-
Články
Top novinky
Reklama- Vzdělávání
- Časopisy
Top články
Nové číslo
- Témata
Top novinky
Reklama- Videa
- Podcasty
Nové podcasty
Reklama- Kariéra
Doporučené pozice
Reklama- Praxe
Top novinky
ReklamaIntegrating HIV and hypertension management in low-resource settings: Lessons from Malawi
Pragna Patel and colleagues describe the implementation of a hypertension management model for HIV-infected people in Malawi.
Published in the journal: . PLoS Med 15(3): e32767. doi:10.1371/journal.pmed.1002523
Category: Health in Action
doi: https://doi.org/10.1371/journal.pmed.1002523Summary
Pragna Patel and colleagues describe the implementation of a hypertension management model for HIV-infected people in Malawi.
Summary points
Hypertension is the leading risk factor for cardiovascular disease, the most common cause of death worldwide.
In 2011, the United Nations declared that lessons learned from national human immunodeficiency virus (HIV)/acquired immunodeficiency syndrome (AIDS), tuberculosis, and malaria programs in low - and middle-income countries should be harnessed for effective integration of communicable and noncommunicable disease initiatives.
HIV clinical service delivery facilities offer a platform on which to enhance care by offering noncommunicable disease interventions.
Given Malawi’s high prevalence of hypertension, with an estimated one-third of adults in the country affected, we sought to incorporate hypertension management in HIV care delivery sites using standardized treatment protocols and patient registries to monitor treatment outcomes.
The overall aim was to create a reproducible and scalable hypertension management model for HIV-infected persons that is cost effective and that can be used to inform national scale-up of hypertension and other chronic disease care models.
We describe pertinent issues that were raised during the design and implementation of the program, particularly important for the enhanced care of HIV-infected persons.
Introduction
Hypertension is the leading risk factor for cardiovascular disease (CVD), the most common cause of death worldwide [1]. Although sub-Saharan Africa (SSA) is among the last regions in the world to undergo the epidemiologic transition of mortality from infectious disease to noncommunicable disease (NCD), there is a high dual burden of communicable and noncommunicable diseases in this region [2,3]. Currently, acquired immunodeficiency syndrome (AIDS) is the leading cause of death in SSA [2]. However, with the successful expansion of access to antiretroviral therapy (ART) in SSA, dramatic reductions in AIDS-related morbidity and mortality are expected, as seen in high-income countries [4]. As persons living with human immunodeficiency virus (PLHIVs) in SSA gain access to ART and achieve virologic suppression, they will live longer and experience a similar life expectancy to HIV-uninfected persons [4]. Thus, comorbidities, such as CVD, will become increasingly prevalent [5].
PLHIVs are at an increased risk for CVD because of an increased prevalence of traditional risk factors and nontraditional risk factors (e.g., inflammation) as well as effects of specific antiretroviral drugs [6]. Given that PLHIVs are at higher risk for CVD [7], the treatment and control of a high-burden, treatable risk factor such as hypertension are important as an entry point to a more comprehensive approach to CVD management. Hypertension is common in SSA, with prevalence estimates in the general adult population ranging from about 15% to 40% [3]. However, the majority of persons with hypertension (60%–90%) are unaware of their condition, and very few (<5%) have achieved blood pressure control [8]. Therefore, there is a demonstrated need for hypertension screening and control programs in the region.
The setting: Malawi
Malawi has a government-funded national healthcare service that is free to all Malawians. Delivery of healthcare occurs at 3 levels: health centers at the local level, regional/rural hospitals one level up, and district hospitals at the highest level. Because of low resources, investigations are limited, and diagnosis is largely based on clinical presentation. Most laboratory, imaging, and testing facilities are often only available at the major district hospitals. Malawi has very few doctors; therefore, clinical officers (who are trained for a minimum of 4 years and are very experienced practitioners) and medical assistants (who are trained for a minimum of 3 years) are the main healthcare cadre [9].
Malawi has one of the highest HIV prevalence rates (10.6%) among persons aged 15–64 years in the world, and 33% of Malawians aged 25–64 years have high blood pressure (BP) [3]. The President’s Emergency Plan for AIDS Relief (PEPFAR) was responsible for the rapid growth of ART clinics in Malawi with decentralization of services, which have provided life-saving ART to over 600,000 PLHIVs at 650 sites nationwide. Although quality HIV programs exist, there remains a large unmet need in Malawi to improve the quality of healthcare services, promote early detection, and optimize clinical management of hypertension to reduce illness and avoid premature deaths. Additionally, while costs are low for routine BP screening during clinical visits, the HIV clinics in Malawi were not routinely offering these services. The extensive PEPFAR-supported clinic network in Malawi illustrated the potential programmatic reach for the management of other chronic diseases using HIV as a platform for service delivery. For these reasons, the Centers for Disease Control and Prevention (CDC) partnered with Malawi’s Ministry of Health (MOH) and the Lighthouse Trust, the largest provider of ART in Malawi, to integrate hypertension screening and treatment into existing PEPFAR-funded HIV care clinics. The Lighthouse Trust provides services to 25,000 PLHIVs of all ages and plays a pivotal role in piloting service delivery models, introducing curricula on behalf of the national HIV program to build capacity. It has its own procurement mechanism, which facilitated and ensured the availability of antihypertensive medications.
Ethical oversight
The investigation followed the guidelines of the United States Department of Health and Human Services regarding protection of human participants. The study protocol was reviewed according to the CDC, the Malawi MOH, and the Lighthouse Trust human participants review process and was determined to be nonresearch.
Health systems strengthening approach
The integrated HIV and hypertension screening and management program was implemented using a health systems strengthening approach and leveraging the public health approach, which was successfully employed for the global HIV response [10]. According to WHO, health systems consist of 6 building blocks that reflect the basic functions they should carry out regardless of how they are organized: service delivery; health workforce; information; medical products, vaccines, and technologies; financing; and leadership and governance (stewardship) [11]. This framework was developed to address health inequalities worldwide.
The key elements of a successful hypertension management program reach beyond clinical care delivery and require agreement and engagement from public health leaders, governments, and healthcare providers, as well as broad policies to support integration with HIV care. The main areas of our focus were policy, systems strengthening, innovation, education, and monitoring/evaluation (Table 1). Ensuring the consistent availability of low-cost, high-quality medications by improving existing supply chains or developing new procurement methods is paramount [12]. As consistent access to medications was available at our sites, we focused attention to optimal hypertension care delivery (Table 1) for low-resource settings [13].
Tab. 1. Recommended elements for successful hypertension and human immunodeficiency virus (HIV) management integration. 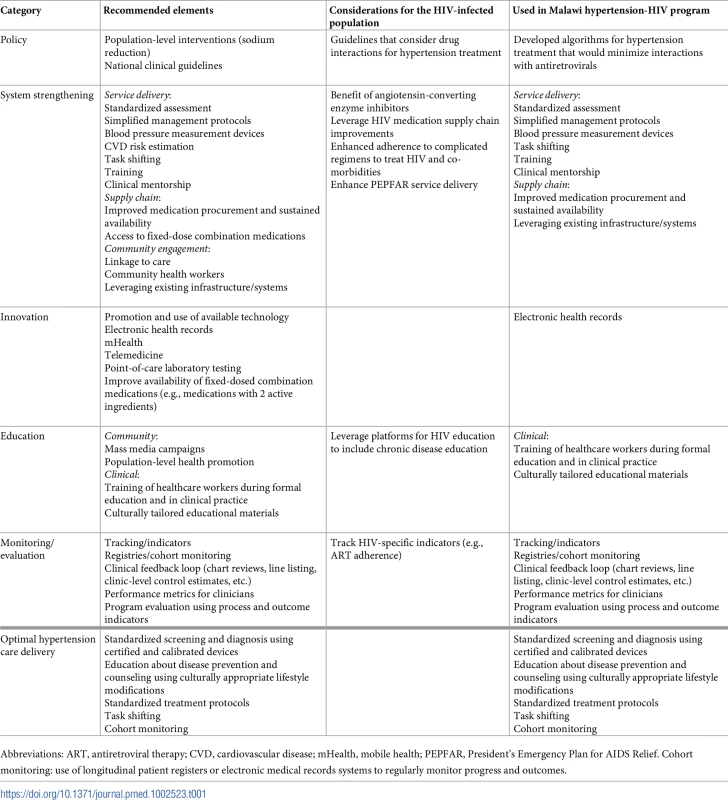
Abbreviations: ART, antiretroviral therapy; CVD, cardiovascular disease; mHealth, mobile health; PEPFAR, President’s Emergency Plan for AIDS Relief. Cohort monitoring: use of longitudinal patient registers or electronic medical records systems to regularly monitor progress and outcomes. The Lighthouse HIV-hypertension integrated model
We initiated a pilot program at 2 high-volume HIV clinics operated by the Lighthouse Trust in Lilongwe, Malawi, as a demonstration project to inform modifications to our integrated hypertension and HIV model and to identify challenges that warrant consideration. The aims of the project were to (1) integrate hypertension screening and treatment in HIV care clinics, (2) optimize hypertension treatment outcomes using standardized hypertension treatment protocols and cohort monitoring, and (3) create a reproducible and scalable hypertension management model that is cost-effective and can be used to inform national scale-up and other chronic disease care models.
We encountered significant design and policy issues, which included the development of standardized hypertension treatment protocols specific to the HIV population and consistent with the Malawi Standard Treatment Guidelines, establishment of an adequate referral network for complicated and resistant cases, and consensus on the need for routine laboratory screening and cardiovascular disease risk assessment in the context of limited resources. Below, we discuss each of these issues in more detail and explain the rationale for our decision-making process.
Developing treatment guidelines
In developing standardized treatment protocols, drug-drug interactions between antihypertensive medications and ART warrant careful consideration. We aimed to minimize the number of patients likely to encounter significant interaction with non-nucleoside reverse transcriptase inhibitor (NNRTI)-based or protease inhibitor (PI)-based regimens, as in SSA virtually all regimens in use include one or the other. In Malawi, the standard treatment guidelines recommend thiazide diuretics as first-line treatment for hypertension and calcium channel blockers as second-line, with no special provisions for PLHIVs. Calcium channel blockers may interact with NNRTIs and PIs, requiring dose adjustment [14], and angiotensin-converting enzyme inhibitors (ACEIs) have been associated with anti-inflammatory effects [15]. Given the potential drug interaction with calcium channel blockers and potential benefit of ACEIs, we used ACEIs as second-line agents for the treatment of hypertension. To prevent electrolyte imbalances, we suggested low-dose therapy of each class of medication with addition of another class rather than titration to maximum dose of current medication for patients with uncontrolled BP. To support the expansion of this model to austere clinical sites, we have developed a recommended algorithm for hypertension treatment for patients who are stable on ART (Fig 1). Furthermore, we received permission for the modification of the hypertension national guidelines from the Malawi Ministry of Health to accommodate necessary changes for the treatment of hypertension among PLHIVs.
Fig. 1. Suggested algorithm for treatment of hypertension among human immunodeficiency virus (HIV)-infected persons. 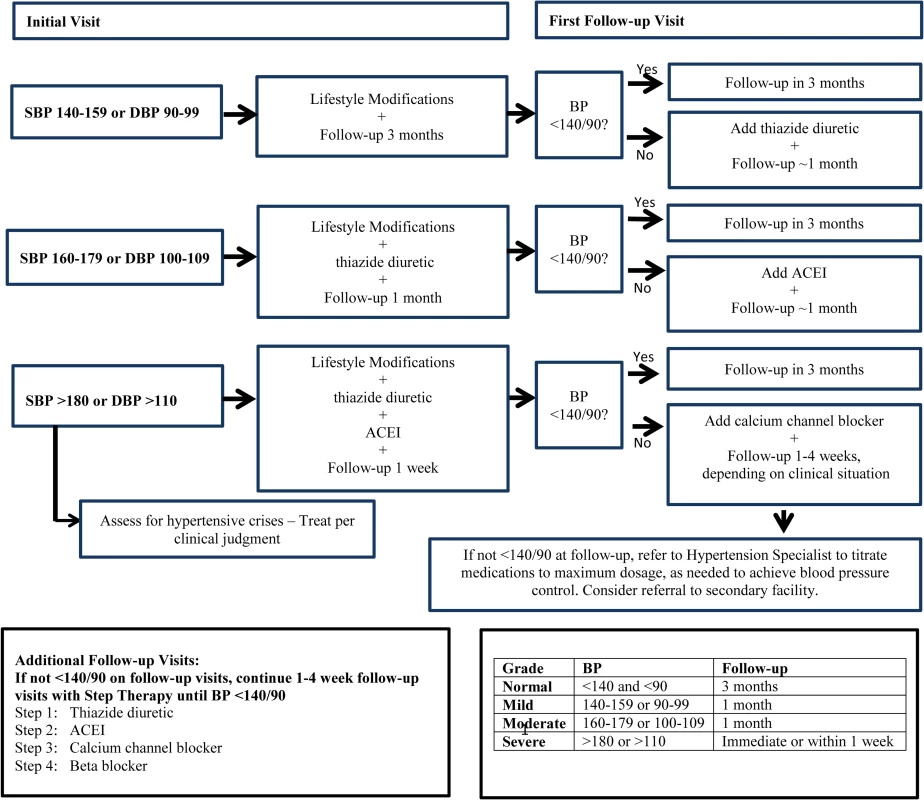
ACEI, angiotensin-converting enzyme inhibitor; BP, blood pressure; DBP, diastolic blood pressure; SBP, systolic blood pressure. Referral network for those with complicated hypertension
Although the majority of hypertension patients will have essential hypertension, the possibility of secondary and resistant hypertension should be assessed in patients with poor response to antihypertensive therapy despite good adherence, in previously stable patients with worsening hypertension, and in patients with stage 3 hypertension (BP > 180/110) and significant target organ disease [16]. The creation of a referral network, which is a type of integrated health service, can facilitate directing persons to appropriate centers as indicated and is thus recommended, as PLHIVs may have additional factors that warrant consideration by a specialist. The use of technology, such as telemedicine, to access clinical specialists for those requiring advanced assessment may also be considered for those communities or clinic populations with inadequate access to care or in geographically isolated areas. We decided to refer patients to an academic physician, who is a local expert in chronic diseases and thus a hypertension specialist, after evaluation by the clinic medical director, who is a certified physician.
Laboratory monitoring
Renal insufficiency, hypokalemia, and other complications may occur with the addition of antihypertensive medications to ART and can be detected with laboratory screening. Laboratory monitoring for those on antihypertensive therapy may not routinely be performed in SSA; however, it may be available for certain clinical indications, such as for patients who develop signs and symptoms that suggest an electrolyte abnormality. If the clinical site is able to conduct phlebotomy and separate serum for laboratory investigations and funding is available to pay for laboratory costs, chemistry panels, which include creatinine and potassium measurements, should be conducted. Testing for creatinine and potassium is recommended at baseline and at the 1-month follow-up visit, particularly for patients starting thiazide diuretics and ACEIs. The need for routine laboratory monitoring is unclear and in extremely resource-poor settings may be impractical to implement. Lack of access to laboratory monitoring should not preclude screening and treatment of hypertension, as the number of patients who experience electrolyte abnormalities is small. Syndromic surveillance can be instituted to assess for potential abnormalities [17]. In our project, we opted to forgo laboratory screening given the challenges with implementation, lack of resources, and expected relatively low yield.
Cardiovascular disease risk assessment
HIV-specific factors such as low CD4+ cell counts and exposure to specific antiretrovirals (ARVs) have been found to be independent risk factors for incident CVD and can increase CVD risk as much as 50%–80% among PLHIVs [7]. Most CVD risk assessment tools tend to underestimate CVD risk among PLHIVs [18]. Therefore, use of CVD risk assessment models may fail to identify substantial numbers of PLHIVs with elevated CVD risk who could potentially benefit from additional medical treatment. Nonetheless, in a low-resource setting, CVD risk assessment can be used to prioritize treatment for those who would benefit most among those PLHIVs who have achieved virologic suppression. We did not institute CVD risk assessment, as further studies on CVD risk assessment among PLHIVs are warranted.
Implementation issues
We encountered key implementation issues, which included training of a cadre of healthcare providers to screen for and treat hypertension among PLHIVs; integrating care for an additional disease entity without overwhelming the present infrastructure in terms of patient load per provider, clinic wait times for patients, and quality of care; and developing routine monitoring and evaluation systems. The medical director provided regular monthly classroom trainings to approximately 25 nurses and clinical officers who staffed the 2 clinics. These trainings were updated periodically to address issues that were of concern; for example, early in implementation, we noted that patients diagnosed with hypertension were not filling their prescriptions right away. These types of issues were addressed at weekly meetings with the medical director, and solutions were incorporated into subsequent trainings. To avoid disrupting clinic flow and ensure a manageable workload, we used a phased screening approach by gradually decreasing the age threshold of eligible persons. Process and outcome indicators developed for the project are summarized in Table 2. Registries can be used to generate performance metrics for healthcare providers as well as inform clinical feedback to identify patients who need follow-up care. Therefore, we developed a hypertension-specific module for the Malawi electronic medical record system that provided screening and management prompts for clinical decision support and facilitated data collection, including process indicators, and analysis for ongoing program evaluation and quality of care improvement. We were particularly concerned about the additional burden of HIV medications affecting adherence to ARVs; therefore, we collected data on adherence, which was already being measured as part of the HIV program.
Tab. 2. Example core process and outcome indicators for an integrated hypertension/human immunodeficiency virus (HIV) clinical management program examined at 6-month intervals. 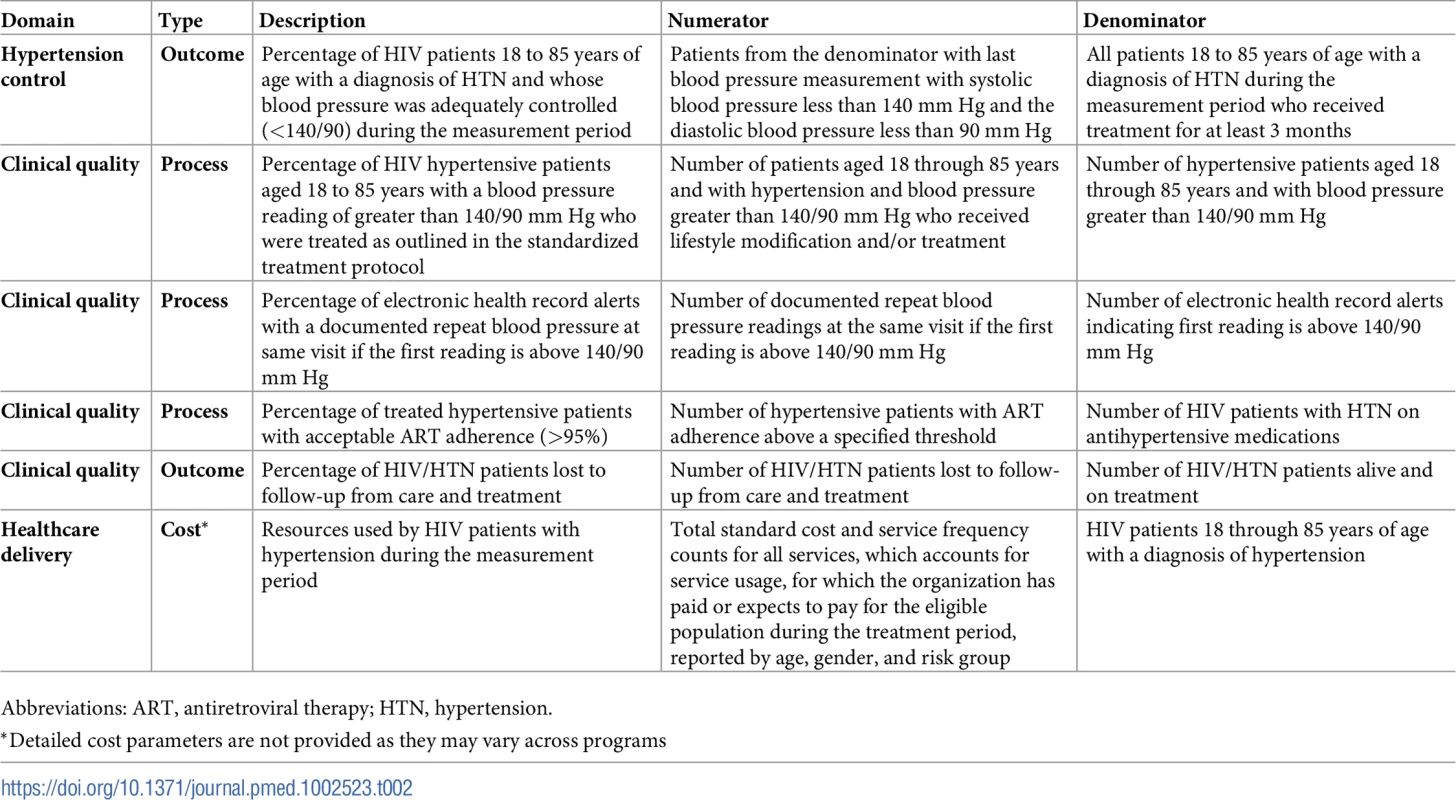
Abbreviations: ART, antiretroviral therapy; HTN, hypertension. Potential to improve HIV outcomes and access hard-to-reach populations
Integrated service delivery and decentralization of care into primary health facilities and communities can improve outcomes among PLHIVs. Expansion in ART coverage, improvement in retention, and reduction in mortality have all been demonstrated in programs that have successfully integrated HIV services into clinics for maternal, newborn, and child care as well as tuberculosis treatment and opiate substitution therapy [19].
The integration of HIV and NCD management may particularly improve access to care for adult males in SSA, a population that has remained elusive despite PEPFAR’s efforts to expand ART [20]. Also, the integration of HIV and NCD services may reduce stigma associated with HIV, especially if these clinics eventually serve the general uninfected population [20]. A key to improving access to ART and HIV outcomes may be to use the platforms that have been developed for HIV care to build health systems that are available to all, thereby addressing the double burden of HIV and NCDs effectively both at an individual as well as a population level. Further research and evaluation of integrated care models are needed to inform efforts to use limited healthcare resources effectively [21].
Discussion
The hypertension management model described here is consistent with the WHO’s framework for health systems strengthening and considers the 6 building blocks that make up the health system [11]. In addition, we promote the use of evidence-based tools and practices to improve BP control.
In our demonstration project, at 12 months, of 29,359 individuals screened, 11% were newly diagnosed with hypertension, and 85% of those with hypertension received treatment per standardized protocols. Among persons with mild and moderate hypertension, BP control rates were 38% and 30% after 6 months of treatment, respectively (Table 3). The additional drug burden for hypertension control did not affect adherence to HIV medications. We did not see any electrolyte abnormalities among persons prescribed antihypertensive medications during the course of the project. This project successfully integrated hypertension screening and management into routine HIV service delivery at 2 Lighthouse Trust HIV clinics; however, expansion within Malawi to government-funded sites is challenging because of the inconsistent supply of medications for these types of facilities. Program evaluation is currently underway.
Tab. 3. Postimplementation program evaluation data for 2 Lighthouse Trust pilot sites in Lilongwe, Malawi, February 2015 to June 2016. 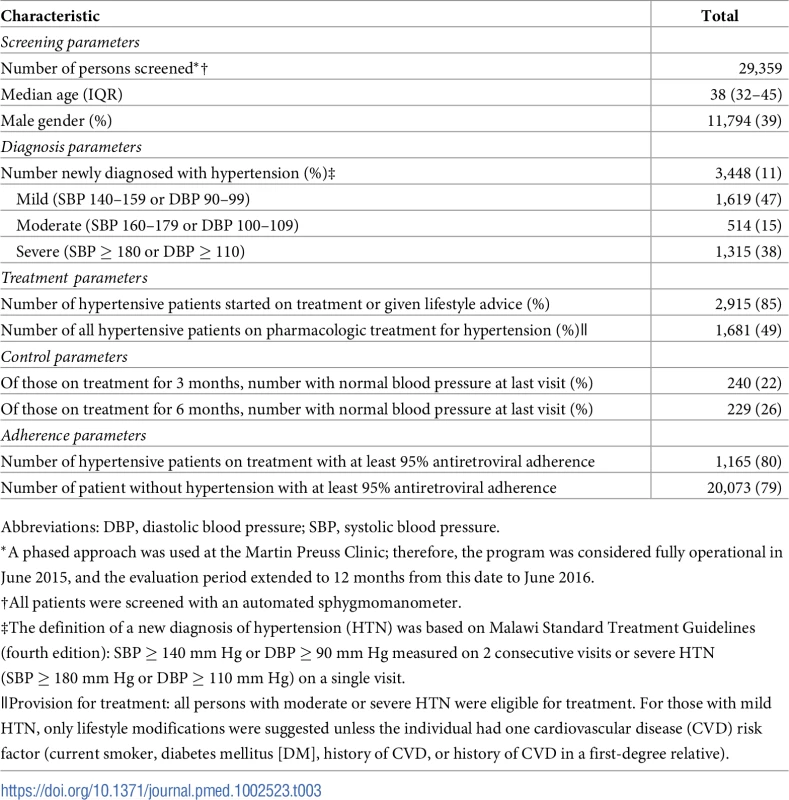
Abbreviations: DBP, diastolic blood pressure; SBP, systolic blood pressure. Site-specific program costs associated with this add-on intervention will provide an estimate of the average treatment cost per patient, and program cost-effectiveness analysis will help assess whether the health return attributable to the intervention may be justified. Such cost-effectiveness information may be useful in advocating for replication of the model among civil society stakeholders and global policy makers, potentially leading to expanded public health impact through the SSA region. Consistent access to medications for hypertension was available at our sites, which may not be the case in many clinics, so this model is generalizable to clinics with similar infrastructure in place. Hypertension and HIV integrated care will need continued investments in supply-chain management because stock-outs of antihypertensive medications commonly occur for the publicly funded clinics in Malawi. In Malawi, these drugs are offered free of charge; however, this creates challenges for public health officials who need to distribute limited resources to a number of programs, especially as support for HIV medications starts to shift from PEPFAR to national ministries. Innovative approaches to paying for medications should be sought. For example, regional procurement mechanisms may reduce overall costs, with bulk procurement rendering medications more available and affordable [12]. In addition, we were not able to implement care for comorbidities such as diabetes given limited resources and staff. Finally, training a cadre of healthcare workers to provide both chronic multidisease and HIV care may pose distinct challenges given limited numbers of available personnel.
We hope that this program will help to inform the larger effort to improve health systems and integrate HIV and NCD services for improved care. As outlined in the NCD global action plan, this project directly relates to the priority action of member states to examine opportunities for HIV-NCD care integration not only to manage NCDs more effectively but also to enhance the care of PLHIVs as they age and live longer due to improve ART coverage throughout the world [22].
Zdroje
1. GBD 2013 Risk Factors Collaborators. Global, regional, and national comparative risk assessment of 79 behavioural, environmental and occupational, and metabolic risks or clusters of risks in 188 countries, 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2015; 386 (10010):2287–2323. doi: 10.1016/S0140-6736(15)00128-2 26364544
2. GBD 2013 Mortality and Causes of Death Collaborators. Global, regional, and national age-sex specific all-cause and cause-specific mortality for 240 causes of death, 1990–2013: a systematic analysis for the Global Burden of Disease Study. Lancet. 2015 Jan 10;385(9963):117–71. doi: 10.1016/S0140-6736(14)61682-2 25530442
3. WHO. STEPS Country Reports 2013. Available from: http://www.who.int/chp/steps/reports/en/.
4. Lessells RJ, Mutevedzi PC, Iwuji CC, Newell ML. Reduction in early mortality on antiretroviral therapy for adults in rural South Africa since change in CD4+ cell count eligibility criteria. J Acquir Immune Defic Syndr. 2014 Jan 1;65(1):e17–24. doi: 10.1097/QAI.0b013e31829ceb14 23756374
5. Mensah GA, Roth GA, Sampson UK, Moran AE, Feigin VL, Forouzanfar MH, et al.; GBD 2013 Mortality and Causes of Death Collaborators. Mortality from cardiovascular diseases in sub-Saharan Africa, 1990–2013: a systematic analysis of data from the Global Burden of Disease Study 2013. Cardiovasc J Afr. 2015; 26(2 Suppl 1):S6–10.
6. Collaboration of Observational HIV Epidemiological Research Europe (COHERE) in EuroCoord, Lewden C, Bouteloup V, De Wit S, Sabin C, Mocroft A, et al. All-cause mortality in treated HIV-infected adults with CD4 ≥500/mm3 compared with the general population: evidence from a large European observational cohort collaboration. Int J Epidemiol. 2012;41 : 433–445. doi: 10.1093/ije/dyr164 22493325
7. Islam FM, Wu J, Jansson J, Wilson DP. Relative risk of cardiovascular disease among people living with HIV: a systematic review and meta-analysis. HIV Med. 2012;13 : 453–468. doi: 10.1111/j.1468-1293.2012.00996.x 22413967
8. Hendriks ME, Wit FWNM, Roos MTL, Brewster LM, Akande TM, de Beer IH, et al. Hypertension in Sub-Saharan Africa: Cross-Sectional Surveys in Four Rural and Urban Communities. PLoS ONE. 2012;7(3): e32638. doi: 10.1371/journal.pone.0032638 22427857
9. Ripple Africa. General information about healthcare in Malawi. Available from: https://www.rippleafrica.org/healthcare-in-malawi-africa/healthcare-in-malawi-africa
10. Gilks CF, Crowley S, Ekpini R, Gove S, Perriens J, Souteyrand T, et al. The WHO public-health approach to antiretroviral treatment against HIV in resource-limited settings. Lancet. 2006; 368 : 505–10. doi: 10.1016/S0140-6736(06)69158-7 16890837
11. WHO. Everybody business: strengthening health systems to improve health outcomes: WHO’s framework for action. 2007. Available from: http://www.who.int/healthsystems/strategy/everybodys_business.pdf
12. Van Mourik MS, Cameron A, Ewen M, Laing RO. Availability, price and affordability of cardiovascular medicines: a comparison across 36 countries using WHO/HAI data. BMC Cardiovasc Disord. 2010; 10 : 25. doi: 10.1186/1471-2261-10-25 20534118
13. Angell SY, DeCock KM, Frieden TR. A public health approach to global management of hypertension. Lancet. 2015;385 : 825–27. doi: 10.1016/S0140-6736(14)62256-X 25752181
14. Peyriere H, Eiden C, Macia JC, Reynes J. Antihypertensive Drugs in Patients Treated with Antiretrovirals. Ann Pharmacother. 2012;46 : 703–9. doi: 10.1345/aph.1Q546 22550277
15. Baker JV, Hullsiek KH, Prosser R, Duprez D, Grimm R, Tracy RP, et al. Angiotensin converting enzyme inhibitor and HMG-CoA reductase inhibitor as adjunct treatment for persons with HIV infection: a feasibility randomized trial. PLoS ONE. 2012;7(10): e46894. doi: 10.1371/journal.pone.0046894 23082133
16. Onusko E. Diagnosing secondary hypertension. Am Fam Physician. 2003; 67(1): 67–74. 12537168
17. Bickett DP. Using ACE Inhibitors appropriately. Am Fam Physician. 2002; 66(3):461–9. 12182524
18. Thompson-Paul AM, Lichtenstein KA, Armon C, Buchacz K, Debes R, Chmiel JS, et al. Cardiovascular disease risk prediction in the HIV Outpatient Study (HOPS). In: Conference on Retroviruses and Opportunistic Infections; 2015 February 23–26; Seattle, Washington (WA). Abstract number 747.
19. Suthar AB, Rutherford GW, Horvath T, Doherty MC, Negussie EK. Improving antiretroviral therpay scale-up and effectiveness through service integration and decentralization. AIDS. 2014; 28(Suppl 2):S175–S185.
20. Sharma M, Ying R, Tarr G, Barnabas R. Systematic review and meta-analysis of community and facility-based HIV testing to address linkage to care gaps in SSA. Nature. 2015; 528: S77–S85. doi: 10.1038/nature16044 26633769
21. Atun R, de Jongh T, Secci F, Ohiri, Adeyi O. A systematic review of the evidence on integration of targeted health interventions into health systems. Health Policy and Planning 2010;25 : 1–14. doi: 10.1093/heapol/czp053 19959485
22. WHO. Global Action Plan for The Prevention and Control of Noncommunicable diseases 2013–2020. 2013. Available from: http://www.who.int/nmh/events/ncd_action_plan/en/.
Štítky
Interní lékařství
Článek vyšel v časopisePLOS Medicine
Nejčtenější tento týden
2018 Číslo 3- Berberin: přírodní hypolipidemikum se slibnými výsledky
- Léčba bolesti u seniorů
- Příznivý vliv Armolipidu Plus na hladinu cholesterolu a zánětlivé parametry u pacientů s chronickým subklinickým zánětem
- Jak postupovat při výběru betablokátoru − doporučení z kardiologické praxe
- Červená fermentovaná rýže účinně snižuje hladinu LDL cholesterolu jako vhodná alternativa ke statinové terapii
-
Všechny články tohoto čísla
- What is the value of multidisciplinary care for chronic kidney disease?
- 2017 Reviewer and Editorial Board Thank You
- Delays in completion and results reporting of clinical trials under the Paediatric Regulation in the European Union: A cohort study
- Surveillance of antimicrobial consumption in animal production sectors of low- and middle-income countries: Optimizing use and addressing antimicrobial resistance
- Causes of death and infant mortality rates among full-term births in the United States between 2010 and 2012: An observational study
- Time for high-burden countries to lead the tuberculosis research agenda
- The importance and challenges of shared decision making in older people with multimorbidity
- Trajectories of functional decline in older adults with neuropsychiatric and cardiovascular multimorbidity: A Swedish cohort study
- Mortality, ethnicity, and country of birth on a national scale, 2001–2013: A retrospective cohort (Scottish Health and Ethnicity Linkage Study)
- Validation of a genetic risk score for atrial fibrillation: A prospective multicenter cohort study
- Multimorbidity and survival for patients with acute myocardial infarction in England and Wales: Latent class analysis of a nationwide population-based cohort
- Integration of postpartum healthcare services for HIV-infected women and their infants in South Africa: A randomised controlled trial
- Cost-effectiveness of multidisciplinary care in mild to moderate chronic kidney disease in the United States: A modeling study
- Role of heme in lung bacterial infection after trauma hemorrhage and stored red blood cell transfusion: A preclinical experimental study
- Patterns and temporal trends of comorbidity among adult patients with incident cardiovascular disease in the UK between 2000 and 2014: A population-based cohort study
- Global child and adolescent mental health: The orphan of development assistance for health
- Cardiovascular disease and multimorbidity: A call for interdisciplinary research and personalized cardiovascular care
- Forced anal examinations to ascertain sexual orientation and sexual behavior: An abusive and medically unsound practice
- Primary prevention of cardiovascular disease: The past, present, and future of blood pressure- and cholesterol-lowering treatments
- Physical activity levels in adults and older adults 3–4 years after pedometer-based walking interventions: Long-term follow-up of participants from two randomised controlled trials in UK primary care
- Effect and cost-effectiveness of educating mothers about childhood DPT vaccination on immunisation uptake, knowledge, and perceptions in Uttar Pradesh, India: A randomised controlled trial
- Comorbidity health pathways in heart failure patients: A sequences-of-regressions analysis using cross-sectional data from 10,575 patients in the Swedish Heart Failure Registry
- Multimorbidity in patients with heart failure from 11 Asian regions: A prospective cohort study using the ASIAN-HF registry
- Antiviral efficacy of favipiravir against Ebola virus: A translational study in cynomolgus macaques
- Transmission of HIV-1 drug resistance mutations within partner-pairs: A cross-sectional study of a primary HIV infection cohort
- A clinical decision support tool for improving adherence to guidelines on anticoagulant therapy in patients with atrial fibrillation at risk of stroke: A cluster-randomized trial in a Swedish primary care setting (the CDS-AF study)
- Integrating HIV and hypertension management in low-resource settings: Lessons from Malawi
- The epidemiology of adolescents living with perinatally acquired HIV: A cross-region global cohort analysis
- Polycystic ovary syndrome, androgen excess, and the risk of nonalcoholic fatty liver disease in women: A longitudinal study based on a United Kingdom primary care database
- Blood pressure-lowering treatment strategies based on cardiovascular risk versus blood pressure: A meta-analysis of individual participant data
- Cerebral white matter disease and functional decline in older adults from the Northern Manhattan Study: A longitudinal cohort study
- HIV treatment eligibility expansion and timely antiretroviral treatment initiation following enrollment in HIV care: A metaregression analysis of programmatic data from 22 countries
- The current and potential health benefits of the National Health Service Health Check cardiovascular disease prevention programme in England: A microsimulation study
- Cardiovascular disease: The rise of the genetic risk score
- Comparative analysis of the association between 35 frailty scores and cardiovascular events, cancer, and total mortality in an elderly general population in England: An observational study
- Progression of diabetes, heart disease, and stroke multimorbidity in middle-aged women: A 20-year cohort study
- PLOS Medicine
- Archiv čísel
- Aktuální číslo
- Informace o časopisu
Nejčtenější v tomto čísle- Forced anal examinations to ascertain sexual orientation and sexual behavior: An abusive and medically unsound practice
- Polycystic ovary syndrome, androgen excess, and the risk of nonalcoholic fatty liver disease in women: A longitudinal study based on a United Kingdom primary care database
- The current and potential health benefits of the National Health Service Health Check cardiovascular disease prevention programme in England: A microsimulation study
- Cardiovascular disease and multimorbidity: A call for interdisciplinary research and personalized cardiovascular care
Kurzy
Zvyšte si kvalifikaci online z pohodlí domova
Současné možnosti léčby obezity
nový kurzAutoři: MUDr. Martin Hrubý
Všechny kurzyPřihlášení#ADS_BOTTOM_SCRIPTS#Zapomenuté hesloZadejte e-mailovou adresu, se kterou jste vytvářel(a) účet, budou Vám na ni zaslány informace k nastavení nového hesla.
- Vzdělávání



