-
Články
Top novinky
Reklama- Vzdělávání
- Časopisy
Top články
Nové číslo
- Témata
Top novinky
Reklama- Videa
- Podcasty
Nové podcasty
Reklama- Kariéra
Doporučené pozice
Reklama- Praxe
Top novinky
ReklamaAssociation between Regimen Composition and Treatment Response in Patients with Multidrug-Resistant Tuberculosis: A Prospective Cohort Study
In this prospective cohort study, Courtney Yuen and colleagues examine the association between regimen composition and treatment response in patients with multidrug-resistant tuberculosis.
Published in the journal: . PLoS Med 12(12): e32767. doi:10.1371/journal.pmed.1001932
Category: Research Article
doi: https://doi.org/10.1371/journal.pmed.1001932Summary
In this prospective cohort study, Courtney Yuen and colleagues examine the association between regimen composition and treatment response in patients with multidrug-resistant tuberculosis.
Introduction
World Health Organization (WHO) guidelines for the treatment of multidrug-resistant tuberculosis (MDR TB) recommend a regimen consisting of at least four second-line drugs that are likely to be effective as well as pyrazinamide [1]. In the absence of drug susceptibility testing (DST) results for a patient’s isolate, likely effectiveness is determined based on previous exposure to a drug, background resistance levels to that drug in the community, and, in patients who were contacts to other known cases, DST results for an associated case. Furthermore, the guidelines indicate that only marginal benefit has been observed for regimens based directly on the DST results for a patient’s isolate [1].
A meta-analysis of cohort studies of patients with MDR TB reported that in vitro susceptibility to individual drugs was consistently and statistically significantly associated with higher odds of treatment success compared to in vitro resistance, suggesting clinical utility for DST in regimen design [2]. In addition, the use of baseline DST results to design individualized regimens involving prolonged use of five or more drugs with likely effectiveness has been associated with decreased risks of treatment failure, death, and relapse among patient cohorts in Peru and the Russian Federation [3–5]. Together, this evidence suggests the need to reassess both the role of DST in regimen design as well as the potential benefit of including more drugs in MDR TB regimens.
To gain insight into how regimen design affects treatment response, we analyzed treatment and microbiological data from the Preserving Effective Tuberculosis Treatment Study (PETTS), a 6-y, multinational prospective cohort study of patients with MDR TB [6]. As our goal was to focus on the association between DST results and the direct microbiological effect of drugs, we used time to sputum culture conversion as an indicator of the bactericidal effect of treatment. We assessed the association between the number of potentially effective drugs included in a regimen and time to sputum culture conversion. In addition, we compared the individual effects of drugs to which DST results indicated susceptibility, drugs to which DST results indicated resistance, and drugs that were not tested.
Methods
Ethics
PETTS was approved by the US Centers for Disease Control and Prevention (CDC) Institutional Review Board and institutional review boards at all participating sites. Written informed consent was obtained from all study participants.
Patient Population and Study Procedures
The PETTS study design and patient population have been described previously [6]. Briefly, this prospective cohort study, conducted in 2005–2010, enrolled consecutive adults with pulmonary MDR TB in nine countries: Estonia (nationwide), Latvia (nationwide), Peru (two districts in Lima), Philippines (greater Manila), Russian Federation (Orel and Vladimir Oblasts), South Africa (Eastern Cape, KwaZulu-Natal, Mpumalanga, and Northwest provinces), South Korea (National Masan Tuberculosis Hospital, Masan, and Korean Institute of Tuberculosis, Seoul), Thailand (Sakon Nakon, Srisaket, Ubon Ratchathani, and Yasothon provinces), and Taiwan (nationwide). Inclusion criteria for the study were (1) pulmonary MDR TB confirmed microbiologically by a local reference laboratory from a specimen collected within 30 d of starting treatment and (2) receipt of second-line drugs for at least 30 d. South Africa restricted enrollment to patients who had not previously been treated for MDR TB. Standardized information was recorded at all sites, including demographic, socioeconomic, and clinical information for each participant, and treatment and laboratory monitoring details.
Culture was performed on a baseline sputum sample, and monthly follow-up sputum samples were collected for the duration of treatment. Local laboratories performed cultures for monitoring and DST for determining patient eligibility. A subset of isolates from patients enrolled in the study were shipped in batches to CDC for centralized DST and genotyping. Patients were eligible for inclusion in this analysis if they had positive cultures at the start of treatment for MDR TB, if they had DST results from CDC for fluoroquinolones (DST was performed for ciprofloxacin and ofloxacin) and second-line injectable drugs (i.e., amikacin, kanamycin, capreomycin), and if resistance to both isoniazid and rifampin were confirmed at CDC. We excluded patients for whom the DST performed at CDC indicated susceptibility to either isoniazid or rifampin in response to a reviewer suggestion, as several of these patients were treated with isoniazid or rifampin. Patients with extensively drug-resistant tuberculosis (XDR TB), defined as MDR TB with additional resistance to any fluoroquinolone and at least one second-line injectable drug, were excluded from the analysis, as were patients for whom a date of culture conversion or censoring could not be determined.
The primary research objective of PETTS was to determine whether the Green Light Committee approval process was associated with reduced amplification of drug resistance; the results of this analysis have been previously reported [7]. However, the study protocol was conceived to produce a dataset that could be used to answer several additional research questions that required rigorous microbiological follow-up of MDR TB patients. The present analysis was not contained in the original analysis plan, but was conceived because several recent publications suggested that regimens based on known drug susceptibilities and regimens containing more drugs were associated with better clinical outcomes [2–5].
Definitions
Initial sputum culture conversion was defined as at least two consecutive negative cultures of sputum samples collected at least 30 d apart. Time to sputum culture conversion was defined as the time in days from the start of MDR TB treatment to the sputum specimen collection date of the first of the consecutive negative cultures. Patients for whom sputum culture conversion did not occur were censored 1 mo before the collection date of the last sputum specimen because they were still at risk to convert during the last month of follow-up.
Classification of each drug’s effectiveness was based on the results of DST performed at CDC on the baseline culture using the indirect agar plate proportion method [6]. DST was performed for isoniazid, rifampin, ethambutol, ciprofloxacin, ofloxacin, amikacin, capreomycin, kanamycin, streptomycin, rifabutin, ethionamide, and para-aminosalicylic acid. Drugs for which DST indicated susceptibility were considered effective. Drugs for which the baseline DST result indicated resistance were considered ineffective. In addition, levofloxacin and moxifloxacin were considered effective if no resistance to ciprofloxacin or ofloxacin was observed, and were considered ineffective if resistance to either ciprofloxacin or ofloxacin was observed. Prothionamide was considered effective if no resistance to ethionamide was observed, and ineffective if resistance to ethionamide was observed. Drugs for which DST was not performed at CDC (cycloserine, terizidone, amoxicillin/clavulanate, clarithromycin, thioacetazone, clofazimine, imipenem, and linezolid) were classified as untested drugs. Pyrazinamide, although not tested routinely, was kept separate from this group of untested drugs because it is a first-line drug with a well-established role in treatment, and it is recommended for routine inclusion in MDR TB regimens [1].
For each individual drug, we calculated the number of days during which the drug was included in a patient’s regimen between initiation of MDR TB treatment and sputum culture conversion or censoring. The number of days a drug was included in a patient’s regimen was inferred from the dates the drug was started and stopped; if a single drug was started and stopped multiple times, the days between each pair of start and stop dates were summed. Drug-days were summed for all the drugs in each of four groups: effective drugs, ineffective drugs, pyrazinamide, and untested drugs. For each group, this sum was divided by the number of days before sputum culture conversion or censoring to calculate the average number of drugs in each group that the patient received per day. In addition, a composite variable was created to reflect the total number of “potentially effective drugs” received per day, which included all effective drugs, pyrazinamide, and untested drugs.
Data Analysis
We analyzed the association between variables of interest and sputum culture conversion using Cox proportional hazards regression. We stratified by country to control for setting-associated confounders. We evaluated proportional hazards assumptions by testing the significance of time-dependent interaction terms for all variables. We were interested in the associations between time to sputum culture conversion and both the number of drugs in a regimen and the presumed effectiveness of these drugs. Therefore, we generated two multivariable models to assess the association between treatment regimen and time to sputum culture conversion. In the first model, the exposure of interest was the average number of potentially effective drugs received per day, analyzed as a categorical variable. In the second model, the exposures of interest were the average numbers of drugs received in each of the four drug groups, analyzed as continuous variables. We considered clinical and demographic covariates for inclusion in the multivariable models based on the strength of univariate associations with sputum culture conversion (covariates with Wald p < 0.1 were eligible for inclusion) or biological plausibility. The resistance pattern at baseline and the number of drugs to which the baseline isolate was resistant were retained in both models because of an established association between the extent of baseline drug resistance and treatment success [8] and because the extent of drug resistance was likely to be associated with resistance to untested drugs. To generate the final models, we used backward elimination, assessing the effect of each elimination on the point estimates and confidence intervals to identify potential confounders.
In the second model, we believed interactions among the different drug groups to be likely. Therefore, we assessed both the main effects model and a model in which we considered all two-way interactions among drug group variables. Collinearity among variables was assessed; a variance inflation factor > 5 or a maximum condition index > 50 were considered evidence of collinearity. As a sensitivity analysis, we restricted the first model to patients who did not receive any Group 4 (oral second-line drugs other than fluoroquinolones) or Group 5 drugs (drugs with antimycobacterial activity but unproven efficacy against drug-resistant TB) [1] for which drug sensitivity was unknown. All analyses were performed using SAS 9.3.
Results
Out of 1,659 patients in the PETTS cohort, 1,137 were included in our analysis (Fig 1). These patients were followed for a median of 20 mo (interquartile range 16–23 mo) after MDR TB treatment initiation. Initial sputum culture conversion occurred for 909 (79.9%) patients at a median of 2 mo (interquartile range 1–3 mo). However, the percentage of patients achieving initial sputum culture conversion within 6 mo varied considerably by country (Table 1).
Fig. 1. Inclusion of patients in the analysis. 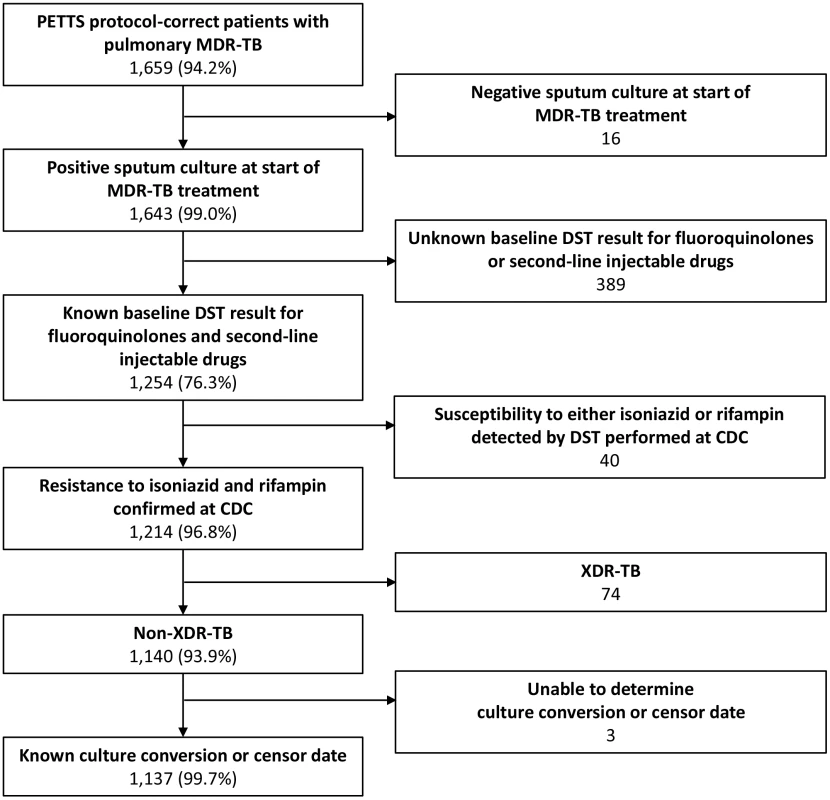
MDR-TB is tuberculosis resistant to at least isoniazid and rifampin; XDR-TB is tuberculosis resistant to at least isoniazid, rifampin, one fluoroquinolone, and one second-line injectable drug. Tab. 1. Baseline drug resistance and treatment characteristics of patients, by country (n = 1,137). 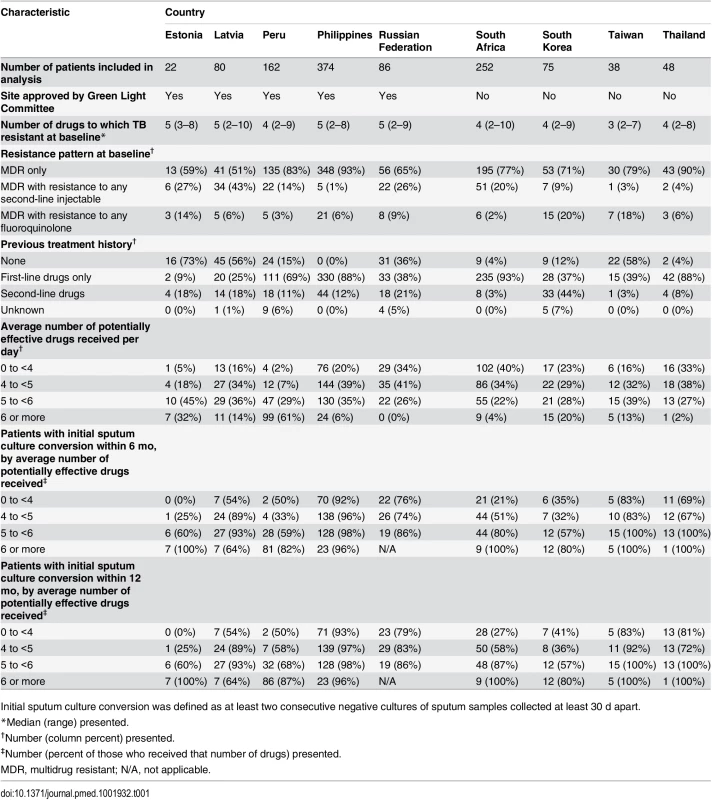
Initial sputum culture conversion was defined as at least two consecutive negative cultures of sputum samples collected at least 30 d apart. Time to initial sputum culture conversion among all patients by average number of potentially effective drugs received per day is show graphically in Fig 2. As baseline drug resistance pattern, drug exposure, and percentage of patients achieving initial sputum culture conversion by 6 mo varied by country (Table 1), we stratified the statistical analysis by country to control for setting-associated confounders. In stratified univariate analysis, receiving an average of at least six potentially effective drugs per day was associated with a 34% increase in the likelihood of sputum culture conversion compared to receiving an average of at least five but fewer than six potentially effective drugs per day (hazard ratio [HR] 1.34 per effective drug, 95% CI 1.08–1.65) (Table 2). In contrast, receiving fewer potentially effective drugs was associated with lower likelihoods of sputum culture conversion (HR for fewer than four drugs 0.37, 95% CI 0.30–0.45; HR for at least four but fewer than five drugs 0.58, 95% CI 0.49–0.68).
Fig. 2. Time to initial sputum culture conversion by average number of potentially effective drugs received per day. 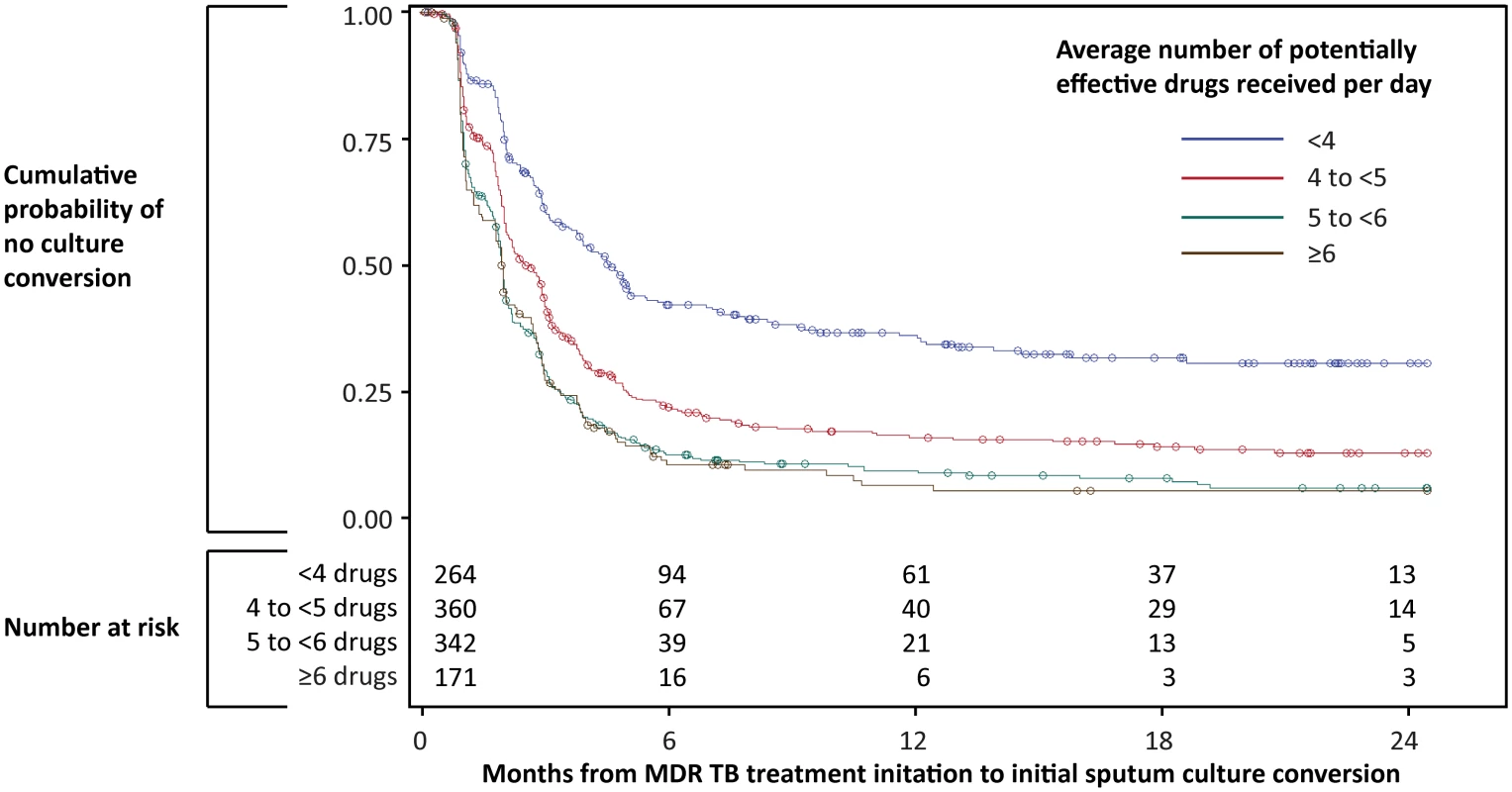
Initial sputum culture conversion was defined as at least two consecutive negative cultures of sputum samples collected at least 30 d apart. Tab. 2. Patient characteristics and univariate associations with sputum culture conversion among patients treated for MDR TB (n = 1,137). 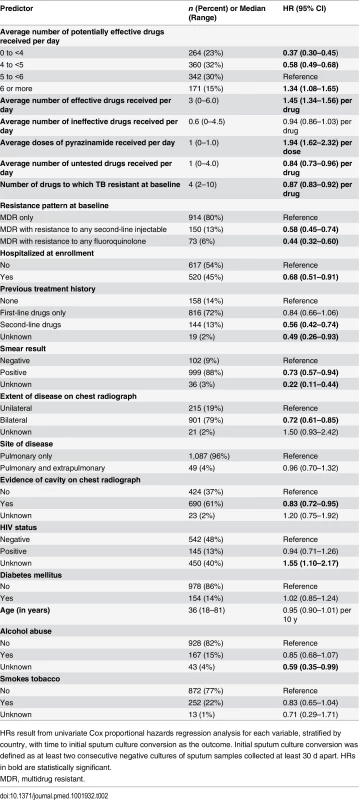
HRs result from univariate Cox proportional hazards regression analysis for each variable, stratified by country, with time to initial sputum culture conversion as the outcome. Initial sputum culture conversion was defined as at least two consecutive negative cultures of sputum samples collected at least 30 d apart. HRs in bold are statistically significant. In univariate analysis, stratified by country, the presence of more effective drugs in the regimen was associated with an increased likelihood of sputum culture conversion (HR 1.45 per effective drug, 95% CI 1.34–1.56), and inclusion of pyrazinamide in the regimen was associated with a doubled likelihood of sputum culture conversion (HR 1.94, 95% CI 1.62–2.32) (Table 2). In contrast, the presence of more untested drugs in the regimen was associated with a slightly but significantly decreased likelihood of sputum culture conversion (HR 0.84 per untested drug, 95% CI 0.73–0.96). The following were all associated with a lower likelihood of sputum culture conversion: baseline resistance to more drugs (HR 0.87, 95% CI 0.83–0.92, per drug), baseline resistance specifically to fluoroquinolones (HR 0.44, 95% CI 0.32–0.60) or second-line injectable drugs (HR 0.58, 95% CI 0.45–0.74), hospitalization at enrollment (HR 0.68, 95% CI 0.51–0.91), previous treatment with second-line drugs (HR 0.56, 95% CI 0.42–0.74), positive baseline sputum smear microscopy result (HR 0.73, 95% CI 0.57–0.94), radiographically determined bilateral disease (HR 0.72, 95% CI 0.61–0.85), and evidence of cavity formation (HR 0.83, 95% CI 0.72–0.95) (Table 2).
The results of the multivariable analyses are summarized in Table 3. In the first multivariable model, receiving an average of at least six potentially effective drugs per day was associated with a 36% greater likelihood of sputum culture conversion than receiving an average of at least five but fewer than six potentially effective drugs per day (adjusted hazard ratio [aHR] 1.36, 95% CI 1.09–1.69), after adjusting for extent and pattern of baseline resistance, previous treatment history, sputum smear result, and extent of disease on chest radiograph. In contrast, receiving fewer potentially effective drugs was associated with lower likelihoods of sputum culture conversion (aHR for fewer than four drugs 0.36, 95% CI 0.29–0.44; aHR for at least four but fewer than five drugs 0.56, 95% CI 0.47–0.66). Similar results were observed when we excluded from analysis 697 patients who received any Group 4 or 5 drug for which drug susceptibility was unknown (S1 Table).
Tab. 3. Multivariable models for the association between regimen composition and sputum culture conversion. 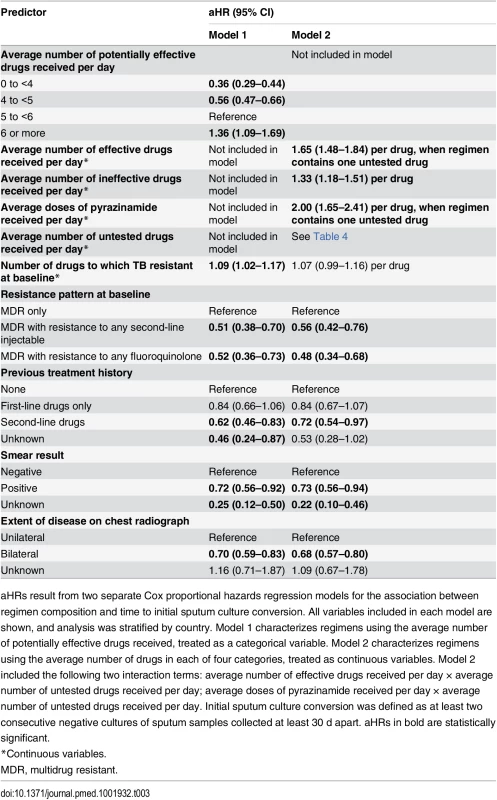
aHRs result from two separate Cox proportional hazards regression models for the association between regimen composition and time to initial sputum culture conversion. All variables included in each model are shown, and analysis was stratified by country. Model 1 characterizes regimens using the average number of potentially effective drugs received, treated as a categorical variable. Model 2 characterizes regimens using the average number of drugs in each of four categories, treated as continuous variables. Model 2 included the following two interaction terms: average number of effective drugs received per day × average number of untested drugs received per day; average doses of pyrazinamide received per day × average number of untested drugs received per day. Initial sputum culture conversion was defined as at least two consecutive negative cultures of sputum samples collected at least 30 d apart. aHRs in bold are statistically significant. In the second multivariable model, HRs associated with each drug group exposure of interest were adjusted for the other drug group exposures, as well as for extent and pattern of baseline resistance, previous treatment history, sputum smear result, and extent of disease on chest radiograph. The main effects model produced similar estimates as the model that considered interaction terms; therefore, we present the model that included the interaction terms, as significant interactions were detected among effective drugs, untested drugs, and pyrazinamide. For patients receiving one untested drug (the median number of untested drugs received), the presence of one additional effective drug in the regimen was associated with a 65% greater likelihood of sputum culture conversion (aHR 1.65, 95% CI 1.48–1.84), and including pyrazinamide in the regimen was associated with a doubled likelihood of sputum culture conversion (aHR 2.00, 95% CI 1.65–2.41). The presence of an additional ineffective drug in a regimen was associated with a 33% greater likelihood of sputum culture conversion (aHR 1.33, 95% CI 1.18–1.51), despite resistance to ineffective drugs on baseline DST (Table 3).
The benefit of including untested drugs was dependent on the other drugs present in the regimen (Table 4). For patients receiving two or fewer effective drugs, the presence of an additional untested drug was not associated with any significant acceleration of sputum culture conversion. For patients receiving three effective drugs (the median number of effective drugs received) and no pyrazinamide, the presence of an additional untested drug was associated with a 39% greater likelihood of sputum culture conversion (aHR 1.39, 95% CI 1.09–1.76). However, for patients receiving three effective drugs as well as pyrazinamide, the presence of an additional untested drug was not associated with any significant increase in the likelihood of sputum culture conversion (aHR 0.93, 95% CI 0.77–1.11). Additional results relating to these interactions are included in S2 and S3 Tables. Drug exposures included in the untested drug group were predominantly cycloserine and terizidone (47% and 25% of drug-days of exposure, respectively), with Group 5 drugs comprising the remainder (a cumulative 28% of drug-days of exposure). Neither bedaquiline nor delamanid, nor any experimental drugs, were used in this cohort.
Tab. 4. Multivariable model 2 adjusted hazard ratios for sputum culture conversion associated with inclusion of one additional untested drug in the regimen, stratified by average number of effective drugs received per day and inclusion of pyrazinamide in the regimen. 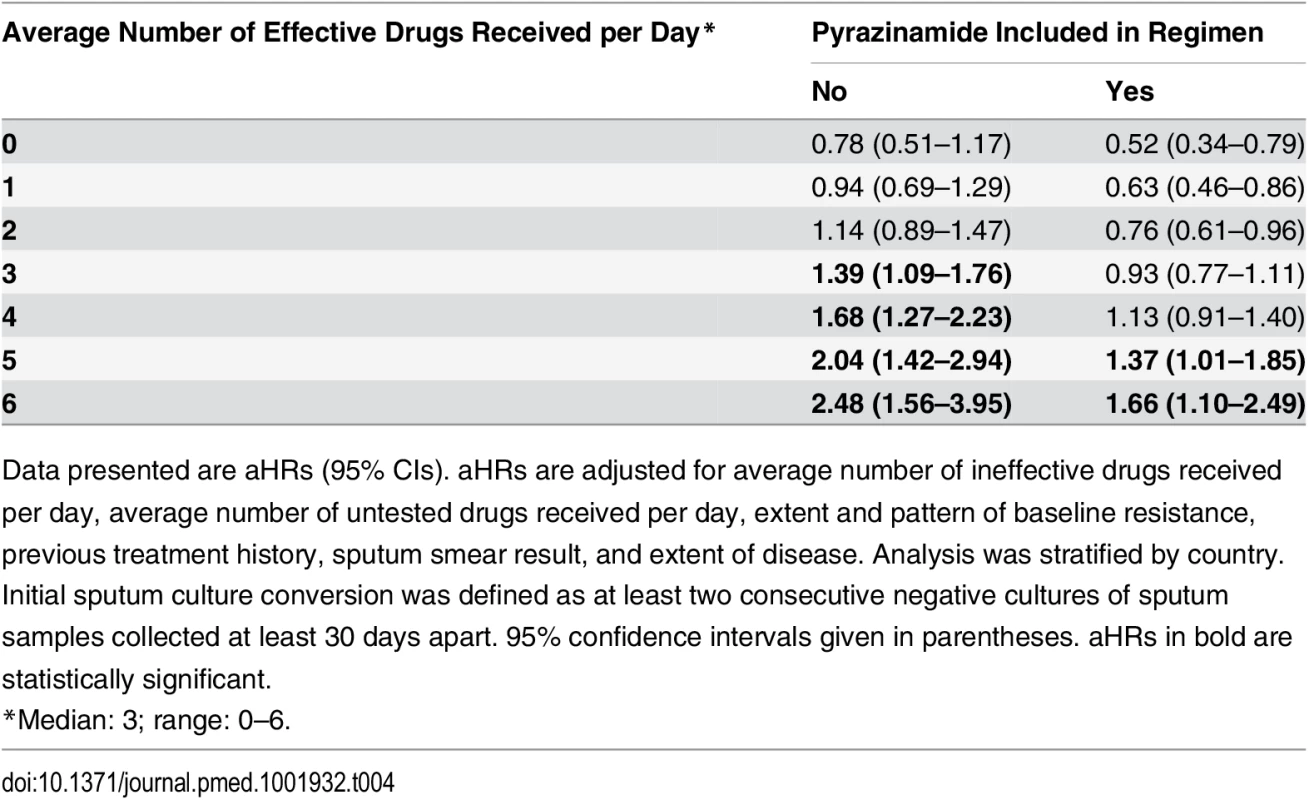
Data presented are aHRs (95% CIs). aHRs are adjusted for average number of ineffective drugs received per day, average number of untested drugs received per day, extent and pattern of baseline resistance, previous treatment history, sputum smear result, and extent of disease. Analysis was stratified by country. Initial sputum culture conversion was defined as at least two consecutive negative cultures of sputum samples collected at least 30 days apart. 95% confidence intervals given in parentheses. aHRs in bold are statistically significant. Independent associations between clinical covariates and sputum culture conversion were similar in both multivariable models (Table 3). Compared to MDR TB with susceptibility to both second-line injectable drugs and fluoroquinolones, MDR TB with added resistance to any second-line injectable drug (model 1, aHR 0.51, 95% CI 0.38–0.70; model 2, aHR 0.56, 95% CI 0.42–0.76) and MDR TB with added resistance to any fluoroquinolone (model 1, aHR 0.52, 95% CI 0.36–0.73; model 2, aHR 0.48, 95% CI 0.34–0.68) were associated with a lower likelihood of sputum culture conversion. The following were independently associated with a decreased likelihood of sputum culture conversion: prior treatment with second-line tuberculosis drugs (model 1, aHR 0.62, 95% CI 0.46–0.83; model 2, aHR 0.72, 95% CI 0.54–0.97), positive sputum smear (model 1, aHR 0.72, 95% CI 0.56–0.92; model 2, aHR 0.73, 95% CI 0.56–0.94), and bilateral disease (model 1, aHR 0.70, 95% CI 0.59–0.83; model 2, aHR 0.68, 95% CI 0.57–0.80). No collinearity was observed among variables included in the multivariable models.
Discussion
In our analysis, greater numbers of potentially effective drugs in an MDR TB treatment regimen were associated with accelerated sputum culture conversion. In general, inclusion of pyrazinamide or additional drugs to which baseline DST indicated susceptibility (i.e., effective drugs) were associated with greater increases in the likelihood of sputum culture conversion than inclusion of drugs to which baseline DST indicated resistance (i.e., ineffective drugs). The presence of untested drugs in the regimen was associated with an increased likelihood of sputum culture conversion only if a minimum number of effective drugs was present in the regimen.
We observed a benefit to receiving a greater number of potentially effective drugs (i.e., drugs without a DST result indicating resistance), as well as an interaction in which the presence of more effective drugs enhanced the benefit of untested drugs. Both of these results add to existing evidence that increasing the number of drugs in MDR TB regimens is advantageous. Patients receiving individualized regimens containing a minimum of five probably effective drugs for prolonged periods after sputum culture conversion have been shown to have decreased risks of treatment failure, death, and relapse compared to patients receiving fewer drugs [3–5]. In addition, high cure rates have been reported with only 9 mo of treatment using a standardized regimen including seven drugs during the intensive phase [9]. In response to the accumulating evidence for the benefit of increasing the number of drugs in regimens for MDR TB, WHO guidelines for MDR TB regimen composition increased the minimum number of drugs recommended from four in 2006 and 2008 to five in 2011 [1,10]. Our results suggest that treatment might be further fortified by adding additional potentially effective drugs.
In our analysis, for most patients, the increased likelihood of sputum culture conversion associated with the presence of an additional effective drug in the regimen was greater than the acceleration associated with the presence of an additional ineffective drug. This result suggests that tailoring regimens based on DST results could improve treatment response. However, we also observed a strong benefit to inclusion of pyrazinamide despite unknown efficacy, which would appear to support the WHO recommendation to include pyrazinamide in MDR TB regimens [1] without relying on DST results, which are known to be unreliable for this drug [11]. But as there were no DST results for pyrazinamide in this cohort, caution must be taken when interpreting this finding. It is possible that clinicians accurately assessed the likelihood that pyrazinamide would be effective before deciding to use it, that the prevalence of pyrazinamide resistance in the analyzed cohort was relatively low, or that the efficacy of pyrazinamide in those patients with pyrazinamide susceptibility was so great that an association was observed even though the drug was ineffective in a proportion of the patients who received it. In situations where undetected resistance renders pyrazinamide ineffective, a five-drug regimen that includes pyrazinamide would actually contain only four effective drugs, which could put patients at risk for poorer outcomes [12].
The drugs classified in our analysis as untested drugs comprise those classified as Group 5 by WHO [10], as well as the second-line drugs cycloserine and terizidone. Cycloserine was not tested at CDC because testing requires Lowenstein–Jensen medium, and CDC performs DST using Middlebrook medium or BACTEC broth medium. Because of inconclusive evidence about the efficacy of Group 5 drugs, WHO recommends that they be used only to supplement regimens if additional drugs are required [1]. Consistent with their supplementary role, we observed that the benefit of including untested drugs was dependent on the other drugs present in the regimen. Without a minimum number of effective drugs present, inclusion of an additional untested drug was not associated with any significant increase in the likelihood of sputum culture conversion. Thus, our results suggest that it would be preferential to use the new drugs bedaquiline and delamanid—which are almost certainly likely to be effective because of their novel mechanisms and lack of prior use—in place of Group 5 drugs in treatment regimens.
Unexpectedly, we observed that the addition of ineffective drugs was associated with a modest but significant acceleration of sputum culture conversion. Possible explanations for this observation include infection with multiple strains with differing drug susceptibilities, strains with low-level resistance in vitro that were still susceptible in vivo to therapeutic drug concentrations, or synergistic effects between drugs. It is also possible that misclassification of drug resistance occurred from our using ciprofloxacin and ofloxacin DST results to determine the likely efficacy of moxifloxacin, as moxifloxacin susceptibility has been reported in approximately 30% of clinical isolates resistant to ofloxacin [13,14] or ciprofloxacin [14]. However, in our study population, only 31 (2.7%) patients received moxifloxacin and had it classified as ineffective based on resistance to ofloxacin or ciprofloxacin; therefore, the influence of this misclassification on our results as a whole was likely limited.
The associations with clinical covariates that we observed are consistent with previous studies involving patients with MDR TB that have shown associations between decreased likelihood of sputum culture conversion and sputum smear positivity [15–17], bilateral extent of disease [18], previous treatment with second-line drugs [16,18], and more extensive baseline drug resistance [16,18].
Our analysis was subject to several important limitations. PETTS was an observational study, not a randomized trial. In addition, while the study involved sites in nine different countries, our results may not be generalizable to other settings with very different MDR TB epidemics. For instance, the prevalence of pre–XDR TB fluoroquinolone resistance in the PETTS cohort was substantially lower than has been reported among MDR TB patients in some South Asian settings [19,20]. Choice of regimen varied across sites, as not all countries had all drugs available. While we attempted to reduce bias by stratifying analysis by country and including clinical covariates in our analysis, complete elimination of bias in a cohort of this diversity is impossible. However, despite the limitations inherent to using observational data from treatment programs, conclusions drawn from these data may in fact be more easily translatable to clinical decision-making since they reflect results from ordinary practice.
A second set of limitations relates to assumptions made about drug efficacy. The range of baseline resistance patterns and regimens received prevented us from assessing the effects of individual drugs and from controlling for the varying efficacy of individual drugs. Thus, in our analysis, the calculation of the average number of drugs received per day in a particular category gave equal weight to all the drugs in that category even though, in reality, some drugs may exert more of an effect than others. Furthermore, as we considered only baseline DST results when determining drug effectiveness, our analysis did not take into account changing efficacy resulting from acquisition of drug resistance during treatment. However, we believe that relatively few patients in our analytic cohort are likely to have acquired resistance prior to sputum culture conversion or censoring, as only 68 PETTS patients acquired XDR TB during the course of the study [7].
Our analysis was also limited by the data collected. Our quantification of drug exposure was derived from the start and stop dates for individual drugs. However, the PETTS protocol specified that a stoppage need be recorded only if a drug was discontinued for at least 2 wk. Therefore, our measures of drug exposure may be overestimates in some cases because brief interruptions lasting less than 2 wk might not have been recorded. In addition, DST was not performed for every drug that patients received, which prevented us from determining the likely efficacy of all drugs included in the analysis. We also did not have adherence data corresponding to each episode of drug prescription, and we assumed that prescription of a drug was equivalent to its having been taken. This assumption was likely valid for Green Light Committee–approved programs, in which all treatment was administered under direct observation. If adherence was poorer in countries without a Green Light Committee–approved program, we would expect associations between drug exposure and sputum culture conversion to be attenuated, biasing our results toward the null.
Finally, the interpretation of our results is limited by our use of time to initial sputum culture conversion as the outcome. We did not have long-term follow-up data to assess the risk of relapse, nor did we consider sputum culture reversion (i.e., positive cultures obtained after initial sputum culture conversion) in our analysis. Time to initial sputum culture conversion is a standard marker for treatment response in patients with tuberculosis, and has been shown to correlate with treatment outcome in patients with MDR TB [18]. In the PETTS cohort, sputum culture conversion at 6 mo was found to be a robust predictor of final treatment outcome [21]. However, our analysis could have been strengthened had we been able to assess the risk of relapse as well, thereby allowing a comparison between the early prognostic marker of initial sputum culture conversion and long-term treatment efficacy.
In conclusion, our analysis suggests that MDR TB regimens including more potentially effective drugs than the minimum of five currently recommended by WHO may encourage improved response to treatment in patients with MDR TB. In addition, rapid access to high-quality DST results could facilitate the design of more effective individualized regimens. However, randomized controlled trials are necessary to confirm whether individualized regimens with more than five drugs can indeed achieve better cure rates than current recommended regimens, and new rapid DST techniques will be required if knowledge of baseline drug resistance is to guide regimen composition at the beginning of treatment.
Supporting Information
Zdroje
1. World Health Organization. Guidelines for the programmatic management of drug-resistant tuberculosis: 2011 update. Geneva: World Health Organization; 2011.
2. Bastos ML, Hussain H, Weyer K, Garcia-Garcia L, Leimane V, Leung CC, et al. Treatment outcomes of patients with multidrug-resistant and extensively drug-resistant tuberculosis according to drug susceptibility testing to first - and second-line drugs: an individual patient data meta-analysis. Clin Infect Dis. 2014;59 : 1364–1374. doi: 10.1093/cid/ciu619 25097082
3. Mitnick CD, Franke MF, Rich ML, Alcantara Viru FA, Appleton SC, Atwood SS, et al. Aggressive regimens for multidrug-resistant tuberculosis decrease all-cause mortality. PLoS ONE. 2013;8:e58664. doi: 10.1371/journal.pone.0058664 23516529
4. Franke MF, Appleton SC, Mitnick CD, Furin JJ, Bayona J, Chalco K, et al. Aggressive regimens for multidrug-resistant tuberculosis reduce recurrence. Clin Infect Dis. 2013;56 : 770–776. doi: 10.1093/cid/cis1008 23223591
5. Velasquez GE, Becerra MC, Gelmanova IY, Pasechnikov AD, Yedilbayev A, Shin SS, et al. Improving outcomes for multidrug-resistant tuberculosis: aggressive regimens prevent treatment failure and death. Clin Infect Dis. 2014;59 : 9–15. doi: 10.1093/cid/ciu209 24729493
6. Dalton T, Cegielski P, Akksilp S, Asencios L, Campos Caoili J, Cho SN, et al. Prevalence of and risk factors for resistance to second-line drugs in people with multidrug-resistant tuberculosis in eight countries: a prospective cohort study. Lancet. 2012;380 : 1406–1417. doi: 10.1016/S0140-6736(12)60734-X 22938757
7. Cegielski JP, Dalton T, Yagui M, Wattanaamornkiet W, Volchenkov GV, Via LE, et al. Extensive drug resistance acquired during treatment of multidrug-resistant tuberculosis. Clin Infect Dis. 2014;59 : 1049–1063. doi: 10.1093/cid/ciu572 25057101
8. Falzon D, Gandhi N, Migliori GB, Sotgiu G, Cox HS, Holtz TH, et al. Resistance to fluoroquinolones and second-line injectable drugs: impact on multidrug-resistant TB outcomes. Eur Respir J. 2013;42 : 156–168. doi: 10.1183/09031936.00134712 23100499
9. Van Deun A, Maug AK, Salim MA, Das PK, Sarker MR, Daru P, et al. Short, highly effective, and inexpensive standardized treatment of multidrug-resistant tuberculosis. Am J Respir Crit Care Med. 2010;182 : 684–692. doi: 10.1164/rccm.201001-0077OC 20442432
10. World Health Organization. Guidelines for the programmatic management of drug-resistant tuberculosis: emergency update 2008. Geneva: World Health Organization; 2008.
11. Zhang Y, Mitchison D. The curious characteristics of pyrazinamide: a review. Int J Tuberc Lung Dis. 2003;7 : 6–21. 12701830
12. Franke MF, Becerra MC, Tierney DB, Rich ML, Bonilla C, Bayona J, et al. Counting pyrazinamide in regimens for multidrug-resistant tuberculosis. Ann Am Thorac Soc. 2015;12 : 674–679. doi: 10.1513/AnnalsATS.201411-538OC 25664920
13. Jo KW, Lee SD, Kim WS, Kim DS, Shim TS. Treatment outcomes and moxifloxacin susceptibility in ofloxacin-resistant multidrug-resistant tuberculosis. Int J Tuberc Lung Dis. 2014;18 : 39–43. doi: 10.5588/ijtld.13.0307 24365550
14. Farhat MR, Mitnick CD, Franke MF, Kaur D, Sloutsky A, Murray M, et al. Concordance of Mycobacterium tuberculosis fluoroquinolone resistance testing: implications for treatment. Int J Tuberc Lung Dis. 2015;19 : 339–341. doi: 10.5588/ijtld.14.0814 25686144
15. Qazi F, Khan U, Khowaja S, Javaid M, Ahmed A, Salahuddin N, et al. Predictors of delayed culture conversion in patients treated for multidrug-resistant tuberculosis in Pakistan. Int J Tuberc Lung Dis. 2011;15 : 1556–1559. doi: 10.5588/ijtld.10.0679 22008773
16. Kurbatova EV, Gammino VM, Bayona J, Becerra MC, Danilovitz M, Falzon D, et al. Predictors of sputum culture conversion among patients treated for multidrug-resistant tuberculosis. Int J Tuberc Lung Dis. 2012;16 : 1335–1343. doi: 10.5588/ijtld.11.0811 23107633
17. Brust JC, Berman AR, Zalta B, Haramati LB, Ning Y, Heo M, et al. Chest radiograph findings and time to culture conversion in patients with multidrug-resistant tuberculosis and HIV in Tugela Ferry, South Africa. PLoS ONE. 2013;8:e73975. doi: 10.1371/journal.pone.0073975 24040132
18. Holtz TH, Sternberg M, Kammerer S, Laserson KF, Riekstina V, Zarovska E, et al. Time to sputum culture conversion in multidrug-resistant tuberculosis: predictors and relationship to treatment outcome. Ann Intern Med. 2006;144 : 650–659. 16670134
19. Selvakumar N, Kumar V, Balaji S, Prabuseenivasan S, Radhakrishnan R, Sekar G, et al. High rates of ofloxacin resistance in Mycobacterium tuberculosis among both new and previously treated patients in Tamil Nadu, South India. PLoS ONE. 2015;10:e0117421. doi: 10.1371/journal.pone.0117421 25738956
20. Kamal SM, Hossain A, Sultana S, Begum V, Haque N, Ahmed J, et al. Anti-tuberculosis drug resistance in Bangladesh: reflections from the first nationwide survey. Int J Tuberc Lung Dis. 2015;19 : 151–156. doi: 10.5588/ijtld.14.0200 25574912
21. Kurbatova EV, Cegielski JP, Lienhardt C, Akksilp R, Bayona J, Becerra MC, et al. Sputum culture conversion as a prognostic marker for end-of-treatment outcome in patients with multidrug-resistant tuberculosis: a secondary analysis of data from two observational cohort studies. Lancet Respir Med. 2015;3 : 201–209. doi: 10.1016/S2213-2600(15)00036-3 25726085
Štítky
Interní lékařství
Článek vyšel v časopisePLOS Medicine
Nejčtenější tento týden
2015 Číslo 12- Berberin: přírodní hypolipidemikum se slibnými výsledky
- Léčba bolesti u seniorů
- Příznivý vliv Armolipidu Plus na hladinu cholesterolu a zánětlivé parametry u pacientů s chronickým subklinickým zánětem
- Jak postupovat při výběru betablokátoru − doporučení z kardiologické praxe
- Červená fermentovaná rýže účinně snižuje hladinu LDL cholesterolu jako vhodná alternativa ke statinové terapii
-
Všechny články tohoto čísla
- Risks and Benefits of Nalmefene in the Treatment of Adult Alcohol Dependence: A Systematic Literature Review and Meta-Analysis of Published and Unpublished Double-Blind Randomized Controlled Trials
- Diversity in Clinical and Biomedical Research: A Promise Yet to Be Fulfilled
- Police Killings and Police Deaths Are Public Health Data and Can Be Counted
- A Successful Failure: Missing the MDG4 Target for Under-Five Mortality in South Africa
- The Ebola Vaccine, Iatrogenic Injuries, and Legal Liability
- Progress in Medicine: Experts Take Stock
- Use of Viremia to Evaluate the Baseline Case Fatality Ratio of Ebola Virus Disease and Inform Treatment Studies: A Retrospective Cohort Study
- Acute Cardiovascular Events after Herpes Zoster: A Self-Controlled Case Series Analysis in Vaccinated and Unvaccinated Older Residents of the United States
- Moving Beyond “Food Deserts”: Reorienting United States Policies to Reduce Disparities in Diet Quality
- Public Health and International Partnerships in the Democratic People’s Republic of Korea
- Self-Administered Outpatient Antimicrobial Infusion by Uninsured Patients Discharged from a Safety-Net Hospital: A Propensity-Score-Balanced Retrospective Cohort Study
- Association between Regimen Composition and Treatment Response in Patients with Multidrug-Resistant Tuberculosis: A Prospective Cohort Study
- 10-y Risks of Death and Emergency Re-admission in Adolescents Hospitalised with Violent, Drug- or Alcohol-Related, or Self-Inflicted Injury: A Population-Based Cohort Study
- World Health Organization Global Estimates and Regional Comparisons of the Burden of Foodborne Disease in 2010
- Bariatric Surgery in the United Kingdom: A Cohort Study of Weight Loss and Clinical Outcomes in Routine Clinical Care
- Traditional and Emerging Lifestyle Risk Behaviors and All-Cause Mortality in Middle-Aged and Older Adults: Evidence from a Large Population-Based Australian Cohort
- Inequalities in Alcohol-Related Mortality in 17 European Countries: A Retrospective Analysis of Mortality Registers
- World Health Organization Estimates of the Global and Regional Disease Burden of 11 Foodborne Parasitic Diseases, 2010: A Data Synthesis
- A Molecular Host Response Assay to Discriminate Between Sepsis and Infection-Negative Systemic Inflammation in Critically Ill Patients: Discovery and Validation in Independent Cohorts
- World Health Organization Estimates of the Global and Regional Disease Burden of 22 Foodborne Bacterial, Protozoal, and Viral Diseases, 2010: A Data Synthesis
- PLOS Medicine
- Archiv čísel
- Aktuální číslo
- Informace o časopisu
Nejčtenější v tomto čísle- Self-Administered Outpatient Antimicrobial Infusion by Uninsured Patients Discharged from a Safety-Net Hospital: A Propensity-Score-Balanced Retrospective Cohort Study
- Risks and Benefits of Nalmefene in the Treatment of Adult Alcohol Dependence: A Systematic Literature Review and Meta-Analysis of Published and Unpublished Double-Blind Randomized Controlled Trials
- World Health Organization Global Estimates and Regional Comparisons of the Burden of Foodborne Disease in 2010
- Diversity in Clinical and Biomedical Research: A Promise Yet to Be Fulfilled
Kurzy
Zvyšte si kvalifikaci online z pohodlí domova
Současné možnosti léčby obezity
nový kurzAutoři: MUDr. Martin Hrubý
Všechny kurzyPřihlášení#ADS_BOTTOM_SCRIPTS#Zapomenuté hesloZadejte e-mailovou adresu, se kterou jste vytvářel(a) účet, budou Vám na ni zaslány informace k nastavení nového hesla.
- Vzdělávání



