-
Články
Top novinky
Reklama- Vzdělávání
- Časopisy
Top články
Nové číslo
- Témata
Top novinky
Reklama- Videa
- Podcasty
Nové podcasty
Reklama- Kariéra
Doporučené pozice
Reklama- Praxe
Top novinky
ReklamaResponsible Governance for Mental Health Research in Low Resource Countries
article has not abstract
Published in the journal: . PLoS Med 8(11): e32767. doi:10.1371/journal.pmed.1001126
Category: Policy Forum
doi: https://doi.org/10.1371/journal.pmed.1001126Summary
article has not abstract
Summary Points
-
Scaling up mental health services in low - and middle-income countries (LMICs) should be informed by a relevant evidence base to prevent harm and maximize effectiveness.
-
International mental health research agenda prioritization exercises have highlighted priorities among which health system issues have gained more importance, and country-level adaptations of these priorities are needed.
-
Mental health research governance mechanisms need to be improved at the national level in LMICs.
-
It is essential to establish and institutionalize the general orientation of mental health research to deal with problems of organizational structure, research prioritization, insufficient involvement of local stakeholders and service users, relatively limited capacity and resources, and operational challenges.
-
There is a need to balance expensive research with assessment of services and resources using low-cost methods, while building mechanisms to strengthen research capacity and to monitor the research process and outcomes.
Introduction
Between 13% and 49% of the world's population develop neuropsychiatric disorders at some point in their life [1]. More and more evidence indicates that mental disorders and problems are common in all countries studied [2]–[4], and supports earlier projections that the burden of mental health problems is increasing in low - and middle-income countries (LMICs) as well [5]. Most people with these disabling conditions now live in LMICs, but at most one in five receives treatment and care [6]–[8]. In order to narrow this gap, the World Health Organization (WHO) launched the Mental Health GAP Action Programme (mhGAP) [9] with the objective of scaling up services for priority mental disorders using evidence-based interventions. In 2009, evidence profiles were compiled based on a systematic review of the literature for interventions that were to form part of the mhGAP Intervention Guide (mhGAP-IG) [10],[11].
These recent initiatives have once again shown that mental health research resources are sparse and unevenly distributed within LMICs, and that most research and publications originate from just 10% of this group of countries [12],[13]. Lack of good mental health research governance seems to be an important reason for the lack of mental health research from LMICs. In this article, we identify the challenges facing sound research governance in LMICs and provide suggestions regarding how research should be governed in this context, including suggestions for a way forward.
Challenges Facing Good Governance
Lack of an Organizational Structure for National Mental Health Research Governance
As is true for health research in general, the availability and strength of organizational structures that can lead and coordinate mental health research are limited and varied across LMICs. Most of the mental health research in LMICs is restricted to few larger countries (e.g., Argentina, Brazil, China, India, the Republic of Korea, and South Africa), and in three-quarters of mental health research, policy makers were not involved in planning or conducting the research [14]. The presence of mental health professionals in LMICs does not automatically translate to an effective “system” that governs mental health research. Universities in most LMICs do not have a strong link with the health system and psychiatrists do not receive much public health training [15]. Mental health research frequently does not follow health system needs [12].
Confusion around the Priority Research Areas
Due to limited financial and human resources, allocation of assets for mental health research needs to be highly selective. Prioritization exercises in high-income countries do not necessarily apply to resource-poor countries. For example, a report from the United States National Institute of Mental Health in 2001 suggested basic science and developing new interventions were top priorities [16]. In contrast, however, priority-setting exercises in less affluent countries yielded different results. For example, The Lancet's 2007 call for action on global mental health highlighted the need for research on health policy and systems and the scaling up and delivery of evidence-based treatments, while de-emphasizing research on the development of new interventions and technologies, drugs, vaccines, or medicines [17],[18]. Table 1 summarizes findings from global mental health agenda exercises, all of which prioritized health service research. Unfortunately local country-level adaptations of these research priorities were not undertaken as part of these exercises; but these are essential to make such recommendations locally relevant.
Tab. 1. Major global mental health research priority-setting exercises. 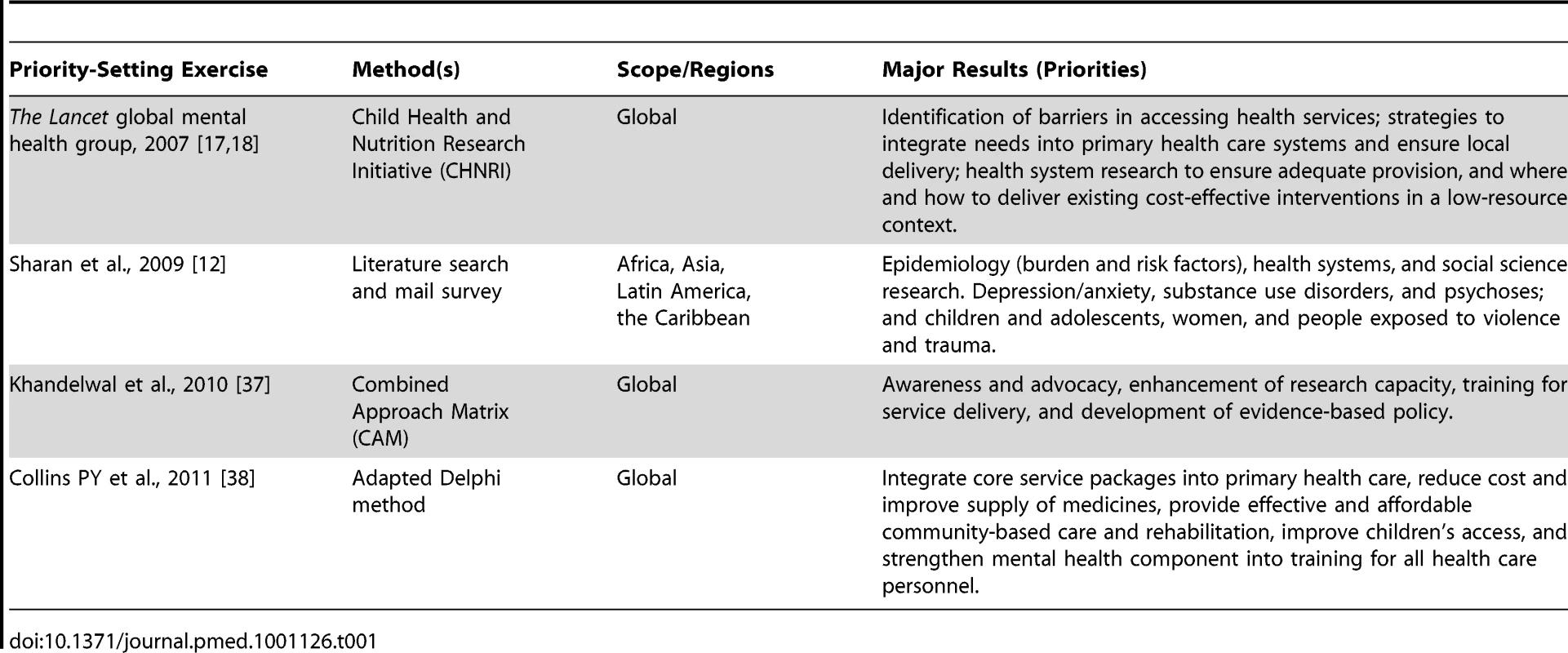
National level priority-setting processes have been characterized as having a relative lack of genuine stakeholder engagement; a wide variation in terms of how priority-setting processes are documented; and an absence of a systematic appeal or feedback process for the identified priorities [19]. A recent exercise involving Peru, Uganda, and Nepal, for example, showed that involvement of grassroots workers can reduce the gap between research relevance and research excellence [20]. Despite the emphasis on health system research in global priority-setting exercises, health system or implementation research is rarely considered a priority. In these countries, biological research or research on new clinical interventions often outweighs research that focuses on delivering effective large-scale interventions within complex health systems that have possibly immediate public health impacts. Also, the issues of poverty and inequity are rarely addressed in research (see also [12]). Due to the fact that local funding for research is often absent, LMIC researchers often need to follow the research agendas of foreign donors rather than local needs.
Research Capacity Constraints
Knowledge, attitude, and skills in the area of mental health research in LMICs needs to be improved [21],[22]. The number of psychiatrists, psychologists, and other behavioral scientists is low, and few have the time and capacity to plan, conduct, and disseminate highly competitive research [23]. In addition, involving local stakeholders in research by multilateral organizations is important [24]. A failure to do this can lead to acrimony affecting ownership of research results, inability to sustain long-term development of research policy, and failure to strengthen local research capacity.
There are other practical issues and context-dependent problems that hinder mental health research in LMICs. Low literacy, relatively poorer training in research methodology, inadequate research infrastructure, and a general apathy towards mental health conditions amongst the larger research community are a few examples. Lack of adequate funds and frequent population migration for better living conditions make large trials and cohort studies a challenge.
Some researchers are optimistic that people in LMICs generally have a reasonable understanding of research [25] and have been able to receive informed consent and conduct the research smoothly [26]. Yet, in many LMICs the capacity to prevent and manage research ethics violations is still limited and more needs to be done about research with people with serious mental health conditions in these countries. Problems with informed consent and the need for supported decision-making become more complicated among mental health service users even in higher income countries [27].
Financial Constraints
Shortage of funds is a common constraint for mental health research in LMICs. Mental health research capacity is unequally distributed even within LMICs. Funding for health research is limited and a recent international survey showed that two-thirds of projects had received external funding [13]. The limited available funds in LMICs are often earmarked for communicable diseases and conditions named in the Millennium Development Goals and rarely available for mental health. Despite some advantages for the targeted areas, concern is growing over the impact of such vertical health programs on general health systems (see also [28],[29]). Funding for such projects is often in vertical silos, which tends to be detrimental to planning or developing other research and services. In addition, in the debates regarding funding for communicable versus non-communicable diseases, integrated approaches to research are lost [30]. The recent focus on mental health research available through some large international funding bodies has been predominantly on biological research—such as genomics—that is not a top priority for research in LMICs.
Actions Required for Sound Mental Health Research Governance
Institutional Arrangements
Governance of mental health research at the country level requires a mechanism for guidance and coordination. In cases where there is a center/unit for health research, mental health research should be established as a division or a branch of it. Such institutions need to set up formal institutional arrangements for engagement with experts in the area of mental health. Collaboration between health experts from different fields, including mental health, will lead to development of more effective programs that could have wider public health implications. For example, improving maternal mental health can influence nutrition status in young children [31]. Establishing collaborative research structures is also important to allow inclusion of key research stakeholders, such as academic institutions (with multi-disciplinary approaches), governmental and non-governmental organizations working in different sectors, and people with mental disorders themselves. Key to this is the development of a research culture and the stimulation of partnerships between researchers and policy makers. Researchers should be aware of the needs of the community and gaps in knowledge that prevent adequate policy development and conduct research that helps to answer those issues. Policy makers should also liaise with researchers and inform them about their needs while trying to understand the limitations of research.
This approach seems to be preferable to a situation where mental health research duplicates the mistake of other health research by being restricted within vertical programs. An integrated arrangement provides opportunities for piggy-backing mental health research on general public health research, which not only means more efficient utilization of a larger pool of funds, but also improved access to overall research funds for mental health. A welcome side effect of this approach would be to contribute to the de-stigmatization of mental health in general.
Finally, mental health research bodies need to develop appropriate stewardship, develop a long-term outlook and strategic plan, identify mental health research gaps and priorities, and monitor and coordinate relevant actions. Mechanisms need to be established to arrange for well-monitored international partnerships tailored to local needs. Positive examples of North–South collaboration with equality and efficiency have been reported [23]. Strengthening South–South partnerships, especially for neighboring countries, has also been suggested based on surveys that highlighted the advanced capacity of some middle-income countries [13],[32].
Taking a Wide Range of Measures to fill the Information Gap
The information required for developing good policies and programs that lead to better mental health delivery models can come from alternative sources beyond traditional academic research proposals. In line with WHO's ongoing data collection exercise on mental health systems and resources, we discuss a logical flow of such information collection that contributes to the development of appropriate mental health services at different levels of care—macro, meso, or micro (see Table 2).
Tab. 2. Proposed knowledge collection from health system data collection to research. 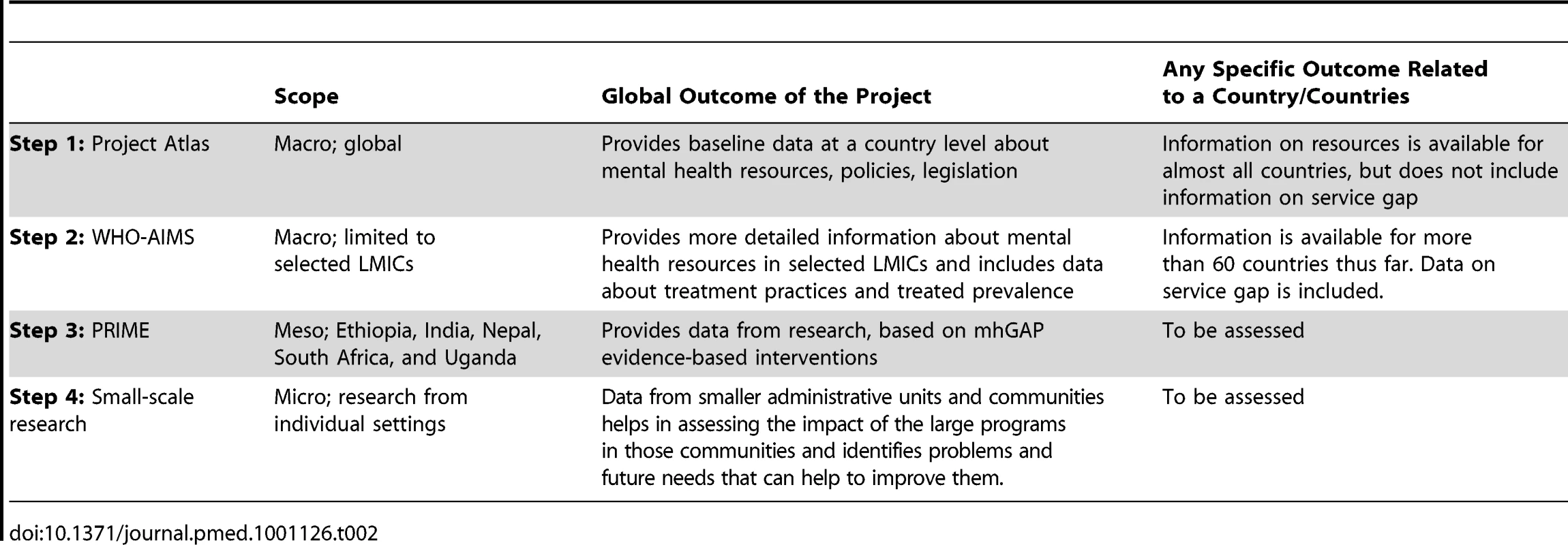
The WHO Mental Health Atlas [33]–[35] and the WHO Assessment Instrument for Mental Health Systems (WHO-AIMS) [23] are two instruments that provide information on mental health systems with very low cost. In 2001, Project Atlas highlighted the gaps in mental health resources across the world for the first time. This laid the stage for the next phase of more in-depth assessment carried out by WHO through the WHO-AIMS project. This study not only corroborated the findings that were obtained earlier through Project Atlas, but also the enormous treatment gap that existed in LMICs that provided such data. Projects such as the WHO Mental Health Atlas and WHO-AIMS are limited by being primarily based on government sources, but they can still provide some indicators to inform action and further research. They also have the scope of being repeated multiple times and thus contribute to the monitoring of progress in services development. Large epidemiological studies help to generate a sound evidence base, but these are expensive and may not give the best value for money in terms of monitoring progress on service delivery. It is in such situations that a stepwise pattern of data gathering carries importance.
A next step is to conduct evaluation studies of health system interventions that aim to scale up a core package of mental health services. Such an initiative has recently begun in the form of the PRogramme for Improving Mental health carE (PRIME) [36], a research consortium led from the University of Cape Town, with trial sites in Ethiopia, India, Nepal, South Africa, and Uganda. This consortium exemplifies the partnership between researchers and policy makers noted above. The final step is to conduct intervention studies (including trials) to evaluate the effectiveness and cost-effectiveness of specific interventions in local settings. It is important to emphasize that these steps are iterative—for example, ongoing local intervention studies can inform the development of policy and services, alongside macro level data collection.
Countries that apply and share such globally employed data collection and mapping instruments not only use the data to inform their national mental health policies and programs, but also contribute to global knowledge that enhances overall improvements in mental health at the global level.
As a complementary step, program evaluation should be added. Such evaluation should include measures of economic and social cost, as well as qualitative information to inform future projects.
Tailoring Programmatic Solutions to Challenges
LMICs have similarities and differences in terms of their mental health research requirements [12],[13]. In Table 3 we have summarized a menu of options for sound governance of mental health research.
Tab. 3. Challenges and proposed arrangements for sound governance of mental health research. 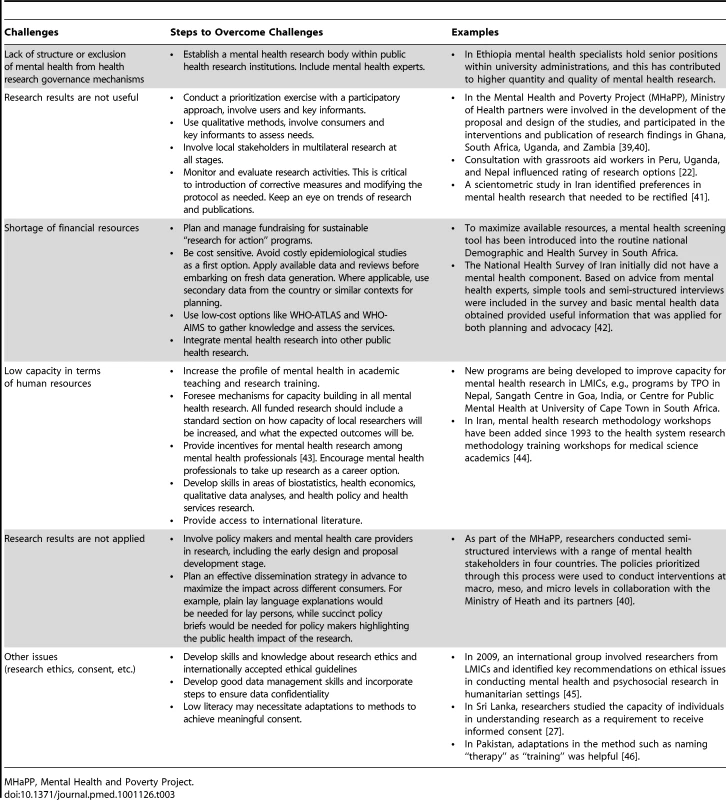
MHaPP, Mental Health and Poverty Project. Conclusion
There is a huge need and a growing demand for mental health services in LMICs. This requires a strong information base generated in the same countries. Locally conducted research would provide more direct evidence for interventions. But the service gap and the information gap go together. Low resource countries face a range of challenges that leads to little or inappropriate research. They need to use their limited financial and human resources for mental health research as effectively as possible. They need sound governance of their mental health research to achieve this, which requires the following:
-
Organizing a structure for mental health research integrated within the available health research institutions;
-
Developing a long-term outlook and strategic plan;
-
Conducting a well-designed prioritization exercise. According to several international priority-setting exercises, mental health system research is the top priority;
-
Raising awareness and developing a culture to understand and facilitate mental health research;
-
Finding locally acceptable solutions for generating the required data such as application of qualitative methods and assessment of mental health systems by using alternative low-cost methods such as WHO-AIMS and the WHO Mental Health Atlas;
-
Setting up routine information systems such as electronic medical systems, disease registries, and treatment outcome databases in LMICs with due consideration of confidentiality issues;
-
Planning and managing fund raising, saving through integration within other health research, and rendering research efficient and sustainable, making the best use of available secondary data and research results from similar context;
-
Capacity building for mental health research, inclusion of a capacity-building plan within any major research project, and information-sharing with policy makers and stakeholders on the benefits and potential utility of research;
-
Establishing quality control, monitoring, and evaluation mechanisms for mental health research, observing ethical issues carefully, and following the trend of mental health research and publications;
-
Planning dissemination from the start, involving policy makers in research governance to ensure knowledge translation; and
-
Searching locally relevant innovative solutions for emerging challenges against mental health research.
This more strategic approach to research governance has the potential to strengthen the planning, execution, dissemination, and use of mental health research in LMICs.
Zdroje
1. [No authors listed] 2000 Cross-national comparisons of the prevalence and correlates of mental disorders. Bull World Health Organ 78 413 425
2. KesslerRCAguilar-GaxiolaSAlonsoJChatterjiSLeeS 2009 The global burden of mental disorders: An update from the WHO World Mental Health (WMH) Surveys. Epidemiol Psichiatr Soc 18 23 33
3. RodriguezJJ 2010 Mental health care systems in Latin America and the Caribbean. Int Rev Psychiatry 22 317 324
4. BorgesGNockMKHaro AbadJMHwangISampsonNA 2010 Twelve-month prevalence of and risk factors for suicide attempts in the World Health Organization World Mental Health Surveys. J Clin Psychiatry 71 1617 1628
5. World Health Organization 2008 The global burden of disease: 2004 update Geneva WHO
6. DemyttenaereKBruffaertsRPosada-VillaJGasquetIKovessV 2004 WHO World Mental Health Survey Consortium. Prevalence, severity and unmet need for treatment of mental disorders in the World Health Organization World Mental Health Surveys. JAMA 291 2581 2590
7. KohnRSaxenaSLevavISaracenoB 2004 The treatment gap in mental health care. Bull World Health Organ 82 858 866
8. WangPSAguilar-GaxiolaSAlonsoJAngermeyerMCBorgesG 2007 Use of mental health services for anxiety, mood, and substance disorders in 17 countries in the WHO world mental health surveys. Lancet 370 841 850
9. World Health Organization 2008 mhGAP: Mental Health Gap Action Programme: scaling up care for mental, neurological and substance use disorders Geneva WHO
10. World health Organization 2010 mhGAP intervention guide for mental, neurological and substance use disorders in non-specialized health settings. Version 1.0 Geneva WHO
11. BarbuiCDuaTvan OmmerenMYasamyMTFleischmannA 2010 Challenges in developing evidence-based recommendations using the GRADE approach: the case of mental, neurological, and substance use disorders. PLoS Med 7 e1000322 doi:10.1371/journal.pmed.1000322
12. SharanPGalloCGurejeOLamberteEMariJJ 2009 Mental health research priorities in low - and middle-income countries of Africa, Asia, Latin America and the Caribbean. Br J Psychiatry 195 354 363
13. RazzoukDSharanPGalloCGurejeOLamberteEE 2010 Scarcity and inequity of mental health research resources in low-and-middle income countries: A global survey. Health Policy 94 211 220
14. SharanPLevavIOlifsonSde FranciscoASaxenaS 2007 Research capacity for mental health in low - and middle-income countries: results of a mapping project Geneva World Health Organization & Global Forum for Health Research
15. SaracenoBvan OmmerenMBatnijiRCohenAGurejeO 2007 Barriers to improvement of mental health services in low-income and middle-income countries. Lancet 370 1164 1174
16. HoagwoodKOlinSS 2002 The NIMH blueprint for change report: research priorities in child and adolescent mental health. J Am Acad Child Adolesc Psychiatry 41 760 767
17. ChisholmDFlisherAJLundCPatelV Lancet Global Mental Health Group 2007 Scale up services for mental disorders: a call for action. Lancet 370 1241 1252
18. TomlinsonMRudanISaxenaSSwartzLTsaiACPatelV 2009 Setting priorities for global mental health research. Bull World Health Organization 87 438 446
19. TomlinsonMChopraMHooseinNRudanI 2011 A review of selected research priority setting processes at national level in low and middle income countries: towards fair and legitimate priority setting. Health Res Policy Syst 9 19
20. TolWAPatelVTomlinsonMBainganaFGalappattiA 2011 Research priorities for mental health and psychosocial support in humanitarian settings. PLoS Med 8 e1001096 doi:10.1371/journal.pmed.1001096
21. SiriwardhanaCSumathipalaASiribaddanaSSamaraweeraSAbeysingheN 2001 Reducing the scarcity in mental health research from low and middle income countries: a success story from Sri Lanka. Int Rev Psychiatry 23 77 83
22. GarnerPMeremikwuMVolminkJXuQSmithH 2004 Putting evidence into practice: how middle and low income countries “get it together”. BMJ 329 1036 1039
23. World Health Organization 2009 Mental health systems in selected low - and middle-income countries: a WHO-AIMS cross-national analysis Geneva WHO
24. LeeKMillsA 2000 Strengthening governance for global health research. BMJ 321 775 776
25. SumathipalaASiribaddanaSHewageSLekamwattageMAthukoraleM 2010 Understanding of Research: a Sri Lankan Perspective. BMC Med Ethics 11 7
26. BoltonPBassJBetancourtTSpeelmanLOnyangoG 2007 Interventions for depression symptoms among adolescent survivors of war and displacement in northern Uganda: a randomized controlled trial. JAMA 298 519 527
27. ChristopherPPFotiMERoy-BujnowskiKAppelbaumPS 2007 Consent form readability and educational levels of potential participants in mental health research. Psychiatr Serv 58 227 232
28. DohertyTChopraMTomlinsonMOliphantNNsibandeD 2010 Moving from vertical to integrated child health: experiences from a multi-country assessment of the Child Health Days approach in Africa. Trop Med Int Health 15 296 305
29. KeugoungBMacqJBuvéAMeliJCrielB 2011 The interface between health systems and vertical programmes in Francophone Africa: the managers' perceptions. Trop Med Int Health 16 478 485
30. De MaeseneerJRobertsRGDemarzoMHeathISewankamboN 2011 Tackling NCDs: a different approach is needed. Lancet E-pub ahead of print 5 September 2011
31. RahmanAMalikASikanderSRobertsCCreedF 2008 Cognitive behaviour therapy-based intervention by community health workers for mothers with depression and their infants in rural Pakistan: a cluster-randomised controlled trial. Lancet 372 902 909
32. RazzoukDGalloCOlifsonSZorzettoRFiestasF 2008 Challenges to reduce the 10/90 gap: mental health research in Latin American and Caribbean countries. Acta Psychiatrica Scandinavica 118 490 498
33. World Health Organization 2001 Atlas: mental health resources in the world Geneva WHO
34. World Health Organization 2005 Mental health atlas Geneva WHO
35. World Health Organization 2011 Mental health atlas Geneva WHO
36. University of Cape Town 2011 Programme for Improving Mental Health carE (PRIME). Available: http://www.health.uct.ac.za/research/groupings/prime/about. Accessed 20 October 2011
37. KhandelwalSAvodéGBainganaFCondeBCruzM 2010 Mental and neurological health research priorities setting in developing countries. Soc Psychiatry Psychiatr Epidemiol 45 487 495
38. CollinsPYPatelVJoestlSSMarchDInselTR 2011 Grand challenges in global mental health. Nature 475 27 30
39. FlisherAJLundCFunkMBandaMBhanaA 2007 Mental health policy development and implementation in four African countries. J Health Psychol 12 505 516
40. LundC 2010 Mental health in Africa: findings from the Mental Health and Poverty Project. Editorial Int Rev Psychiatry 22 547 549
41. SharifiVRahimi-MovagharAMohammadiMRGoodarziRRIzadianES 2008 Analysis of mental health research in the Islamic Republic of Iran over 3 decades: a scientometric study. East Mediterr Health J 14 1060 1069
42. NoorbalaAABagheri YazdiSAYasamyMTMohammadK 2004 Mental health survey of the adult population in Iran. Br J Psychiatry 184 70 73
43. FiestasFGalloCPolettiGBustamanteIAlarcónRD 2009 Improving mental and neurological health research in Latin America: a qualitative study. BMC Public Health 9 344
44. YasamyMTShahmohammadiDBagheri YazdiSALayeghiHBolhariJ 2001 Mental health in the Islamic Republic of Iran: achievements and areas of need. East Mediterr Health J 7 381 391
45. AlldenKJonesLWeissbeckerIWessellsMBoltonP 2009 Mental health and psychosocial support in crisis and conflict: report of the Mental Health Working Group. Prehosp Disaster Med 24 Suppl 2 s217 s227
46. RahmanA 2007 Challenges and opportunities in developing a psychological intervention for perinatal depression in rural Pakistan – a multi-method study. Arch Womens Ment Health 10 211 219
Štítky
Interní lékařství
Článek vyšel v časopisePLOS Medicine
Nejčtenější tento týden
2011 Číslo 11- Berberin: přírodní hypolipidemikum se slibnými výsledky
- Léčba bolesti u seniorů
- Příznivý vliv Armolipidu Plus na hladinu cholesterolu a zánětlivé parametry u pacientů s chronickým subklinickým zánětem
- Červená fermentovaná rýže účinně snižuje hladinu LDL cholesterolu jako vhodná alternativa ke statinové terapii
- Jak postupovat při výběru betablokátoru − doporučení z kardiologické praxe
-
Všechny články tohoto čísla
- Voluntary Medical Male Circumcision: Strategies for Meeting the Human Resource Needs of Scale-Up in Southern and Eastern Africa
- Voluntary Medical Male Circumcision: Translating Research into the Rapid Expansion of Services in Kenya, 2008–2011
- Quality of Maternal Health Care: A Call for Papers for a Maternal Health Task Force–PLoS Collection
- Voluntary Medical Male Circumcision: Matching Demand and Supply with Quality and Efficiency in a High-Volume Campaign in Iringa Region, Tanzania
- Priorities for Research on Equity and Health: Towards an Equity-Focused Health Research Agenda
- What Research Is Needed to Stop TB? Introducing the
- Responsible Governance for Mental Health Research in Low Resource Countries
- Voluntary Medical Male Circumcision: Modeling the Impact and Cost of Expanding Male Circumcision for HIV Prevention in Eastern and Southern Africa
- Effect of Supplementation with Zinc and Other Micronutrients on Malaria in Tanzanian Children: A Randomised Trial
- HIV, Gender, Race, Sexual Orientation, and Sex Work: A Qualitative Study of Intersectional Stigma Experienced by HIV-Positive Women in Ontario, Canada
- Voluntary Medical Male Circumcision: A Framework Analysis of Policy and Program Implementation in Eastern and Southern Africa
- Voluntary Medical Male Circumcision: Logistics, Commodities, and Waste Management Requirements for Scale-Up of Services
- Optimal Uses of Antiretrovirals for Prevention in HIV-1 Serodiscordant Heterosexual Couples in South Africa: A Modelling Study
- Managing the Demand for Global Health Education
- Post-neonatal Mortality, Morbidity, and Developmental Outcome after Ultrasound-Dated Preterm Birth in Rural Malawi: A Community-Based Cohort Study
- Voluntary Medical Male Circumcision: An Introduction to the Cost, Impact, and Challenges of Accelerated Scaling Up
- On the Futility of Screening for Genes That Make You Fat
- Rapid Diagnosis of Tuberculosis with the Xpert MTB/RIF Assay in High Burden Countries: A Cost-Effectiveness Analysis
- Physical Activity Attenuates the Influence of Variants on Obesity Risk: A Meta-Analysis of 218,166 Adults and 19,268 Children
- A Head-to-Head Comparison of Four Artemisinin-Based Combinations for Treating Uncomplicated Malaria in African Children: A Randomized Trial
- Evidence-Based Guidelines for Mental, Neurological, and Substance Use Disorders in Low- and Middle-Income Countries: Summary of WHO Recommendations
- PLOS Medicine
- Archiv čísel
- Aktuální číslo
- Informace o časopisu
Nejčtenější v tomto čísle- Evidence-Based Guidelines for Mental, Neurological, and Substance Use Disorders in Low- and Middle-Income Countries: Summary of WHO Recommendations
- Voluntary Medical Male Circumcision: Strategies for Meeting the Human Resource Needs of Scale-Up in Southern and Eastern Africa
- Rapid Diagnosis of Tuberculosis with the Xpert MTB/RIF Assay in High Burden Countries: A Cost-Effectiveness Analysis
- Physical Activity Attenuates the Influence of Variants on Obesity Risk: A Meta-Analysis of 218,166 Adults and 19,268 Children
Kurzy
Zvyšte si kvalifikaci online z pohodlí domova
Současné možnosti léčby obezity
nový kurzAutoři: MUDr. Martin Hrubý
Všechny kurzyPřihlášení#ADS_BOTTOM_SCRIPTS#Zapomenuté hesloZadejte e-mailovou adresu, se kterou jste vytvářel(a) účet, budou Vám na ni zaslány informace k nastavení nového hesla.
- Vzdělávání



