-
Články
Top novinky
Reklama- Vzdělávání
- Časopisy
Top články
Nové číslo
- Témata
Top novinky
Reklama- Videa
- Podcasty
Nové podcasty
Reklama- Kariéra
Doporučené pozice
Reklama- Praxe
Top novinky
ReklamaAssociations between Intimate Partner Violence and Health among Men Who Have Sex with Men: A Systematic Review and Meta-Analysis
Background:
Intimate partner violence (IPV) among men who have sex with men (MSM) is a significant problem. Little is known about the association between IPV and health for MSM. We aimed to estimate the association between experience and perpetration of IPV, and various health conditions and sexual risk behaviours among MSM.Methods and Findings:
We searched 13 electronic databases up to 23 October 2013 to identify research studies reporting the odds of health conditions or sexual risk behaviours for MSM experiencing or perpetrating IPV. Nineteen studies with 13,797 participants were included in the review. Random effects meta-analyses were performed to estimate pooled odds ratios (ORs). Exposure to IPV as a victim was associated with increased odds of substance use (OR = 1.88, 95% CIOR 1.59–2.22, I2 = 46.9%, 95% CII2 0%–78%), being HIV positive (OR = 1.46, 95% CIOR 1.26–1.69, I2 = 0.0%, 95% CII2 0%–62%), reporting depressive symptoms (OR = 1.52, 95% CIOR 1.24–1.86, I2 = 9.9%, 95% CII2 0%–91%), and engagement in unprotected anal sex (OR = 1.72, 95% CIOR 1.44–2.05, I2 = 0.0%, 95% CII2 0%–68%). Perpetration of IPV was associated with increased odds of substance use (OR = 1.99, 95% CIOR 1.33–2.99, I2 = 73.1%). These results should be interpreted with caution because of methodological weaknesses such as the lack of validated tools to measure IPV in this population and the diversity of recall periods and key outcomes in the identified studies.Conclusions:
MSM who are victims of IPV are more likely to engage in substance use, suffer from depressive symptoms, be HIV positive, and engage in unprotected anal sex. MSM who perpetrate IPV are more likely to engage in substance use. Our results highlight the need for research into effective interventions to prevent IPV in MSM, as well as the importance of providing health care professionals with training in how to address issues of IPV among MSM and the need to raise awareness of local and national support services.
Please see later in the article for the Editors' Summary
Published in the journal: . PLoS Med 11(3): e32767. doi:10.1371/journal.pmed.1001609
Category: Research Article
doi: https://doi.org/10.1371/journal.pmed.1001609Summary
Background:
Intimate partner violence (IPV) among men who have sex with men (MSM) is a significant problem. Little is known about the association between IPV and health for MSM. We aimed to estimate the association between experience and perpetration of IPV, and various health conditions and sexual risk behaviours among MSM.Methods and Findings:
We searched 13 electronic databases up to 23 October 2013 to identify research studies reporting the odds of health conditions or sexual risk behaviours for MSM experiencing or perpetrating IPV. Nineteen studies with 13,797 participants were included in the review. Random effects meta-analyses were performed to estimate pooled odds ratios (ORs). Exposure to IPV as a victim was associated with increased odds of substance use (OR = 1.88, 95% CIOR 1.59–2.22, I2 = 46.9%, 95% CII2 0%–78%), being HIV positive (OR = 1.46, 95% CIOR 1.26–1.69, I2 = 0.0%, 95% CII2 0%–62%), reporting depressive symptoms (OR = 1.52, 95% CIOR 1.24–1.86, I2 = 9.9%, 95% CII2 0%–91%), and engagement in unprotected anal sex (OR = 1.72, 95% CIOR 1.44–2.05, I2 = 0.0%, 95% CII2 0%–68%). Perpetration of IPV was associated with increased odds of substance use (OR = 1.99, 95% CIOR 1.33–2.99, I2 = 73.1%). These results should be interpreted with caution because of methodological weaknesses such as the lack of validated tools to measure IPV in this population and the diversity of recall periods and key outcomes in the identified studies.Conclusions:
MSM who are victims of IPV are more likely to engage in substance use, suffer from depressive symptoms, be HIV positive, and engage in unprotected anal sex. MSM who perpetrate IPV are more likely to engage in substance use. Our results highlight the need for research into effective interventions to prevent IPV in MSM, as well as the importance of providing health care professionals with training in how to address issues of IPV among MSM and the need to raise awareness of local and national support services.
Please see later in the article for the Editors' SummaryIntroduction
Violence by an intimate partner affects nearly one in three women globally, ranging from 16.3% in East Asia to 65.6% in central sub-Saharan Africa [1]–[3]. The associated adverse health consequences for female victims include depression, anxiety, post-traumatic stress disorder, eating disorders [4],[5], and sexual and reproductive health problems [6],[7]. However, intimate partner violence (IPV) is not exclusive to opposite-sex relationships, and there is a growing body of research highlighting the prevalence of IPV in same-sex relationships [8]–[14]. Recent reviews suggest that the prevalence in same-sex couples, in particular male–male couples, is as high as or higher than it is for women in opposite-sex relationships [15]–[18]. The reported lifetime experience of IPV in gay male relationships lies between 15.4% and 51% [9],[11],[15],[18], depending on the population studied [11],[17], the definition of “partner” or “relationship” [11], and the type of measures used [19]. Most reviews addressing of IPV in the LGBT (lesbian, gay, bisexual, and transgender) population focus on the prevalence of IPV, with limited research on the health associations of IPV [20]. The two existing reviews that explored this association [11],[17] used a narrative approach, which summarises and explains results in words rather than pooling quantitative results, and concluded that further research was needed to understand the range of health conditions associated with IPV among MSM.
A UK study on safety planning and advocacy services for men affected by IPV, found that gay and heterosexual men need different services and approaches to accessing support [21]. Insight into IPV health associations for this population will both inform the identification of opportunities for intervention, and guide the design of tailored interventions. To our knowledge this systematic review and meta-analysis is the first to quantitatively synthesise evidence on the association between exposure to IPV as a victim and a perpetrator with health conditions and sexual risk behaviours among men who have sex with men (MSM). We aimed to assess whether MSM who experience or perpetrate IPV have increased odds of common mental health disorder symptoms, eating disorder symptoms, substance misuse, sexually transmitted infections (STIs), HIV positive status, or sexual risk-taking behaviours compared with MSM who are not experiencing or perpetrating IPV.
Methods
The review followed PRISMA [22] and MOOSE [23] guidelines (see Table S1 for the PRISMA checklist). Thirteen bibliographic databases (MEDLINE, EMBASE, Global Health, PsycINFO, the Health Management Information Consortium database [HMIC], Social Policy and Practice, the Cumulative Index to Nursing and Allied Health Literature [CINAHL], the International Bibliography of the Social Sciences [IBSS], Web of Science, Africa Web, Index Medicus for South-East Asia Region [IMSEAR], Index Medicus for the Eastern Mediterranean Region [IMEMR], and Latin American and Caribbean Health Sciences Literature [LILACS]) were searched using controlled vocabulary terms and key/text words from first record to 23 October 2013. Terms for IPV and MSM were adapted from Cochrane protocols and peer-reviewed systematic reviews [24]–[27]. Terms for mental disorders were adapted from a review by Trevillion and colleagues [5]. No language restrictions were applied. Reference lists of all included studies were also searched and backward and forward citation tracking used to identify additional potentially relevant studies. Three LGBT specialised journals that featured in our searches (Journal of Homosexuality, Journal of Gay & Lesbian Social Services, and Journal of LGBT Issues in Counseling) were hand searched. Furthermore, experts were asked to identify additional studies. An example search strategy is provided in Text S1, and the protocol of the review can be found in Text S2.
Inclusion and Exclusion Criteria
The study selection process is summarised in the flowchart in Figure 1. Studies were eligible for inclusion if they (a) measured IPV in any of its forms (physical, emotional, and/or sexual); (b) reported results for men who defined themselves as gay or bisexual and/or reported having had sex with men, and who were 18 y or older; (c) were cohort studies, case-control studies, or cross-sectional studies; and (d) measured the prevalence and odds or risk of the health outcomes selected for inclusion in this review, or reported data from which these statistics could be calculated. Studies were excluded if they (a) reported on adult sexual assault or non-consensual sex outside of an intimate relationship; (b) reported IPV in a specific group that made it difficult to generalise the results to the wider population, such as IPV in the armed forces, among prison inmates, or in HIV positive individuals. Health conditions included in the review were selected based upon the most frequent outcomes associated with IPV in the broader literature [11],[20],[28]–[30]. They were classified in two groups: health conditions (depression, anxiety, and post-traumatic stress symptoms; suicide ideation and suicide attempt; substance use; eating disorders; STIs; and HIV) and sexual risk behaviours (unprotected receptive or insertive anal intercourse and number of sexual partners).
Fig. 1. Flow diagram of screened and included papers. 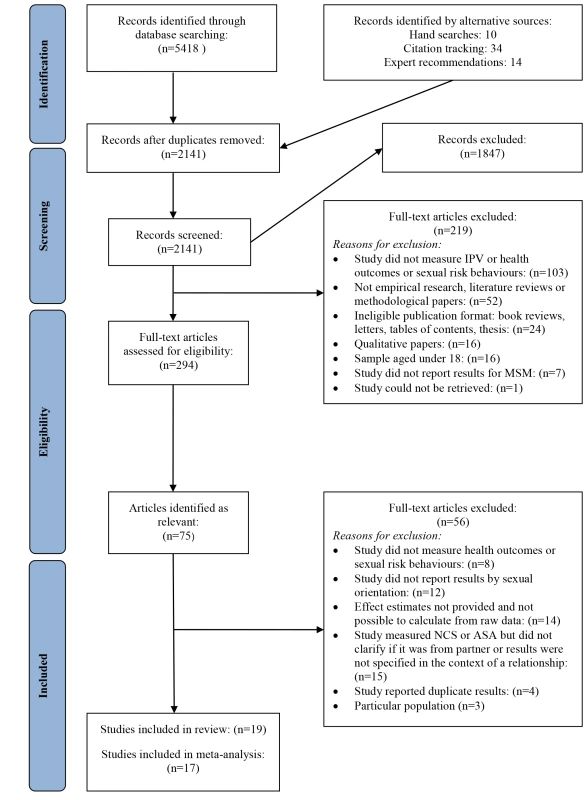
ASA, adult sexual assault; NCS, non-consensual sex. Screening and Data Extraction
AM. B. and L. J. B. screened the abstracts and full texts of potentially eligible studies. Details of the 1,848 excluded papers and reasons for exclusion were documented. Data from included papers were extracted by AM. B. and L. J. B. into a customised Excel spreadsheet. Extracted data included the following: study design; sample characteristics; definitions and measures of IPV; the health conditions and sexual risk behaviours measured; and their effect estimates and measures of uncertainty. Details about confounders controlled for were also recorded.
Quality Appraisal
The quality of each association estimate was appraised by AM. B. and L. J. B. using criteria adapted from validated tools [31] and STROBE (Strengthening the Reporting of Observational Studies in Epidemiology) [32]. An appraisal checklist for included studies was developed. The checklist provided explanatory notes for extracting each data element to ensure consistency between reviewers (see Text S3). The inter-rater agreement rate between reviewers for the quality appraisal was high (K = 0.86), and discrepancies were resolved through discussion with a third reviewer (K. M. D.).
Data Analyses
All analyses were conducted by K. M. D. and AM. B using Stata 12.0 [33]. Descriptive statistics on study characteristics and quality are presented. We computed an overall quality score (Table 1) for descriptive purposes, but in accordance with recommended practice, this was not used to weight studies in the meta-analysis [34]. Random effects meta-analysis was used to calculate the pooled prevalence of different forms of violence and to calculate pooled odds ratios (ORs) representing associations between exposure to IPV and various health outcomes and sexual risk behaviours. Where studies did not report prevalence estimates or ORs, these were calculated from raw data where possible. One study [35] reported a risk ratio, which was converted to an OR using the formula of Zhang and Kai [36]. Higgins's I2 statistic, which describes the percentage of variability in point estimates that is due to heterogeneity rather than sampling error [37], was calculated. We also calculated confidence intervals for each I2 statistic using the heterogi command in Stata [38]. Following other reviews 25%, 50%, and 75% were taken to indicate low, moderate, and high levels of heterogeneity, respectively [39],[40]. Meta-regression analyses were run in order to establish predictors of heterogeneity.
Tab. 1. Quality assessment of estimates in studies included in the review. 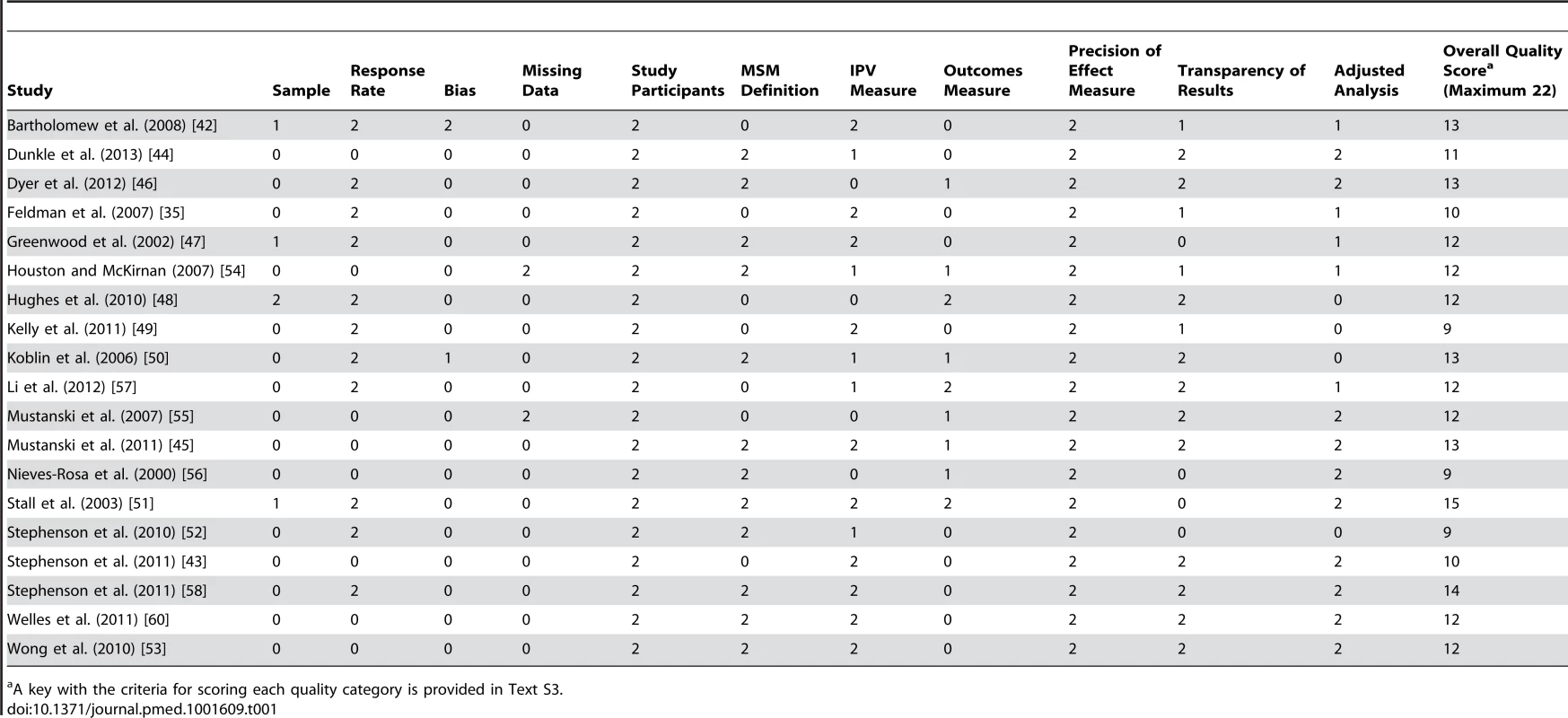
A key with the criteria for scoring each quality category is provided in Text S3. Some studies reported results in multiple publications or had multiple estimates using overlapping measures of either violence or health outcomes. To avoid double-counting participants, which can lead to falsely precise pooled estimates, we selected only the least biased estimate per study. Decisions were based on the quality criteria described above and the following algorithm: preference was given to multivariate estimates over bivariate, to where the reference group was unexposed to any violence, and to where the estimate was most precise (i.e., smallest confidence interval). To investigate small study effects and possible publication bias, we constructed contour funnel plots in Stata [41] (Figure S1). For this we used all available estimates for a given outcome (rather than choosing one per study).
Results
Study Characteristics
Nineteen studies describing 18 datasets (Greenwood et al. [47] and Stall et al. [51] are based on the same dataset) with 13,797 participants, and reporting 87 estimates, met the inclusion criteria; 17 studies were included in the meta-analysis. Sixteen studies were conducted in the US, one in Canada [42], one in South Africa [43], and one in China [44] (study characteristics are shown in Tables 2 and S2). The mean age of participants ranged from 19 [45] to 47 [46] y old. Average participation rate was 63%, with 11 studies [35],[42],[46]–[52],[57],[58] reporting it.
Tab. 2. Characteristics of studies included in the review. 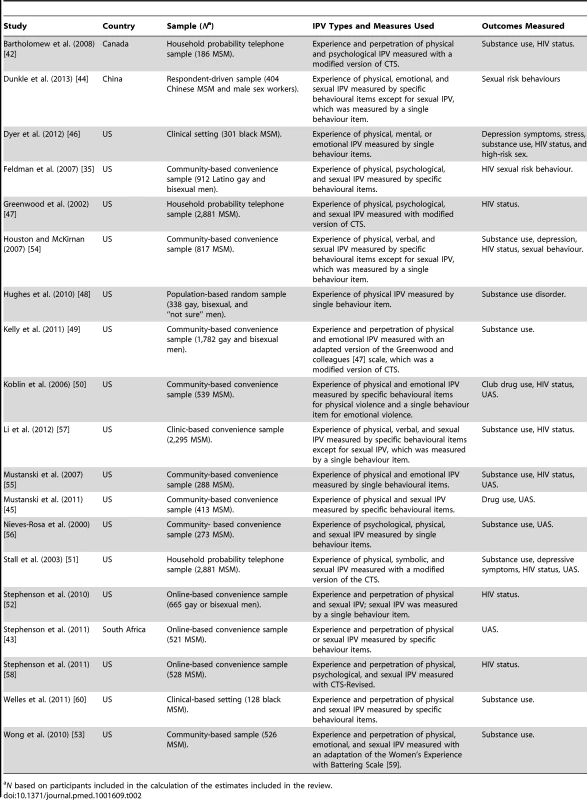
N based on participants included in the calculation of the estimates included in the review. Table 1 summarises estimates' quality. Most studies used convenience, non-probabilistic samples, with the exception of one study that used a population-based sample [48] and three studies that used random samples of particular cities in the US and Canada [42],[47],[51]. Response bias was addressed in two studies [42],[50]. Similarly, two studies [54],[55] reported their missing data policy or performed a sensitivity analysis. All the estimates reported or calculated from the raw data had uncertainty measures, and four studies [47],[51],[52],[56] did not report their non-significant results. Four studies [48]–[50],[52] did not control for confounders within the analyses, or we calculated the estimates from raw data and did not control for confounders. Confounders included a wide range of variables, with most studies controlling for age, ethnicity, level of education, substance use, and HIV status.
Only nine of 19 studies used validated self-report measures of depressive symptoms [46],[51],[54], substance use [48],[51],[54], or sexual risk behaviours [45],[48],[55],[56], or biological samples to establish HIV seropositivity [50],[51],[57]. Measures were otherwise unvalidated self-report measures for health conditions, including HIV status. Studies included in the review reported on different populations: gay only, gay and bisexual, MSM only, MSM and bisexual, and LGBT. Most (12) studies used behavioural measures to define their study populations as MSM. Seven studies [35],[42],[43],[48],[49],[55],[57] relied on self-reported sexual orientation to define their study population.
The recall times for which IPV was measured included “lifetime prevalence”, “past 5 years”, “in the last 12 months”, “in the past three months”, and “in your current relationship”. Five studies [42],[47],[49],[51],[58] reported using an adapted version of the Conflict Tactics Scale (CTS), and one [53] used an adapted version of a scale by Smith and colleagues [59]. Four studies used unique IPV measures developed by the authors that included multiple behaviours to measure all the types of IPV included in the study [35],[43],[45],[60], five studies used multiple behaviour measures for physical IPV but not for emotional or sexual violence [44],[50],[52],[54],[57], and four studies used single behaviour items to measure all types of IPV included in the study [46],[48],[55],[56]. Physical violence was measured in all 19 studies (13,812 participants). Emotional violence included verbal and psychological violence, and it was measured in 14 studies [35],[42],[44],[46],[47],[49]–[51],[53]–[58] (11,732 participants), and sexual violence was measured in 13 studies [35],[43],[44],[45],[47],[51]–[54],[56]–[58],[60] (10,363 participants).
Intimate Partner Violence Victimisation: Prevalence and Health Associations
Combined measures of any lifetime violence (physical, sexual, or emotional) were reported in six studies [35],[50],[53]–[56] with 3,355 participants. Estimates ranged from 32% [54] to 82% [53], with a pooled prevalence of 48% (95% CIp 31.23–64.99) and a high level of heterogeneity between pooled estimates (I2 = 95.7, 95% CII2 92%–98%). Removal of the outlying estimate [53] did not improve heterogeneity. When asking about experience of any kind of IPV in the last 5 y, a pooled prevalence of 31.95% (95% CIp 19.32–44.58) in four studies [44], with 7,362 participants was found. Estimates ranged from 16% to 51%, and there was a high level of heterogeneity between estimates (I2 = 99.3, 95% CI2 99%–100%) (Table 3). Eight studies included prevalence measures of any type of IPV victimisation [58],[60], physical violence only [48], or a combination of two types of violence [43],[45],[46],[50],[52], with various recall periods.
Tab. 3. Pooled prevalence for IPV victimisation. 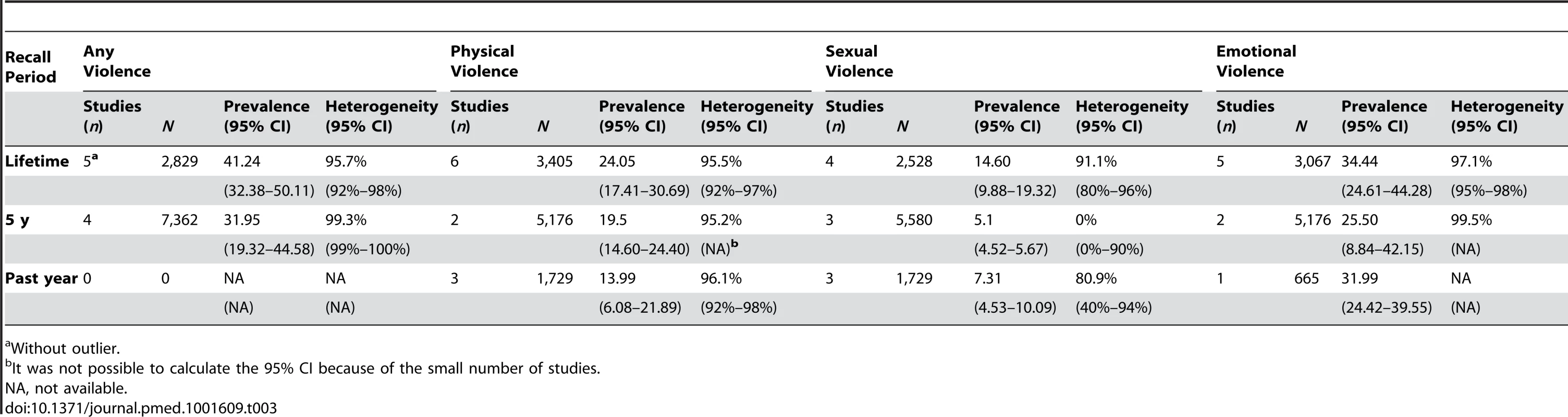
Without outlier. Estimates of the association between IPV victimisation and substance use were provided in nine studies [46],[48]–[51],[53],[54],[57],[60] that included 9,607 MSM who had been exposed to any kind of IPV and had consumed different kinds of substances (Figure 2). We found that exposure to IPV was associated with increased odds of substance use, with an OR for pooled estimates of 1.88, (95% CIOR 1.59–2.22), but with moderate heterogeneity between studies (I2 = 46.9%, 95% CII2 0%–78%) (Table 4). In order to investigate sources of heterogeneity for this meta-analysis we ran meta-regressions to test the impact of IPV modality and type of drug consumed on heterogeneity. Our results showed that none of these variables explained the heterogeneity (Table 5).
Fig. 2. Meta-analysis of the association between IPV and health outcomes and sexual risk behaviours in MSM who are victims of IPV. 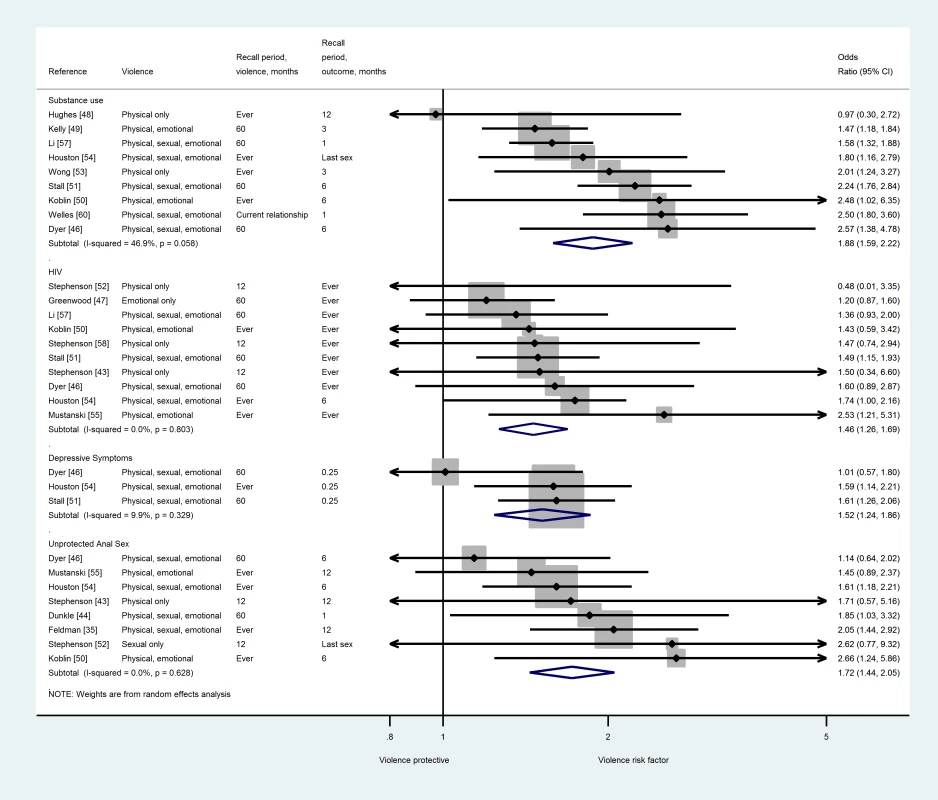
Tab. 4. Random-effects pooled odds ratios for health associations (victimisation and perpetration). 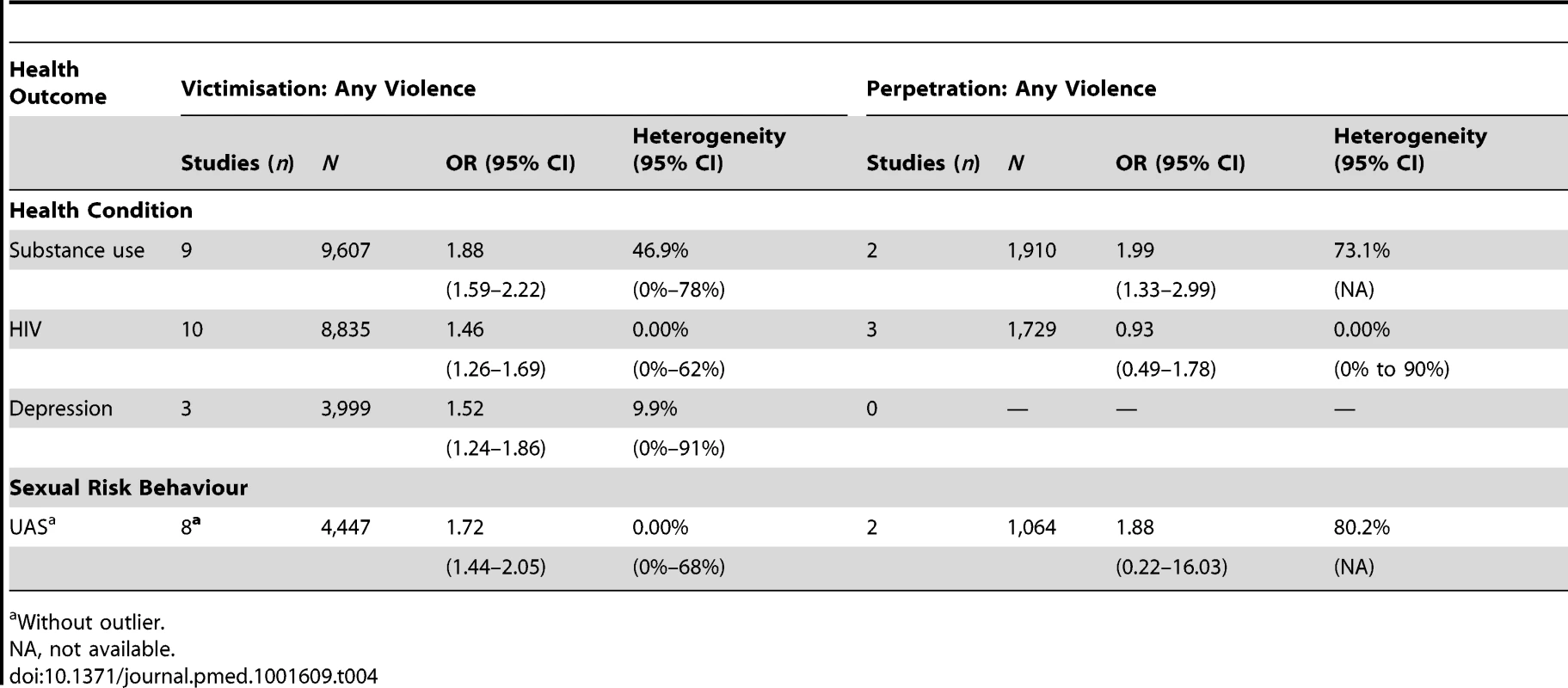
Without outlier. Tab. 5. Meta-regression exploring potential sources of heterogeneity in substance use meta-analysis. 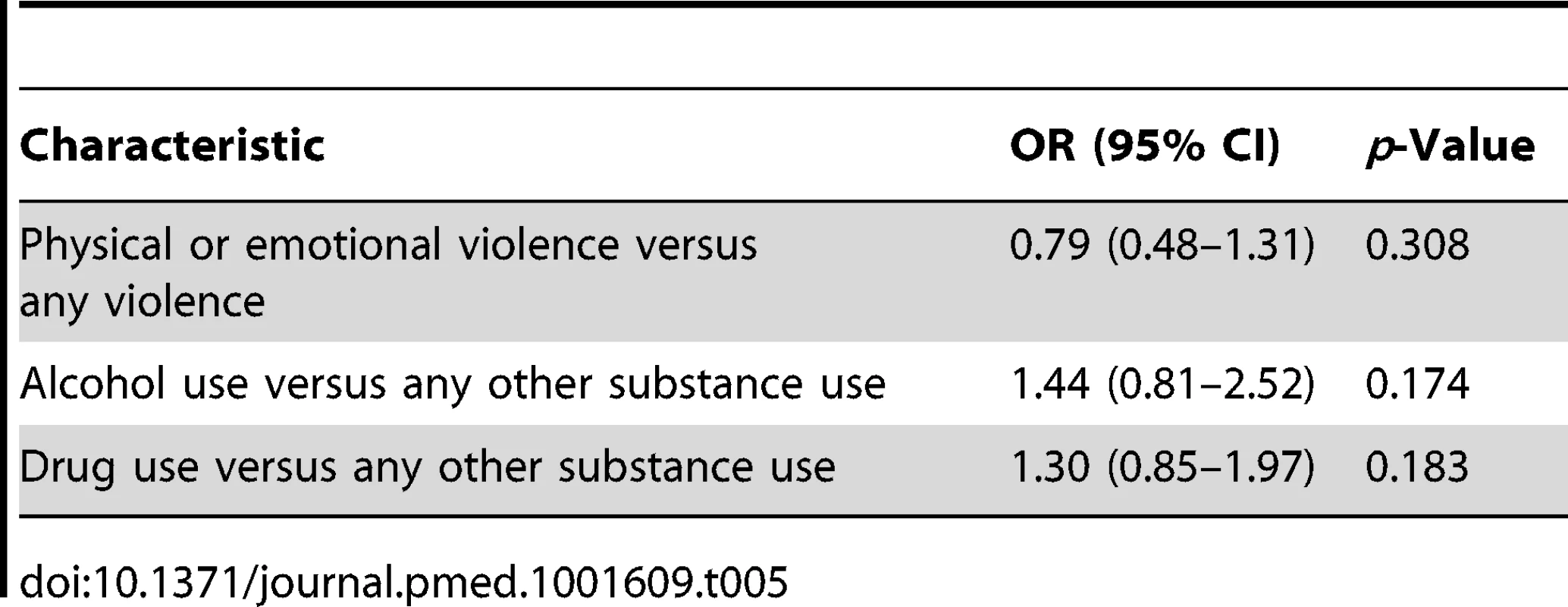
Estimates for the odds of HIV were provided in ten studies [43],[46],[47],[50]–[52],[54],[55],[57],[58] that included 8,835 MSM who had been exposed to any kind of IPV (Figure 2). Exposure to IPV was associated with a positive HIV status, with a pooled OR of 1.46 (95% CIOR 1.26–1.69) and high consistency between pooled estimates (I2 = 0.0%, 95% CII2 0%–62%) (Table 4).
MSM exposed to any kind of violence also had increased odds of reporting depression symptoms. Depression symptoms were measured in three studies including 3,999 MSM using the Center for Epidemiologic Studies Depression Scale (CESD) [46],[51],[54], with a pooled OR of 1.52 (95% CIOR 1.24–1.86, I2 = 9.9%, 95% CII2 0%–91%) (Figure 2; Table 4). Estimates for unprotected anal sex (UAS) were calculated in nine studies [35],[44]–[46],[50],[52],[54],[56],[58]. After running the meta-analysis and removing an outlier study [56], we kept eight estimates with a total population of 4,447 MSM (Figure 2). We found that exposure to IPV was associated with increased odds of engaging in UAS (pooled OR = 1.72, 95% CIOR 1.44–2.05, I2 = 0.0%, 95% CII2 0%–68%) (Table 4). Contour-enhanced funnel plots showed no evidence of publication bias for substance use, HIV, and UAS results (Figure S1). In these plots studies are missing from the left side of the graph, but across areas of both statistical significance and non-significance. This suggests that publication bias is not responsible for funnel plot asymmetry [41]. The small number of studies that could be pooled for the depression symptoms meta-analysis precluded the use of such plots [46],[61],[62] for this health correlate.
Intimate Partner Violence Perpetration: Prevalence and Health Associations
Prevalence rates of IPV perpetration among MSM were reported in seven studies [42],[43],[49],[52],[53],[58],[60] with a total population of 4,336 MSM. These studies reported prevalence for different types of violence and different recall periods, precluding the possibility of meta-analysis. Estimates for the odds of substance use among perpetrators were provided in two studies [49],[60] that included 1,910 MSM who disclosed perpetration of IPV. Perpetration of IPV was associated with increased odds of substance use (pooled OR = 1.99, 95% CIOR 1.33–2.99) (Table 4). The results showed moderate heterogeneity (I2 = 73.1%). Due to the small number of studies, CII2 could not be calculated for this result. Likewise, it was not possible to assess publication bias. No other significant associations between IPV perpetration and health outcomes or sexual risk behaviours were found when conducting the meta-analyses (Table 4).
Discussion
Main Findings
Our findings suggest that IPV victimisation is prevalent among MSM. We also found evidence that exposure to IPV as a victim is associated with increased odds of substance use, depressive symptoms, being HIV positive, and UAS among MSM. Relatively few studies measured perpetration of IPV, but these studies suggested an association between IPV perpetration and substance use. However, these results should be interpreted with caution given the methodological limitations in the included studies.
The associations of IPV with both UAS and being HIV positive suggested in this review are consistent with the existence of a causal pathway. Emotional, physical, or sexual violence (or a combination of all three) could increase risk for UAS [28],[63], which in turn could increase risk for HIV infection. Further research is needed to investigate this link, including the specific associations between different types of IPV and HIV status. In particular, the intersection of IPV and HIV seropositivity might be problematic. MSM may fear partner violence following disclosure of HIV status and may experience difficulties adhering to treatment regimes and accessing health services. Sexual health and HIV services are opportune points of intervention for MSM affected by IPV [64], and these findings underscore the need for these services to provide comprehensive sexual health care and awareness of repeat STI or positive HIV status as indicators for IPV and vice versa among the MSM population. Our findings on the association of substance use and depression symptoms with IPV confirm previous findings [48],[65] and also highlight the need for mental health and substance misuse services to address IPV issues. Men who are depressed or engage in heavy substance use and are also part of a violent relationship might find it hard to seek help, to end the relationship, or adhere to prescribed treatment.
Strengths and Limitations of This Review
To our knowledge this is the first systematic review to quantitatively summarise the associations between IPV victimisation and perpetration with various health conditions in MSM. Our review entailed extensive searches of the international research literature without any time or language restrictions, and most of our results were consistent and showed no publication bias. Despite this, the review has some limitations. First, prevalence results are only for studies included in the review and should be interpreted with caution. Second, we did not contact authors for additional data. Third, for studies that did not provide ORs, it was not possible to control for confounders when ORs were calculated from raw data [48]–[50],[52].
Limitations of Included Studies
The included studies had a number of methodological weaknesses, and the search produced few published studies addressing the association between IPV and health among MSM. Similar to other meta-analyses with a low number of studies, confidence intervals for the heterogeneity estimates were very wide [66]. This means that if further studies were to be conducted on the associations between IPV and health outcomes among MSM the results could be more homogenous or more heterogeneous. Heterogeneity in our review could have been due to different factors such as different recall periods, types of IPV included, the use of convenience samples, different definitions of sexual identity, and the quality of tools used to assess IPV and health outcomes. Unfortunately, tests for sources of heterogeneity have low power with small numbers of studies.
Furthermore, all studies included were cross-sectional, and there was a lack of uniformity regarding the recall periods for IPV and key outcomes, which made it impossible to assess the temporality of the associations. Most studies used convenience, non-probabilistic samples, which makes it difficult to generalise the results to the wider population. Few studies used validated tools to measure IPV, health outcomes, or sexual risk behaviours. HIV measurement relied mainly on self-report, which can provide a biased measure of HIV prevalence. There was a lack of consistency in the types of IPV measured in the studies; however, most authors used either a modified version of CTS or specific behavioural acts to measure IPV. Studies used scales that have been validated for heterosexual samples, which did not necessarily capture MSM's experience of IPV, and most studies used an author's IPV measure without discussing issues of validity or psychometric characteristics. Measures of sexual violence were limited and usually included a single behaviour item asking about forced or unwanted sex, thus potentially resulting in an underestimation of this type of abuse. Additionally, most of the IPV was measured without considering contextual factors such as the frequency with which the abuse occurred or its perceived impact [67]. A step towards a validated tool for IPV among MSM in the US has been taken by Stephenson and Finneran [19], which may be useful in future studies.
Another limitation arises from the fact that we included studies that used different kinds of sexual identities (i.e., self-recognised as gay or bisexual, reporting same-sex sexual encounters, or both). Men's experiences of IPV and the impact it has on their health may be affected by their identification as gay or not, which in turn might be related to their levels of internalised homophobia. Further studies including a differentiated analysis by sexual identity and sexual behaviour might help to understand these relationships better. One such study found that men who identified themselves as gay had a higher prevalence of IPV compared to men who disclosed same-sex sexual behaviour, but did not identify themselves as gay or bisexual [18]. The term “partner” was not clearly operationalised in many of the studies. Studies measuring IPV often define “partner” as someone with whom the respondent has had sex. Therefore, some studies may have captured violence and abuse experienced in the context of casual encounters. This may have diluted the association between health outcomes and IPV because it is less likely that these relationships are characterised by a pattern of abuse and coercive, controlling behaviour that escalates over time [68],[69]. Moreover, the role of sexual agreements, which can be monogamous or non-monogamous [70] and are common among gay couples [70],[71], was missing from the studies identified. Lastly, there was a dearth of research relating to MSM in low - and middle-income countries [72], where MSM are at elevated risk of HIV infection and in some countries might face serious discrimination and multiple barriers to accessing health care [73].
Implications for Research
Future research should include national studies using probability-based samples to establish more reliable estimates of the prevalence of different types of IPV experience and perpetration amongst MSM. Further studies should try to establish the impact of particular (more common) forms of IPV among MSM in order to clarify the connections between specific forms of violence and health conditions. Additionally, the sexual orientation and identity of participants should be clearly established, and analysis should differentiate between the two. This will help determine whether the factors that drive IPV and the consequences of IPV are different across men who identify as gay or bisexual compared with men who have same-sex sexual behaviours but do not identify themselves as gay or bisexual.
Longitudinal studies are needed to establish the causal pathway between IPV and adverse health outcomes and sexual risk behaviours. The concepts of bi-directional violence or reciprocity of violence, common in the literature on IPV in MSM, should be taken into consideration in future research. Future studies should also use measurement tools validated for MSM populations and prospective biological measures of STIs and HIV. Other health outcomes and health risk behaviours for which we did not find any studies, such as eating disorders, repeated STIs, sexual compulsivity [74], and concurrent sexual partnerships [70],[71],[75], may also be important in understanding the impact that IPV has for this particular population. Furthermore, in view of the increasing evidence that the chronic stress of both childhood and adulthood abuse is associated with inflammatory markers that increase the risk of long term diseases including cardiovascular disease and diabetes [76],[77], longer term adverse health outcomes are also possible and should be measured in future studies.
Implications for Practice
The findings of this review underscore the need for health professionals to be aware that IPV is a problem for the MSM population and to carefully assess for IPV and refer affected individuals to appropriate support services in the community. Therefore, same-sex IPV awareness training for health professionals caring for this population is needed. This training should include developing skills for asking about IPV [78],[79], dealing with partner notification and safety issues, and making referrals to specialist IPV support services [80]. However, the availability of local and national support services for MSM experiencing or perpetrating IPV varies considerably internationally, and there are very limited data available on their effectiveness [81]. From a health services perspective, adequate protocols for dealing with IPV should be in place, ensuring that all primary and secondary health care services provide holistic care. Addressing IPV is a global health priority, and rigorous evaluations of the feasibility and effectiveness of health service interventions for IPV amongst MSM are needed to inform future policy and practice.
Supporting Information
Zdroje
1. Garcia-MorenoC, JansenHAFM, EllsbergM, HeiseL, WattsCH (2006) Prevalence of intimate partner violence: findings from the who multi-country study on women's health and domestic violence. Lancet 368 : 1260–1269.
2. Walters M, Chen J, Breiding M (2013) The National Intimate Partner and Sexual Violence Survey (NISVS): 2010 findings on victimization by sexual orientation. Atlanta (Georgia): US Centers for Disease Control and Prevention National Center for Injury Prevention and Control.
3. DevriesKM, MakJYT, García-MorenoC, PetzoldM, ChildJC, et al. (2013) The global prevalence of intimate partner violence against women. Science 340 : 1527–1528.
4. EllsbergM, JansenHAFM, HeiseL, WattsCH, Garcia-MorenoC (2008) Intimate partner violence and women's physical and mental health in the who multi-country study on women's health and domestic violence: an observational study. Lancet 371 : 1165–1172.
5. TrevillionK, OramS, FederG, HowardLM (2012) Experiences of domestic violence and mental disorders: a systematic review and meta-analysis. PLoS ONE 7: e51740.
6. SharpsPW, LaughonK, GiangrandeSK (2007) Intimate partner violence and the childbearing year: maternal and infant health consequences. Trauma Violence Abuse 8 : 105–116.
7. CokerAL (2007) Does physical intimate partner violence affect sexual health? A systematic review. Trauma Violence Abuse 8 : 149–177.
8. AlexanderCJ (2002) Violence in gay and lesbian relationships. J Gay Lesbian Soc Serv 14 : 95–98.
9. Henderson L (2003) Prevalence of domestic violence among lesbians and gay men. London: Sigma Research.
10. MakWW, ChongES, KwongMM (2010) Prevalence of same-sex intimate partner violence in Hong Kong. Public Health 124 : 149–152.
11. NowinskiSN, BowenE (2012) Partner violence against heterosexual and gay men: prevalence and correlates. Aggress Violent Behav 17 : 36–52.
12. OwenSS, BurkeTW (2004) An exploration of prevalence of domestic violence in same-sex relationships. Psychol Rep 95 : 129–132.
13. BarrettBJ, St. PierreM (2013) Intimate partner violence reported by lesbian-, gay-, and bisexual-identified individuals living in Canada: an exploration of within-group variations. J Gay Lesbian Soc Serv 25 : 1–23.
14. ChongESK, MakWWS, KwongMMF (2013) Risk and protective factors of same-sex intimate partner violence in Hong Kong. J Interpers Violence 28 : 1476–1497.
15. StanleyJL, BartholomewK, TaylorT, OramD, LandoltM (2006) Intimate violence in male same-sex relationships. J Fam Violence 21 : 31–42.
16. MerrillGS, WolfeVA (2000) Battered gay men: an exploration of abuse, help seeking, and why they stay. J Homosex 39 : 1–30.
17. FinneranC, StephensonR (2013) Intimate partner violence among men who have sex with men. A systematic review. Trauma Violence Abuse 14 : 168–185.
18. GoldbergNG, MeyerIH (2013) Sexual orientation disparities in history of intimate partner violence: results from the California Health Interview Survey. J Interpers Violence 28 : 1109–1118.
19. StephensonR, FinneranC (2013) The IPV-GBM scale: a new scale to measure intimate partner violence among gay and bisexual men. PLoS ONE 8: e62592.
20. RandleAA, GrahamCA (2011) A review of the evidence on the effects of intimate partner violence on men. Psychol Men Masc 12 : 97–111.
21. Robinson A, Rowland J (2007) What do men want? Safe Domestic Abuse Q 22 : 4–76. London: Women's Aid.
22. MoherD, LiberatiA, TetzlaffJ, AltmanDG, ThePG (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA Statement. PLoS Med 6: e1000097.
23. StroupDF, BerlinJA, MortonSC, OlkinI, WilliamsonGD, et al. (2000) Meta-analysis of observational studies in epidemiology: A proposal for reporting. JAMA 283 : 2008–2012.
24. ZhangL, QianH-z, BlevinsML, YinL, RuanY, et al. (2011) Internet-based behavioral interventions for preventing HIV infection in men who have sex with men (MSM). Cochrane Database Syst Rev 2011: CD009525 doi:10.1002/14651858.CD009525
25. RamsayJ, CarterY, DavidsonL, DunneD, EldridgeS, et al. (2009) Advocacy interventions to reduce or eliminate violence and promote the physical and psychosocial well-being of women who experience intimate partner abuse. Cochrane Database Syst Rev 2009: CD005043 doi:10.1002/14651858.CD005043.pub2
26. JohnsonWD, DiazRM, FlandersWD, GoodmanM, HillAN, et al. (2008) Behavioral interventions to reduce risk for sexual transmission of HIV among men who have sex with men. Cochrane Database Syst Rev 2008: CD001230 doi:10.1002/14651858.CD001230.pub2
27. CoulthardP, YongSL, AdamsonL, WarburtonA, WorthingtonHV, et al. (2010) Domestic violence screening and intervention programmes for adults with dental or facial injury. Cochrane Database Syst Rev 2010: CD004486 doi:10.1002/14651858.CD004486.pub3
28. RelfMV (2001) Battering and HIV in men who have sex with men: a critique and synthesis of the literature. J Assoc Nurses AIDS Care 12 : 41–48.
29. MurrayCE, MobleyAJ, BufordAP, Seaman-DeJohnMM (2006) Same-sex intimate partner violence: dynamics, social context, and counseling implications. J LGBT Issues Couns 1 : 7–30.
30. McClennenJC (2005) Domestic violence between same-gender partners: recent findings and future research. J Interpers Violence 20 : 149–154.
31. DownsSH, BlackN (1998) The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non-randomised studies of health care interventions. J Epidemiol Community Health 52 : 377–384.
32. von ElmE, AltmanDG, EggerM, PocockSJ, GøtzschePC, et al. (2007) The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet 370 : 1453–1457.
33. StataCorp (2011) Stata statistical software: release 12 version [computer program]. College Station (Texas): StataCorp.
34. Alderson P, Green S, Higgins J (2004) Cochrane handbook for systematic reviews of interventions, version 4.2.2 (updated March 2004). Oxford: Cochrane Collaboration.
35. FeldmanMB, DiazRM, ReamGL, El-BasselN (2007) Intimate partner violence and HIV sexual risk behavior among Latino gay and bisexual men. J LGBT Health Res 3 : 9–19.
36. ZhangJ, KaiFY (1998) What's the relative risk? JAMA 280 : 1690–1691.
37. HigginsJ, ThompsonSG (2002) Quantifying heterogeneity in a meta-analysis. Stat Med 21 : 1539–1558.
38. Nicola O, Matteo B, Julian H, Iain B (2005) Heterogi: Stata module to quantify heterogeneity in a meta-analysis. S449201. Boston: Boston College Department of Economics.
39. FazelS, GulatiG, LinsellL, GeddesJR, GrannM (2009) Schizophrenia and violence: systematic review and meta-analysis. PLoS Med 6: e1000120.
40. ChengY-J, LiuZ-H, YaoF-J, ZengW-T, ZhengD-D, et al. (2013) Current and former smoking and risk for venous thromboembolism: a systematic review and meta-analysis. PLoS Med 10: e1001515.
41. PalmerTM, PetersJL, SuttonAJ, MorenoSG (2008) Contour-enhanced funnel plots for meta-analysis. Stata J 8 : 242–254.
42. BartholomewK, ReganKV, OramD, WhiteMA (2008) Correlates of partner abuse in male same-sex relationships. Violence Vict 23 : 344–360.
43. StephensonR, de VouxA, SullivanPS (2011) Intimate partner violence and sexual risk-taking among men who have sex with men in south africa. West J Emerg Med 12 : 343–347.
44. DunkleKL, WongFY, NehlEJ, LinL, HeN, et al. (2013) Male-on-male intimate partner violence and sexual risk behaviors among money boys and other men who have sex with men in shanghai, china. Sex Transm Dis 40 : 362–365.
45. MustanskiB, NewcombME, ClerkinEM (2011) Relationship characteristics and sexual risk-taking in young men who have sex with men. Health Psychol 30 : 597–605.
46. DyerTP, ShoptawS, GuadamuzTE, PlankeyM, KaoU, et al. (2012) Application of syndemic theory to black men who have sex with men in the Multicenter AIDS Cohort Study. J Urban Health 89 : 697–708.
47. GreenwoodGL, RelfMV, HuangB, PollackLM, CancholaJA, et al. (2002) Battering victimization among a probability-based sample of men who have sex with men. Am J Public Health 92 : 1964–1969.
48. HughesT, McCabeSE, WilsnackSC, WestBT, BoydCJ (2010) Victimization and substance use disorders in a national sample of heterosexual and sexual minority women and men. Addiction 105 : 2130–2140.
49. KellyBC, IzienickiH, BimbiDS, ParsonsJT (2011) The intersection of mutual partner violence and substance use among urban gays, lesbians, and bisexuals. Deviant Behav 32 : 379–404.
50. KoblinBA, TorianL, XuG, GuilinV, MakkiH, et al. (2006) Violence and HIV-related risk among young men who have sex with men. AIDS Care 18 : 961–967.
51. StallR, MillsTC, WilliamsonJ, HartT, GreenwoodG, et al. (2003) Association of co-occurring psychosocial health problems and increased vulnerability to HIV/AIDS among urban men who have sex with men. Am J Public Health 93 : 939–942.
52. StephensonR, KhosropourC, SullivanP (2010) Reporting of intimate partner violence among men who have sex with men in an online survey. West J Emerg Med 11 : 242–246.
53. WongCF, WeissG, AyalaG, KipkeMD (2010) Harassment, discrimination, violence, and illicit drug use among young men who have sex with men. AIDS Educ Prev 22 : 286–298.
54. HoustonE, McKirnanDJ (2007) Intimate partner abuse among gay and bisexual men: risk correlates and health outcomes. J Urban Health 84 : 681–690.
55. MustanskiB, GarofaloR, HerrickA, DonenbergG (2007) Psychosocial health problems increase risk for HIV among urban young men who have sex with men: preliminary evidence of a syndemic in need of attention. Ann Behav Med 34 : 37–45.
56. Nieves-RosaLE, Carballo-DieguezA, DolezalC (2000) Domestic abuse and HIV-risk behavior in Latin American men who have sex with men in New York City. J Gay Lesbian Soc Serv 11 : 77–90.
57. LiY, BakerJJ, KorostyshevskiyVR, SlackRS, PlankeyMW (2012) The association of intimate partner violence, recreational drug use with HIV seroprevalence among msm. AIDS Behav 16 : 491–498.
58. StephensonR, RentschC, SalazarLF, SullivanPS (2011b) Dyadic characteristics and intimate partner violence among men who have sex with men. West J Emerg Med 12 : 324–332.
59. SmithPH, EarpJA, DeVellisR (1994) Measuring battering: development of the Women's Experience with Battering (WEB) Scale. Womens Health 1 : 273–288.
60. WellesSL, CorbinTJ, RichJA, ReedE, RajA (2011) Intimate partner violence among men having sex with men, women, or both: early-life sexual and physical abuse as antecedents. J Community Health 36 : 477–485.
61. HayashinoY, NoguchiY, FukuiT (2005) Systematic evaluation and comparison of statistical tests for publication bias. J Epidemiol 15 : 235–243.
62. Glasziou P, Irwig L, Bain C, Colditz G (2001) Systematic reviews in health care: a practical guide. Cambridge: Cambridge University Press.
63. ValentineSE, PantaloneDW (2013) Correlates of perceptual and behavioral definitions of abuse in HIV-positive sexual minority men. Psychol Trauma 5 : 417–425.
64. UK Department of Health (2013) A framework for sexual health improvement in England. Available: https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/142592/9287-2900714-TSO-SexualHealthPolicyNW_ACCESSIBLE.pdf. Accessed 9 November 2013.
65. SiemieniukRAC, MillerP, WoodmanK, KoK, KrentzHB, et al. (2013) Prevalence, clinical associations, and impact of intimate partner violence among HIV-infected gay and bisexual men: a population-based study. HIV Med 14 : 293–302.
66. IoannidisJP, PatsopoulosNA, EvangelouE (2007) Uncertainty in heterogeneity estimates in meta-analyses. BMJ 335 : 914.
67. Donovan C, Hester M, Holmes J, McCarry M (2006) Comparing domestic abuse in same sex and heterosexual relationships. Available: http://www.bris.ac.uk/sps/research/projects/completed/2006/rc1307/rc1307finalreport.pdf. Sunderland (UK): University of Sunderland. Accessed 15 July 2013.
68. Stark E (2007) Coercive control: how men entrap women in personal life. Oxford: Oxford University Press.
69. JohnsonMP, LeoneJM (2005) The differential effects of intimate terrorism and situational couple violence findings from the national violence against women survey. J Fam Issues 26 : 322–349.
70. ParsonsJT, StarksTJ, DuBoisS, GrovC, GolubSA (2013) Alternatives to monogamy among gay male couples in a community survey: implications for mental health and sexual risk. Arch Sex Behav 42 : 303–312.
71. ParsonsJT, StarksTJ, GamarelKE, GrovC (2012) Non-monogamy and sexual relationship quality among same-sex male couples. J Fam Psychol 26 : 669.
72. FinneranC, ChardA, SineathC, SullivanP, StephensonR (2012) Intimate partner violence and social pressure among gay men in six countries. West J Emerg Med 13 : 260–271.
73. BaralS, SifakisF, CleghornF, BeyrerC (2007) Elevated risk for HIV infection among men who have sex with men in low - and middle-income countries 2000–2006: a systematic review. PLoS Med 4: e339.
74. StarksTJ, GrovC, ParsonsJT (2013) Sexual compulsivity and interpersonal functioning: sexual relationship quality and sexual health in gay relationships. Health Psychol 32 : 1047–1056.
75. GrovC, StarksTJ, RendinaHJ, ParsonsJ (2012) Rules about casual sex partners, relationship satisfaction, and HIV risk in partnered gay and bisexual men. J Sex Marital Ther E-pub ahead of print. doi:10.1080/0092623X.2012.691948
76. Bertone-JohnsonER, WhitcombBW, MissmerSA, KarlsonEW, Rich-EdwardsJW (2012) Inflammation and early-life abuse in women. Am J Prev Med 43 : 611–620.
77. OutD, HallRJ, GrangerDA, PageGG, WoodsSJ (2012) Assessing salivary C-reactive protein: longitudinal associations with systemic inflammation and cardiovascular disease risk in women exposed to intimate partner violence. Brain Behav Immun 26 : 543–551.
78. Bacchus L, Aston G, Torres Vitolas C, Jordan P, et al. (2007) A theory-based evaluation of a multi-agency domestic violence service based in maternity and genitourinary services at Guys and St Thomas NHS Foundation Trust. London: Kings College London.
79. Torres-VitolasC, BacchusLJ, AstonG (2010) A comparison of the training needs of maternity and sexual health professionals in a London teaching hospital with regards to routine enquiry for domestic abuse. Public Health 124 : 472–478.
80. Wood S, Bellis MA, Watts C (2010) Intimate partner violence. A review of evidence for prevention from the UK Focal Point for Violence and Injury Prevention. Available: http://www.eviper.org.uk/downloads/intemate_partner.pdf. Accessed 8 January 2014.
81. National Institute for Health and Care Excellence (2014) Domestic violence and abuse. Identification and prevention. London: National Institute for Health and Care Excellence. Available: http://guidance.nice.org.uk/PHG/44#tab1.
Štítky
Interní lékařství
Článek vyšel v časopisePLOS Medicine
Nejčtenější tento týden
2014 Číslo 3- Berberin: přírodní hypolipidemikum se slibnými výsledky
- Léčba bolesti u seniorů
- Příznivý vliv Armolipidu Plus na hladinu cholesterolu a zánětlivé parametry u pacientů s chronickým subklinickým zánětem
- Červená fermentovaná rýže účinně snižuje hladinu LDL cholesterolu jako vhodná alternativa ke statinové terapii
- Jak postupovat při výběru betablokátoru − doporučení z kardiologické praxe
-
Všechny články tohoto čísla
- How Can Journals Respond to Threats of Libel Litigation?
- and Water, Sanitation, and Hygiene: A Committed Relationship
- Representation and Misrepresentation of Scientific Evidence in Contemporary Tobacco Regulation: A Review of Tobacco Industry Submissions to the UK Government Consultation on Standardised Packaging
- Building Research Capacity in Africa: Equity and Global Health Collaborations
- Associations between Intimate Partner Violence and Health among Men Who Have Sex with Men: A Systematic Review and Meta-Analysis
- Active or Passive Exposure to Tobacco Smoking and Allergic Rhinitis, Allergic Dermatitis, and Food Allergy in Adults and Children: A Systematic Review and Meta-Analysis
- The Effectiveness of Community Action in Reducing Risky Alcohol Consumption and Harm: A Cluster Randomised Controlled Trial
- Assessing Causality in the Association between Child Adiposity and Physical Activity Levels: A Mendelian Randomization Analysis
- The Impact of Pyrethroid Resistance on the Efficacy of Insecticide-Treated Bed Nets against African Anopheline Mosquitoes: Systematic Review and Meta-Analysis
- Lung Function and Incidence of Chronic Obstructive Pulmonary Disease after Improved Cooking Fuels and Kitchen Ventilation: A 9-Year Prospective Cohort Study
- Early Experiences Implementing Pre-exposure Prophylaxis (PrEP) for HIV Prevention in San Francisco
- The Role of Viral Introductions in Sustaining Community-Based HIV Epidemics in Rural Uganda: Evidence from Spatial Clustering, Phylogenetics, and Egocentric Transmission Models
- PLOS Medicine
- Archiv čísel
- Aktuální číslo
- Informace o časopisu
Nejčtenější v tomto čísle- and Water, Sanitation, and Hygiene: A Committed Relationship
- Representation and Misrepresentation of Scientific Evidence in Contemporary Tobacco Regulation: A Review of Tobacco Industry Submissions to the UK Government Consultation on Standardised Packaging
- The Impact of Pyrethroid Resistance on the Efficacy of Insecticide-Treated Bed Nets against African Anopheline Mosquitoes: Systematic Review and Meta-Analysis
- The Role of Viral Introductions in Sustaining Community-Based HIV Epidemics in Rural Uganda: Evidence from Spatial Clustering, Phylogenetics, and Egocentric Transmission Models
Kurzy
Zvyšte si kvalifikaci online z pohodlí domova
Současné možnosti léčby obezity
nový kurzAutoři: MUDr. Martin Hrubý
Všechny kurzyPřihlášení#ADS_BOTTOM_SCRIPTS#Zapomenuté hesloZadejte e-mailovou adresu, se kterou jste vytvářel(a) účet, budou Vám na ni zaslány informace k nastavení nového hesla.
- Vzdělávání



