-
Články
Top novinky
Reklama- Vzdělávání
- Časopisy
Top články
Nové číslo
- Témata
Top novinky
Reklama- Videa
- Podcasty
Nové podcasty
Reklama- Kariéra
Doporučené pozice
Reklama- Praxe
Top novinky
ReklamaAssociations between Intimate Partner Violence and Termination of Pregnancy: A Systematic Review and Meta-Analysis
Background:
Intimate partner violence (IPV) and termination of pregnancy (TOP) are global health concerns, but their interaction is undetermined. The aim of this study was to determine whether there is an association between IPV and TOP.Methods and Findings:
A systematic review based on a search of Medline, Embase, PsycINFO, and Ovid Maternity and Infant Care from each database's inception to 21 September 2013 for peer-reviewed articles of any design and language found 74 studies regarding women who had undergone TOP and had experienced at least one domain (physical, sexual, or emotional) of IPV. Prevalence of IPV and association between IPV and TOP were meta-analysed. Sample sizes ranged from eight to 33,385 participants. Worldwide, rates of IPV in the preceding year in women undergoing TOP ranged from 2.5% to 30%. Lifetime prevalence by meta-analysis was shown to be 24.9% (95% CI 19.9% to 30.6%); heterogeneity was high (I2>90%), and variation was not explained by study design, quality, or size, or country gross national income per capita. IPV, including history of rape, sexual assault, contraceptive sabotage, and coerced decision-making, was associated with TOP, and with repeat TOPs. By meta-analysis, partner not knowing about the TOP was shown to be significantly associated with IPV (pooled odds ratio 2.97, 95% CI 2.39 to 3.69). Women in violent relationships were more likely to have concealed the TOP from their partner than those who were not. Demographic factors including age, ethnicity, education, marital status, income, employment, and drug and alcohol use showed no strong or consistent mediating effect. Few long-term outcomes were studied. Women welcomed the opportunity to disclose IPV and be offered help. Limitations include study heterogeneity, potential underreporting of both IPV and TOP in primary data sources, and inherent difficulties in validation.Conclusions:
IPV is associated with TOP. Novel public health approaches are required to prevent IPV. TOP services provide an opportune health-based setting to design and test interventions.
Please see later in the article for the Editors' Summary
Published in the journal: . PLoS Med 11(1): e32767. doi:10.1371/journal.pmed.1001581
Category: Research Article
doi: https://doi.org/10.1371/journal.pmed.1001581Summary
Background:
Intimate partner violence (IPV) and termination of pregnancy (TOP) are global health concerns, but their interaction is undetermined. The aim of this study was to determine whether there is an association between IPV and TOP.Methods and Findings:
A systematic review based on a search of Medline, Embase, PsycINFO, and Ovid Maternity and Infant Care from each database's inception to 21 September 2013 for peer-reviewed articles of any design and language found 74 studies regarding women who had undergone TOP and had experienced at least one domain (physical, sexual, or emotional) of IPV. Prevalence of IPV and association between IPV and TOP were meta-analysed. Sample sizes ranged from eight to 33,385 participants. Worldwide, rates of IPV in the preceding year in women undergoing TOP ranged from 2.5% to 30%. Lifetime prevalence by meta-analysis was shown to be 24.9% (95% CI 19.9% to 30.6%); heterogeneity was high (I2>90%), and variation was not explained by study design, quality, or size, or country gross national income per capita. IPV, including history of rape, sexual assault, contraceptive sabotage, and coerced decision-making, was associated with TOP, and with repeat TOPs. By meta-analysis, partner not knowing about the TOP was shown to be significantly associated with IPV (pooled odds ratio 2.97, 95% CI 2.39 to 3.69). Women in violent relationships were more likely to have concealed the TOP from their partner than those who were not. Demographic factors including age, ethnicity, education, marital status, income, employment, and drug and alcohol use showed no strong or consistent mediating effect. Few long-term outcomes were studied. Women welcomed the opportunity to disclose IPV and be offered help. Limitations include study heterogeneity, potential underreporting of both IPV and TOP in primary data sources, and inherent difficulties in validation.Conclusions:
IPV is associated with TOP. Novel public health approaches are required to prevent IPV. TOP services provide an opportune health-based setting to design and test interventions.
Please see later in the article for the Editors' SummaryIntroduction
Intimate partner violence (IPV) has been defined by the World Health Organization (WHO) as “behaviour within an intimate relationship that causes physical, sexual or psychological harm, including acts of physical aggression, sexual coercion, psychological abuse and controlling behaviours” encompassing both current and past intimate partners [1]. Estimated prevalence varies globally and within countries, and is partly dependent on definition and methodology; lifetime exposure has been found to range from 15% in Japan to 71% in Ethiopia (estimated by WHO multi-country studies), has been estimated at 24% in the UK based on UK Home Office crime statistics [2], and has been estimated to be around 35% (inclusive of stalking) in the US [3]. Rape within intimate relationships has been reported to be common across a number of continents, with lifetime prevalence of forced sex ranging from 5.9% to 42% [4].
Health consequences of IPV are known to include, but not be limited to, increased physical injuries and gastrointestinal, gynaecological, and psychiatric co-morbidities [4]–[7]. Violence may begin or intensify during pregnancy and is associated with adverse obstetric outcomes [8] and maternal death [9],[10]. Increased homicide [5],[11],[12] and suicide are found among individuals experiencing IPV [5],[13].
Randomised trial evidence has shown that training primary care professionals in selective questioning of women about IPV increases disclosure and referral to specialist IPV services [14]. Antenatal routine questioning for IPV is recommended in both the US and UK [15],[16], despite uncertainty over the harms and benefits of universal questioning and subsequent intervention [17]. Ongoing pregnancy is considered to be a time of increased risk of IPV, yet women seeking termination of pregnancy (TOP) are not such a focus of attention [18]. An evidence-based understanding of the association between IPV and TOP would directly inform the development of strategies for effective interventions for IPV. To our knowledge there has been no previous systematic review of the literature.
The aim of this study was to determine whether there is an association between IPV and TOP.
Methods
Selection Criteria
Studies were considered eligible for inclusion if they (1) included women who were seeking or had undergone a TOP and studied at least one aspect of IPV in this group; (2) were a randomised control trial, case-control study, cohort study, cross-sectional analysis, experimental study, or secondary study with data of interest; and (3) were peer reviewed. Studies focusing on violence by individuals other than current or former intimate partners were excluded. No restrictions were placed on the setting, time, or language of the studies. Quantitative data were not necessary for inclusion.
Search Strategy
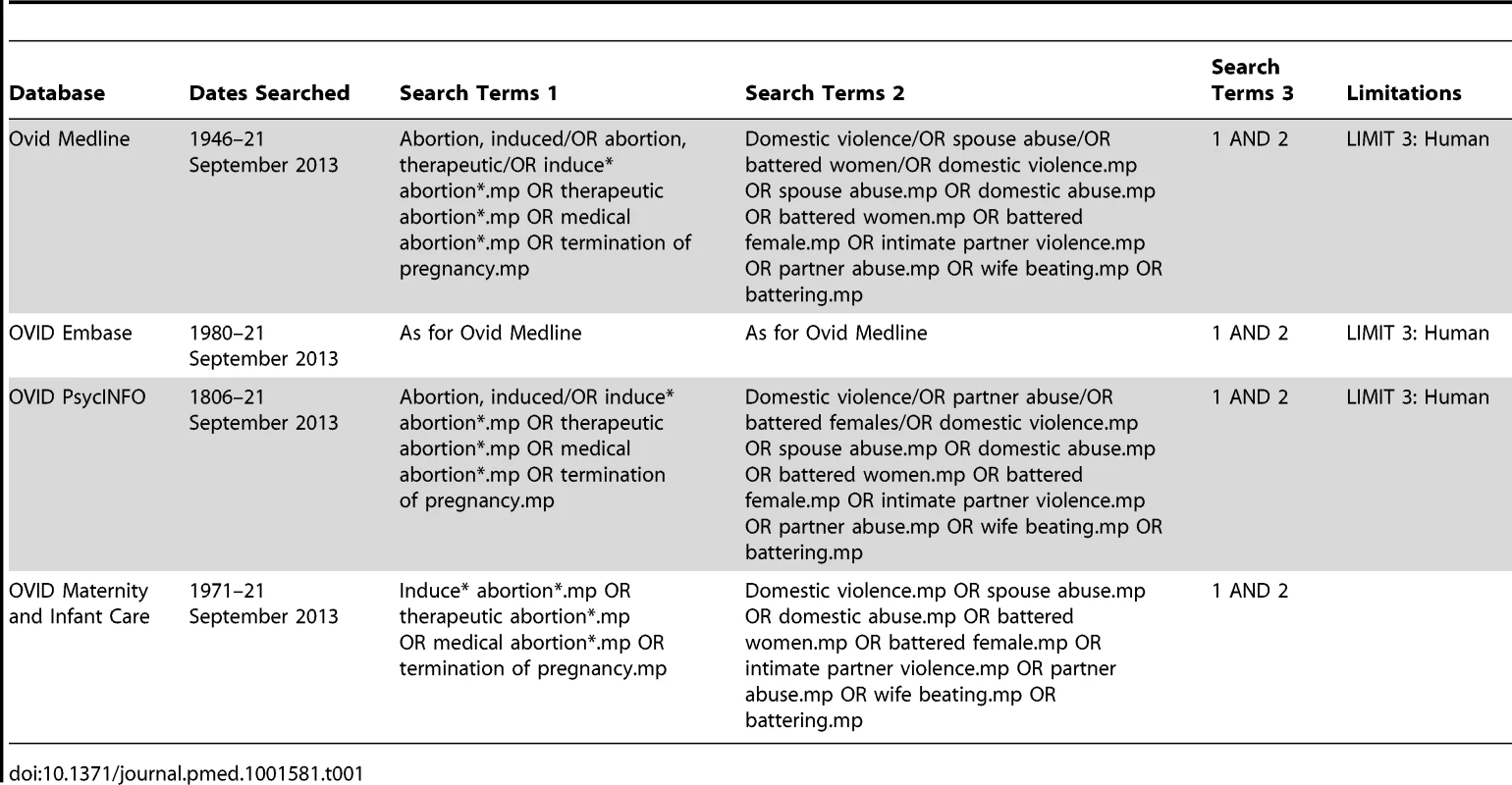
The population of interest was women seeking or having undergone a TOP in any setting; the exposure was the presence or absence of IPV; the control group, where reported, was a separate cohort of comparable individuals (e.g., pregnant women not seeking TOP, pregnant women not reporting IPV, or women attending a gynaecology clinic); the statistic of interest was the association between IPV and TOP. We included articles where the relative timing of IPV and TOP could not be delineated. The search strategy was devised using a combination of Medical Subject Headings (MeSH terms) and free text terms with synonyms (see Table 1). Searches were carried out in Medline (1946–21 September 2013), Embase (1980–21 September 2013), PsycINFO (1806–21 September 2013), and Ovid Maternity and Infant Care (1971–21 September 2013) from the earliest possible date until 21 September 2013. In addition, a search of Web of Science and hand searches of reference lists of all included articles were carried out. Nine authors were contacted regarding results, and they identified further articles. There was no restriction on language. If multiple articles based on the same study were identified, duplication was avoided by only using the data reported for different sub-groups.
Data Extraction
All titles were independently screened by two authors (M. H. and S. B.). If either considered a title relevant, both reviewers independently screened the abstract. All articles were included for full-text assessment if either author considered the abstract relevant or there was uncertainty. Full-text assessment to determine inclusion was independently carried out by two authors (M. H. and S. B.). Any disagreements were discussed, and any study whose inclusion remained ambivalent was referred to a third author (L. C. C.).
A standard form was devised (see Table S1) prior to data extraction and quality scoring. Data were extracted on study type; population; setting, country, and region; demographic and health factors; intervention; comparator population; definition of IPV; screening tools used; and incidence and prevalence of IPV among general populations and in relation to TOP. Data from the articles were independently extracted by two authors (M. H. and B. L. P.). Results addressing violence by individuals other than current or previous intimate partners were excluded. Any uncertainties were discussed, and referred to a third author (L. C. C.) if necessary. Data extraction and quality scoring of articles published in languages other than English (n = 3) were undertaken by one author (M. H.) and the translator.
Quality Appraisal
Quality appraisal of quantitative and qualitative studies was carried out using Critical Appraisal Skills Programme (CASP) scales [19] as modified by Oram and colleagues [20] (see Tables S2 and S3), consisting of 15 and ten criteria, respectively, each of which could be scored between zero and two (maximum scores 30 and 20). Two authors (M. H. and B. L. P.) carried out full quality appraisal of all articles. Any disagreements were discussed, and referred to a third author (L. C. C.) if necessary. Quantitative CASP scores of ≥25, ≥20, ≥15, and ≤14 and qualitative CASP scores of ≥17, ≥14, ≥12, and ≤11 were considered high, medium, low, and very low quality, respectively.
Meta-Analysis and Regression
The prevalences of IPV (as percentages) were converted to log odds prior to combining using the DerSimonian and Laird random effects method of meta-analysis [21]. Resulting estimates and confidence intervals were reconverted to percentages prior to display. Forest plots show actual percentages on the log-odds scale and are displayed sub-grouped by gross national income (GNI) per capita, as previous reports (e.g., from WHO) have chosen similar economic groupings [22]. Comparisons between groups used odds ratios (ORs). Estimated heterogeneity (I2) is displayed for all group and sub-group analyses. We investigated the possibility of a sub-group of recent or high-quality studies with consistent methods and consistent results that could be used to give generally applicable results.
Meta-analysis regression is a meta-analysis technique developed specifically to explain large and unexplained differences in results between studies (also known as heterogeneity). The method used assumes that the differences are in part random and in part explainable [23].
Potential sources of heterogeneity were investigated using meta-analysis regression: country's GNI per capita (in intervals of INT$10,000), study quality (measured by CASP score), date of study (decade), study design (cross-sectional, cohort, or case-control), setting (urban versus regional versus national), and study size (total number of participants as a continuous variable). Egger's test was performed in order to assess potential publication bias [24].
The review was performed according to protocol (Text S1) and in line with PRISMA guidelines (Table S4).
Results
Study Selection Process
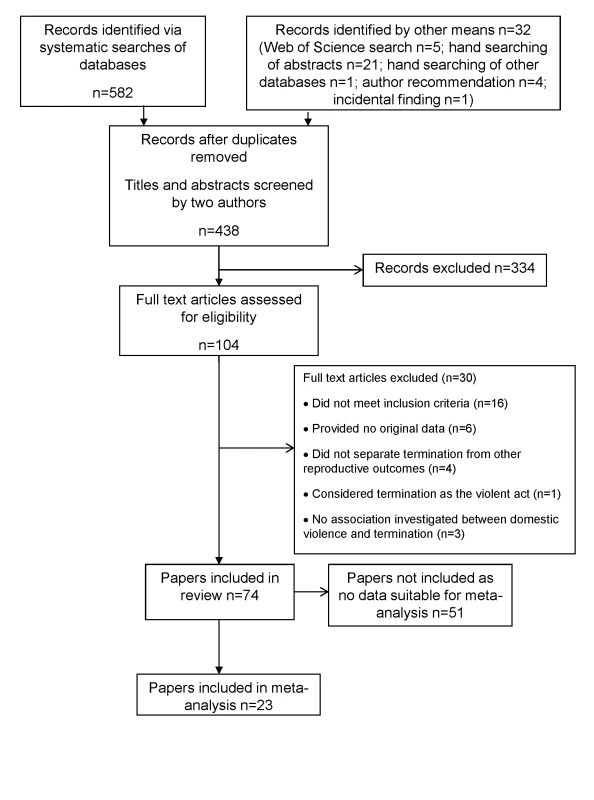
The study selection process is shown in Figure 1. Of a total of 438 articles identified for screening after removal of duplicates, 104 were considered eligible for full-text screening, and 74 were included in the review [25]–[98]. Tables 2–9 detail the studies, grouped into tables by design—and additionally by continent for cross-sectional studies—and listed within tables by reverse chronology.
Tab. 2. Characteristics of included cohort studies. 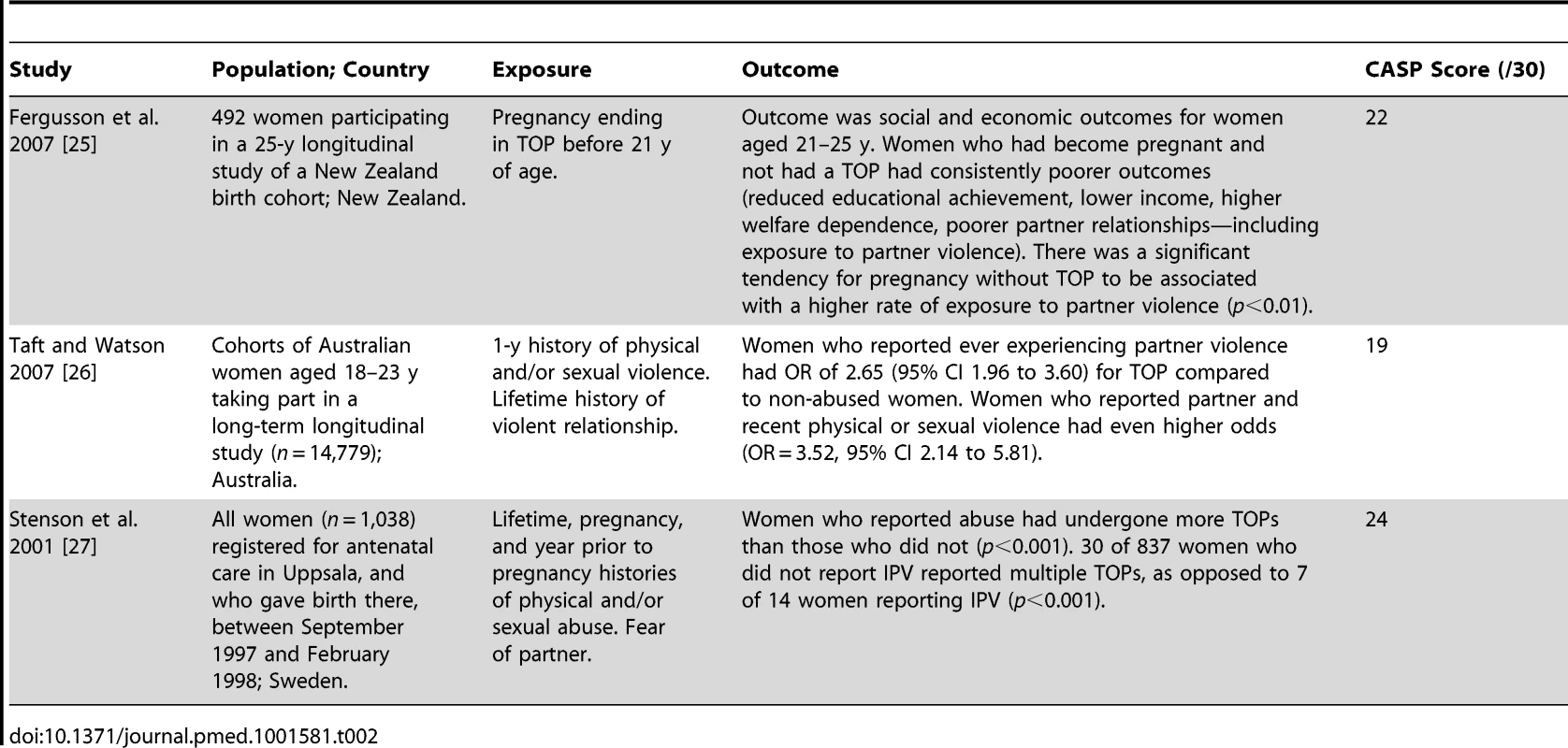
Tab. 3. Characteristics of included case-control studies. 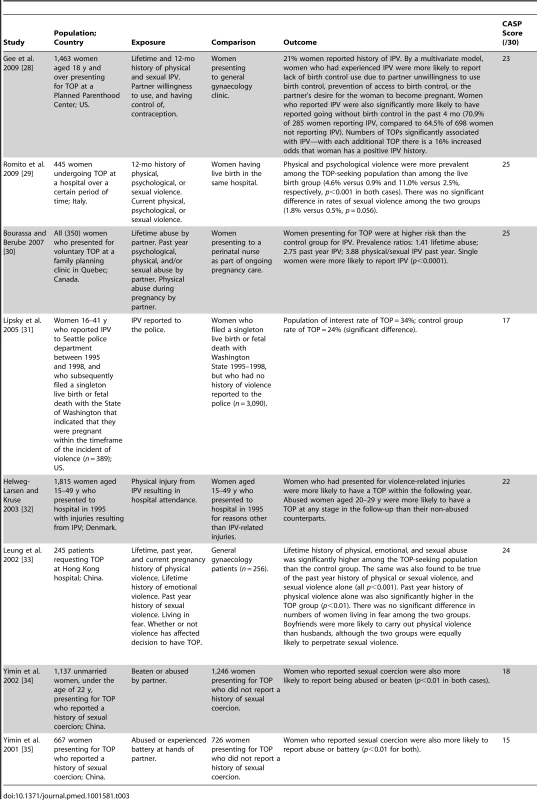
Tab. 4. Characteristics of included cross-sectional studies from the Americas. 
Percentages in brackets are calculated percentages not reported in the original studies. Tab. 5. Characteristics of included cross-sectional studies from Europe. 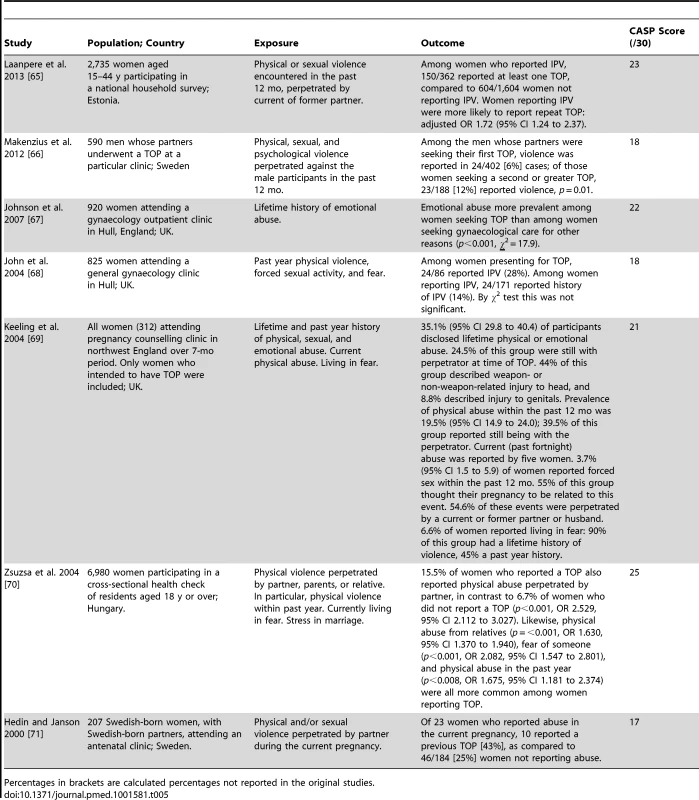
Percentages in brackets are calculated percentages not reported in the original studies. Tab. 6. Characteristics of included cross-sectional studies from Africa. 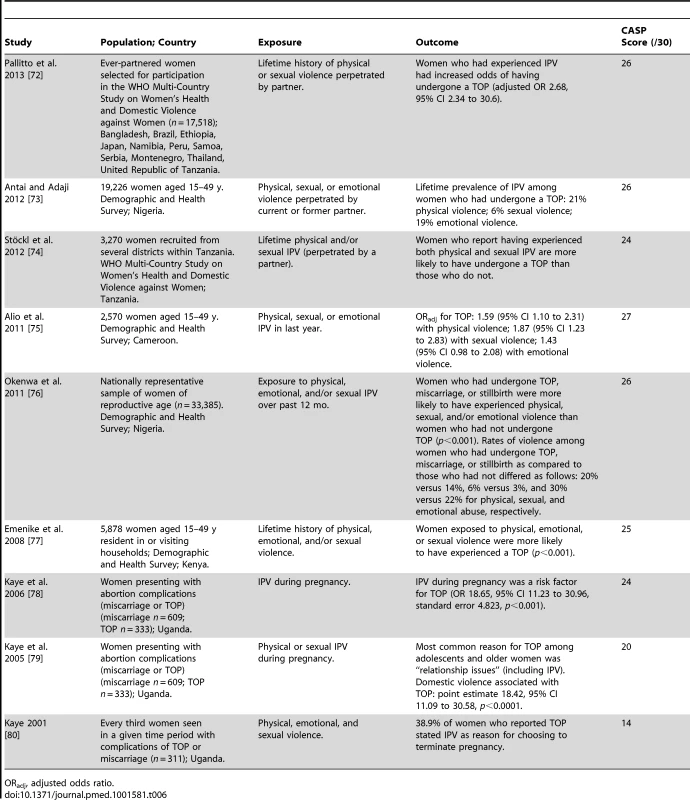
ORadj, adjusted odds ratio. Tab. 7. Characteristics of included cross-sectional studies from Asia. 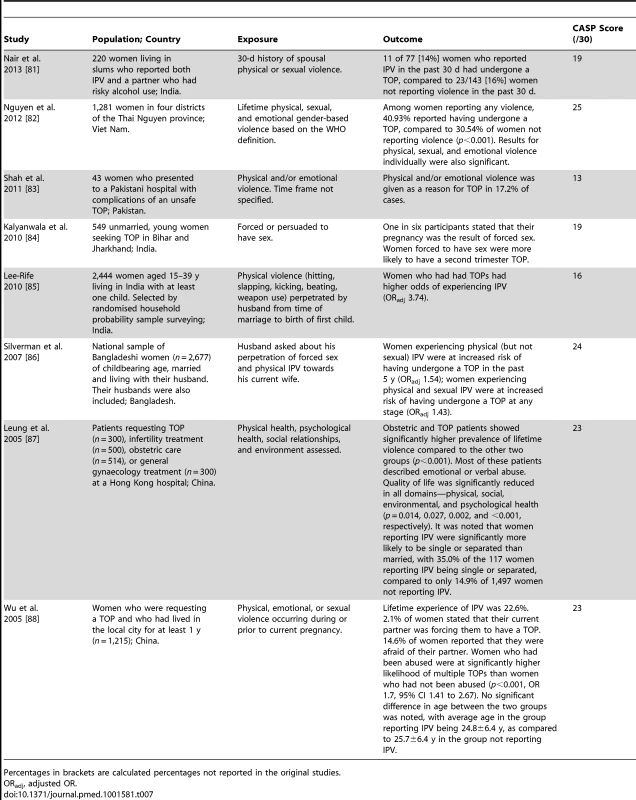
Percentages in brackets are calculated percentages not reported in the original studies. Tab. 8. Characteristics of included cross-sectional studies from Australasia. 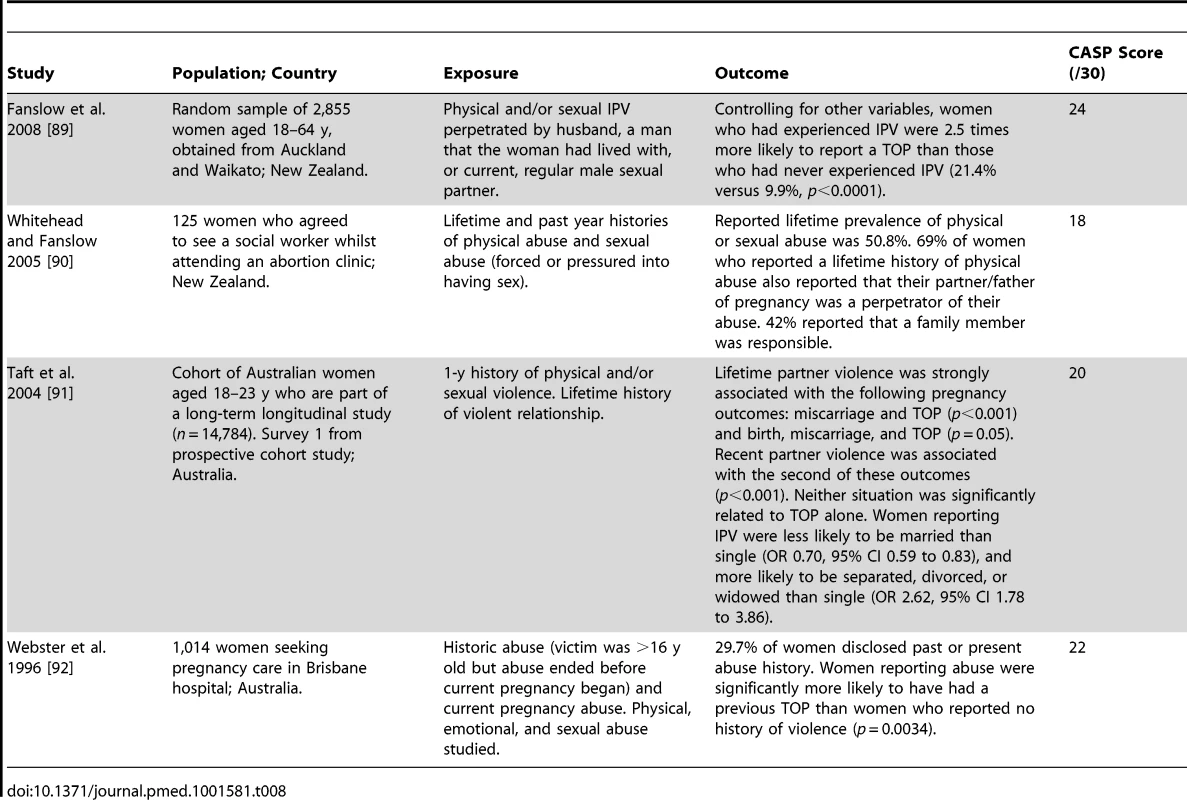
Tab. 9. Characteristics of included qualitative studies. 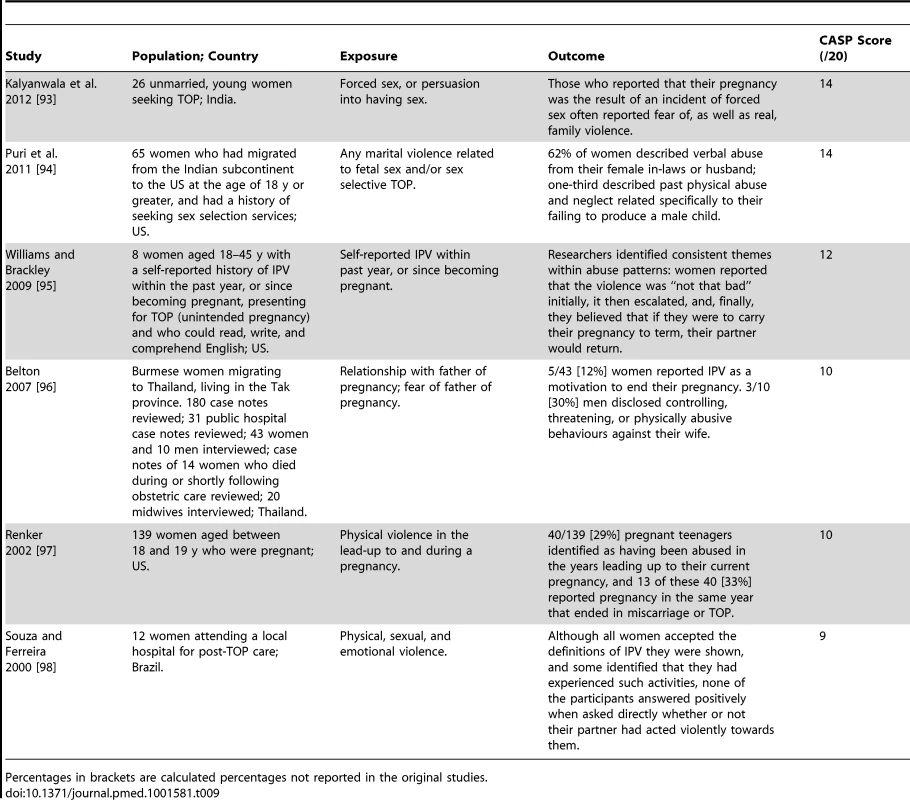
Percentages in brackets are calculated percentages not reported in the original studies. Key Features of Studies
The publication dates of the studies ranged from 1985 to 2013, with the majority (67/74, 91%) having been reported since 2000. Sixty-eight studies included quantitative data, with six being exclusively qualitative. The majority of quantitative studies were cross-sectional (57), with the remaining being cohort (three) and case-control (eight, of which five used a pregnant and three used a non-pregnant comparator group). Geographically, the study locations spanned six continents: North America (35), Asia (12), Europe (10), Africa (8), Australasia (6), and South America (2), with one further study analysing data from several continents. Women were asked about IPV in a variety of settings, including home, gynaecology wards, termination clinics, and other specialist medical clinics, and in various ways, including telephone or written questionnaire and national scale surveys. Among the quantitative studies there were 10 high, 31 medium, 19 low, and eight very low quality reports (mean score 20.2, standard deviation 4.0). Of the qualitative studies two were medium, one low, and three very low quality (mean score 11.5, standard deviation 2.2). The majority of studies analysed exclusively women (69), with few analysing exclusively men (two) or both men and women (three). Sample sizes ranged from eight to 33,385 participants (eight, 30, and 36 studies had <100, 100–999, and ≥1,000 participants, respectively; median number of participants 942, interquartile range 208 to 2,391). The exposures included physical violence (53), sexual violence (47), and emotional violence (19), with many articles looking at combinations (42). Table S5 shows the associations of clinical and demographic factors with IPV in women seeking TOP.
Prevalence and Meta-Analysis of Lifetime Prevalence
Among women who underwent TOP, reported rates of IPV in the preceding year ranged from 2.5% [43] to 30% [76], while lifetime rates of IPV in this population varied from 14% [88] to 40% [59]. Meta-analysis of lifetime prevalence of IPV among TOP-seeking populations was found to be 24.9% (95% CI 19.9% to 30.6%), as shown in Figure 2. Following systematic meta-analysis regression, we found that the high level of variation between studies was not explicable by study quality, type, or size, or country GNI per capita (Table S6). The association between IPV and TOP is shown in Figure 3; variation is not explained by GNI per capita. I2 values for heterogeneity were high, as expected when pooling data with proportions.
Fig. 2. Prevalence of intimate partner violence among women seeking termination of pregnancy grouped by country's gross national income per capita (in intervals of Int,000). 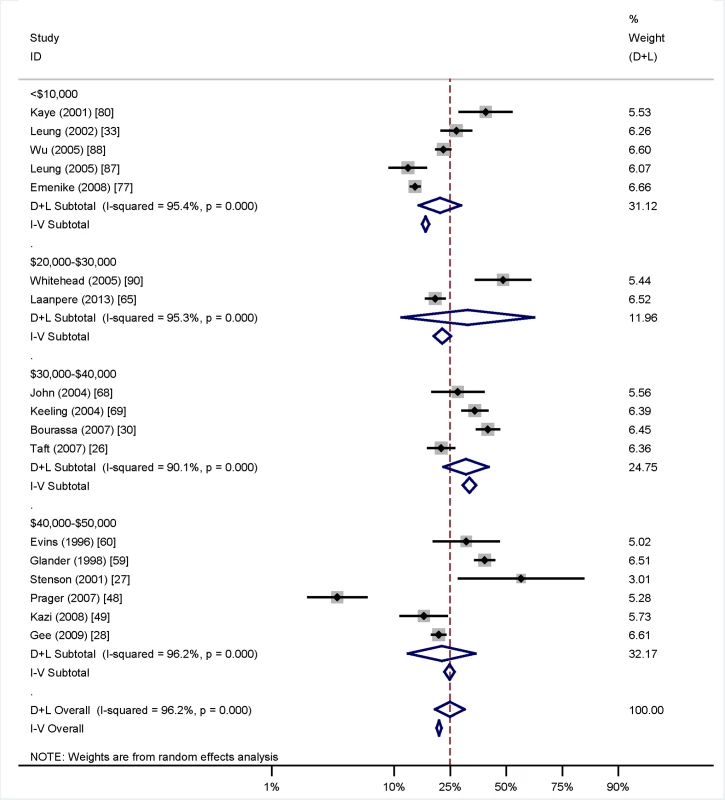
Weights are from random effects analysis. D+L, combined effects using the DerSimonian and Laird [21] random effects method; I-V, combined effects using the inverse variance fixed effects method. Fig. 3. Associations between intimate partner violence and termination of pregnancy grouped by country's gross national income per capita (in intervals of Int,000) and with setting (urban, regional, or national) given. 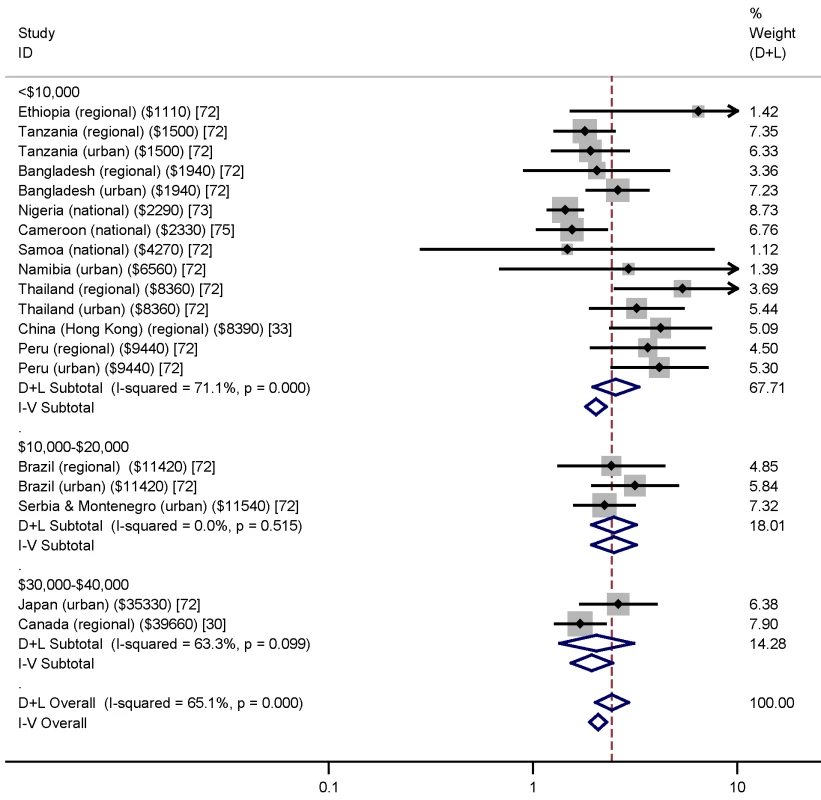
Weights are from random effects analysis. D+L, combined effects using the DerSimonian and Laird [21] random effects method; I-V, combined effects using the inverse variance fixed effects method. Countries grouped by GNI (shown in parentheses). Meta-Analysis of Risk Factors
Meta-analysis was undertaken for four factors where data were available (woman being single versus married, partner not knowing about the TOP, partner support for the TOP, and previous TOP), but was not possible for others, as the definitions of both IPV and the risk factors varied, or there was a lack of numerical data or only a single study in many cases. Figure 4 shows no association (pooled OR 2.97, 95% CI 2.39 to 3.69) between being single and IPV among a TOP-seeking population. There was an association (pooled OR 2.32, 95% CI 2.00 to 2.69) between partner not knowing about the TOP and IPV (Figure 5), but no association between partner support for the TOP and IPV (pooled OR 1.37, 95% CI 0.82 to 2.30) (Figure 6). Meta-analysis of three studies reporting on the association between IPV and previous TOP showed no significant association (pooled OR 1.42, 95% CI 0.85 to 2.36) (Figure 7), but five of six further studies reported individual significant associations, though with inadequate quantitative data to include in the meta-analysis. Table S5 shows the associations of clinical and demographic factors with IPV in women seeking TOP.
Fig. 4. Single status and intimate partner violence. 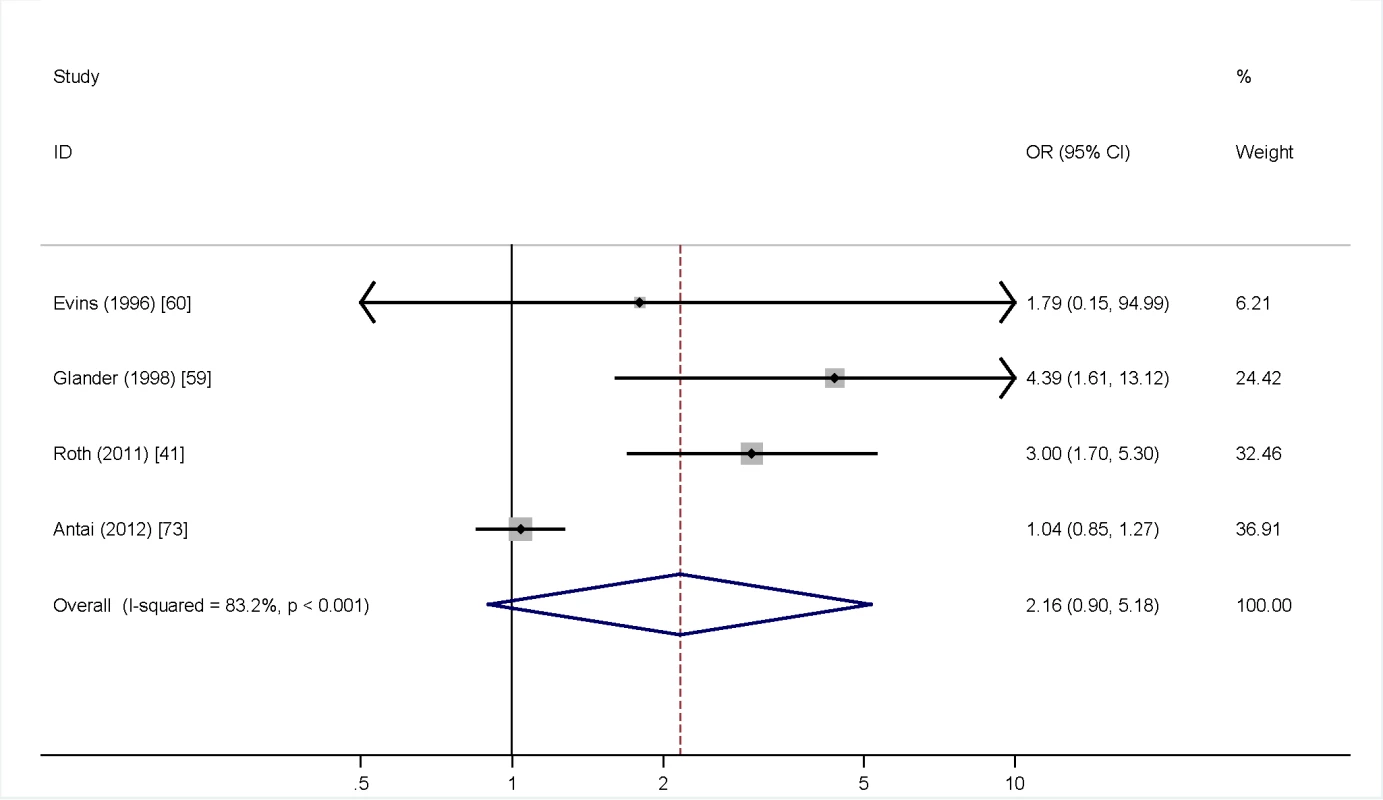
Weights are from random effects analysis. OR, odds ratio. Fig. 5. Partner knowledge of termination of pregnancy and intimate partner violence. 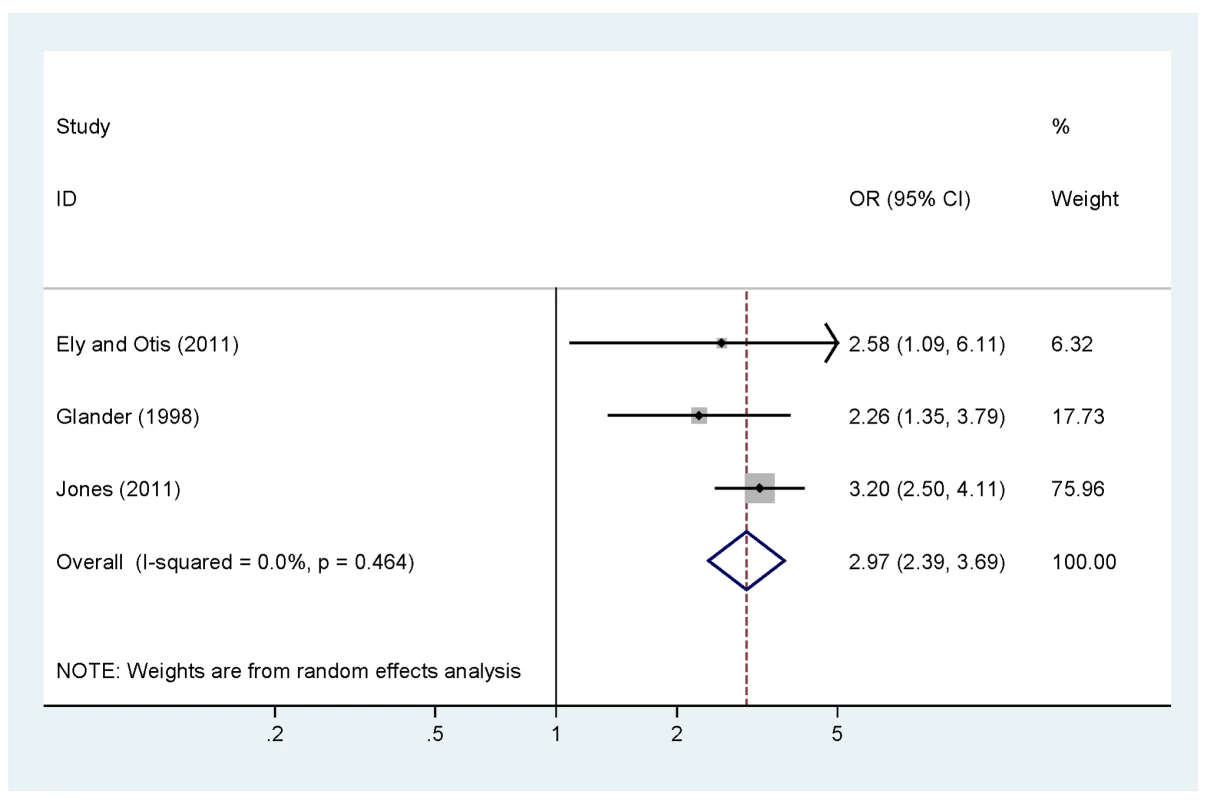
Weights are from random effects analysis. OR, odds ratio. Fig. 6. Partner support for termination of pregnancy and intimate partner violence. 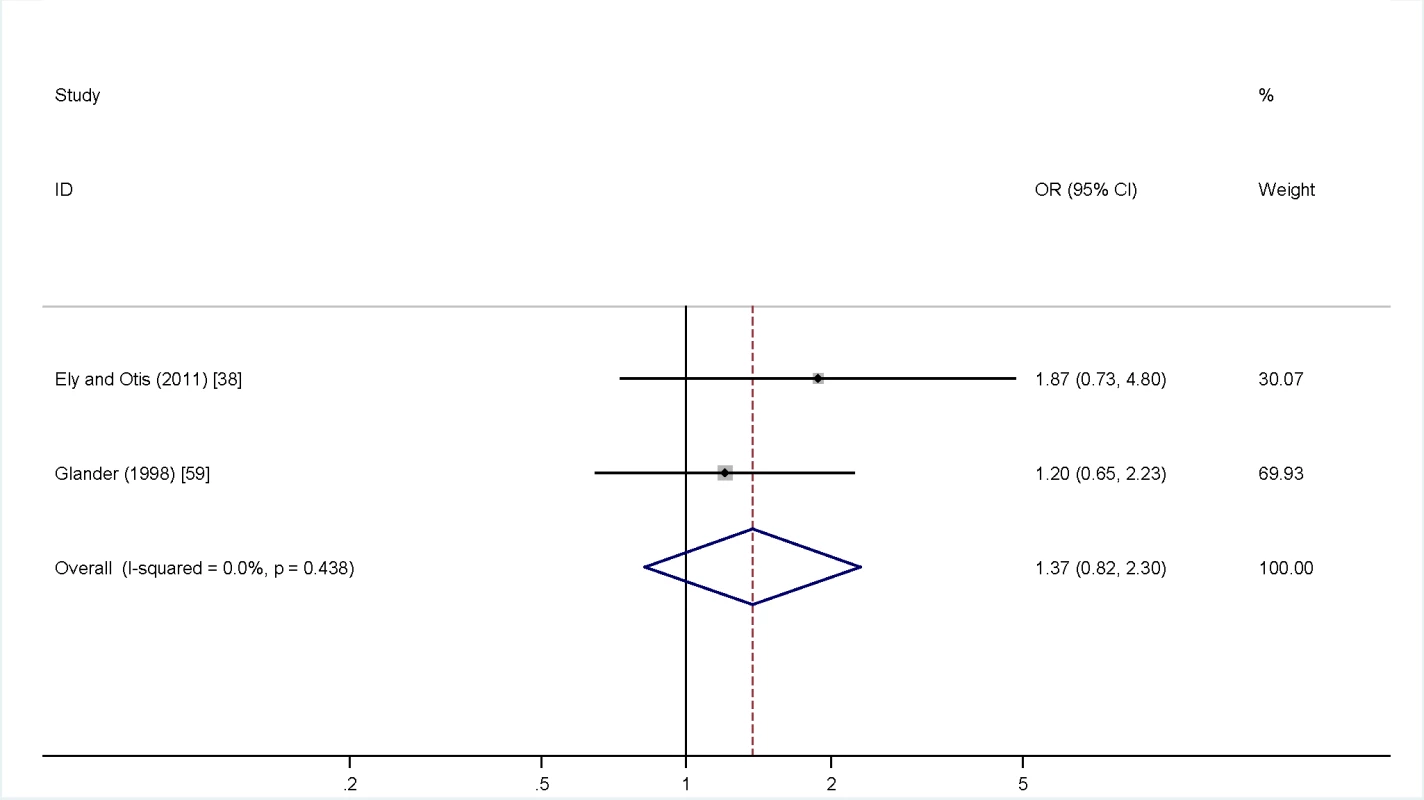
Weights are from random effects analysis. OR, odds ratio. Fig. 7. Previous terminations of pregnancy and intimate partner violence. 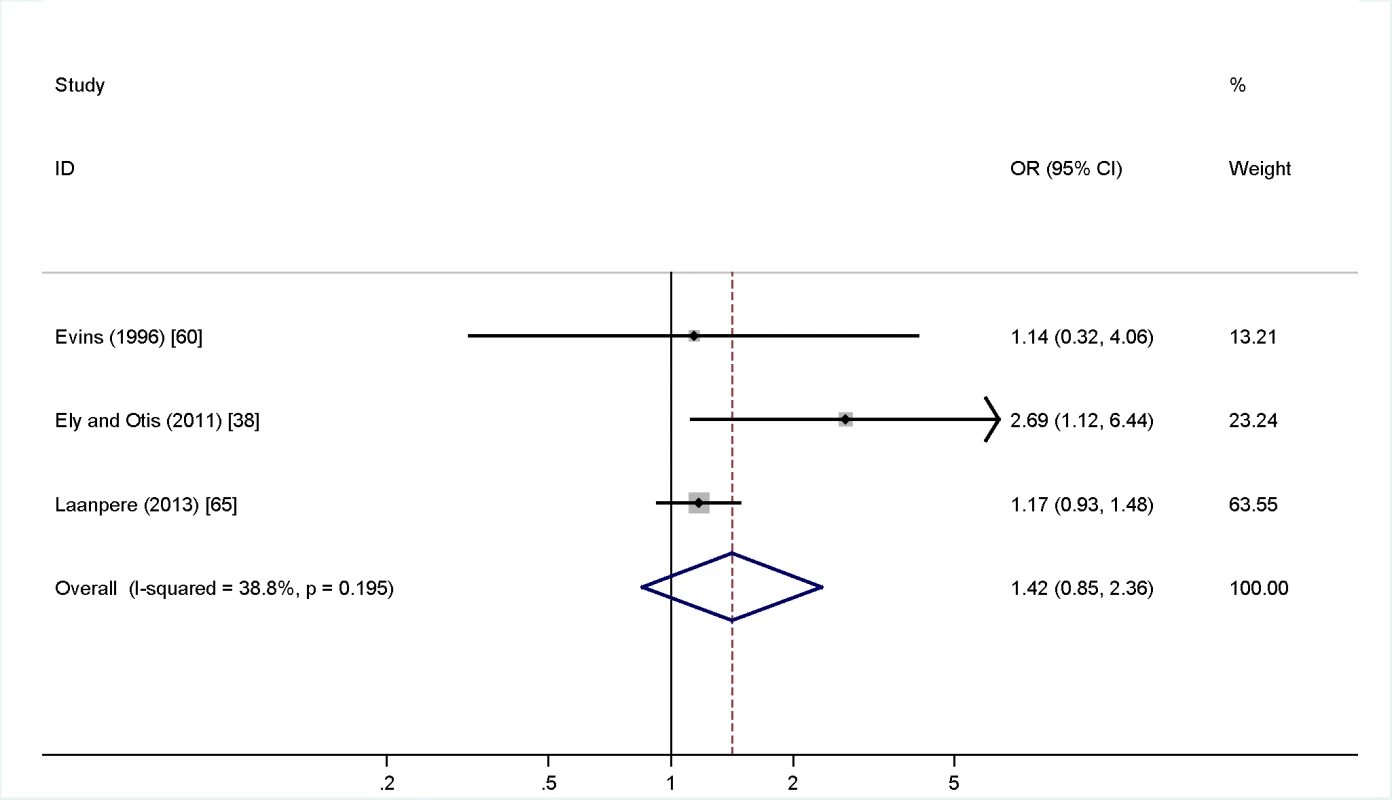
Weights are from random effects analysis. OR, odds ratio. Associations with Reproductive and Pregnancy Factors
Past obstetric history
Nine studies showed that women who reported IPV were more likely than the comparator group to have a history of multiple TOPs (Tables 3–5) [27],[28],[38],[41],[42],[44],[51],[60],[65]. The highest quality study found that women presenting for a third TOP were over two and half times more likely to have a history of physical or sexual violence than women presenting for their first [51]. There was no significant association between number of pregnancies and IPV (gravidity in group of women reporting IPV: mean 3.2, standard deviation 2.0; among women not reporting IPV: mean 3.0, standard deviation 2.0) [41], although one medium quality study found a higher odds of history of previous miscarriage among women reporting IPV at a termination clinic, as compared to those not reporting IPV (OR 1.6, 95% CI 1.1–2.2) [41].
Coercion, contraception, and conception
One study investigating pregnancy intention found that women in violent relationships were more likely to say that the pregnancy “had been imposed” upon them by their partner (13% versus 2% for women not in physically or sexually violent relationship) [29]. A further two studies found that pregnancy associated with sexual coercion and ending in TOP was also 1.8 - to 3.8-fold more likely to be associated with IPV [34],[35]. One study found that women in violent relationships were significantly more likely to report going without contraceptives compared to women not reporting IPV (Table 3) [28], with another study finding that they were more likely to use them (Table 4) [38]. In four studies, of which two were very low quality, women reported being actively prevented from obtaining contraception by their partner, or that their partner was refusing or deceiving them about birth control use (Tables 3 and 4) [28],[38],[45],[52]. It was reported that a partner preventing access to contraception led to concealed use of contraceptives among some women [45].
One cross-sectional population telephone survey of over 4,000 women found that over 46% of 616 “completed rapes” were perpetrated by a husband or boyfriend, and that 50% of 20 rape-related pregnancies ended in TOP [61]. One low quality study of women who migrated as adults from the Indian subcontinent to the US and had a history of seeking sex selection services found that a third of 65 women described past physical abuse and neglect related specifically to not producing a male child [94].
Factors Relating to Termination of Pregnancy
Decision-making
Women reporting IPV were more likely to report an unwanted pregnancy (7.4% of 163 women not reporting IPV versus 23.3% of 44 women reporting IPV) [53]. Additionally, a high quality study, though with small numbers, found that women attending a termination clinic with a planned pregnancy were more likely to report IPV (50% of 12 women) than those who did not plan their pregnancy (5.6% of 337 women) [30]. There was evidence from very low quality studies that some women felt coerced by their violent partner into having a TOP (Table 4) [45],[52]. One medium quality study found that 2% of 1,215 women in a termination clinic reported being forced into the decision by their partner [88]. One small, very low quality study of 38 women participating in a hospital-based IPV programme found that 18% reported feeling “pressured” into TOP and 5% were forced into undergoing the procedure [52].
There was consistent evidence that women in violent relationships were more likely not to tell their partner about their decision to terminate (pooled OR 2.97, 95% CI 2.39 to 3.69; Figure 5) [38],[39],[54]. Women with an IPV history were less likely to have their partner fund their TOP (27% of 25 women reporting IPV had their partner pay for their TOP versus 63% of 155 women not reporting IPV) [38].
Gestation and method of termination of pregnancy
Two studies, one of high and one of low quality, failed to find any association between IPV and gestation at TOP [54],[57], although one lower quality study reported that women having a second trimester TOP were more likely to report a history of forced sex than women having a first trimester TOP (35.3% of 410 versus 11.5% of 139), [84], and another found that women later in their second trimester (over 16 versus 13–15 weeks' gestation) at time of TOP were more likely to report IPV (OR 1.23, 95% CI 0.79 to 1.91) [40]. One further study found that women who reported IPV were more likely to have the gestational age of the fetus redated on ultrasound (64.9% of 243 women reporting IPV versus 49.9% of 817 women not reporting IPV) [41].
Psychosocial problems
In women who had undergone TOP, there was a significant association between reported IPV and psychosocial problems including depression [38],[47], suicidal ideation [47], stress [38],[47], and disturbing thoughts [47], although the temporal relationships were unclear (Table 4) [38],[47]. No studies identified the subsequent impact of IPV and TOP on the woman, her partner, or their relationship.
Disclosure and intervention
Five studies examined disclosure in termination clinics: IPV questionnaires were highly acceptable [90], although non-responding women differed from those who responded and had undergone more TOPs [41]. Women in violent relationships were as likely to attend for follow-up (52.2% of 413 non-abused women defaulted versus 46.6% of 88 abused women) [33] and more likely to know about community resources for IPV (80% of 16 women reporting IPV versus 67% of 35 women not reporting IPV) [60]. Some women reported events that would meet the definition of IPV but did not identify themselves as experiencing IPV [98]. Nevertheless, many women wished to talk about IPV with regard to further management or intervention [33], with some citing their doctor as the main source of information [60]. However, during a period of universal screening only 51% of 499 women were asked about IPV; certain sub-groups of women were more likely to be asked about IPV (e.g., white women, in a Canadian study, in which white women made up 55% of the TOP-seeking population [n = 499], but 63% of those asked about IPV [n = 254] [57]).
Demographic Factors
Female factors
The majority of studies focused on female factors. The results relating to impact of age on the association between IPV and TOP were discrepant, and interpretation is hindered by different age groups being used. One paper reported that past year incidence of IPV was higher among women under the age of 20 y seeking TOP (50.0%) than among those 20 y or over (26.9%); however, the converse [29],[30] or no significant association (Tables 4, 6, and 7) [41],[57],[75],[88] has also been reported.
There was contradictory evidence for variance between women of different race or ethnicity, with two studies finding converse associations; one found that significantly fewer white Caucasian women (12% of 160 women) reported IPV as compared to non-white women (21% of 94 women, p = 0.003) [57]; another study of women seeking elective pregnancy termination reported that a greater proportion of white women (48% of 226) had experienced IPV compared to black women (31% of 223, p = 0.001) [59]. This finding may not be generalisable to other locations. No significant associations were found with women's level of education in two studies [41],[88] or with women's income [41]. Three studies reported no significant association with employment status [41],[69],[88], whilst two suggested that unemployed women or non-skilled labourers were more likely to report both IPV and TOP (25.3% of 291 women seeking TOP and reporting IPV were unemployed versus 19.1% of 1,096 women seeking TOP and not reporting IPV) [28],[33].
Three studies of similar medium quality assessed drug and alcohol use; one study found that, compared to women not reporting IPV, women in a termination clinic who reported IPV were also more likely to smoke (25.6% of 117 women experiencing IPV versus 11.0% of 1,497 non-abused women) and drink (12.8% of women experiencing IPV versus 4.9% of non-abused women) [87], but other studies found no significant association [88] or reported an association only anecdotally [59].
An association between negative physical quality of life scores and IPV and TOP was found in one medium quality study (Table 7) [87].
Relationship factors
Five studies, one of high and four of medium quality, found that, compared to married women, those who were single, separated, divorced, or widowed were more likely to have a history of IPV and TOP (Tables 3, 4, and 7) [30],[41],[43],[87],[91], though one medium quality study found no significant association [88], and one further study of women experiencing IPV found married women were more likely to report a TOP (89% of 23,909 married women compared to 11% of 9,408 unmarried women) [73]. Women who reported difficulties in their relationship were also more likely to report IPV when asked at a termination clinic in all studies (with one study finding that 7.7% of 350 women undergoing a TOP reported difficulties in their relationship, as opposed to 1.8% of 653 women continuing pregnancy) [30],[38],[59]. One study found no significant association between prevalence of IPV and household income (27.2% of 669 women reporting TOP were in the lowest income bracket, as compared to 26.5% of 139 women not reporting TOP) [54].
Male factors
One article studied men attending community health centres and identified that men who admitted to IPV perpetration were more likely to report having “been involved in a pregnancy” that ended in TOP (48.9% of 188 men reporting IPV perpetration also reported involvement in TOP, as opposed to 22.7% of 402 men not reporting IPV perpetration) [44]. Another study of partners of women having a first or subsequent TOP found higher rates of IPV experienced by the men involved in a second or more TOP (12% of 188 men whose partner was having a second or subsequent TOP reported “being a victim” of IPV versus 6% of men whose partner was having a first TOP) [66]. One low quality study noted that 36% of 16 women reporting IPV stated that their perpetrating partner had been the victim of abuse as a child [60].
For IPV in women presenting for TOP, there was no evidence of bias relating to non-publication of small non-significant studies; Egger's test [24] for small-study effects was non-significant (p = 0.13). These associations, the uncertainties, and gaps in knowledge are shown diagrammatically in Figure 8.
Fig. 8. Matrix of associations between domestic violence and termination of pregnancy. 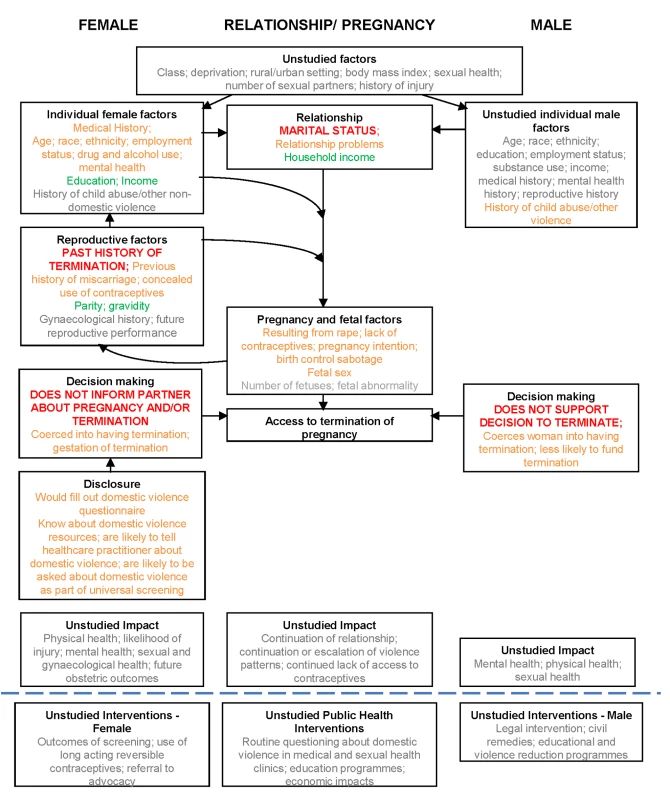
Key to associations: red, associations meta-analysed; amber, associations not meta-analysed but shown in literature; green, no significant association described in the literature; grey, not studied. There were no intervention studies.
Discussion
Summary of Main Findings
The literature is extensive, but variable in quality, and largely focused on female factors. High rates of physical, sexual, and emotional IPV were found across six continents among women seeking a TOP. According to meta-analysis, partner not knowing about the TOP was associated with IPV among women seeking TOP. However, lack of partner support for TOP is not associated with IPV among women seeking TOP. The literature also suggests that women in abusive relationships were more likely to report inability to make autonomous contraceptive choices, partner contraceptive sabotage, and sexual violence, and they were less likely to have informed their partner about the pregnancy or involved him in decision-making about it. IPV was cited as a reason for wanting TOP, and rape-related pregnancy had a particularly high chance of leading to TOP. The meta-analysis did not find that multiple TOPs were associated with IPV, but its credibility is undermined by both the number of studies that did (albeit unquantified) and the association reported by men who stated they had been perpetrators of IPV. Although it was not always determined whether experiencing IPV was a determining factor in the decision to end, rather than continue, a pregnancy, the findings support the concept that violence can sometimes lead to an initial pregnancy (via coercion, rape, sexual assault, or contraceptive sabotage) and to a subsequent TOP (via coercion). There was a lack of data regarding long-term outcomes for women in violent relationships who underwent TOP, but associations with repeat TOP (and possibly miscarriage) lend support to the notion of a repetitive cycle of abuse and pregnancy. Not informing the male partner may then be explicable as a reason to avoid partner involvement or further abuse.
Strengths and Limitations
Strengths of the review and meta-analysis include use of multiple databases, no language restriction, hand searching of reference lists, double data entry, and quality assessment of both quantitative and qualitative studies from a wide variety of settings, thus improving reliability and generalisability. Limitations include unexplained large differences in both prevalences and odds ratios between studies (heterogeneity), likelihood of underreporting of both IPV [99] and TOP (particularly when both are stigmatised) in the primary data sources, and inherent difficulties in validation. There is potential publication bias towards research showing a positive relationship. The meta-analysis may be biased, as only those studies quantitatively reporting a significant result could be included, whilst those stating an association (without providing data for inclusion) had to be excluded. It was not possible to determine the legality of, or access to, TOP for each country or state at the specific time point of study; thus, the analysis has not included evaluation of such barriers. It was not possible to determine temporal relationships and patterns of abuse, pregnancy, and TOP.
Comparison with Other Studies
Only one review has previously examined the association between IPV and TOP within a study of broader sexual health issues [100], concluding that TOP and repeat TOP were associated with IPV, but without reporting on other associations. The review was single-authored, lacked systematic analysis, and included only eight studies. Other relevant systematic reviews and observational studies on IPV have included women with ongoing pregnancies, women with pregnancy loss, or all women of reproductive age, noting poorer mental, physical, and pregnancy outcomes for the women experiencing IPV [101]–[104]. One review found an association between presence of depressive or anxiety disorders in women and increased likelihood of IPV compared to women without mental disorders, but the direction of causality could not be determined, as few studies were longitudinal [104]. IPV was also associated with physical injury: presentation to hospital accident and emergency departments with unwitnessed head, neck, or facial injuries was a significant marker for IPV [103]. A large observational study conducted by WHO found that women who reported a history of partner violence were more likely to report physical and mental health problems including emotional distress and suicidal thoughts, as well as difficulties with activities of daily living [101]. Comparison groups that might prove useful would be women with ongoing but unplanned pregnancy (no specific studies available) and women with ongoing wanted pregnancy. In ongoing pregnancies, IPV was associated with 1.5-fold increased risks of low birth weight and preterm birth [102]. A large observational study has reported poorer maternal outcomes, including hypertension, renal and urinary tract infection, and vaginal bleeding, with IPV [8].
Implications and Clinical Relevance
Health-care professionals should be aware of the high rates of physical, sexual, and emotional violence among women seeking TOP, and particularly the clinical factors associated with greatest risk: previous TOP, lack of contraception, initially planned pregnancy, ultrasound redating, and the partner not funding or not being told about the TOP. There are potential associations for IPV with young age, marital status, ethnicity, and low household income. IPV compromises both the safety and health of the woman requesting the TOP, and potentially that of her partner and any existing children if a woman retaliates or children witness or experience the violence directly. In attempting to prevent repeat TOP [105], a narrow focus, especially on long-acting contraception, that excludes addressing the wider needs of a woman in a violent relationship might leave a woman less likely to become pregnant but just as vulnerable to IPV. Good practice obligates that termination services should have robust policies for ensuring women's safety and confidentiality, providing information and referral pathways for those who disclose IPV, and exemplar guidance exists [16].
Some groups have evaluated whether screening for IPV is justified in selected populations of women. Theoretically, early identification and effective intervention for violence may reduce repeat unintended pregnancy and TOP, as well as improve longer term health outcomes. Three systematic reviews [106]–[108] have concluded that screening is warranted, leading the US Preventative Task Force to recommend that clinicians should screen women of childbearing age for interpersonal violence, such as IPV, and refer women who screen positive to intervention services [109]. The UK National Institute for Health and Care Excellence is currently undertaking a consultation regarding guidance on identification and prevention of IPV [110]. However, interventions in this area are inherently complex and difficult to research [111], and evidence for the effectiveness of counselling intervention programmes or other interventions remains limited [106],[112],[113]. Of all approaches evaluated, intensive advocacy (aiming to provide women with information and support to facilitate access to community resources) appears the most promising in reducing physical abuse 1–2 y after the intervention, but impact on quality of life or mental health is not proven [112]. The majority of interventions studied have focused on the female experiencing IPV, but some have undertaken theoretical analysis of models in which changes in the behaviours of the male perpetrators are included [114]. A comparative study of promising health-based IPV interventions in primary care and maternity services across Europe found that key implementation issues of IPV interventions included clinical champions, leadership roles, funded and coordinated multiagency partnerships with clear referral pathways, multidisciplinary and participant feedback, and evaluation of outcomes [115]. Interventions as part of the pathway for women seeking TOP require further consideration.
Future Research
No study we found set out to examine the association or temporal relationships between IPV and TOP, which would require (at a minimum) including women with and without an IPV history and with and without a history of TOP. There is extremely limited information about male partners of women seeking TOP, as perpetrators or as experiencing IPV, and which male-related factors contribute to increased likelihood of IPV. Greater information is required on long-term outcomes of violence and TOP on both partners. The findings of pregnancy “concealment” and higher rates of murder and suicide with IPV [116],[117] mean that researchers must be cautious and aware of women's safety. Harms have been identified following health-based IPV interventions, such as breaches of confidentiality [115]. Therefore, a public health approach that does not focus solely on the woman (either as “problem” or “solution”) or health services should be considered, for example, using educational, social norm, and/or criminal justice interventions. Nevertheless, given the clear associations, termination services provide an appropriate setting in which to assess screening for, or give information about, IPV, whether pre - or post-TOP, and for offering an intervention that women desire, such as a “one stop” offer of referral to specialist IPV services, especially in view of low return to clinics for follow-up [118]. Given that routine identification of women experiencing IPV and provision of a standard intervention has recently been shown to have no impact on quality of life or mental well-being, there is now a need for considering new strategies, including alternative intervention models and targeting perpetrators as well as the women affected [119]–[121]. On the basis of this review, research into the suitability, acceptability, and design of an intervention programme is justified, and should be tested preferably in a randomised control trial. Any legal barriers to intervention and reporting, such as criminalisation of TOP, should also be investigated and described.
Conclusion
IPV is associated with TOP. Novel public health approaches are required to address IPV against women and repeat TOP. Termination services provide an opportune health-based setting in which to design and test interventions at the individual level.
Supporting Information
Zdroje
1. World Health Organization, London School of Hygiene and Tropical Medicine (2010) Preventing intimate partner and sexual violence against women: taking action and generating evidence. Geneva: World Health Organization. 94 p.
2. UK Home Office (2012) Home Office statistical bulletin: homicides, firearm offences and intimate violence 2010/11: supplementary volume 2 to crime in England and Wales 2010/11. Available: https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/116483/hosb0212.pdf. Accessed 10 March 2013.
3. Black M, Basile K, Breiding M, Smith S, Walters M, et al.. (2010) National Intimate Partner and Sexual Violence Survey: 2010 summary report. Available: http://www.cdc.gov/violenceprevention/pdf/nisvs_report2010-a.pdf. Accessed 10 March 2013.
4. Krug EG, Dahlberg LL, Mercy JA, Zwi AB, Lozano R, editors (2002) World report on violence and health. Geneva: World Health Organization. 346 p.
5. CampbellJC (2002) Health consequences of intimate partner violence. Lancet 359 : 1331–1336.
6. DevriesKM, MakJY, BacchusLJ, ChildJC, FalderG, et al. (2013) Intimate partner violence and incident depressive symptoms and suicide attempts: a systematic review of longitudinal studies. PLoS Med 10: e1001439 doi:10.1371/journal.pmed.1001439
7. HowardLM, OramS, GalleyH, TrevillionK, FederG (2013) Domestic violence and perinatal mental disorders: a systematic review and meta-analysis. PLoS Med 10: e1001452 doi:10.1371/journal.pmed.1001452
8. SilvermanJG, DeckerMR, ReedE, RajA (2006) Intimate partner violence victimization prior to and during pregnancy among women residing in 26 U.S. states: associations with maternal and neonatal health. Am J Obstet Gynecol 195 : 140–148.
9. Lewis G, editor (2007) Confidential Enquiry into Maternal and Child Health. Saving mothers' lives: revisiting maternal deaths to make motherhood safer—2003–2005. The seventh report on Confidential Enquiries into Maternal Deaths in the United Kingdom. London: Confidential Enquiry into Maternal and Child Health.
10. CantwellR, Clutton-BrockT, CooperG, DawsonA, DrifeJ, et al. (2011) Saving mothers' lives: reviewing maternal deaths to make motherhood safer: 2006–2008. The eighth report of the Confidential Enquiries into Maternal Deaths in the United Kingdom. BJOG 118 (Suppl 1) 1–203.
11. AbrahamsN, MathewsS, MartinLJ, LombardC, JewkesR (2013) Intimate partner femicide in South Africa in 1999 and 2009. PLoS Med 10: e1001412 doi:10.1371/journal.pmed.1001412
12. StöcklH, DevriesK, RotsteinA, AbrahamsN, CampbellJ, et al. (2013) The global prevalence of intimate partner homicide: a systematic review. Lancet 382 : 859–865.
13. DevriesK, WattsC, YoshihamaM, KissL, SchraiberLB, et al. (2011) Violence against women is strongly associated with suicide attempts: evidence from the WHO multi-country study on women's health and domestic violence against women. Soc Sci Med 73 : 79–86.
14. FederG, DaviesRA, BairdK, DunneD, EldridgeS, et al. (2011) Identification and referral to improve safety (IRIS) of women experiencing domestic violence with a primary care training and support programme: a cluster randomised controlled trial. Lancet 378 : 1788–1795.
15. UK Department of Health (2004 October 20) Health minister announces new steps to aid victims of domestic violence. London: UK Department of Health. Available: https://webarchive.nationalarchives.gov.uk//www.dh.gov.uk/en/Publicationsandstatistics/Pressreleases/DH_4091530. Accessed 18 March 2012.
16. ACOG Committee opinion No. 518: intimate partner violence. Obstet Gynecol 119 : 412–417.
17. RamsayJ, RichardsonJ, CarterYH, DavidsonLL, FederG (2002) Should health professionals screen women for domestic violence? Systematic review. BMJ 325 : 314.
18. AstonG, BewleyS (2009) Abortion and domestic violence. Obstetrician Gynaecologist 11 : 163–168.
19. Critical Appraisal Skills Programme (2013) Appraising the evidence. Available: http://www.casp-uk.net/find-appraise-act/appraising-the-evidence/. Accessed 10 March 2013.
20. OramS, StocklH, BuszaJ, HowardLM, ZimmermanC (2012) Prevalence and risk of violence and the physical, mental, and sexual health problems associated with human trafficking: systematic review. PLoS Med 9: e1001224 doi:10.1371/journal.pmed.1001224
21. DerSimonianR, LairdN (1986) Meta-analysis in clinical trials. Control Clin Trials 7 : 177–188.
22. Garcia-Moreno C, Jansen HA, Ellsberg M, Heise L, Watts C (2005) WHO multi-country study on women's health and domestic violence against women: initial response on prevalence, health outcomes and women's responses. Geneva: World Health Organization.
23. KnappG, HartungJ (2003) Improved tests for a random effects meta-regression with a single covariate. Stat Med 22 : 2693–2710.
24. EggerM, Davey SmithG, SchneiderM, MinderC (1997) Bias in meta-analysis detected by a simple, graphical test. BMJ 315 : 629–634.
25. FergussonDM, BodenJM, HorwoodL (2007) Abortion among young women and subsequent life outcomes. Perspect Sex Reprod Health 39 : 6–12.
26. TaftAJ, WatsonLF (2007) Termination of pregnancy: associations with partner violence and other factors in a national cohort of young Australian women. Aust N Z J Public Health 31 : 135–142.
27. StensonK, HeimerG, LundhC, NordstromML, SaarinenH, et al. (2001) The prevalence of violence investigated in a pregnant population in Sweden. J Psychosom Obstet Gynaecol 22 : 189–197.
28. GeeRE, MitraN, WanF, ChavkinDE, LongJA (2009) Power over parity: intimate partner violence and issues of fertility control. Am J Obstet Gynecol 201 : 148e1–7.
29. RomitoP, Escriba-AguirV, PomicinoL, LucchettaC, ScriminF, et al. (2009) Violence in the lives of women in Italy who have an elective abortion. Womens Health Issues 19 : 335–343.
30. BourassaD, BerubeJ (2007) The prevalence of intimate partner violence among women and teenagers seeking abortion compared with those continuing pregnancy. J Obstet Gynaecol Can 29 : 415–423.
31. LipskyS, HoltVL, EasterlingTR, CritchlowCW (2005) Police-reported intimate partner violence during pregnancy: who is at risk? Violence Vict 20 : 69–86.
32. Helweg-LarsenK, KruseM (2003) Violence against women and consequent health problems: a register-based study. Scand J Public Health 31 : 51–57.
33. LeungTW, LeungWC, ChanPL, HoPC (2002) A comparison of the prevalence of domestic violence between patients seeking termination of pregnancy and other general gynecology patients. Int J Gynaecol Obstet 77 : 47–54.
34. YiminC, ShouqingLI, ArzhuQU, YukeZ, JianhuaW, et al. (2002) Sexual coercion among adolescent women seeking abortion in China. J Adolesc Health 31 : 482–486.
35. YiminC, BaohuaK, TieyanW, XuejunH, HuanS, et al. (2001) Case-controlled study on relevant factors of adolescent sexual coercion in China. Contraception 64 : 77–80.
36. JonesRK, FrohwirthL, MooreAM (2013) More than poverty: disruptive events among women having abortions in the USA. J Fam Plann Reprod Health Care 39 : 36–43.
37. ElyGE, NugentWR, CerelJ, VimbbaM (2011) The relationship between suicidal thinking and dating violence in a sample of adolescent abortion patients. Crisis 32 : 246–253.
38. ElyGE, OtisMD (2011) An examination of intimate partner violence and psychological stressors in adult abortion patients. J Interpers Violence 26 : 3248–3266.
39. JonesRK, MooreAM, FrohwirthLF (2011) Perceptions of male knowledge and support among U.S. women obtaining abortions. Womens Health Issues 21 : 117–123.
40. JonesR, FinerL (2012) Who has second-trimester abortions in the United States? Contraception 85 : 544–551.
41. RothL, SheederJ, TealSB (2011) Predictors of intimate partner violence in women seeking medication abortion. Contraception 85 : 76–80.
42. SteinbergJR, FinerLB (2011) Examining the association of abortion history and current mental health: a reanalysis of the National Comorbidity Survey using a common-risk-factors model. Soc Sci Med 72 : 72–82.
43. SaftlasAF, WallisAB, ShochetT, HarlandKK, DickeyP, et al. (2010) Prevalence of intimate partner violence among an abortion clinic population. Am J Public Health 100 : 1412–1415.
44. SilvermanJG, DeckerMR, McCauleyHL, GuptaJ, MillerE, et al. (2010) Male perpetration of intimate partner violence and involvement in abortions and abortion-related conflict. Am J Public Health 100 : 1415–1417.
45. Thiel de BocanegraH, RostovtsevaDP, KheraS, GodhwaniN (2010) Birth control sabotage and forced sex: experiences reported by women in domestic violence shelters. Violence Against Women 16 : 601–612.
46. ColemanP, RueV, CoyleC (2009) Induced abortion and intimate relationship quality in the Chicago Health and Social Life Survey. Public Health 123 : 331–338.
47. ElyGE, NugentWR, FlahertyC (2009) The relationship between dating violence and psychosocial problems in a sample of adolescent pregnancy termination patients. Violence Vict 24 : 577–590.
48. PragerSW, SteinauerJE, FosterDG, DarneyPD, DreyEA (2007) Risk factors for repeat elective abortion. Am J Obstet Gynecol 197 : 575.e1–6.
49. KaziS, ReevesMF, CreininMD (2008) The prevalence of domestic violence in volunteers for abortion and contraceptive research studies. Contraception 78 : 79–83.
50. FinerLB, FrohwirthLF, DauphineeLA, SinghS, MooreAM (2005) Reasons U.S. women have abortions: quantitative and qualitative perspectives. Perspect Sex Reprod Health 37 : 110–118.
51. FisherWA, SinghSS, ShuperPA, CareyM, OtchetF, et al. (2005) Characteristics of women undergoing repeat induced abortion. CMAJ 172 : 637–641.
52. HathawayJE, WillisG, ZimmerB, SilvermanJG (2005) Impact of partner abuse on women's reproductive lives. J Am Med Womens Assoc 60 : 42–45.
53. RajA, LiuR, McCleary-SillsJ, SilvermanJG (2005) South Asian victims of intimate partner violence more likely than non-victims to report sexual health concerns. J Immigr Health 7 : 85–91.
54. WooJ, FineP, GoetzlL (2005) Abortion disclosure and the association with domestic violence. Obstet Gynecol 105 : 1329–1334.
55. JanssenPA, HoltVL, SuggNK, EmanuelI, CritchlowCM, et al. (2003) Intimate partner violence and adverse pregnancy outcomes: a population-based study. Am J Obstet Gynecol 188 : 1341–1347.
56. WinnN, RecordsK, RiceM (2003) The relationship between abuse, sexually transmitted diseases, & group B streptococcus in childbearing women. MCN Am J Matern Child Nurs 28 : 106–110.
57. WiebeER, JanssenP (2001) Universal screening for domestic violence in abortion. Womens Health Issues 11 : 436–441.
58. LetourneauEJ, HolmesM, Chasedunn-RoarkJ (1999) Gynecologic health consequences to victims of interpersonal violence. Womens Health Issues 9 : 115–120.
59. GlanderSS, MooreML, MichielutteR, ParsonsLH (1998) The prevalence of domestic violence among women seeking abortion. Obstet Gynecol 91 : 1002–1006.
60. EvinsG, ChescheirN (1996) Prevalence of domestic violence among women seeking abortion services. Womens Health Issues 6 : 204–210.
61. HolmesMM, ResnickHS, KilpatrickDG, BestCL (1996) Rape-related pregnancy: estimates and descriptive characteristics from a national sample of women. Am J Obstet Gynecol 175 : 320–324.
62. TorresA, ForrestJD (1988) Why do women have abortions? Fam Plann Perspect 20 : 169–176.
63. BorinsEF, ForsythePJ (1985) Past trauma and present functioning of patients attending a women's psychiatric clinic. Am J Psychiatry 142 : 460–463.
64. DinizNM, GesteiraSM, LopesRL, Santos MotaR, PerezBA, et al. (2011) [Voluntary abortion and domestic violence among women attended at a public maternity hospital of Salvador-BA.]. Rev Bras Enferm 64 : 1010–1015.
65. LaanpereM, RingmetsI, PartK, KarroH (2013) Intimate partner violence and sexual health outcomes: a population-based study among 16–44-year-old women in Estonia. Eur J Public Health 23 : 688–693.
66. MakenziusM, TydenT, DarjE, LarssonM (2012) Risk factors among men who have repeated experience of being the partner of a woman who requests an induced abortion. Scand J Public Health 40 : 211–216.
67. JohnsonJK, JohnR, HumeraA, KukrejaS, FoundM, et al. (2007) The prevalence of emotional abuse in gynaecology patients and its association with gynaecological symptoms. Eur J Obstet Gynecol Reprod Biol 133 : 95–99.
68. JohnR, JohnsonJK, KukrejaS, FoundM, LindowSW (2004) Domestic violence: prevalence and association with gynaecological symptoms. BJOG 111 : 1128–1132.
69. KeelingJ, BirchL, GreenP (2004) Pregnancy counselling clinic: a questionnaire survey of intimate partner abuse. J Fam Plann Reprod Health Care 30 : 165–168.
70. ZsuzsaG, JenoL, SzilviaA, MariaK (2004) [The psycho-social background factors of induced abortions based on a representative national survey.]. Lege Artis Med 14 : 512–519.
71. HedinLW, JansonPO (2000) Domestic violence during pregnancy. The prevalence of physical injuries, substance use, abortions and miscarriages. Acta Obstet Gynecol Scand 79 : 625–630.
72. PallittoCC, Garcia-MorenoC, JansenHAFM, HeiseL, EllsbergM, et al. (2013) Intimate partner violence, abortion, and unintended pregnancy: results from the WHO Multi-country Study on Women's Health and Domestic Violence. Int J Gynaecol Obstet 120 : 3–9.
73. AntaiD, AdajiS (2012) Community-level influences on women's experience of intimate partner violence and terminated pregnancy in Nigeria: a multilevel analysis. BMC Pregnancy Childbirth 12 : 128.
74. StöcklH, FilippiV, WattsC, MbwamboJK (2012) Induced abortion, pregnancy loss and intimate partner violence in Tanzania: a population based study. BMC Pregnancy Childbirth 12 : 12.
75. AlioAP, SalihuHM, NanaPN, ClaytonHB, MbahAK, et al. (2011) Association between intimate partner violence and induced abortion in Cameroon. Int J Gynaecol Obstet 112 : 83–87.
76. OkenwaL, LawokoS, JanssonB (2011) Contraception, reproductive health and pregnancy outcomes among women exposed to intimate partner violence in Nigeria. Eur J Contracept Reprod Health Care 16 : 18–25.
77. EmenikeE, LawokoS, DalalK (2008) Intimate partner violence and reproductive health of women in Kenya. Int Nurs Rev 55 : 97–102.
78. KayeDK, MirembeFM, BantebyaG, JohanssonA, EkstromAM (2006) Domestic violence as risk factor for unwanted pregnancy and induced abortion in Mulago Hospital, Kampala, Uganda. Trop Med Int Health 11 : 90–101.
79. KayeDK, MirembeF, BantebyaG, JohanssonA, EkstromAM (2005) Reasons, methods used and decision-making for pregnancy termination among adolescents and older women in Mulago Hospital, Uganda. East Afr Med J 82 : 579–585.
80. KayeD (2001) Domestic violence among women seeking post-abortion care. Int J Gynaecol Obstet 75 : 323–325.
81. NairS, RajA, SaggurtiN, NaikDD, DasguptaA, et al. (2013) Reproductive health concerns of women contending with spousal violence and husband's alcohol use in a Mumbai slum community. Int J Gynaecol Obstet 122 : 268–269.
82. NguyenPH, NguyenSV, NguyenMQ, NguyenNT, KeithlySC, et al. (2012) The association and a potential pathway between gender-based violence and induced abortion in Thai Nguyen province, Vietnam. Glob Health Action 5 : 1–11.
83. ShahN, HossainN, NoonariM, KhanNH (2011) Maternal mortality and morbidity of unsafe abortion in a university teaching hospital of Karachi, Pakistan. J Pak Med Assoc 61 : 582–586.
84. KalyanwalaS, ZavierAJF, JejeebhoyS, KumarR (2010) Abortion experiences of unmarried young women in India: evidence from a facility-based study in Bihar and Jharkhand. Int Perspect Sex Reprod Health 36 : 62–71.
85. Lee-RifeSM (2010) Women's empowerment and reproductive experiences over the lifecourse. Soc Sci Med 71 : 634–642.
86. SilvermanJG, GuptaJ, DeckerMR, KapurN, RajA (2007) Intimate partner violence and unwanted pregnancy, miscarriage, induced abortion, and stillbirth among a national sample of Bangladeshi women. BJOG 114 : 1246–1252.
87. LeungTW, LeungWC, NgEHY, HoPC (2005) Quality of life of victims of intimate partner violence. Int J Gynaecol Obstet 90 : 258–262.
88. WuJ, GuoS, QuC (2005) Domestic violence against women seeking induced abortion in China. Contraception 72 : 117–121.
89. FanslowJ, SilvaM, WhiteheadA, et al. (2008) Pregnancy outcomes and intimate partner violence in New Zealand. Aust N Z J Obstet Gynaecol 48 : 391–397.
90. WhiteheadA, FanslowJ (2005) Prevalence of family violence amongst women attending an abortion clinic in New Zealand. Aust N Z J Obstet Gynaecol 45 : 321–324.
91. TaftA, WatsonL, LeeC (2004) Violence against young Australian women and associations with reproductive events: a cross-sectional analysis of a national sample. Aust N Z J Public Health 28 : 324–329.
92. WebsterJ, ChandlerJ, BattistuttaD (1996) Pregnancy outcomes and health care use: effects of abuse. Am J Obstet Gynecol 174 : 760–767.
93. KalyanwalaS, JejeebhoySJ, ZavierAJF, KumarR (2012) Experiences of unmarried young abortion-seekers in Bihar and Jharkhand, India. Cult, Health Sex 14 : 241–255.
94. PuriS, AdamsV, IveyS, NachtigallRD (2011) “There is such a thing as too many daughters, but not too many sons”: qualitative study of son preference and fetal sex selection among Indian immigrants in the United States. Soc Sci Med 72 : 1169–1176.
95. WilliamsGB, BrackleyMH (2009) Intimate partner violence, pregnancy and the decision for abortion. Issues Ment Health Nurs 30 : 272–278.
96. BeltonS (2007) Borders of fertility: unplanned pregnancy and unsafe abortion in Burmese women migrating to Thailand. Health Care Women Int 28 : 419–433.
97. RenkerPR (2002) “Keep a blank face. I need to tell you what has been happening to me.”: teens' stories of abuse and violence before and during pregnancy. MCN Am J Matern Child Nurs 27 : 109–116.
98. SouzaVL, FerreiraSL (2000) [Impact of spouse violence on the decision to have an abortion]. Rev Bras Enferm 53 : 375–385.
99. JewkesR, WattsC, AbrahamsN, Penn-KekanaL, Garcia-MorenoC (2000) Ethical and methodological issues in conducting research on gender-based violence in Southern Africa. Reprod Health Matters 8 : 93–103.
100. CokerAL (2007) Does physical intimate partner violence affect sexual health? A systematic review. Trauma Violence Abuse 8 : 149–177.
101. EllsbergM, JansenHA, HeiseL, WattsCH, Garcia-MorenoC, et al. (2008) Intimate partner violence and women's physical and mental health in the WHO multi-country study on women's health and domestic violence: an observational study. Lancet 371 : 1165–1172.
102. ShahPS, ShahJ (2010) Knowledge Synthesis Group on Determinants of Preterm LBWB (2010) Maternal exposure to domestic violence and pregnancy and birth outcomes: a systematic review and meta-analyses. J Womens Health (Larchmt) 19 : 2017–2031.
103. WuV, HuffH, BhandariM (2010) Pattern of physical injury associated with intimate partner violence in women presenting to the emergency department: a systematic review and meta-analysis. Trauma Violence Abuse 11 : 71–82.
104. TrevillionK, OramS, FederG, HowardLM (2012) Experiences of domestic violence and mental disorders: a systematic review and meta-analysis. PLoS ONE 7: e51740 doi:10.1371/journal.pone.0051740
105. Department of Health (2010/11) Guidance on the NHS standard contract for community services 2010/11. Available: http://webarchive.nationalarchives.gov.uk/20130107105354/http://www.dh.gov.uk/prod_consum_dh/groups/dh_digitalassets/dh/en/ps/documents/digitalasset/dh_111266.pdf. Accessed 10 March 2013.
106. O'ReillyR, BealeB, GilliesD (2010) Screening and intervention for domestic violence during pregnancy care: a systematic review. Trauma Violence Abuse 11 : 190–201.
107. O'CampoP, KirstM, TsamisC, ChambersC, AhmadF (2011) Implementing successful intimate partner violence screening programs in health care settings: evidence generated from a realist-informed systematic review. Soc Sci Med 72 : 855–866.
108. Nelson HD, Bougatsos C, Blazina I (2012) Screening women for intimate partner violence and elderly and vulnerable adults for abuse: systematic review to update the 2004 U.S. Preventive Services Task Force recommendation. Rockville (Maryland): Agency for Healthcare Research and Quality.
109. MoyerVA (2013) Screening for intimate partner violence and abuse of elderly and vulnerable adults: U.S. Preventive Services Task Force recommendation statement. Ann Int Med 158 : 478–486.
110. National Institute for Health and Care Excellence (2013) Domestic violence and abuse—identification and prevention. Available: http://guidance.nice.org.uk/PHG/44. Accessed 3 December 2013.
111. Lee R, Stanko E (2002) Researching violence: methodology and measurement. London: Routledge.
112. RamsayJ, CarterY, DavidsonL, DunneD, EldridgeS, et al. (2009) Advocacy interventions to reduce or eliminate violence and promote the physical and psychosocial well-being of women who experience intimate partner abuse. Cochrane Database Syst Rev 2009: CD005043.
113. JahanfarS, JanssenPA, HowardLM, DowswellT (2013) Interventions for preventing or reducing domestic violence against pregnant women. Cochrane Database Syst Rev 2013: CD009414.
114. CismaruM, LavackAM (2011) Campaigns targeting perpetrators of intimate partner violence. Trauma Violence Abuse 12 : 183–197.
115. Bacchus L, Aston G, Torres Vitolas C, Jordan P, Murray SF (2007) A theory-based evaluation of a multi-agency domestic violence service at Guy's and St Thomas' NHS Foundation Trust. Available: http://www.caada.org.uk/policy/Bacchus-et-al-2007-full-report-MOZAIC.pdf. Accessed 12 December 2013.
116. GranjaAC, ZacariasE, BergstromS (2002) Violent deaths: the hidden face of maternal mortality. BJOG 109 : 5–8.
117. GisslerM, BergC, Bouvier-ColleMH, BuekensP (2005) Injury deaths, suicides and homicides associated with pregnancy, Finland 1987–2000. Eur J Public Health 15 : 459–463.
118. GrossmanD, EllertsonC, GrimesDA, WalkerD (2004) Routine follow-up visits after first-trimester induced abortion. Obstet Gynecol 103 : 738–745.
119. HegartyK, O'DohertyL, TaftA, ChondrosP, BrownS, et al. (2013) Screening and counselling in the primary care setting for women who have experienced intimate partner violence (WEAVE): a cluster randomised controlled trial. Lancet 382 : 249–258.
120. JewkesR (2013) Intimate partner violence: the end of routine screening. Lancet 382 : 190–191.
121. World Health Organization (2013) Responding to intimate partner violence and sexual violence against women: WHO clinical and policy guidelines. Geneva: World Health Organization.
Štítky
Interní lékařství
Článek vyšel v časopisePLOS Medicine
Nejčtenější tento týden
2014 Číslo 1- Berberin: přírodní hypolipidemikum se slibnými výsledky
- Příznivý vliv Armolipidu Plus na hladinu cholesterolu a zánětlivé parametry u pacientů s chronickým subklinickým zánětem
- Červená fermentovaná rýže účinně snižuje hladinu LDL cholesterolu jako vhodná alternativa ke statinové terapii
- Léčba bolesti u seniorů
- Jak postupovat při výběru betablokátoru − doporučení z kardiologické praxe
-
Všechny články tohoto čísla
- Soon Will Be Ten: A Call for Papers on the Health of Pre-adolescent Children
- Home Blood Pressure Monitoring: New Evidence for an Expanded Role
- Cervical Cancer Screening in Older Women: New Evidence and Knowledge Gaps
- Taxes on Sugar-Sweetened Beverages to Curb Future Obesity and Diabetes Epidemics
- The Failure of Screening and Treating as a Malaria Elimination Strategy
- Averting Obesity and Type 2 Diabetes in India through Sugar-Sweetened Beverage Taxation: An Economic-Epidemiologic Modeling Study
- Managing Incidental Genomic Findings in Clinical Trials: Fulfillment of the Principle of Justice
- Associations between Intimate Partner Violence and Termination of Pregnancy: A Systematic Review and Meta-Analysis
- Developing a Sustainable Nutrition Research Agenda in Sub-Saharan Africa—Findings from the SUNRAY Project
- Scale-up of Malaria Rapid Diagnostic Tests and Artemisinin-Based Combination Therapy: Challenges and Perspectives in Sub-Saharan Africa
- Preterm Birth and Childhood Wheezing Disorders: A Systematic Review and Meta-Analysis
- Cervical Screening at Age 50–64 Years and the Risk of Cervical Cancer at Age 65 Years and Older: Population-Based Case Control Study
- Improving Women's Health through Universal Health Coverage
- A Risk Prediction Model for the Assessment and Triage of Women with Hypertensive Disorders of Pregnancy in Low-Resourced Settings: The miniPIERS (Pre-eclampsia Integrated Estimate of RiSk) Multi-country Prospective Cohort Study
- Risk Stratification by Self-Measured Home Blood Pressure across Categories of Conventional Blood Pressure: A Participant-Level Meta-Analysis
- Impact of Intermittent Screening and Treatment for Malaria among School Children in Kenya: A Cluster Randomised Trial
- Muscle-Strengthening and Conditioning Activities and Risk of Type 2 Diabetes: A Prospective Study in Two Cohorts of US Women
- PLOS Medicine
- Archiv čísel
- Aktuální číslo
- Informace o časopisu
Nejčtenější v tomto čísle- Associations between Intimate Partner Violence and Termination of Pregnancy: A Systematic Review and Meta-Analysis
- Risk Stratification by Self-Measured Home Blood Pressure across Categories of Conventional Blood Pressure: A Participant-Level Meta-Analysis
- A Risk Prediction Model for the Assessment and Triage of Women with Hypertensive Disorders of Pregnancy in Low-Resourced Settings: The miniPIERS (Pre-eclampsia Integrated Estimate of RiSk) Multi-country Prospective Cohort Study
- Scale-up of Malaria Rapid Diagnostic Tests and Artemisinin-Based Combination Therapy: Challenges and Perspectives in Sub-Saharan Africa
Kurzy
Zvyšte si kvalifikaci online z pohodlí domova
Současné možnosti léčby obezity
nový kurzAutoři: MUDr. Martin Hrubý
Všechny kurzyPřihlášení#ADS_BOTTOM_SCRIPTS#Zapomenuté hesloZadejte e-mailovou adresu, se kterou jste vytvářel(a) účet, budou Vám na ni zaslány informace k nastavení nového hesla.
- Vzdělávání