-
Články
Top novinky
Reklama- Vzdělávání
- Časopisy
Top články
Nové číslo
- Témata
Top novinky
Reklama- Videa
- Podcasty
Nové podcasty
Reklama- Kariéra
Doporučené pozice
Reklama- Praxe
Top novinky
ReklamaThe Effectiveness of Emergency Obstetric Referral Interventions in Developing Country Settings: A Systematic Review
Background:
Pregnancy complications can be unpredictable and many women in developing countries cannot access health facilities where life-saving care is available. This study assesses the effects of referral interventions that enable pregnant women to reach health facilities during an emergency, after the decision to seek care is made.Methods and findings:
Selected bibliographic databases were searched with no date or language restrictions. Randomised controlled trials and quasi experimental study designs with a comparison group were included. Outcomes of interest included maternal and neonatal mortality and other intermediate measures such as service utilisation. Two reviewers independently selected, appraised, and extracted articles using predefined fields. Forest plots, tables, and qualitative summaries of study quality, size, and direction of effect were used for analysis.
Nineteen studies were included. In South Asian settings, four studies of organisational interventions in communities that generated funds for transport reduced neonatal deaths, with the largest effect seen in India (odds ratio 0·48 95% CI 0·34–0·68). Three quasi experimental studies from sub-Saharan Africa reported reductions in stillbirths with maternity waiting home interventions, with one statistically significant result (OR 0.56 95% CI 0.32–0.96). Effects of interventions on maternal mortality were unclear. Referral interventions usually improved utilisation of health services but the opposite effect was also documented. The effects of multiple interventions in the studies could not be disentangled. Explanatory mechanisms through which the interventions worked could not be ascertained.Conclusions:
Community mobilisation interventions may reduce neonatal mortality but the contribution of referral components cannot be ascertained. The reduction in stillbirth rates resulting from maternity waiting homes needs further study. Referral interventions can have unexpected adverse effects. To inform the implementation of effective referral interventions, improved monitoring and evaluation practices are necessary, along with studies that develop better understanding of how interventions work.
: Please see later in the article for the Editors' Summary
Published in the journal: . PLoS Med 9(7): e32767. doi:10.1371/journal.pmed.1001264
Category: Research Article
doi: https://doi.org/10.1371/journal.pmed.1001264Summary
Background:
Pregnancy complications can be unpredictable and many women in developing countries cannot access health facilities where life-saving care is available. This study assesses the effects of referral interventions that enable pregnant women to reach health facilities during an emergency, after the decision to seek care is made.Methods and findings:
Selected bibliographic databases were searched with no date or language restrictions. Randomised controlled trials and quasi experimental study designs with a comparison group were included. Outcomes of interest included maternal and neonatal mortality and other intermediate measures such as service utilisation. Two reviewers independently selected, appraised, and extracted articles using predefined fields. Forest plots, tables, and qualitative summaries of study quality, size, and direction of effect were used for analysis.
Nineteen studies were included. In South Asian settings, four studies of organisational interventions in communities that generated funds for transport reduced neonatal deaths, with the largest effect seen in India (odds ratio 0·48 95% CI 0·34–0·68). Three quasi experimental studies from sub-Saharan Africa reported reductions in stillbirths with maternity waiting home interventions, with one statistically significant result (OR 0.56 95% CI 0.32–0.96). Effects of interventions on maternal mortality were unclear. Referral interventions usually improved utilisation of health services but the opposite effect was also documented. The effects of multiple interventions in the studies could not be disentangled. Explanatory mechanisms through which the interventions worked could not be ascertained.Conclusions:
Community mobilisation interventions may reduce neonatal mortality but the contribution of referral components cannot be ascertained. The reduction in stillbirth rates resulting from maternity waiting homes needs further study. Referral interventions can have unexpected adverse effects. To inform the implementation of effective referral interventions, improved monitoring and evaluation practices are necessary, along with studies that develop better understanding of how interventions work.
: Please see later in the article for the Editors' SummaryIntroduction
The importance of referral in an obstetric emergency is related to the unpredictability of pregnancy complications and their potential to progress rapidly to become severe and life threatening. For example, a serious haemorrhage can lead to death of a woman and the unborn fetus within minutes or hours [1],[2]. In the poorest countries, two-thirds of women deliver at home, far from emergency services or without access to a health professional [3]. Maternal and neonatal deaths could therefore be prevented if functional referral systems were in place to allow pregnant women to reach appropriate health services when complications occur. A recent systematic review of maternal health initiatives indicated that the most successful programmes included the establishment of referral systems as a component [4].
The three delays model provides a conceptual framework of the factors influencing the timely arrival to appropriate care in obstetric emergencies [5]. The “three delays” are (I) delays in the recognition of the problem and the decision to seek care in the household, (II) delays in reaching the appropriate facility, and (III) delays in the care received once the woman reaches the facility. The delays of interest in this review are the phase II delays—those experienced after the decision to seek care is made, and before obtaining adequate care.
Figure 1 depicts the conceptual framework for this review, which was originally proposed by Thaddeus & Maine [5]. The reasons that phase II delays occur have been well documented and include difficult geographical terrain, costs of transport, lack of phones and vehicles, suboptimal distribution and location of health facilities, and poor decision making of health professionals [5],[6], so interventions usually address these barriers. Although the problems identified in the diagram are presented as distinct from each other, it is likely that they are interlinked, so one intervention might affect more than one problem area or lead to several consequences. For example, if a health facility was placed nearer to women's homes to improve the distribution of services, it is possible that access to a phone or specialised emergency vehicle might also be improved. The new health facility may lead to positive consequences (such as decreased travel time or increased utilisation of the service, which may result in decreased maternal morbidity and mortality), but may also have negative or unintended effects (for example, if the health provider in the facility is over worked and does not effectively carry out triage of cases, s/he may cause delays in referring the most urgent cases).
Fig. 1. Conceptual framework for the review. 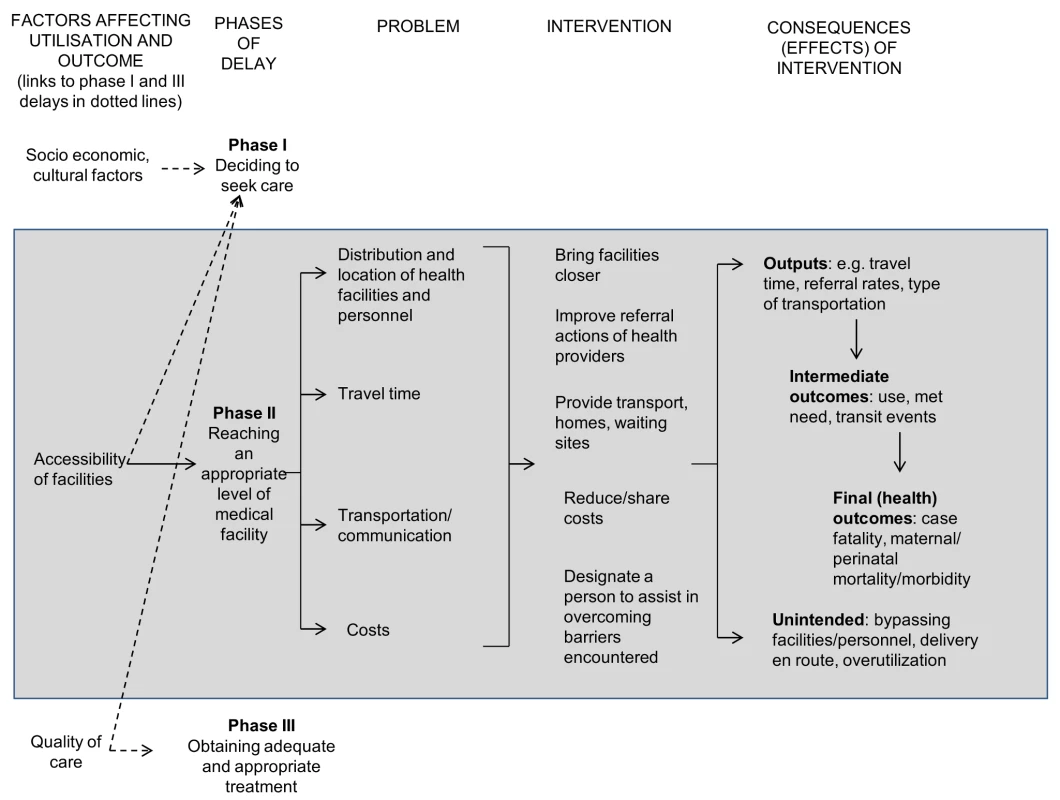
A large number of interventions to overcome phase II delays are being implemented within maternal mortality reduction programmes. Many report improvements, especially in terms of health service indicators such as referral rates and utilization. Reviews of the literature have so far not attempted to systematically collate and appraise the reported effects. This systematic review aims to assess the effects of emergency obstetric referral interventions that overcome phase II delays, enabling pregnant women to reach health facilities in developing countries.
Methods
PRISMA guidelines (Text S1) and a study protocol (Text S2) were used as a basis for the overall study approach.
Inclusion and Exclusion Criteria
Studies of referral systems for emergency maternity care from published and grey literature were included if they were randomised controlled trials (RCTs) or other quasi experimental study designs—i.e., studies lacking randomisation such as controlled before-after (CBA) studies and interrupted time series (ITS)—provided comparison groups were available. Participants were pregnant and post partum women with an obstetric complication, referred as an emergency from the community or from a primary care centre to a higher level comprehensive emergency obstetric care facility. Interventions included aimed to overcome delays in reaching the appropriate facility (phase II delay), which improved emergency referrals antenatally, during labour, or up to 42 d after delivery. Examples of interventions of interest were technologies such as telephones, radios, and vehicles for transport; financing and incentive schemes; guidelines and protocols to help health professionals make decisions on referrals; reorganisation of care systems (such as introducing intermediate services like maternity waiting homes or by linking different referral modalities); and mobilisation of community members (including traditional birth attendants) to actively participate in referral activities (such as accompany the women or drive vehicles). Interventions that addressed phase II delays, combined with those that improved phase I and III delays, were included. Studies from low - and middle-income developing countries as classified by the World Bank [7] were eligible.
Studies with no comparison group, and interventions that referred the newborn, women without maternity related conditions, non-emergency cases, and between hospitals were excluded. Interventions that only improved phase I and III delays were omitted. Studies in refugee, war zone, and mass casualty settings were not included as these special settings were likely to confound the effect of obstetric referral. Interventions to change traditional birth attendants' (and other lay carers of pregnant women) decision making for referral were not included (unless there was active engagement of the carer in enabling transfer to a facility), as we considered these to mainly affect decision making. Isolated interventions to introduce first-aid practices to stabilise or treat the woman during referral (such as training community health workers in special procedures) were excluded as these procedures do not affect the delay in reaching a facility but enable improvement of the woman's condition while awaiting transfer. First aid is, however, normal practice during referral and if it was provided as part of an intervention to reduce phase II delays, the study would be included.
The outcomes of interest were guided by the conceptual framework (Figure 1). These were: maternal and neonatal mortality comprising stillbirths, live births, and case fatalities; intermediate outcomes such as utilisation levels and care for maternal complications (expressed as the “met need for obstetric care,” which is the proportion of complications seen to expected); and outputs or processes such as travel time, referral rates, type of transport or communication, costs (payments for transport, health facility fees, and loss of income), women's knowledge of pregnancy or post partum complications, and satisfaction with the intervention.
Search Strategy
The electronic search strategy was based on terms related to referral, transport, or transfer, in obstetric emergencies and conducted between July and November 2010. The full search strategy is available as Text S3. It was run in MEDLINE, then adapted for the following databases: EMBASE, CAB abstracts, Cochrane Central Register of Controlled Trials (CENTRAL), CINAHL, and Effective Pregnancy and Organisation of Care (EPOC) by selecting appropriate MeSH and/or keywords from their respective thesauri with no date or language restrictions. The search was subsequently extended to LILACS and the African Index Medicus. Electronic search citations were downloaded using Reference Manager 12. Reference lists from retrieved papers were screened. Published and grey literature was included at this point. Authors were contacted to ask for additional information if required.
Data Extraction, Quality Assessment, and Analysis
Appraisal of titles, abstracts, and full text articles was conducted independently by two reviewers on the basis of the inclusion and exclusion criteria. Disagreements were resolved by discussion among all members of the review team.
Quality assessment was guided by Effective Public Health Practice Project criteria [8], summarised in Table 1. Two reviewers independently assigned quality scores and compared judgements. Uncertainties were resolved through arbitration with one other reviewer.
Tab. 1. Quality assessment summary table. 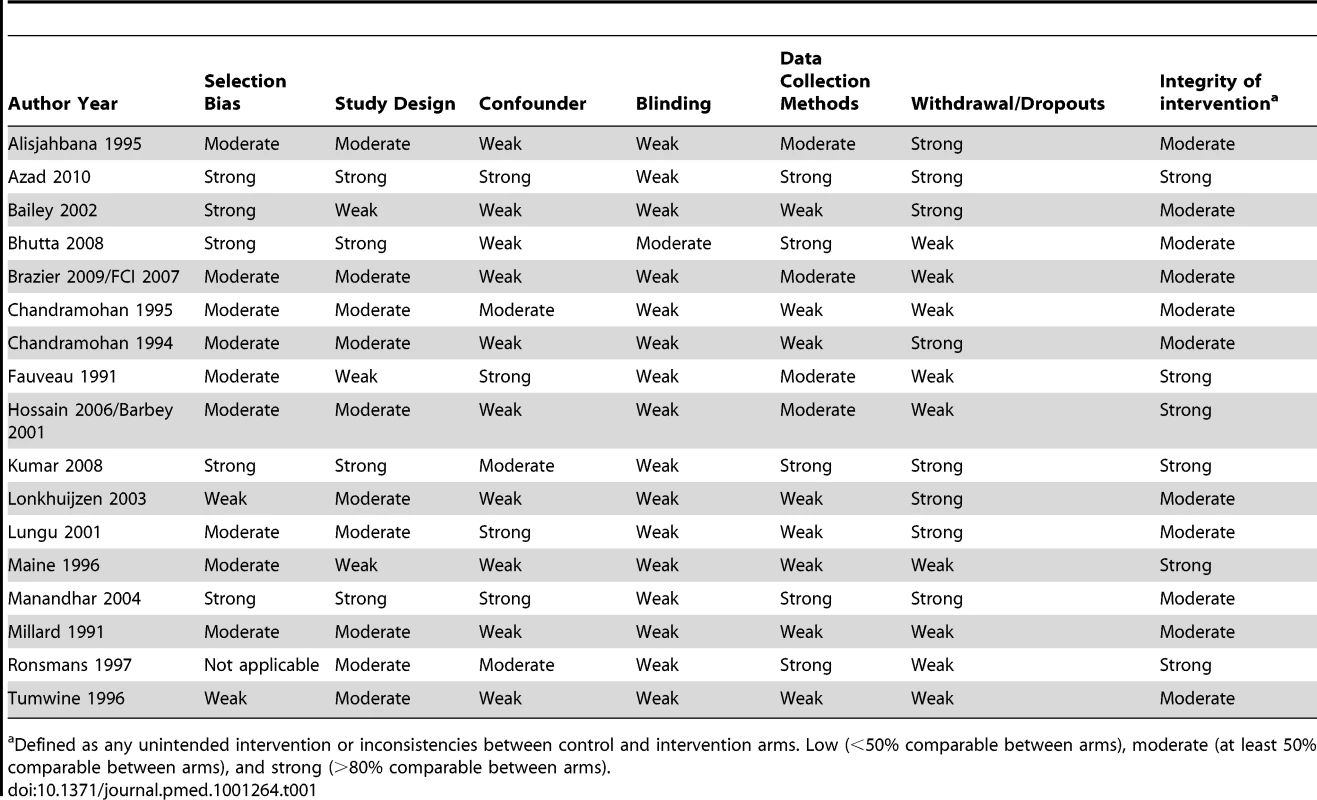
Defined as any unintended intervention or inconsistencies between control and intervention arms. Low (<50% comparable between arms), moderate (at least 50% comparable between arms), and strong (>80% comparable between arms). Synthesis of the studies involved categorising interventions by their characteristics, narrating and summarising study quality, size and direction of effect, and presenting data visually as odds ratios, forest plots, and tables. Data extraction and analyses was done with Review Manager Version 5. In our analysis, the effect estimates of cluster RCTs were corrected to account for this design using inverse variance. Denominators used were based on the total numbers of pregnant women, live births, or total births (in the case of stillbirths) in the catchment areas of the respective studies.
Results
The search results are summarised in Figure 2. Nineteen papers met the study criteria, describing 14 different interventions (Table 2).
Fig. 2. Study selection flow chart. 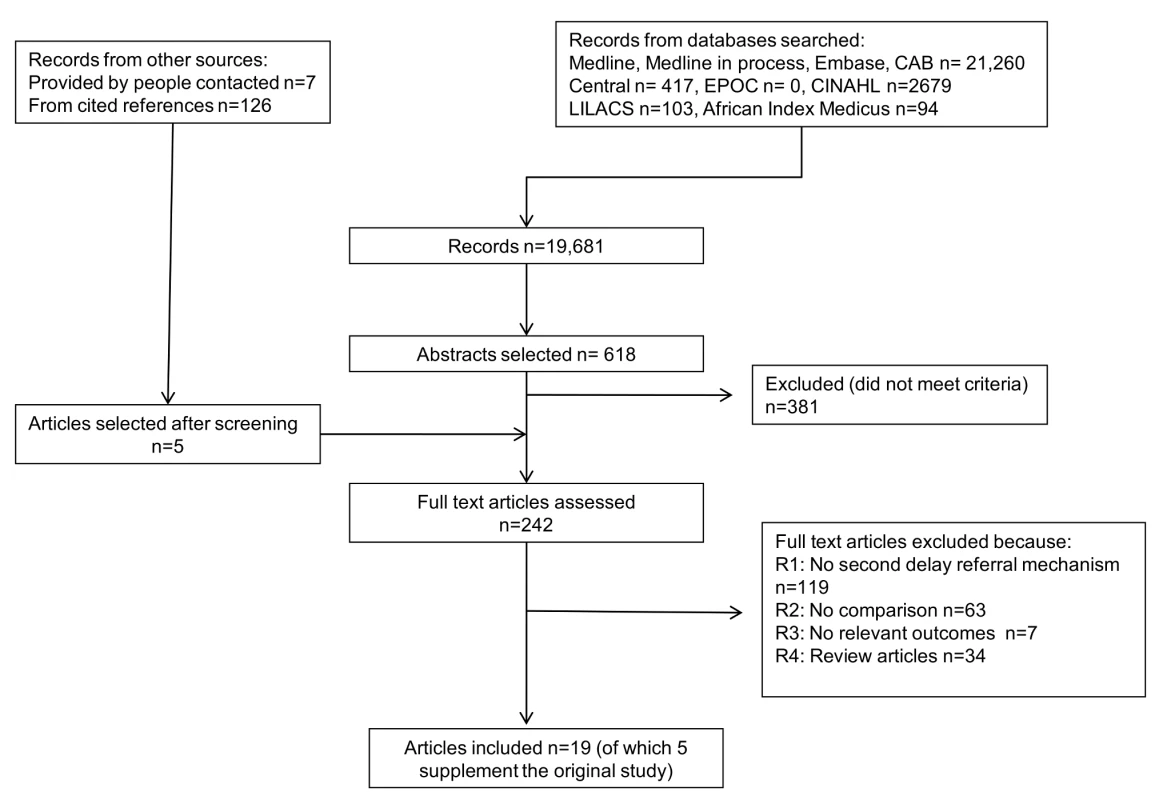
Tab. 2. Summary of characteristics of included studies. 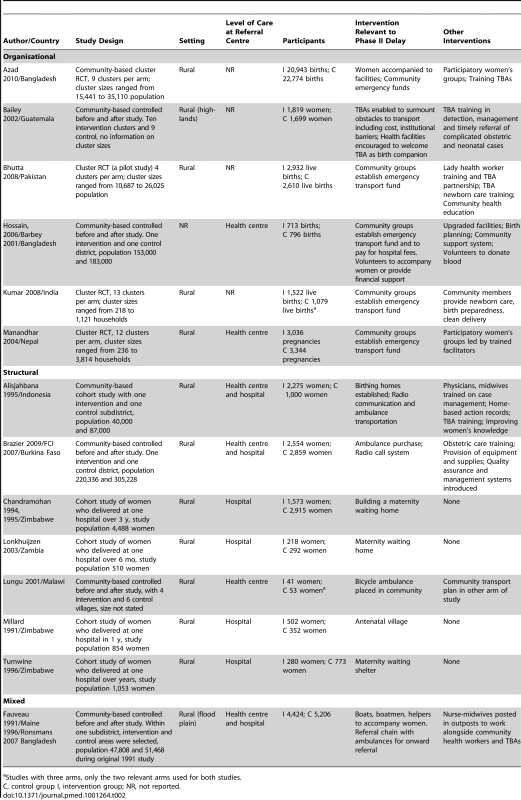
Studies with three arms, only the two relevant arms used for both studies. Description of Studies
The studies were categorised using the EPOC taxonomy of interventions for practice change [9]. Fourteen interventions from 19 papers were included in this review. Of the 14 interventions, six were organisational in nature and seven structural. One study used structural and organisational mechanisms to enhance various types and levels of transport and the linkages between them. Interventions in a number of the included studies comprised several components, some of which were not related to referral.
The six organisational interventions involved surmounting obstacles to emergency transport, especially those of cost. All targeted women and community members including traditional birth attendants (TBAs) [10]–[16]. In five studies, community groups were organised to generate emergency funds for transport [10],[12]–[16]. Some of these studies indicated that the idea of emergency funds was generated through community mobilisation activities and was not pre-decided [10],[16], although the origin of the intervention was not so clearly described in other studies. The study in the rural highlands of Guatemala [11] comprised slightly different organisational mechanisms. In this study, TBAs accompanied women to health facilities, helped women surmount cost barriers, and were welcomed as birth companions in health facilities. None of the interventions solely addressed phase II delays and included other components such as improving integration between different health providers [12], education and awareness raising of complications [10],[15], and upgrading of facilities [13]. The organisational interventions included 4 RCTs. All were cluster randomised studies. In three of the RCTs [10],[15],[16], the authors of the original articles described their method of analysis, taking clustering into account and by intention to treat. One RCT [12] was a pilot study and details of how clustering was taken into account was not clear.
There were seven structural interventions that involved the use of maternity waiting homes, radios, and ambulances to overcome phase II delays [17]–[25]. Various forms of maternity or birthing homes were established, where pregnant women could stay, away from their own homes but close to a health facility. In Indonesia [17], the birthing home was located near a rural health centre and combined with several other health service improvements that addressed other phases of delay. The four sub-Saharan African studies described maternity waiting homes located close to a hospital [20]–[22],[24],[25] and were not combined with other interventions. The way in which the maternity waiting homes were used varied. Some women stayed because of risk factors or complications while others stayed by choice, even if there was no medical reason to do so. A transport intervention was studied in Malawi, where bicycles with an attached stretcher on wheels were located in the community [23]. In Burkina Faso and Indonesia, vehicles and radio communications were provided, but these were put into place alongside a variety of other interventions which affected phase I and II delays [17]–[19].
One intervention in Bangladesh included both organisational and structural characteristics [26]–[28]. Boats and ambulances were provided and in addition to these structural transportation elements, organisational traits were included such as assignment of boatmen and helpers to accompany women and improvement of linkages for onward referral to a district hospital and deployment of staff.
Four interventions were described in more than one paper. In the organisational intervention from Bangladesh [13],[14], the findings on effectiveness were found in the published paper [13], while the report [14] was used to provide details relating to the intervention and to confirm our understanding of the findings in the published paper. The same was done with the papers from Burkina Faso [18],[19]. In the case of the two papers on the maternity waiting home intervention in Zimbabwe [20],[21], one paper reported effects on maternal outcomes, and the other on perinatal mortality, so the two papers were used to extract information on different outcomes for the same intervention. In the mixed intervention from Bangladesh, the original paper [26] described the intervention and its effects on maternal mortality covering only the 3 y before and the 3 y after implementation of the intervention. The subsequent paper [28] reported on care for maternal complications and utilisation of services, using data from the original period and area. The third paper [27] presented maternal mortality data from the same geographical area in relation to the same intervention (which continued after the original study), but over a longer time period, covering the 11 y before and 7 y after the intervention.
All studies collected community-based data and provided information on outcomes at the population level, with the exception of the four maternity waiting home studies [20]–[22],[24],[25] and the study by Maine and colleagues [28], where the outcomes were in women attending hospital for delivery.
Effects of Interventions on Health Outcomes
Seven papers provided maternal mortality data (Figure 3). The three RCTs of community-targeted organisational interventions [10],[12],[16] showed varying effects, the sample sizes of the individual studies were not of adequate magnitude to measure this outcome with statistical confidence.
Fig. 3. Effects of interventions on maternal deaths per live births. 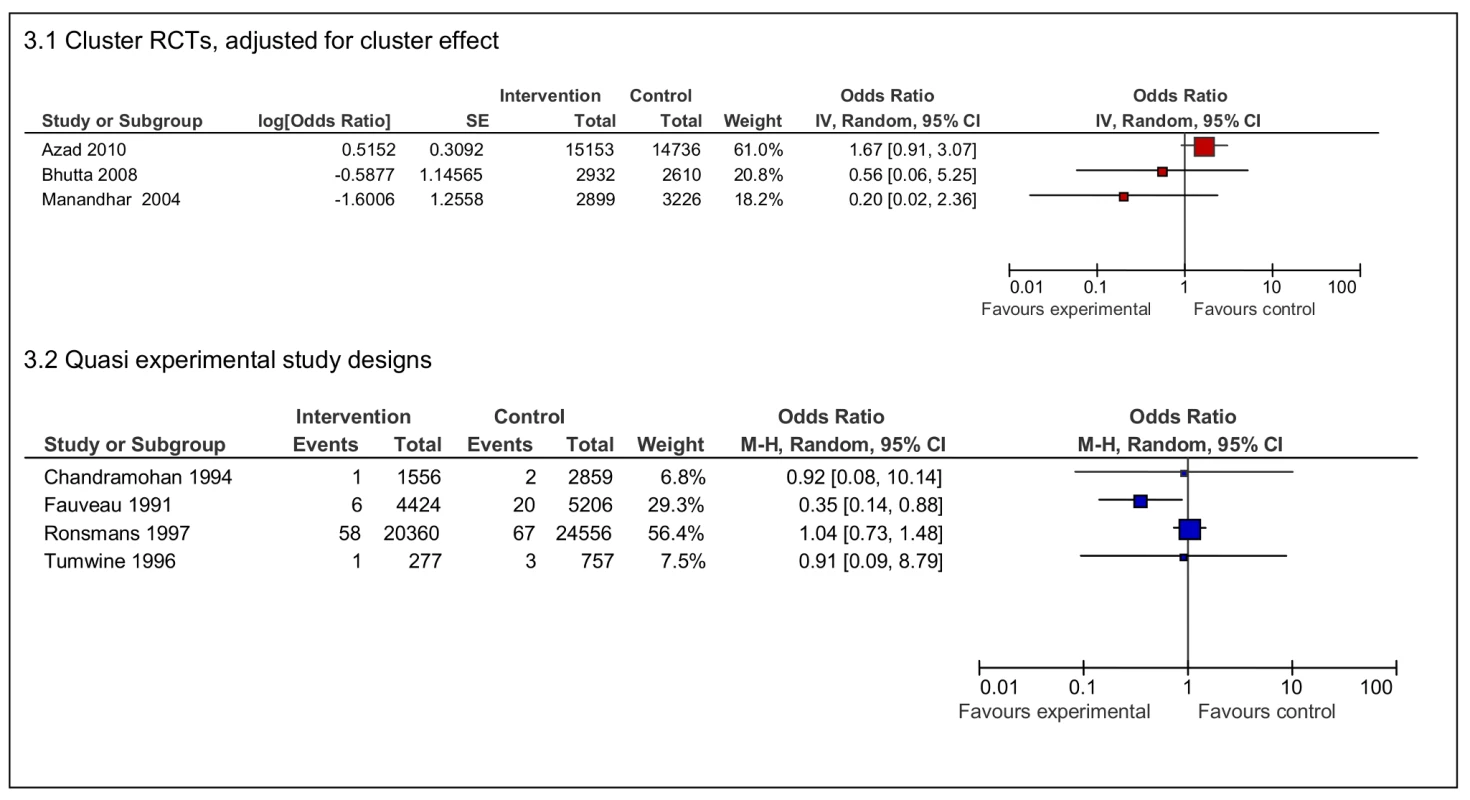
Of the quasi experimental studies reporting maternal mortality, the mixed organisational-structural intervention [26], which included transport improvements but also health staff deployment, showed a reduction in maternal mortality (odds ratio [OR] 0·35 95% CI 0·14–0·88), yet the study of the same intervention in the same site, which analysed mortality trends over a longer time, did not show the reduction to be sustained [27]. Two studies of maternity waiting homes [20],[25] had small numbers of maternal deaths confined to a hospital population and did not show reductions in maternal mortality. Maternal case fatality was only available from one study (forest plot not provided), which showed no difference between intervention and control groups (OR 0·68 95% CI 0·06–7·69) [28].
Neonatal deaths in four RCTs [10],[12],[15],[16] of organisational interventions were reduced, although the effects found were not equally strong (Figure 4). The largest effect was shown in the study from India (OR 0·48 95% CI 0·34–0·68) [15]. Neonatal deaths were also reduced in the quasi experimental studies of maternity waiting homes, although statistical significance was not demonstrated in these studies.
Fig. 4. Effects of interventions on neonatal deaths per live births. 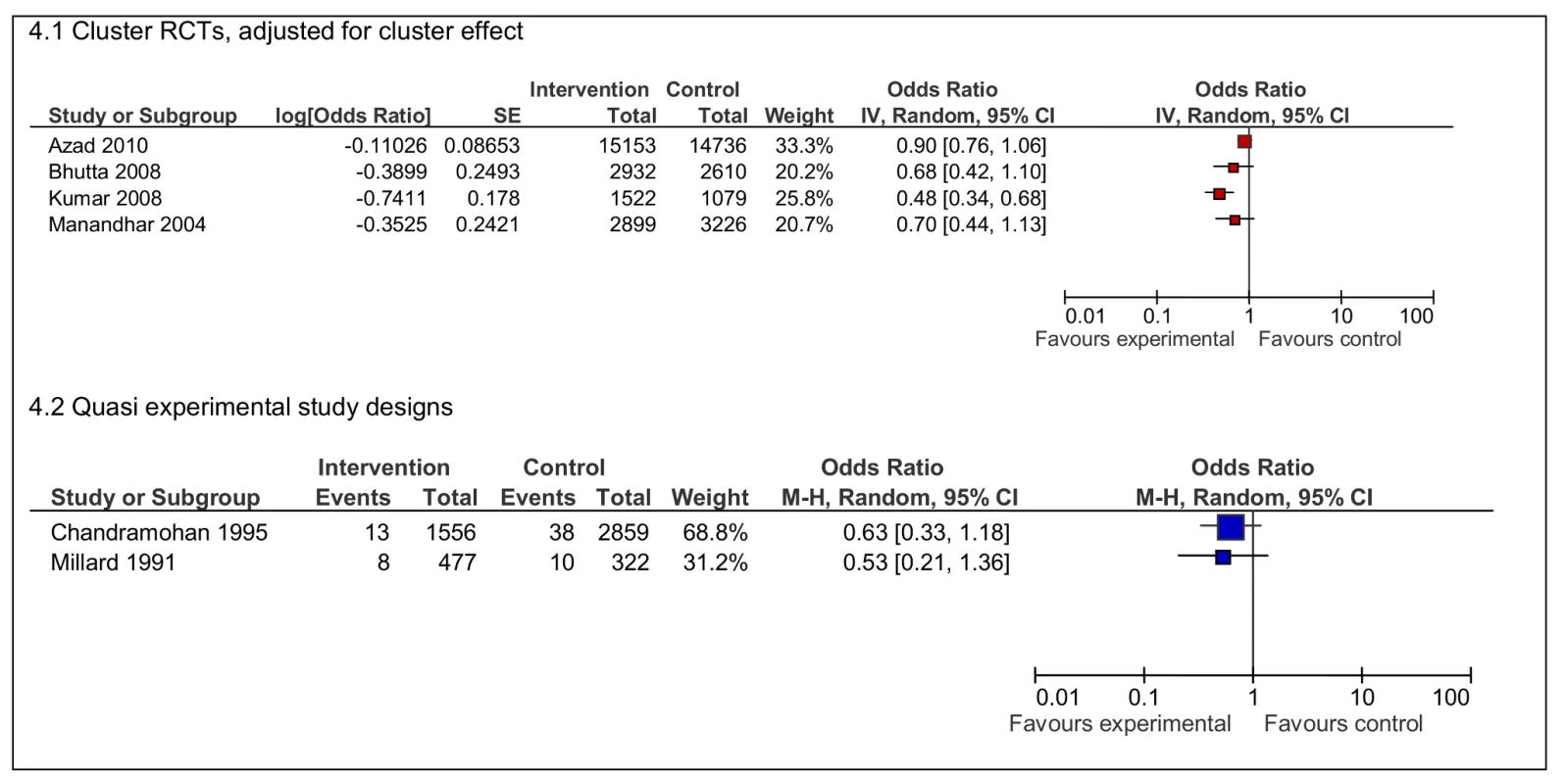
There is less consistency in the data on stillbirths (Figure 5). Two RCTs demonstrate improvements in the intervention group [12],[15] but the ORs were close to one in the other two RCTs. Three quasi experimental studies on maternity waiting homes [21],[24],[25] demonstrated reductions in stillbirths, with one statistically significant result from Zimbabwe (OR 0.56 95% CI 0.32–0.96) [21].
Fig. 5. Effects of interventions on stillbirths per total live births. 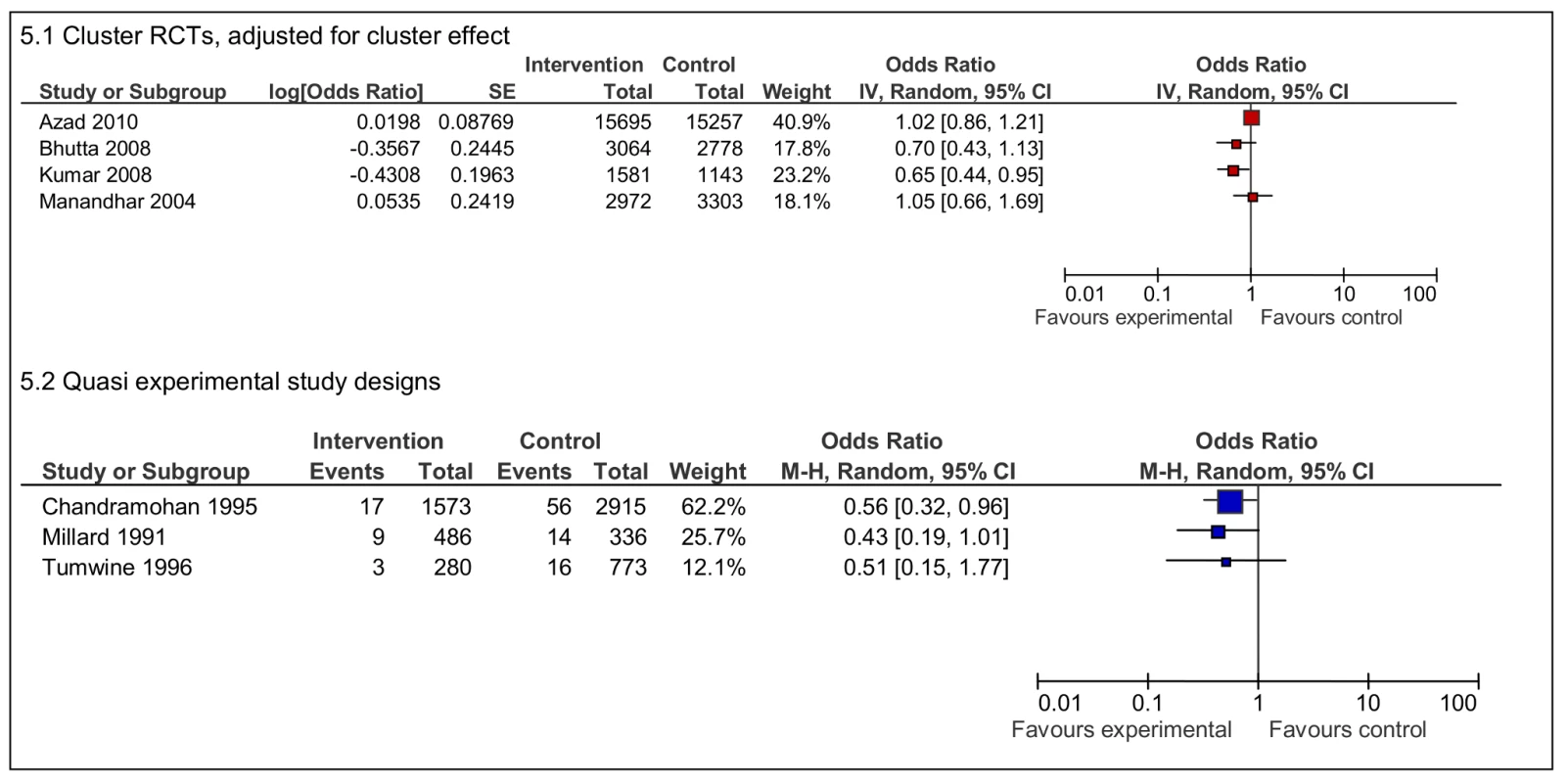
Other Effects of Interventions
Table 3 summarises the data available on outputs and intermediate effects of the various referral interventions. ORs could not be calculated for a number of studies because of a lack of data. Four studies: two organisational [15],[16] and two structural [17],[18], reported a higher proportion of deliveries with health professionals. One study [10] observed a lower rate in the intervention arm, but uptake of health services was noted to be higher in the control group even before the intervention.
Tab. 3. Summary table of intermediate outcomes and process measures, after intervention. 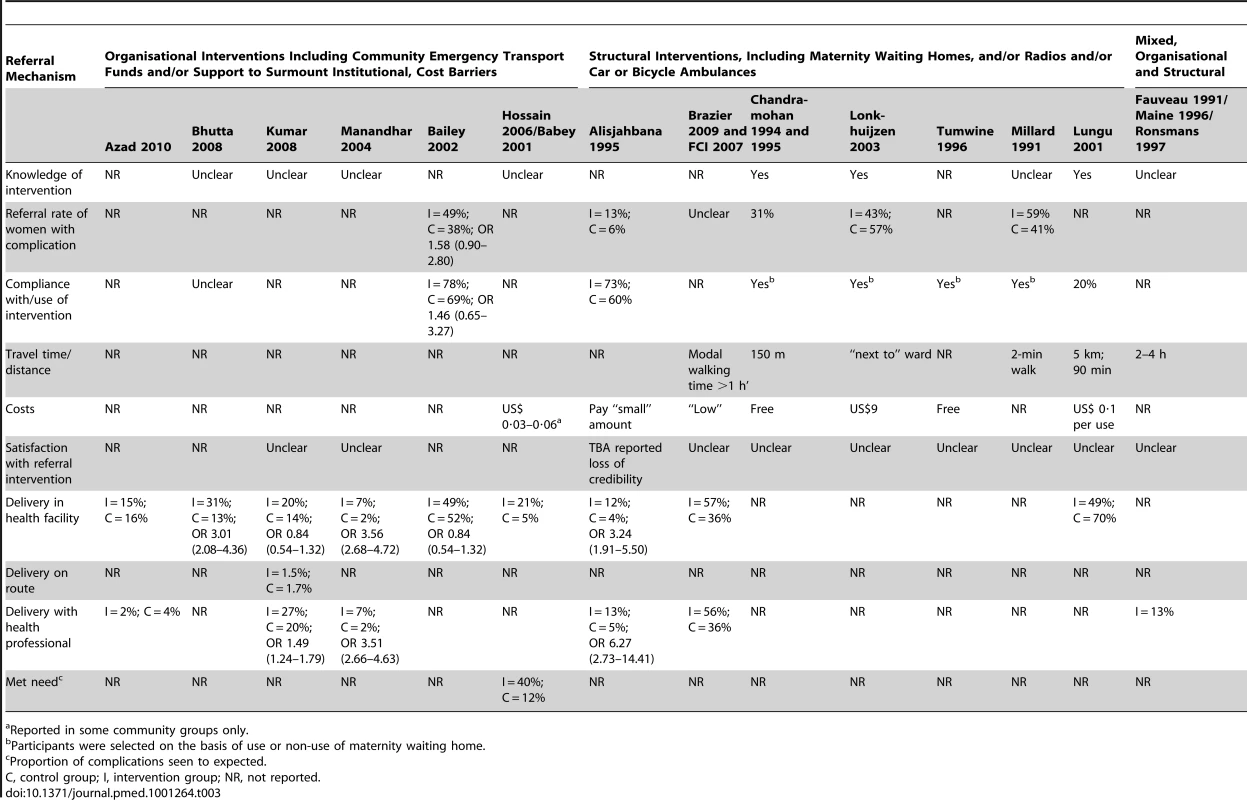
Reported in some community groups only. Data on health facility utilisation were available from nine studies. Six [12]–[18] showed increases in the proportion of deliveries in health facilities. The two RCTs that targeted the community reported improved health facility utilisation in intervention arms (OR 3.56 95% CI 2.68–4.72) [16] and (OR 3.01 95% CI 2.08–4.36) [12]. Of the remaining three studies that showed lower rates of delivery in health facilities in the intervention group, the reported effect of bicycle ambulances was most striking [23]. During the study, more women from villages without bicycle ambulances delivered in health facilities—70% in control villages compared to 49% of women in villages with bicycles. Furthermore, 22% of institutional deliveries during the study period came from villages provided with the bicycles and 42% from control villages (unpublished data). Of 20 instances where the bicycles were used, only four were for obstetric referrals, the rest for other medical conditions. The negative effect of the intervention on health facility utilisation was postulated to be due to a perception that bicycles brought unwanted attention to women during labour, so they preferred to walk to health facilities or deliver at home.
Discussion
We focused our review on interventions that aimed to overcome phase II delays. We were not able to establish the effectiveness of referral interventions on maternal mortality or other intermediate or process outcomes such as uptake of care. Although we found some reductions in neonatal mortality and in stillbirths, inference of effect due to interventions that specifically overcome phase II delays is not possible due to design limitations of the individual studies.
Reduction in neonatal deaths were found in four South Asian RCTs of community mobilisation interventions, which included the generation of funds for transport, to overcome phase II delays [10],[12],[15],[16]. It was not possible to disentangle the effects of the phase II intervention with other components that addressed other types of delays or that improved care. The changes observed may have been a result of the other components, or may have occurred only if the various elements are combined. This finding confirms other reviews demonstrating the success of complex, community-based interventions in reducing neonatal mortality [29]–[31] but the contribution of referral to such improvements cannot be surmised.
There is a possibility that maternity waiting homes in sub-Saharan Africa may reduce stillbirth rates. Unlike the RCTs on community mobilisation, this group of studies on maternity waiting homes [20]–[22],[24],[25] focused on use of this structure enabling pregnant women to live physically closer to a health facility, so the interpretation regarding effect of the intervention may be less problematic. Nevertheless, the evidence is weak. The number of events recorded in these studies was small, the way the maternity waiting homes were used varied across and within studies, and bias likely in the studies, both because of the way the participants were selected as well as the restriction of the studies to facility-based data. Another systematic review of maternity waiting facilities was conducted in 2009 [32], concluding that there was insufficient evidence of effectiveness on maternal and perinatal outcomes, but stillbirths were not investigated as a specific outcome. It is plausible that being in a maternity waiting home will allow women to be seen more rapidly in the case of any untoward event. Assuming that rapid and effective action (such as monitoring of fetal wellbeing and/or expediting delivery) is taken, an intrauterine death could be averted. Maternity waiting homes are extensively used in many countries [33] despite the lack of evidence surrounding its effectiveness, so our finding provides an added rationale to support the conduct of well designed, primary studies on waiting homes. The mechanisms through which this intervention might work and the factors important for success (e.g., availability of surgery, or regular assessment of women staying in the maternity waiting home), could not be elicited from the studies included. Alongside questions of effectiveness, future research in this area should specify the intervention rigorously and explore pathways of effect.
Transport and communication interventions were another group of studies investigated in this review [17],[18],[23],[26]. Most comprised only one part of a multifaceted intervention that addressed other health service improvements, so few conclusions can be drawn regarding their effect on phase II delays. Common sense tells us that interventions that reduce travel time and link up the referral system are likely to be important; however, this review shows that what are apparently “good ideas” do need to be carefully assessed. The use of bicycle ambulances is one example. Many studies describe their utility [33], but this should not be assumed for all situations, as demonstrated by the adverse effect documented from the study in Malawi [23]. The relatively recent introduction of new technologies such as mobile phones may well improve referral. Although we came across studies describing the use of mobile phones and related technologies in obstetric referral [33], none fulfilled our study criteria. None of the included studies mentioned the use of mobile phones.
The outputs and intermediate effects of the various referral interventions were arranged in Table 3 in order of a postulated sequence of effect. For the referral intervention to have an effect, women would have to know about an intervention and/or be referred in the first instance. They would then have to comply with, or use, the referral intervention and subsequently overcome barriers they encounter, in order to reach “appropriate” care, which can be measured using proxies such as delivery at health facility, delivery with a health professional, or receipt of care during an obstetric complication (met need). Data were inconclusive and we were unable to use these indicators to trace or explain mechanisms through which the referral intervention might have worked. Two studies, from Guatemala and Indonesia, provided data on referral rate, compliance and utilisation. We were unable to ascertain whether the proportions reported in the Guatemalan study [11] shared the same denominators. The Indonesian study [17] found that 13% of pregnant women in the intervention group were referred. Of these, 73% complied, resulting in a statistically significant increase in deliveries with health professionals and in health facilities (Table 3), although perinatal mortality was not improved (OR 1.19 95% CI 0.81–1.75) (unpublished data).
Other reviews on referral interventions are available [5],[6],[33]–[36]. The three delays model [5] provided what is now a well-established paradigm for barriers in accessing emergency obstetric care. Two papers offer insights on factors likely to improve the implementation of referral interventions [6],[34]. Various technologies, transport, and physical communication options have been summarised [35]. Some reviews have improved understanding of barriers, such as transport and cost, that affect referral [6],[33],[36]. Underfunding of health systems has also been implicated in leading to inefficient referral [4]. Modelling techniques have predicted that maternal mortality decline will reach a threshold of less than 35% decline if access to emergency obstetric care is not provided, and that referral and transport strategies, alongside other interventions, could contribute to as much as an 80% reduction in maternal mortality [37]. Our systematic review provides a contribution to knowledge in this field by focusing on the quality of evidence and summarising estimates of effects. We faced considerable constraints because of the design and multi-component nature of some of the interventions. The heterogeneity we encountered (in terms of differences in interventions, selection of participants, study design, and reported effects) implied that a meta-analysis would not have provided coherent data nor helped with the difficulties encountered in disentangling the effects of complex interventions. It is possible that our search may not have exhaustively covered literature from low - and middle-income countries, especially if not in English [38],[39]. We believe it is unlikely we have missed key studies as discussions with colleagues and other groups studying obstetric referral and extension of our search to databases like LILACs and the African Index Medicus provided no new eligible studies.
Much remains unknown. Does function of the health system, terrain, or whether the intervention targets antenatal, intrapartum, or post partum periods matter when selecting which interventions to implement? The studies that met our inclusion criteria were set in rural areas—we can make no conclusions on urban settings or any other contextual factors. Investigating phase II delays in isolation may be an oversimplification as phase I and III factors will have effects on phase II and referral interventions work through complex mechanisms. However, the literature base on referral interventions as a whole is very large and until efforts are made to break down the various components into manageable parts, progress in understanding referral interventions cannot be made. Despite the wealth of literature describing means to improve women's access to maternity care during emergencies, know-how for effective implementation remains limited. The 19 out of over 600 potentially relevant studies that met the criteria for inclusion in our study, and the findings of other recent reviews on referral linkages [31],[33] is testimony to the low priority given to careful design of studies and good practice in monitoring and evaluation. In addition, studies found were not explicitly designed to explain how the effects of the referral interventions were achieved. Ten years ago, the tracking of individuals who have been referred was recommended as a way to address this gap [34],[36], but little new knowledge has been generated in this area. Now that a start has been made in appraising the referral literature systematically, studies to investigate causal pathways and mechanisms of effect are necessary to understand how the interventions work as one part of a chain reliant on other components of the health system, rather than in isolation.
Conclusion
The limitations inherent in the studies included in this review mean that findings should be interpreted with caution. We found that complex, community-targeted interventions reduce neonatal mortality but not how the referral components contributed. The reduction in stillbirths observed in studies of maternity waiting homes makes this a potentially promising intervention that needs further investigation. While continuing to invest in implementing referral interventions within maternal and newborn health programmes, we urge health planners to ensure that the interventions are rigorously monitored and evaluated, and operations research studies designed with controls and comparisons. There should be awareness that referral interventions may have adverse effects. Future research should aim to understand how the interventions work and why, by using methods that provide understanding of causal pathways and mechanisms of action.
Supporting Information
Zdroje
1. AbouZahrC 1998 Antepartum and postpartum hemorrhage. Chapter 4. Murray C, Lopez A, editors. Health dimensions of sex and reproduction Boston Harvard School of Public Health
2. KhanRUEl-RafaeyH 2006 Pathophysiology of post partum haemorrhage and third stage of labour Chapter 8. B-LynchCKeithLGLalondeABKaroshiM A textbook of post partum haemorrhage London Sapiens publishing 62 69
3. UNICEF 2009 State of the world's children New York UNICEF
4. NyamtemaASUrassaDPvan RoosmalenJ 2011 Maternal health interventions in resource limited countries: a systematic review of packages, impacts and factors for change. BMC Pregnancy Childbirth 11 30
5. ThaddeusSMaineD 1994 Too far to walk: maternal mortality in context. Soc Sc Med 38(8) 1091 1110
6. JahnAde BrouwereV 2001 Referral in pregnancy and childbirth: concepts and strategies. Available: http://www.jsieurope.org/safem/collect/safem/pdf/s2940e/s2940e.pdf Accessed 29 December 2011
7. World Bank 2011 Country and lending groups. Available: http://data.worldbank.org/about/country-classifications/country-and-lending-groups Accessed 29 December 2011
8. Effective Public Health Practice Project 2009 Quality assessment tool. Available: http://www.ephpp.ca/Tools.html Accessed 29 December 2011
9. WalterINutleySDaviesH 2003 Developing a taxonomy of interventions used to increase the impact of research: Appendix I. Available: http://www.ruru.ac.uk/PDFs/Taxonomy%20development%20paper%20070103.pdf Accessed 29 December 2011
10. AzadKBarnettSBanerjeeBShahaSKhanK 2010 Effects of scaling up women's groups on birth outcomes in three rural districts in Bangladesh: a cluster randomised trial. Lancet 375 1193 1202
11. BaileyPSzaszdiJGloverL 2002 Obstetric complications: does training traditional birth attendants make a difference? Pan Am J Public Health 11 15 23
12. BhuttaZMemonZSoofiSSalatMCousensS 2008 Implementing community-based perinatal care: results from pilot study in rural Pakistan. Bull World Health Organ 86 452 459
13. HossainJRossS 2006 The effect of addressing demand for as well as supply of emergency obstetric care in Dinajpur, Bangladesh. Int J Gynecol Obstet 92 320 328
14. BarbeyAFaiselAMyeyaJStavrouVStewartJ 2001 Dinajpur SafeMother Initiative: final evaluation report. Available: http://webtest.dhaka.net/care/publication/Publication_6871971.pdf. Accessed 29 December 2011
15. KumarVMohantySKumarAMisraRPSantoshamM 2008 Effect of community-based behaviour change management on neonatal mortality in Shivgarh, Uttar Pradesh, India: a cluster-randomised controlled trial. Lancet 372 1151 1162
16. ManandharDSOsrinDShresthaBPMeskoNMorrisonJ 2004 Effect of a participatory intervention with women's groups on birth outcomes in Nepal: cluster-randomised controlled trial. Lancet 364 970 979
17. AlisjahbanaAWilliamsCDharmayantiRHermawanDKwastB 1995 An integrated village maternity service to improve referral patterns in a rural area in West Java. Int J Gynecol Obstet 48 Suppl. S83 S94
18. BrazierEAndrzejewskiCPerkinsMThemmenEKnightR 2009 Improving poor women's access to maternity care: findings from a primary care intervention in Burkina Faso. Soc Sc Med 69 682 690
19. FCI Family Care International Burkina Faso 2007 Testing approaches for increasing skilled care during childbirth: key findings from Ouargaye, Burkina Faso. Available: http://www.familycareintl.org/UserFiles/File/SCI%20Burkina%20Faso%20Summary.pdf. Accessed 29 December 2011
20. ChandramohanDCuttsFChandraR 1994 Effects of a maternity waiting home on adverse maternal outcomes and the validity of antenatal risk screening. Int J Gynecol Obstet 46 279 284
21. ChandramohanDCuttsFMillardP 1995 The effect of stay in a maternity waiting home on perinatal mortality in rural Zimbabwe. J Trop Med Hyg 98 261 267
22. LonkhuijzenLStegemanMNyirongoRvan RoosmalenJ 2003 Use of maternity waiting home in rural Zambia. Afr J Reprod Health 7 32 36
23. LunguKKamfoseVHusseinJAshwood-SmithH 2001 Are bicycle ambulances and community transport plans effective in strengthening obstetric referral systems in Southern Malawi. Malawi Med J 13 16 18
24. MillardPBaileyJHansonJ 1991 Antenatal village stay and pregnancy outcome in rural Zimbabwe. Cent Afr J Med 37 1 4
25. TumwineJDungareP 1996 Maternity waiting shelters and pregnancy outcome: experience from a rural area in Zimbabwe. Ann Trop Paediatr 16 55 59
26. FauveauVStewartKKhanSChakrabortyJ 1991 Effect on mortality of community based maternity care programme in rural Bangladesh. Lancet 338 1183 1186
27. RonsmansCVannesteAChakrabortyJGinnekenJ 1997 Decline in maternal mortality in Matlab, Bangladesh: a cautionary tale. Lancet 350 1810 1814
28. MaineDAklinMChakrabortyJFranciscoAStrongM 1996 Why did maternal mortality decline in Matlab? Stud Fam Plann 27 179 187
29. KidneyEWinterHKhanKSGülmezogluAMMeadsCA 2009 Systematic review of effect of community level interventions to reduce maternal mortality. BMC Pregnancy Childbirth 9 2
30. LassiZSHaiderBABhuttaZA 2010 Community-based intervention packages for reducing maternal and neonatal morbidity and mortality and improving neonatal outcomes. Cochrane Database Syst Rev 11 CD007754
31. LeeACCLawnJCousensSKumarVOsrinD 2009 Linking families and facilities for care at birth: what works to avert intrapartum-related deaths? Int J Gynecol Obstet 107 Suppl. S65 S88
32. LonkhuijzenLStekelenburgJvan RoosmalenJ 2009 Maternity waiting facilities for improving maternal and neonatal outcome in low-resource countries. Cochrane Database Syst Rev 3 CD006759
33. HolmesWKennedyE 2010 Reaching emergency obstetric care: overcoming the second delay. Melbourne: Burnet Institute Available: http://www.wchknowledgehub.com.au/our-resources Accessed 29 December 2011
34. MurraySFPearsonSC 2006 Maternity referral systems in developing countries: current knowledge and future research needs. Soc Sc Med 62 2205 2215
35. KrasovecK 2004 Auxiliary technologies related to transport and communication for obstetric emergencies. Int J Gynecol Obstet 85 S14 S23
36. MacintyreKHotchkissD 1999 Referral revisited: community financing schemes and emergency transport in rural Africa. Soc Sc Med 49 1473 1487
37. GoldieSSweetSCarvalhoNNatchuUHuD 2010 Alternative strategies to reduce maternal mortality in India: a cost-effectiveness analysis. PLoS Med 7 e1000264 doi:10.1371.journal.pmed.1000264
38. PilkingtonKBoshnakovaAClarkeMRichardsonJ 2005 No language restrictions in database searches: what does this really mean? J Altern Complement Med 11 205 207
39. WhitingPWestwoodMBurkeMSterneJGlanvilleJ 2008 Systematic reviews of test accuracy should search a range of databases to identify primary studies. J Clin Epid 61 357 364
Štítky
Interní lékařství
Článek Risk of Venous Thromboembolism in Patients with Cancer: A Systematic Review and Meta-AnalysisČlánek The Co-Management of Tuberculosis and Diabetes: Challenges and Opportunities in the Developing WorldČlánek Researching New Methods of Screening for Adverse Pregnancy Outcome: Lessons from Pre-eclampsiaČlánek HIV Treatment as Prevention: Models, Data, and Questions—Towards Evidence-Based Decision-MakingČlánek United States Private-Sector Physicians and Pharmaceutical Contract Research: A Qualitative Study
Článek vyšel v časopisePLOS Medicine
Nejčtenější tento týden
2012 Číslo 7- Berberin: přírodní hypolipidemikum se slibnými výsledky
- Léčba bolesti u seniorů
- Příznivý vliv Armolipidu Plus na hladinu cholesterolu a zánětlivé parametry u pacientů s chronickým subklinickým zánětem
- Červená fermentovaná rýže účinně snižuje hladinu LDL cholesterolu jako vhodná alternativa ke statinové terapii
- Jak postupovat při výběru betablokátoru − doporučení z kardiologické praxe
-
Všechny články tohoto čísla
- HIV Treatment as Prevention: Issues in Economic Evaluation
- Risk of Venous Thromboembolism in Patients with Cancer: A Systematic Review and Meta-Analysis
- HIV Treatment as Prevention: Natural Experiments Highlight Limits of Antiretroviral Treatment as HIV Prevention
- HIV Treatment as Prevention: Optimising the Impact of Expanded HIV Treatment Programmes
- Reduction in Infection Rates after Mandatory Hospital Public Reporting: Findings from a Longitudinal Cohort Study in Canada
- Medical Device Regulation: Time to Improve Performance
- Averting an Impending Storm: Can We Reengineer Health Systems to Meet the Needs of Aging Populations?
- Thinking Forward: The Quicksand of Appeasing the Food Industry
- The Co-Management of Tuberculosis and Diabetes: Challenges and Opportunities in the Developing World
- Community Mobilization in Mumbai Slums to Improve Perinatal Care and Outcomes: A Cluster Randomized Controlled Trial
- Researching New Methods of Screening for Adverse Pregnancy Outcome: Lessons from Pre-eclampsia
- Social Entrepreneurship for Sexual Health (SESH): A New Approach for Enabling Delivery of Sexual Health Services among Most-at-Risk Populations
- Lessons from Agriculture for the Sustainable Management of Malaria Vectors
- HIV Treatment as Prevention: Modelling the Cost of Antiretroviral Treatment—State of the Art and Future Directions
- HIV Treatment as Prevention: Considerations in the Design, Conduct, and Analysis of Cluster Randomized Controlled Trials of Combination HIV Prevention
- Antiretroviral Therapy for Prevention of Tuberculosis in Adults with HIV: A Systematic Review and Meta-Analysis
- The Effectiveness of Emergency Obstetric Referral Interventions in Developing Country Settings: A Systematic Review
- Digital Humanitarianism: Collective Intelligence Emerging
- The Ethics of Switch/Simplify in Antiretroviral Trials: Non-Inferior or Just Inferior?
- “Big Food,” the Consumer Food Environment, Health, and the Policy Response in South Africa
- Plasma Phospholipid Fatty Acid Concentration and Incident Coronary Heart Disease in Men and Women: The EPIC-Norfolk Prospective Study
- HIV Treatment as Prevention: The Utility and Limitations of Ecological Observation
- How Does Medical Device Regulation Perform in the United States and the European Union? A Systematic Review
- HIV Treatment as Prevention: Models, Data, and Questions—Towards Evidence-Based Decision-Making
- Risk Factors for Death among Children Less than 5 Years Old Hospitalized with Diarrhea in Rural Western Kenya, 2005–2007: A Cohort Study
- United States Private-Sector Physicians and Pharmaceutical Contract Research: A Qualitative Study
- HIV Treatment as Prevention: Debate and Commentary—Will Early Infection Compromise Treatment-as-Prevention Strategies?
- HIV Treatment as Prevention: Principles of Good HIV Epidemiology Modelling for Public Health Decision-Making in All Modes of Prevention and Evaluation
- Effect of a Community-Based Nursing Intervention on Mortality in Chronically Ill Older Adults: A Randomized Controlled Trial
- Surveillance of Infection Severity: A Registry Study of Laboratory Diagnosed
- Consequences of Gestational Diabetes in an Urban Hospital in Viet Nam: A Prospective Cohort Study
- Integrating Mental Health and Development: A Case Study of the BasicNeeds Model in Nepal
- Treatment of Young Children with HIV Infection: Using Evidence to Inform Policymakers
- The Impact of Transnational “Big Food” Companies on the South: A View from Brazil
- HIV Treatment as Prevention: Systematic Comparison of Mathematical Models of the Potential Impact of Antiretroviral Therapy on HIV Incidence in South Africa
- PLOS Medicine
- Archiv čísel
- Aktuální číslo
- Informace o časopisu
Nejčtenější v tomto čísle- HIV Treatment as Prevention: Issues in Economic Evaluation
- HIV Treatment as Prevention: Modelling the Cost of Antiretroviral Treatment—State of the Art and Future Directions
- HIV Treatment as Prevention: The Utility and Limitations of Ecological Observation
- Consequences of Gestational Diabetes in an Urban Hospital in Viet Nam: A Prospective Cohort Study
Kurzy
Zvyšte si kvalifikaci online z pohodlí domova
Současné možnosti léčby obezity
nový kurzAutoři: MUDr. Martin Hrubý
Všechny kurzyPřihlášení#ADS_BOTTOM_SCRIPTS#Zapomenuté hesloZadejte e-mailovou adresu, se kterou jste vytvářel(a) účet, budou Vám na ni zaslány informace k nastavení nového hesla.
- Vzdělávání



