-
Články
Top novinky
Reklama- Vzdělávání
- Časopisy
Top články
Nové číslo
- Témata
Top novinky
Reklama- Videa
- Podcasty
Nové podcasty
Reklama- Kariéra
Doporučené pozice
Reklama- Praxe
Top novinky
ReklamaThe Role of Health Systems Factors in Facilitating Access to Psychotropic Medicines: A Cross-Sectional Analysis of the WHO-AIMS in 63 Low- and Middle-Income Countries
Background:
Neuropsychiatric conditions comprise 14% of the global burden of disease and 30% of all noncommunicable disease. Despite the existence of cost-effective interventions, including administration of psychotropic medicines, the number of persons who remain untreated is as high as 85% in low - and middle-income countries (LAMICs). While access to psychotropic medicines varies substantially across countries, no studies to date have empirically investigated potential health systems factors underlying this issue.Methods and Findings:
This study uses a cross-sectional sample of 63 LAMICs and country regions to identify key health systems components associated with access to psychotropic medicines. Data from countries that completed the World Health Organization Assessment Instrument for Mental Health Systems (WHO-AIMS) were included in multiple regression analyses to investigate the role of five major mental health systems domains in shaping medicine availability and affordability. These domains are: mental health legislation, human rights implementations, mental health care financing, human resources, and the role of advocacy groups. Availability of psychotropic medicines was associated with features of all five mental health systems domains. Most notably, within the domain of mental health legislation, a comprehensive national mental health plan was associated with 15% greater availability; and in terms of advocacy groups, the participation of family-based organizations in the development of mental health legislation was associated with 17% greater availability. Only three measures were related with affordability of medicines to consumers: level of human resources, percentage of countries' health budget dedicated to mental health, and availability of mental health care in prisons. Controlling for country development, as measured by the Human Development Index, health systems features were associated with medicine availability but not affordability.Conclusions:
Results suggest that strengthening particular facets of mental health systems might improve availability of psychotropic medicines and that overall country development is associated with affordability.
: Please see later in the article for the Editors' Summary
Published in the journal: . PLoS Med 9(1): e32767. doi:10.1371/journal.pmed.1001166
Category: Research Article
doi: https://doi.org/10.1371/journal.pmed.1001166Summary
Background:
Neuropsychiatric conditions comprise 14% of the global burden of disease and 30% of all noncommunicable disease. Despite the existence of cost-effective interventions, including administration of psychotropic medicines, the number of persons who remain untreated is as high as 85% in low - and middle-income countries (LAMICs). While access to psychotropic medicines varies substantially across countries, no studies to date have empirically investigated potential health systems factors underlying this issue.Methods and Findings:
This study uses a cross-sectional sample of 63 LAMICs and country regions to identify key health systems components associated with access to psychotropic medicines. Data from countries that completed the World Health Organization Assessment Instrument for Mental Health Systems (WHO-AIMS) were included in multiple regression analyses to investigate the role of five major mental health systems domains in shaping medicine availability and affordability. These domains are: mental health legislation, human rights implementations, mental health care financing, human resources, and the role of advocacy groups. Availability of psychotropic medicines was associated with features of all five mental health systems domains. Most notably, within the domain of mental health legislation, a comprehensive national mental health plan was associated with 15% greater availability; and in terms of advocacy groups, the participation of family-based organizations in the development of mental health legislation was associated with 17% greater availability. Only three measures were related with affordability of medicines to consumers: level of human resources, percentage of countries' health budget dedicated to mental health, and availability of mental health care in prisons. Controlling for country development, as measured by the Human Development Index, health systems features were associated with medicine availability but not affordability.Conclusions:
Results suggest that strengthening particular facets of mental health systems might improve availability of psychotropic medicines and that overall country development is associated with affordability.
: Please see later in the article for the Editors' SummaryIntroduction
Access to treatments for mental disorders is inadequate in a large majority of low - and middle-income countries (LAMICs). The percentage of individuals who have severe disorders such as schizophrenia, bipolar disorder, and major depressive disorder, but who remain untreated, is estimated to be as high as 85% in these settings [1]. This so-called “treatment gap” is particularly disconcerting when the prevalence and debilitating impacts of these illnesses are taken into account. Approximately 450 million people worldwide have a mental illness, as such accounting for an estimated one-third of all years lived with disability [2],[3]. Coupled with severity of associated symptoms, mental disorders comprise approximately 13.5% of the global burden of disease (GBD) [4] and 30% of the noncommunicable disease burden worldwide [5].
Roughly 80% of persons with mental illnesses live in LAMICs [4]. However, in part because of high rates of infectious diseases, those countries that are the poorest typically spend the least on mental health and rely upon a framework of institutionalized care [6],[7]. For example, only 52% of low-income countries, as compared to 97% of high-income countries, provide community-based care for patients [8]. This dearth of financial resources directed towards mental health is also associated with a shortage of human resources trained in mental health care, ranging from levels of primary to tertiary care [9]–[11].
A burgeoning literature is developing on the efficacy and cost-effectiveness of specific treatment interventions [12],[13]. In terms of efficacy, studies have shown that both psychosocial and pharmacological interventions are effective in treating major depressive disorder [14]–[21], schizophrenia [22]–[25], alcohol dependence [26]–[29], and developmental disabilities [30]–[35]. In terms of the cost-effectiveness of interventions in LAMIC settings, one recent systematic review found over 450 trials on the utility of first generation antipsychotic drugs for the treatment of schizophrenia, in addition to more than 200 trials on tricyclic antidepressants for major depressive disorder, both of which are stated as cost-effective by the Disease Control Priorities Project [36]. Nevertheless, access to medicines—both in terms of availability and affordability—is exceedingly limited in LAMIC settings, and only a small number of studies have critically analyzed access to psychotropic medicines in LAMICs. At the conceptual level, inadequate and poorly distributed financial resources [37], a shortage of human resources [38],[39], and overregulation due to the potential for abuse of certain drugs [40] have been highlighted as significant impediments to access. In addition, country-specific analyses have identified contextual shortcomings such as inadequate human resources training [41],[42] and cultural norms and perceptions of mental illness [43]–[46].
A foremost challenge in improving access to psychotropic medicines is bringing a conceptual perspective of what should, in theory, work to bear on the context-specific situations of individual countries. Cross-national analyses that take into account empirical data relating aspects of mental health care systems—for example, number of health workers, government mental health policies, and involvement of different stakeholders—may serve to shed light on target areas that should be prioritized for improvement. One method for achieving this improvement would be to approach the issue of access to psychotropic drugs from a health systems perspective.
Assuming a health systems approach to understanding and addressing mental health care entails an evaluation of the country-level framework and the major building blocks liable to affect treatment coverage [47]. According to the World Health Organization Assessment Instrument for Mental Health Systems (WHO-AIMS), these building blocks include leadership and governance, the distribution of human resources for mental health, a system of health services delivery, a scheme for financing and appropriating resources, access to treatments including a human rights framework to protect patients, and an information systems to collect data and monitor performance over time [48]. While each health system is context-specific, health systems that function well tend to share certain basic characteristics [49]. For example, while the content of a national mental health plan should be expected to vary according to unique needs within a country, it is fundamental that all countries have a plan that contains actionable items monitored and evaluated over time [47],[50],[51].
This study utilizes data from 63 developing countries or country regions—representing approximately 1.9 billion people worldwide—to identify associations with access to and affordability of psychotropic medicines across five health systems domains. For the purposes of these analyses, domains are defined in terms of: mental health legislation, human rights training and inspection, financing, level of human resources working within mental health facilities, and mental health advocacy and promotion by a variety of stakeholders. To date, a cross-national cross-sectional analysis of this kind has not been conducted.
Methods
Respondent Sample
Sixty-three countries or country regions that completed the WHO-AIMS before June 2010 were included in the study. Of the 63 LAMICs, 58 provided sufficient information on availability of psychotropic medicines and 54 on affordability. Comparing countries with and without sufficient information, there were no significant differences in terms of gross national income (GNI) per capita, level of specificity in mental health legislation or overall rates of human resources (p>0.05 in each instance), indicating that these subsamples were not characteristically biased.
WHO-AIMS was created in 2004 as a tool for enabling LAMICs to evaluate core components of their mental health systems, with the ultimate goal of providing critical information for the strengthening of mental health policies and service delivery [48]. The instrument comprises 155 items across six health systems domains (outlined above). Items are quantitative, defined as numbers, rates, proportions, and ordinal scales, and predominately represent process rather than outcome measures. Data are collected by country-based focal points, often within countries' Ministries of Health, and are evaluated and revised through an iterative process in conjunction with WHO headquarters in Geneva, Switzerland. A set of instructions and operational definitions are also provided by WHO headquarters. A full overview of the data collection process and instrument content is available at the WHO's WHO-AIMS web page [52].
In eight datasets—Hunan Province, China; Uttarakhand State, India; Gujarat State, India; South Central Somalia; Somaliland Somalia; Anguilla; Kosovo; and West Bank and Gaza—the data are representative of specific country regions or territories. Thus, in two countries, India and Somalia, two datasets were included for a single country. In the case of India—a country comprising approximately 1.2 billion citizens—a single measure cannot characterize the level of heterogeneity observed across relatively decentralized states. In the case of Somalia, ongoing civil war has left the nation largely divided, with Somaliland considered a separatist region that maintains its own governing body. For the sake of simplicity, observations in this study will be referred to as countries, while acknowledging that the reality is more subtle [53]. This study includes 15 low-income, 36 lower-middle income, and 13 upper-middle income countries according to current World Bank classifications [54]. Additional descriptive characteristics of the sample, including summary measures of availability and affordability of psychotropic medicines, are provided in Table 1.
Tab. 1. Descriptive statistics of the sample. 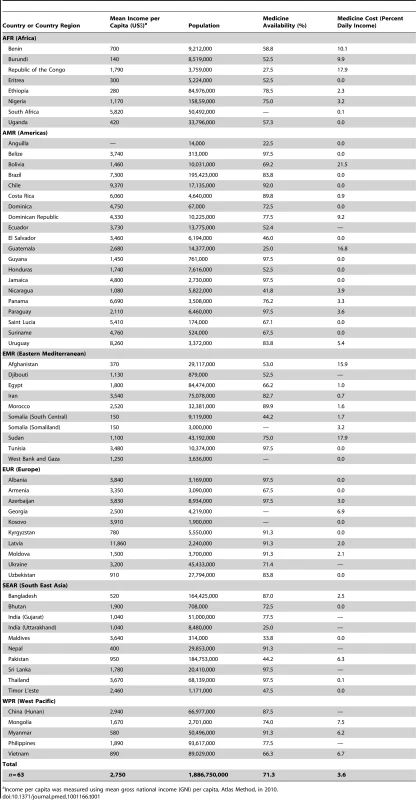
Income per capita was measured using mean gross national income (GNI) per capita, Atlas Method, in 2010. Health System Domain Measures
The five health system domains assessed in this study map closely to the conceptual framework outlined in WHO-AIMS and WHO Mental Health Atlas instruments and represent core content areas of most well-functioning systems. Within each of the five mental health systems domains, indicators that were thought to be theoretically related to medicine access on the basis of the existing literature, that were representative of overarching constructs, and that did not contain significant missingness (i.e., roughly 90% or more of participating countries provided data) were identified for investigation. Owing to limited sample size, only one to three summary measurements per health systems domain were included in order to prevent overspecificity in model fitting.
Domain 1: Legislation
The WHO-AIMS instrument contains information on both the existence and contents of national mental health policies, plans, and laws. Preliminary analyses using bivariate associations revealed that the specificity of content within mental health policies and plans were closely related. On the basis of the stronger implementation focus of plans as compared to policies, specificity of national plans was selected as the more relevant measure. As there were 12 content areas identified for national mental health plans, a summary score was created such that countries' scores could range from 0 (no mental health plan) to 12 (all content areas addressed). The associated Cronbach's alpha of this scale—a measure of internal consistency—was α = 0.96, connoting strong consistency of responses across items. In a similar vein, content of mental health laws comprised eight content items and were integrated into a scale of 0 to 8 (α = 0.95).
Domain 2: Human rights
Respondents to the WHO-AIMS are asked to identify whether the country inspects human rights violations at mental hospitals and at community-based inpatient psychiatric units, as well as whether staff at both types of facilities are trained on the human rights protections of patients. Human rights inspection and training were strongly interrelated; as such, a composite measure for human rights implementations was created, whereby countries could score from 0% (no human rights inspection or training at either type of facilities) to 100% (all facilities have training and inspection). The associated Cronbach's alpha of this scale was α = 0.74. A secondary measure of human rights monitoring was also included in analyses and reflects the level of mental health care provided to incarcerated citizens. The ordinal scale for this ranged from 0 (no prisons provide mental health care) to 4 (all or most prisons—80–100%—provide mental health care).
Domain 3: Financing
Financing for mental health care was measured as the percentage of government health expenditures directed towards mental health. This figure pertains to expenditures allocated by governments' health departments and therefore does not include the private sector; however, in most LAMICs, public provisions are the primary source of mental health care.
Domain 4: Human resources
Mental health infrastructure can be thought of both in terms of physical facilities and the level of human resources existing within facilities to care for and monitor patients. As these measures are often highly correlated with one another, including in the present sample, level of human resources was utilized. The number of psychiatrists, nurses, psychologists, social workers, and occupational therapists working within mental health facilities (per 100,000 population) were summed to represent the total number of specialized human resources currently working within the field of mental health. A secondary measure relating to human resources was also documented—namely, the availability of treatment protocols for mental illness in physician-based primary care settings. This comprised a 5-point ordinal scale ranging from no availability in primary care facilities (0%) to available in all or almost all primary care facilities (81%–100%).
Domain 5: Advocacy
A variety of stakeholders in mental health treatment and delivery exist outside of the formal government. Separate measurements were created for the three most prominent of these groups: user associations, associations comprised of those affected by mental illness; family member associations, associations formed by family members of those affected by mental illness; and additional nongovernmental organizations (NGOs). For the first two, a yes/no question identifying whether these associations are involved in formulation of mental health legislation was utilized. For NGOs, the overall rate of membership per 100,000 population was used.
Outcome Measures
The term access encapsulates two interrelated concepts: availability, which refers to the supply dimension of access, and affordability, which refers to consumers' financial means to purchase the product. Separate scales, based on WHO-AIMS responses, were created for each of these constructs.
Availability of psychotropic medicines
Availability of psychotropic medicines is operationally defined within the WHO-AIMS instrument as “the percentage of mental health facilities in which there is at least one psychotropic medication of each therapeutic category (antipsychotic, antidepressant, mood stabilizer, anxiolytic medicines, and antiepileptic medicines) available all year long.” These percentages were averaged across the four types of mental health facilities within countries—mental hospitals, outpatient facilities, community-based inpatient facilities, and primary care facilities—in order that the final measure of availability reflect all potential points of patient access [5].
Affordability of psychotropic medicines to consumers
The affordability of psychotropic medications comprises two components that must be integrated: first, the cost of psychotropic medicines relative to a measurement of consumer income, and second, an estimate of the level of government subsidies to reduce consumer costs [55]. Regarding the former, WHO-AIMS provides a figure for the price of the lowest-cost generic antidepressant available within the country relative to minimum wage. For two reasons, this value was utilized as a proxy for medication costs. First, in part because of the higher prevalence of major depressive disorder relative to other mental illnesses, data on antidepressant prices are more widely documented across countries than data on other psychotropic medicines [56]. Second, a denominator value such as daily minimum wage or lowest-paid government worker allows one to observe the effect of prices on an average consumer and is a metric available across countries [57]. In terms of government subsidization, the percentage of the population with free access to essential psychotropic medicines was utilized to determine how much of the cost is carried by consumers as opposed to the government. Final consumer costs must reflect cost to consumers once subsidization levels are taken into account [55]. As such, cost to consumers was multiplied by the percentage within the country not covered by subsidies. This value represents the percentage of daily minimum wage needed to purchase medicine by an average consumer.
The Human Development Index
Availability and affordability of psychotropic medicines are related to more general measurements of a country's development status. For example, income per capita, life expectancy, and average years of education are all strongly associated with one another and negatively associated with medicine availability and affordability. On the one hand, including a composite measure of these, best embodied by the Human Development Index (HDI) [58], allows for inspection of the role of different mental health system domains while controlling for the effects of these more general factors. This would, in turn, benefit external validity and permit greater generalizability of results across LAMICs. On the other hand, given that the functional integrity of health systems is itself intrinsically related to measures like income per capita and life expectancy, controlling for HDI may risk diminishing ecological validity insofar as doing so creates an artificial scenario in which HDI is exogenous to health systems measurements. To accommodate both perspectives, regression analyses were performed first without and then with HDI as a covariate.
Data Analysis
Data analysis was conducted in two phases. In the initial phase, pairwise correlations were used to inform decisions about selection of independent variables within each health systems' domain. Associations greater than 0.4 were flagged as a potential indication of collinearity, and the variable was either removed from analyses or integrated with its associated counterpart to represent a more general measurement construct. For instance, the number of psychiatrists, nurses, psychologists, social workers, and occupational therapists within a country (per 100,000 population) were strongly associated and were therefore totaled in order to represent the broader construct of overall human resources for mental health. Alongside this approach, the potential for collinearity within regression models was assessed by analyzing the variance inflation factor (VIF) associated with individual independent variables, for which a VIF greater than 10 is often considered an indication of collinearity [59]. In all instances, independent variables had VIFs less than 2.
In the second phase of data analysis, ordinary least squares (OLS) multiple linear regression analyses were conducted using independent variables within each mental health systems' domain of interest. In total, five regressions—one for each health systems' domain—were conducted. Regressions were first run without the HDI measurement as a covariate and then with this measurement included. All betas reported in the results section are unstandardized. For individual regression analyses, missing data were addressed with multiple imputation analysis using STATA 11.0's MI command (multiple imputation suite package). This approach considers the relationship of missing data to other observed characteristics in the data set, thereby reducing bias, in addition to accounting for sampling variability across imputations by introducing an error term for each imputed value [60]. Overall, the level of missingness ranged from 2% (for legislation content and protocols for treatment) to 11% (total level of human resources). All analyses were conducted in STATA/SE 11.0 at the 0.05 alpha level. Given that multiple analyses were conducted, it should be noted that the possible occurrence of a type 1 error was greater than 0.05, although this was considered a necessary limitation granted the sample size (for further discussion, see [61]).
As the response values for the availability outcome ranged from 0% to 100%, residual analysis was conducted to assess OLS assumptions. This was done in two steps: first, studentized residuals were inspected with quantile normal plots. At this step, no obvious departures from normality were observed. Second, Shapiro-Wilk W tests for normal data were used to formally evaluate the normality of the distribution of studentized residuals. On this measure, there was only one instance in which this test was marginally significant (p = 0.05): namely, when availability was regressed on measures of governance (i.e., specificity of national mental health plans and legislation), without the inclusion of HDI as a covariate. In order to observe the impact of this effect, a square transformation was performed on the availability outcome, after which the Shapiro-Wilk test was no longer significant (p>0.10). Given that regression results did not differ considerably between the original model and this model, the original (nontransformed) result was retained in order to facilitate interpretability and consistency.
Results
Availability of Medicines across Facilities
Of the 63 countries in the sample, 58 provided data on availability of medicines at all four types of mental health facilities. On average, 71% (standard deviation [SD] = 22%) of facilities had at least one psychotropic medicine of each therapeutic category—antipsychotic, antidepressant, mood stabilizer, anxiolytic, and antiepileptic medicines—available. Mean availability was 70% in low (SD = 17%, n = 15) and lower-middle income countries (SD = 25%, n = 31), as compared to 82% (SD = 10%, n = 11) in upper-middle income countries. Ten countries, all of which were low or lower-middle income, reported that psychotropic medicines were available in fewer than half of facilities.
Multiple regression analyses identified significant associations with medicine availability in each of the five health systems domains. In terms of legislation, both the specificity of national mental health plans (β = 1.27, p<0.05) and mental health laws (β = 1.65, p<0.05) were positively associated with availability. Similarly, human rights training and inspection was related to availability (β = 0.27, p<0.01), as was the percentage of the health budget directed towards mental health (β = 3.57, p<0.05), with a 1% increase in health expenditures associated with a 3.57% increase in availability across facilities.
In terms of human resources and infrastructure, the availability of assessment and treatment protocols at the primary health care level was related to availability (β = 4.30, p<0.05); a 1-unit increase on the ordinal scale (e.g., from 21%–50% to 51%–80% availability of protocols) was associated with a 4.3% increase in medicine availability. Lastly, with respect to advocacy organizations, the participation of family associations in the formation and implementation of mental health policies was associated with a 16.7% increase in availability of psychotropic medicines (β = 16.73, p = 0.01). In contrast, participation of user associations (β = 5.55, p>0.05) and other NGOs (β = −1.09, p>0.05) was not significantly related with availability. Table 2 presents an overview of these results.
Tab. 2. Domain-specific associations with medicine availability. 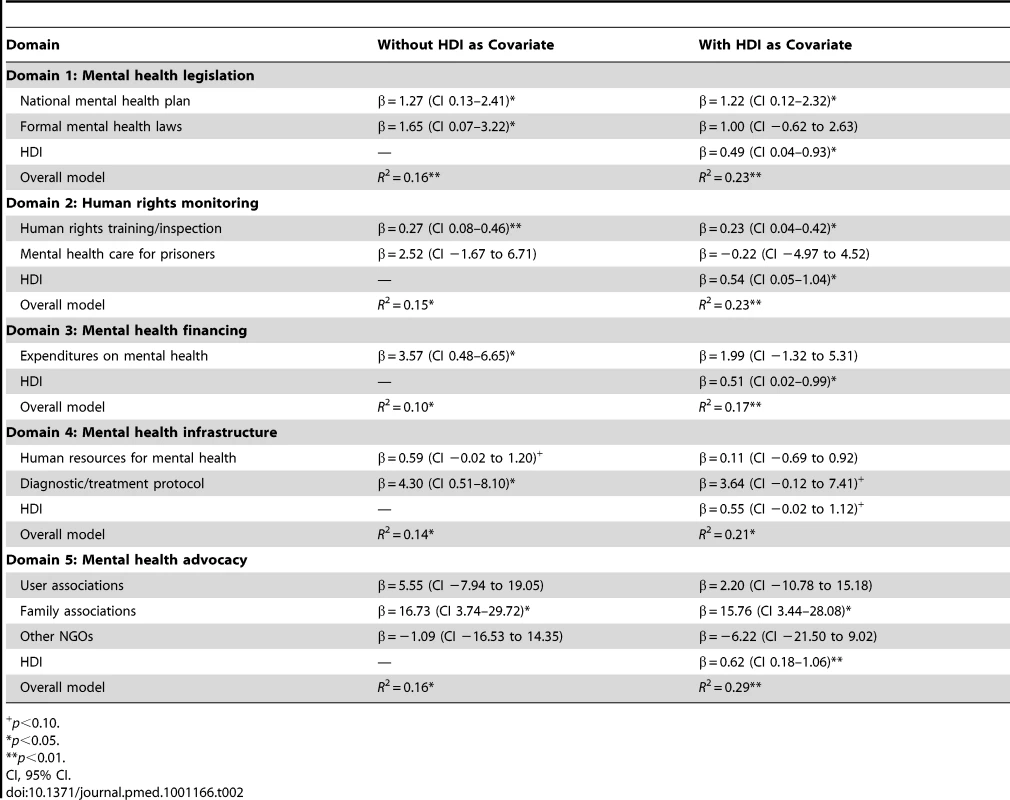
+p<0.10. When the HDI was taken into account as a covariate, the percent of health expenditures on mental health (β = 1.99, p>0.05) became nonsignificant as an independent variable, a finding to be expected given that income per capita, one aspect of HDI, is strongly associated with allocation of financing and medicine availability. Additionally, the effect of mental health laws (β = 1.00, p>0.05) and treatment protocols (β = 3.64, p>0.05) became nonsignificant with the inclusion of HDI, although there was a trend towards significance (p<0.10) in the latter.
Figure 1 illustrates the relationship between medicine availability and two of the independent variables: involvement of family associations in the formation of mental health legislation, and access to treatment protocols for diagnosis and treatment of mental illness at the level of primary care.
Fig. 1. Medicine availability in relation to involvement of family associations and existence of treatment protocols. 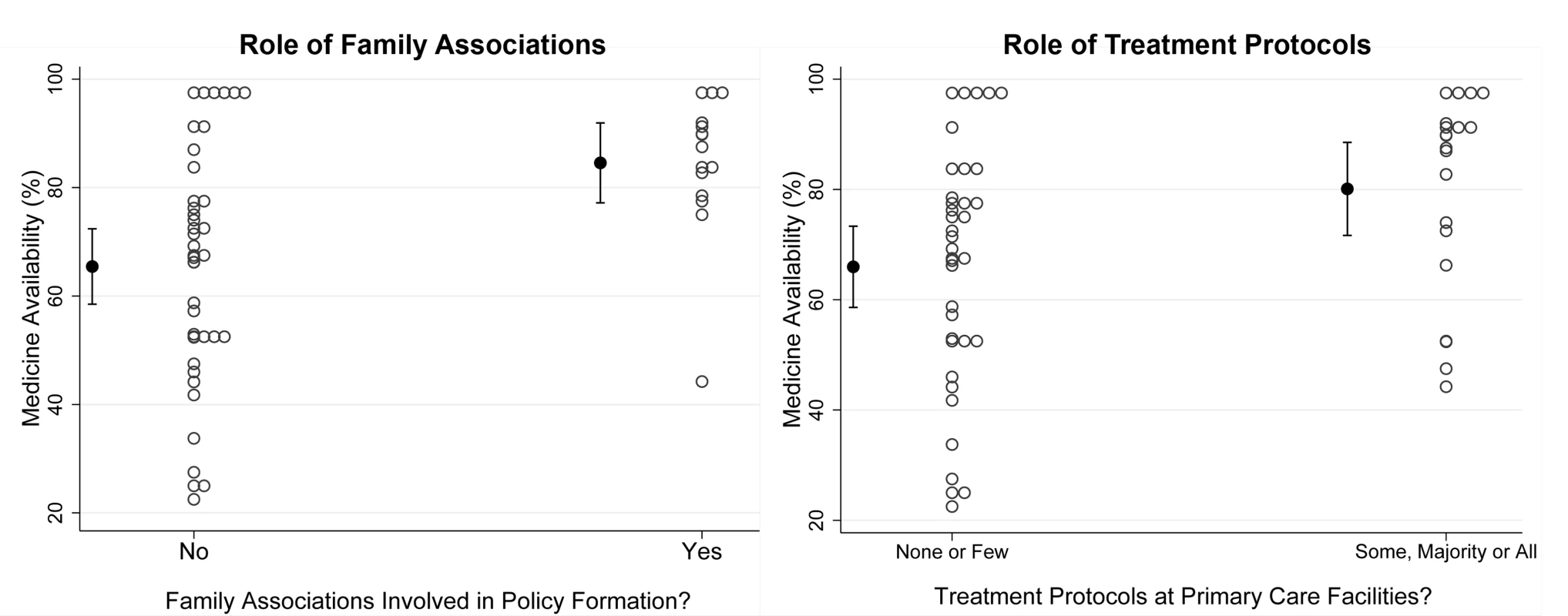
Countries with family associations participating in mental health policy formation have psychotropic medicines available at 85% of facilities, as compared to <70% of facilities in countries without family associations. Countries with protocols in some, most, or all primary care facilities have 80% availability, as compared to 66% availability in countries with no or few facilities with protocols in place. Affordability of Medicines to Consumers
Fifty-four countries provided data on affordability of psychotropic medicines to consumers. While the average cost of psychotropic medicine was 3.6% of daily income, variation in price was considerable (SD = 5.5% daily income). In total, individuals in 26% (n = 14) of respondent countries have to pay greater than 5% of daily income, and individuals in 11% (n = 6) of countries greater than 10% of daily income. Estimated costs also varied by income group classification: On average, purchasing price was 4.6% of daily income in low income countries (SD = 4.7%, n = 15), 4.0% in lower-middle income countries (SD = 6.7%, n = 26), and 1.7% in upper-middle income countries (SD = 2.9%, n = 12).
Three independent measures were significantly associated with affordability of medicines to consumers. The overall rate of human resources working within the mental health sector of the country was negatively associated with cost to consumers (β = −0.20, p<0.05), with an increase of ten health workers per 100,000 population associated with a two percentage point decrease in daily income needed to purchase medicines. Similarly, increasing health expenditures dedicated to mental health by 1% was associated with a 1.2% decrease in percentage daily income needed to acquire medicine (β = −1.17, p<0.01). Additionally, availability of mental health care to prisoners was also negatively associated with affordability (β = −1.23, p = 0.02). Table 3 presents an overview of these results.
Tab. 3. Domain-specific associations with medicine affordability. 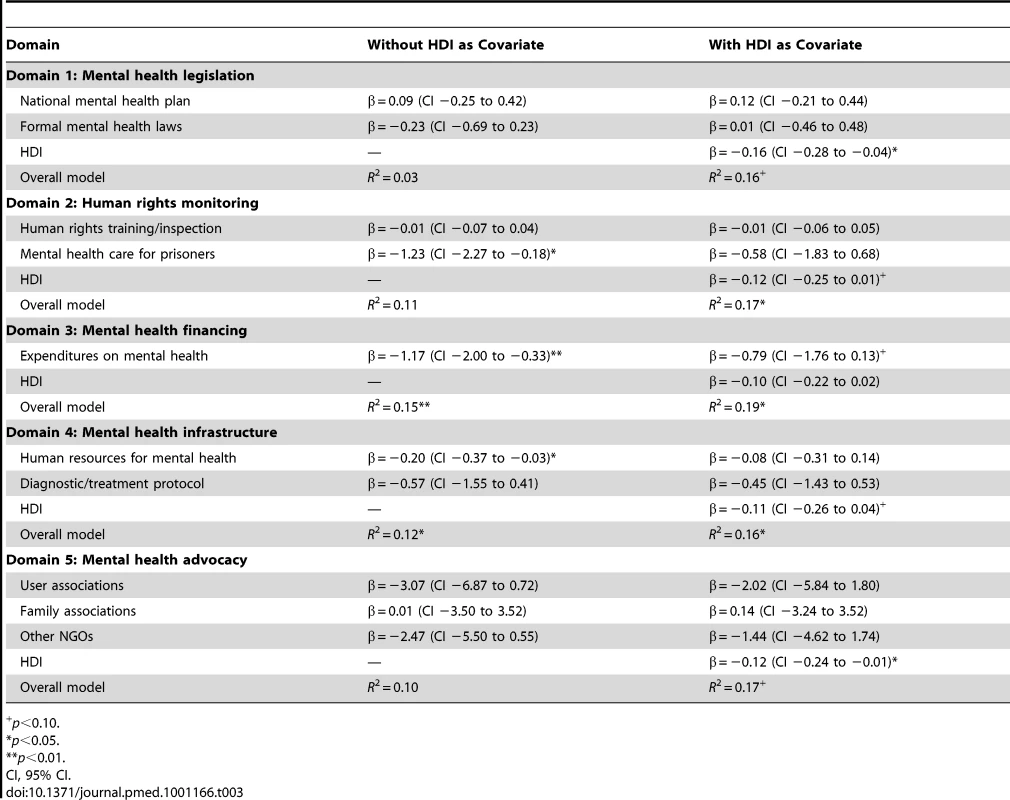
+p<0.10. Across health systems domains, no indicator variable remained significant when HDI was included as a covariate. However, HDI itself was strongly associated with medicine costs to consumers (r = −0.38, p<0.01) and played a significant role in regression analyses, as such indicating the centrality of overall country development in relation to affordability of medicines to consumers. Figure 2 illustrates this relationship.
Fig. 2. Association between HDI and affordability. 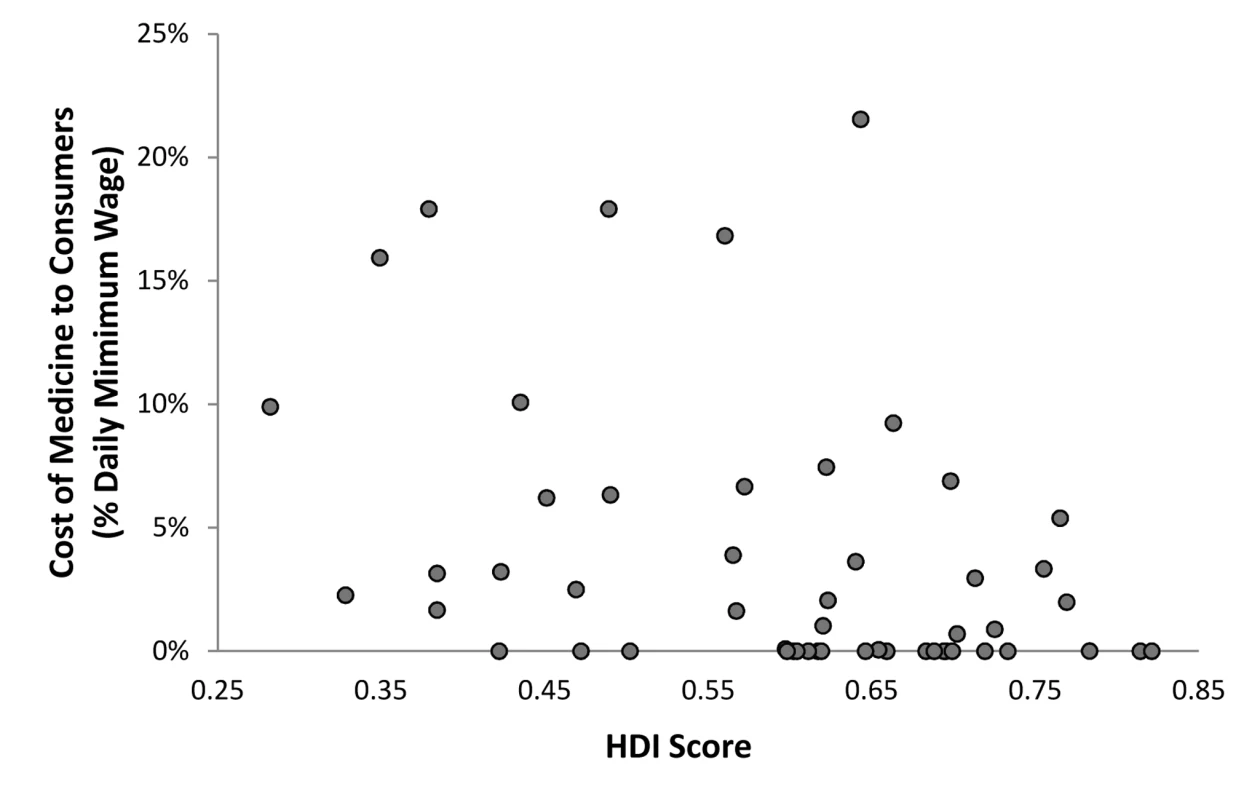
HDI represents a composite measure of a country's average life expectancy, educational attainment, and gross domestic product per capita. The strength of this measurement's association with affordability of psychotropic medicines is r = −0.38, p<0.01. Discussion
To our knowledge, this is the first study to examine the association between health systems measures and access to psychotropic medicines across a diverse group of LAMICs. These data indicate that access to medicines is associated with the content of structures within countries' mental health systems, but also that there are distinctions between availability and affordability outcomes; in particular, overall country development is more strongly associated with affordability compared to availability.
Availability of Psychotropic Medicines
Availability of psychotropic medicines was associated with components within each of the five mental health systems domains. One possible explanation for the association between human rights training and inspection and increased availability of psychotropic medicines is that countries that place greater emphasis on the protection of vulnerable populations, including those with mental illness, may be more likely to consider availability of medications among those protections deemed necessary [62]. More generally, this finding suggests that cultivating a public perception that patients with mental illness deserve fundamental protections has potential to expand access to treatment, a finding supported by the role of family associations in promoting access (see below). However, it is also noteworthy that the magnitude of the effect is relatively modest: a 10% increase in training and inspection across facilities corresponds to an estimated 2.5% increase in availability.
Greater budget allocation towards mental health was associated with increased availability of psychotropic medicines, but this association was mitigated in countries with low HDI. This finding is relatively unsurprising given previous research showing that poorer countries allocate less of their budget towards mental health [8]. Indeed, in poorer countries infectious diseases and maternal and child health issues account for a greater percentage of morbidity and mortality and likely affect the priority of mental health care [63]. Additionally, there is an underestimation of the magnitude of mental health problems in LAMICs, which is compounded by stigma and negative cultural perceptions towards these problems [64].
Within the realm of mental health legislation, the specificity of content in mental health plans and laws were both associated with availability; however, only the association with mental health plans remained significant when controlling for the effect of HDI. The more stable effect of a national plan is in accordance with the contemporary nature of this form of legislation: While the median year of countries' most recent national plan revisions was 2003, the median year of countries' most recent law revisions was 1985. Insofar as plans are more current, they are more liable to characterize governments' present efforts to strengthen their mental health systems, irrespective of development status. Although previous reports have posited a conceptual link between government legislation and expansion of access to treatment [5],[6],[8],[65], this study reports an empirical association at the cross-national level. Overall, a national mental health policy that meets all 12 content specifications is associated with 15% greater availability of medicines across facilities, and mental health laws that meet all eight content specifications 13% greater availability, as compared to having no legislation.
With regard to advocacy groups, only family associations—and more specifically the involvement of family associations in shaping the formulation of mental health legislation—were associated with greater availability of medicines: Participation of families was associated with a 16.5% increase in availability of medicines. In contrast, user association involvement and the presence of NGOs were not significant. Family associations may play a special role inasmuch as individuals who comprise them identify with those affected by illness, but may also hold more influence than users, as users often represent a particularly vulnerable and often marginalized population, which may not be granted a voice to advocate for themselves [62],[66]. Furthermore, the interests and priorities of users often differ from those of their family members [66]. Indeed, in many instances families may value the effect of medicines more than users, who often prefer psychosocial treatments. However, it is unclear from our results whether users have not been active in policy formation in general or have not voiced a specific desire for greater access to psychotropic medicines; further research along these lines is required.
The presence of protocols for diagnosis and treatment of mental disorders in primary care settings was also associated with medicine availability: The existence of protocols in all or almost all primary care facilities correlates with 17% greater availability of medicines, as compared to having no protocols in place. From one perspective, protocols may serve to increase health workers' ability to detect and diagnose mental disorders, and in turn generate greater demand for availability of medicines as part of treatment [67],[68]. Yet, it may also be the case that higher income countries have the ability to supply both treatment protocols and medicines to primary care facilities. This latter view is supported by the finding that the association between protocols and availability is weakened by the inclusion of HDI.
Overall, our results suggest a foundational role for health system strengthening in promoting the availability of psychotropic medicines: Detailed mental health legislation, involvement of family associations in policy formation, greater allocation of financial resources to mental health, and the existence of protocols for diagnosis and treatment of mental disorders are all associated with greater medicine availability.
Affordability of Psychotropic Medicines
While a variety of health systems inputs contribute to the availability of psychotropic medicines at mental health facilities, a more limited array of indicators was related to the affordability of these drugs to consumers. Without taking HDI into account, only three independent variables were significantly associated with affordability: the percentage of health expenditures directed towards mental health, the number of human resources working in the field of mental health (per 100,000 population), and availability of mental health care to prisoners.
The finding that affordability is associated with the percentage of the health budget directed towards mental health again highlights the central importance of allocating financial resources towards mental health in order to broaden access, though the effect of this is modest. Similarly, greater levels of human resources were related to affordability, with an increase of ten mental health workers per 100,000 population associated with a 2% decrease in wages needed to pay for psychotropic medicines.
While both findings highlight a potential role for resource allocation in promoting affordability, there are competing interpretations of these results. On the one hand, greater allocation of resources to mental health may reflect government prioritization of treating mental illness. However, this conclusion is challenged by the findings that neither national mental health plans nor national mental health laws correlated with affordability (p>0.50). On the other hand, overall country development, as reflected by HDI, might have a role in determining whether the country has resources available. This finding is supported by the role of HDI, which, when included as a covariate, contributes to the nonsignificance of both variables (i.e., the effects of financial and human resources) at the 0.05 alpha level.
Results also suggest a relationship between mental health care for prisoners and affordability of medications to consumers: In contexts where prisoners are granted greater access to mental health care, medicines tend to be more affordable. While speculative, it is plausible that the wealth of a country acts as a prior determinant, whereby richer countries can both subsidize medicines and afford mental health care for prisoners. However, further research is required to investigate this linkage.
Irrespective of a country's development status as measured by HDI, the integrity of mental health systems remains associated with availability of medicines, but not to affordability of medicines to consumers. One principal interpretation of this result relates to the emphasis that intergovernmental organizations like the World Health Organization place on countries' construction of an essential medicines list, which promotes a modest level of essential psychotropic medicines across countries, largely independent of development status [69]. For this reason, factors more exogenous to development—namely, those relating more to the functional integrity of the countries' mental health system—are liable to relate to availability. In contrast, there is a less clear-cut set of operationalized standards and strategies for how to make essential medications affordable to consumers within countries. Therefore, one would expect affordability to have a much more direct relationship with country development outside the health sector. Poorer countries that cannot afford to subsidize psychotropic drugs may be encouraged to make drugs available to consumers, but nevertheless the consumers may have to bear the purchasing costs.
Consistent with the present results, other studies have similarly demonstrated the importance of country wealth in promoting treatment of mental disorders. For example, Large and colleagues found a significant association between country GDP and duration of untreated psychosis in LAMICs, whereby mean duration of untreated psychosis fell by 6 wk for every US$1,000 of GDP (purchasing power parity) [70]. In a similar vein, wealthier LAMICs are more likely to publish research on mental disorders [71]. These findings, as well as those concluded upon from this study, underscore a common narrative: country wealth and development appear to play central roles in promoting the mental health research and treatment agenda of LAMICs.
In addition to the meta-level impact of HDI on affordability, it is also important to note the wide variation in affordability scores across countries at similar levels of HDI, as indicated by the dispersion of data points in Figure 2. Interpreting and accounting for this variability in future analyses will entail the acquisition of more detailed data, the refinement of assessment tools, and a conceptual focus on what works at the meso - and micro-levels of health systems.
Study Limitations
Several limitations should be acknowledged. First, the number of observations in this study is relatively small and therefore precluded analysis of a large number of variables within each mental health systems' domain. This limitation was addressed, in part, by the creation of composite measures that characterize the broader aspects of each domain. However, one important consequence of this is that specificity of individual associations may be lost: for example, the relationship between total human resources and access could be examined, but individual relationships between psychiatrists, nurses, and psychologists and outcomes of interest could not be established. Similarly, regression analysis across health system domains could not be conducted and would likely have contributed to significantly improved model fit. As more countries participate in the WHO-AIMS project, such analyses will become increasingly feasible.
Secondly, given the usage of cross-sectional data, the present analyses cannot distinguish the directionality of individual relationships. Associations identified in this study are helpful insofar as they pinpoint commonalities among those health systems with greater access to medicines. Moreover, while the inclusion of HDI as a covariate has the effect of making independent measures more comparable across countries, it also risks overcontrolling for social processes, as it is not a strictly economic measure.
Lastly, while WHO-AIMS data are collected by country focal points using a specific set of instructions and are reviewed by WHO headquarters, the data are still imprecise insofar as most LAMICs do not have advanced technologies for gathering mental health systems data. However, such imprecision would likely bias results towards nonsignificance and therefore bolsters the validity of associations identified here. The use of country focal points also increases the possibility that some countries reported biased results. In general, all countries should have a similar impetus to bias estimates upwards. However, results from analyses would only be affected insofar as countries that overestimate results differ in a significant and systematic way from countries which do not and this difference is related to the outcomes of interest, a scenario that seems unlikely.
Conclusion
Improving access to psychotropic medicines constitutes an essential and cost-effective component in the treatment of mental illnesses, including mood disorders, psychotic disorders, and anxiety disorders. We found that availability of medicines at mental health facilities was associated with components within all five mental health systems domains. In contrast, a limited set of indicators was associated with affordability. While correlates of availability remained significant when controlling for HDI, none remained significant in relation to affordability. Results suggest that strengthening specific mental health systems features might be an important way to facilitate access to psychotropic medicines, and results also underscore the differentially greater role of country development in promoting affordability. However, given the associational nature of these analyses and limited sample size, future analyses should be conducted to extend the main findings of this study. Furthermore, in light of the heterogeneity of findings across countries at similar levels of HDI, research should continue to identify what kinds of interventions can positively influence affordability, including within the health sector.
Zdroje
1. DemyttenaereKBruffaertsRPosada-VillaJGasquetIKovessV 2004 Prevalence, severity, and unmet need for treatment of mental disorders in the World Health Organization World Mental Health Surveys. JAMA 291 2581 2590
2. WHO 2001 The world health report 2001 - mental health: new understanding, New Hope Geneva World Health Organization
3. MathersCDLoncarD 2006 Projections of global mortality and burden of disease from 2002 to 2030. PLoS Med 3 e442
4. PrinceMPatelVSaxenaSMajMMaselkoJ 2007 No health without mental health. Lancet 370 859 877
5. WHO 2008 mhGAP Mental Health Action Programme: scaling up care for mental, neurological and substance abuse disorders Geneva World Health Organization
6. SaxenaSSharanPGarridoMSaracenoB 2006 World Health Organization's Mental Health Atlas 2005: implications for policy development. World Psychiatry 5 179 184
7. WHO 2005 Mental health atlas 2005 Geneva WHO
8. SaxenaSThornicroftGKnappMWhitefordH 2007 Resources for mental health: scarcity, inequity, and inefficiency. Lancet 370 878 889
9. PatelV 2009 The future of psychiatry in low - and middle-income countries. Psychol Med 39 1759 1762
10. PatelVMajMFlisherAJMJDESKoschorkeM 2010 Reducing the treatment gap for mental disorders: a WPA survey. World Psychiatry 9 169 176
11. BhanaAPetersenIBaillieKLFlisherAJ The Mhapp Research Programme C 2010 Implementing the World Health Report 2001 recommendations for integrating mental health into primary health care: a situation analysis of three African countries: Ghana, South Africa and Uganda. Int Rev Psychiatry 22 599 610
12. WHO 2008 mhGAP: Mental health gap action programme Geneva World Health Organization
13. PatelVThornicroftG 2009 Packages of care for mental, neurological, and substance use disorders in low - and middle-income countries: PLoS Medicine Series. PLoS Med 6 e1000160 doi:10.1371/journal.pmed.1000160
14. ArayaRRojasGFritschRGaeteJRojasM 2003 Treating depression in primary care in low-income women in Santiago, Chile: a randomised controlled trial. Lancet 361 995 1000
15. PatelVChisholmDRabe-HeskethSDias-SaxenaFAndrewG 2003 Efficacy and cost-effectiveness of drug and psychological treatments for common mental disorders in general health care in Goa, India: a randomised, controlled trial. Lancet 361 33 39
16. LiuPHeFFBaiWPYuQShiW 2004 Menopausal depression: comparison of hormone replacement therapy and hormone replacement therapy plus fluoxetine. Chin Med J (Engl) 117 189 194
17. AliBSRahbarMHNaeemSGulAMubeenS 2003 The effectiveness of counseling on anxiety and depression by minimally trained counselors: a randomized controlled trial. Am J Psychother 57 324 336
18. BassJNeugebauerRCloughertyKFVerdeliHWickramaratneP 2006 Group interpersonal psychotherapy for depression in rural Uganda: 6-month outcomes: randomised controlled trial. Br J Psychiatry 188 567 573
19. BoltonPBassJNeugebauerRVerdeliHCloughertyKF 2003 Group interpersonal psychotherapy for depression in rural Uganda: a randomized controlled trial. JAMA 289 3117 3124
20. PatelVWeissHAChowdharyNNaikSPednekarS 2010 Effectiveness of an intervention led by lay health counsellors for depressive and anxiety disorders in primary care in Goa, India (MANAS): a cluster randomised controlled trial. Lancet 376 2086 2095
21. AliNSAliBSAzamISKhuwajaAK 2010 Effectiveness of counseling for anxiety and depression in mothers of children ages 0–30 months by community workers in Karachi, Pakistan: a quasi experimental study. BMC Psychiatry 10 57
22. LiebermanJAPhillipsMGuHStroupSZhangP 2003 Atypical and conventional antipsychotic drugs in treatment-naive first-episode schizophrenia: a 52-week randomized trial of clozapine vs chlorpromazine. Neuropsychopharmacology 28 995 1003
23. LiZArthurD 2005 Family education for people with schizophrenia in Beijing, China: randomised controlled trial. Br J Psychiatry 187 339 345
24. RanMSXiangMZChanCLLeffJSimpsonP 2003 Effectiveness of psychoeducational intervention for rural Chinese families experiencing schizophrenia–a randomised controlled trial. Soc Psychiatry Psychiatr Epidemiol 38 69 75
25. ChienWTChanSWThompsonDR 2006 Effects of a mutual support group for families of Chinese people with schizophrenia: 18-month follow-up. Br J Psychiatry 189 41 49
26. BaltieriDADe AndradeAG 2004 Acamprosate in alcohol dependence: a randomized controlled efficacy study in a standard clinical setting. J Stud Alcohol 65 136 139
27. BaltieriDAde AndradeAG 2003 Efficacy of acamprosate in the treatment of alcohol-dependent outpatients. Rev Bras Psiquiatr 25 156 159
28. AhmadiJBabaeebeigiMMaanyIPorterJMohagheghzadehM 2004 Naltrexone for alcohol-dependent patients. Ir J Med Sci 173 34 37
29. BaborTFGrantMAcudaWBurnsFHCampilloC 1994 A randomized clinical trial of brief interventions in primary care: summary of a WHO project. Addiction 89 657 660; discussion 660–678
30. DaveUPChauvanVDalviJ 1993 Evaluation of BR-16 A (Mentat) in cognitive and behavioural dysfunction of mentally retarded children–a placebo-controlled study. Indian J Pediatr 60 423 428
31. SzobotCMKetzerCCunhaRDParenteMALanglebenDD 2003 The acute effect of methylphenidate on cerebral blood flow in boys with attention-deficit/hyperactivity disorder. Eur J Nucl Med Mol Imaging 30 423 426
32. RussellPSal JohnJKLakshmananJL 1999 Family intervention for intellectually disabled children. Randomised controlled trial. Br J Psychiatry 174 254 258
33. LagerkvistB 1992 Community-based rehabilitation–outcome for the disabled in the Philippines and Zimbabwe. Disabil Rehabil 14 44 50
34. Lundgren-LindquistBNordholmLA 1996 The impact of community-based rehabilitation as perceived by disabled people in a village in Botswana. Disabil Rehabil 18 329 334
35. O'TooleB 1988 A community-based rehabilitation programme for pre-school disabled children in Guyana. Int J Rehabil Res 11 323 334
36. PatelVArayaRChatterjeeSChisholmDCohenA 2007 Treatment and prevention of mental disorders in low-income and middle-income countries. Lancet 370 991 1005
37. KnappMFunkMCurranCPrinceMGriggM 2006 Economic barriers to better mental health practice and policy. Health Policy Plan 21 157 170
38. NarasimhanVBrownHPablos-MendezAAdamsODussaultG 2004 Responding to the global human resources crisis. Lancet 363 1469 1472
39. ThirthalliJChandPK 2009 The implications of medication development in the treatment of substance use disorders in developing countries. Curr Opin Psychiatry 22 274 280
40. OdejideAO 2006 Status of drug use/abuse in Africa. Int J Ment Health Addict 4 87 105
41. DieyeAMSyllaMNdiayeANdiayeMSyGY 2006 Benzodiazepines prescription in Dakar: a study about prescribing habits and knowledge in general practitioners, neurologists and psychiatrists. Fundam Clin Pharmacol 20 235 238
42. NaqviHA 2005 Mental health care and mental health legislation in Pakistan: no mercy for losers. PLoS Med 2 e397 doi:10.1371/journal.pmed.0020397
43. JainSJadhavS 2009 Pills that swallow policy: clinical ethnography of a Community Mental Health Program in northern India. Transcult Psychiatry 46 60 85
44. PatelVAndradeC 2003 Pharmacological treatment of severe psychiatric disorders in the developing world: lessons from India. CNS Drugs 17 1071 1080
45. PatelV 1995 Explanatory models of mental illness in sub-Saharan Africa. Soc Sci Med 40 1291 1298
46. GhaneSKolkAMEmmelkampPM 2010 Assessment of explanatory models of mental illness: effects of patient and interviewer characteristics. Soc Psychiatry Psychiatr Epidemiol 45 175 182
47. WHO 2009 Improving mental health systems and services for mental health Geneva World Health Organization
48. WHO 2005 WHO-AIMS version 2.2: World Health Organization assessment instrument for mental health systems Geneva World Health Organization
49. WHO 2007 Everybody's business: strengthening health systems to improve health outcomes Geneva World Health Organization
50. WHO 2004 Mental health policy, plans and programmes Geneva World Health Organization
51. TownsendCWhitefordHBainganaFGulbinatWJenkinsR 2004 The mental health policy template: domains and elements for mental health policy formulation. Int Rev Psychiatry 16 18 23
52. WHO 2011 WHO-AIMS - General Information Geneva WHO
53. LoraAKohnRLevavIMcBainRMorrisJ Accessibility, patterns of care and the treatment gap in schizophrenic disorders: A WHO-AIMS survey in 50 low - and middle-income countries. Bull World Health Organ. Available: http://www.who.int/bulletin/online_first/11-089284.pdf. Accessed 26 December 2011. In press
54. World Bank 2010 Country and lending groups Washington (D.C.) The World Bank
55. WHO 2008 Measuring medicine price, availability, affordability and price components Geneva WHO
56. CameronAEwenMRoss-DegnanDBallDLaingR 2009 Medicine prices, availability, and affordability in 36 developing and middle-income countries: a secondary analysis. Lancet 373 240 249
57. NiensLMBrouwerWB 2009 Better measures of affordability required. Lancet 373 1081; author reply 1081–1082
58. UNDP 2010 Human Development Report 2010 – the real wealth of nations: pathways to human development New York United Nations Development Programme
59. O'BrienR 2007 A caution regarding rules of thumb for variance inflation factors. Qual Quant 41 673 690
60. RubinDB 1987 Multiple imputation for nonresponse in surveys New York Wiley
61. CupplesLAHeerenTSchatzkinAColtonT 1984 Multiple testing of hypotheses in comparing two groups. Ann Intern Med 100 122 129
62. WHO 2010 Mental health and development: targeting people with mental health conditions as a vulnerable group Geneva World Health Organization
63. WHO 2008 The global burden of disease–2004 update Geneva World Health Organization
64. SaracenoBvan OmmerenMBatnijiRCohenAGurejeO 2007 Barriers to improvement of mental health services in low-income and middle-income countries. Lancet 370 1164 1174
65. PetersenILundCSteinDJ 2011 Optimizing mental health services in low-income and middle-income countries. Curr Opin Psychiatry 24 318 323
66. FunkMMinolettiADrewNTaylorJSaracenoB 2006 Advocacy for mental health: roles for consumer and family organizations and governments. Health Promot Int 21 70 75
67. KaramustafaliogluO 2010 Major depressive disorder, mental health care, and the use of guidelines in the Middle East. J Clin Psychiatry 71 Suppl E1 e07
68. HickieI 2004 Treatment guidelines for depression in the Asia Pacific region: a review of current developments. Australas Psychiatry 12 Suppl S33 37
69. WHO 2009 WHO model list of essential medicines: 16th list, March, 2009 Geneva World Health Organization
70. LargeMFarooqSNielssenOSladeT 2008 Relationship between gross domestic product and duration of untreated psychosis in low - and middle-income countries. Br J Psychiatry 193 272 278
71. LargeMNielssenOFarooqSGlozierN 2010 Increasing rates of psychiatric publication from low - and middle-income countries. Int J Soc Psychiatry 56 497 506
Štítky
Interní lékařství
Článek Trends in Compulsory Licensing of Pharmaceuticals Since the Doha Declaration: A Database AnalysisČlánek Effect of Sanitation on Soil-Transmitted Helminth Infection: Systematic Review and Meta-AnalysisČlánek A New Year at : Maintaining a Focus on the World's Health Priorities and Identifying the Gaps
Článek vyšel v časopisePLOS Medicine
Nejčtenější tento týden
2012 Číslo 1- Berberin: přírodní hypolipidemikum se slibnými výsledky
- Léčba bolesti u seniorů
- Příznivý vliv Armolipidu Plus na hladinu cholesterolu a zánětlivé parametry u pacientů s chronickým subklinickým zánětem
- Jak postupovat při výběru betablokátoru − doporučení z kardiologické praxe
- Červená fermentovaná rýže účinně snižuje hladinu LDL cholesterolu jako vhodná alternativa ke statinové terapii
-
Všechny články tohoto čísla
- What Will It Take to Eliminate Pediatric HIV? Reaching WHO Target Rates of Mother-to-Child HIV Transmission in Zimbabwe: A Model-Based Analysis
- Challenging Medical Ghostwriting in US Courts
- The Inadequate Treatment of Pain: Collateral Damage from the War on Drugs
- A United Nations General Assembly Special Session for Mental, Neurological, and Substance Use Disorders:
- Trends in Compulsory Licensing of Pharmaceuticals Since the Doha Declaration: A Database Analysis
- Monitoring the Introduction of Pneumococcal Conjugate Vaccines into West Africa: Design and Implementation of a Population-Based Surveillance System
- The Role of Health Systems Factors in Facilitating Access to Psychotropic Medicines: A Cross-Sectional Analysis of the WHO-AIMS in 63 Low- and Middle-Income Countries
- Trends in Resource Utilization by Children with Neurological Impairment in the United States Inpatient Health Care System: A Repeat Cross-Sectional Study
- Hitting Hotspots: Spatial Targeting of Malaria for Control and Elimination
- Effect of Sanitation on Soil-Transmitted Helminth Infection: Systematic Review and Meta-Analysis
- Effects of Two Commercial Electronic Prescribing Systems on Prescribing Error Rates in Hospital In-Patients: A Before and After Study
- A New Year at : Maintaining a Focus on the World's Health Priorities and Identifying the Gaps
- Long-Term Survival in a Large Cohort of Patients with Venous Thrombosis: Incidence and Predictors
- Ensemble Modeling of the Likely Public Health Impact of a Pre-Erythrocytic Malaria Vaccine
- Adult Mortality Attributable to Preventable Risk Factors for Non-Communicable Diseases and Injuries in Japan: A Comparative Risk Assessment
- PLOS Medicine
- Archiv čísel
- Aktuální číslo
- Informace o časopisu
Nejčtenější v tomto čísle- Ensemble Modeling of the Likely Public Health Impact of a Pre-Erythrocytic Malaria Vaccine
- Adult Mortality Attributable to Preventable Risk Factors for Non-Communicable Diseases and Injuries in Japan: A Comparative Risk Assessment
- What Will It Take to Eliminate Pediatric HIV? Reaching WHO Target Rates of Mother-to-Child HIV Transmission in Zimbabwe: A Model-Based Analysis
- Challenging Medical Ghostwriting in US Courts
Kurzy
Zvyšte si kvalifikaci online z pohodlí domova
Současné možnosti léčby obezity
nový kurzAutoři: MUDr. Martin Hrubý
Všechny kurzyPřihlášení#ADS_BOTTOM_SCRIPTS#Zapomenuté hesloZadejte e-mailovou adresu, se kterou jste vytvářel(a) účet, budou Vám na ni zaslány informace k nastavení nového hesla.
- Vzdělávání



