-
Články
Top novinky
Reklama- Vzdělávání
- Časopisy
Top články
Nové číslo
- Témata
Top novinky
Reklama- Videa
- Podcasty
Nové podcasty
Reklama- Kariéra
Doporučené pozice
Reklama- Praxe
Top novinky
ReklamaA Novel Brief Therapy for Patients Who Attempt Suicide: A 24-months Follow-Up Randomized Controlled Study of the Attempted Suicide Short Intervention Program (ASSIP)
In a randomized controlled trial, Konrad Michel and colleagues test the efficacy of a manual-based therapy intended to prevent repeat suicide attempts.
Published in the journal: . PLoS Med 13(3): e32767. doi:10.1371/journal.pmed.1001968
Category: Research Article
doi: https://doi.org/10.1371/journal.pmed.1001968Summary
In a randomized controlled trial, Konrad Michel and colleagues test the efficacy of a manual-based therapy intended to prevent repeat suicide attempts.
Introduction
The high toll of deaths by suicide is a major global public health problem [1]. In spite of a broad range of prevention efforts, suicide rates have not declined [2]. Rates in the US have increased in recent years [3], and the number of suicide attempts in adults has been estimated to be about 1.3 million per year [4]. Individuals with a history of attempted suicide have rightly been identified as a main target group for clinical suicide prevention [5]. A recent meta-analysis reported a 1-year rate of hospital admissions due to repeat attempts of 17%, with a rate of self-reported reattempts of 21.9% [6]. The risk of completed suicide for individuals who have previously attempted suicide is from 40 to over a 100 times higher than that of the general population [7,8]. The risk increases with each subsequent suicide attempt, and remains high for more than 30 years [9]. However, there is a lack of interventions demonstrating a long-term reduction of suicidal behavior [10,11]. Exceptions are the treatment studies by Fleischmann et al. [12], Brown et al. [11], and, most recently, Rudd et al. [13] reporting significant risk reductions over 18, and 24 months. The Fleischmann et al. study was a multicenter study in which 1,867 individuals who had attempted suicide were offered a brief psychoeducative session combined with long-term contact with phone calls or visits over a period of 18 months. The intervention group had significantly fewer deaths from suicide than the group with usual treatment. In the Brown et al. study, which included 120 participants who had attempted suicide, the intervention group received at least ten (up to 24) sessions of cognitive therapy with an emphasis on developing safety plans for future suicidal crises. Case managers ensured treatment adherence of “no show” patients and compliance to ongoing psychiatric treatment. The cognitive therapy group had a significantly lower reattempt rate and a 50% reduced risk of reattempting suicide during 18 months of follow-up. In their study with 152 active-duty soldiers, Rudd and co-workers found that a brief cognitive-behavioral therapy with 12 to 16 or more sessions plus usual mental health care (including case managers) was associated with a 60% lower risk of attempting suicide during 24 months of follow-up. Other studies have found that minimal outreach interventions after attempted suicide, such as contacting patients with regular postcards or standardized letters, are associated with a reduction of suicides [14–16], although findings have not been consistent [17,18]. Considering the limited resources available for the provision of adequate treatment for patients who attempt suicide, there is a clear need for brief, focused, and effective treatments [19].
A major barrier to effective treatment is poor treatment compliance, with 50% or more of patients failing to attend or withdrawing from follow-up treatment within 1 week [20,21]. One reason for this may be that suicidal patients often feel misunderstood by health professionals [22]. According to the traditional medical model, clinicians tend to see suicide as a symptom of mental disorder, while, for people in a suicidal crisis, the central issue is their very personal experience of pain, anguish, hopelessness, and loss of self-esteem [23]. Although adequate treatment of the psychiatric disorder associated with suicidal behavior is important, exploring the very individual, subjective experience of a suicidal crisis requires a patient-centered, collaborative treatment approach [22]. In line with such an approach is the concept of suicide as goal-directed action [24], in which suicide is seen as a solution to a subjectively unbearable mental state. Central to action theory is the notion that people have the narrative competence to explain their actions, i.e., how they reached the point of harming themselves. We previously reported an association between a narrative interviewing style and therapeutic alliance [25].
Therapeutic alliance is a consistent predictor of outcome across psychotherapies [26]. Based on guidelines for clinicians formulated by an international working group [27], we developed a brief therapy program for patients who have recently attempted suicide, the Attempted Suicide Short Intervention Program (ASSIP). A major focus of ASSIP lies in the development of an early therapeutic alliance, combined with psychoeducation, a cognitive case conceptualization, safety planning, and continued long-term outreach contact.
The primary objective of the study was to evaluate the efficacy of ASSIP plus treatment as usual (TAU) compared to TAU alone in reducing the rate of repeated suicide attempts during 24-month of follow-up. Secondary outcome measures were suicidal ideation, depression, and health-care utilization. Furthermore, we investigated the moderating effect of baseline factors such as therapeutic alliance in the therapy sessions, prior suicide attempts, depression at baseline, and diagnosis on outcome.
Methods
Design
Patients admitted to the emergency unit of the Bern University General Hospital following attempted suicide were seen on a routine basis by the duty psychiatrist, who asked them for their consent to be contacted by the study team. The signed agreement forms were then forwarded to the study team. Patients who fulfilled the inclusion criteria were randomly assigned to the ASSIP or the control group. Simple randomization was carried out using shuffled unmarked sealed envelopes. Similar to a modified Zelen design [28,29], participants were contacted following randomization and informed that they had been allocated to one of the two groups. Participants in the control group were offered a single assessment interview. This was considered necessary for ethical and safety reasons [30]. Written informed consent was obtained from participants of both groups after detailed description of the study. Suicidality was assessed with the Suicide Status Form (SSF-III) [31] at the initial session. Both groups continued TAU. Study therapists did not have any influence on TAU. A set of questionnaires was filled out by participants after the initial session and at 6, 12, 18, and 24 months.
Local regulations did not require registration of the study before patient recruitment started in 2009. In Switzerland, the Federal Act on Research Involving Human Beings, which requires registration in a public registry, was implemented January 1, 2014. Registration at ClinicalTrials.gov was done after completion of the study. We have not conducted and are not currently conducting any related clinical trials. Future trials will be registered prospectively.
The study procedure was approved by the local ethics committee in accordance with the Declaration of Helsinki [32]. The original project description was evaluated by the research ethics committee of the University of Bern (registration number 144/08, Kantonale Ethikkommission Bern). The trial protocol was submitted on October 9, 2008, resubmitted on April 27, 2009, and accepted on May 22, 2009 (S1 Text).
The study was conducted according to the trial protocol, with minor changes made in the course of the study: (1) the total number of participants in the study protocol (80) was later increased to 120 due to a revised power calculation; (2) time intervals of more than 3 months between suicide attempt and first interview were allowed due to the high number of referrals to the study; (3) habitual self-harm as an exclusion criterion was added later for clarification (see the definition of attempted suicide in “Participants”); (4) in response to peer review, reattempt-free survival, hazard ratios, and group differences were calculated based on multiple imputed datasets.
Power Analysis and Sample Size
Power calculations were based on the results of previous randomized controlled trials with a comparable design [33,34]. We estimated an expected repetition risk of 30% in the control group, and 15% in the treatment group. We calculated the required sample size for the comparison of survival curves between two groups under the Cox proportional hazards model for clinical trials [35]. For a desired statistical power of 80% to detect a hazard ratio of 0.44 for time to next suicide attempt between treatment groups, with a two-sided alpha level of 0.05, a total sample size of n = 116 was required.
Participants
All participants included in the study had recently attempted suicide. Attempted suicide was defined according to Silverman et al. [36] as a “self-inflicted, potentially injurious behavior with a nonfatal outcome for which there is evidence (either explicit or implicit) of intent to die.” In German-speaking countries, similar to in North America, self-harm is usually defined as non-suicidal self-injury, different from suicidal behavior with intent to die [37]. We therefore deemed it necessary to explicitly exclude habitual self-harm, which is typically associated with a diagnosis of borderline personality disorder (BPD). Further exclusion criteria were serious cognitive impairment, psychotic disorder, insufficient mastery of the German language, and residency outside the hospital catchment area. Information regarding the circumstances of the suicide attempt was collected from the hospital records. For diagnostic information, we used the hospital diagnoses based on the 10th revision of the International Classification of Diseases [38]. Up to four psychiatric diagnoses per participant were recorded.
ASSIP Treatment Protocol
ASSIP was administered in three 60 - to 90-min sessions, usually on a weekly basis. A fourth session was added if necessary. These face-to-face therapy sessions were supplemented by regular, personalized letters to the participants for 24 months. The manual used throughout the study was first published in German [39] in May 2013; the translation in English [40] followed in June 2015. The manual is highly structured, and interventions for each session are described in detail.
First session
A narrative interview [41] was conducted in which patients were asked to tell their personal stories about how they had reached the point of attempting suicide. The aim of the narrative interview is to reach—in a biographical context—a patient-centered understanding of the individual mechanisms leading to suicidal behavior and to elicit specific vulnerability factors and trigger events. All interviews were video-recorded, with the patients’ written consent. Suicide risk was assessed using the SSF-III [31].
Second session
Patient and therapist, seated side-by-side, watched sequences of the video-recorded first session. The aim of the video playback [42] is to reactivate the patient’s mental state during the suicidal crisis, in a safe environment, and provide a detailed reconstruction of the transition from an experience of psychological pain and stress to the suicidal action. Automatic thoughts, emotions, physiological changes, and contingent behavior were identified. Patients received a psychoeducative handout (“Suicide Is Not a Rational Act”) as a homework task (S2 Text), to be returned with personal comments at the next session. Following the session, the therapist prepared a written draft of the case conceptualization.
Third session
The patients’ comments to the handout were discussed. The case conceptualization was revised collaboratively. A list of long-term goals, individual warning signs, and safety strategies was developed in close cooperation with the patient. The written case conceptualization and the personal safety strategies were printed out and given to the patient, with additional copies for other health professionals involved in treatment. Long-term goals, warning signs, and safety strategies were copied to a credit-card-size folded leaflet and given to the patient. In addition, participants received a crisis card with a list of telephone numbers of private and professional helpers who could be contacted in case of a suicidal crisis. Patients were instructed to carry both with them at all times, and to use them in the event of a crisis.
Letters
Participants were sent semi-standardized letters over a period of 24 months, every 3 months in the first year and every 6 months in the second year. The letters reminded participants of the long-term risk of future suicidal crises and the importance of the safety strategies. Letters were signed personally by the ASSIP therapist. Usually, one or two personal sentences were added, and participants were invited to give feedback about how things were going.
For further details see ASSIP manual [40].
Control Group
Participants assigned to the control group underwent a single clinical interview, which included a structured suicide risk assessment using the SSF-III. A written summary of the risk assessment was sent to the health professionals responsible for the participant’s usual clinical care.
ASSIP Therapists
ASSIP was provided by four therapists: two clinicians experienced in clinical suicide prevention (K. M., psychiatrist, and A. G.-M., psychologist) and two therapists (M. M. and S. Bühler, both psychologists) with an average of 2 years in clinical practice, who were introduced to ASSIP and the study procedures during a 1-week training. Adherence to the highly structured treatment manual, which provides clear tasks for each session, was ensured by regular peer reviews and supervision using the video-recorded interviews.
Treatment as Usual
Information on the co-active treatment was based on patient’s self-reports in the set of questionnaires completed every 6 months. In both groups, TAU included inpatient, day patient, and individual outpatient care as considered necessary by the clinicians in charge of patient management. Some patients changed from inpatient to outpatient status during ASSIP sessions. Thirty-eight (63%) participants in the ASSIP group and 32 (53%) in the control group were on psychotropic drugs at the time of the initial interview.
Measures
The set of questionnaires was completed by the study participants at the conclusion of the initial session, and identical questionnaires were sent to both groups every 6 months over a period of 2 years.
Personal and sociodemographic characteristics
A 33-item questionnaire was developed to collect sociodemographic and health-related data, including information on suicidal behavior. The questions related to suicidal behavior and self-harm were as follows: (1) “Did you in the past 6 months try to take your own life?”; (2) “How often did you in the past 6 months have thoughts about taking your own life?”; and (3) “How often did you in the past 6 months physically harm yourself (e.g., cutting, burning, hitting)?”. According to the definition of attempted suicide used in this study, physical self-harm during follow-up was not recorded as a suicide attempt. In order to complete outcome data at the end of the follow-up period, we searched hospital records and contacted the responsible general practitioners and therapists to check for suicide attempts and completed suicide.
Penn Helping Alliance Questionnaire
The 11-item self-rating Penn Helping Alliance Questionnaire (HAq) [43] was used to evaluate the quality of the patient–therapist relationship (therapeutic alliance). The HAq has demonstrated good validity for psychotherapy outcomes [44]. The German version [45] was used.
Beck Depression Inventory
The 21-item Beck Depression Inventory (BDI) was used to measure the severity of depression [46,47].
Beck Scale for Suicide Ideation
The Beck Scale for Suicide Ideation (BSS)—a 21-item self-report instrument measuring the intensity of the patients’ attitudes, behaviors, and plans related to suicidal behavior [48,49]—was used.
Statistical Analysis
Analysis was conducted on the intention-to-treat (ITT) population to ensure unbiased comparisons between the two groups and to address concerns regarding withdrawal and noncompliance. To address the issue of missing data, multiple imputations by chained equations were implemented. Estimates of 20 imputed datasets were combined using Rubin’s rule; the mean and 95% CI of the test statistics and p-values are reported. We calculated standard errors and CIs for the Cox hazards coefficients based on the square root of the within-individual variance of the individual imputed datasets and the between-individual variance across the multiple imputed datasets. We found no differences between analyses conducted with the original and the imputed dataset. In the survival analysis, binary events were used (0 = no suicide attempt in the follow-up; 1 = one or more suicide attempts in the follow-up). A p-value less than 0.05 was considered statistically significant, and all tests were two-sided. Survival analyses of participants who made a repeat suicide attempt at least once during the follow-up period were conducted using the Kaplan-Meier estimator [50]. Log-rank tests (Mantel-Haenszel test) were performed to calculate survival curve differences between the two groups, and associated Wald χ2 tests were conducted to test the null hypothesis of no difference between treatments at any assessment time point. A Cox proportional hazards regression model [51] for discrete data using “exact partial likelihoods” was used to determine hazard ratios for the two groups. Demographic data and secondary outcome measures were analyzed using nonparametric methods (χ2 tests, Mann-Whitney U test) in the case of count variables (e.g., days of hospitalization, number of suicide attempts) or where data were not normally distributed. BSS and BDI scores were analyzed using ANCOVA. As a sensitivity analysis and to account for potentially autoregressive relationships among scores, we also fitted mixed effects regression models.
All analyses were performed using the SPSS 18.0 software package and R (version 3.2.1; http://www.r-project.org) with the packages “survival” (v. 2.38) and “mice” (v. 2.22).
Data are deposited in the Dryad Digital Repository: http://dx.doi.org/10.5061/dryad.85nf3 [52].
Results
Enrollment Statistics
Between June 2009 and December 2012, 291 individuals were referred to the study (see Fig 1); 98 (34%) did not meet the inclusion criteria, and 73 (25%) refused to participate in the study. The most frequent reasons for exclusion were language problems and psychotic disorders. Of those who refused to participate, several denied having had suicidal intention and others refused any kind of treatment or gave circumstantial reasons, such as work commitments and lack of child care, for not being able to attend treatment sessions. Ultimately, 120 patients were randomly assigned to the study groups.
Fig. 1. Study flow chart. 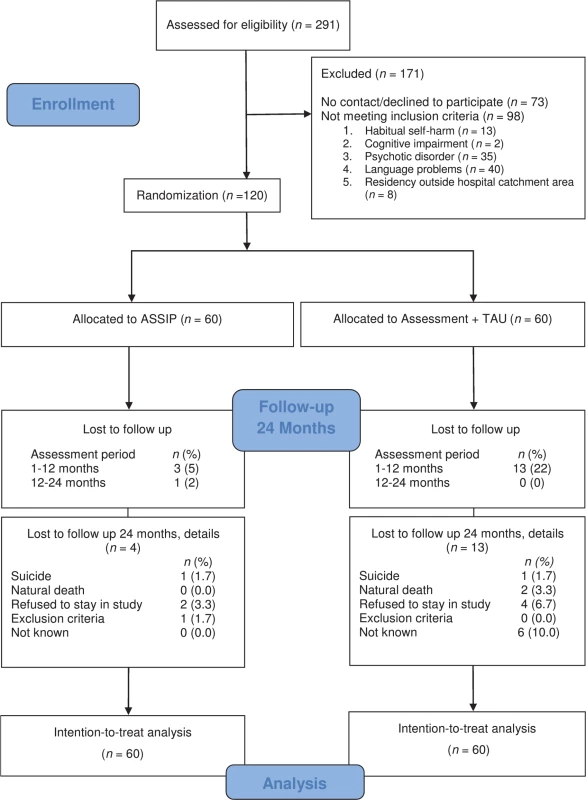
Flow chart of participants in the randomized controlled trial. Participant Characteristics
Fifty-four (45%) male (mean age 40 years, SD = 14) and sixty-six (55%) female (mean age 36 years, SD = 14) participants entered the study (see Table 1). Sixty-three percent were diagnosed with affective disorder, 44% with neurotic and stress-related disorder, and 25% with substance abuse disorder (see Table 1). Prior suicide attempts were reported by 50%; 26% had a history of multiple (two or more) prior suicide attempts. Intentional overdosing was the most frequent method used (68%), followed by cutting (13%), jumping (7%), and hanging, shooting, and drowning (10%). Treatment and control groups did not differ in demographic or clinical variables, with the exception of the number of outpatient sessions prior to the index suicide attempt.
Tab. 1. Baseline demographic and clinical characteristics of study participants. 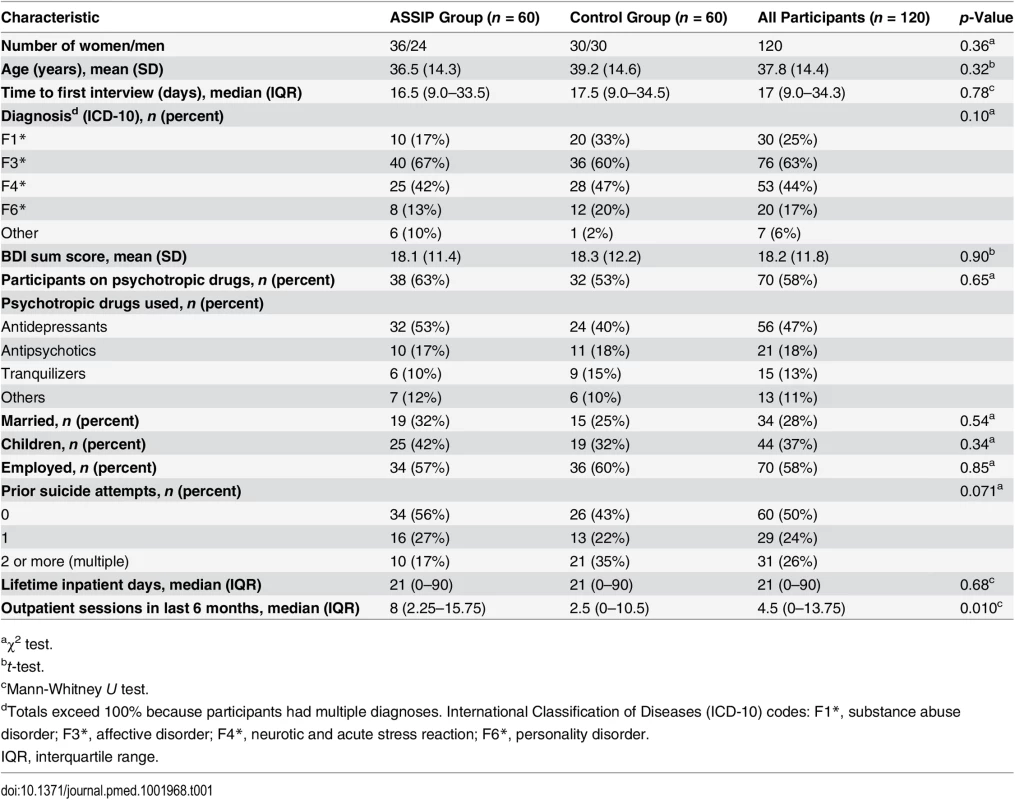
aχ2 test. Attrition Rates and Missing Data
The dropout rates for the ASSIP and control groups were 5% (n = 3) and 22% (n = 13) at 12 months, and 7% (n = 4) and 22% (n = 13) at 24 months, respectively. Reasons for withdrawal from the study were, e.g., refusal to cooperate because of change of ASSIP therapist during follow-up, or, in the control group, seeing “too little profit.” In each group, one death by suicide was recorded: one participant in the ASSIP group died by suicide in an acutely psychotic state, and one participant in the control group died by suicide while in hospital care. Three natural deaths occurred in the control group. The number of missed assessments (questionnaires) did not significantly differ between groups (χ23 = 7.08, p = 0.07), with the largest difference in missed assessments observed at 24 months (ASSIP group: 10%; control group: 37%).
Primary Outcome Measures
Repeated suicide attempts
During the 24-month follow-up period, five reattempts were recorded in the ASSIP group, and 41 reattempts in the control group (see Table 2). The rates of participants reattempting suicide at least once were 8.3% (n = 5) and 26.7% (n = 16), respectively (ITT analysis). Using the Kaplan-Meier estimator with multiple imputations, the estimated mean suicide-attempt-free survival rate at 12 months was 0.99 (95% CI 0.98–1.00) in the ASSIP group and 0.93 (95% CI 0.89–0.96) in the control group (Fig 2; Table 3). At 24 months, the mean rates were 0.95 (95% CI 0.90–1.00) and 0.79 (95% CI 0.71–0.87), respectively. The group difference in number of participants reattempting suicide was significant (log-rank/Mantel-Haenszel test, mean χ21 = 16.5, 95% CI 15.4–17.6; mean p < 0.001). The mean hazard ratio was 0.17 (95% CI 0.07–0.46), indicating that the ASSIP group had an 83% reduced risk of attempting suicide during the 24-month follow-up period compared to the control group (Wald χ21 = 13.1, 95% CI 12.4–13.7, p < 0.001).
Fig. 2. Survival curves. 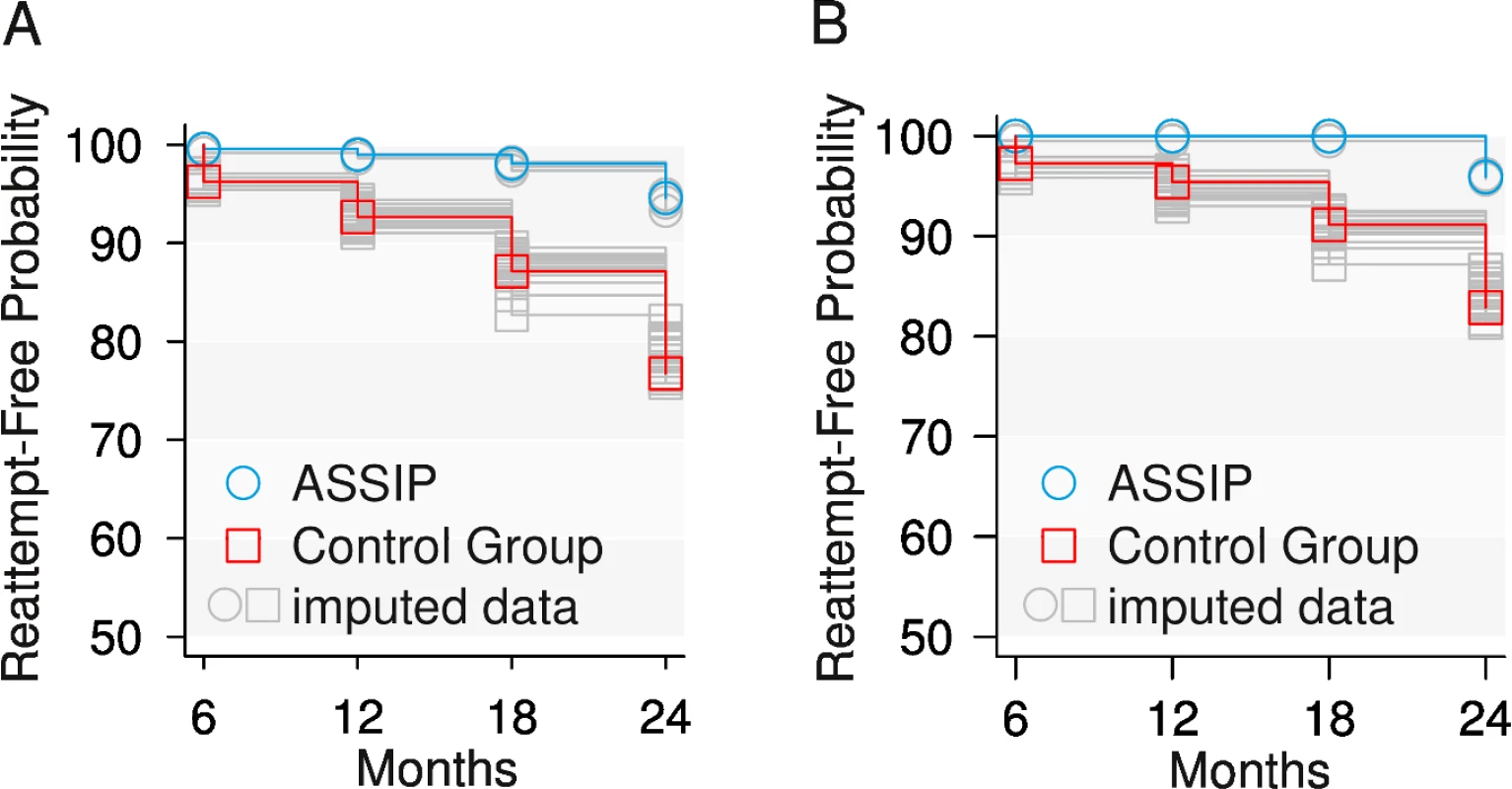
Suicide-attempt-free survival of participants who attempted suicide at least once during the 24-month follow-up period. (A) All participants (n = 120). (B) Participants without BPD (n = 100). Tab. 2. Repeated suicide attempts during 24-month follow up: ITT analysis (n = 120). 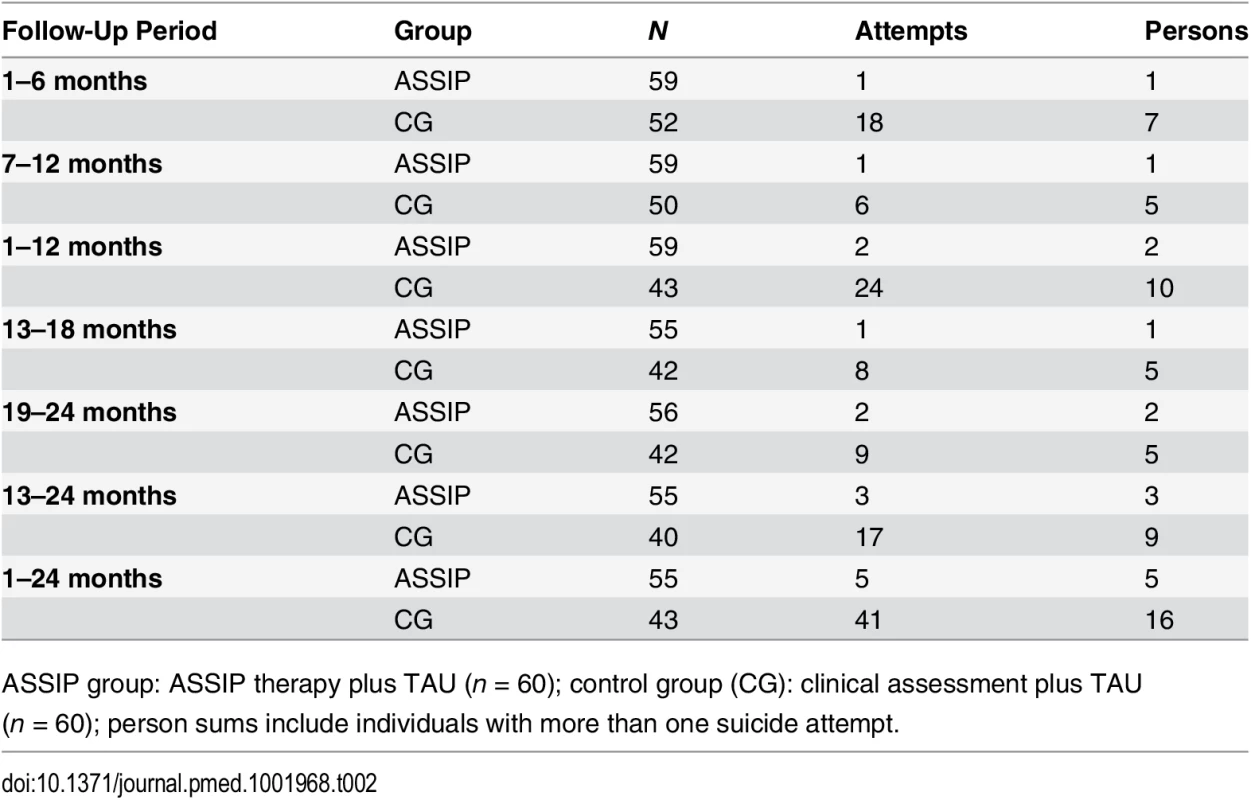
ASSIP group: ASSIP therapy plus TAU (n = 60); control group (CG): clinical assessment plus TAU (n = 60); person sums include individuals with more than one suicide attempt. Tab. 3. Estimated reattempt-free survival probability during 24-month follow-up. 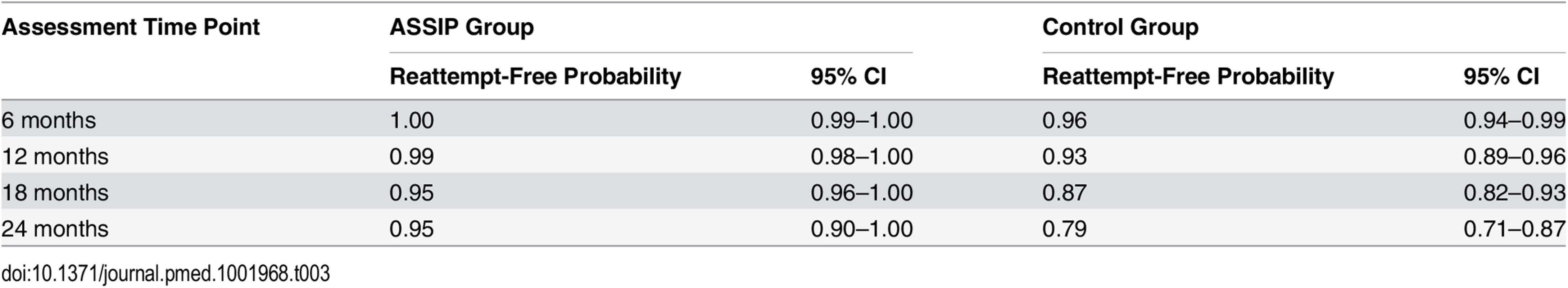
We used a multivariable Cox proportional hazards model to investigate the effect of four baseline covariates on outcome: BDI sum score, previous suicide attempts, diagnosis (substance abuse disorder, affective disorder, neurotic and acute stress reaction, personality disorder), and recent outpatient treatment (number of sessions in the past 6 months). This model revealed a hazard ratio for suicide reattempt for the ASSIP group of 0.15 (95% CI 0.05–0.44, p < 0.001) compared to the control group. For the BDI sum score and the diagnosis of personality disorders the hazard ratios were 0.96 (95% CI 0.93–0.99, p = 0.016) and 0.39 (95% CI 0.17–0.89, p = 0.022), respectively. Prior suicide attempts, a diagnosis of substance abuse, and number of outpatient sessions did not contribute to the model. The overall model showed a significant group difference (Wald χ28 = 31.9, 95% CI 30.3–33.4, p < 0.001). ASSIP was associated with an 85% reduced risk of participants making at least one repeat suicide attempt. A diagnosis of personality disorder was associated with a 61% higher risk of reattempting suicide, while the BDI sum score increased the risk by 4% per unit.
Furthermore, we tested the effect of a history of multiple suicide attempts on outcome by including “two or more prior attempts” as a covariate. The treatment effect remains, with a hazard ratio of 0.22 (95% CI 0.08–0.61), indicating a 78% reduction of risk due to ASSIP. The overall model is significant (Wald χ22 = 23.5, 95% CI 22.4–24.6, p < 0.001).
Participants with a diagnosis of BPD had more previous suicide attempts (median = 2, interquartile range [IQR] = 1–2.25) than other participants (median = 0, IQR = 0–1, W = 1,450, p < 0.001). We therefore separated the 20 participants with BPD from the total sample for additional analysis. For the 100 remaining participants, suicide-attempt-free survival at 24-month was 0.96 (95% CI 0.91–1.00) for the ASSIP group and 0.84 (95% CI 0.76–0.93) for the control group (see Fig 2). The therapy effect was significant (χ21 = 12.7, 95% CI 11.8–13.5, p < 0.001), with a mean hazard ratio of 0.11 (95% CI 0.03–0.49), indicating that when individuals with BPD were excluded, the ASSIP group had a 89% lower risk of attempting suicide during the 24-month follow-up period than the control group (Wald χ21 = 8.7, 95% CI 8.3–9.1, p = 0.004).
We additionally tested the sensitivity of the treatment effect. In our model, we predicted the primary outcome, one or more suicide reattempts, by treatment and by previous suicide attempts using a logistic regression. We found a significant effect of treatment (coefficient = 1.66, 95% CI 0.58–2.88, p = 0.004), while the effect of previous suicide attempts was not significant (coefficient = 0.20, 95% CI −0.02 to 0.44, p = 0.08). This finding is consistent across all imputed datasets (therapy effect, mean p = 0.004, 95% CI 0.003–0.006; previous suicide attempts, mean p = 0.10, 95% CI 0.07–0.12).
Secondary Outcome Measures
Suicide ideation
Differences in suicide ideation (BSS) during the four follow-up measurements were investigated using a mixed-model ANCOVA on the imputed data. We found a significant reduction in suicide ideation over time (F3,354 = 8.83, p < 0.001; 24-month coefficient: −0.12, 95% CI −0.20 to −0.05), but no group effect (F1,114 = 0.69, p = 0.41). No interaction of group × time was found (F3,354 = 1.0, p = 0.40). Because of differences in diagnoses and number of previous suicide attempts (Table 1), these variables were included as covariates in the ANCOVA, revealing a significant effect of prior suicide attempts (F1,114 = 17.0, p < 0.001; coefficient: 0.05, 95% CI 0.02–0.07) and diagnoses (F1,114 = 12.8, p < 0.001) on BSS scores. Prior suicide attempts correlated positively with BSS scores (Spearman’s rho = 0.27, p < 0.001), indicating more suicide ideation in this patient group. These results were supported by using a linear mixed model. We found a significant effect over time (at 18 months: coefficient = −0.07, 95% CI −0.13 to −0.02, t357 = −2.55, p = 0.011; at 24 months: coefficient = −0.14, 95% CI −0.20 to −0.09, t357 = −5.03, p < 0.001), but no group effect (coefficient = −0.02, t114 = −0.52, p = 0.60). Three diagnoses (affective disorder: coefficient = −0.19, 95% CI −0.32 to −0.07, t114 = −3.01, p = 0.003; substance abuse disorder: coefficient = −0.23, 95% CI −0.41 to −0.05, t114 = −2.48, p = 0.014; neurotic and acute stress reaction: coefficient = −0.38, 95% CI −0.52 to −0.23, t114 = −5.18, p < 0.001) and prior suicide attempts (coefficient = 0.05, 95% CI 0.02–0.07, t114 = 4.12, p < 0.001) were significantly associated with BSS scores.
Health-care utilization
In the first 12 months, 16 participants (27%) in the ASSIP group and 20 participants (33%) in the control group were admitted to psychiatric inpatient treatment. ASSIP participants had 72% fewer days of inpatient care (median = 29, IQR = 7–68) than control participants (median = 105, IQR = 39–158, W = 94.5, p = 0.038). At 24 months, 18 (30%) ASSIP participants and 23 (38%) control participants had been admitted to hospital. ASSIP was associated with 63% fewer days of hospitalization (median = 33, IQR = 11–65) than control treatment (median = 90, IQR = 23–180), but the difference at 24 months did not reach significance (W = 139.5, p = 0.08). The groups did not differ with respect to the total number of outpatient sessions at 12 months (W = 1,392.5, p = 0.41) and 24 months (W = 1,487.5, p = 0.57).
Depression
Although ASSIP was not expected to have an effect on depression, we analyzed the BDI scores during follow-up using a mixed-model ANCOVA on the imputed data. Similar to the results for the BSS, we found a significant reduction over time (F3,354 = 18.9, p < 0.001), but no group effect (F1,114 = 1.99, p = 0.16). The covariates previous suicide attempts (F1,114 = 8.5, p = 0.004) and diagnoses (F1,114 = 20.5, p < 0.001) had a significant effect on BDI scores; a diagnosis of personality disorder was associated with higher BDI scores. These results were supported by using a linear mixed model. We found a significant effect over time (at 12 months: coefficient = −2.25, 95% CI −3.79 to −0.72, t357 = −2.89, p = 0.004; at 18 months: coefficient = −2.35, 95% CI −3.89 to −0.82, t357 = −3.02, p = 0.003; at 24 months: coefficient = −5.79, 95% CI −7.33 to −4.26, t357 = −7.44, p < 0.001), but no group effect (coefficient = 0.10, t114 = 0.08, p = 0.94). Three main diagnoses (affective disorder: coefficient = −9.76, 95% CI −13.2 to −6.34, t114 = −5.65, p < 0.001; substance abuse disorder: coefficient = −10.5, 95% CI −15.4 to −5.46, t114 = −4.15, p < 0.001; neurotic and acute stress reaction: coefficient = −13.5, 95% CI −17.4 to −9.52, t114 = −5.18, p < 0.001) and prior suicide attempts (coefficient = 0.90, 95% CI 0.29–1.51, t114 = 2.92, p = 0.004) were significantly associated with BDI scores.
Therapeutic Alliance as Moderating Factor
In the ASSIP group, a linear model demonstrated that therapeutic alliance (HAq score) at the first ASSIP session was inversely related to BSS score at 12 months follow-up (t57 = −3.02, p = 0.004; coefficient: −0.26, 95% CI −0.43 to −0.09, R2 = 0.18) and 24 months (t57 = −3.11, p = 0.003; coefficient: −0.21, 95% CI −0.35 to −0.08, R2 = 0.30); the relationship between HAq scores at the third ASSIP session and BSS scores was not significant. Furthermore, the ASSIP group showed a significant increase in therapeutic alliance from the first to the third session (HAq at first session, median = 4.91, IQR = 4.3–5.2; HAq at third session, median = 5.32, IQR = 4.9–5.6, W = 257.5, p < 0.001, paired test).
Discussion
This randomized controlled trial evaluated the efficacy of ASSIP, a novel brief therapy for individuals who have attempted suicide administered in addition to TAU. The ASSIP group had a 18.4% lower rate of participants making at least one repeat suicide attempt compared to the control group at 24 months, indicating a 83% reduction of the risk of further suicide attempts in the survival analysis. It has been estimated that interventions that reduce suicide attempts by 25% may lead to a 2.6% reduction in the suicide rate, resulting in approximately 1,000 lives saved annually in the US [53]. Emergency department visits and inpatient hospitalizations due to suicidal ideation and suicide attempts have been estimated to result in over 1 million hospital visits per year, leading to costs of US$4.7 billion [1,54]. ASSIP fulfills the demands for a low-cost intervention [55]. Considering the generally limited treatment resources for this patient group, we believe that ASSIP may have a considerable potential for reducing suicidal behavior, increasing treatment provision for patients attempting suicide, and reducing health-care costs. Large pragmatic trials will be needed to conclusively establish the efficacy of ASSIP and replicate our findings in other clinical settings.
A strength of the study is that the intervention was based on a published manual. The treatment protocol is highly structured and, in our experience, easy to understand for therapists as well as for patients. In Finland, ASSIP is currently being used in an increasing number of crisis centers [56]. Thus, we believe that ASSIP can be easily applied in other treatment settings. The study has high external validity due to its real-world setting. Similar to clinical practice, patients seen in the emergency department were informed that referral to ASSIP was part of the routine procedure following attempted suicide. Patients at high risk of suicide were seen for a first interview as soon as they were considered safe for escorted transport to the study premises at the outpatient department. The proportion of participants with a history of one or more prior suicide attempts at baseline was relatively high (50%); other studies report a range of 13% to 24% [57]. This indicates that our sample had a relatively high proportion of individuals with increased suicide risk.
Remarkably, the treatment group spent less time in the hospital during the follow-up period. This may be for two reasons. First, patients in the ASSIP group were often discharged from inpatient care earlier, presumably because the clinicians relied on ASSIP as an effective add-on treatment. Second, the low number of days spent in the hospital by the treatment group probably reflects the reduction of suicide attempts during follow-up.
The treatment effect on suicidal behavior was not reflected in the BSS, measuring primarily suicidal ideation. This finding is consistent with the main objective of ASSIP, which is to implement safety strategies targeting suicidal behavior, and not to reduce suicidality. As part of the therapy interventions, participants were informed that suicidal crises could again be triggered at any time in the future. Furthermore, the results are in line with other studies [11] that found no significant effect of cognitive-behavioral therapy on suicide ideation.
ASSIP is informed by multiple theories and models. But what makes it effective? First, we believe that it is important for patients to know that the goals of the therapy are limited. Patients were informed that they had an increased risk of future suicidal crises and that the therapy would not cure them from suicidality. The declared aim of the therapy was for patients to understand what makes them suicidal, and to develop safety strategies in case of future suicidal crises. The psychoeducative handout is consistent with this aim, promoting the concept of the suicidal mode as an out-of-the-ordinary state of mind that can be triggered at any time by specific adverse experiences [58], and stating that the safety strategies must be applied before the suicidal mode is fully activated. Second, we believe that ASSIP’s patient-centered, collaborative approach to suicidal behavior promotes therapeutic alliance and maximizes treatment engagement, a central element of ASSIP. This is supported by the association of therapeutic alliance measures with outcome and the increase in the scores of therapeutic alliance (HAq) in the ASSIP group between session one and session three. The latter is consistent with results from psychotherapy research, which suggest that ratings of alliance in the third therapy session are a good predictor of adherence to treatment and outcome [59]. Key elements of ASSIP are designed to promote “the active and purposeful collaboration between patient and therapist” [60] and include narrative interviewing [25] and video playback [42], both novel concepts in the treatment of suicidal individuals. Third, ASSIP incorporates established therapeutic concepts, such as safety planning [61] and follow-up contact with regular, personalized letters [14,16]. To our knowledge, so far, no published treatment studies have combined psychological interventions with subsequent ongoing contact through letters. We assume that the regular letters not only provided a feeling of connectedness with the ASSIP therapist, but also may have acted as reminders of patients’ increased suicide risk and may have increased awareness of problems that could trigger future suicidal crises.
There are a number of limitations to be considered. First of all, it has to be taken into account that small trials may result in large effect sizes. Therefore, larger studies will be needed to determine the evidence for the efficacy of ASSIP in reducing suicidal behavior. A problem of treatment studies with long-term follow-up is dropouts and missing data. The cumulative dropout rates increased during follow-up, with higher rates in the control group. This is a well-known phenomenon [54], which was dealt with by ITT analysis, as recommended in the CONSORT guidelines for reporting randomized controlled trial results [55]. The problem of missing data was addressed by using multiple imputations. Multiple imputations reduce bias attributable to missing outcome data and resulted in our study in a more conservative treatment effect compared to the original data.
The groups differed in a few clinical baseline variables, although these differences were not statistically significant, except for the number of outpatient sessions prior to study inclusion. An analysis using a multivariate Cox proportional hazards model with these baseline variables as covariates had no significant influence on the treatment effect: risk reduction for the ASSIP group remained above 80%. The proportion of participants with a history with two or more prior attempts was higher in the control group. However, using “two or more prior attempts” as a covariate did not significantly reduce the treatment effect of ASSIP relative to control treatment.
Information on repeated suicidal behavior was primarily based on participants’ self-reports in the questionnaires. Others [6,33] have reported on the problem of under - and over-reporting in patients’ self-reports of suicidal behavior, and the discrepancy between self-reports and hospital-based data. We dealt with this problem by complementing self-reported data with searching medical records and contacting health professionals involved in TAU.
Data on co-active treatment consisted of self-reports every 6 months on the setting and the duration of TAU. We did not collect information on the nature of the co-active follow-up treatment. Generally, the provision of psychiatric in - and outpatient treatment in the region of Bern can be considered to fulfill high standards of clinical care. The health-care system is a mixture of state and private funding, with mandatory health insurance. Psychiatric outpatient treatment is easily available, with a heavy emphasis on psychotherapy, and with no restrictions on duration. This suggests that the treatment effect cannot be attributed to insufficient co-active treatment.
“Contamination” of ASSIP and control group could not be avoided. Others [62] have commented on the difficulty therapists experience in keeping control and experimental groups “pure.” In our study, initial assessment interviews with the control group were conducted by the therapists who also delivered ASSIP. In practice, the interviews with the control group often included narrative elements. Furthermore, ongoing personal contact with the control group was maintained through the study questionnaires sent to participants with a personally signed letter. In addition, some control participants contacted the therapist for help during the follow-up period. This kind of contamination most likely had the effect of reducing group differences in the primary and secondary outcome measures.
Comparison with Other Studies and Implications
With three therapy sessions, ASSIP is considerably shorter than any other specific treatments for individuals who have attempted suicide [11,13,33,63,64]. An exception is the treatment in the Fleischmann et al. study [12], in which individuals who had attempted suicide were offered a single psychoeducative session, supplemented by regular outreach contact after discharge. Other effective therapy protocols [11,13] have included elements of active outreach contact (phone calls, home visits). It has been pointed out that outreach elements providing a “lifeline,” ideally based on a therapeutic relationship, may be important for the reduction of suicide risk [65]. In line with this, ASSIP combines face-to-face sessions with regular personalized letters during follow-up. The results support the notion that psychological interventions combined with regular outreach elements may be particularly effective in reducing the risk of further suicidal behavior. Furthermore, the present study suggests that a therapeutic relationship can be established in a brief psychological intervention. The finding that the HAq scores of the first ASSIP session were associated with less suicidal ideation during follow-up suggests that a narrative interview technique may be an important element for establishing an early therapeutic alliance. Other interventions in ASSIP such as cognitive case conceptualization based on a vulnerability–trigger model, psychoeducation, and collaboratively developed crisis response plans are elements used in cognitive-behavioral therapy treatment protocols. A relapse prevention task [38,66] was added to the ASSIP manual as an optional session after completion of the study, and was thus not administered in the present study.
A shortcoming of current therapies is that, to our knowledge, none of the randomized controlled treatment studies so far have been replicated. The probability that a treatment will be implemented and evaluated in other clinical settings will be higher when the therapy protocol is simple and highly structured. We believe that ASSIP fulfills these requirements.
Conclusions
ASSIP, a manual-based brief therapy for patients who have attempted suicide, administered in a real-world clinical setting, was efficacious in reducing suicidal behavior over 24 months. ASSIP thus fulfills the need for a brief, easy-to-implement, and low-cost intervention. We believe that ASSIP has the potential for dissemination in various treatment settings and for reducing of the costs of health care for patients attempting suicide. Large pragmatic trials will be needed to conclusively establish the efficacy of ASSIP and to replicate our findings in other clinical settings.
Supporting Information
Zdroje
1. Hoyert DL, Kung H - C, Smith BL. Deaths: preliminary data for 2003. Natl Vital Stat Rep. 2005;53 : 1–48.
2. Centers for Disease Control and Prevention. Suicide among adults aged 35–64 years United States, 1999–2010. MMWR Morb Mortal Wkly Rep. 2013;62 : 321–325. 23636024
3. Drapeau CW, McIntosh JL. U.S.A. suicide: 2013 official final data. Washington (District of Columbia): American Association of Suicidology; 2015.
4. Substance Abuse and Mental Health Services Administration. The NSDUH report: substance use and mental health estimates from the 2013 national survey on drug use and health—overview of findings. Rockville (Maryland): Substance Abuse and Mental Health Services Administration; 2014.
5. National Action Alliance for Suicide Prevention. A prioritized research agenda: an action plan to save lives. Rockville (Maryland): National Institute of Mental Health and Research Prioritization Task Force; 2014.
6. Carroll R, Metcalfe C, Gunnell D. Hospital presenting self-harm and risk of fatal and non-fatal repetition: systematic review and meta-analysis. PLoS ONE. 2014;9:e89944. doi: 10.1371/journal.pone.0089944 24587141
7. Hawton K, Zahl D, Weatherall R. Suicide following deliberate self-harm: long-term follow-up of patients who presented to a general hospital. Br J Psychiatry. 2003;182 : 537–542. 12777346
8. Runeson BS. Suicide after parasuicide. BMJ. 2002;325 : 1125–1126.
9. Haw C, Bergen H, Casey D, Hawton K. Repetition of deliberate self‐harm: a study of the characteristics and subsequent deaths in patients presenting to a general hospital according to extent of repetition. Suicide Life Threat Behav. 2007;37 : 379–396. 17896879
10. Beautrais AL. Intervening to prevent suicide. Lancet Psychiatry. 2014;1 : 165–166. doi: 10.1016/S2215-0366(14)70304-9 26360713
11. Brown GK, Ten Have T, Henriques GR, Xie SX, Hollander JE, Beck AT. Cognitive therapy for the prevention of suicide attempts: a randomized controlled trial. JAMA. 2005;294 : 563–570. 16077050
12. Fleischmann A, Bertolote JM, Wasserman D, De Leo D, Bolhari J, Botega NJ, et al. Effectiveness of brief intervention and contact for suicide attempters: a randomized controlled trial in five countries. Bull World Health Organ. 2008;86 : 703–709. 18797646
13. Rudd MD, Bryan CJ, Wertenberger EG, Peterson AL, Young-McCaughan S, Mintz J, et al. Brief cognitive-behavioral therapy effects on post-treatment suicide attempts in a military sample: results of a randomized clinical trial with 2-year follow-up. Am J Psychiatry. 2015 : 172 : 441–449. doi: 10.1176/appi.ajp.2014.14070843 25677353
14. Motto JA, Bostrom AG. A randomized controlled trial of postcrisis suicide prevention. Psychiatr Serv. 2001;52 : 828–833. 11376235
15. Carter GL, Clover K, Whyte IM, Dawson AH, D’Este C. Postcards from the EDge: 24-month outcomes of a randomised controlled trial for hospital-treated self-poisoning. Br J Psychiatry. 2007;191 : 548–553. doi: 10.1192/bjp.bp.107.038406 18055960
16. Carter GL, Clover K, Whyte IM, Dawson AH, D’Este C. Postcards from the EDge: 5-year outcomes of a randomised controlled trial for hospital-treated self-poisoning. Br J Psychiatry. 2013;202 : 372–380. doi: 10.1192/bjp.bp.112.112664 23520223
17. Beautrais AL, Gibb SJ, Faulkner A, Fergusson DM, Mulder RT. Postcard intervention for repeat self-harm: randomised controlled trial. Br J Psychiatry. 2010;197 : 55–60. doi: 10.1192/bjp.bp.109.075754 20592434
18. Kapur N, Gunnell D, Hawton K, Nadeem S, Khalil S, Longson D, et al. Messages from Manchester: pilot randomised controlled trial following self-harm. Br J Psychiatry. 2013;203 : 73–74. doi: 10.1192/bjp.bp.113.126425 23818535
19. Lizardi D, Stanley B. Treatment engagement: a neglected aspect in the psychiatric care of suicidal patients. Psychiatr Serv. 2010;61 : 1183–1191. doi: 10.1176/appi.ps.61.12.1183 21123401
20. Granboulan V, Roudot-Thoraval F, Lemerle S, Alvin P. Predictive factors of post-discharge follow-up care among adolescent suicide attempters. Acta Psychiatr Scand. 2001;104 : 31–36. 11437747
21. Monti K, Cedereke M, Ojehagen A. Treatment attendance and suicidal behavior 1 month and 3 months after a suicide attempt: a comparison between two samples. Arch Suicide Res. 2003;7 : 167–174.
22. Jobes DA. Collaborating to prevent suicide: a clinical‐research perspective. Suicide Life Threat Behav. 2000;30 : 8–17. 10782715
23. Maltsberger JT. The descent into suicide. Int J Psychoanal. 2004;85 : 653–668. 15228702
24. Michel K, Valach L. Suicide as goal-directed action. Arch Suicide Res. 1997;3 : 213–221.
25. Michel K, Dey P, Stadler K, Valach L. Therapist sensitivity towards emotional life-career issues and the working alliance with suicide attempters. Arch Suicide Res. 2004;8 : 203–213. doi: 10.1080/13811110490436792 16081387
26. Horvath AO, Del Re AC, Flückiger C, Symonds D. Alliance in individual psychotherapy. Psychotherapy. 2011;48 : 9–16. doi: 10.1037/a0022186 21401269
27. Michel K, Maltsberger JT, Jobes DA, Leenaars AA, Orbach I, Stadler K, et al. Discovering the truth in attempted suicide. Am J Psychother. 2002;56 : 424–437. 12400207
28. Hatcher S, Sharon C, Coggan C. Beyond randomized controlled trials in attempted suicide research. Suicide Life Threat Behav. 2009;39 : 396–407. doi: 10.1521/suli.2009.39.4.396 19792981
29. Zelen M. A new design for randomized clinical trials. N Engl J Med. 1979;300 : 1242–1245. doi: 10.1056/NEJM197905313002203 431682
30. Pearson JL, Stanley B, King CA, Fisher CB. Intervention research with persons at high risk for suicidality: safety and ethical considerations. J Clin Psychiatry. 2001;62(Suppl 25):17–26. 11765091
31. Jobes DA. Managing suicidal risk: a collaborative approach. New York: Guilford Press; 2006.
32. Rickham PP. Human experimentation. Code of ethics of the World Medical Association. Declaration of Helsinki. BMJ. 1964;2 : 177. 14150898
33. Morthorst B, Krogh J, Erlangsen A, Alberdi F, Nordentoft M. Effect of assertive outreach after suicide attempt in the AID (assertive intervention for deliberate self harm) trial: randomised controlled trial. BMJ. 2012;345:e4972. doi: 10.1136/bmj.e4972 22915730
34. Hvid M, Wang AG. Preventing repetition of attempted suicide. I. Feasibility (acceptability, adherence, and effectiveness) of a Baerum-model like aftercare. Nord J Psychiatry. 2009;63 : 148–153. doi: 10.1080/08039480802423022 19016074
35. Freedman LS. Tables of the number of patients required in clinical trials using the log-rank test. Stat Med. 1982;1 : 121–129. 7187087
36. Silverman MM, Berman AL, Sanddal ND, O’Carroll P W, Joiner TE. Rebuilding the tower of Babel: a revised nomenclature for the study of suicide and suicidal behaviors. Part 2: suicide-related ideations, communications, and behaviors. Suicide Life Threat Behav. 2007;37 : 264–277. doi: 10.1521/suli.2007.37.3.264 17579539
37. Skegg K. Self-harm. Lancet. 2005;366 : 1471–1483. doi: 10.1016/S0140-6736(05)67600-3 16243093
38. World Health Organization. The ICD-10 classification of mental and behavioral disorders: clinical descriptions and diagnostic guidelines. Geneva: World Health Organization; 2014.
39. Gysin-Maillart A, Michel K. Kurztherapie nach Suizidversuch: ASSIP—Attempted Suicide Short Intervention Program. Bern: Hans Huber; 2013.
40. Michel K, Gysin-Maillart A. ASSIP—Attempted Suicide Short Intervention Program: a manual for clinicians. Göttingen: Hogrefe Publishing; 2015.
41. Michel K, Valach L. The narrative interview with the suicidal patient. In: Michel K, Jobes DA, editors. Building a therapeutic alliance with the suicidal patient. Washington (District of Columbia): American Psychological Association; 2011. pp. 63–80.
42. Young RA, Valach L. The self-confrontation interview in suicide research. Lifenotes. 2002;7 : 12–14.
43. Alexander LB, Luborsky L. The Penn Helping Alliance Scales. In: Greenberg LS, Pinsoff WM, editors. The psychotherapeutic process: a research handbook. New York: Guilford Press; 1986. pp. 325–366.
44. Fenton LR, Cecero JJ, Nich C, Frankforter TL, Carroll KM. Perspective is everything: the predictive validity of six working alliance instruments. J Psychother Pract Res. 2001;10 : 262–268. 11696653
45. Bassler M, Potratz B, Krauthauser H. Der Helping Alliance Questionnaire (HAq) von Luborsky. Möglichkeiten zur Evaluation des therapeutischen Prozesses von stationärer Psychotherapie. Psychotherapeut. 1995;40 : 23–32.
46. Beck AT, Steer RA. BDI, Beck depression inventory: manual. New York: Psychological Corporation; 1987.
47. Hautzinger M, Bailer M, Worall H, Keller F. Beck-depressions-inventar (BDI). Bearbeitung der deutschen Ausgabe. Testhandbuch. Bern: Huber. 1994.
48. Beck AT, Steer RA. Manual for the Beck scale for suicide ideation. San Antonio: Psychological Corporation; 1991.
49. Fidy R. Psychologische Suizidalitäts-Diagnostik im Internet. Zürich: Universität Zürich; 2008.
50. Kaplan EL, Meier P. Nonparametric estimation from incomplete observations. J Am Stat Assoc. 1958;53 : 457–481.
51. Cox DR. Regression models and life-tables. J R Stat Soc Series B Stat Methodol. 1972;34 : 187–220.
52. Gysin-Maillart A, Schwab S, Soravia LM, Megert M, Michel K. Data from: A novel brief therapy for patients who attempt suicide: a 24-month follow-up randomized controlled study of the Attempted Suicide Short Intervention Program (ASSIP). Dryad Digital Repository. Available: http://dx.doi.org/10.5061/dryad.85nf3.
53. Lewis G, Hawton K, Jones P. Strategies for preventing suicide. Br J Psychiatry. 1997;171 : 351–354. 9373424
54. Yang B, Lester D. Recalculating the economic cost of suicide. Death Stud. 2006;31 : 351–361.
55. Oquendo MA, Courtet P. Suicidal behaviour: identifying the best preventive interventions. Lancet Psychiatry. 2015;2 : 5–6. doi: 10.1016/S2215-0366(14)00059-5 26359594
56. Ruishalme O, Narumo R. The implementation of the Swiss ASSIP-Model (Attempted Suicide Short Intervention Program) in Finland [abstract]. 28th World Congress of the International Association for Suicide Prevention; 16–20 Jun 2015; Montreal, Quebec, Canada.
57. Beautrais AL. Suicides and serious suicide attempts: two populations or one? Psychol Med. 2001;31 : 837–845. 11459381
58. Rudd MD. The suicidal mode: a cognitive‐behavioral model of suicidality. Suicide Life Threat Behav. 2000;30 : 18–33. 10782716
59. Saltzman C, Luetgert MJ, Roth CH, Creaser J, Howard L. Formation of a therapeutic relationship: experiences during the initial phase of psychotherapy as predictors of treatment duration and outcome. J Consult Clin Psychol. 1976;44 : 546–555. 939838
60. Gaston L, Thompson L, Gallagher D, Cournoyer L, Gagnon R. Alliance, technique, and their interactions in predicting outcome of behavioural, cognitive, and brief dynamic therapy. Psychother Res. 1998;8 : 190–209.
61. Stanley B, Brown GK. Safety planning intervention: a brief intervention to mitigate suicide risk. Cogn Behav Pract. 2012;19 : 256–264.
62. Hatcher S, Sharon C, House A, Collins N, Collings S, Pillai A. The ACCESS study: Zelen randomised controlled trial of a package of care for people presenting to hospital after self-harm. Br J Psychiatry. 2015;206 : 229–236. doi: 10.1192/bjp.bp.113.135780 25614531
63. Slee N, Garnefski N, van der Leeden R, Arensman E, Spinhoven P. Cognitive-behavioural intervention for self-harm: randomised controlled trial. Br J Psychiatry. 2008;192 : 202–211. doi: 10.1192/bjp.bp.107.037564 18310581
64. Arensman E, Townsend E, Hawton K, Bremner S, Feldman E, Goldney R, et al. Psychosocial and pharmacological treatment of patients following deliberate self-harm: the methodological issues involved in evaluating effectiveness. Suicide Life Threat Behav. 2001;31 : 169–180. 11459249
65. Hepp U, Wittmann L, Schnyder U, Michel K. Psychological and psychosocial interventions after attempted suicide: an overview of treatment studies. Crisis. 2004;25 : 108–117. 15387237
66. Wenzel A, Brown GK, Beck AT. Cognitive therapy for suicidal patients: scientific and clinical applications. Washington (District of Columbia): American Psychological Association; 2009.
Štítky
Interní lékařství
Článek vyšel v časopisePLOS Medicine
Nejčtenější tento týden
2016 Číslo 3- Berberin: přírodní hypolipidemikum se slibnými výsledky
- Léčba bolesti u seniorů
- Příznivý vliv Armolipidu Plus na hladinu cholesterolu a zánětlivé parametry u pacientů s chronickým subklinickým zánětem
- Jak postupovat při výběru betablokátoru − doporučení z kardiologické praxe
- Červená fermentovaná rýže účinně snižuje hladinu LDL cholesterolu jako vhodná alternativa ke statinové terapii
-
Všechny články tohoto čísla
- Trans-Pacific Partnership Provisions in Intellectual Property, Transparency, and Investment Chapters Threaten Access to Medicines in the US and Elsewhere
- An Uninformative Truth: The Logic of Amarin’s Off-Label Promotion
- Performance of the GeneXpert Ebola Assay for Diagnosis of Ebola Virus Disease in Sierra Leone: A Field Evaluation Study
- Pragmatic Trials for Noncommunicable Diseases: Relieving Constraints
- Antibiotic Resistance in India: Drivers and Opportunities for Action
- Global Role and Burden of Influenza in Pediatric Respiratory Hospitalizations, 1982–2012: A Systematic Analysis
- Routine Pediatric Enterovirus 71 Vaccination in China: a Cost-Effectiveness Analysis
- Increased Duration of Paid Maternity Leave Lowers Infant Mortality in Low- and Middle-Income Countries: A Quasi-Experimental Study
- Planned Repeat Cesarean Section at Term and Adverse Childhood Health Outcomes: A Record-Linkage Study
- Experimental Treatment with Favipiravir for Ebola Virus Disease (the JIKI Trial): A Historically Controlled, Single-Arm Proof-of-Concept Trial in Guinea
- A Novel Brief Therapy for Patients Who Attempt Suicide: A 24-months Follow-Up Randomized Controlled Study of the Attempted Suicide Short Intervention Program (ASSIP)
- Comparison of the Schwartz and CKD-EPI Equations for Estimating Glomerular Filtration Rate in Children, Adolescents, and Adults: A Retrospective Cross-Sectional Study
- Cardiovascular and Renal Outcomes of Renin–Angiotensin System Blockade in Adult Patients with Diabetes Mellitus: A Systematic Review with Network Meta-Analyses
- Length of Stay After Childbirth in 92 Countries and Associated Factors in 30 Low- and Middle-Income Countries: Compilation of Reported Data and a Cross-sectional Analysis from Nationally Representative Surveys
- Transformative Innovations in Reproductive, Maternal, Newborn, and Child Health over the Next 20 Years
- Compassionate and Proactive Interventions by Health Workers in the United Kingdom: A Better Approach to Prevent and Respond to Female Genital Mutilation?
- Translational Research for Tuberculosis Elimination: Priorities, Challenges, and Actions
- The Community As the Patient in Malaria-Endemic Areas: Preempting Drug Resistance with Multiple First-Line Therapies
- PLOS Medicine
- Archiv čísel
- Aktuální číslo
- Informace o časopisu
Nejčtenější v tomto čísle- Experimental Treatment with Favipiravir for Ebola Virus Disease (the JIKI Trial): A Historically Controlled, Single-Arm Proof-of-Concept Trial in Guinea
- Comparison of the Schwartz and CKD-EPI Equations for Estimating Glomerular Filtration Rate in Children, Adolescents, and Adults: A Retrospective Cross-Sectional Study
- Performance of the GeneXpert Ebola Assay for Diagnosis of Ebola Virus Disease in Sierra Leone: A Field Evaluation Study
- A Novel Brief Therapy for Patients Who Attempt Suicide: A 24-months Follow-Up Randomized Controlled Study of the Attempted Suicide Short Intervention Program (ASSIP)
Kurzy
Zvyšte si kvalifikaci online z pohodlí domova
Současné možnosti léčby obezity
nový kurzAutoři: MUDr. Martin Hrubý
Všechny kurzyPřihlášení#ADS_BOTTOM_SCRIPTS#Zapomenuté hesloZadejte e-mailovou adresu, se kterou jste vytvářel(a) účet, budou Vám na ni zaslány informace k nastavení nového hesla.
- Vzdělávání



