-
Články
Top novinky
Reklama- Vzdělávání
- Časopisy
Top články
Nové číslo
- Témata
Top novinky
Reklama- Videa
- Podcasty
Nové podcasty
Reklama- Kariéra
Doporučené pozice
Reklama- Praxe
Top novinky
ReklamaTrends in Resource Utilization by Children with Neurological Impairment in the United States Inpatient Health Care System: A Repeat Cross-Sectional Study
Background:
Care advances in the United States (US) have led to improved survival of children with neurological impairment (NI). Children with NI may account for an increasing proportion of hospital resources. However, this assumption has not been tested at a national level.Methods and Findings:
We conducted a study of 25,747,016 US hospitalizations of children recorded in the Kids' Inpatient Database (years 1997, 2000, 2003, and 2006). Children with NI were identified with International Classification of Diseases, 9th Revision, Clinical Modification diagnoses resulting in functional and/or intellectual impairment. We assessed trends in inpatient resource utilization for children with NI with a Mantel-Haenszel chi-square test using all 4 y of data combined. Across the 4 y combined, children with NI accounted for 5.2% (1,338,590) of all hospitalizations. Epilepsy (52.2% [n = 538,978]) and cerebral palsy (15.9% [n = 164,665]) were the most prevalent NI diagnoses. The proportion of hospitalizations attributable to children with NI did not change significantly (p = 0.32) over time. In 2006, children with NI accounted for 5.3% (n = 345,621) of all hospitalizations, 13.9% (n = 3.4 million) of bed days, and 21.6% (US$17.7 billion) of all hospital charges within all hospitals. Over time, the proportion of hospitalizations attributable to children with NI decreased within non-children's hospitals (3.0% [n = 146,324] in 1997 to 2.5% [n = 113,097] in 2006, p<.001) and increased within children's hospitals (11.7% [n = 179,324] in 1997 to 13.5% [n = 209,708] in 2006, p<0.001). In 2006, children with NI accounted for 24.7% (2.1 million) of bed days and 29.0% (US$12.0 billion) of hospital charges within children's hospitals.Conclusions:
Children with NI account for a substantial proportion of inpatient resources utilized in the US. Their impact is growing within children's hospitals. We must ensure that the current health care system is staffed, educated, and equipped to serve this growing segment of vulnerable children.
: Please see later in the article for the Editors' Summary
Published in the journal: . PLoS Med 9(1): e32767. doi:10.1371/journal.pmed.1001158
Category: Research Article
doi: https://doi.org/10.1371/journal.pmed.1001158Summary
Background:
Care advances in the United States (US) have led to improved survival of children with neurological impairment (NI). Children with NI may account for an increasing proportion of hospital resources. However, this assumption has not been tested at a national level.Methods and Findings:
We conducted a study of 25,747,016 US hospitalizations of children recorded in the Kids' Inpatient Database (years 1997, 2000, 2003, and 2006). Children with NI were identified with International Classification of Diseases, 9th Revision, Clinical Modification diagnoses resulting in functional and/or intellectual impairment. We assessed trends in inpatient resource utilization for children with NI with a Mantel-Haenszel chi-square test using all 4 y of data combined. Across the 4 y combined, children with NI accounted for 5.2% (1,338,590) of all hospitalizations. Epilepsy (52.2% [n = 538,978]) and cerebral palsy (15.9% [n = 164,665]) were the most prevalent NI diagnoses. The proportion of hospitalizations attributable to children with NI did not change significantly (p = 0.32) over time. In 2006, children with NI accounted for 5.3% (n = 345,621) of all hospitalizations, 13.9% (n = 3.4 million) of bed days, and 21.6% (US$17.7 billion) of all hospital charges within all hospitals. Over time, the proportion of hospitalizations attributable to children with NI decreased within non-children's hospitals (3.0% [n = 146,324] in 1997 to 2.5% [n = 113,097] in 2006, p<.001) and increased within children's hospitals (11.7% [n = 179,324] in 1997 to 13.5% [n = 209,708] in 2006, p<0.001). In 2006, children with NI accounted for 24.7% (2.1 million) of bed days and 29.0% (US$12.0 billion) of hospital charges within children's hospitals.Conclusions:
Children with NI account for a substantial proportion of inpatient resources utilized in the US. Their impact is growing within children's hospitals. We must ensure that the current health care system is staffed, educated, and equipped to serve this growing segment of vulnerable children.
: Please see later in the article for the Editors' SummaryIntroduction
Neurological impairment (NI) comprises a heterogeneous group of static and progressive health conditions that involve the central and peripheral nervous systems and result in functional and/or intellectual impairment. This group includes children with epilepsy, infants who are born prematurely and have hypoxic-ischemic injury to the brain, and children with genetic and metabolic disorders that affect the nervous system.
Although the impact that children with NI have on the pediatric health care system remains largely unknown, emerging evidence describes epidemiologic and care delivery phenomena that suggest this impact may be substantial. The rising prevalence and improved survival of extremely premature infants was associated with an increased risk of cerebral palsy during the 1990s [1],[2]. Children with spina bifida, muscular dystrophy, and other NI-related diagnoses are also surviving longer [3],[4], in part because of improved co-morbid condition management of gastroesophageal reflux disease, oromotor dysfunction, and chronic lung disease [5],[6].
In the US, many children with NI receive uncoordinated, crisis-driven care that is believed to contribute to excessive health care utilization and cost [7]–[11]. They have a disproportionately high use of emergency care health services, and they experience frequent hospitalizations, with subsequently high readmission rates [12],[13]. When hospitalized, they tend to stay longer and have more expensive admissions than other children [14]. It is estimated that a large proportion of lifetime health-related costs for a children with severe NI is attributable to inpatient care [15].
This evidence and our clinical experience suggest that children with NI may account for an increasing proportion of hospital resources. However, this assumption has not been tested at a national level for the US. We undertook this study to (1) evaluate national trends in hospitalizations for children with NI over time within different types of hospitals and (2) describe the patient characteristics and reasons why children with NI are hospitalized.
Methods
Ethics Statement
This study was approved by the Children's Hospital Boston Institutional Review Board with a waiver for informed consent. The investigation was conducted according to the principles expressed in the Declaration of Helsinki.
Study Design and Setting
This is a retrospective, repeat cross-sectional analysis of the Healthcare Cost and Utilization Project Kids' Inpatient Database (KID) for the years 1997, 2000, 2003, and 2006. The KID is a multi-state database of US hospitalizations for children aged 0–18 y [16],[17]. From 1997 to 2006, the KID sample increased from 1.9 million hospital discharges from 2,521 hospitals in 22 states to 3.1 million hospital discharges from 3,739 hospitals in 38 states [16],[17]. The dataset includes a weight variable for each observation that was used to produce national estimates of inpatient resource utilization for children with specific diagnoses while accounting for differences in the KID hospital sampling frame and oversampling of patient sub-populations that could have occurred over time.
Study Population
We identified hospitalizations for children aged 0–18 y with NI as determined by International Classification of Diseases, 9th Revision, Clinical Modification (ICD-9-CM) diagnostic codes. Up to 15 separate ICD-9-CM diagnostic codes are available for each hospitalization in the KID [17]. We assembled an initial list of 606 NI ICD-9-CM codes from previous studies and the tabular index of ICD-9-CM coding [18]–[20].
Pediatric neurologist review of NI ICD-9-CM codes
Two board-certified pediatric neurologists (A. P. and J. L. B.) from different institutions reviewed the initial NI code list [21]. They considered candidate NI ICD-9-CM codes using the following definition: “diagnosis is consistent with NI (static or progressive) and typically results in either functional and/or intellectual impairment” (Figure 1) [19],[20]. The reviewers independently classified each code as “yes,” (diagnosis consistent with NI), “no” (diagnosis not consistent with NI), or “maybe” (diagnosis may be consistent with NI). Code consensus was defined as classification agreement between the reviewers. The reviewers then discussed the codes for which there was classification disagreement (n = 276 [46%]) until consensus was reached (n = 265 [96%]) or was not reached (n = 11 [4%]). A third pediatric neurologist (F. Filloux) classified the remaining non-consensus codes.
Fig. 1. Neurological impairment diagnosis code evaluation. 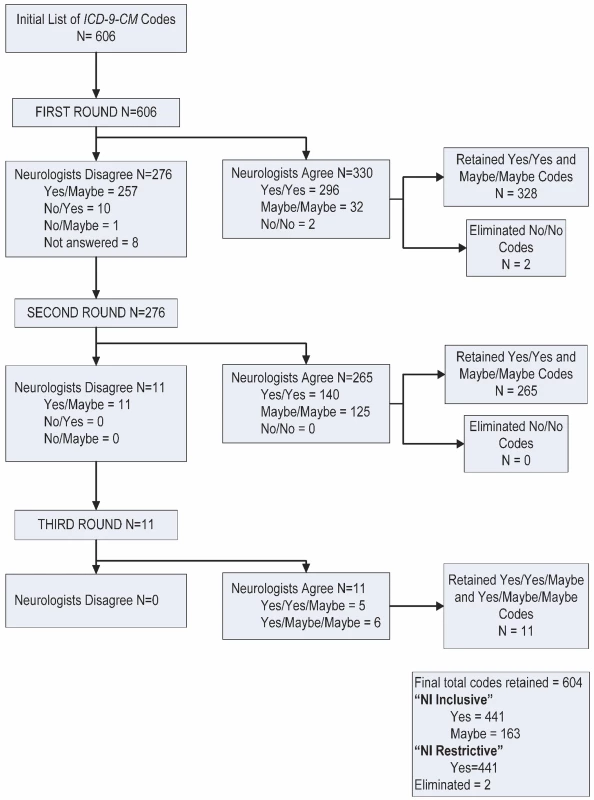
This figure describes the results of the NI diagnosis code evaluation by independent pediatric neurologists. For the main analyses, we retained the NI codes classified “yes–yes” (n = 436), “yes–maybe” (n = 5), and “maybe–maybe” (n = 163). We labeled the codes “NI inclusive.” For the subsequent sensitivity analysis, we excluded the “maybe–maybe” codes from analysis and labeled the retained codes “NI restricted” (Figure 1).
The NI restricted codes were then compared to a list describing coding changes over time assembled by the National Center for Health Statistics and the Centers for Medicare and Medicaid Services. Eleven NI ICD-9-CM codes changed from 1997 to 2006. We incorporated these code changes into our analysis. NI-related hospitalizations were identified from the presence of one or more NI ICD-9-CM codes in any of the discharge diagnoses. The NI ICD-9-CM codes are presented in Table S1.
Main Outcomes
We evaluated the number of hospitalizations, total number of days spent in the hospital, and total charges for admissions associated with the NI inclusive and NI restricted admissions for each year.
Hospital type
We analyzed the measures of NI inpatient resource utilization within all hospitals, children's hospitals, and non-children's hospitals [16],[17]. “Children's hospital” designation was given to hospitals based on specifications from the National Association of Children's Hospitals and Related Institutions. Children's hospitals included freestanding children's hospitals, children's hospitals within adult general hospitals, and children's specialty hospitals.
Reasons for hospitalization
We evaluated patient demographic and clinical characteristics that may correlate with trends in hospital resource use for children with NI over time. Patient demographic variables included patient age (<1 y, 1–4 y, 5–12 y, and 13–18 y) and insurance type (public, private, and other). Race/ethnicity was described but not analyzed because of the extent of missing data (17%–28% for the years under study).
We also analyzed each NI hospitalization to determine if an NI-related surgical procedure occurred. These procedures were classified based on ICD-9-CM procedure codes from previous literature on surgical procedures that these children frequently encounter [6],[14],[20],[22],[23]. We specifically assessed hospitalizations where a gastrostomy (codes beginning with 43.1 or 44.32) and/or fundoplication (codes 44.66 or 44.67) occurred.
We analyzed the principal reason for each hospitalization in children with NI based on the ICD-9-CM Major Diagnostic Category (MDC). MDCs represent 25 mutually exclusive diagnosis domains primarily organized by organ system (nervous system, respiratory system, circulatory system, etc.). One MDC is assigned for each hospitalization from the patient's principal ICD-9-CM diagnosis code. The “newborns and other neonates” MDC includes newborns cared for in a neonatal intensive care unit or in a healthy newborn unit of a maternity hospital.
Statistical Analyses
We evaluated national inpatient resource utilization trends for children with and without NI using all of the years of KID data with a Mantel-Haenszel chi-square test. We used SAS version 9.1.2 (SAS Institute) survey procedures to account for the changing KID sampling frame through a weight variable calculated from the demographic characteristics of the hospitals contributing to the database (ownership/control, bed size, teaching status, children's hospital status, rural/urban location, and state/region) and their hospitalized patients. As the sampling frame expanded over time, the discharge weight decreased so that the increasing proportion of actual records did not falsely inflate the national estimates [24]. All patient-level data were clustered within each hospital and stratified by the demographic characteristics of each hospital to generate national estimates and associated variances of the proportion of inpatient resource utilization attributable to children with NI. Significance threshold was defined as p≤0.05. We adjusted total hospital charges for inflation to 2006 US dollars [25],[26].
Results
There were 25,747,016 hospitalizations for children aged 0–18 y identified from 1997, 2000, 2003, and 2006 combined. Of these, 1,338,590 (5.2%) hospitalizations were associated with children who had NI inclusive diagnoses, and 1,032,829 (4.0%) hospitalizations were associated with children who had NI restricted diagnoses (i.e., the NI codes classified as “maybe–maybe” were excluded). NI inclusive results are presented throughout the Results, with NI restricted results displayed in the table and figures. The most prevalent diagnoses among all hospitalized children with NI were epilepsy (52.2% [n = 538,978]) and cerebral palsy (15.9% [n = 164,665]) (Figure 2). The NI diagnoses varied by age: cerebral palsy was diagnosed in 1.1% (n = 4,708) of hospitalized infants with NI, compared with 17.4% (n = 102,590) of children aged 13–18 y.
Fig. 2. Neurological impairment diagnoses of hospitalized children, Kids' Inpatient Database 1997, 2000, 2003, and 2006. 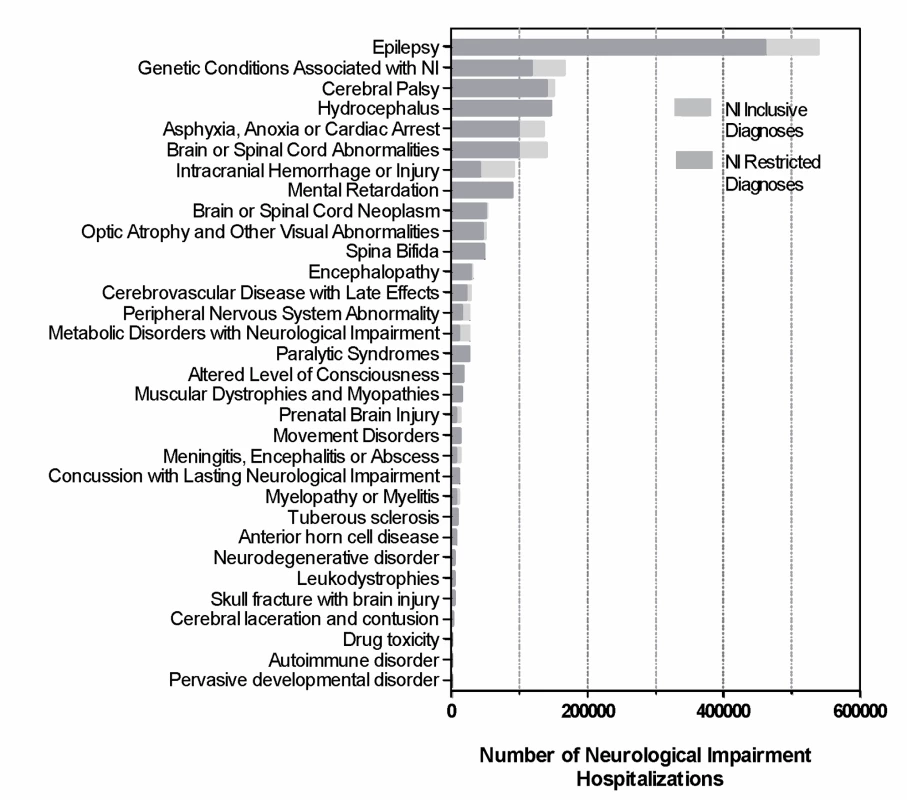
This graph describes the proportion of total NI hospitalizations attributable to each of the NI diagnosis categories. Throughout the study period the proportion of hospitalized children aged 13–18 y that had NI increased from 7.3% to 9.9% (p<0.001) (Table 1). Children with NI aged 13–18 y had a greater increase in hospitalizations (27.8% increase [52,459 in 1997 to 67,045 in 2006]) than children without NI (8.4% decrease [666,403 in 1997 to 610,246 in 2006]). Similar demographic results were observed in children with an NI restricted diagnosis and in children utilizing children's hospitals and non-children's hospitals (data not shown).
Tab. 1. Demographic data for children hospitalized with neurological impairment, Kids' Inpatient Database. 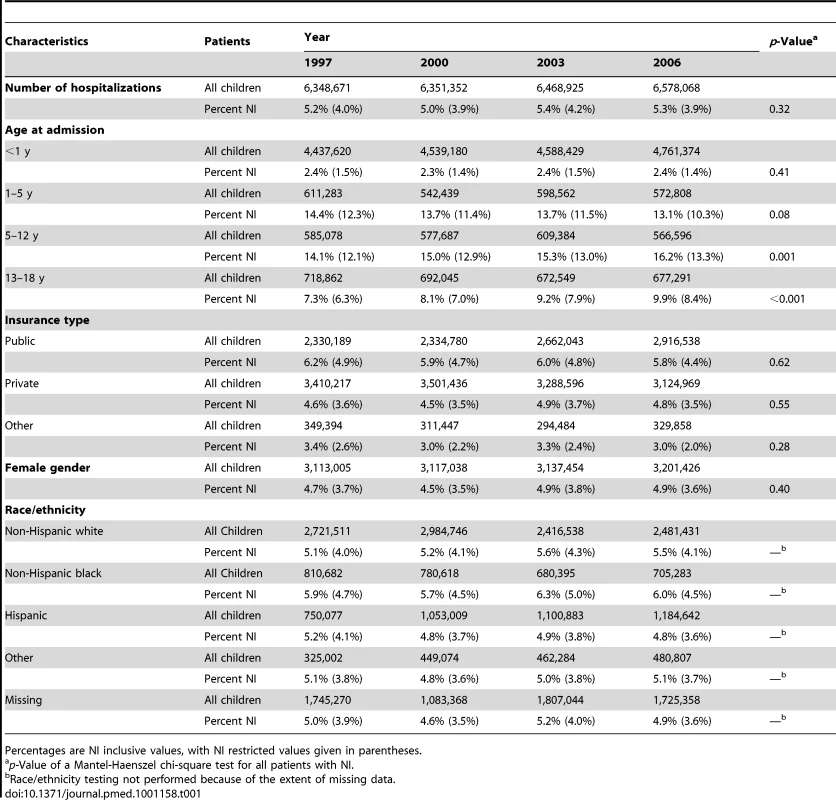
Percentages are NI inclusive values, with NI restricted values given in parentheses. All Hospitals
Inpatient resource utilization
There was no significant change in the proportion of hospitalizations attributable to children with NI (5.1% [n = 325,556] in 1997 to 5.3% [n = 345,621] in 2006, p = 0.32) or the proportion of total charges (20.8% [US$9.8 billion] in 1997 to 21.6% [US$17.7 billion] in 2006, p = 0.09) (Figure 3). However, children with NI accounted for an increasing proportion of hospital days (12.9% in 1997 to 13.9% in 2006, p = 0.05). They experienced a greater increase in hospital days (22.2% increase [2.8 million in 1997 to 3.4 million in 2006]) than children without NI (11.6% increase [18.9 million in 1997 to 21.1 million in 2006], p = 0.05). Similar patterns were observed for children with NI restricted diagnoses.
Fig. 3. Inpatient resource utilization attributable to children with neurological impairment, Kids' Inpatient Database 1997, 2000, 2003, and 2006, by hospital type. 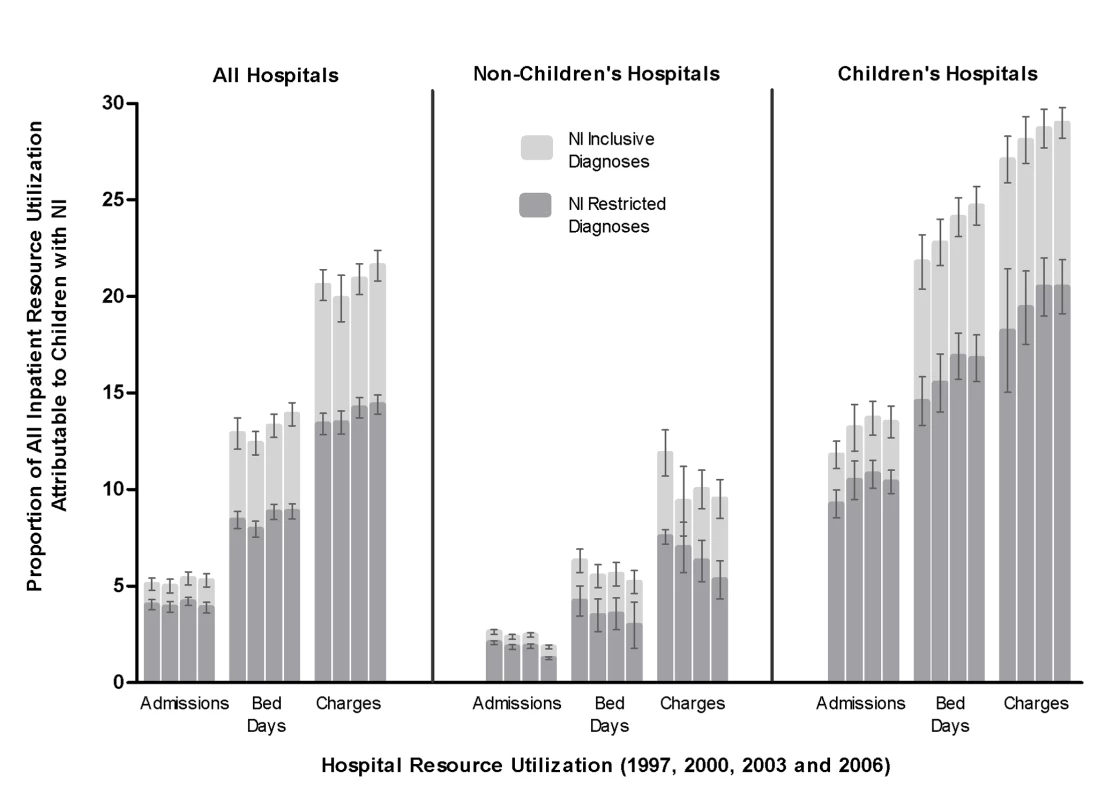
These graphs describe the proportion of all pediatric inpatient health resources attributable to NI from each year. Proportion (with 95% confidence interval) of total number of hospitalizations, hospital bed days, and total aggregate charges are shown for all hospitals, non-children's hospitals, and children's hospitals. Each bar represents 1 y of data. The four bars in each group represent data from 1997, 2000, 2003, and 2006. Reasons for admission
There was a greater increase in admissions for infants with NI (15.6% increase [57,147 in 1997 to 66,046 in 2006]) than for infants without NI (9.9% increase [3,832,736 in 1997 to 4,212,576 in 2006], p<0.001). There were opposing trends in neurological admissions for children with NI (7.0% increase [105,911 in 1997 to 113,321 in 2006]) and children without NI (8.1% decrease [65,731 in 1997 to 60,437 in 2006], p<0.001). There was a greater decrease in respiratory admissions for children with NI (20.5% decrease [48,334 in 1997 to 38,390 in 2006]) than children without NI (13.2% decrease [546,111 in 1997 to 474,125 in 2006], p<0.001). There was an increase in the number of gastrostomy/fundoplication procedures that was similar for children with NI (27.1% increase [7,579 in 1997 to 9,638 in 2006]) and children without NI (23.7% increase [6,507 in 1997 to 8,048 in 2006], p = 0.5).
In 2006, the most common reasons for admission in children with NI were for neonatal care (19.1%, n = 66,046), seizures (16.9%, n = 58,253), or other neurologic (13.6%, n = 46,932) or respiratory (11.1%, n = 38,390) problems.
Non-Children's Hospitals
Inpatient resource utilization
Within non-children's hospitals, children with NI accounted for a decreasing proportion of hospitalizations (3.0% in 1997 to 2.5% in 2006, p<0.001]) (Figure 3). Children with NI experienced a decreasing admission trend (22.7% decrease [146,232 in 1997 to 113,097 in 2006]) that was greater than that for children without NI (4.2% decrease [4,678,507 in 1997 to 4,483,695 in 2006], p<0.001). Children with NI accounted for a decreasing proportion of hospital charges (14.2% in 1997 to 13.0% in 2006, p<0.001). They experienced an increase in charges (39.1% increase [US$3.4 billion in 1997 to US$4.7 billion in 2006]) that was less than the increase for children without NI (47.1% increase [US$20.6 billion in 1997 to US$30.3 billion in 2006], p<0.001). There was no significant change in the proportion of bed days attributable to children with NI (8.0% [n = 1.1 million] in 1997 versus 7.7% [n = 1.1 million] in 2006, p = 0.62). Similar patterns were observed in patients with an NI restricted diagnosis.
Reasons for admission
Within non-children's hospitals, there was a greater increase in admissions for infants with NI (8.1% increase [35,544 in 1997 to 38,425 in 2006]) than for infants without NI (3.8% increase [3,272,710 in 1997 to 3,395,539 in 2006], p<0.001). There was a decreasing neurological admissions trend that was greater in children with NI (33.1% decrease [40,968 in 1997 to 27,386 in 2006]) than in children without NI (25.9% decrease [34,957 in 1997 to 25,889 in 2006], p<0.001). There was also a decreasing respiratory admissions trend that was greater in children with NI (50.1% decrease [25,802 in 1997 to 12,882 in 2006]) than in children without NI (24.9% decrease [374,151 in 1997 to 280,729 in 2006], p<0.001).
In 2006, neonatal admissions accounted for 33.9% (n = 38,425) of all NI pediatric admissions, 65.7% (n = 727,465) of NI hospital days, and 62.7% (US$2.9 billion) of NI hospital charges within non-children's hospitals.
Children's Hospitals
Inpatient resource utilization
Throughout the study period, children with NI accounted for an increasing proportion of hospitalizations (11.7% in 1997 to 13.5% in 2006, p<0.001) within children's hospitals (Figure 3). They experienced a greater increase in admissions (16.9% increase [179,324 in 1997 to 209,708 in 2006]) than children without NI (0.2% increase [1,344,608 in 1997 to 1,347,041 in 2006], p<0.001). Children with NI accounted for an increasing proportion of bed days (21.8% in 1997 to 25.0% in 2006, p<0.001). They experienced a greater increase in bed days (22.0% increase [1.7 million in 1997 to 2.1 million in 2006]) than children without NI (4.0% increase [6.1 million in 1997 to 6.3 million in 2006], p<0.001). Children with NI accounted for an increasing proportion of hospital charges (27.1% in 1997 to 29.0% in 2006, p<0.001). They experienced a greater increase in hospital charges (84.2% increase [US$6.5 to $12.0 billion]) than children without NI (67.3% increase [US$17.4 billion to 29.2 billion], p<0.001). Similar patterns were observed in patients with a NI restricted diagnosis (Figure 3).
Reasons for admission
Within children's hospitals, there were opposing trends for neonatal admissions in infants with NI (5.0% increase [21,799 in 1997 to 22,882 in 2006]) and infants without NI (1.5% decrease [560,026 in 1997 to 551,807 in 2006], p<0.001). There was an increasing neurological admissions trend for children with NI (25.2% increase [63,234 in 1997 to 79,232 in 2006]) that was not observed in children without NI (0.0% increase [30,774 in 1997 to 30,630 in 2006], p<0.001). There were opposing trends observed in respiratory admissions for children with NI (1.2% increase [22,686 in 1997 to 22,958 in 2006]) versus for children without NI (6.4% decrease [171,959 in 1997 to 161,026 in 2006], p<0.001). Similar results were observed for children with NI restricted diagnoses.
In 2006, the most common reasons for admission of children with NI within children's hospitals were for seizures (17.8%, n = 37,246), other neurologic problems (20.0%, n = 41,986), respiratory problems (10.9%, n = 22,958), or neonatal care (10.9%, n = 22,883).
Discussion
The main findings from this study suggest that inpatient resource utilization for children with NI in the US has changed from 1997 to 2006. The changes were largely attributable to children with NI utilizing children's hospitals more over time. Within children's hospitals, they accounted for both increasing trends and a substantial proportion of resources over the study period, including nearly one-third of all hospital charges. Within all hospitals, infants and children with NI experienced a greater increase in neonatal and neurological admissions and a greater decrease in respiratory admissions than children without NI. The majority of admissions for children with NI occurred for non-nervous-system problems, suggesting that co-morbid conditions affecting other organ systems were a major contributor to inpatient utilization.
Our study contributes to existing literature by describing national inpatient utilization for children with NI who had underlying primary neurological diagnoses (e.g., cerebral palsy) or other diagnoses that are characteristically associated with co-morbid nervous system impairment (e.g., Down Syndrome). As expected, studies restricted to a cohort of children with primary neuromuscular diagnoses report less inpatient utilization (e.g., 2% of all pediatric admissions and 7% of all pediatric hospital charges) than the present study [27]. Our findings are consistent with adult studies reporting that NI associated with intellectual disabilities and dementia ranks among the top determinants of health care cost [28],[29]. Although the underlying diagnoses and reasons for NI may be different across the age spectrum, patients with NI may account for a substantial share of both pediatric and adult health care resources.
There is a rising proportion of children's hospital use by children with NI, as the total number of hospitalizations for children without NI did not increase within children's hospitals over time. Most US child neurologists work within children's hospitals, and there has been an emergence of multi-disciplinary care coordination clinics that provide comprehensive care for children with NI at children's hospitals [30],[31]. Children with NI may be utilizing children's hospitals more often to seek care from providers who are more familiar with and comfortable managing their health problems. Further study is necessary to evaluate whether clinician NI knowledge and care delivery differ between children's and non-children's hospitals.
US physicians have demonstrated deficiencies in working knowledge of the most common forms of NI, and negative provider attitudes toward this population are associated with substandard acute care practices [32],[33]. Parents of adolescents with NI report this as a contributing factor that complicates the transfer of their child's health care from pediatric to adult providers [34]. In the present study, we observed a trend of rising hospitalizations in adolescent children with NI that was greater than that for children without NI. Further investigation is necessary to determine whether hindered care transition is contributing to this trend.
The rise in the number of admissions associated with gastrostomy with and without fundoplication operations in children with and without NI over time may represent a change in approach to more interventions to bypass oromotor dysfunction, mitigate aspiration from oral feeds, and improve gastroesophageal reflux management in these children. The appropriateness and effectiveness of these operations in children with NI are currently under investigation. It is possible that the decrease in the absolute number of respiratory admissions for children with NI could be related to the rise in gastrostomy and/or fundoplication operations: future studies should investigate whether these operations help prevent pneumonia admissions due to reflux and aspiration [35]. We were unable to evaluate this directly in the present study, as the KID does not track individual patients before and after operations.
In the present study, the absolute number of respiratory admissions decreased for children both with and without NI. Prior small area studies report that children with intellectual disability are at higher risk for respiratory hospitalizations that may be ambulatory care sensitive than children without intellectual disability [36]. Our study suggests that, nationally, children with NI may have received an equivalent or greater benefit from efforts to improve respiratory heath in children, including better respiratory preventive measures and acute and chronic respiratory care treatments [37],[38]. It is possible that some children with NI could have gained exposure to these efforts through improved care coordination within medical homes or other structured clinical programs [31].
The increasing trend of neonatal admissions for infants with NI is supported by prior studies that report a rising incidence of NI associated with increasing preterm infant deliveries and preterm infant survival [1]. However, some recent studies show that the neonatal prevalence of certain NI-related diagnoses, such as cerebral palsy, is now decreasing [39]. This may be related to perinatal care improvements that minimize the risk of brain injury, as well as to changing practices associated with prenatal congenital malformation screening and elective termination [40]. Using inpatient administrative billing codes to detect NI among neonates limits the interpretation of the trends observed in the present study. Some infants may not be diagnosed with NI until well after their neonatal hospitalization.
Our study has several other limitations. We were unable to determine whether the trends could have been a function of the changing population prevalence of children with NI at large in the US. US census data indicate that the population of all children aged 0–18 y increased by 5.6% from 1997 to 2006. However, to our knowledge, true population prevalence trends of all children with NI remain unknown.
The large shift in the inclusion of hospitals from different states in the KID sampling frame could have affected the study findings. In a post hoc analysis, we restricted the cohort to patients admitted to hospitals that were present in both the 1997 and 2006 KID samples. Similar results were observed. The KID contains hospital discharge rather than individual patient data, which prevented us from being able to determine whether the same sized population of children with NI was being hospitalized more frequently over time. This will be important to evaluate in future health resource utilization and epidemiologic studies of children with NI.
Continuous years of data may be preferable for studying hospital utilization trends when compared with four discrete time points in a 10-y period. The hospitals within the KID used ICD-9-CM coding for all the years of the study. It will be important to evaluate the identification of NI diseases using ICD-10 and other coding systems, as many countries are currently using or implementing them. Errors in ICD-9-CM coding exist, and billing reimbursement may influence which codes are entered for a patient during hospitalization. In some cases, NI may be regarded as a subjective medical condition that cannot be correlated with a specific diagnosis code. As such, the hospital resource use described in the present study may underrepresent children with NI who are hospitalized with that situation. The KID contains hospital charge data, but not cost data. Charge data represent the amount that hospitals billed for services but does not reflect how much hospital services actually cost or the specific amounts that hospitals received in payment.
Despite these limitations, this study demonstrates that children with NI account for a substantial proportion of inpatient resources utilized in the US. Their impact is growing within children's hospitals. Use of large administrative databases like the KID, by itself or in conjunction with other databases, may provide unique perspectives to answer the clinical questions raised by the study findings, including the following. (1) Does care quality differ for children with NI depending on the type of hospital they use? (2) Does inpatient resource utilization for children with NI vary depending on their access to medical homes and preventive care? And (3) How does substandard transition of health care services from pediatric to adult health care providers affect hospital use for adolescents and young adults with NI?
As a higher proportion of hospital resources are accounted for by children with NI over time, children's hospitals, in particular, will need to ensure that (1) adequate clinical and coordinated expertise is focused on the needs of these children, (2) NI clinical assessment and care management training is developed for trainees and junior graduates in pediatric postgraduate educational programs, (3) partnerships between families of children with NI and hospitals are developed and implemented, and (4) care treatment strategies of both nervous and non-nervous-system problems are rigorously evaluated for these children. These system-based efforts have the potential to promote continued quality of care for children with NI. We must ensure that the current health care system is staffed, educated, and equipped to serve, with efficiency and quality, this growing segment of vulnerable children.
Supporting Information
Zdroje
1. ArpinoCCompagnoneEMontanaroMLCacciatoreDDe LucaA 2010 Preterm birth and neurodevelopmental outcome: a review. Childs Nerv Syst 26 1139 1149
2. MeadowWLeeGLinKLantosJ 2004 Changes in mortality for extremely low birth weight infants in the 1990s: implications for treatment decisions and resource use. Pediatrics 113 1223 1229
3. PlioplysAVKasnickaILewisSMollerD 1998 Survival rates among children with severe neurologic disabilities. South Med J 91 161 172
4. TennantPWPearceMSBythellMRankinJ 2010 20-year survival of children born with congenital anomalies: a population-based study. Lancet 375 649 656
5. SullivanPBLambertBRoseMFord-AdamsMJohnsonA 2000 Prevalence and severity of feeding and nutritional problems in children with neurological impairment: Oxford Feeding Study. Dev Med Child Neurol 42 674 680
6. MurphyNSuch-NeibarT 2003 Cerebral palsy diagnosis and management: the state of the art. Curr Probl Pediatr Adolesc Health Care 33 146 169
7. FeudtnerCLevinJESrivastavaRGoodmanDMSlonimAD 2009 How well can hospital readmission be predicted in a cohort of hospitalized children? A retrospective, multicenter study. Pediatrics 123 286 293
8. GhoseR 2003 Complications of a medically complicated child. Ann Intern Med 139 301 302
9. PantilatSZLindenauerPKKatzPPWachterRM 2002 Primary care physician attitudes regarding communication with hospitalists. Dis Mon 48 218 229
10. RoyCLPoonEGKarsonASLadak-MerchantZJohnsonRE 2005 Patient safety concerns arising from test results that return after hospital discharge. Ann Intern Med 143 121 128
11. SacchettiASacchettiCCarraccioCGerardiM 2000 The potential for errors in children with special health care needs. Acad Emerg Med 7 1330 1333
12. BerryJGHallDKuoDCohenAAgrawalR 2011 Characteristics of patients experiencing recurrent readmissions to children's hospitals. JAMA. In press
13. MassinMMMontesantiJGerardPLepageP 2006 Children with chronic conditions in a paediatric emergency department. Acta Paediatr 95 208 213
14. MurphyNAHoffCJorgensenTNorlinCYoungPC 2006 Costs and complications of hospitalizations for children with cerebral palsy. Pediatr Rehabil 9 47 52
15. Centers for Disease Control and Prevention 2004 Economic costs associated with mental retardation, cerebral palsy, hearing loss, and vision impairment—United States, 2003. MMWR Morb Mortal Wkly Rep 53 57 59
16. Agency for Healthcare Research and Quality 2005 Introduction to the HCUP Kids' Inpatient Database (KID) 2003 Rockville (Maryland) Agency for Healthcare Research and Quality
17. Agency for Healthcare Research and Quality 2008 Introduction to the HCUP Kids' Inpatient Database (KID) 2006 Rockville (Maryland) Agency for Healthcare Research and Quality
18. LasserMSLiaoJGBurdRS 2006 National trends in the use of antireflux procedures for children. Pediatrics 118 1828 1835
19. SchneierAJShieldsBJHostetlerSGXiangHSmithGA 2006 Incidence of pediatric traumatic brain injury and associated hospital resource utilization in the United States. Pediatrics 118 483 492
20. SrivastavaRDowneyECFeolaPSamoreMCoburnL 2007 Quality of life of children with neurological impairment who receive a fundoplication for gastroesophageal reflux disease. J Hosp Med 2 165 173
21. HassonFKeeneySMcKennaH 2000 Research guidelines for the Delphi survey technique. J Adv Nurs 32 1008 1015
22. MurphyNAHoffCJorgensenTNorlinCFirthS 2006 A national perspective of surgery in children with cerebral palsy. Pediatr Rehabil 9 293 300
23. WilliamsKAlbermanE 1998 Survival in cerebral palsy: the role of severity and diagnostic labels. Dev Med Child Neurol 40 376 379
24. ChuRHouchensRElixhauserARossD 2007 Using the KIDS' Inpatient Database (KID) to estimate trends Rockville (Maryland) Agency for Healthcare Research and Quality
25. FriedmanM 2009 The inflation calculator [database]. Available: http://www.westegg.com/inflation/. Accessed 12 December 2011
26. JanjuaNNasarALynchJKQureshiAI 2007 Thrombolysis for ischemic stroke in children: data from the nationwide inpatient sample. Stroke 38 1850 1854
27. SimonTDBerryJFeudtnerCStoneBLShengX 2010 Children with complex chronic conditions in inpatient hospital settings in the United States. Pediatrics 126 647 655
28. MeerdingWJBonneuxLPolderJJKoopmanschapMAvan der MaasPJ 1998 Demographic and epidemiological determinants of healthcare costs in Netherlands: cost of illness study. BMJ 317 111 115
29. TaylorDHJrSloanFA 2000 How much do persons with Alzheimer's disease cost Medicare? J Am Geriatr Soc 48 639 646
30. WernerRMPolskyD 2005 Comparing the supply of pediatric subspecialists and child neurologists. J Pediatr 146 20 25
31. BerryJGAgrawalRKuoDZCohenERiskoW 2011 Characteristics of hospitalizations for patients who use a structured clinical care program for children with medical complexity. J Pediatr 159 284 290
32. ParisMJ 1993 Attitudes of medical students and health-care professionals toward people with disabilities. Arch Phys Med Rehabil 74 818 825
33. MartinHLRowellMMReidSMMarksMKReddihoughDS 2005 Cerebral palsy: what do medical students know and believe? J Paediatr Child Health 41 43 47
34. TuffreyCPearceA 2003 Transition from paediatric to adult medical services for young people with chronic neurological problems. J Neurol Neurosurg Psychiatry 74 1011 1013
35. SrivastavaRBerryJGHallMDowneyECO'GormanM 2009 Reflux related hospital admissions after fundoplication in children with neurological impairment: retrospective cohort study. BMJ 339 b4411
36. BaloghRBrownellMOuellette-KuntzHColantonioA 2010 Hospitalisation rates for ambulatory care sensitive conditions for persons with and without an intellectual disability—a population perspective. J Intellect Disabil Res 54 820 832
37. GrijalvaCGNuortiJPArbogastPGMartinSWEdwardsKM 2007 Decline in pneumonia admissions after routine childhood immunisation with pneumococcal conjugate vaccine in the USA: a time-series analysis. Lancet 369 1179 1186
38. PfisterRHGoldsmithJP 2010 Quality improvement in respiratory care: decreasing bronchopulmonary dysplasia. Clin Perinatol 37 273 293
39. RobertsonCMWattMJYasuiY 2007 Changes in the prevalence of cerebral palsy for children born very prematurely within a population-based program over 30 years. JAMA 297 2733 2740
40. PellerAJWestgateMNHolmesLB 2004 Trends in congenital malformations, 1974–1999: effect of prenatal diagnosis and elective termination. Obstet Gynecol 104 957 964
Štítky
Interní lékařství
Článek Trends in Compulsory Licensing of Pharmaceuticals Since the Doha Declaration: A Database AnalysisČlánek Effect of Sanitation on Soil-Transmitted Helminth Infection: Systematic Review and Meta-AnalysisČlánek A New Year at : Maintaining a Focus on the World's Health Priorities and Identifying the Gaps
Článek vyšel v časopisePLOS Medicine
Nejčtenější tento týden
2012 Číslo 1- Berberin: přírodní hypolipidemikum se slibnými výsledky
- Léčba bolesti u seniorů
- Příznivý vliv Armolipidu Plus na hladinu cholesterolu a zánětlivé parametry u pacientů s chronickým subklinickým zánětem
- Červená fermentovaná rýže účinně snižuje hladinu LDL cholesterolu jako vhodná alternativa ke statinové terapii
- Jak postupovat při výběru betablokátoru − doporučení z kardiologické praxe
-
Všechny články tohoto čísla
- What Will It Take to Eliminate Pediatric HIV? Reaching WHO Target Rates of Mother-to-Child HIV Transmission in Zimbabwe: A Model-Based Analysis
- Challenging Medical Ghostwriting in US Courts
- The Inadequate Treatment of Pain: Collateral Damage from the War on Drugs
- A United Nations General Assembly Special Session for Mental, Neurological, and Substance Use Disorders:
- Trends in Compulsory Licensing of Pharmaceuticals Since the Doha Declaration: A Database Analysis
- Monitoring the Introduction of Pneumococcal Conjugate Vaccines into West Africa: Design and Implementation of a Population-Based Surveillance System
- The Role of Health Systems Factors in Facilitating Access to Psychotropic Medicines: A Cross-Sectional Analysis of the WHO-AIMS in 63 Low- and Middle-Income Countries
- Trends in Resource Utilization by Children with Neurological Impairment in the United States Inpatient Health Care System: A Repeat Cross-Sectional Study
- Hitting Hotspots: Spatial Targeting of Malaria for Control and Elimination
- Effect of Sanitation on Soil-Transmitted Helminth Infection: Systematic Review and Meta-Analysis
- Effects of Two Commercial Electronic Prescribing Systems on Prescribing Error Rates in Hospital In-Patients: A Before and After Study
- A New Year at : Maintaining a Focus on the World's Health Priorities and Identifying the Gaps
- Long-Term Survival in a Large Cohort of Patients with Venous Thrombosis: Incidence and Predictors
- Ensemble Modeling of the Likely Public Health Impact of a Pre-Erythrocytic Malaria Vaccine
- Adult Mortality Attributable to Preventable Risk Factors for Non-Communicable Diseases and Injuries in Japan: A Comparative Risk Assessment
- PLOS Medicine
- Archiv čísel
- Aktuální číslo
- Informace o časopisu
Nejčtenější v tomto čísle- Ensemble Modeling of the Likely Public Health Impact of a Pre-Erythrocytic Malaria Vaccine
- Adult Mortality Attributable to Preventable Risk Factors for Non-Communicable Diseases and Injuries in Japan: A Comparative Risk Assessment
- What Will It Take to Eliminate Pediatric HIV? Reaching WHO Target Rates of Mother-to-Child HIV Transmission in Zimbabwe: A Model-Based Analysis
- Challenging Medical Ghostwriting in US Courts
Kurzy
Zvyšte si kvalifikaci online z pohodlí domova
Současné možnosti léčby obezity
nový kurzAutoři: MUDr. Martin Hrubý
Všechny kurzyPřihlášení#ADS_BOTTOM_SCRIPTS#Zapomenuté hesloZadejte e-mailovou adresu, se kterou jste vytvářel(a) účet, budou Vám na ni zaslány informace k nastavení nového hesla.
- Vzdělávání



