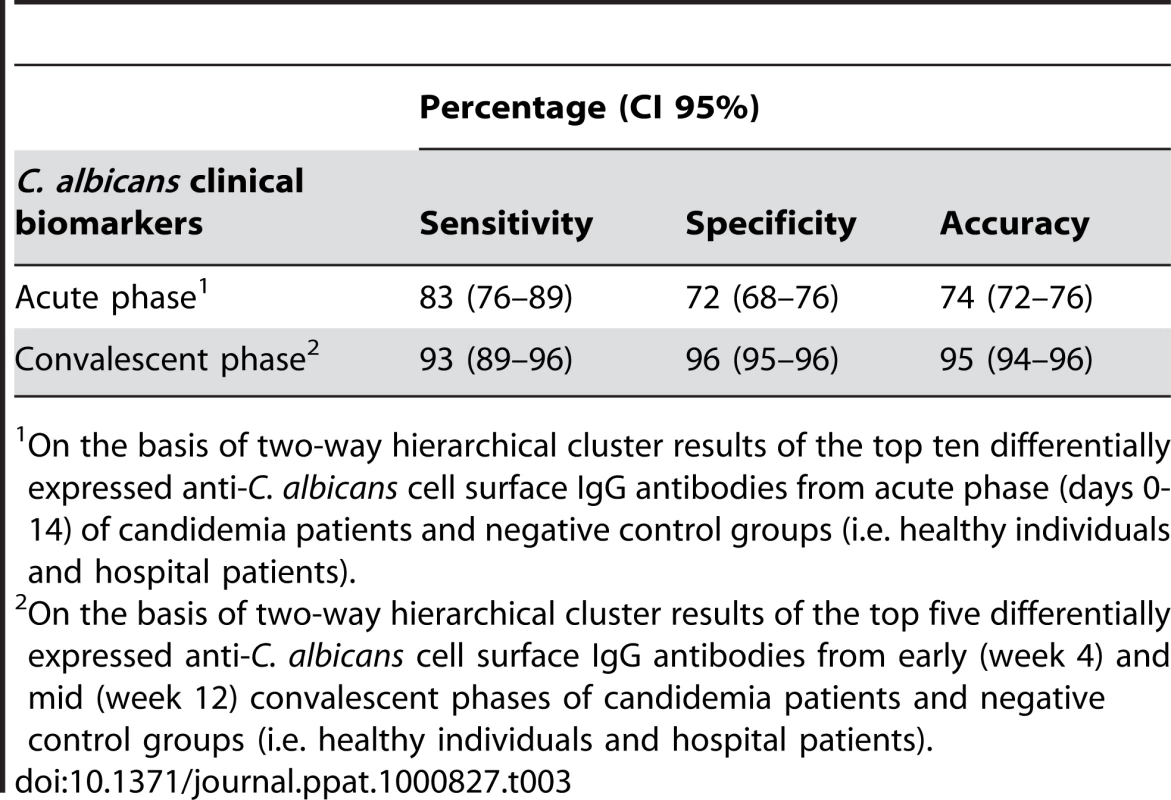
On the basis of two-way hierarchical cluster results of the top ten differentially expressed anti-C. albicans cell surface IgG antibodies from acute phase (days 0-14) of candidemia patients and negative control groups (i.e. healthy individuals and hospital patients). Identification of antigens correlative with the convalescent-stage of candidemia
We were next interested in identifying antigens that are significantly different between the early/mid convalescent candidemia patients (weeks 4 and 12 of the infection, respectively) and the negative control groups. The convalescent patient sera consisted of three patients whose serum was drawn under all three disease phases (acute phase, early and mid convalescent phases), 4 patients who had blood drawn at the acute and early convalescent phases, and 3 patients whose blood was drawn only at the early convalescent phase. Using BH adjusted Cyber-T p-values <0.05, we identified 33 antigens, 11 of which are from the 13 diagnostic antigens for the acute phase of infection (Table 4). Among the identified convalescent biomarkers were marked expansions in proteins involved in iron acquisition (Rbt5, Csa1, Flc1, and Cfl91) (Table 4). Cfl91 is a putative ferric reductase similar to Fre10, which is required for the release of iron from transferrin and the reduction to ferrous iron [38]. The protein Flc1 has been identified as having heme uptake activity [39] whereas, both Rbt5 and Csa1 have been implicated as receptors of hemoglobin whose function is to deliver the hemoglobin by endocystosis to the vacuole where iron is released by acidification [40],[41]. The remainders of the identified proteins have roles in cell wall biogenesis, membrane lipid organization, and drug resistance.
Tab. 4. Antigenic biomarkers of the early and mid convalescent candidemia patients. 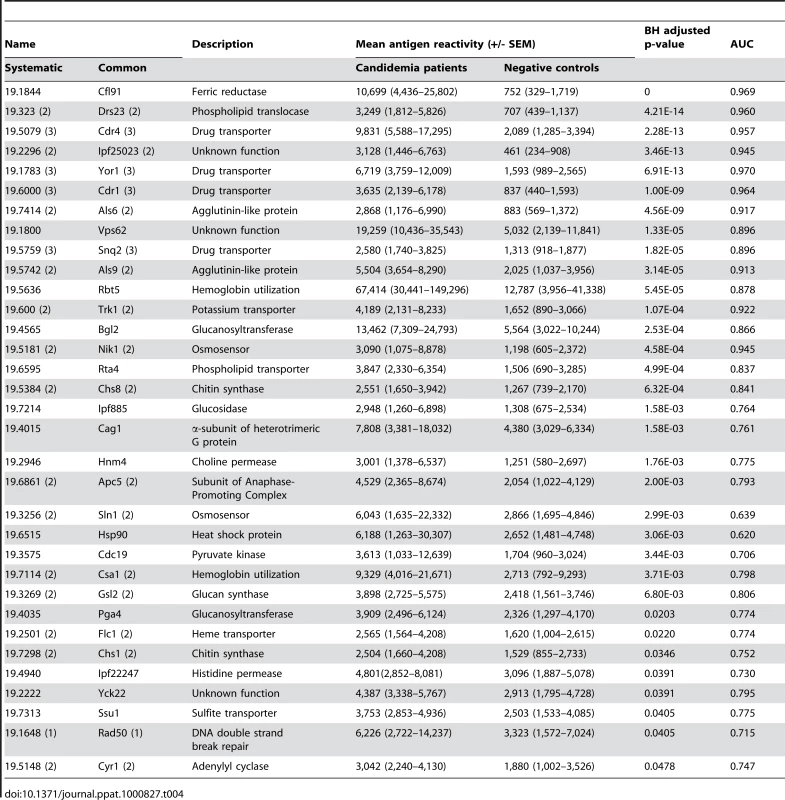
We next evaluated antibody response to the 33 antigens in the acute, convalescent candidemia patients and the negative control groups by two-way hierarchical cluster analysis. The individuals in Cluster II were the same as those identified previously with 13 serodiagnostic antigens (Figure 2A and 3A) with the addition of one convalescent candidemia patient whose only sera was drawn during week 4 of the infection. Individuals in Cluster I consisted of candidemia patients with the exception of the one uninfected hospital patient from Figure 2A. Three of the candidemia patients' acute and convalescent profiles were all found in Cluster I, whereas four candidemia patients' profiles converted from Cluster II to I during the convalescence phase of the disease. In addition, the remaining two-candidemia patients whose only blood draws were during week 4 also grouped in Cluster I (Figure 3A). This conversion of the antigenic profile from the negative control groups (Cluster II) to the antigenic profile consistent with candidemia (Cluster I), indicates an adaptive immune response to C. albicans that is different from commensal sensitization. Again, PCA was used to further confirm that the antigenic signatures identified during the convalescent phase of candidemia differed from the negative control groups (Figure 3B, 3C and 3D). ROC curves were generated to assess the ability to separate the control and convalescent candidemia. AUC was determined for each of the 33-serodiagnostic antigens and listed in Table 4 in decreasing order. The top-five ORFs all have an AUC greater than 0.94. We then used SVMs to build multiplex classifiers with 2, 5, and 10 antigens with the highest-ranking AUC from Table 4. The results were validated with 10 runs of three-fold cross-validation (Figure 3E). Increasing the antigen number from 2 to 5 maintained the diagnostic accuracy in the classifier and a reduction in accuracy occurred as the antigens increased to 10 due to over-fitting. The top-five serodiagnostic antigens are associated with xenobiotic-transporting activity (Cdr4 and Yor1) [36], phospholipid-transporting activity (Drs23), a putative ferric reductase (Cfl91), and a mucin-like cell wall protein (Ipf25023) (Table 4). Using the top-five antigens, the classifier predicts 93% (95% CI, 89–96%) sensitivity, 96% (95% CI, 95–96%) specificity, and 95% (95% CI, 94–96%) accuracy in the differentiation of early/mid convalescent phase candidemia from the negative controls (healthy individuals and uninfected hospital patients) (Table 3).
Fig. 3. Discrimination of convalescent candidemia patients from the study population. 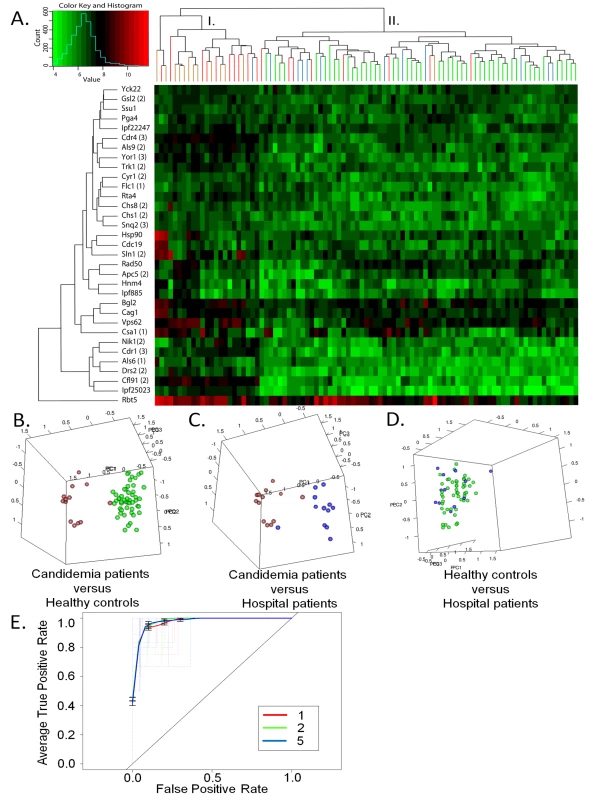
(A) Two-way hierarchical cluster analyses of the 33 differentially expressed anti-C. albicans cell surface antibodies from early/mid convalescent candidemia sera. The heatmap is organized with antigens, in rows, and acute candidemia patients (n = 18), early and mid convalescent patients (n = 10) and negative control groups (hospital patients (n = 12) and healthy individuals (n = 50)) in columns. The colorized scale ranks the antigens with red being the strongest, bright green the weakest, and black in between. (B, C & D) Principal component analyses of serum anti-C. albicans cell surface IgG antibody expression profiles that discriminate between convalescent candidemia patients and each negative control group (hospital patients and health individuals). Each circle denotes the anti-C. albicans cell surface antibody profile of asingle serum specimen. Samples are color coded as the following acute candidemia patients (red), convalescent candidemia patients (brown), healthy individuals (green), and hospital patients (blue). (E) The graph shows the ROC curves generated using different sets of serodiagnostic antigens. Having identified 33 antigens that are correlative with convalescent candidemia in comparison to the negative control groups, we next wanted to determine the temporal change in IgG response to these 33 antigens during the transition from acute infection (AI), to early convalescent (EC), and mid convalescent (MC). A two-way hierarchical cluster analyses was performed on differential IgG responses to the 33 antigens in 3 patients with AI, EC and MC sera, and 4 patients with only AI and EC sera (Figure S3). A one tailed t-test was carried out to look for differences where the EC antigen intensity is significantly greater than the AI antigen intensity, possibly indicating the selection of a protective antibody response. We observed a significant increase in the IgG response from AI to EC in the following antigens, which are ranked according to their p-values: Apc5 (2) (1.12E-03), Drs23 (3) (1.23E-03), Vps62 (1.57E-03), Rad50 (1.83E-03), Ssu1 (3.17E-03), Yor1 (3) (5.33E-03), Ipf885 (5.33E-03), Pga4 (5.88E-03), Cdr4 (3) (7.22E-03), Cfl91 (2) (0.0231), Cyr1 (2) (0.0274), Ipf25023 (2) (0.0330), Gsl2 (2) (0.0374), Chs1 (2) (0.0393), and Snq2 (3) (0.0486). The identified antigens could potentially be efficacious vaccine candidates due to the fact that the IgG response is being positively selected over the course of infection.
Discussion
In this study, we have developed a C. albicans cell surface protein microarray and profiled host humoral responses during conmmensal colonization and during the progression of candidemia. Thirteen novel serodiagnostic antigens were identified for differentiating acute candidemia from commensal sensitization and 33 antigens were found to discriminate convalescent candidemia from non-candidemia controls. The sensitivity and specificity for the identification of acute candidemia determined by the top 10 antigens from the set of 13 serodiagnostic markers are comparable to that obtained using the method of 2D-PAGE and immunoblots [17]. When using the top 5 antigens from the set of 33, both sensitivity and specificity are dramatically improved for convalescent candidemia. Pitarch et al. reported that the anti-Bgl2p IgG antibody levels mainly define the proteomic signature for candidemia patients [17]. In this study, Bgl2 is on the list of 33 diagnostic antigens from convalescent sera. Although it is classified as a serodominant antigen by acute candidemia sera, the BH-adjusted p-value of Bgl2 (0.116) is just above cutoff (0.05) to be considered as diagnostic by our definition, and the mean anti-Bgl2 antibodies in acute candidemia is higher than the mean in non-candidemia controls. Bgl2 is a glycoprotein and the glycan moieties on other b-1,3-glucanosyltransferases seem to contribute to antigenicity. Since our Bgl2 is expressed in vitro without any glycosylation, its antigenicity is likely different from the Bgl2 produced by C. albicans used in the 2D-PAGE immunoblots. The previously identified immunogenic heat shock protein 90 (Hsp90) is also one of 33 biomarkers for convalescent candidemia identified from this study. Hsp90 has been shown to elicit a protective humoral response [42],[43] and its antibodies are known to associate with patients that recover from candidiasis. The use of protein microarray technology allowed us to identify new diagnostic antigens that were missed by previous studies. The use of 2-D PAGE to accurately identify and separate clinical markers of candidemia from commensal sensitization is limited by the range in protein abundance and various properties associated with peptides such as their mass, isoelectric point, hydrophobicity, and post-translational modification, as well as the semi-quantitative nature of a Western [18]. Using a C. albicans cell surface protein microarray helped us overcome many of the technical difficulties found with traditional proteomics, since the expression level of recombinant-derived proteins vary by only a single log and the use of fluorescent-labeled antibodies allows for greater linearity, precision, and sensitivity in the quantitative measurement of the humoral response to C. albicans. One of the most beneficial aspects in the use of the protein microarray assay is its ability to detect significant differences in the IgG response that under traditional immunoblot conditions would be below the detectable threshold. However, a potential limitation to our study is that the microarray is based on recombinant peptides. Because of the cell free nature of our in vitro translated peptides, potential epitopes may have been lost due to miss folding and a lack of glycosylation, both of which may affect the conformational structure of the native protein. On the other hand, the removal of posttranslational modifications, such as glycosylation, from the peptides may have revealed hidden peptide epitopes only seen during a strong host immune response. A large collection of peptide epitopes may increase the specificity in diagnosis of infection. In support of this, our study has identified many new clinical biomarkers that are associated with differing states of interactions with the host as well as the characterization of potential new targets for therapeutics and vaccine candidates. To our knowledge, this is the first study using a protein microarray to analyze the serological response to an organism that is capable of existing as both commensal flora and an opportunistic pathogen in the human population.
Commensal colonization of C. albicans is common in humans and attenuated host immunity is a perquisite for the transition from commensal colonization to infection. Historically, it was believed that C. albicans switched from a commensal to a pathogen using distinct pathogen-associated genetic programs when the host immune status was altered. An intriguing review challenges this notion, Hube postulates that C. albicans exists in a permanent host-pathogen interplay where overgrowth and invasion is only observed under immunocompromising conditions[44]. The review puts forth two-models of a permanent infection strategy: (1) constitutive gene expression where attenuated immunity induces little or no change in the pathogenic profile of C. albicans or (2) a variable transcriptional profile where C. albicans expression is dependent on the stage - and tissue-specific interactions with the host. Our study indicates the existence of permanent host-pathogen interplay with variable gene expression over the course of infection. The serological response to the entire C. albicans cell surface protein microarray detected considerable homogeneity as well as differences in the patterns of antigens recognized among patients and healthy individuals. The majority of healthy individuals and uninfected hospital patients have moderate to strong IgG responses to many C. albicans cell surface proteins that have long been associated with virulence or hyphal-regulation (a hallmark of virulence in itself). In agreement with our protein microarray data, Naglik et al. observed similar levels of IgG titers to the hyphal wall protein Hwp1 in patients with oral candidiasis and asymptomatic mucosal infections as well as healthy culture-negative controls [23]. These serodominant cross-reactive antigens include adhesins such as Als1, Als3, Als5, Hwp1 and Int1 and hyphal-regulated genes such as Als3, Hwp1, Ece1, Hyr1, and Cdc24. Both functional groups are known to be important for invasion and virulence [45]. Among the identified serodominant antigens are many previously characterized immunogenic peptides such as Bgl2 [17], Tkl1 [15], Hwp1 [13],[23], Eft2 [15], and Cdc24 [13]. Intriguingly, the average signal intensities to the top-forty serodominant antigens are higher in the healthy individuals than the uninfected hospital patients and acute candidiasis patients (10,380 vs. 8,837 and 8,825, respectively). It is interesting to speculate whether the healthy individuals' IgG response limits colonization and overgrowth since many of the serodominant antigens are against adhesins. In particular is the strong humoral response to the integrin-like protein, Int1, which may play dual roles in limiting both intestinal colonization of the cecum and systemic invasion of deep tissue organs [46],[47]. Another interesting serodominant antibody response is to the protein Ece1, which has been shown to promote adhesion and is important for GI colonization[48]. ECE1 transcription is highly expressed during GI colonization and invasion of host tissue [33],[48]. However, one can not discount that the high IgG titer of colonized individuals may be due to a previous superficial infections such candidal vaginitis [49],[50].
The microenvironmental conditions during commensal colonization of the host may also play a role in the induction of the IgG response to certain cell surface proteins. Previous studies have evaluated characteristics common to the GI and/or vulvovaginal tract such as blood, hypoxia, iron restriction and weak acid as modifiers of gene expression [9], [51]–[53]. Intriguingly, the expressions of these genes share common features to the identified serodominant antibodies. Interestingly, genes transcriptionally up-regulated in blood (Als1, Als3, Hwp1, Ece1, Hyr1, and Bgl2) were serodominant and cross-reactive with both positive and negative candidiasis individuals, as were genes up-regulated under hypoxic conditions (Als1, Als3, Hwp1, Rbt5, Utr2, and Tos1), iron restriction (Int1, Rbt5, and Fet35), and weak acid (Crp1, Fet35, and Ipf9655) (Table 1). Furthermore, some of the serodominant antigens (i.e. Als3, Ece1, Hwp1, and Rbt5) have been shown to be induced during the invasion of epithelial or endothelial cells [11],[33]. Therefore, the expression of the serodominant antigens in healthy individuals indicates the existence of permanent host-pathogen interplay during commensal colonization. In addition, the presence of serodominant IgGs in all 50 healthy individuals suggests that commensal colonization is much more prevalent than previously reported.
One of the most challenging tasks in characterizing serodiagnostic antigens from C. albicans is the identification of discriminating peptides that can differentiate between commensal colonization and candidemia with high sensitivity and specificity. By profiling antibody response from patients with varying stages of candidemia against healthy individuals and candidemia-negative hospital patients, we have identified 13 diagnostic antigens for acute phase of candidemia and 33 for the early/mid convalescent candidemia. The serologic signature in candidemia patients likely reflects an alteration in the level of those proteins due to a change either in transcription and/or protein stability. Stage - and tissue-specific gene expression during the course of systemic infection is expected as C. albicans cells transition through differing microenvironments of the host. Among the 13 diagnostic antigens for acute candidemia, three are associated with drug resistance (Cdr1, Cdr4, and Yor1) [36]. The exposure to antifungal drugs in patients undergoing acute candidemia may have acted as an additional environmental stress that stimulates the expression of these antifungal drug transporters [54]. Intriguingly, two out of the 13 biomarkers are the osmosensors Sln1 and Nik1 for the HOG pathway that is responsible for osmotic and oxidative stress adaptation in C. albicans [34],[35]. The host-pathogen interaction commonly associated with oxidative stress is typically seen during phagocytosis by neutrophils, the initiating immune response to C. albicans overgrowth and infection. Furthermore, a study of global transcriptional responses to oxidative stress observed an increase in the transcriptional expression of CDR4 (4.1-fold), RAS2 (2.5-fold) and ALS9 (1.5-fold) [35]. Taken together, our data indicates a strong correlation between the IgG response to oxidative stress-related cell surface proteins and the initial cell-mediated immune response during acute candidemia. In further agreement, previous studies have shown that oxidative stress functions are primarily induced when C. albicans is initially exposed to human blood or following phagocytosis by neutrophils and granulocytes [7],[9],[10],[55]. The 33 convalescent diagnostic antigens include proteins involved in iron acquisition, cell wall biogenesis, membrane lipid organization, and drug resistance. Of particular interest is the dramatic increase in antibodies to proteins for iron acquisition (Cfl91, ferric reductase; Rbt5 and Csa1, hemoglobin receptors; and Flc1, heme uptake). Iron is an essential nutrient for C. albicans. Circulating iron in serum is bound to transferrin and ferric reductases are required in the acquisition of iron from transferrin. Interestingly, Cfl91 is found as a biomarker for both acute and convalescent candidemia patients. Of particular interest is the increase antibody response to hemoglobin and heme-related proteins as these molecules are normally sequestered in erythrocytes [56]. The proteins Rbt5, Csa1 and Flc1 are required for iron acquisition from hemoglobin or heme [39],[40] and are diagnostic antigens only for convalescent candidemia. Thus, it is interesting to speculate whether free hemoglobin becomes a by-product of lysed erythrocytes after post-operative surgery or other invasive clinical procedures. Nevertheless, the data from this study should provide critical information for the development of diagnostic antigenic profiles for patients at risk for candidemia and for the assessment of progression of hematogenously disseminated candidiasis. Future studies will need to be done to determine whether serological differences exist between superficial and systemic infections, as well as commensal sensitization.
The development of the antigenic profiles over the course of candidiasis (acute infection, early convalescence, and mid convalescence) may also provide insight into a protective humoral response against C. albicans. Even though previous sensitization to commensal colonization does not limit mortality or even morbidity in patients, experimental studies have identified protective antibodies against hematogenously disseminated candidiasis, such as heat shock protein 90 (Hsp90) or β-mannan [57]–[60]. Future studies will need to address whether the serodiagnostic antigens identified in this study could provide protection from hematogenously disseminated candidiasis. Of particular interest are the convalescent serodiagnostic antigens where the EC antigen intensity is significantly greater than the AI antigen intensity, which may possibly indicate the selection of a protective antibody response.
Materials and Methods
Ethics statement
Human sera from candidemia patients and hospitalized patients were collected from SH-UF under protocols approved and created by the UF Institutional Review Board. Sera from healthy individuals were obtained from volunteers at the General Clinical Research Center at the University of California, Irvine. Written, informed consent was obtained from participants.
Collection of candidemia and control sera
Candidemia was defined as the recovery of C. albicans from blood cultures. Sera from candidemia patients and hospitalized patients (no clinical or microbiological evidence of candidemia) were collected from SH-UF as previously published [61]. Briefly, patients at SH-UF were identified on the day blood cultures were positive for C. albicans. The Infectious Diseases Consultation Service at SH-UF identified controls. Sera were collected and stored at −70°C in the repository at the UF Mycology Research Unit. For patients with candidemia, sera were obtained from the earliest possible date on or after the date that the first positive cultures were drawn. In all cases, this was within 7 days of the first positive culture (acute-phase sera). For ten patients with candidemia, sera were also recovered 4 to 12 weeks after the date on which the first positive cultures were drawn (convalescent-phase sera).
Microarray construction and antibody profiling
Cell surface proteins were selected from the Candida Genome Database (CGD) using keywords such as “cell surface”, “plasma membrane”, and “cell wall”. The CGD annotation of cell surface proteins is based on published experiments [32], [62]–[66], function-based prediction of cellular localization, and sequence prediction. Known antigenic proteins are also included as controls (Bgl2, Eno1, Pgk1, Gap1, Cdc19, Tkl1, Hsp90, and members of the Hsp70 family) [15],[17]. Coding regions of the genes were PCR amplified from the clinical isolate SC5314 of C. albicans with primers listed in Table S2, and cloned into a pXT7 expression vector with a HA-tag at the N-terminus and His-tag at the C-terminus by homologous recombination in E. coli as described [67]. Protein expression was carried out using an E. coli based cell-free in vitro transcription/translation system (RTS 100 E. coli HY kit, Roche). The protein microarray was made by printing the peptides onto nitrocellulose-coated FAST glass slides (Schleicher & Schuell) using the OmniGrid 100 (GeneMachines) in the UCI Microarray Facility. Each peptide was printed in duplicate and showed homogenous spot morphology as well as low background. Internal controls consisting of buffer alone and a reaction mixture with no DNA were also printed onto the FAST slides. After the addition of the plasma samples the microarray was incubated with a biotin-conjugated donkey anti-human IgG Fcγ fragment specific secondary antibody (Jackson Immunoresearch). The secondary antibody was then removed and the microarray was incubated with Streptavidin: SureLight ® P-3 (Columbia Biosciences). Details concerning microarray construction and controls, antibody profiling, data normalization, as well as the reproducibility and validity of the microarray are given in the Text S1.
Statistical analysis
All analysis was performed using the R statistical environment (http://www.r-project.org). It has been noted in the literature that data derived from microarray platforms is heteroskedatic [68]–[70]. This mean-variance dependence has been observed in the arrays presented in this manuscript [71],[72]. In order to stabilize the variance, the vsn method [73] implemented as part of the Bioconductor suite (www.bioconductor.org) was applied to the quantified array intensities. In addition to removing heteroskedacity, this procedure corrects for non-specific noise effects by finding maximum likelihood shifting and scaling parameters for each array such that the variances of a large number (default setting used: 85%) of the spots on the array are minimized. In other words, the method assumes that variance in binding for the vast majority of the proteins on the array are due to noise rather than true differential immunological response. In essence, 85% of the spots on the array are used as controls for sample-by-sample normalization. This calibration method has been shown to be effective on a number of platforms [74]–[76]. A simple ranking normalization where all of the proteins are ordered for each sample by binding intensity and assigning the integer rank was performed as well with similar results (results not shown). Finally, VSN normalized data is retransformed with the ‘sinh’ function to allow visualization and discussion at an approximate raw scale.
Diagnostic biomarkers between groups were determined using a Bayes regularized t-test adapted from Cyber-T for protein arrays [69],[77]. To account for multiple testing conditions, the Benjamini and Hochberg (BH) method was used to control the false discovery rate [78]. Statistical analyses were performed with R 2.0 (www.r-project.org) and STATA (version 10.0, StataCorp). Multiple antigen classifiers were constructed using linear and non-linear Support Vector Machines (SVMs) using the “e1071” R package. To prevent overfitting and show the generalization of the classification method, 10 repeats of three-fold cross-validation were performed. In this methodology, the data is split into 3 class-stratified subsets. For each subset, a classifier is trained using the remaining two-thirds of the data. The classifier is then evaluated on the one-third of the data not used for training. This process is repeated for each split and for 10 different splits, yielding 30 evaluation measures. The ROCR package was used to construct receiver-operating-characteristic curves and perform sensitivity and specificity analyses. Blast2Go (www.blast2go.org) was used for gene ontology annotation and enrichment analysis. To confirm that the identified antigens were accurate, their vectors were resequenced. The Tables S3 and S4 list the statistical data of acute and convalescent candidemia patients, respectively.
Accession numbers
Detailed information for the genes/proteins from this study can be found at the Candida Genome Database http://www.candidagenome.org. The gene names and ORF numbers are listed here: INT1 (19.4257), CWH41 (19.4421), PGA13 (19.6420), RBT5 (19.5636), HWP1 (19.1321), SLK19 (19.6763), YPS7 (19.6481), ALS3 (19.1816), CHS2 (19.7298), EFT2 (19.5788), IPF9655 (19.3988), GNP3 (19.7565), PHR3 (19.5632), ECE1 (19.3374), BGL2 (19.4565), PAN1 (19.19.886), OSH2 (19.5095), CRP1 (19.4784), PRY1 (19.2787), PGA60 (19.5588), UTR2 (19.1671), HNM1 (19.2003), HYR1 (19.4975), WSC4 (19.7251), CDC24 (19.3174), HYR3 (19.575), DNF2 (19.932), MEP2 (19.5672), GCA1 (19.4899), CWH43 (19.3225), FRE10 (19.1415), ALS5 (19.5736), ALS1 (19.5741), SLN1 (19.3256), FCY21 (19.1357), TOS1 (19.1690), FET34 (19.4215), TKL1 (19.5112), CDR1 (19.6000), CFL91 (19.1844), CDR4 (19.5079), ALS9 (19.5742), CDC19 (19.3575), NIK1 (19.5181), CHS8 (19.5384), RTA4 (19.6595), TRK1 (19.600), YOR1 (19.1783), CSC25 (19.6926), RAS2 (19.5902), DRS23 (19.323), IPF25023 (19.2296), ALS6 (19.7414), VPS62 (19.1800), SNQ2 (19.5759), IPF885 (19.7214), CAG1 (19.4015), HNM4 (19.2946), APC5 (19.6861), HSP90 (19.6515), CSA1 (19.7114), GSL2 (19.3269), PGA4 (19.4035), FLC1 (19.2501), CHS1 (19.7298), IPF22247 (19.4940), YCK22 (19.2222), SSU1 (19.7313), RAD50 (19.1648), and CYR1 (19.5148).
Supporting Information
Zdroje
1. BendelCM
2003 Colonization and epithelial adhesion in the pathogenesis of neonatal candidiasis. Semin Perinatol 27 357 364
2. Kwon-ChungKJ
BennettJE
1992 Medical mycology. Philadelphia: Lea & Febiger. ix, 866 p
3. KohAY
KohlerJR
CoggshallKT
Van RooijenN
PierGB
2008 Mucosal damage and neutropenia are required for Candida albicans dissemination. PLoS Pathog 4 e35 doi:10.1371/journal.ppat.0040035
4. ColeGT
HalawaAA
AnaissieEJ.
The Role of the Gastrointestinal Tract in Hematogenous Candidiasis: From the Laboratory to the Bedside. Clinical Infectious Diseases 22 S73 S88
5. RaadI
HannaH
BoktourM
GirgawyE
DanawiH
2004 Management of central venous catheters in patients with cancer and candidemia. Clin Infect Dis 38 1119 1127
6. BrownAJ
OddsFC
GowNA
2007 Infection-related gene expression in Candida albicans. Curr Opin Microbiol 10 307 313
7. Rubin-BejeranoI
FraserI
GrisafiP
FinkGR
2003 Phagocytosis by neutrophils induces an amino acid deprivation response in Saccharomyces cerevisiae and Candida albicans. Proc Natl Acad Sci U S A 100 11007 11012
8. LorenzMC
BenderJA
FinkGR
2004 Transcriptional response of Candida albicans upon internalization by macrophages. Eukaryot Cell 3 1076 1087
9. FradinC
KretschmarM
NichterleinT
GaillardinC
d'EnfertC
2003 Stage-specific gene expression of Candida albicans in human blood. Mol Microbiol 47 1523 1543
10. FradinC
De GrootP
MacCallumD
SchallerM
KlisF
2005 Granulocytes govern the transcriptional response, morphology and proliferation of Candida albicans in human blood. Mol Microbiol 56 397 415
11. ZakikhanyK
NaglikJR
Schmidt-WesthausenA
HollandG
SchallerM
2007 In vivo transcript profiling of Candida albicans identifies a gene essential for interepithelial dissemination. Cell Microbiol 9 2938 2954
12. EckertSE
HeinzWJ
ZakikhanyK
ThewesS
HaynesK
2007 PGA4, a GAS homologue from Candida albicans, is up-regulated early in infection processes. Fungal Genet Biol 44 368 377
13. ChengS
ClancyCJ
CheckleyMA
HandfieldM
HillmanJD
2003 Identification of Candida albicans genes induced during thrush offers insight into pathogenesis. Mol Microbiol 48 1275 1288
14. BerenguerJ
BuckM
WitebskyF
StockF
PizzoP
1993 Lysis-centrifugation blood cultures in the detection of tissue-proven invasive candidiasis. Disseminated versus single-organ infection. Diagn Microbiol Infect Dis 17 103 109
15. PitarchA
AbianJ
CarrascalM
SanchezM
NombelaC
2004 Proteomics-based identification of novel Candida albicans antigens for diagnosis of systemic candidiasis in patients with underlying hematological malignancies. Proteomics 4 3084 3106
16. PitarchA
Diez-OrejasR
MoleroG
PardoM
SanchezM
2001 Analysis of the serologic response to systemic Candida albicans infection in a murine model. Proteomics 1 550 559
17. PitarchA
JimenezA
NombelaC
GilC
2006 Decoding serological response to Candida cell wall immunome into novel diagnostic, prognostic, and therapeutic candidates for systemic candidiasis by proteomic and bioinformatic analyses. Mol Cell Proteomics 5 79 96
18. HanashS
2003 Disease proteomics. Nature 422 226 232
19. StellerS
AngenendtP
CahillDJ
HeubergerS
LehrachH
2005 Bacterial protein microarrays for identification of new potential diagnostic markers for Neisseria meningitidis infections. Proteomics 5 2048 2055
20. ZhuH
HuS
JonaG
ZhuX
KreiswirthN
2006 Severe acute respiratory syndrome diagnostics using a coronavirus protein microarray. Proc Natl Acad Sci U S A 103 4011 4016
21. LiB
JiangL
SongQ
YangJ
ChenZ
2005 Protein microarray for profiling antibody responses to Yersinia pestis live vaccine. Infect Immun 73 3734 3739
22. ButlerG
RasmussenMD
LinMF
SantosMA
SakthikumarS
2009 Evolution of pathogenicity and sexual reproduction in eight Candida genomes. Nature 459 657 662
23. NaglikJR
FostiraF
RupraiJ
StaabJF
ChallacombeSJ
2006 Candida albicans HWP1 gene expression and host antibody responses in colonization and disease. J Med Microbiol 55 1323 1327
24. BassilanaM
BlythJ
ArkowitzRA
2003 Cdc24, the GDP-GTP Exchange Factor for Cdc42, Is Required for Invasive Hyphal Growth of Candida albicans. Eukaryotic Cell 2 9 18
25. GaleCA
BendelCM
McClellanM
HauserM
BeckerJM
1998 Linkage of adhesion, filamentous growth, and virulence in Candida albicans to a single gene, INT1. Science 279 1355 1358
26. StaabJF
BradwaySD
FidelPL
SundstromP
1999 Adhesive and Mammalian Transglutaminase Substrate Properties of Candida albicans Hwp1. Science 283 1535 1538
27. FuY
IbrahimA
SheppardD
ChenY
FrenchS
2002 Candida albicans Als1p: an adhesin that is a downstream effector of the EFG1 filamentation pathway. Mol Microbiol 44 61 72
28. PhanQT
MyersCL
FuY
SheppardDC
YeamanMR
2007 Als3 is a Candida albicans invasin that binds to cadherins and induces endocytosis by host cells. PLoS Biol 5 e64 doi:10.1371/journal.pbio.0050064
29. GaurNK
KlotzSA
HendersonRL
1999 Overexpression of the Candida albicans ALA1 Gene in Saccharomyces cerevisiae Results in Aggregation following Attachment of Yeast Cells to Extracellular Matrix Proteins, Adherence Properties Similar to Those of Candida albicans. Infect Immun 67 6040 6047
30. BirseCE
IrwinMY
FonziWA
SypherdPS
1993 Cloning and characterization of ECE1, a gene expressed in association with cell elongation of the dimorphic pathogen Candida albicans. Infect Immun 61 3648 3655
31. BaileyD
FeldmannP
BoveyM
GowN
BrownA
1996 The Candida albicans HYR1 gene, which is activated in response to hyphal development, belongs to a gene family encoding yeast cell wall proteins. J Bacteriol 178 5353 5360
32. Alberti-SeguiC
MoralesAJ
XingH
KesslerMM
WillinsDA
2004 Identification of potential cell-surface proteins in Candida albicans and investigation of the role of a putative cell-surface glycosidase in adhesion and virulence. Yeast 21 285 302
33. ThewesS
KretschmarM
ParkH
SchallerM
FillerSG
2007 In vivo and ex vivo comparative transcriptional profiling of invasive and non-invasive Candida albicans isolates identifies genes associated with tissue invasion. Mol Microbiol 63 1606 1628
34. RomanE
NombelaC
PlaJ
2005 The Sho1 Adaptor Protein Links Oxidative Stress to Morphogenesis and Cell Wall Biosynthesis in the Fungal Pathogen Candida albicans. Mol Cell Biol 25 10611 10627
35. EnjalbertB
SmithDA
CornellMJ
AlamI
NichollsS
2006 Role of the Hog1 stress-activated protein kinase in the global transcriptional response to stress in the fungal pathogen Candida albicans. Mol Biol Cell 17 1018 1032
36. CannonRD
LampingE
HolmesAR
NiimiK
BaretPV
2009 Efflux-Mediated Antifungal Drug Resistance. Clin Microbiol Rev 22 291 321
37. BarbourAG
JasinskasA
KayalaMA
DaviesDH
SteereAC
2008 A genome-wide proteome array reveals a limited set of immunogens in natural infections of humans and white-footed mice with Borrelia burgdorferi. Infect Immun 76 3374 3389
38. KnightSAB
VilaireG
LesuisseE
DancisA
2005 Iron Acquisition from Transferrin by Candida albicans Depends on the Reductive Pathway. Infect Immun 73 5482 5492
39. ProtchenkoO
Rodriguez-SuarezR
AndrophyR
BusseyH
PhilpottCC
2006 A screen for genes of heme uptake identifies the FLC family required for import of FAD into the endoplasmic reticulum. J Biol Chem 281 21445 21457
40. WeissmanZ
KornitzerD
2004 A family of Candida cell surface haem-binding proteins involved in haemin and haemoglobin-iron utilization. Mol Microbiol 53 1209 1220
41. BraunBR
HeadWS
WangMX
JohnsonAD
2000 Identification and characterization of TUP1-regulated genes in Candida albicans. Genetics 156 31 44
42. MatthewsR
HodgettsS
BurnieJ
1995 Preliminary assessment of a human recombinant antibody fragment to hsp90 in murine invasive candidiasis. J Infect Dis 171 1668 1671
43. MatthewsR
BurnieJ
TabaqchaliS
1984 Immunoblot analysis of the serological response in systemic candidosis. Lancet 2 1415 1418
44. HubeB
2004 From commensal to pathogen: stage - and tissue-specific gene expression of Candida albicans. Curr Opin Microbiol 7 336 341
45. BiswasS
Van DijckP
DattaA
2007 Environmental Sensing and Signal Transduction Pathways Regulating Morphopathogenic Determinants of Candida albicans. Microbiol Mol Biol Rev 71 348 376
46. KinnebergKM
BendelCM
JechorekRP
CebelinskiEA
GaleCA
1999 Effect of INT1 Gene on Candida albicans Murine Intestinal Colonization. Journal of Surgical Research 87 245 251
47. BendelC
KinnebergK
JechorekR
GaleC
ErlandsenS
1999 Systemic infection following intravenous inoculation of mice with Candida albicans int1 mutant strains. Mol Genet Metab 67 343 351
48. WhiteSJ
RosenbachA
LephartP
NguyenD
BenjaminA
2007 Self-regulation of Candida albicans population size during GI colonization. PLoS Pathog 3 e184 doi:10.1371/journal.ppat.0030184
49. GiraldoP
Von NonwaskonskiA
GomesFAM
LinharesI
NevesNA
2000 Vaginal colonization by Candida in asymptomatic women with and without a history of recurrent vulvovaginal candidiasis. Obstetrics & Gynecology 95 413 416
50. TomsikovaA
TomaierovaV
KotalL
NovackovaD
1980 An immunologic study of vaginal candidiasis. Int J Gynaecol Obstet 18 398 403
51. SosinskaGJ
de GrootPWJ
Teixeira de MattosMJ
DekkerHL
de KosterCG
2008 Hypoxic conditions and iron restriction affect the cell-wall proteome of Candida albicans grown under vagina-simulative conditions. Microbiology 154 510 520
52. LanC
RodarteG
MurilloL
JonesT
DavisR
2004 Regulatory networks affected by iron availability in Candida albicans. Mol Microbiol 53 1451 1469
53. RamsdaleM
SelwayL
SteadD
WalkerJ
YinZ
2008 MNL1 regulates weak acid-induced stress responses of the fungal pathogen Candida albicans. Mol Biol Cell 19 4393 4403
54. CannonRD
LampingE
HolmesAR
NiimiK
TanabeK
2007 Candida albicans drug resistance another way to cope with stress. Microbiology 153 3211 3217
55. EnjalbertB
MacCallumDM
OddsFC
BrownAJ
2007 Niche-specific activation of the oxidative stress response by the pathogenic fungus Candida albicans. Infect Immun 75 2143 2151
56. PendrakML
YanSS
RobertsDD
2004 Sensing the host environment: recognition of hemoglobin by the pathogenic yeast Candida albicans. Arch Biochem Biophys 426 148 156
57. MatthewsRC
RiggG
HodgettsS
CarterT
ChapmanC
2003 Preclinical assessment of the efficacy of mycograb, a human recombinant antibody against fungal HSP90. Antimicrob Agents Chemother 47 2208 2216
58. PachlJ
SvobodaP
JacobsF
VandewoudeK
van der HovenB
2006 A randomized, blinded, multicenter trial of lipid-associated amphotericin B alone versus in combination with an antibody-based inhibitor of heat shock protein 90 in patients with invasive candidiasis. Clin Infect Dis 42 1404 1413
59. HanY
RiesselmanMH
CutlerJE
2000 Protection against candidiasis by an immunoglobulin G3 (IgG3) monoclonal antibody specific for the same mannotriose as an IgM protective antibody. Infect Immun 68 1649 1654
60. HanY
UlrichMA
CutlerJE
1999 Candida albicans mannan extract-protein conjugates induce a protective immune response against experimental candidiasis. J Infect Dis 179 1477 1484
61. ClancyCJ
NguyenML
ChengS
HuangH
FanG
2008 Immunoglobulin G responses to a panel of Candida albicans antigens as accurate and early markers for the presence of systemic candidiasis. J Clin Microbiol 46 1647 1654
62. BraunBR
van Het HoogM
d'EnfertC
MartchenkoM
DunganJ
2005 A human-curated annotation of the Candida albicans genome. PLoS Genet 1 e1 doi:10.1371/journal.pgen.0010001
63. FanJ
ChaturvediV
ShenSH
2002 Identification and phylogenetic analysis of a glucose transporter gene family from the human pathogenic yeast Candida albicans. J Mol Evol 55 336 346
64. MonteolivaL
MatasML
GilC
NombelaC
PlaJ
2002 Large-scale identification of putative exported proteins in Candida albicans by genetic selection. Eukaryot Cell 1 514 525
65. De GrootPW
HellingwerfKJ
KlisFM
2003 Genome-wide identification of fungal GPI proteins. Yeast 20 781 796
66. UrbanC
SohnK
LottspeichF
BrunnerH
RuppS
2003 Identification of cell surface determinants in Candida albicans reveals Tsa1p, a protein differentially localized in the cell. FEBS Lett 544 228 235
67. DaviesDH
LiangX
HernandezJE
RandallA
HirstS
2005 Profiling the humoral immune response to infection by using proteome microarrays: high-throughput vaccine and diagnostic antigen discovery. Proc Natl Acad Sci U S A 102 547 552
68. IdekerT
ThorssonV
SiegelAF
HoodLE
2000 Testing for Differentially-Expressed Genes by Maximum-Likelihood Analysis of Microarray Data. Journal of Computational Biology 7 805 817
69. BaldiP
LongAD
2001 A Bayesian framework for the analysis of microarray expression data: regularized t -test and statistical inferences of gene changes. Bioinformatics 17 509 519
70. DurbinBP
HardinJS
HawkinsDM
RockeDM
2002 A variance-stabilizing transformation for gene-expression microarray data. Bioinformatics 18 Suppl 1 S105 110
71. SundareshS
DoolanDL
HirstS
MuY
UnalB
2006 Identification of humoral immune responses in protein microarrays using DNA microarray data analysis techniques. Bioinformatics 22 1760 1766
72. SundareshS
RandallA
UnalB
PetersenJM
BelisleJT
2007 From protein microarrays to diagnostic antigen discovery: a study of the pathogen Francisella tularensis. Bioinformatics 23 i508 518
73. HuberW
von HeydebreckA
SultmannH
PoustkaA
VingronM
2002 Variance stabilization applied to microarray data calibration and to the quantification of differential expression. Bioinformatics 18 Suppl 1 S96 104
74. KreilDP
KarpNA
LilleyKS
2004 DNA microarray normalization methods can remove bias from differential protein expression analysis of 2D difference gel electrophoresis results. Bioinformatics 20 2026 2034
75. BarbacioruCC
WangY
CanalesRD
SunYA
KeysDN
2006 Effect of various normalization methods on Applied Biosystems expression array system data. BMC Bioinformatics 7 533
76. SarkarD
ParkinR
WymanS
BendoraiteA
SatherC
2009 Quality assessment and data analysis for microRNA expression arrays. Nucleic Acids Res 37 e17
77. BaldiP
Brunak Sr
2001 Bioinformatics: the machine learning approach: MIT Press. 400 p
78. HochbergY
BenjaminiY
1990 More powerful procedures for multiple significance testing. Stat Med 9 811 818
Štítky
Hygiena a epidemiologie Infekční lékařství Laboratoř
Článek vyšel v časopisePLOS Pathogens
Nejčtenější tento týden
2010 Číslo 3- Jak souvisí postcovidový syndrom s poškozením mozku?
- Měli bychom postcovidový syndrom léčit antidepresivy?
- Farmakovigilanční studie perorálních antivirotik indikovaných v léčbě COVID-19
- 10 bodů k očkování proti COVID-19: stanovisko České společnosti alergologie a klinické imunologie ČLS JEP
-
Všechny články tohoto čísla
- All Mold Is Not Alike: The Importance of Intraspecific Diversity in Necrotrophic Plant Pathogens
- Tsetse EP Protein Protects the Fly Midgut from Trypanosome Establishment
- Perforin and IL-2 Upregulation Define Qualitative Differences among Highly Functional Virus-Specific Human CD8 T Cells
- N-Acetylglucosamine Induces White to Opaque Switching, a Mating Prerequisite in
- Origin and Evolution of Sulfadoxine Resistant
- Rapid Evolution of Pandemic Noroviruses of the GII.4 Lineage
- Natural Strain Variation and Antibody Neutralization of Dengue Serotype 3 Viruses
- Fine-Tuning Translation Kinetics Selection as the Driving Force of Codon Usage Bias in the Hepatitis A Virus Capsid
- Structural Basis of Cell Wall Cleavage by a Staphylococcal Autolysin
- Direct Visualization by Cryo-EM of the Mycobacterial Capsular Layer: A Labile Structure Containing ESX-1-Secreted Proteins
- Lipopolysaccharide Is Synthesized via a Novel Pathway with an Evolutionary Connection to Protein -Glycosylation
- MicroRNA Antagonism of the Picornaviral Life Cycle: Alternative Mechanisms of Interference
- Limited Trafficking of a Neurotropic Virus Through Inefficient Retrograde Axonal Transport and the Type I Interferon Response
- Direct Restriction of Virus Release and Incorporation of the Interferon-Induced Protein BST-2 into HIV-1 Particles
- RNAIII Binds to Two Distant Regions of mRNA to Arrest Translation and Promote mRNA Degradation
- Direct TLR2 Signaling Is Critical for NK Cell Activation and Function in Response to Vaccinia Viral Infection
- The Essentials of Protein Import in the Degenerate Mitochondrion of
- Dynamic Imaging of Experimental Induced Hepatic Granulomas Detects Kupffer Cell-Restricted Antigen Presentation to Antigen-Specific CD8 T Cells
- An Accessory to the ‘Trinity’: SR-As Are Essential Pathogen Sensors of Extracellular dsRNA, Mediating Entry and Leading to Subsequent Type I IFN Responses
- Innate Killing of by Macrophages of the Splenic Marginal Zone Requires IRF-7
- Exoerythrocytic Parasites Secrete a Cysteine Protease Inhibitor Involved in Sporozoite Invasion and Capable of Blocking Cell Death of Host Hepatocytes
- Inhibition of Macrophage Migration Inhibitory Factor Ameliorates Ocular -Induced Keratitis
- Membrane Damage Elicits an Immunomodulatory Program in
- Fatal Transmissible Amyloid Encephalopathy: A New Type of Prion Disease Associated with Lack of Prion Protein Membrane Anchoring
- Nucleophosmin Phosphorylation by v-Cyclin-CDK6 Controls KSHV Latency
- A Combination of Independent Transcriptional Regulators Shapes Bacterial Virulence Gene Expression during Infection
- Inhibition of Host Vacuolar H-ATPase Activity by a Effector
- Human Cytomegalovirus Protein pUL117 Targets the Mini-Chromosome Maintenance Complex and Suppresses Cellular DNA Synthesis
- Dispersion as an Important Step in the Biofilm Developmental Cycle
- Kaposi's Sarcoma-Associated Herpesvirus ORF57 Protein Binds and Protects a Nuclear Noncoding RNA from Cellular RNA Decay Pathways
- Differential Regulation of Effector- and Central-Memory Responses to Infection by IL-12 Revealed by Tracking of Tgd057-Specific CD8+ T Cells
- The Human Polyoma JC Virus Agnoprotein Acts as a Viroporin
- Expansion, Maintenance, and Memory in NK and T Cells during Viral Infections: Responding to Pressures for Defense and Regulation
- T Cell-Dependence of Lassa Fever Pathogenesis
- HIV and Mature Dendritic Cells: Trojan Exosomes Riding the Trojan Horse?
- Endocytosis of the Anthrax Toxin Is Mediated by Clathrin, Actin and Unconventional Adaptors
- A Capsid-Encoded PPxY-Motif Facilitates Adenovirus Entry
- Homeostatic Interplay between Bacterial Cell-Cell Signaling and Iron in Virulence
- Serological Profiling of a Protein Microarray Reveals Permanent Host-Pathogen Interplay and Stage-Specific Responses during Candidemia
- YfiBNR Mediates Cyclic di-GMP Dependent Small Colony Variant Formation and Persistence in
- PLOS Pathogens
- Archiv čísel
- Aktuální číslo
- Informace o časopisu
Nejčtenější v tomto čísle- Kaposi's Sarcoma-Associated Herpesvirus ORF57 Protein Binds and Protects a Nuclear Noncoding RNA from Cellular RNA Decay Pathways
- Endocytosis of the Anthrax Toxin Is Mediated by Clathrin, Actin and Unconventional Adaptors
- Perforin and IL-2 Upregulation Define Qualitative Differences among Highly Functional Virus-Specific Human CD8 T Cells
- Inhibition of Macrophage Migration Inhibitory Factor Ameliorates Ocular -Induced Keratitis
Kurzy
Zvyšte si kvalifikaci online z pohodlí domova
Současné možnosti léčby obezity
nový kurzAutoři: MUDr. Martin Hrubý
Všechny kurzyPřihlášení#ADS_BOTTOM_SCRIPTS#Zapomenuté hesloZadejte e-mailovou adresu, se kterou jste vytvářel(a) účet, budou Vám na ni zaslány informace k nastavení nového hesla.
- Vzdělávání



