-
Články
Top novinky
Reklama- Vzdělávání
- Časopisy
Top články
Nové číslo
- Témata
Top novinky
Reklama- Videa
- Podcasty
Nové podcasty
Reklama- Kariéra
Doporučené pozice
Reklama- Praxe
Top novinky
ReklamaRotating Night Shift Work and Risk of Type 2 Diabetes: Two Prospective Cohort Studies in Women
Background:
Rotating night shift work disrupts circadian rhythms and has been associated with obesity, metabolic syndrome, and glucose dysregulation. However, its association with type 2 diabetes remains unclear. Therefore, we aimed to evaluate this association in two cohorts of US women.Methods and Findings:
We followed 69,269 women aged 42–67 in Nurses' Health Study I (NHS I, 1988–2008), and 107,915 women aged 25–42 in NHS II (1989–2007) without diabetes, cardiovascular disease, and cancer at baseline. Participants were asked how long they had worked rotating night shifts (defined as at least three nights/month in addition to days and evenings in that month) at baseline. This information was updated every 2–4 years in NHS II. Self-reported type 2 diabetes was confirmed by a validated supplementary questionnaire. We documented 6,165 (NHS I) and 3,961 (NHS II) incident type 2 diabetes cases during the 18–20 years of follow-up. In the Cox proportional models adjusted for diabetes risk factors, duration of shift work was monotonically associated with an increased risk of type 2 diabetes in both cohorts. Compared with women who reported no shift work, the pooled hazard ratios (95% confidence intervals) for participants with 1–2, 3–9, 10–19, and ≥20 years of shift work were 1.05 (1.00–1.11), 1.20 (1.14–1.26), 1.40 (1.30–1.51), and 1.58 (1.43–1.74, p-value for trend <0.001), respectively. Further adjustment for updated body mass index attenuated the association, and the pooled hazard ratios were 1.03 (0.98–1.08), 1.06 (1.01–1.11), 1.10 (1.02–1.18), and 1.24 (1.13–1.37, p-value for trend <0.001).Conclusions:
Our results suggest that an extended period of rotating night shift work is associated with a modestly increased risk of type 2 diabetes in women, which appears to be partly mediated through body weight. Proper screening and intervention strategies in rotating night shift workers are needed for prevention of diabetes.
: Please see later in the article for the Editors' Summary
Published in the journal: . PLoS Med 8(12): e32767. doi:10.1371/journal.pmed.1001141
Category: Research Article
doi: https://doi.org/10.1371/journal.pmed.1001141Summary
Background:
Rotating night shift work disrupts circadian rhythms and has been associated with obesity, metabolic syndrome, and glucose dysregulation. However, its association with type 2 diabetes remains unclear. Therefore, we aimed to evaluate this association in two cohorts of US women.Methods and Findings:
We followed 69,269 women aged 42–67 in Nurses' Health Study I (NHS I, 1988–2008), and 107,915 women aged 25–42 in NHS II (1989–2007) without diabetes, cardiovascular disease, and cancer at baseline. Participants were asked how long they had worked rotating night shifts (defined as at least three nights/month in addition to days and evenings in that month) at baseline. This information was updated every 2–4 years in NHS II. Self-reported type 2 diabetes was confirmed by a validated supplementary questionnaire. We documented 6,165 (NHS I) and 3,961 (NHS II) incident type 2 diabetes cases during the 18–20 years of follow-up. In the Cox proportional models adjusted for diabetes risk factors, duration of shift work was monotonically associated with an increased risk of type 2 diabetes in both cohorts. Compared with women who reported no shift work, the pooled hazard ratios (95% confidence intervals) for participants with 1–2, 3–9, 10–19, and ≥20 years of shift work were 1.05 (1.00–1.11), 1.20 (1.14–1.26), 1.40 (1.30–1.51), and 1.58 (1.43–1.74, p-value for trend <0.001), respectively. Further adjustment for updated body mass index attenuated the association, and the pooled hazard ratios were 1.03 (0.98–1.08), 1.06 (1.01–1.11), 1.10 (1.02–1.18), and 1.24 (1.13–1.37, p-value for trend <0.001).Conclusions:
Our results suggest that an extended period of rotating night shift work is associated with a modestly increased risk of type 2 diabetes in women, which appears to be partly mediated through body weight. Proper screening and intervention strategies in rotating night shift workers are needed for prevention of diabetes.
: Please see later in the article for the Editors' SummaryIntroduction
Rotating night shift work is common and is becoming increasingly prevalent in industrialized nations [1]. Several studies have suggested that rotating night shift work is associated with an increased risk of obesity [2] and metabolic syndrome [3],[4], conditions closely related to type 2 diabetes. However, few studies have investigated the association between rotating night shift work and type 2 diabetes. Mikuni et al. [5] reported a higher prevalence of diabetes among rotating night shift workers in a male Japanese population. Several cohort studies reported an increased risk of impaired glucose metabolism [3],[6], and two prospective studies in male Japanese workers have revealed that alternation/shift worker had an increased risk of impaired glucose metabolism and diabetes compared with day workers [7],[8]. However, information on the duration of rotating night shift work was not available in these studies, the sample sizes were relatively small, and the study population was limited to Japanese males.
Therefore, we prospectively examined the relationship between duration of rotating night shift work and risk of incident type 2 diabetes in two large cohorts of women in the United States: the Nurses' Health Study (NHS) I and NHS II, with 18–20 y of follow-up. In a secondary analysis, we examined whether duration of shift work was associated with greater weight gain.
Methods
Ethics Statement
The study protocol was approved by the institutional review boards of Brigham and Women's Hospital and Harvard School of Public Health (Boston, Massachusetts, United States).
Study Population
We used data from two prospective cohort studies: NHS I (established in 1976, n = 121,704) [9], and NHS II (established in 1989, n = 116,677) [10]. In both cohorts, questionnaires were administered at baseline and biennially thereafter, to collect and update information on lifestyle practice and occurrence of chronic diseases. The follow-up rates in these cohorts have both exceeded 90%. Women who answered the 1988 questionnaire in NHS I (n = 86,672, age range 42–67 y) and 1989 questionnaire in NHS II (n = 116,677, age range 25–42 y) served as the baseline population for our analyses, because the information of rotating night shift work was first available in these years. Participants were excluded if they had diabetes, heart diseases, stroke, or cancer at baseline (n = 14,766 in NHS I, and n = 7,222 in NHS II), missing information on diabetes diagnosis date (n = 1,452 in NHS I, and n = 749 in NHS II), or age (n = 234 in NHS II), or shift work measures (n = 1,185 in NHS I, and n = 557 in NHS II). Finally, 69,269 women in NHS I and 107,915 women in NHS II were included in our analyses.
Ascertainment of Rotating Night Shift Work
In NHS I, participants were asked at a single time point in 1988 how many years in total they had worked rotating night shifts (defined as at least three nights/month in addition to days and evenings in that month), with eight prespecified response categories: never, 1–2, 3–5, 6–9, 10–14, 15–19, 20–29, and ≥30 y. In NHS II, participants were asked the same question in 1989, with seven prespecified response categories: never, 1–2, 3–5, 6–9, 10–14, 15–19, and ≥20 y. The information was updated in 1991, 1993, 1997, 2001, and 2005 in NHS II. The 1991, 1993, and 1997 questionnaires collected information about the total number of months during which the nurse had worked rotating night shifts in the past 2 y with prespecified response categories: none, 1–4 mo, 5–9, 10–14, 15–19, and ≥20 mo. Additionally, in 2001, gaps were filled by asking for duration of rotating night shifts in 1993–1995, 1995–1997, 1997–1999, and 1999–2001. In 2005, data on the duration of rotating night shifts in 2001–2003 and 2003–2005 were collected. We assigned and added together midpoint values in years (or months) and calculated the total years of rotating night shifts for the women. In the final analysis, the participants were classified into five categories: never, 1–2, 3–9, 10–19, and ≥20 y of rotating night shift work.
Ascertainment of Incident Type 2 Diabetes
In both cohorts, a supplementary questionnaire regarding symptoms, diagnostic tests, and hypoglycemic therapy was mailed to participants who reported a diagnosis of diabetes. A case of type 2 diabetes was considered confirmed if at least one of the following was reported on the supplementary questionnaire according to the National Diabetes Data Group criteria [11]: (1) one or more classic symptoms (excessive thirst, polyuria or frequent urination, weight loss, hunger) plus fasting plasma glucose levels of at least 7.8 mmol/l or random plasma glucose levels of at least 11.1 mmol/l; (2) at least two elevated plasma glucose concentrations on different occasions (fasting levels of at least 7.8 mmol/l, random plasma glucose levels of at least 11.1 mmol/l, and/or concentrations of at least 11.1 mmol/l after ≥2 h shown by oral glucose tolerance testing) in the absence of symptoms; or (3) treatment with hypoglycemic medication (insulin or oral hypoglycemic agent). The diagnostic criteria changed in June 1998, and a fasting plasma glucose of 7.0 mmol/l was considered the threshold for the diagnosis of diabetes instead of 7.8 mmol/l according to the American Diabetes Association criteria [12].
The self-reported type 2 diabetes diagnosis through supplemental questionnaire confirmation has been demonstrated to be highly accurate in a validation study: of 62 type 2 diabetes cases in NHS I who were confirmed by the supplementary questionnaire, 61 (98%) were reconfirmed by medical records [13]. Moreover, in another substudy to assess the prevalence of undiagnosed diabetes in NHS I, fasting plasma glucose and plasma fructosamine were measured in a random sample of participants (n = 200) who did not report a previous diagnosis of diabetes. Only one (0.5%) of the women had an elevated fasting plasma glucose or plasma fructosamine level in the diabetic range, and her levels were barely above the diagnostic cutoffs [14]. By confirming all self-reported cases of diabetes, we exclude false-positive results, and the NHS I results suggest that the false-negative rate is low because most nurses have ready access to medical care, and only cases confirmed by the supplemental questionnaires were included.
Assessment of Covariates
In the biennial follow-up questionnaires, we inquired and updated information on risk factors for chronic diseases, such as body weight, cigarette smoking, physical activity, family history of diabetes, menopausal status, and hormone use. Dietary information (including alcohol) was assessed using a validated semi-quantitative food frequency questionnaire every 4 y starting from 1986 (NHS I) and 1991 (NHS II) [15]. A low-risk diet score was defined as a diet low in trans-fat and glycemic load, while high in cereal fiber and ratio of polyunsaturated to saturated fat. The dietary score is a sum of the quintile values of the four nutrients/components with five representing the lowest-risk quintile in each dietary factor. This method was described in detail elsewhere [10]. Information on daily hours of sleep and snoring frequency was collected in 1986, 2000, and 2002 in NHS I, information about the participants' own education and her husband's education level was inquired in 1992 for NHS I.
Statistical Analysis
Person-years for each participant were calculated from the return date of the baseline questionnaire to the date of diagnosis of type 2 diabetes, death, or the end of the follow-up period (June 30, 2008 for NHS I and June 30, 2007 for NHS II), whichever came first. Time-dependent Cox proportional hazards models were used to estimate the hazard ratios (HRs) of developing type 2 diabetes in rotating night shift workers. The comparison group was women who did not report a history of rotating night shift work. In the multivariate analysis, we adjusted for age (continuous), questionnaire cycle (each 2-y interval), ethnicity (white, nonwhite), family history of diabetes (yes, no), smoking status (never, past, current 1–14/d, 15–24/d, ≥25/d), alcohol intake (0, 0.1–4.9, 5.0–14.9, ≥15 g/d), physical activity (<3, 3–8.9, 9–17.9, 18–26.9, ≥27 MET-h/wk), current aspirin use (yes, no), menopausal status and hormone use (premenopausal, postmenopausal never users, postmenopausal past users, postmenopausal current users), oral contraceptive use (yes, no; NHS II participants only), and quintiles of total energy and dietary score. In additional analyses, we further adjusted for body mass index (BMI; <23, 23–24.9, 25–29.9, 30–34.9, ≥35 kg/m2) to examine the degree to which the association between type 2 diabetes and shift work was mediated by BMI. The above time-varying covariates included in the multivariate analyses were updated every 2 or 4 y, using the most recent data for each 2-y follow-up interval. The last value was carried forward for one 2-y cycle to replace missing values. If the last value was missing, then a missing value indicator was created. In a sensitivity analysis, we adjusted for waist circumference (which was assessed in 1986 for NHS I, and 1993 for NHS II) instead of BMI.
To further explore whether duration of shift work was associated with subsequent weight gain, we conducted a secondary analysis in NHS II because more detailed information was collected on duration of shift work and the participants were young and middle-aged women who were prone to weight gain. In this analysis, women with missing information on body weight were further excluded (n = 252). Obesity status in 2007 and weight gain from 1989 to 2007 were used as the outcomes, and duration of shift work was updated until 2007 and was used as the exposure. We performed logistic regression analyses to estimate the odds ratio of obesity (defined by BMI ≥30 kg/m2) and excessive weight gain (more than 5% of baseline body weight) by duration of shift work category. We used linear regression to estimate the mean BMI or weight-gain difference corresponding to each 5-y increase in shift work, adjusting for aforementioned covariates including baseline BMI.
Proportional hazards assumption was tested with a time-dependent variable by including an interaction term between duration of rotating night shift work and months to events (p>0.05 for all tests). Tests for linear trend were conducted by assigning the median value to each category and modeling this value as a continuous variable. We pooled estimates from the two cohorts using the fixed-effect models because they were similar in terms of population characteristics, study design, and sample size. We also conducted a sensitivity analysis of using random-effects models, and the results were not materially altered. All p-values were two-sided, and data were analyzed with SAS 9.1 (SAS Institute Inc).
Results
Baseline characteristics of the cohorts are reported in Table 1. The mean age at baseline was 53.9 (standard deviation [SD] 7.1) y in NHS I, and 34.3 (SD 4.7) y in NHS II. Of all women in NHS I, 59.0% reported ever having engaged in ≥1 y of rotating night shift work, with 11.3% reporting shift work for ≥10 y. In the younger cohort (NHS II) at baseline (1989), 61.9% reported ever having engaged in ≥1 y of shift work, with only 4.4% reporting shift work for ≥10 y. In 2001, 12 y postbaseline for the NHS II cohort, the mean age was 46.1 (SD, 4.7) y, and the two proportions related to shift work increased to 69.0% and 7.9%, respectively. In both cohorts, women with more years spent in rotating night shift work were older, more likely to have a higher BMI, and to be current smokers. In NHS I, women with more years of rotating night shift work were more likely to be diagnosed with hypertension, to report regular snoring and <6 h sleep. No appreciable differences in dietary factors were observed across durations of shift work.
Tab. 1. Age and age-standardized baseline characteristics of the study population at baseline by category of years spent in rotating night shift work. 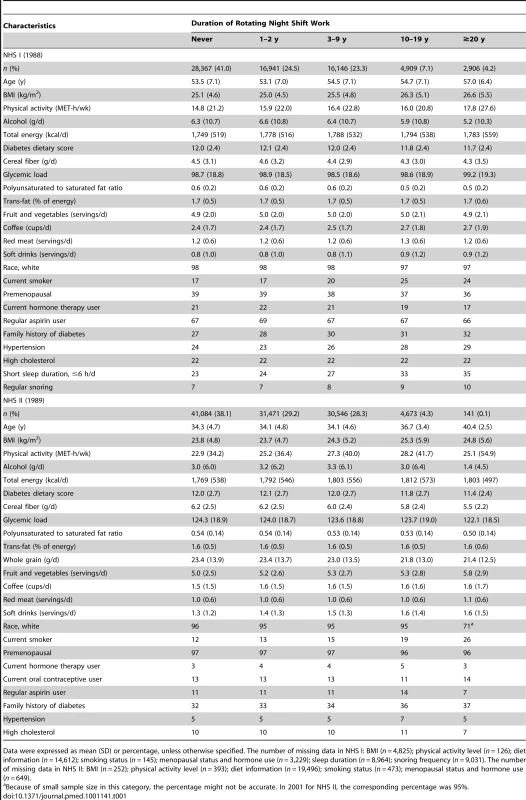
Data were expressed as mean (SD) or percentage, unless otherwise specified. The number of missing data in NHS I: BMI (n = 4,825); physical activity level (n = 126); diet information (n = 14,612); smoking status (n = 145); menopausal status and hormone use (n = 3,229); sleep duration (n = 8,964); snoring frequency (n = 9,031). The number of missing data in NHS II: BMI (n = 252); physical activity level (n = 393); diet information (n = 19,496); smoking status (n = 473); menopausal status and hormone use (n = 649). A total of 6,165 incident type 2 diabetes cases were documented during 1,260,694 person-years in NHS I, and 3,961 cases during 1,865,320 person-years in NHS II. In the age - and questionnaire-cycle–adjusted models, duration of rotating night shift work was monotonically associated with an increased risk of type 2 diabetes in both cohorts (p for trend <0.001) (Table 2). Compared with women who reported no rotating night shift work, the HRs (95% CIs) for participants with 1–2, 3–9, 10–19, and ≥20 y of rotating night shift work were 0.99 (0.93–1.06), 1.17 (1.10–1.25), 1.42 (1.29–1.55), and 1.64 (1.46–1.83) in NHS I, as well as 1.13 (1.04–1.23), 1.34 (1.23–1.45), 1.76 (1.57–1.96), and 2.50 (2.00–3.14) in NHS II, respectively. This association was slightly attenuated after controlling for other covariates except BMI. Additional adjustment for updated BMI further attenuated the association, although it was still monotonic and significant, and the corresponding HRs (95% CI) were 1.00 (0.94–1.07), 1.06 (0.99–1.13), 1.09 (0.99–1.20), and 1.20 (1.07–1.34) in NHS I, as well as 1.07 (0.98–1.16), 1.05 (0.97–1.14), 1.10 (1.00–1.25), and 1.44 (1.15–1.80) in NHS II, respectively. The pooled HRs (95% CI) were 1.03 (0.98–1.08), 1.06 (1.01–1.11), 1.10 (1.02–1.18), and 1.24 (1.13–1.37, p for trend <0.001).
Tab. 2. Hazard ratio of type 2 diabetes by years of working rotating night shifts. 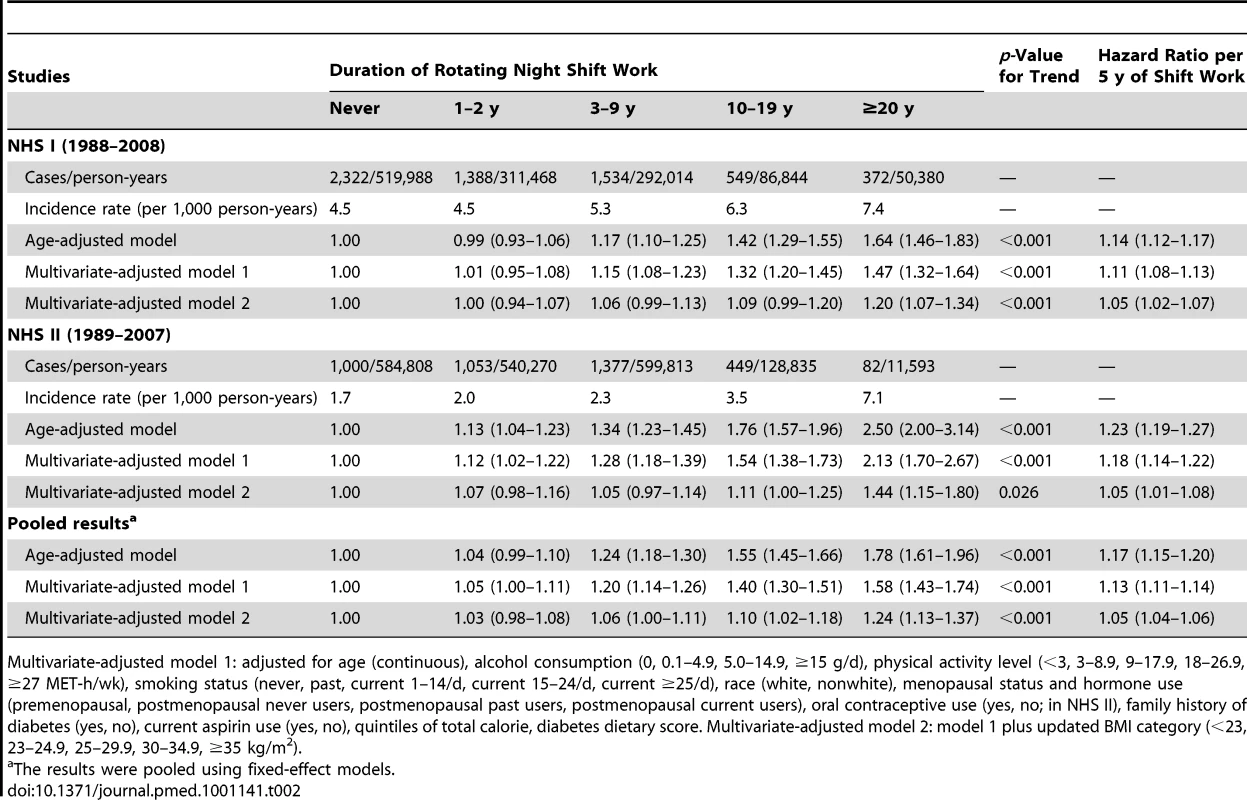
Multivariate-adjusted model 1: adjusted for age (continuous), alcohol consumption (0, 0.1–4.9, 5.0–14.9, ≥15 g/d), physical activity level (<3, 3–8.9, 9–17.9, 18–26.9, ≥27 MET-h/wk), smoking status (never, past, current 1–14/d, current 15–24/d, current ≥25/d), race (white, nonwhite), menopausal status and hormone use (premenopausal, postmenopausal never users, postmenopausal past users, postmenopausal current users), oral contraceptive use (yes, no; in NHS II), family history of diabetes (yes, no), current aspirin use (yes, no), quintiles of total calorie, diabetes dietary score. Multivariate-adjusted model 2: model 1 plus updated BMI category (<23, 23–24.9, 25–29.9, 30–34.9, ≥35 kg/m2). In NHS I, further adjustment for sleep duration, snoring frequency, and the nurse's own and her husband's education levels did not change the results, and no significant interaction between rotating night shift work and sleep duration was found. In both cohorts, further adjustment for baseline histories of hypertension and hypercholesterolemia did not appreciably change the results, and the pooled HRs (95% CI) were 1.02 (0.97–1.08), 1.05 (0.99–1.10), 1.09 (1.02–1.17), and 1.23 (1.11–1.36). The results were the same in white participants only and no interaction with ethnicity was found. In a sensitivity analysis of adjustment for waist circumference instead of BMI, the HRs (95% CI) were 1.01 (0.95–1.08), 1.13 (1.06–1.20), 1.24 (1.13–1.36), and 1.36 (1.21–1.51) in NHS I, as well as 1.11 (1.02–1.21), 1.23 (1.13–1.33), 1.44 (1.28–1.61), and 1.83 (1.46–2.30) in NHS II, respectively. The results did not appreciably change in sensitivity analyses of adjustment for waist-hip ratio or continuous BMI instead of categorical BMI.
In the model without BMI, every 5-y increase of rotating night shift work was associated with an 11% (95% CI 8%–13%) and 18% (95% CI 14%–22%) elevated risk of type 2 diabetes in NHS I and II, respectively, and this estimate was reduced to 5% (95% CI 2%–7%) and 5% (95% CI 1%–8%) after adjustment for BMI, respectively. No significant interaction between rotating night shift work and baseline BMI was found.
In a secondary analysis conducted in NHS II (n = 107,663), we found that rotating night shift work was associated with an elevated risk of obesity and excessive weight gain during the follow-up period (Figure 1). In the multivariate analysis, each 5-y increase in rotating night shift work was associated with an increase of 0.17 units in BMI (95% CI 0.14–0.19) and an increase of 0.45 kg in weight gain (95% CI 0.38–0.53). In addition, women who started their shift works between 1989 and 2007 were also at a high risk of weight gain: the corresponding increase was 0.39 (95% CI 0.28–0.50) units in BMI and 1.02 (95% CI 0.70–1.33) kg in weight gain for each 5-y increase in rotating night shift work, when we excluded those reporting a history of shift work before 1989.
Fig. 1. Rotating night shift work and risk of obesity and weight gain in Nurses' Health Study II. 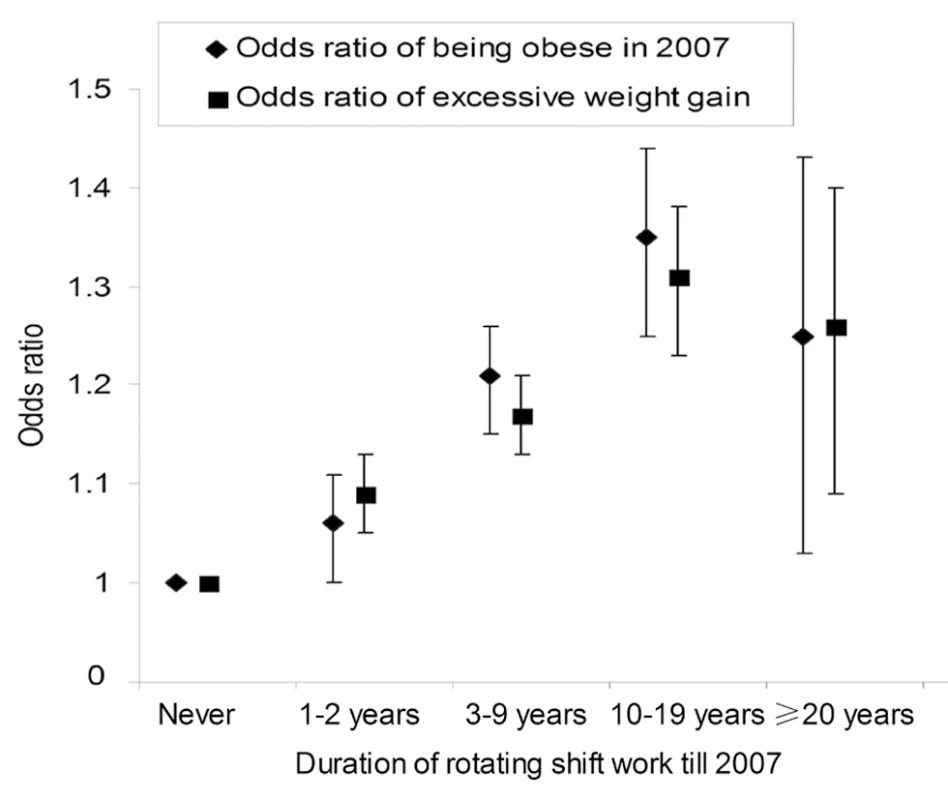
The figure shows the odds ratio (95% CI) of being obese in 2007 and excessive weight gain between 1989 and 2007 by categories of rotating night shift work in Nurses' Health Study II. Excessive weight gain was defined as weight gain between 1989 and 2007 of more than 5% of the baseline body weight in 1989. The model was adjusted for baseline age, BMI, alcohol consumption, physical activity level, smoking status, ethnicity, menopausal status and hormone use, oral contraceptive use, family history of diabetes, current aspirin use, quintiles of total calorie and dietary score in 1989. Discussion
In the two prospective cohort studies with 18–20 y of follow-up, we found that women had a modestly increased risk of type 2 diabetes after extended periods of rotating night shift work. This association appears to be partly mediated through body weight. The NHS I and II cohorts captured different age groups, but the results were fairly consistent across cohorts suggesting that the increased risk of type 2 diabetes was not limited to a particular age group.
Two prospective studies in male Japanese workers revealed that alternation/shift work was an independent risk factor for impaired glucose metabolism and diabetes [7],[8]. These studies, however, did not have information on duration of rotating night shift work. In a previous analysis using NHS II data with 6 y of follow-up (1993–1999), we found that the positive association between years in rotating night shift work and diabetes was entirely mediated by BMI [10]. In that analysis, a history of rotating night shift work ≥10 y was associated with a 64% increased risk of type 2 diabetes in the age-adjusted model. The association disappeared after adjusting for BMI. There were multiple limitations to that analysis including a small sample size (356 total type 2 diabetes cases, 35 cases in women with ≥10 y of shift work), a short follow-up duration (6 y), and few women with longer years of shift work (≥20 y). In our updated analysis, we found that BMI mediated only part of the association, and women with ≥20 y of shift work still had a 44% increased risk of developing type 2 diabetes after adjusting for BMI in NHS II. Our current analysis provides compelling evidence that an extended period of rotating night shift work is associated with a moderately increased risk of type 2 diabetes, which was not completely explained by BMI.
The increased risk of type 2 diabetes associated with rotating night shift work is also consistent with previously reported positive associations of rotating shift work with obesity and/or weight gain [2], metabolic syndrome [3],[4], and cardiovascular disease [16]. There are several potential mechanisms underlying this association. First, a wide range of biological processes are regulated by the circadian rhythms, including sleep-wake cycles, body temperature, energy metabolism, cell cycle, and hormone secretion. Rotating night shift work is generally associated with chronic misalignment between the endogenous circadian timing system and the behavior cycles. This circadian misalignment has been found to result in adverse metabolic and cardiovascular consequences, including a decrease in leptin, an increase in glucose and insulin, an increase in mean arterial blood pressure, and reduced sleep efficiency [17]. Furthermore, the increase in glucose seems to be the result of an exaggerated postprandial glucose response [17].
Second, unfavorable changes in health behaviors (such as increased smoking and irregular meals) related to rotating night shift workers may partly explain the observed association. However, our study and previous studies showed only small differences in nutritional intake and eating patterns between daytime and shift workers [18]–[20], although shifting the time of food intake may influence the postprandial glucose and insulin levels [21],[22], and increase body mass [23]. Nevertheless, the long-term effects of eating habits on health status in rotating night shift workers remain unclear. In our study, women with more years of rotating night shift work were more likely to be current smokers, while no significant difference was found for total energy intake and dietary score between daytime and rotating night shift workers. Third, working in a rotational shift, particularly when it involves night work, may influence both quality and quantity of sleep [24]. Accumulating evidence from prospective studies suggests an increased risk of type 2 diabetes associated with sleep deprivation and sleep disorders [25],[26]. In our analysis, women with more years of rotating night shift work were more likely to sleep ≤6 h per day and snore regularly in NHS I. However, the association between rotating night shift work and type 2 diabetes was not explained by sleep duration and snoring frequency in NHS I. Other factors such as disturbed socio-temporal patterns (resulting from atypical work hours leading to family problems, reduced social support, and stress) and unfavorable changes to biomarkers (e.g., cholesterol and other lipids, plasminogen, blood pressure, and cardiac activity) might also impact the association [16],[27].
The strengths of this study include its prospective design, the large sample size and detailed information on a wide range of potential confounders, and long-term follow-up. To the best of our knowledge, this is the largest cohort study in a female population investigating the association between rotating night shift work and diabetes. We are also aware of several limitations of this study. First, our study populations primarily consisted of white female nurses. The homogeneity of our study participants minimized confounding by socioeconomic status and enhanced the response rate and the quality of the questionnaire data, but the generalizability of our data to other populations, particularly men and other racial or ethnic groups, may be limited. The two above-mentioned studies in Japanese male workers, however, also suggested a positive association between rotating night shift work and diabetes compared with day workers [7],[8]. Second, information on rotating night shift work was self-reported, which may have led to misclassifications of the exposure. However, because of the prospective nature of our study, these misclassifications were more likely to have attenuated our results towards the null.
Third, the underascertainment and misclassification of diabetes outcome are possible because the incident cases were self-reported. However, our validity studies indicated that self-reported diabetes was highly reliable in this group of health professionals. The association could be biased if there was differential detection of diabetes by categories of work schedules. However, when analyses were restricted to symptomatic cases of type 2 diabetes, findings were not materially altered, suggesting that surveillance bias by work schedules was unlikely.
Furthermore, although we controlled for a wide range of covariates including lifestyle factors (e.g., smoking, physical activity, and diet quality), the possibility of unmeasured and residual confounding cannot be fully excluded. Lower socioeconomic status and less healthy lifestyles have been associated with shift work [28]. However, controlling for the participant's own and her husband's education levels and working status in a sensitivity analysis in NHS I did not alter the results. On the other hand, health-related selection could also lead to an underestimate of the association [29],[30]. It is possible that some rotating night shift workers who remained on night shift schedules were healthier than those who worked on daytime schedules or switched back to day routines or withdrew from work for health reasons [29],[30] and thus were less likely to accumulate a longer duration of rotating night shift work. Therefore, the association between duration of rotating night shift work and diabetes may be underestimated if the reference group included some of the women who worked on daytime schedules or withdrew from work for health reasons. Lastly, since our study is observational in nature, causality could not be inferred. Randomized clinical trials may better address the issue of causality, but the study design may not be feasible for this case.
In conclusion, the results from these two large, well-established, long-term cohort studies suggest a positive association between rotating night shift work and diabetes risk. Long duration of shift work was also associated with greater weight gain. Additional studies are needed to confirm our findings in men and other ethnic groups and to further investigate the underlying mechanisms for the association. Because a large proportion of the working population is involved in some kind of permanent night and rotating night shift work, our study has potential public health significance. Recognizing that rotating night shift workers are at a higher risk of type 2 diabetes should prompt additional research into preventive strategies in this group.
Zdroje
1. McMenaminTM 2007 A time to work: recent trends in shift work and flexible schedules. Monthly Labor Review 130 : 3–15. Available: http://www.bls.gov/opub/mlr/2007/12/mlr200712.pdf. Accessed 17 January 2011
2. AntunesLCLevandovskiRDantasGCaumoWHidalgoMP 2010 Obesity and shift work: chronobiological aspects. Nutr Res Rev 23 155 168
3. De BacquerDVan RisseghemMClaysEKittelFDe BackerG 2009 Rotating shift work and the metabolic syndrome: a prospective study. Int J Epidemiol 38 848 854
4. LinYCHsiaoTJChenPC 2009 Persistent rotating shift-work exposure accelerates development of metabolic syndrome among middle-aged female employees: a five-year follow-up. Chronobiol Int 26 740 755
5. MikuniEOhoshiTHayashiKMiyamuraK 1983 Glucose intolerance in an employed population. Tohoku J Exp Med 141 suppl S251 S256
6. SuwazonoYDochiMOishiMTanakaKKobayashiE 2009 Shiftwork and impaired glucose metabolism: a 14-year cohort study on 7104 male workers. Chronobiol Int 26 926 941
7. MorikawaYNakagawaHMiuraKSoyamaYIshizakiM 2005 Shift work and the risk of diabetes mellitus among Japanese male factory workers. Scand J Work Environ Health 31 179 183
8. SuwazonoYSakataKOkuboYHaradaHOishiM 2006 Long-term longitudinal study on the relationship between alternating shift work and the onset of diabetes mellitus in male Japanese workers. J Occup Environ Med 48 455 461
9. HuFBMansonJEStampferMJColditzGLiuS 2001 Diet, lifestyle, and the risk of type 2 diabetes mellitus in women. N Engl J Med 345 790 797
10. KroenkeCHSpiegelmanDMansonJSchernhammerESColditzGA 2007 Work characteristics and incidence of type 2 diabetes in women. Am J Epidemiol 165 175 183
11. National Diabetes Data Group 1979 Classification and diagnosis of diabetes mellitus and other categories of glucose intolerance. Diabetes 28 1039 1057
12. 1997 Report of the Expert Committee on the Diagnosis and Classification of Diabetes Mellitus. Diabetes Care 20 1183 1197
13. MansonJERimmEBStampferMJColditzGAWillettWC 1991 Physical activity and incidence of non-insulin-dependent diabetes mellitus in women. Lancet 338 774 778
14. FieldAECoakleyEHMustASpadanoJLLairdN 2001 Impact of overweight on the risk of developing common chronic diseases during a 10-year period. Arch Intern Med 161 1581 1586
15. FeskanichDRimmEBGiovannucciELColditzGAStampferMJ 1993 Reproducibility and validity of food intake measurements from a semiquantitative food frequency questionnaire. J Am Diet Assoc 93 790 796
16. PuttonenSHarmaMHublinC 2010 Shift work and cardiovascular disease - pathways from circadian stress to morbidity. Scand J Work Environ Health 36 96 108
17. ScheerFAHiltonMFMantzorosCSSheaSA 2009 Adverse metabolic and cardiovascular consequences of circadian misalignment. Proc Natl Acad Sci U S A 106 4453 4458
18. LennernasMHambraeusLAkerstedtT 1995 Shift related dietary intake in day and shift workers. Appetite 25 253 265
19. SudoNOhtsukaR 2001 Nutrient intake among female shift workers in a computer factory in Japan. Int J Food Sci Nutr 52 367 378
20. de AssisMANahasMVBellisleFKupekE 2003 Meals, snacks and food choices in Brazilian shift workers with high energy expenditure. J Hum Nutr Diet 16 283 289
21. LundJArendtJHamptonSMEnglishJMorganLM 2001 Postprandial hormone and metabolic responses amongst shift workers in Antarctica. J Endocrinol 171 557 564
22. KnutssonAKarlssonBOrnklooKLandstromULennernasM 2002 Postprandial responses of glucose, insulin and triglycerides: influence of the timing of meal intake during night work. Nutr Health 16 133 141
23. FonkenLKWorkmanJLWaltonJCWeilZMMorrisJS 2010 Light at night increases body mass by shifting the time of food intake. Proc Natl Acad Sci U S A 107 18664 18669
24. SallinenMKecklundG 2010 Shift work, sleep, and sleepiness - differences between shift schedules and systems. Scand J Work Environ Health 36 121 133
25. AyasNTWhiteDPAl-DelaimyWKMansonJEStampferMJ 2003 A prospective study of self-reported sleep duration and incident diabetes in women. Diabetes Care 26 380 384
26. Al-DelaimyWKMansonJEWillettWCStampferMJHuFB 2002 Snoring as a risk factor for type II diabetes mellitus: a prospective study. Am J Epidemiol 155 387 393
27. HausESmolenskyM 2006 Biological clocks and shift work: circadian dysregulation and potential long-term effects. Cancer Causes Control 17 489 500
28. ScottAJLaDouJ 1990 Shiftwork: effects on sleep and health with recommendations for medical surveillance and screening. Occup Med 5 273 299
29. CarpenterLBeralVFraserPBoothM 1990 Health related selection and death rates in the United Kingdom Atomic Energy Authority workforce. Br J Ind Med 47 248 258
30. CostaG 2003 Shift work and occupational medicine: an overview. Occup Med 53 83 88
Štítky
Interní lékařství
Článek vyšel v časopisePLOS Medicine
Nejčtenější tento týden
2011 Číslo 12- Berberin: přírodní hypolipidemikum se slibnými výsledky
- Léčba bolesti u seniorů
- Příznivý vliv Armolipidu Plus na hladinu cholesterolu a zánětlivé parametry u pacientů s chronickým subklinickým zánětem
- Jak postupovat při výběru betablokátoru − doporučení z kardiologické praxe
- Červená fermentovaná rýže účinně snižuje hladinu LDL cholesterolu jako vhodná alternativa ke statinové terapii
-
Všechny články tohoto čísla
- The Toxic Effects of Cigarette Additives. Philip Morris' Project Mix Reconsidered: An Analysis of Documents Released through Litigation
- The Role of Group Dynamics in Scientific Inconsistencies: A Case Study of a Research Consortium
- Violent Crime, Epilepsy, and Traumatic Brain Injury
- Disclosure of Investigators' Recruitment Performance in Multicenter Clinical Trials: A Further Step for Research Transparency
- Shift Work as a Risk Factor for Future Type 2 Diabetes: Evidence, Mechanisms, Implications, and Future Research Directions
- Estimating the Burden of Malaria: The Need for Improved Surveillance
- Rotating Night Shift Work and Risk of Type 2 Diabetes: Two Prospective Cohort Studies in Women
- Measuring the Population Burden of Injuries—Implications for Global and National Estimates: A Multi-centre Prospective UK Longitudinal Study
- Cognitive Performance in Late Adolescence and the Subsequent Risk of Subdural Hematoma: An Observational Study of a Prospective Nationwide Cohort
- Sex-Specific Immunization for Sexually Transmitted Infections Such as Human Papillomavirus: Insights from Mathematical Models
- A Comprehensive Framework for Human Resources for Health System Development in Fragile and Post-Conflict States
- Absorbable Versus Silk Sutures for Surgical Treatment of Trachomatous Trichiasis in Ethiopia: A Randomised Controlled Trial
- Risk of Violent Crime in Individuals with Epilepsy and Traumatic Brain Injury: A 35-Year Swedish Population Study
- Poor Diet in Shift Workers: A New Occupational Health Hazard?
- The Primacy of Public Health Considerations in Defining Poor Quality Medicines
- Worldwide Incidence of Malaria in 2009: Estimates, Time Trends, and a Critique of Methods
- Surgery Versus Epilation for the Treatment of Minor Trichiasis in Ethiopia: A Randomised Controlled Noninferiority Trial
- PLOS Medicine
- Archiv čísel
- Aktuální číslo
- Informace o časopisu
Nejčtenější v tomto čísle- Violent Crime, Epilepsy, and Traumatic Brain Injury
- Rotating Night Shift Work and Risk of Type 2 Diabetes: Two Prospective Cohort Studies in Women
- Surgery Versus Epilation for the Treatment of Minor Trichiasis in Ethiopia: A Randomised Controlled Noninferiority Trial
- Worldwide Incidence of Malaria in 2009: Estimates, Time Trends, and a Critique of Methods
Kurzy
Zvyšte si kvalifikaci online z pohodlí domova
Současné možnosti léčby obezity
nový kurzAutoři: MUDr. Martin Hrubý
Všechny kurzyPřihlášení#ADS_BOTTOM_SCRIPTS#Zapomenuté hesloZadejte e-mailovou adresu, se kterou jste vytvářel(a) účet, budou Vám na ni zaslány informace k nastavení nového hesla.
- Vzdělávání



