-
Články
Top novinky
Reklama- Vzdělávání
- Časopisy
Top články
Nové číslo
- Témata
Top novinky
Reklama- Videa
- Podcasty
Nové podcasty
Reklama- Kariéra
Doporučené pozice
Reklama- Praxe
Top novinky
ReklamaBenefits and safety of gabapentinoids in chronic low back pain: A systematic review and meta-analysis of randomized controlled trials
In a systematic review and metanalysis, Harsha Shanthanna and colleagues examine the evidence for the benefits and safety of gabapentoids for chronic low back pain.
Published in the journal: . PLoS Med 14(8): e32767. doi:10.1371/journal.pmed.1002369
Category: Research Article
doi: https://doi.org/10.1371/journal.pmed.1002369Summary
In a systematic review and metanalysis, Harsha Shanthanna and colleagues examine the evidence for the benefits and safety of gabapentoids for chronic low back pain.
Introduction
Chronic Low Back Pain (CLBP) is very common and is associated with significant patient burden and heath resource expenditure [1–3]. It is largely nonspecific in nature and in up to 85% of patients lacks a clear pathoanatomical diagnosis when present in isolation [1–4]. We have previously highlighted the etiological and treatment considerations for CLBP, along with the limitations within the existing evidence [5]. A large proportion of CLBP patients are treated with routine analgesic medications with unsatisfactory results leading to frequent exploration of second line options including gabapentinoids [6, 7]. In particular, the use of gabapentin (GB) and pregabalin (PG) is made on the rationale of modulating the enhanced neurotransmission at the level of presynaptic receptors of the afferent neurons. Both of these medications primarily act on the α-2 delta-2 subunit of the voltage-dependent calcium channels [8, 9] and can be considered to have very similar pharmacodynamic actions on pain and other symptoms. They are considered to be very effective for neuropathic pain (NP) conditions. Attempts at exploiting their therapeutic potential for other pain conditions have shown mixed results [10, 11]. Use of gabapentinoids for CLBP requires slow titration to therapeutic doses and establishing maintenance on a long-term basis. With prolonged treatment, the potential gain over possible adverse effects and risks could become unclear [9]. There have been concerns over the excessive off-label use of GB, despite there being a clear lack of clinical studies [12], necessitating advisory guidelines by the National Health Services (NHS), United Kingdom on the risk of the misuse of gabapentinoids [13]. Our primary objectives were to assess the benefits of GB and PG in CLBP in decreasing pain and to examine the risk of adverse effects. Secondarily, we assessed the effects of PG and GB on the Initiative on Methods, Measurement and Pain Assessment in Clinical Trials (IMMPACT) outcomes [14]. The outcomes considered were physical and emotional functioning, participant ratings of global improvement and satisfaction with treatment, and participant disposition. Additionally, we attempted to assess whether the use of gabapentinoids selectively improve pain relief in patients with predominant neuropathic CLBP.
Methods
As this is a systematic review, ethics committee approval is not applicable.
Protocol and registration
Our review was registered with PROSPERO with the registration number CRD42016034040. This report has been prepared according to PRISMA guidelines [15], as suggested by the Enhancing the QUAlity and Transparency Of health Research (EQUATOR) network (S1 PRISMA checklist). Our detailed review protocol has been previously published [5].
Eligibility criteria
We included randomized controlled trials (RCTs) involving adult patients (>18 years of age) with predominant CLBP of 3 months or more, with or without leg pain. We did not have any language exclusions. Studies with mixed population of chronic pain were only included if they report outcomes separately for our study population of interest, or if at least 90% of the trial patients are >18 years with predominant CLBP. Studies were further screened for interventions and were included if they randomized patients to receive “PG” or “GB,” either “alone” or “in combination with other treatment,” and compared it with any active or inactive treatments.
Information sources
We searched the electronic databases of EMBASE, MEDLINE, and the Cochrane Central Registry of Controlled Trials (CENTRAL), from their inception until January 26th, 2016. WHO clinical trial registry (http://apps.who.int/trialsearch/Default.aspx), and clinical trial registry (https://clinicaltrials.gov/), were also searched to look for any registered studies, fulfilling our eligibility criteria, and crosschecked for their resulting publications. To be comprehensive, bibliographies of relevant reviews and selected studies were examined. Since performing the original search, we also repeated our search on December 20th, 2016 to ensure that we have not missed any recent publications.
Search strategy
The search was performed using a sensitive strategy by an experienced librarian for each specific database. We included terms referring to study population of low back pain, and terms referring to study interventions such as GB, PG, and anticonvulsants [5]. The strategy is provided as a supplementary file (S1 Text).
Study screening and selection
Using paired reviewers screening independently and in duplicate, study selection was performed in 2 stages. Titles and abstracts were screened in the first stage, followed by full text screening on citations felt potentially eligible. A calibration exercise between reviewer pairs ensured consistency in screening and disagreement were resolved by consensus or through discussion with the principal investigator (HS). A quadratic kappa statistic on the full article final decision was estimated as a measure of interobserver agreement [16].
Data collection process
The same paired reviewers extracted the data independently and in duplicate, using electronic data extraction forms that were piloted between the reviewers for consistency and accuracy. An instruction manual was provided to assist with the data extraction process.
Data items
Data items extracted from each study included study characteristics, risk of bias (RoB) items, demographic information, participant disposition through the study, and our review outcomes on continuous and binary measures captured on 6 core domains as recommended by the IMMPACT statement guidelines [14].
RoB in individual studies
RoB was assessed using the Cochrane RoB tool modified to capture the components of random sequence generation; allocation concealment; blinding of participants; blinding of outcome assessment; and analysis of incomplete outcome data. Further, we modified the response options of domains as “definitely yes,” “probably yes,” “probably no,” and “definitely no.” For each domain, the responses of “definitely yes” and “probably yes” categories were assigned a high RoB and those in the “probably no” and “definitely no” categories a low RoB[17]. Crossover studies were assessed for reasonable washout period [18]. No attempt was made to contact authors for clarification on the RoB items. Selective outcome reporting was judged based on the outcomes described in the methods section but not reported in the results section [19].
Additional RoB items
Additionally, we considered the domains for chronic pain studies as suggested by Moore et al. [20] and added the domains of outcome assessment time (12 weeks or more as low risk), outcome assessment threshold (>30% improvement in pain relief as low risk), and potential for publication bias based on the sample size threshold (>50 as low risk) to identify a trial as having the potential for publication bias based on low sample size. Trials with low sample size can increase the chances of erroneously large treatment effect sizes and indirectly contribute to publication bias [21, 22].
Outcomes and prioritization
A priori, we specified pain relief and safety (adverse effects) as our primary outcomes and others as secondary outcomes, and prioritized the use of intent to treat analysis. Pain relief expressed as both continuous and categorical outcomes, and at various time points, was extracted for all reported time points. For pooling, we considered the most common type and the longest duration of follow-up reported. A priori, we prioritized change scores over end scores for pooling analysis. Change scores are considered more efficient and powerful than comparison of final scores, as it removes a component of between-person variability from the analysis [18]. For pain relief expressed as continuous scores, we converted all study outcomes into a common 0–10 numerical rating scale, as it is commonly used and easy to interpret [14]. The approach to conversion into a common scale is shown in S2 Text. Safety was assessed by comparing the risk of serious adverse events causing death, hospitalisation, or study withdrawal. If unclear, we considered reporting the most commonly reported adverse effects. Due to the expected differences within measurement scales, secondary outcomes of improvement in physical and emotional functioning, and participant ratings of global improvement and satisfaction were not converted into a single common scale.
Synthesis of results and summary measures
Data were pooled only if there are 3 or more studies contributing to an outcome domain. Our selection criteria allowed for a relatively homogeneous population of CLBP who tend to be approached similarly from a clinical situation. However, we recognized the potential for heterogeneity based on study interventions and comparator interventions. In view of these obvious sources of heterogeneity, we decided a priori to pool studies using PG or GB, either alone or in combination, separately. Extracted data were compiled and checked for accuracy using Microsoft Excel. RoB was assessed using a modified Cochrane RoB tool that is described below. For the primary analysis, we used a complete case analysis, as reported in individual studies. Sensitivity analyses for incomplete outcome data were performed. Analysis and synthesis was carried out using Review Manager (RevMan) [Computer program], Version 5.3. Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2014; and Microsoft Excel 2011 (Mac version). Based on the comparator and interventions, if we did not expect much between study variance, a fixed effects model was used for pooling. However, if we suspected between study variance, or in the presence of unexplained heterogeneity, a random effects model was chosen [18]. For crossover studies, we prioritized the results from a paired test. If not provided, results of unpaired tests were considered. If there was a potential for carryover effect, or if there is a significant drop out rate (>20%), the results from the first period only were considered [18]. Statistical heterogeneity was estimated using Cochrane’s Q test, with a threshold of p-value at 0.10, and the percentage variability in individual effect estimates was described by I2 statistic [18]. Risk Ratio (RR), and mean difference (MD) or standardized mean differences (SMDs) as appropriate, were estimated along with their 95% confidence intervals (CI). We planned to report the findings in measures of absolute risk, if they were observed to be statistically significant. Rating of quality of evidence was done using GRADE approach, with a summary of findings (SOF) table.
Additional analysis
A subgroup analysis was considered in studies that screened for the presence of NP using a screening questionnaire at baseline and reported pain relief in patients of NP separately. Sensitivity analyses for the outcome of pain relief was carried out for studies reporting >5% loss to follow-up (LTFU). These were carried out using well-described imputation strategies [23, 24].
Results
Study selection
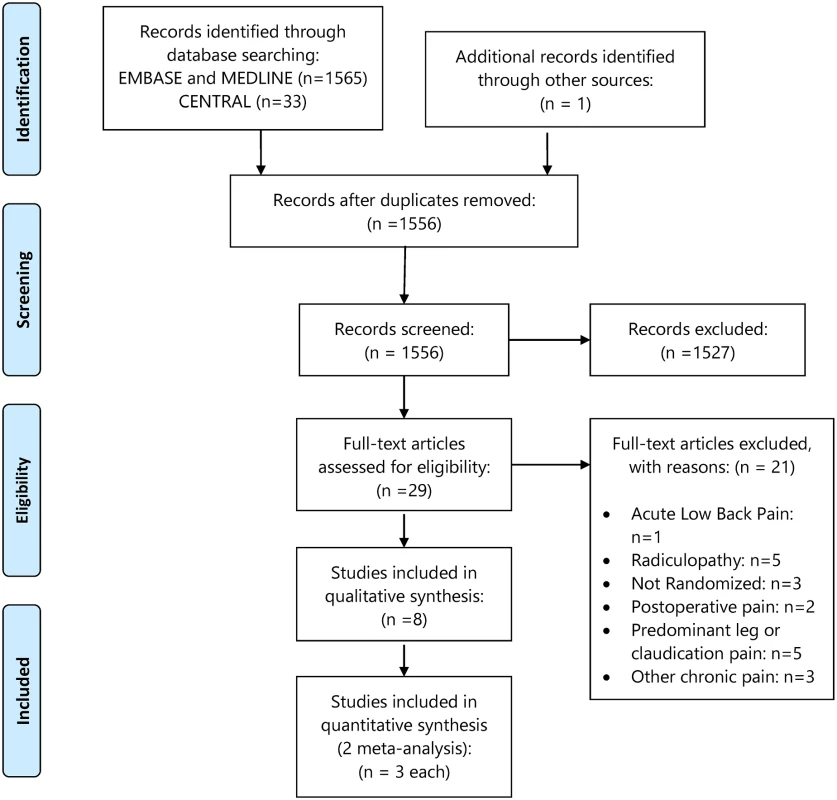
Our search identified a total of 1,385 citations after exclusion of duplicates. Among the 29 articles assessed for full text, 21 studies were excluded with reasons that are shown in Fig 1. Eight studies were included for qualitative and six for quantitative analysis (Fig 1). There was almost perfect agreement, indicated by kappa = 0.82, between reviewers at the full-text screening stage.
Study characteristics
Important characteristics of the study population and treatments are provided in Table 1. Of the 8 studies, 3 compared the use of GB to placebo treatment [25, 27], and 5 used PG [28–32]. There were 2 crossover studies using GB [26] and PG [31]. Only 2 studies were multicentered and had external funding for the conduct of their trial [25, 28]. Among the PG trials, 3 trials used an active comparator (amitryptline, celebrex, tramacet) versus PG alone [29, 31, 32]. As the study by Romano et al. had 3 arms [31], they compared PG alone versus celebrex (CX) versus a combination of PG plus CX. So, there were 3 comparisons involving PG as an adjunct to an analgesic medication versus their respective analgesic medication [28, 30, 31]. The mean age ranged between 41.6 to 58.5 years, except in the study by Sakai et al. [32]. However, the duration of pre-existing CLBP had a much wider range of 13 to 213 months. The treatment doses were titrated for clinical effect in all studies, except for Sakai et al., who had a fixed dosing of PG [32]. The doses ranged from 300 to 3,600 mg/day with GB and 100 to 600 mg/day with PG, in divided doses. Only 3 studies assessed specifically for NP using a screening questionnaire [28, 31, 32].
Tab. 1. Characteristics of included studies: design, population, and interventions. 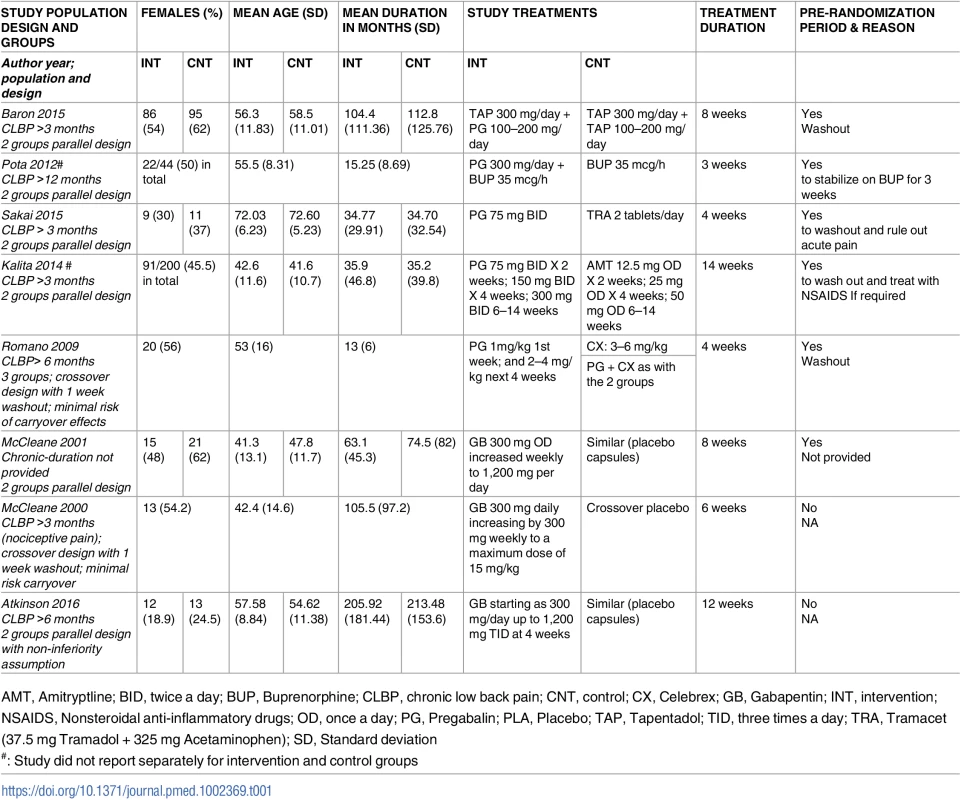
AMT, Amitryptline; BID, twice a day; BUP, Buprenorphine; CLBP, chronic low back pain; CNT, control; CX, Celebrex; GB, Gabapentin; INT, intervention; NSAIDS, Nonsteroidal anti-inflammatory drugs; OD, once a day; PG, Pregabalin; PLA, Placebo; TAP, Tapentadol; TID, three times a day; TRA, Tramacet (37.5 mg Tramadol + 325 mg Acetaminophen); SD, Standard deviation RoB within studies (Fig 2)
Fig. 2. RoB within the included studies. 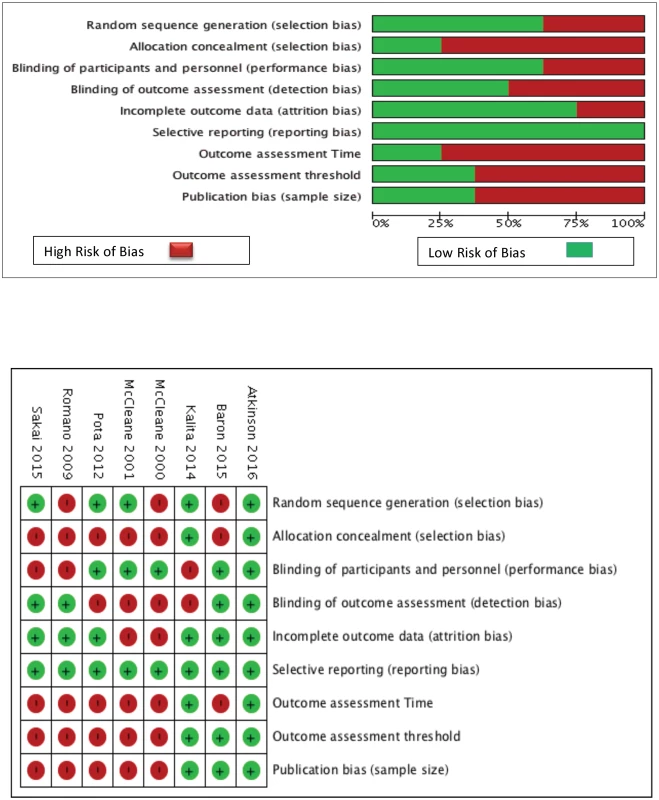
RoB, risk of bias. Six of the eight studies had a risk of selection bias, six for allocation concealment and three for sequence generation, and four involved a risk of detection bias. The studies by Baron et al. [28], and Atkinson et al. [25] were rated as having low RoB for most domains, and both crossover studies had a higher risk of selection bias [26, 31].
Study outcomes and synthesis of results
Except 2 studies that reported using 0–100 scale [30, 31], all others reported their pain scores on a scale of 0–10 NRS or Visual Analogue Scale (VAS). Five studies provided a dichotomous measure of treatment success by varying thresholds [25–29, 32]. All studies reported on one or more adverse effects. Functional improvement was reported in 5 studies [25, 26, 28, 29, 32], quality of life (QOL) improvement by 2 studies [28, 32], psychological improvement or improvement in depression by 3 studies [25, 28, 32], and global impression of change (GIC) only by 2 studies [25, 28].
Pain relief
Pain relief expressed in NRS or VAS scales were converted into a common scale of 0–10 NRS. Authors of 2 studies were successfully contacted to obtain final results of pain scores, as it was not clear in their reporting [25, 32]. We were unable to use the change scores as many studies did not report their change in standard deviations (SDs), and imputing them based on another study or by using a correlation coefficient of change was observed to be inappropriate and not precise [18]. So, pooling was performed using end scores. Based on the variability in the study comparisons, we decided to pool studies for the use of GB and PG. In the first group (Fig 3a), studies using GB (n = 91) versus placebo (n = 94) were combined using a fixed effects model. Compared with placebo, the GB group had a small reduction in pain (MD = 0.22 units, 95% CI [−0.51 to 0.07], I2 = 0%). There were no studies comparing PG with placebo. PG (n = 163) was compared with an active comparator (n = 169) in 3 studies (Fig 3b), using random effects model. This analysis showed an improvement in pain favoring the use of the active comparator group (MD = 0.42 units, 95% CI [0.20 to 0.64], I2 = 0). Both the above comparisons were rated as very low quality evidence by GRADE (Table 2). The third group consisted of comparisons that used PG as an adjunct to another analgesic medication (n = 215), such as buprenorphine (BUP) [30], tapentadol (TAP) [28], and CX [30], and compared it with the use of analgesic medication alone (n = 208). We decided that it was not appropriate to pool these studies considering the clinical heterogeneity involved within the studies, on the sides of both intervention and comparator. This was supported by the substantial statistical heterogeneity observed with such an attempt using random effects model, I2 = 77%. The forest plot for this comparison is shown as S1 Fig. Among these 3 studies, the largest study by Baron et al. did not find any difference by adding PG to TP at their 10-week follow-up [28]. However, the smaller studies by Pota et al. [30] and Romano et al. [31] observed important differences in pain scores (difference of more than 2 points in 0–10 NRS) by using PG as an adjunct to BP and CX, respectively. There were also no significant differences when patients were assessed as success or failure with either GB versus placebo (Fig 3c) or PG versus active comparator (Fig 3d).
Fig. 3. Analyses of pain relief with GB or PG in patients with CLBP. 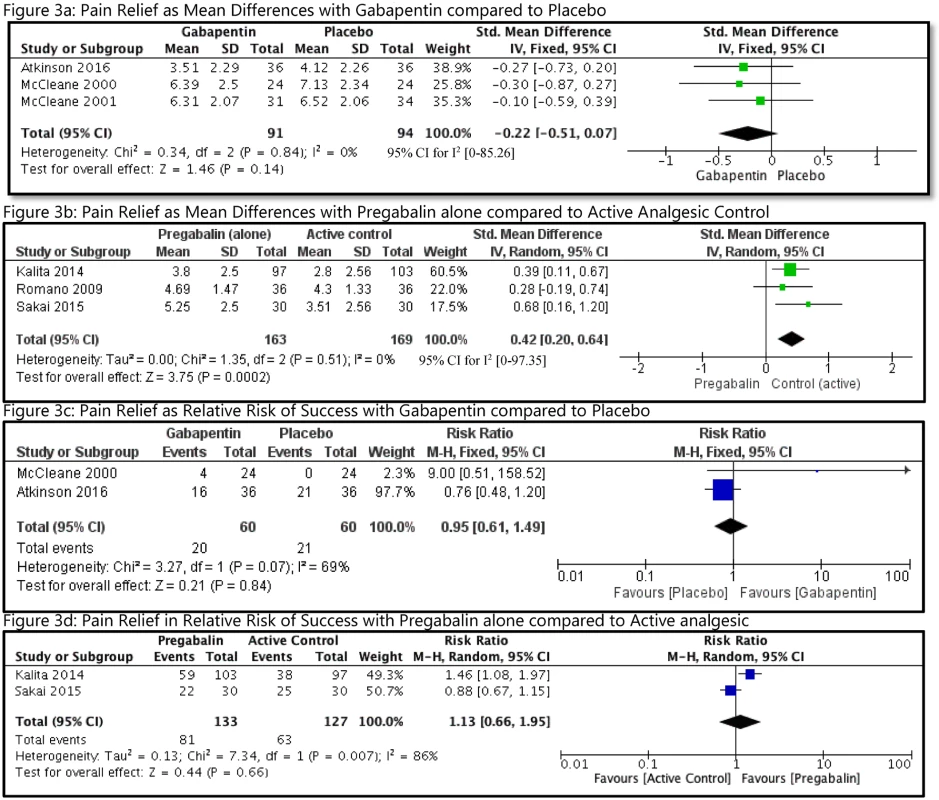
CLBP, chronic low back pain; GB, gabapentin; IV, intravenous; M-H, Mantel-Haenszel; PG, pregabalin. Tab. 2. GRADE summary of findings. 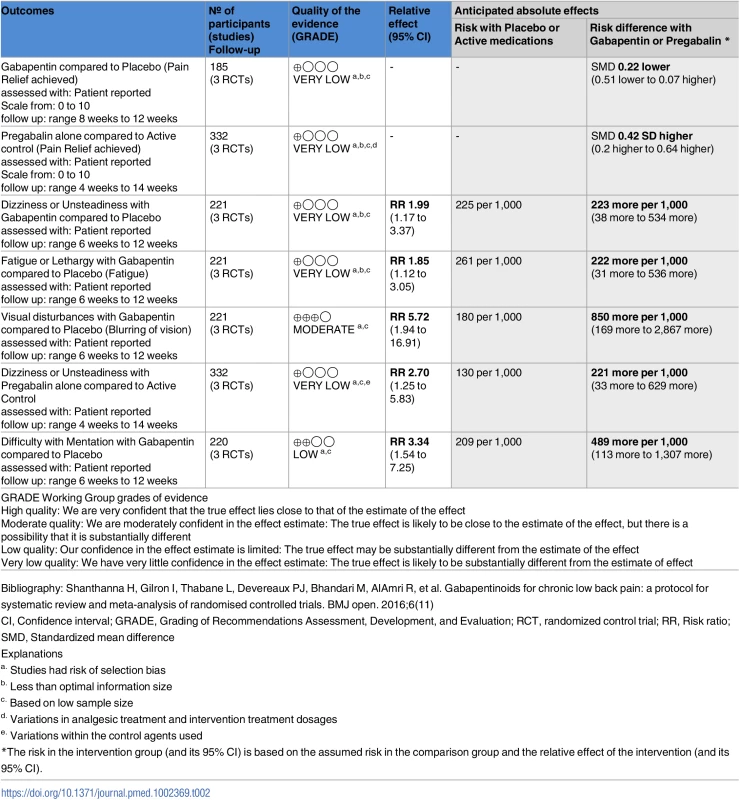
Gabapentin or pregabalin compared to placebo or active medications for chronic low back pain: A systematic review and meta-analysis of randomized control trials. Adverse effects
There were no deaths or hospitalizations reported. The reasons for study withdrawal were not provided in all studies. All adverse effects reported in more than 1 study are summarized in Table 3. Compared with placebo, the following adverse events were more commonly reported with GB: dizziness-(RR = 1.99, 95% CI [1.17 to 3.37], I2 = 49); fatigue (RR = 1.85, 95% CI [1.12 to 3.05], I2 = 0); difficulties with mentation (RR = 3.34, 95% CI [1.54 to 7.25], I2 = 0); and visual disturbances (RR = 5.72, 95% CI [1.94 to 16.91], I2 = 0) (Fig 4). The GRADE quality of evidence was noted to be very low for dizziness and fatigue, low for difficulties with mentation, and moderate for visual disturbances (Table 2). The resulting absolute risk increase (ARI) percentage and necessary number needed to harm (NNH) with 95% CI for dizziness, fatigue, mental difficulties, and visual disturbances were 14% and 7 (4 to 30), 13% and 8 (4 to 44), 16% and 6 (4 to 15), and 15% and 6 (4 to 13), respectively. With PG, dizziness was more common compared to the active comparator (RR = 2.70, 95% CI [1.25 to 5.83], I2 = 0), with very low quality of evidence. The ARI% and NNH were 9% and 11(6 to 30).
Fig. 4. Analyses of adverse effects observed with GB or PG in CLBP. 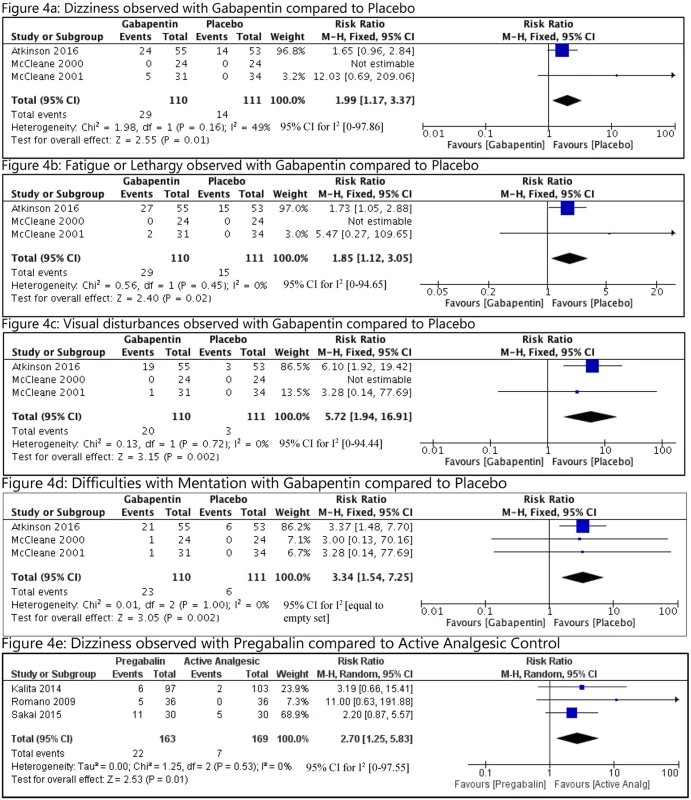
CLBP, chronic low back pain; GB, gabapentin; IV, intravenous; M-H, Mantel-Haenszel; PG, pregabalin. Tab. 3. Summary of adverse effects observed in more than one study. 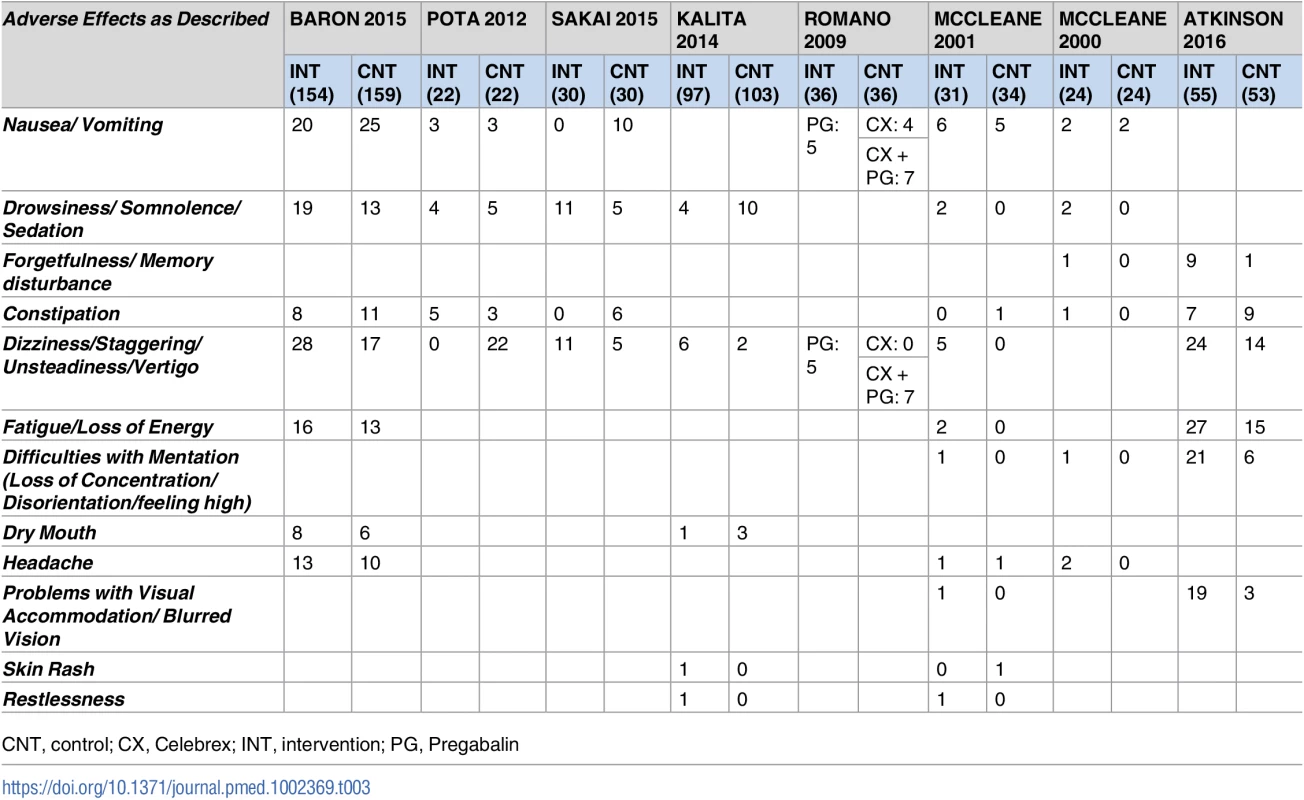
CNT, control; CX, Celebrex; INT, intervention; PG, Pregabalin Secondary outcomes
These are summarized in Tables 4 and 5. All studies except Pota et al. had patients who were LTFU [30]. There were 5 studies that did include LTFU, even with >5% of their randomized sample, in their final analysis [25–27, 31, 32]. Functional improvement was observed in 5 studies using various scales [25, 26, 28, 29, 32]. The results indicate that there were improvements from the baseline in both treatment and control groups, without much difference between the groups. Emotional functioning was observed by 3 studies, but 2 studies reported the final scores, with no between-group differences [25, 28]. Global improvement of change was reported as physician-reported by Atkinson et al. [25] and patient-reported by Baron et al. [28]. There were no between-group differences in studies with GB or PG, respectively.
Tab. 4. Summary of secondary outcomes-participant disposition. 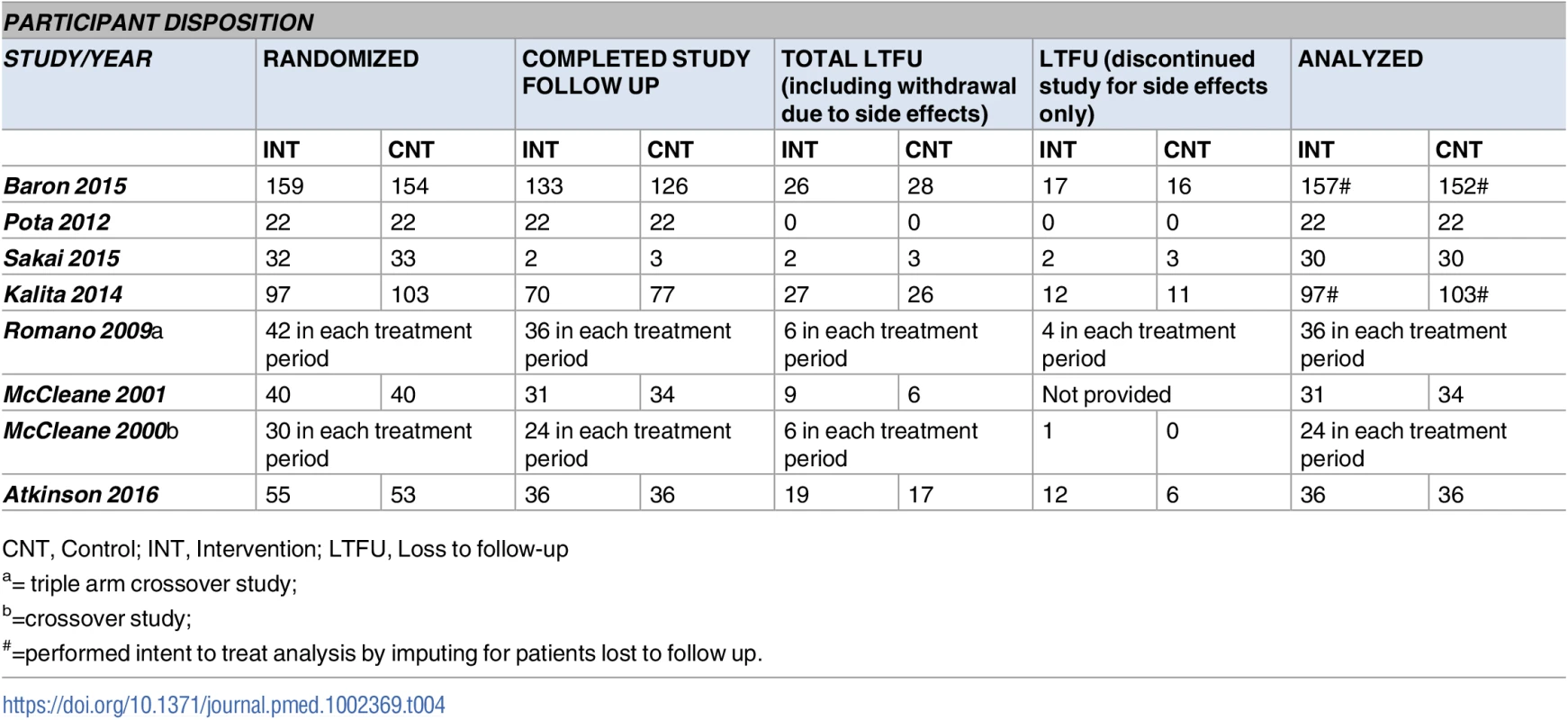
CNT, Control; INT, Intervention; LTFU, Loss to follow-up Tab. 5. Summary of secondary outcomes. 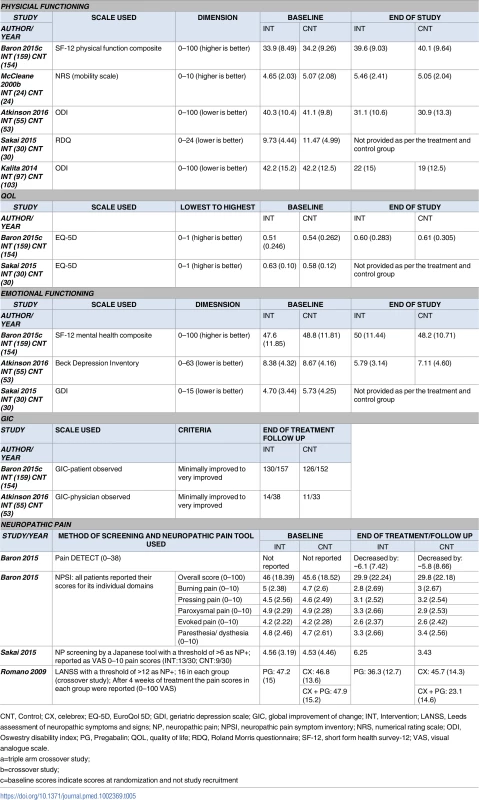
CNT, Control; CX, celebrex; EQ-5D, EuroQol 5D; GDI, geriatric depression scale; GIC, global improvement of change; INT, Intervention; LANSS, Leeds assessment of neuropathic symptoms and signs; NP, neuropathic pain; NPSI, neuropathic pain symptom inventory; NRS, numerical rating scale; ODI, Oswestry disability index; PG, Pregabalin; QOL, quality of life; RDQ, Roland Morris questionnaire; SF-12, short form health survey-12; VAS, visual analogue scale. RoB across studies (Fig 2)
Based on our criteria, potential bias due to outcome threshold, assessment time point, and publication bias due to low sample size was observed largely by 5 studies [26, 27, 30–32].
Subgroup analysis
NP was assessed using a screening questionnaire in 3 studies. Sakai et al. observed pain scores to decrease more with tramacet compared to PG in NP patients [32]. Baron et al. observed no differences in the components of neuropathic pain symptom inventory scores using PG plus TP in comparison to TP alone [28]. Whereas, Romano et al. observed that pain scores decreased significantly in patients of NP with PG as well as in combination with CX [31].
Sensitivity analysis
The analyses for GB versus placebo, and PG versus active comparator withstood sensitivity analysis for LTFU >5% using progressively stringent imputation strategies for mean pain scores.
Discussion
Despite the widespread use, our systematic review with meta-analysis found that there are very few RCTs that have attempted to assess the benefit of using GB or PG in patients of CLBP. Use of GB and PG, compared to placebo and active analgesic comparators, respectively, were associated with significant increase in adverse effects without limited evidence for improvement in pain scores or other outcomes. We were unable to examine the pooled effect of using PG as an adjuvant analgesic medication given the limited evidence and heterogeneity of studies. It is reasonable to assume that the clinical benefit would depend upon the primary medication and its potency within each study. The differences within the results of Pota et al. [30] and Romano et al. [31], compared to Baron et al. [28] could be attributed to methodological differences. The study by Baron et al. had a larger sample size along with longer duration of follow up. Hence, the existing evidence does not support the use of gabapentinoids for predominant CLBP, and calls for larger, high quality RCTs to more definitively inform this issue.
Considering the expanding use of gabapentinoids for chronic pain and CLBP [33, 34], this review fulfils the immediate need to scrutinize and closely examine the existing evidence. Noting that there is a published Cochrane protocol [35], ours is the first review combined with meta-analysis to examine the benefits and safety of gabapentinoids in CLBP. Results of our review are in contrast with nonrandomized studies that have shown benefit with PG in patients of CLBP [36, 37]. Gabapentinoids have proven efficacy in NP conditions [38]. However, they are also widely used for conditions in which the neuropathic component is difficult to establish, most of which are off label uses [12]. This development perhaps reflects the penumbra sort of effect (clinicians generalizing the selection criteria of clinical studies into their patient population without recognizing the limitations) [39]. In England, there was a 46% and 53% rise in the prescription use of GB and PG respectively from 2011 to 2013 alone [13]. A recent Canadian study showed that the off-label use of PG is as high as 75%, and the most prevalent condition of use was CLBP [40]. The true burden of NP in CLBP is hard to establish [41]. Distribution of pain can be considered as a corollary of the pathological process, and it is important to broadly classify patients based on their predominance of axial or leg pain for diagnosis and management [2]. A common assumption is of leg pain indicating NP. However, in most cases leg pain is nonspecific and inconsistent with radicular pain, and only a painful radiculopathy with sensory signs would fulfill the diagnosis of definite NP [41]. Even if one considers that gabapentinoids are effective against NP related to CLBP, contrasting evidences are observed in literature. In patients of radicular pain or pain of spinal stenosis, observational studies of CLBP demonstrate significant improvements with PG [42, 43]. However, RCTs performed by Baron et al. in patients of lumbar radiculopathy and Markman et al. in patients of spinal stenosis did not find clinical improvements when PG was compared with placebo [44, 45]. Cohen et al. examined the benefit of GB in patients of leg pain and found no difference as compared to epidural steroid injections [46]. Even within the included study by Baron et al., the reduction of pain and NP symptoms was similar with the combination of PG with TP, compared to TP [28]. Our results are important for practitioners across several specialties who treat patients with CLBP and have to decide on the relative merits and demerits of treatment with gabapentinoids.
Our review is not without its limitations. We excluded studies in patients of predominant leg pain or spinal stenosis. This was done to limit the heterogeneity within our study population. Although the measure of heterogeneity (I2-proportion of variability that can be explained by individual studies) was low in many comparisons, the CIs around those I2 were very wide, reflecting that there is uncertainty in any claim of homogeneity. Heterogeneity has been shown to be an issue with meta-analyses involving a smaller number of trials or events [47]. Topiramate was not considered in this review, as it has a slightly different mechanism of action and is not commonly used, although some controlled studies have shown benefit [48]. The use of PG or GB is associated with significant adverse effects, cost [13], and potential for misuse [34, 49].
Our review demonstrates that there is limited evidence on the use of gabapentinoids in nonspecific CLBP, and the existing evidence in the form of RCTs does not support their use. It is possible that ongoing or unpublished studies [50, 51] may more definitively inform us on this issue, although one such study specific to CLBP was withdrawn prior to enrollment [52].
Supporting Information
Zdroje
1. Deyo RA, Weinstein JN. Low back pain. The New England journal of medicine. 2001;344(5):363–70. doi: 10.1056/NEJM200102013440508 11172169
2. Hooten WM, Cohen SP. Evaluation and Treatment of Low Back Pain: A Clinically Focused Review for Primary Care Specialists. Mayo Clin Proc. 2015;90(12):1699–718. doi: 10.1016/j.mayocp.2015.10.009 26653300
3. Hoy D, Bain C, Williams G, March L, Brooks P, Blyth F, et al. A systematic review of the global prevalence of low back pain. Arthritis Rheum. 2012;64(6):2028–37. doi: 10.1002/art.34347 22231424
4. Morlion B. Chronic low back pain: pharmacological, interventional and surgical strategies. Nature reviews Neurology. 2013;9(8):462–73. doi: 10.1038/nrneurol.2013.130 23817349
5. Shanthanna H, Gilron I, Thabane L, Devereaux PJ, Bhandari M, AlAmri R, et al. Gabapentinoids for chronic low back pain: a protocol for systematic review and meta-analysis of randomised controlled trials. BMJ open. 2016;6(11).
6. Chou R, Huffman LH. Medications for acute and chronic low back pain: a review of the evidence for an American Pain Society/American College of Physicians clinical practice guideline. Ann Intern Med. 2007;147(7):505–14. 17909211
7. White AP, Arnold PM, Norvell DC, Ecker E, Fehlings MG. Pharmacologic management of chronic low back pain: synthesis of the evidence. Spine. 2011;36(21 Suppl):S131–43. 21952185
8. Patel R, Dickenson AH. Mechanisms of the gabapentinoids and alpha 2 delta-1 calcium channel subunit in neuropathic pain. Pharmacol Res Perspect. 2016;4(2):e00205. doi: 10.1002/prp2.205 27069626
9. Maizels M, McCarberg B. Antidepressants and antiepileptic drugs for chronic non-cancer pain. Am Fam Physician. 2005;71(3):483–90. 15712623
10. Moore RA, Straube S, Wiffen PJ, Derry S, McQuay HJ. Pregabalin for acute and chronic pain in adults. Cochrane Database Syst Rev. 2009(3):Cd007076. doi: 10.1002/14651858.CD007076.pub2 19588419
11. Chaparro LE, Smith SA, Moore RA, Wiffen PJ, Gilron I. Pharmacotherapy for the prevention of chronic pain after surgery in adults. Cochrane Database Syst Rev. 2013(7):Cd008307. doi: 10.1002/14651858.CD008307.pub2 23881791
12. Mack A. Examination of the evidence for off-label use of gabapentin. J Manag Care Pharm. 2003;9(6):559–68. doi: 10.18553/jmcp.2003.9.6.559 14664664
13. Public Health England and National Health Services, UK. Advice for prescribers on the risk of the misuse of pregabalin and gabapentin. https://www.gov.uk/government/publications/pregabalin-and-gabapentin-advice-for-prescribers-on-the-risk-of-misuse. First published 14 December 2014. Last accessed 22 January, 2017.
14. Dworkin RH, Turk DC, Farrar JT, Haythornthwaite JA, Jensen MP, Katz NP, et al. Core outcome measures for chronic pain clinical trials: IMMPACT recommendations. Pain. 2005;113(1–2):9–19. doi: 10.1016/j.pain.2004.09.012 15621359
15. Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. International journal of surgery (London, England). 2010;8(5):336–41.
16. Viera AJ, Garrett JM. Understanding interobserver agreement: the kappa statistic. Family medicine. 2005;37(5):360–3. 15883903
17. Schandelmaier S, Ebrahim S, Burkhardt SC, de Boer WE, Zumbrunn T, Guyatt GH, et al. Return to work coordination programmes for work disability: a meta-analysis of randomised controlled trials. PLoS ONE. 2012;7(11):e49760. doi: 10.1371/journal.pone.0049760 23185429
18. Higgins JPT G S. Cochrane Handbook for Systematic Reviews of Interventions. Version 5.1.0 The Cochrane Collaboration: The Cochrane Collaboration; 2011. Last accessed 22 January 2017. http://handbook.cochrane.org/
19. Chan AW, Altman DG. Identifying outcome reporting bias in randomised trials on PubMed: review of publications and survey of authors. BMJ (Clinical research ed). 2005;330(7494):753.
20. Andrew Moore R, Eccleston C, Derry S, Wiffen P, Bell RF, Straube S, et al. "Evidence" in chronic pain—establishing best practice in the reporting of systematic reviews. Pain. 2010;150(3):386–9. 20627575
21. Ioannidis JP, Cappelleri JC, Lau J. Issues in comparisons between meta-analyses and large trials. Jama. 1998;279(14):1089–93. 9546568
22. Sterne JA, Gavaghan D, Egger M. Publication and related bias in meta-analysis: power of statistical tests and prevalence in the literature. Journal of clinical epidemiology. 2000;53(11):1119–29. 11106885
23. Ebrahim S, Johnston BC, Akl EA, Mustafa RA, Sun X, Walter SD, et al. Addressing continuous data measured with different instruments for participants excluded from trial analysis: a guide for systematic reviewers. J Clin Epidemiol 2014 May;67(5):560–70. doi: 10.1016/j.jclinepi.2013.11.014 24613497
24. Akl EA, Johnston BC, Alonso-Coello P, Neumann I, Ebrahim S, Briel M, et al. Addressing dichotomous data for participants excluded from trial analysis: a guide for systematic reviewers. PLoS ONE. 2013;8(2):e57132. doi: 10.1371/journal.pone.0057132 23451162
25. Atkinson JH, Slater MA, Capparelli EV, Patel SM, Wolfson T, Gamst A, et al. A randomized controlled trial of gabapentin for chronic low back pain with and without a radiating component. Pain. 2016;157(7):1499–507. doi: 10.1097/j.pain.0000000000000554 26963844
26. McCleane GJ. Gabapentin reduces chronic benign nociceptive pain: a double-blind, placebo-controlled cross-over study. The Pain Clinic. 2000;12(2):81–5.
27. McCleane GJ. Does gabapentin have an analgesic effect on background, movement and referred pain? A randomised, double-blind, placebo controlled study. The Pain Clinic. 2001;13(2):103–7.
28. Baron R, Martin-Mola E, Muller M, Dubois C, Falke D, Steigerwald I. Effectiveness and Safety of Tapentadol Prolonged Release (PR) Versus a Combination of Tapentadol PR and Pregabalin for the Management of Severe, Chronic Low Back Pain With a Neuropathic Component: A Randomized, Double-blind, Phase 3b Study. Pain Pract. 2015;15(5):455–70. doi: 10.1111/papr.12200 24738609
29. Kalita J, Kohat AK, Misra UK, Bhoi SK. An open labeled randomized controlled trial of pregabalin versus amitriptyline in chronic low backache. J Neurol Sci. 2014;342(1–2):127–32. doi: 10.1016/j.jns.2014.05.002 24857356
30. Pota V, Barbarisi M, Sansone P, Moraci M, Pace MC, Passavanti MB, et al. Combination therapy with transdermal buprenorphine and pregabalin for chronic low back pain. Pain Manag. 2012;2(1):23–31. doi: 10.2217/pmt.11.71 24654615
31. Romano CL, Romano D, Bonora C, Mineo G. Pregabalin, celecoxib, and their combination for treatment of chronic low-back pain. J Orthop Traumatol. 2009;10(4):185–91. doi: 10.1007/s10195-009-0077-z 19921480
32. Sakai Y, Ito K, Hida T, Ito S, Harada A. Pharmacological management of chronic low back pain in older patients: a randomized controlled trial of the effect of pregabalin and opioid administration. European spine journal: official publication of the European Spine Society, the European Spinal Deformity Society, and the European Section of the Cervical Spine Research Society. 2015;24(6):1309–17.
33. Morlion B. Pharmacotherapy of low back pain: targeting nociceptive and neuropathic pain components. Current medical research and opinion. 2011;27(1):11–33. doi: 10.1185/03007995.2010.534446 21083513
34. Chiappini S, Schifano F. A Decade of Gabapentinoid Misuse: An Analysis of the European Medicines Agency's 'Suspected Adverse Drug Reactions' Database. CNS drugs. 2016;30(7):647–54. doi: 10.1007/s40263-016-0359-y 27312320
35. Bezerra DM, El Dib R, Vidal EIO, De Barros GAM, Chou R, Fukushima F. Anticonvulsants for chronic low-back pain. Cochrane Database of Systematic Reviews. 2014(6). CD011171
36. Tetsunaga T, Tetsunaga T, Tanaka M, Sugimoto Y, Takigawa T, Ozaki T. Outcomes of pregabalin in lumbar-disease patients with depression. Journal of orthopaedic science: official journal of the Japanese Orthopaedic Association. 2014;19(2):229–34.
37. Sakai Y, Ito K, Hida T, Ito S, Harada A. Neuropathic pain in elderly patients with chronic low back painand effects of pregabalin: a preliminary study. Asian spine journal. 2015;9(2):254–62. doi: 10.4184/asj.2015.9.2.254 25901238
38. Finnerup NB, Attal N, Haroutounian S, McNicol E, Baron R, Dworkin RH, et al. Pharmacotherapy for neuropathic pain in adults: a systematic review and meta-analysis. Lancet Neurol. 2015;14(2):162–73. doi: 10.1016/S1474-4422(14)70251-0 25575710
39. Simunovic M, Baxter NN. Knowledge translation research: a review and new concepts from a surgical case study. Surgery. 2009;145(6):639–44. doi: 10.1016/j.surg.2008.11.011 19486766
40. Giladi H, Choinière M, Fitzcharles M-A, Ware MA, Tan X, Shir Y. Pregabalin for chronic pain: does one medication fit all? Current medical research and opinion. 2015;31(7):1403–11. doi: 10.1185/03007995.2015.1040750 25868712
41. Baron R, Binder A, Attal N, Casale R, Dickenson AH, Treede RD. Neuropathic low back pain in clinical practice. Eur J Pain. 2016; 20(6): 861–873. doi: 10.1002/ejp.838 26935254
42. Taguchi T, Igarashi A, Watt S, Parsons B, Sadosky A, Nozawa K, et al. Effectiveness of pregabalin for the treatment of chronic low back pain with accompanying lower limb pain (neuropathic component): a non-interventional study in Japan. J Pain Res. 2015;8 : 487–97. doi: 10.2147/JPR.S88642 26346468
43. Orita S, Yamashita M, Eguchi Y, Suzuki M, Inoue G, Miyagi M, et al. Pregabalin for Refractory Radicular Leg Pain due to Lumbar Spinal Stenosis: A Preliminary Prospective Study. Pain Research and Management. 2016;2016 : 10.
44. Baron R, Freynhagen R, Tolle TR, Cloutier C, Leon T, Murphy TK, et al. The efficacy and safety of pregabalin in the treatment of neuropathic pain associated with chronic lumbosacral radiculopathy. Pain. 2010;150(3):420–7. doi: 10.1016/j.pain.2010.04.013 20493632
45. Markman JD, Frazer ME, Rast SA, McDermott MP, Gewandter JS, Chowdhry AK, et al. Double-blind, randomized, controlled, crossover trial of pregabalin for neurogenic claudication. Neurology. 2015;84(3):265–72. doi: 10.1212/WNL.0000000000001168 25503625
46. Cohen SP, Hanling S, Bicket MC, White RL, Veizi E, Kurihara C, et al. Epidural steroid injections compared with gabapentin for lumbosacral radicular pain: multicenter randomized double blind comparative efficacy study. BMJ: British Medical Journal. 2015;350:h1748. doi: 10.1136/bmj.h1748 25883095
47. Thorlund K, Imberger G, Johnston BC, Walsh M, Awad T, Thabane L, et al. Evolution of heterogeneity (I2) estimates and their 95% confidence intervals in large meta-analyses. PLoS ONE. 2012;7(7):e39471. doi: 10.1371/journal.pone.0039471 22848355
48. Muehlbacher M, Nickel MK, Kettler C, Tritt K, Lahmann C, Leiberich PK, et al. Topiramate in treatment of patients with chronic low back pain: a randomized, double-blind, placebo-controlled study. Clin J Pain. 2006;22(6):526–31. 16788338
49. Spence D. Bad medicine: gabapentin and pregabalin. BMJ (Clinical research ed). 2013;347:f6747.
50. Mathieson S, Maher CG, McLachlan AJ, Latimer J, Koes BW, Hancock MJ, et al. PRECISE—pregabalin in addition to usual care for sciatica: study protocol for a randomised controlled trial. Trials. 2013;14(1):213.
51. Clinical Trials Registry. https://clinicaltrials.gov/ct2/show/NCT02273908. Last accessed 22 January, 2017.
52. Clinical Trials Registry. https://www.clinicaltrials.gov/ct2/show/NCT01298466. Last accessed 22 January, 2017.
Štítky
Interní lékařství
Článek vyšel v časopisePLOS Medicine
Nejčtenější tento týden
2017 Číslo 8- Berberin: přírodní hypolipidemikum se slibnými výsledky
- Léčba bolesti u seniorů
- Příznivý vliv Armolipidu Plus na hladinu cholesterolu a zánětlivé parametry u pacientů s chronickým subklinickým zánětem
- Jak postupovat při výběru betablokátoru − doporučení z kardiologické praxe
- Červená fermentovaná rýže účinně snižuje hladinu LDL cholesterolu jako vhodná alternativa ke statinové terapii
-
Všechny články tohoto čísla
- Harmonization of community health worker programs for HIV: A four-country qualitative study in Southern Africa
- Gestational diabetes mellitus and interpregnancy weight change: A population-based cohort study
- Association of pre-pregnancy body mass index with offspring metabolic profile: Analyses of 3 European prospective birth cohorts
- Pregnant and breastfeeding women: A priority population for HIV viral load monitoring
- Malaria, malnutrition, and birthweight: A meta-analysis using individual participant data
- Childhood adiposity and risk of type 1 diabetes: A Mendelian randomization study
- Unsupervised primaquine for the treatment of malaria relapses in southern Papua: A hospital-based cohort study
- Effectiveness of a brief behavioural intervention on psychological distress among women with a history of gender-based violence in urban Kenya: A randomised clinical trial
- Impact of fortified versus unfortified lipid-based supplements on morbidity and nutritional status: A randomised double-blind placebo-controlled trial in ill Gambian children
- Identification of factors associated with stillbirth in the Indian state of Bihar using verbal autopsy: A population-based study
- Counting stillbirths and achieving accountability: A global health priority
- Evaluating the impact of Affordable Care Act repeal on America's opioid epidemic
- Benefits and safety of gabapentinoids in chronic low back pain: A systematic review and meta-analysis of randomized controlled trials
- Evaluation of novel computerized tomography scoring systems in human traumatic brain injury: An observational, multicenter study
- Assessing the impact of healthcare research: A systematic review of methodological frameworks
- Lay worker-administered behavioral treatments for psychological distress in resource-limited settings: Time to move from evidence to practice?
- Antimicrobial resistance: The complex challenge of measurement to inform policy and the public
- PLOS Medicine
- Archiv čísel
- Aktuální číslo
- Informace o časopisu
Nejčtenější v tomto čísle- Childhood adiposity and risk of type 1 diabetes: A Mendelian randomization study
- Benefits and safety of gabapentinoids in chronic low back pain: A systematic review and meta-analysis of randomized controlled trials
- Lay worker-administered behavioral treatments for psychological distress in resource-limited settings: Time to move from evidence to practice?
- Evaluating the impact of Affordable Care Act repeal on America's opioid epidemic
Kurzy
Zvyšte si kvalifikaci online z pohodlí domova
Současné možnosti léčby obezity
nový kurzAutoři: MUDr. Martin Hrubý
Všechny kurzyPřihlášení#ADS_BOTTOM_SCRIPTS#Zapomenuté hesloZadejte e-mailovou adresu, se kterou jste vytvářel(a) účet, budou Vám na ni zaslány informace k nastavení nového hesla.
- Vzdělávání