-
Články
Top novinky
Reklama- Vzdělávání
- Časopisy
Top články
Nové číslo
- Témata
Top novinky
Reklama- Videa
- Podcasty
Nové podcasty
Reklama- Kariéra
Doporučené pozice
Reklama- Praxe
Top novinky
ReklamaValidation of a genetic risk score for atrial fibrillation: A prospective multicenter cohort study
In prospective cohort study, Eric Topol and colleague validate a genetic risk score for identification of patients at the highest risk of developing atrial fibrillation.
Published in the journal: . PLoS Med 15(3): e32767. doi:10.1371/journal.pmed.1002525
Category: Research Article
doi: https://doi.org/10.1371/journal.pmed.1002525Summary
In prospective cohort study, Eric Topol and colleague validate a genetic risk score for identification of patients at the highest risk of developing atrial fibrillation.
Introduction
Stroke remains the fifth leading cause of death in the United States, despite increased recognition and better management of overall cardiovascular disease risk, which has led to a decline in stroke mortality [1]. More than 750,000 people experience a stroke event each year in the US, with a prevalence of 2.6% in the US adult population [1]. While conventional risk factors for stroke—including cigarette smoking, hypertension, diabetes mellitus, dyslipidemia, and heart failure—account for a sizable portion of stroke episodes, atrial fibrillation (AF) is associated with a quarter of all stroke events [2–4].
AF is the most common pathological cardiac arrhythmia, present in nearly 6 million people in the US alone, with the prevalence estimated to grow to over 12 million people by 2030 [5]. It is not uncommon for AF to remain undetected in asymptomatic individuals. AF has been documented in asymptomatic individuals not only in patients with implanted cardiac devices [6,7], but also in population-based screening studies using smartphone electrocardiogram (ECG) sensors [8–11]. These efforts to better diagnose subclinical, asymptomatic AF may be useful for implementing appropriate therapies to reduce the risk of stroke [12].
To this end, efforts have been made to predict the occurrence of AF using risk scores based on clinical factors associated with disease [13,14]. While clinical risk factors for AF (e.g., obesity, hypertension, and obstructive sleep apnea) are well established, risk scores incorporating these factors have fallen short in validation studies [15]. Therefore, efforts continue to improve risk prediction by incorporating genetic risk factors. Genetic factors are estimated to account for ~40% of a person’s total AF risk [16], and genome-wide association studies (GWASs) of increasing size have identified multiple single nucleotide polymorphisms (SNPs) associated with AF on the genome-wide level [17–23]. For AF, several genetic risk scores (GRSs) have been characterized and tested in various studies, illustrating their ability to identify individuals at increased risk of AF [24–29]. But some of these findings pertain to a lifetime risk of AF or >14 years of follow-up, and have not yet provided any insight on immediate risk for an individual with established risk factors presenting with symptoms.
Here, in this multicenter study of symptomatic participants without prior diagnosis of AF, we aimed to prospectively validate a 12-SNP AF GRS for identifying patients at an increased risk for AF during 2 weeks of ambulatory cardiac rhythm monitoring.
Methods
Participant recruitment and inclusion and exclusion criteria
The study was approved by the institutional review board (IRB) at the Scripps Clinic (La Jolla, CA), which provided overall study oversight, in addition to the individual IRBs affiliated with each recruitment center. Participants were enrolled from December 2, 2013, through January 19, 2016. The complete list of recruitment centers is provided in S1 Table. Informed consent was provided by each patient prior to enrollment. Patients presenting with any symptoms suggestive of AF determined by the clinician to necessitate ambulatory cardiac rhythm monitoring were evaluated for inclusion in this study. Patients were eligible for enrollment if they were 40 years of age or older and were capable of providing informed consent in addition to providing a blood sample for genetic analysis. Study participants were also required to have at least 1 of the following clinical characteristics: hypertension, ischemic stroke with no defined etiology within the past 6 months, high BMI (>30 kg/m2), history of heart failure, clinically significant murmur, first degree atrioventricular block (PR interval > 200 ms), chronic kidney disease, hypertrophic cardiomyopathy, congenital heart disease, chronic obstructive pulmonary disease, obstructive sleep apnea, diabetes mellitus, regular excess alcohol consumption (males >14 drinks/week, females >7 drinks/week), or a family history of AF. Patients with a prior diagnosis of AF or atrial flutter were excluded. Additionally, patients with cardiac surgery (coronary artery bypass grafting, valve replacement or repair, pericardial stripping, etc.) within the previous 30 days, with hyperthyroidism, receiving permanent pacing therapy, with skin allergies or sensitivities to adhesives, or who were anticipated to have exposure to high frequency surgical equipment during the monitoring period were not eligible for enrollment. An independent data and safety monitoring board provided ongoing study oversight throughout the trial period. This study (S1 Protocol) was registered with ClinicalTrials.gov (NCT01970969) and is reported as per the TRIPOD guidelines (S1 Checklist).
Cardiac rhythm monitoring and event adjudication
The primary event was an instance of AF/atrial flutter as defined by standard electrocardiographic criteria for a minimum duration of 5 seconds (AF event). AF events were assessed either by ambulatory cardiac rhythm monitoring or on 12-lead ECG. Patients meeting the specified inclusion criteria presenting to an outpatient clinic for evaluation of symptoms with high clinical suspicion for AF were either provided an adhesive patch monitor (Zio patch, iRhythm Technologies), if enrolled at centers within the US, or fitted with a long-term Holter monitor (Spiderflash, Soren Group) at Canadian centers. Participants were instructed to wear the cardiac rhythm monitor for the life of the device (~2 weeks). Symptomatic patients presenting with the first diagnosis of AF on 12-lead ECG were not required to have additional ambulatory cardiac rhythm monitoring. Events that were considered possible occurrences of AF were independently adjudicated by 2 separate physicians with expertise in cardiac rhythm interpretation, with a third physician’s review available for incongruent cases.
Genotyping
DNA was extracted from whole blood using the MagNA Pure 96 instrument and reagent kit (Roche Life Science). SNaPshot multiplex genotyping (Thermo Fisher Scientific) was used to simultaneously genotype 12 SNPs comprising the AF GRS (Table 1).
Tab. 1. Single nucleotide polymorphisms associated with AF used for the determination of the AF GRS. 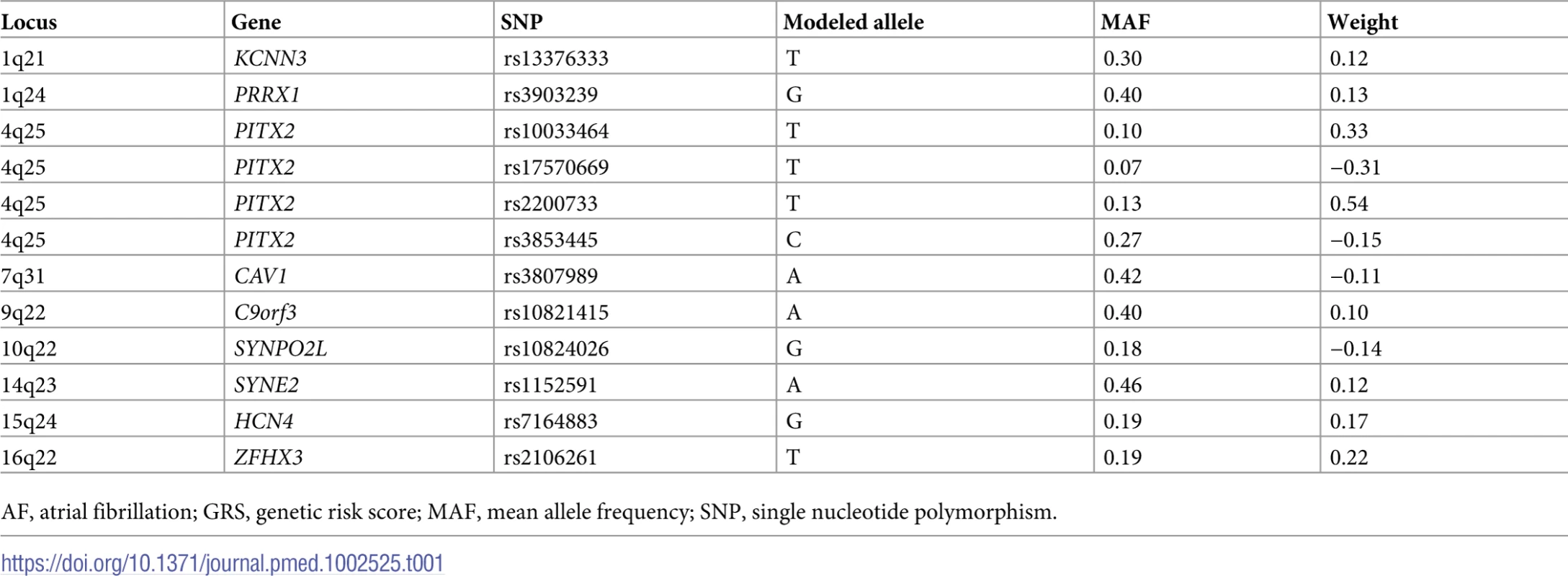
AF, atrial fibrillation; GRS, genetic risk score; MAF, mean allele frequency; SNP, single nucleotide polymorphism. Modeling of GRS and statistical analyses
Comparisons of baseline characteristics between patients with and without detected AF were conducted using chi-squared and t tests for categorical and quantitative traits, respectively. We sought to validate an existing 12-SNP AF GRS that had previously been examined in a retrospective manner [27]. The AF GRS in this study was calculated using a weighted allele-counting approach from previously reported weights [27] (Table 1). Expected AF events in the 2 groups were calculated using reference to previous studies [30,31]. We expected roughly 80 AF events in 1,000 at-risk patients. Using this event rate, and based on a simulation in which the absolute rate of AF increased by 2% per AF GRS quintile (AF rate is half the population average in the lowest quintile and 1.5 times the population average in the highest quintile), we had 90% power to detect an association between AF GRS quintile and AF at an alpha of 5% (S1 Text). To account for the small number of missing genotype data (15 genotypes, 0.14% missing rate across all markers), missing genotypes were replaced with the average genotype at that marker based on additive coding. The association between AF GRS and newly detected AF was assessed using logistic regression. Two approaches to model AF GRS were used: (1) coding the AF GRS as a quantitative, continuous variable and (2) coding the AF GRS as a quantitative variable using quintile categories. Results are presented conditional (adjusted) and not conditional (unadjusted) for the following covariates: age, sex, smoking status, BMI, the presence of diabetes mellitus, and history of hypertension, myocardial infarction, and heart failure. All analyses were performed in R version 3.2.3 (R Project for Statistical Computing).
Results
Patient characteristics
A total of 934 participants were enrolled from December 2, 2013, through January 19, 2016. The final analysis excluded 30 participants who did not provide a blood sample for genotyping, were missing adhesive patch monitor data, or had a prior diagnosis of AF identified upon chart review. Accounting for these exclusions, the final analysis included 904 participants. A total of 85 participants were discovered to have AF from the adhesive patch monitor (n = 44) or ECG (n = 41) during the study. The mean wear time was 10 days and 21 hours for the adhesive patch monitors and 13 days and 18 hours for the long-term Holter monitors. There was no difference in wear time between participants with and without the diagnosis of AF (p = 0.49). The primary presenting indication for which cardiac rhythm monitoring was pursued was palpitations/tachycardia (72%), followed by syncope/near-syncope (14%), transient ischemic attack/stroke (9%), and chest pain/dyspnea (5%).
Baseline characteristics for participants with and without AF are provided in Table 2. The self-reported ethnicity of participants was predominantly white (92.6%), with other ethnicities including African-American (5.2%), Asian (1.7%), and Native American (0.2%). The mean age for participants with AF (68.5 years [SD 11.2]) was greater than for participants without AF (65.9 years [SD 11.8], p = 0.046). Men made up the majority of participants with AF (52%) and the minority for participants without AF (36%). Participants with AF had a higher mean BMI (31.7 kg/m2) than the group without AF (29.4 kg/m2, p = 0.02), but the prevalence of diabetes was lower (13% for those with AF compared with 23% for those without AF, p = 0.04). There were no intergroup differences in the prevalence of the other comorbidities evaluated. Additionally, the stroke risk as evaluated by CHADS2 and CHA2DS2-VASc scores did not differ between the 2 groups.
Tab. 2. Baseline characteristics. 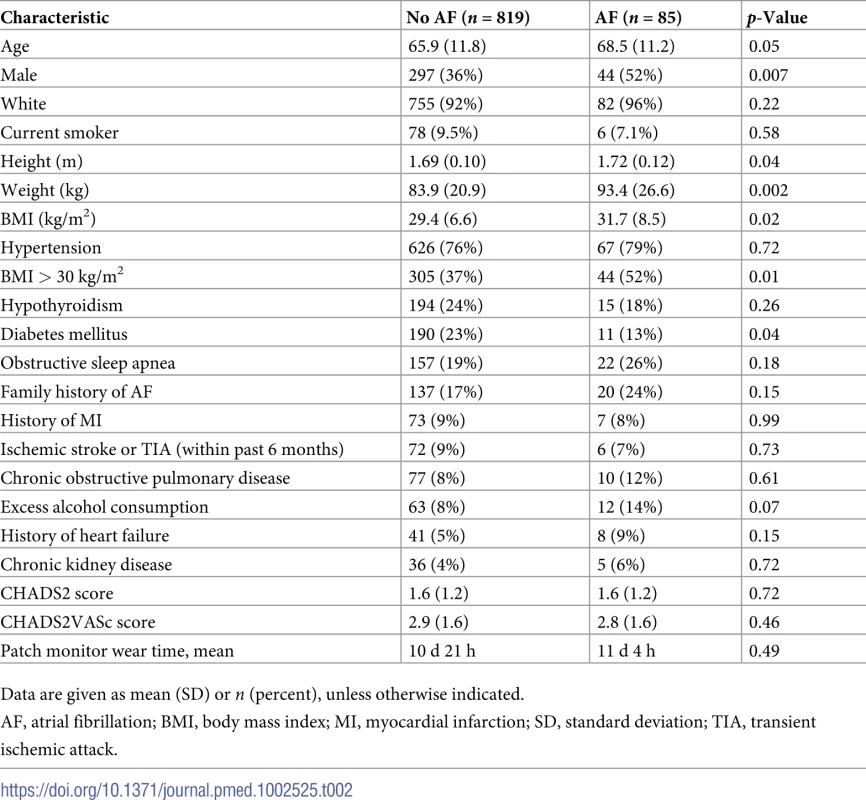
Data are given as mean (SD) or n (percent), unless otherwise indicated. AF GRS and AF events
The AF GRS was calculated as a weighted sum of the 12 SNPs (Table 1) for each participant based on their genotype for these SNPS, and the scores ranged from −0.84 to 1.78. The mean AF GRS for the 85 participants diagnosed with AF during the study was significantly higher than the mean AF GRS for the 819 participants without AF (mean [SD]: 0.582 [0.378] versus 0.439 [0.382], p = 0.001). The incidence of AF increased across increasing quintiles of AF GRS (Table 3), with the odds per SD increase in AF GRS increasing by a factor of 1.43 (95% CI 1.15–1.77; p = 0.001). In an unadjusted analysis, participants in the highest quintile of AF GRS (>0.77) had an increased risk of having an AF event during the course of the study (odds ratio [OR] 2.83; 95% CI 1.21–6.61; p = 0.02) as compared with participants in the lowest AF GRS quintile. After adjusting for age, sex, smoking status, BMI, diabetes mellitus, hypertension, prior myocardial infarction, and heart failure, the odds per SD increase in AF GRS increased by a factor of 1.45 (95% CI 1.16–1.83; p = 0.001), with participants in the highest AF GRS quintile having greater than 3 times the odds (OR 3.11; 95% CI 1.27–7.58; p = 0.01) of AF diagnosis compared with those at lowest AF GRS quintile (Table 3). Modeling AF GRS increased the C-statistic from 0.687 to 0.719 over a model that considered only age, sex, smoking status, BMI, diabetes mellitus, hypertension, prior myocardial infarction, and heart failure (p = 0.001). Additionally, when the AF GRS was assessed according to GRS tertiles, the highest AF GRS tertile had greater than 2 times the risk of an AF event compared to the lowest tertile (unadjusted OR 2.26; 95% CI 1.27–4.01; p < 0.01; adjusted OR 2.32; 95% CI 1.28–4.20; p = 0.006). Alternative time-to-event approaches are not presented due to the short AF monitoring period, though the results were consistent with the logisticregression results.
Tab. 3. Risk estimates of AF events according to AF GRS quintile (12 SNPs). 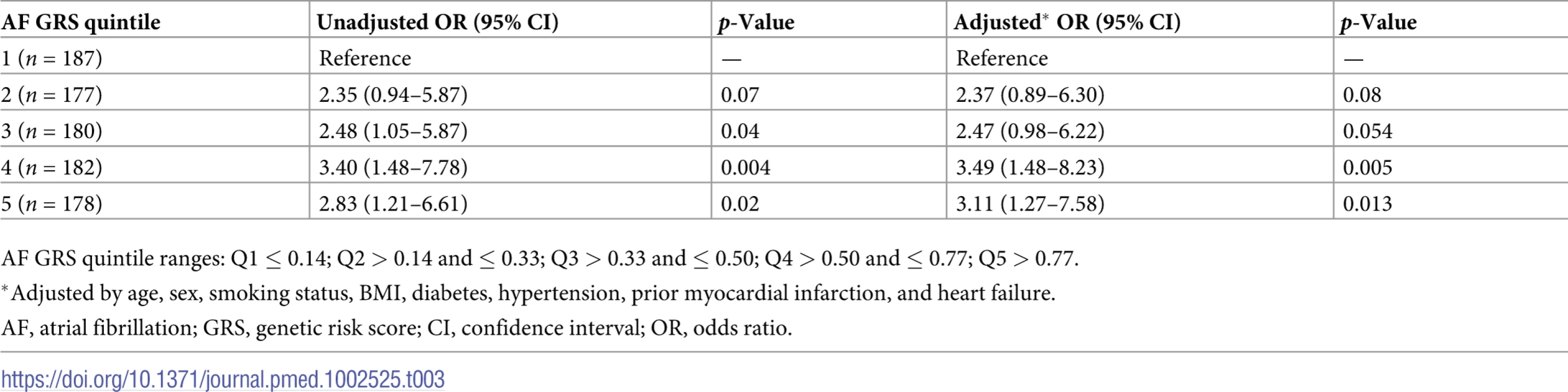
AF GRS quintile ranges: Q1 ≤ 0.14; Q2 > 0.14 and ≤ 0.33; Q3 > 0.33 and ≤ 0.50; Q4 > 0.50 and ≤ 0.77; Q5 > 0.77. In an effort to examine the individual contributions of the 12 SNPs that composed the AF GRS, we evaluated the association of each SNP with AF in both unadjusted and adjusted models (S2 Table), though this study was not well powered to detect individual marker effects. Eleven of the 12 SNPs were consistent with prior results: either the direction of the effect allele was consistent with previous reports, or the result was not nominally significant (p < 0.05). However, rs10033464 (4q25, PITX2) displayed a risk estimate in the opposite direction than had been previously reported by others. This discrepancy appears to be in part due to linkage disequilibrium between this marker and the nearby SNP with the strongest association in this gene, rs2200733 (p = 0.005). We and others have observed that the risk alleles at these markers are negatively associated with each other. There remains uncertainty in the optimal genetic risk model for AF, and superior models will certainly evolve in the future as more genetic discoveries are made. In this light, we also considered a modified AF GRS that included only the most strongly associated SNP in each gene—which is a common solution in GRS estimation to eliminate confounding due to linkage disequilibrium [32]. The resulting 9-SNP model included rs2200733 for PITX2 and the other 8 SNPs from the other genes. The risk of AF with this modified AF GRS, as in the 12-SNP model, was greater for the highest AF GRS quintile than for the lowest AF GRS quintile (OR 5.07; 95% CI 2.04–12.60; p < 0.001), and this model appeared to better differentiate risk of AF throughout the distribution of genetic risk (S3 Table). As expected, the risk estimates derived for both AF GRS models remained significant in an analysis limited to participants who self-reported as white (S4 Table).
Discussion
We aimed to assess the ability of a previously developed AF GRS comprising 12 common SNPs (minor allele frequency > 5%) that have been found to be associated with AF at a genome-wide significance level to identify patients at the highest risk of developing AF in a prospective manner. Indeed, in this cohort of 904 participants of predominantly white ethnicity, 85 had AF events, and participants in the highest quintile of AF GRS had a risk greater than 3 times that of participants in the lowest AF GRS quintile. These findings are consistent with the original report [27] of this specific AF GRS, in addition to other studies utilizing a multi-allele GRS [26,28]; however, all of these studies were conducted on a retrospective basis.
By harnessing advanced technology to realize the benefits of long-term cardiac rhythm monitoring using an adhesive patch monitor in lieu of the dated 24-hour Holter monitor [33], participants were monitored for over 10 days after presenting to a clinic with specific symptoms prompting cardiac rhythm monitoring with a suspicion for AF. It has become clear that extended periods of ambulatory cardiac rhythm monitoring increase the yield of AF detection, especially in patients with cryptogenic stroke [34]. AF is the most common arrhythmia, and with age being an important risk factor, its prevalence is estimated to increase steadily as humans live longer and with more chronic disease. While documented AF accounts for 1 out of every 6 strokes, a quarter of all strokes are initially categorized as “cryptogenic” with no identifiable cause. With prolonged rhythm monitoring strategies, many of these cryptogenic strokes are subsequently attributed to AF [12,34–36]. An AF GRS may help identify individuals at the highest risk of subclinical and paroxysmal AF who would benefit from a cardiac rhythm monitoring strategy even before a devastating stoke event. Improving identification of patients with AF, and initiating appropriate anticoagulant therapies when appropriate, is important given the risk of embolic stroke, which is more likely to be associated with major neurological deficits than non-embolic stroke [37].
To date, the relative risk of AF associated with individual SNPs ranges from just above 1 to a highest value of 1.64 (rs6817105, PITX2). Thus, the ability to combine common SNPs into an AF GRS with the ability to differentiate a greater than 3-fold increased risk of AF in a population on a prospective basis may be useful. Such a panel of SNPs could be assayed at low cost and be used in conjunction with an evaluation of a patient with possible AF. For example, even 10 days of patch-based monitoring may not yield the diagnosis of subclinical AF and indicate that additional monitoring would be useful [34,35].
Several limitations of our study should be examined. Despite our efforts to recruit patients from various geographic regions across the US and Canada ranging from rural to urban settings, the vast majority of participants (93%) self-reported as white, with only minor representation from other ethnicities. The bulk of our understanding of genetic variants in association with disease has come from GWASs in populations of European ancestry, such that considerable assessment in other ancestries is important, and the 12-SNP panel we used in the study cannot be extrapolated beyond those of European ancestry [38,39]. With the inclusion of more ethnically diverse populations in genetic studies, the importance of ethnicity in determining the association of SNPs with disease will be magnified and will certainly need to be accounted for in future GRS calculations [40,41]. It was recently shown that rs10824026 (10q22), 1 of the SNPs utilized in the current AF GRS, conferred a greater risk for AF in white individuals than in black individuals [42]. Although the current study is underpowered to assess AF risk by ethnicity, self-identified African-American participants in this study were far more likely to carry the risk allele (G) (53% GA and 38% GG) compared to self-identified white participants (26% GA and 2% GG).
Since the initiation of our study, additional SNPs associated with AF have been identified, and we expect this trend to continue as the genetic datasets expand. Our AF GRS did not include 5 recently discovered SNPs [43], though 1 of these SNPs was specific for a Japanese population and the others had lower relative risks than the SNPs already included in our AF GRS. Additionally, our preliminary finding that demonstrated greater differentiation in AF based on a 9-SNP (1 SNP per gene) model simply shows that improvements can be made. Future efforts in developing polygenetic risk predictors of AF should focus on optimizing the set of markers and, potentially, population-specific weights assigned to individual markers. Yet, improving the predictive performance of a risk score solely based on genetic data will reach an upper limit [44]. As additional AF biomarkers are determined through multi-omics approaches (proteomics, lipidomics, and metabolomics) or multiparameter physiological sensors, the addition of more complex clinical, physiological, and biomarker components to the AF GRS will be an exciting next step to developing a comprehensive AF risk score.
In terms of AF events, the mean monitoring time for patients evaluated with adhesive patch monitoring was less than 11 days, and there could have been patients for whom we did not capture their AF event during this time. Prolonged monitoring periods, as have been achieved using implantable monitoring devices, have been shown to detect increasingly more AF events over time, especially in patients with cryptogenic stroke [34–36]. Currently, there is little guidance regarding optimal length of monitoring. While we do not feel that the future of diagnostic ambulatory cardiac rhythm monitoring is grounded in expensive, implantable devices, this role may instead be filled using unobtrusive and passive wearables. A SNP-based AF GRS, however, provides a fixed overall lifetime genetic risk assessment for AF, and given the short-term follow-up time in the current study, we expect that the ability of the AF GRS to identify individuals with the highest AF risk would likely increase with a longer monitoring period and follow-up. Likewise, we illustrate the strength of a GRS-based approach to disease screening and demonstrate the ability of the AF GRS to temporally stratify symptomatic patients with the probability of an AF diagnosis during 2 weeks of rhythm monitoring. In doing so, we have moved from the typical retrospective GWAS, without temporal association, to a prospective GRS screen that leverages the genomic risk for an individual under evaluation.
In conclusion, we prospectively validated a GRS for AF that may prove useful in the diagnostic evaluation of certain individuals who are being assessed for subclinical presence of this arrhythmia, and potentially as a means to help its prevention in the future.
Supporting Information
Zdroje
1. Writing Group Members, Mozaffarian D, Benjamin EJ, Go AS, Arnett DK, Blaha MJ, et al. Heart disease and stroke statistics—2016 update: a report from the American Heart Association. Circulation. 2016;133: e38–360. doi: 10.1161/CIR.0000000000000350 26673558
2. Healey JS, Connolly SJ, Gold MR, Israel CW, Van Gelder IC, Capucci A, et al. Subclinical atrial fibrillation and the risk of stroke. N Engl J Med. 2012;366 : 120–9. doi: 10.1056/NEJMoa1105575 22236222
3. Wolf PA, Kannel WB, Thomas HE, Dawber TR. Epidemiologic assessment of chronic atrial fibrillation and risk of stroke: The Framingham study. Neurology. 1978;28 : 973–7. 570666
4. Wolf PA, Abbott RD, Kannel WB. Atrial fibrillation: a major contributor to stroke in the elderly. The Framingham study. Arch Intern Med. 1987;147 : 1561–4. 3632164
5. Colilla S, Crow A, Petkun W, Singer DE, Simon T, Liu X. Estimates of current and future incidence and prevalence of atrial fibrillation in the U.S. adult population. Am J Cardiol. 2013;112 : 1142–7. doi: 10.1016/j.amjcard.2013.05.063 23831166
6. Glotzer TV, Hellkamp AS, Zimmerman J, Sweeney MO, Yee R, Marinchak R, et al. Atrial high rate episodes detected by pacemaker diagnostics predict death and stroke: report of the Atrial Diagnostics Ancillary Study of the MOde Selection Trial (MOST). Circulation. 2003;107 : 1614–9. doi: 10.1161/01.CIR.0000057981.70380.45 12668495
7. Glotzer TV, Daoud EG, Wyse DG, Singer DE, Ezekowitz MD, Hilker C, et al. The relationship between daily atrial tachyarrhythmia burden from implantable device diagnostics and stroke risk: the TRENDS study. Circ Arrhythm Electrophysiol. 2009;2 : 474–80. doi: 10.1161/CIRCEP.109.849638 19843914
8. Kaasenbrood F, Hollander M, Rutten FH, Gerhards LJ, Hoes AW, Tieleman RG. Yield of screening for atrial fibrillation in primary care with a hand-held, single-lead electrocardiogram device during influenza vaccination. Europace. 2016;18 : 1514–20. doi: 10.1093/europace/euv426 26851813
9. Chan N, Choy C. Screening for atrial fibrillation in 13 122 Hong Kong citizens with smartphone electrocardiogram. Heart. 2017;103 : 24–31. doi: 10.1136/heartjnl-2016-309993 27733533
10. Lowres N, Neubeck L, Salkeld G, Krass I, McLachlan AJ, Redfern J, et al. Feasibility and cost-effectiveness of stroke prevention through community screening for atrial fibrillation using iPhone ECG in pharmacies. The SEARCH-AF study. Thromb Haemost. 2014;111 : 1167–76. doi: 10.1160/TH14-03-0231 24687081
11. Svennberg E, Engdahl J, Al-Khalili F, Friberg L, Frykman V, Rosenqvist M. Mass screening for untreated atrial fibrillation: the STROKESTOP study. Circulation. 2015;131 : 2176–84. doi: 10.1161/CIRCULATIONAHA.114.014343 25910800
12. Hess PL, Healey JS, Granger CB, Connolly SJ, Ziegler PD, Alexander JH, et al. the role of cardiovascular implantable electronic devices in the detection and treatment of subclinical atrial fibrillation. JAMA Cardiol. 2017;;2 : 324–31. doi: 10.1001/jamacardio.2016.5167 28097334
13. Alonso A, Norby FL. Predicting atrial fibrillation and its complications. Circ J. 2016;80 : 1061–6. doi: 10.1253/circj.CJ-16-0239 27008924
14. Christophersen IE, Yin X, Larson MG, Lubitz SA, Magnani JW, McManus DD, et al. A comparison of the CHARGE-AF and the CHA2DS2-VASc risk scores for prediction of atrial fibrillation in the Framingham Heart Study. Am Heart J. 2016;178 : 45–54. doi: 10.1016/j.ahj.2016.05.004 27502851
15. Kolek MJ, Graves AJ, Xu M, Bian A, Teixeira PL, Shoemaker MB, et al. Evaluation of a prediction model for the development of atrial fibrillation in a repository of electronic medical records. JAMA Cardiol. 2016;1 : 1007–13. doi: 10.1001/jamacardio.2016.3366 27732699
16. Lubitz SA, Yin X, Fontes JD, Magnani JW, Rienstra M, Pai M, et al. Association between familial atrial fibrillation and risk of new-onset atrial fibrillation. JAMA. 2010;304 : 2263–9. doi: 10.1001/jama.2010.1690 21076174
17. Gudbjartsson DF, Arnar DO, Helgadottir A, Gretarsdottir S, Holm H, Sigurdsson A, et al. Variants conferring risk of atrial fibrillation on chromosome 4q25. Nature. 2007;448 : 353–7. doi: 10.1038/nature06007 17603472
18. Lubitz SA, Sinner MF, Lunetta KL, Makino S, Pfeufer A, Rahman R, et al. Independent susceptibility markers for atrial fibrillation on chromosome 4q25. Circulation. 2010;122 : 976–84. doi: 10.1161/CIRCULATIONAHA.109.886440 20733104
19. Benjamin EJ, Rice KM, Arking DE, Pfeufer A, van Noord C, Smith AV, et al. Variants in ZFHX3 are associated with atrial fibrillation in individuals of European ancestry. Nat Genet. 2009;41 : 879–81. doi: 10.1038/ng.416 19597492
20. Ellinor PT, Lunetta KL, Glazer NL, Pfeufer A, Alonso A, Chung MK, et al. Common variants in KCNN3 are associated with lone atrial fibrillation. Nat Genet. 2010;42 : 240–4. doi: 10.1038/ng.537 20173747
21. Ellinor PT, Lunetta KL, Albert CM, Glazer NL, Ritchie MD, Smith AV, et al. Meta-analysis identifies six new susceptibility loci for atrial fibrillation. Nat Genet. 2012;44 : 670–5. doi: 10.1038/ng.2261 22544366
22. Christophersen IE, Rienstra M, Roselli C, Yin X, Geelhoed B, Barnard J, et al. Large-scale analyses of common and rare variants identify 12 new loci associated with atrial fibrillation. Nat Genet. 2017;49 : 946–52. doi: 10.1038/ng.3843 28416818
23. Tucker NR, Clauss S, Ellinor PT. Common variation in atrial fibrillation: navigating the path from genetic association to mechanism. Cardiovasc Res. 2016;109 : 493–501. doi: 10.1093/cvr/cvv283 26733238
24. Goldstein BA, Yang L, Salfati E, Assimes TL. Contemporary considerations for constructing a genetic risk score: an empirical approach. Genet Epidemiol. 2015;39 : 439–45. doi: 10.1002/gepi.21912 26198599
25. Smith JA, Ware EB, Middha P, Beacher L, Kardia SLR. Current applications of genetic risk scores to cardiovascular outcomes and subclinical phenotypes. Curr Epidemiol Rep. 2015;2 : 180–90. doi: 10.1007/s40471-015-0046-4 26269782
26. Everett BM, Cook NR, Conen D, Chasman DI, Ridker PM, Albert CM. Novel genetic markers improve measures of atrial fibrillation risk prediction. Eur Heart J. 2013;34 : 2243–51. doi: 10.1093/eurheartj/eht033 23444395
27. Tada H, Shiffman D, Smith JG, Sjögren M, Lubitz SA, Ellinor PT, et al. Twelve-single nucleotide polymorphism genetic risk score identifies individuals at increased risk for future atrial fibrillation and stroke. Stroke. 2014;45 : 2856–62. doi: 10.1161/STROKEAHA.114.006072 25123217
28. Lubitz SA, Lunetta KL, Lin H, Arking DE, Trompet S, Li G, et al. Novel genetic markers associate with atrial fibrillation risk in Europeans and Japanese. J Am Coll Cardiol. 2014;63 : 1200–10. doi: 10.1016/j.jacc.2013.12.015 24486271
29. Lubitz SA, Yin X, Lin HJ, Kolek M, Smith JG, Trompet S, et al. Genetic risk prediction of atrial fibrillation. Circulation. 2017;135 : 1311–20. doi: 10.1161/CIRCULATIONAHA.116.024143 27793994
30. Schnabel RB, Sullivan LM, Levy D, Pencina MJ, Massaro JM, D’Agostino RB, et al. Development of a risk score for atrial fibrillation (Framingham Heart Study): a community-based cohort study. Lancet. 2009;373 : 739–45. doi: 10.1016/S0140-6736(09)60443-8 19249635
31. Liao J, Khalid Z, Scallan C, Morillo C, O’Donnell M. Noninvasive cardiac monitoring for detecting paroxysmal atrial fibrillation or flutter after acute ischemic stroke: a systematic review. Stroke. 2007;38 : 2935–40. doi: 10.1161/STROKEAHA.106.478685 17901394
32. Mega JL, Stitziel NO, Smith JG, Chasman DI, Caulfield MJ, Devlin JJ, et al. Genetic risk, coronary heart disease events, and the clinical benefit of statin therapy: an analysis of primary and secondary prevention trials. Lancet. 2015;385 : 2264–71. doi: 10.1016/S0140-6736(14)61730-X 25748612
33. Barrett PM, Komatireddy R, Haaser S, Topol S, Sheard J, Encinas J, et al. Comparison of 24-hour Holter monitoring with 14-day novel adhesive patch electrocardiographic monitoring. Am J Med. 2014;127 : 95.e11–7.
34. Sanna T, Diener H-C, Passman RS, Di Lazzaro V, Bernstein R a, Morillo CA, et al. Cryptogenic stroke and underlying atrial fibrillation. N Engl J Med. 2014;370 : 2478–86. doi: 10.1056/NEJMoa1313600 24963567
35. Gladstone DJ, Spring M, Dorian P, Panzov V, Thorpe KE, Hall J, et al. Atrial fibrillation in patients with cryptogenic stroke. N Engl J Med. 2014;370 : 2467–77. doi: 10.1056/NEJMoa1311376 24963566
36. Kishore A, Vail A, Majid A, Dawson J, Lees KR, Tyrrell PJ, et al. Detection of atrial fibrillation after ischemic stroke or transient ischemic attack: a systematic review and meta-analysis. Stroke. 2014;45 : 520–6. doi: 10.1161/STROKEAHA.113.003433 24385275
37. Arboix A, Alió J. Cardioembolic stroke: clinical features, specific cardiac disorders and prognosis. Curr Cardiol Rev. 2010;6 : 150–61. doi: 10.2174/157340310791658730 21804774
38. Popejoy AB, Fullerton SM. Genomics is failing on diversity. Nature. 2016;538 : 161–4. doi: 10.1038/538161a 27734877
39. Marcus GM, Alonso A, Peralta CA, Lettre G, Vittinghoff E, Lubitz SA, et al. European ancestry as a risk factor for atrial fibrillation in African Americans. Circulation. 2010;122 : 2009–15. doi: 10.1161/CIRCULATIONAHA.110.958306 21098467
40. Manrai AK, Funke BH, Rehm HL, Olesen MS, Maron BA, Szolovits P, et al. Genetic misdiagnoses and the potential for health disparities. N Engl J Med. 2016;375 : 655–65. doi: 10.1056/NEJMsa1507092 27532831
41. Rosenberg NA, Huang L, Jewett EM, Szpiech ZA, Jankovic I, Boehnke M. Genome-wide association studies in diverse populations. Nat Rev Genet. 2010;11 : 356–66. doi: 10.1038/nrg2760 20395969
42. Roberts JD, Hu D, Heckbert SR, Alonso A, Dewland TA, Vittinghoff E, et al. Genetic investigation into the differential risk of atrial fibrillation among black and white individuals. JAMA Cardiol. 2016;1 : 442–50. doi: 10.1001/jamacardio.2016.1185 27438321
43. Sinner MF, Tucker NR, Lunetta KL, Ozaki K, Smith JG, Trompet S, et al. Integrating genetic, transcriptional, and functional analyses to identify 5 novel genes for atrial fibrillation. Circulation. 2014;130 : 1225–35. doi: 10.1161/CIRCULATIONAHA.114.009892 25124494
44. Manolio TA. Bringing genome-wide association findings into clinical use. Nat Rev Genet. 2013;14 : 549–58. doi: 10.1038/nrg3523 23835440
Štítky
Interní lékařství
Článek vyšel v časopisePLOS Medicine
Nejčtenější tento týden
2018 Číslo 3- Berberin: přírodní hypolipidemikum se slibnými výsledky
- Léčba bolesti u seniorů
- Příznivý vliv Armolipidu Plus na hladinu cholesterolu a zánětlivé parametry u pacientů s chronickým subklinickým zánětem
- Jak postupovat při výběru betablokátoru − doporučení z kardiologické praxe
- Červená fermentovaná rýže účinně snižuje hladinu LDL cholesterolu jako vhodná alternativa ke statinové terapii
-
Všechny články tohoto čísla
- What is the value of multidisciplinary care for chronic kidney disease?
- 2017 Reviewer and Editorial Board Thank You
- Delays in completion and results reporting of clinical trials under the Paediatric Regulation in the European Union: A cohort study
- Surveillance of antimicrobial consumption in animal production sectors of low- and middle-income countries: Optimizing use and addressing antimicrobial resistance
- Causes of death and infant mortality rates among full-term births in the United States between 2010 and 2012: An observational study
- Time for high-burden countries to lead the tuberculosis research agenda
- The importance and challenges of shared decision making in older people with multimorbidity
- Trajectories of functional decline in older adults with neuropsychiatric and cardiovascular multimorbidity: A Swedish cohort study
- Mortality, ethnicity, and country of birth on a national scale, 2001–2013: A retrospective cohort (Scottish Health and Ethnicity Linkage Study)
- Validation of a genetic risk score for atrial fibrillation: A prospective multicenter cohort study
- Multimorbidity and survival for patients with acute myocardial infarction in England and Wales: Latent class analysis of a nationwide population-based cohort
- Integration of postpartum healthcare services for HIV-infected women and their infants in South Africa: A randomised controlled trial
- Cost-effectiveness of multidisciplinary care in mild to moderate chronic kidney disease in the United States: A modeling study
- Role of heme in lung bacterial infection after trauma hemorrhage and stored red blood cell transfusion: A preclinical experimental study
- Patterns and temporal trends of comorbidity among adult patients with incident cardiovascular disease in the UK between 2000 and 2014: A population-based cohort study
- Global child and adolescent mental health: The orphan of development assistance for health
- Cardiovascular disease and multimorbidity: A call for interdisciplinary research and personalized cardiovascular care
- Forced anal examinations to ascertain sexual orientation and sexual behavior: An abusive and medically unsound practice
- Primary prevention of cardiovascular disease: The past, present, and future of blood pressure- and cholesterol-lowering treatments
- Physical activity levels in adults and older adults 3–4 years after pedometer-based walking interventions: Long-term follow-up of participants from two randomised controlled trials in UK primary care
- Effect and cost-effectiveness of educating mothers about childhood DPT vaccination on immunisation uptake, knowledge, and perceptions in Uttar Pradesh, India: A randomised controlled trial
- Comorbidity health pathways in heart failure patients: A sequences-of-regressions analysis using cross-sectional data from 10,575 patients in the Swedish Heart Failure Registry
- Multimorbidity in patients with heart failure from 11 Asian regions: A prospective cohort study using the ASIAN-HF registry
- Antiviral efficacy of favipiravir against Ebola virus: A translational study in cynomolgus macaques
- Transmission of HIV-1 drug resistance mutations within partner-pairs: A cross-sectional study of a primary HIV infection cohort
- A clinical decision support tool for improving adherence to guidelines on anticoagulant therapy in patients with atrial fibrillation at risk of stroke: A cluster-randomized trial in a Swedish primary care setting (the CDS-AF study)
- Integrating HIV and hypertension management in low-resource settings: Lessons from Malawi
- The epidemiology of adolescents living with perinatally acquired HIV: A cross-region global cohort analysis
- Polycystic ovary syndrome, androgen excess, and the risk of nonalcoholic fatty liver disease in women: A longitudinal study based on a United Kingdom primary care database
- Blood pressure-lowering treatment strategies based on cardiovascular risk versus blood pressure: A meta-analysis of individual participant data
- Cerebral white matter disease and functional decline in older adults from the Northern Manhattan Study: A longitudinal cohort study
- HIV treatment eligibility expansion and timely antiretroviral treatment initiation following enrollment in HIV care: A metaregression analysis of programmatic data from 22 countries
- The current and potential health benefits of the National Health Service Health Check cardiovascular disease prevention programme in England: A microsimulation study
- Cardiovascular disease: The rise of the genetic risk score
- Comparative analysis of the association between 35 frailty scores and cardiovascular events, cancer, and total mortality in an elderly general population in England: An observational study
- Progression of diabetes, heart disease, and stroke multimorbidity in middle-aged women: A 20-year cohort study
- PLOS Medicine
- Archiv čísel
- Aktuální číslo
- Informace o časopisu
Nejčtenější v tomto čísle- Forced anal examinations to ascertain sexual orientation and sexual behavior: An abusive and medically unsound practice
- Polycystic ovary syndrome, androgen excess, and the risk of nonalcoholic fatty liver disease in women: A longitudinal study based on a United Kingdom primary care database
- The current and potential health benefits of the National Health Service Health Check cardiovascular disease prevention programme in England: A microsimulation study
- Cardiovascular disease and multimorbidity: A call for interdisciplinary research and personalized cardiovascular care
Kurzy
Zvyšte si kvalifikaci online z pohodlí domova
Současné možnosti léčby obezity
nový kurzAutoři: MUDr. Martin Hrubý
Všechny kurzyPřihlášení#ADS_BOTTOM_SCRIPTS#Zapomenuté hesloZadejte e-mailovou adresu, se kterou jste vytvářel(a) účet, budou Vám na ni zaslány informace k nastavení nového hesla.
- Vzdělávání



