-
Články
Top novinky
Reklama- Vzdělávání
- Časopisy
Top články
Nové číslo
- Témata
Top novinky
Reklama- Videa
- Podcasty
Nové podcasty
Reklama- Kariéra
Doporučené pozice
Reklama- Praxe
Top novinky
ReklamaClinical Action against Drunk Driving
In advance of a safety campaign on 17 March 2017, Donald Redelmeier and Allan Detsky call on physicians and clinical colleagues to reduce the chances that patients will drive drunk.
Published in the journal: . PLoS Med 14(2): e32767. doi:10.1371/journal.pmed.1002231
Category: Perspective
doi: https://doi.org/10.1371/journal.pmed.1002231Summary
In advance of a safety campaign on 17 March 2017, Donald Redelmeier and Allan Detsky call on physicians and clinical colleagues to reduce the chances that patients will drive drunk.
In 2014, over 100,000 people in the United States were hospitalized because of alcohol-related traffic crashes, and 9,967 died (exceeding the 6,721 US deaths from HIV in the same year) [1,2]. On 17 March 2017, the National Highway Traffic Safety Administration (NHTSA) plans to promote a safety campaign against drunk driving. Past estimates suggest that law enforcement against drunk driving reduces traffic fatalities by 20% and that high-probability detection is more effective than high-severity punishment [3,4]. Yet, 12 states in the US, including the large states of Texas and Minnesota, prohibit random sobriety checkpoints, and the remaining have uneven efforts against drunk driving [5]. This Perspective identifies some groups with a vested interest in preventing drunk driving, describes reasons for the relative inaction, and proposes more action by physicians.
Traditionally, physicians and allied health care providers have deferred to others about how to address the health risks of drunk driving. One explanation is that drunk driving is a behavioral choice, and behavioral change is difficult to effect in a time-limited clinical encounter [6]. Moreover, preventive care may provide less evident benefit to the patient than prescribing an acid blocker, for example, to treat symptomatic alcohol-induced gastritis. While a pregnant woman who drinks alcohol is likely to be warned by her obstetrician or midwife on the risks to fetal development, most patients in our experience who are prone to drunk driving are easily missed because physicians rarely ask about drunk driving, despite often asking about alcohol. As a consequence, standard care may fail to identify this prevalent, modifiable, and serious health risk.
Vehicle manufacturers are the most powerful commercial group that can promote traffic safety. Over time, this industry has carefully developed and marketed technologies to protect drivers, such as seat belts, airbags, antilock brakes, and safety glass. Currently, the main technology to prevent drunk driving is an ignition interlock that forces drivers to have a breath test before engine engagement. This device, now imposed only on the vehicles of convicted drunk drivers, is unlikely to be adopted broadly any time soon unless manufacturers want to boast that they make the safest cars for those prone to drunk driving. The net result is that vehicle regulators in the US are unable to rely on manufacturer innovations or economic forces to prevent drunk driving.
Other large groups have even less incentive to promote sobriety while driving. Alcohol manufacturers promote “responsible drinking,” which is a vacuous tautology because adverse events can be deemed “irresponsible” by rhetorical hindsight. Celebrities in the entertainment industry are occasionally charged with drunk driving yet rarely express enduring regret. Lawyers gain little financial benefit from deterring drunk drivers, whereas some profit substantially by defending those who have deep pockets and are charged with drunk driving. Individual police officers themselves sometimes consider traffic enforcement as low-prestige work with little career satisfaction [7]. Driving enthusiasts argue that enforcement mostly inconveniences safe drivers to catch a few deviants. Those caught driving drunk are rarely grateful for the penalties.
Sometimes medical science can inspire behavior change, and drunk driving could seem amenable to research because of the large number of incidents. A rigorous clinical trial, however, cannot be conducted unless broad regions are willing to implement interventions in a thorough manner. An epidemiological analysis contrasting different states would also be easily misinterpreted because of dissimilarities across regions and diversity within regions (for example, the risk of dying in an alcohol-related traffic crash is three times higher in South Carolina than in New Jersey even though both states allow random sobriety checkpoints) [1]. Because individuals are not randomly assigned to driving locations, furthermore, the confounders are almost boundless [8]. These research limitations mean that scientific evidence is unlikely to cause people to stop drunk driving [9].
Activism and Politics
The most prominent body advocating change has been Mothers Against Drunk Driving (MADD), a citizen group with deeply motivated members [10]. The mission of MADD is to “stop drunk driving, support the victims of this violent crime, and prevent underage drinking.” MADD has successfully pushed for drunk-driving laws, increased public awareness, designated-driver initiatives, alcohol ignition interlock programs, and victim impact panels. Yet, MADD is mostly a volunteer organization, with fewer than 500 employees. MADD has also been criticized for having administrative costs and for shifting towards broader prohibitions against alcohol consumption [11]. Ultimately, MADD has no power to enforce drunk-driving laws.
Politicians in the US seldom discuss traffic safety with the same zeal that they direct at debates on economic growth, domestic terrorism, public scandals, gun deaths, climate change, and other public-policy priorities. Indeed, making a political issue of drunk driving can carry particular risks because the historical failure of prohibition decades ago (1920 to 1933) means that a well-intentioned politician is easily ridiculed or mischaracterized as being antialcohol [11]. A US politician who seeks re-election will rarely promise action against drunk driving. The US political process, therefore, exchanges safety for freedom and tolerates a remarkably high rate of alcohol-related traffic fatalities relative to other countries (Fig 1).
Fig. 1. Alcohol-related traffic fatalities in the US and other countries. 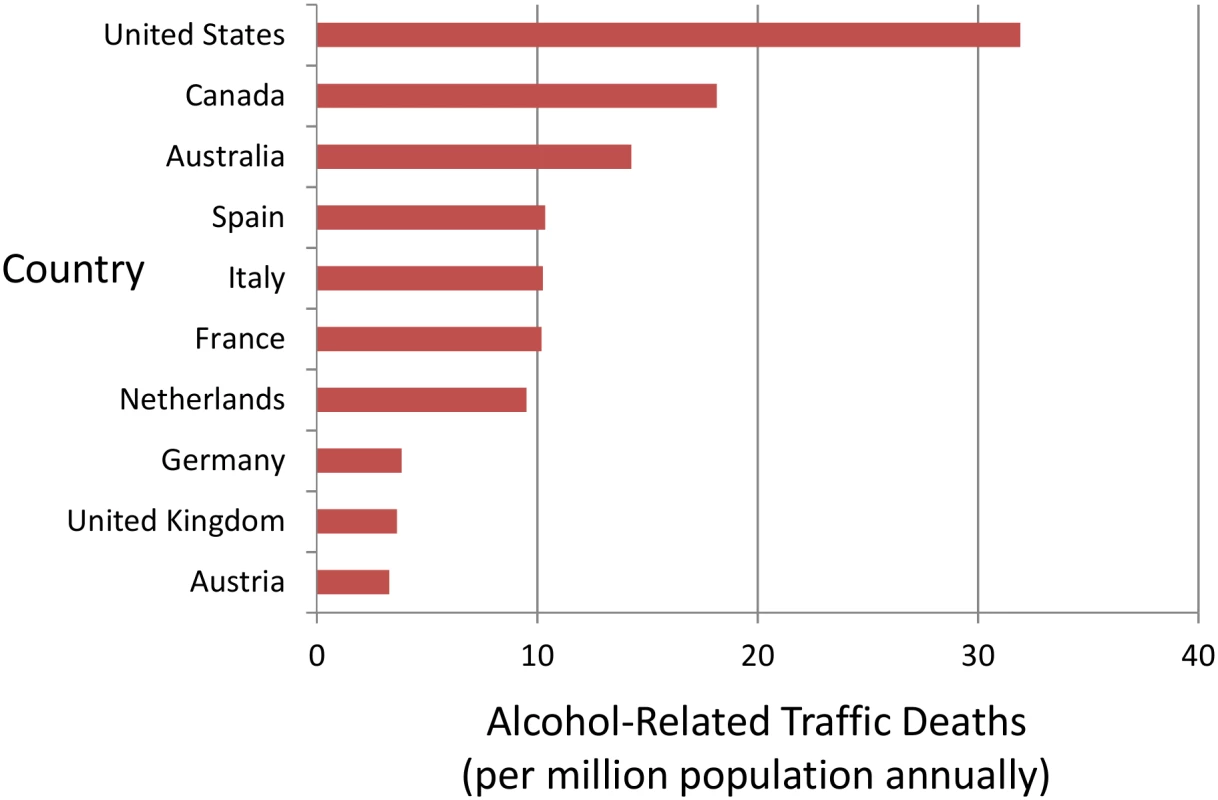
Histogram of alcohol-related traffic fatalities in the US and other countries. The vertical axis shows ten countries sequenced by death rates. The horizontal axis shows alcohol-related traffic deaths as fatalities per million population annually. Data are from the Organisation for Economic Co-operation and Development (OECD) Road Safety Annual Report 2015 authored by the International Traffic Safety Data and Analysis Group (IRTAD) and available at the following website: http://www.oecd-ilibrary.org/transport/road-safety-annual-report-2015_irtad-2015-en. The death rates were calculated from Table 1.3 of the report and individual country alcohol profiles. The results show high rates of alcohol-related traffic fatalities in the US relative to other countries. Medical Initiatives
Health care providers are perhaps the one remaining large powerful group with a profound commitment to health. Physicians and allied life-saving professionals sometimes advocate to reduce cigarette smoking, drug abuse, domestic violence, or other societal epidemics. Drunk driving causes major mortality and morbidity that is utterly preventable, unlike many advanced diseases. The losses are also tragic because offenders usually have no malicious intent yet many lives are irrevocably altered (including their own). Because the market forces for commercial industries run in a different direction, physicians could advocate more for what works against drunk driving (Box 1) [12]. Civic advocacy, however, rarely leads to immediate gratification and sometimes deteriorates into dissenting backlash [13].
Box 1. Physician Strategies to Prevent Drunk Driving
Alcohol screening and brief interventions for patients with alcohol problems
Physician warnings for patients who sometimes drink and drive
Treatment of patients diagnosed with alcohol dependence
Counseling of patients not to ride with drunk drivers
Supporting enforcement of laws against drunk driving
Promoting sobriety checkpoints in local communities
Lending voice to mass media campaigns against drunk driving
Joining multicomponent interventions in coalitions of community group members
Patients do not want to become traffic statistics, tend to listen to their physicians, and take advice seriously. When asked about alcohol consumption, for example, patients often respond truthfully inside a private medical relationship. A simple extension, therefore, might be for physicians to also ask patients about past episodes of drinking and driving. Patients identified, in turn, could be recommended a taxi service, ride-sharing option (e.g., Uber and Lyft), or a designated-driver substitute. The intent is to suggest safer alternatives so patients who drink do not need to drive [14]. The intent is not to preach sobriety or to betray patient trust. Ideally, these harm-reduction strategies should be planned in advance because later inebriation will predictably impair judgment.
In Canada, recent financial incentives have been effective at motivating physicians’ warnings for medically unfit drivers and reducing the risk of a traffic crash for patients diagnosed with alcoholism [15]. A direct incentive for physicians’ warnings against drunk driving could be considered to address the problem in the US (the fee in Canada is C$36.25). Physicians need to first realize, of course, that an average drunk driver has a 5%–15% lifetime risk of dying in a traffic crash, physician warnings lead to a one-third relative reduction in the subsequent risk of a serious traffic crash, and most adults who drink and drive visit a physician in the year before dying [16]. The epidemic of drunk driving needs to be addressed in the US, and 17 March 2017 is a time for physicians to think more about clinical action against drunk driving.
Zdroje
1. Department of Transportation (US), National Highway Traffic Safety Administration (NHTSA). Traffic Safety Facts 2014 data: alcohol-impaired driving. Washington, DC: NHTSA; 2015. http://www-nrd.nhtsa.dot.gov/Pubs/812231.pdf
2. Department of Health and Human Services (US). Centers for Disease Control and Prevention. Deaths: Final Data for 2014: Table 10. Washington, DC: CDC; 2016. http://www.cdc.gov/nchs/data/nvsr/nvsr65/nvsr65_04.pdf
3. Elder RW, Shults RA, Sleet DA, Nichols JL, Zaza S, Thompson RS. Effectiveness of sobriety checkpoints for reducing alcohol-involved crashes. Traffic Injury Prevention 2002;3(4): 266–274.
4. Bergen G, Pitan A, Qu S, Shults RA, Chattopadhyay SK, Elder RW, et al; Community Preventive Services Task Force. Publicized sobriety checkpoint programs: a community guide systematic review. Am J Prev Med. 2014;46(5): 529–539. doi: 10.1016/j.amepre.2014.01.018 24745644
5. Fell JC, Ferguson SA, Williams AF, Fields M. Why are sobriety checkpoints not widely adopted as an enforcement strategy in the United States? Accid Anal Prev. 2003;35(6): 897–902. 12971924
6. Redelmeier DA, McLellan BA. Modern medicine is neglecting road traffic crashes. PLoS Med. 2013;10(6): e1001463. doi: 10.1371/journal.pmed.1001463 23776413
7. Redelmeier DA, Tibshirani RJ, Evans L. Traffic-law enforcement and risk of death from motor-vehicle crashes: case-crossover study. Lancet. 2003;361(9376): 2177–2182. doi: 10.1016/S0140-6736(03)13770-1 12842370
8. PLoS Medicine Editors. Preventing road deaths—time for data. PLoS Med. 2010;7(3): e1000257. doi: 10.1371/journal.pmed.1000257 20361021
9. Koehlmoos TP. Why aren't we listening yet? A decade of road safety begins quietly. PLoS Med. 2013;10(6): e1001464. doi: 10.1371/journal.pmed.1001464 23776414
10. Mothers Against Drunk Driving (MADD). Mission Statement. Irving, Texas: MADD National Office; 2016. http://www.madd.org/about-us/
11. Lerner BH. One for the road: Drunk driving since 1900. 1st ed. Baltimore: The Johns Hopkins University Press; 2011.
12. Centers for Disease Control and Prevention (CDC). What works: Strategies to reduce or prevent drunk driving. Atlanta:US Department of Health & Human Services; 2016. http://www.cdc.gov/motorvehiclesafety/impaired_driving/strategies.html
13. Redelmeier DA, Tversky A. Discrepancy between medical decisions for individual patients and for groups. N Engl J Med. 1990;322(16): 1162–1164. doi: 10.1056/NEJM199004193221620 2320089
14. Brazil N, Kirk DS. Uber and Metropolitan Traffic Fatalities in the United States. Am J Epidemiol. 2016;184(3): 192–198. doi: 10.1093/aje/kww062 27449416
15. Redelmeier DA, Yarnell CJ, Thiruchelvam D, Tibshirani RJ. Physicians' warnings for unfit drivers and the risk of trauma from road crashes. N Engl J Med. 2012;367(13): 1228–1236. doi: 10.1056/NEJMsa1114310 23013074
16. Redelmeier DA, Vinkatesh V, Stanbrook MB. Mandatory reporting by physicians of patients potentially unfit to drive. Open Med. 2008;2(1): e8–e17. 21602950
Štítky
Interní lékařství
Článek vyšel v časopisePLOS Medicine
Nejčtenější tento týden
2017 Číslo 2- Berberin: přírodní hypolipidemikum se slibnými výsledky
- Léčba bolesti u seniorů
- Příznivý vliv Armolipidu Plus na hladinu cholesterolu a zánětlivé parametry u pacientů s chronickým subklinickým zánětem
- Jak postupovat při výběru betablokátoru − doporučení z kardiologické praxe
- Červená fermentovaná rýže účinně snižuje hladinu LDL cholesterolu jako vhodná alternativa ke statinové terapii
-
Všechny články tohoto čísla
- Clinical Action against Drunk Driving
- Evidence for scaling up HIV treatment in sub-Saharan Africa: A call for incorporating health system constraints
- Performance and Cost-Effectiveness of Computed Tomography Lung Cancer Screening Scenarios in a Population-Based Setting: A Microsimulation Modeling Analysis in Ontario, Canada
- Clinical applicability and cost of a 46-gene panel for genomic analysis of solid tumours: Retrospective validation and prospective audit in the UK National Health Service
- Precision oncology: Charting a path forward to broader deployment of genomic profiling
- Taxes and Subsidies for Improving Diet and Population Health in Australia: A Cost-Effectiveness Modelling Study
- Delays and loss to follow-up before treatment of drug-resistant tuberculosis following implementation of Xpert MTB/RIF in South Africa: A retrospective cohort study
- Haemolysis in G6PD Heterozygous Females Treated with Primaquine for Malaria: A Nested Cohort in a Trial of Radical Curative Regimens
- Housing Improvements and Malaria Risk in Sub-Saharan Africa: A Multi-Country Analysis of Survey Data
- Estimated impact on birth weight of scaling up intermittent preventive treatment of malaria in pregnancy given sulphadoxine-pyrimethamine resistance in Africa: A mathematical model
- Serotonin transporter gene polymorphism and susceptibility to a home-visiting maternal-infant attachment intervention delivered by community health workers in South Africa: Reanalysis of a randomized controlled trial
- Serelaxin as a potential treatment for renal dysfunction in cirrhosis: Preclinical evaluation and results of a randomized phase 2 trial
- Refining Lung Cancer Screening Criteria in the Era of Value-Based Medicine
- Renewing ’s editorial board in times of global distraction
- Hope for HIV control in southern Africa: The continued quest for a vaccine
- The potential benefit of scaling up malaria prevention to reduce low birth weight in Africa
- PLOS Medicine
- Archiv čísel
- Aktuální číslo
- Informace o časopisu
Nejčtenější v tomto čísle- Precision oncology: Charting a path forward to broader deployment of genomic profiling
- Taxes and Subsidies for Improving Diet and Population Health in Australia: A Cost-Effectiveness Modelling Study
- Refining Lung Cancer Screening Criteria in the Era of Value-Based Medicine
- Renewing ’s editorial board in times of global distraction
Kurzy
Zvyšte si kvalifikaci online z pohodlí domova
Současné možnosti léčby obezity
nový kurzAutoři: MUDr. Martin Hrubý
Všechny kurzyPřihlášení#ADS_BOTTOM_SCRIPTS#Zapomenuté hesloZadejte e-mailovou adresu, se kterou jste vytvářel(a) účet, budou Vám na ni zaslány informace k nastavení nového hesla.
- Vzdělávání



