-
Články
Top novinky
Reklama- Vzdělávání
- Časopisy
Top články
Nové číslo
- Témata
Top novinky
Reklama- Videa
- Podcasty
Nové podcasty
Reklama- Kariéra
Doporučené pozice
Reklama- Praxe
Top novinky
ReklamaSoft Targets: Nurses and the Pharmaceutical Industry
article has not abstract
Published in the journal: . PLoS Med 5(2): e5. doi:10.1371/journal.pmed.0050005
Category: Policy Forum
doi: https://doi.org/10.1371/journal.pmed.0050005Summary
article has not abstract
“Our Special Projects Division produces a wide portfolio of therapy and topic-specific materials…available for sponsorship by companies who wish to promote their products or services, while visibly supporting nurse education,” [1] invites Nursing Standard, the journal of the United Kingdom Royal College of Nursing.
The commercial sponsorship of nursing education exemplified by this advertisement reflects the fact that nurses have increasing power to choose products and services, and to influence choices made by medical and other colleagues [2]. Prescription pharmaceuticals provide a notable example of how nurses have become, as proclaimed above, a desirable target for a powerful industry.
This industry has been robustly critiqued in the medical literature for exploiting patients and doctors using a range of techniques: direct-to-consumer advertising (DTCA) [3–6], sponsored teaching materials [7], advertising in professional media [8,9], research funding [10–14], ghost writing [15,16], gifts, free meals, and travel [7,13,17].
The nursing literature has yet to pay much attention to the expansive reach of the pharmaceutical industry into the nursing profession. In this article, we examine some of the key literature on the influence of drug companies upon nurses, consider the limitations of this literature, and define a strategy for heightening awareness and strengthening the skills of nurses to manage the impact of commercial interests.
Our Literature Search
We searched MedLine (http://www.ncbi.nlm.nih.gov/pubmed/) and CINAHL (http://www.cinahl.com/prodsvcs/cinahldb.htm) databases without date restriction in May 2007, using the terms “pharmaceutical industry,” “drug sales,” “direct-to-consumer,” and “pharmaceutic*,” and restricted to nursing journals. We searched the same terms without the nursing journal restriction, combined with the truncated search terms “nurs*” and prescri*.” A search combining the term “nurs*” with “gift,” a hand search, and references from colleagues completed our research.
We included all articles making reference to nursing's relationship to drug companies and those that included the perspectives of the pharmaceutical industry on this issue. As our intention was to understand the field, we examined all types of articles, from empirical research papers to pure opinion.
We found 32 articles that met our inclusion criteria. Of these, seven were empirical studies (summarised in Table 1), two were theoretical, using anthropological or ethical frameworks to describe the implications of the gift exchange, and 23 were perspectives, commentaries, opinions, and non-systematic (narrative) reviews. There were 16 articles from nursing journals, nine from nurse practitioner journals, two from medical journals, and five from multi-disciplinary journals.
Tab. 1. Summary of Empirical Findings Regarding Pharmaceutical Industry Influence on Nurses 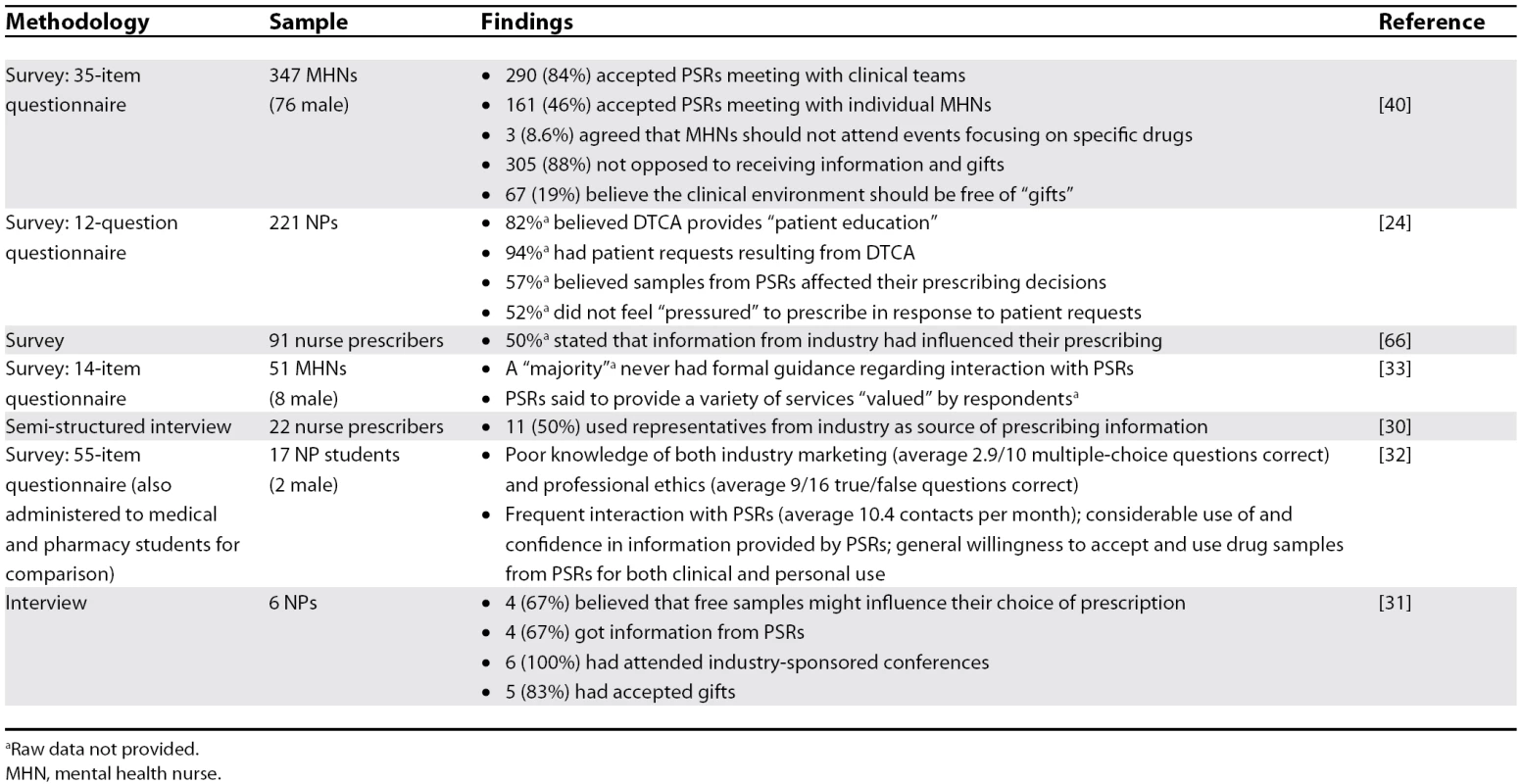
a Raw data not provided. From these 32 articles, we identified and grouped topics and concerns, and positioned them relative to debates in the medical literature about the influence of the pharmaceutical industry upon patient and professional education, gift giving, DTCA, provision of free drug samples, and other determinants of prescribing practice.
Our Findings
Balance of criticism versus support.
Given the vociferous debate in the medical literature, we anticipated positioned papers that would take clear stances for or against the involvement of the pharmaceutical industry in the nursing profession. Such a dichotomy was not evident in the articles we located. Of the 32 articles, 13 expressed or reported serious concerns about the role of the pharmaceutical industry, and four were clearly industry-friendly; these are explored in greater depth in Table 2. The remaining publications either expressed mild concern about the pharmaceutical industry, viewed the support of the industry as generally favourable, or identified both the harms and benefits of the industry's involvement in health care.
Tab. 2. Summary of Article Positions and Competing Interests 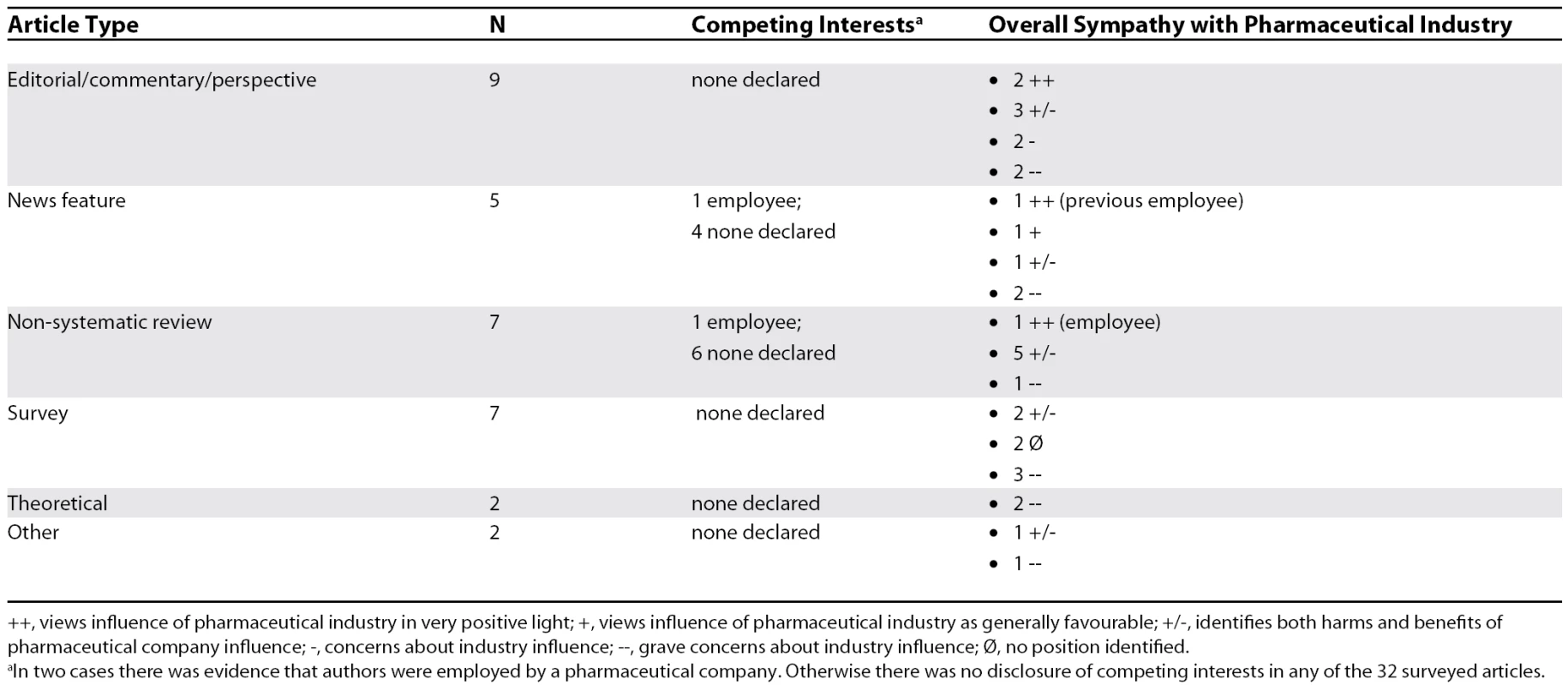
++, views influence of pharmaceutical industry in very positive light; +, views influence of pharmaceutical industry as generally favourable; +/−, identifies both harms and benefits of pharmaceutical company influence; −, concerns about industry influence; −−, grave concerns about industry influence; Ø, no position identified. Direct-to-consumer advertising.
Seven articles address DTCA, three of these providing overviews and identifying consequent problems for patient–clinician communication. The overviews draw upon the medical literature, and lament the scant research available to assess the impact of DTCA on nurses [18–20], but offer limited criticism. One of these overviews focused on presenting a balanced report of the benefits and harms of DTCA, presenting a number of arguments both for and against the practice, but concluding with the view that DTCA might benefit patients by prompting them to seek medical attention, and suggesting that a “balance” is required [19].
An opinion piece, written by health advocate Charles Inlander for a nursing economics journal, praises DTCA as an antidote to medicine's self-interested reluctance to share information [21]. Another, written by employees of the industry, speaks of guarding the line between promotion and education, but not surprisingly concludes that the industry has an important role to play in patient education—one that these authors hope will expand [22]. Three articles encourage health care professionals to work with the pharmaceutical industry to promote accurate patient information, and not to be predisposed against DTCA [20,23,24].
Professional education.
Many of the articles (ten out of 31) draw attention to the substantial role that information from the pharmaceutical industry plays in the education of nurses [22,25–33]. Sponsored professional education, drug samples and information, small gifts, and patient services are portrayed as beneficial, even though caution is advised in their use—unethical behaviour is cast as possible, but exceptional [28,34]. Lynore DeSilets, a nursing educator, recommends robust professional guidelines and accreditation as safeguards [27].
Samples and gifts from, or contacts with, pharmaceutical sales representatives.
Fifteen of the articles consider pharmaceutical sales representatives (PSRs) and/or their provision of drug samples to prescribing nurses. In an advice column to nurse practitioners (NPs), lawyer Cathy Klein acknowledges evidence that provision of samples influences medical prescribing, and increases rather than decreases costs, but also views pharmaceutical representatives as an important source of practical guidance and information for nurses [35]. Bambi Alexander-Banys, in a guest editorial for the Journal of Pediatric Health Care, starts by acknowledging and appreciating the pharmaceutical industry's support of NPs, and then criticises the industry for failing to court NPs or make reference to them in DTCA as they do doctors. This, the author suggests, reinforces traditional perceptions of the latter as the credible provider of patient care, to the detriment of the NP role [36].
In an editorial exchange in The Nurse Practitioner, student family nurse practitioner Sarah Sidiqi argues that NPs may be unwitting victims of the pharmaceutical industry's commercial agenda [37], but receives a sceptical response from the editor, who questions the evidence that NPs have been approached inappropriately in the ways that doctors have, and points out that NPs are generally ignored by the industry [38]. A pilot interview study of six NPs found that all believed pharmaceutical companies influenced their prescribing, with both positive and negative consequences [31]. A survey of 221 oncology NPs found that over half (57%) of respondents viewed the provision of sample drugs as having affected their prescribing choice [24].
Many articles conclude that small gifts from PSRs are acceptable. Jill Davies and Steve Hemingway, both nursing educators, suggest such gifts should not exceed UK£5 (~US$10) [26], while an editor of The Nurse Practitioner, Marilyn Edmunds, as well as clinical nurse specialist Patricia O'Malley, see US$100 as the top range for such gifts [28,39]. Not surprisingly, a “medical writer” with “12 years' experience in pharmaceutical sales training” writing in Advance for Nurse Practitioners refers to promotional objects as a normal part of professional practice and fails to offer any critical consideration of the gift or its consequences [29]. Melodie Young, president of the Dermatology Nurses' Association, mirrors this approach in her article, which promotes PSRs as providing important support for nurses in Dermatology Nursing [34].
Michael Monaghan and colleagues used a cross-sectional survey to determine that NP students (n = 17) had both more positive attitudes towards PSRs and more contact with them than pharmacy students (n = 54) [32]. Similarly, in a large survey of mental health nursing students at two universities in the United Kingdom, 88% (305 out of 347) believed it was acceptable to receive some form of gift from industry [40]. Over half (57%) of the students believed that pharmaceutical representatives did not always give unbiased information, but thought that they and mental health nurses in general would be able to detect any bias. Only 20% believed that the clinical environment should be free of promotional objects. A study of 51 psychiatric nurses reported that an unspecified “majority” had received no guidance about working with the pharmaceutical industry [33].
Three industry-friendly articles [22,29,34], two of which were written by previous or current employees of the pharmaceutical industry [22,29], applaud the role of PSRs, noting their role in education. Whilst the authors' history of working for industry is described, this history is presented as a credential for, rather than risk to, the credibility of their claims. Willis, in an article on career options, recommends the pharmaceutical sales force as a career option for nurses and uncritically equates pharmaceutical sales to promoting solutions to patients [41].
Concern about the pharmaceutical industry.
Thirteen of 31 articles express or report unequivocal concerns about the risks to practice presented by the pharmaceutical industry. Nursing professor Lisa Day's theoretical discussion of gift exchange argues that any gift, however small, places an obligation on recipients, resulting in unwanted debt. Such debt may be repaid by prescribers and those influencing them [42].
A similarly critical view of the industry is apparent in two general news articles reporting current events and describing concerns about drug companies' influences on nurses, voiced by a union leader in the first article, and by a range of nursing, pharmacy, and medical experts speaking to the UK House of Commons about drug company marketing strategies in the second [43,44]. Lecturers in mental health nursing Russell Ashmore and Neil Carver are particularly sceptical about supposed benefits of information provided by industry, and point out that mental health nurses may be particularly vulnerable to pharmaceutical company advertising and “clinical support” [18,40]. Nurse ethicist Nancy Crigger's assessment of pharmaceutical promotion and NP decision making offers a critique of the industry, and argues for guidelines to reduce potential harms, but is diluted by PSR Larry Bennison's counterargument in the same article [45].
Four nonsystematic narrative reviews address nursing education, and how guidelines and professional responsibilities may help to shift nursing education from commercial to professional sources of information [26,39,46,47]. Many of these articles point out the ethical challenges of pharmaceutical gift giving but offer few, if any, solutions. There is a comfortable sense that nurses, once alerted, will not be “caught” by marketing practices, that skills central to the nursing profession inherently provide nurses with the ability to evaluate information effectively [26,46], that ethics committees will give adequate guidance [48], and that guidelines or codes will prevent the problem [47,49]. A strongly worded debate between a sceptical NP and a PSR concludes with vague references to guidelines and raising awareness [45]. Sidiqi's letter to the editor of The Nurse Practitioner is just as strongly worded, but similarly, is quickly deflated by the editor's comments about NPs being unlikely to get “caught” in the same way as doctors [37,38].
Remarkably, none of the articles from the nursing literature reviewed here included author disclosure about possible competing interests. Over the past two decades, medical journals have increasingly required authors to declare competing interests, as these are recognised as potential sources of bias in the collection, analysis, and interpretation of data [50]. As we have seen, nurses are subject to many of the same conflicts of interest as doctors, yet the nursing literature lacks even this most basic means of detecting possible bias.
Discussion
Nursing education fails to prepare graduates to deal with pharmaceutical promotion. From the scant empirical work available, many nurses would appear to accept promotional material uncritically. Nurses, just like doctors, might benefit from understanding marketing and persuasion [51].
Nurses should be encouraged to re-evaluate the educational benefits of promotional information, which is carefully selected, prone to bias, and hardly likely to be as beneficial as many believe [52,53]. Similarly, they should reconsider the presumed educational benefit and lack of bias in DTCA, as these presumptions have now been widely refuted [54–56]. Rather simplistically, many articles about nurses and DTCA have announced that nurses must be “cognizant” or “aware”—suggesting that by knowing the scope of the problem, and by working “with” the industry, nurses will be able to avoid complicity in unethical promotion [19,20,24,34,49].
This optimistic approach belies the fact that many nurses are not trained in critical appraisal, and appear to understand little of the mechanisms by which marketing strategies operate. Numerous studies have found that doctors, regardless of seniority, tend to have poor understanding of marketing, and of their own vulnerability, decision-making processes, and conflicts of interest [57–59]. Nurses are less well-studied in this regard, but are likely to have similar difficulties, exacerbated by their relatively meagre training in pharmacology, statistical inference, and critical appraisal.
Understanding the nursing perspective.
Nursing's relationship to medicine may provide some insight into the lack of critical outcry in the nursing literature regarding pharmaceutical marketing. Direct-to-consumer advertising and the ubiquity of PSRs allow both patients and nurses to circumvent the doctor as source of authoritative knowledge. Information access, however biased, has thus become a source of independence for nurses and patients alike.
The importance of improving nurse–doctor relationships may underlie the prevalent belief among nurses that contact with the pharmaceutical industry is beneficial, opening channels of communication and providing information that enables them to interact with doctors on a more even footing. It seems likely that the ability to seek information from non-medical sources may be perceived by some nurses as a way to escape traditional medical dominance. The perception of DTCA as a means to redress this power imbalance is captured in the commentary of patient advocate Charles Inlander, who in 1991 opined in Nursing Economic$ that DTCA is a tool by which patients could circumvent medical paternalism [21]. Disdain towards medical dominance is also apparent in NP publications, whose authors seem to be indignant that doctors get “courted” by the pharmaceutical industry, while NPs are ignored [36,38].
Both the doctor–patient and the doctor–nurse relationship have evolved in recent years. Ethicists Ezekiel Emanuel and Linda Emanuel have pointed out that the doctor–patient interaction has historically been paternalistic, where the doctor—with superior education and knowledge of human biology—was better positioned than patients to determine their best interest [60]. However, both nurses and patients now have greater access to information outside the clinical encounter, notably including DTCA, PSRs, and the Internet, accelerating changes to these relationships. However, transferring the power imbalance from a paternalistic to a commercial relationship is hardly the last word in liberation. This model purports to transfer autonomy, yet presents information designed to sell, rather than to enable rational treatment choices.
The nursing profession's responsibility.
We propose a three-pronged approach including education, clinical policy, and research to aid nurses with the challenges of pharmaceutical promotion.
Firstly, nurses require training to understand and manage the impact of commercial activity, ideally well before post-graduate training [32]. Nurses already in the work force should receive continuing education on the range of interests promoted in health care, including those motivated by profit.
Little in their training provides nurses with adequate understanding of relevant fields such as pharmacology, epidemiology, public health, evidence-based medicine, critical appraisal, psychology, social science, management, and communications studies, to the extent that would allow them to reliably understand and manage commercial promotion [61]. Educational institutions and licensing authorities should ensure that their students or registrants receive training on the influences of commercialism and have unbiased resources to support prescribing and clinical decisions. Nurses will hopefully come to appreciate the vulnerability they share with doctors to the charms of the PSR.
Secondly, institutional guidelines, policy, and quality assurance should be developed to complement such education. The exclusion of commercial sponsorship from nursing education would leave a gap; careful consideration should be made about how this gap may be filled with information based on best practice and made transparent with respect to its inherent biases.
Policy makers and managers in health care must identify and prevent the intrusion of external interests in clinical decisions. The Stanford University initiative to ban PSRs from its hospitals is an interesting case in point. Whilst on the one hand, it makes bold steps towards curtailing the presence of the pharmaceutical industry in its facilities, on the other, it makes no specific reference to nurses [62]. Such policies should carefully consider the issues of sponsorship and gifts in reference to nurses as well as physicians.
The final prong in our strategy is to gain a better understanding of nurses' role in and influence on prescribing. In the United Kingdom, for example, a drive to nurse prescribing is part of the professionalisation of nursing, and is seen to enhance nursing's status, patient care, and the use of health care resources [63]. This prescribing practice places nurses in an analogous position vis-à-vis the pharmaceutical industry as their medical colleagues.
But it is not only prescribing nurses who must be the focus of these strategies. As we have described above, non-subscribing nurses play an under-appreciated role in prescription and administration choices. One of us (AJ), an experienced staff nurse, recalls guiding new house staff in the choice of treatment; the other (DBM) was grateful for such guidance as a medical intern.
Research is required into the mechanisms by which nurses influence medical prescribing, and the frequency of such influence in various settings. There are a myriad of likely ways in which their influence may be applied, from nurseled clinics where the decision to refer is in the nurse's hands, to drug cabinet stocking, treatment monitoring and assessment, and protocol development. Nurses must identify and acknowledge these roles, and the enormous responsibility they confer, to avoid being a soft target for commercial promotion.
Conclusion
The pharmaceutical industry recognises nursing influence on medical prescribing and identifies nurses as a marketing target. The industry has had its eye on nurses and nurse practitioners for over a decade [64], and is heavily invested in wooing them [65]. Unfortunately, its success in this area has been at the expense of the health budget, evidence-based care, and nursing integrity. All three can and must be reclaimed.
Zdroje
1. Nursing Standard
2007
‘Special projects’ sponsorship.
Available: http://www.nursing-standard.co.uk/advertising/specprods.asp. Accessed 27 December 2007
2. BurnsD
2002
Nurse prescribing. Nurses' influence on GPs' prescribing.
Nurs Times
98
41
42
3. MansfieldPRMintzesBRichardsDToopL
2005
Direct to consumer advertising.
BMJ
330
5
6
4. MansfieldPRMintzesB
2003
Direct-to-consumer advertising is more profitable if it is misleading.
N Z Med J
116
U610
5. MintzesBBarerMLKravitzRLKazanjianABassettK
2002
Influence of direct-to-consumer pharmaceutical advertising and patients' requests on prescribing decisions: two site cross sectional survey.
BMJ
324
278
279
6. HealyD
2006
The latest mania: Selling bipolar disorder.
PLoS Med
3
e185
doi:10.1371/journal.pmed.0030185
7. WazanaA
2000
Physicians and the pharmaceutical industry. Is a gift ever just a gift.
JAMA
283
373
380
8. SmithR
2003
Medical journals and pharmaceutical companies: uneasy bedfellows.
BMJ
326
1202
1205
9. SmithR
2002
Making progress with competing interests—still some way to go.
BMJ
325
1375
1376
10. BakerCJohnsrudMTCrismonMRosenheckRAWoodsSW
2003
Quantitative analysis of sponsorship bias in economic studies of antidepressants.
Br J Psychiatry
183
498
506
11. BoydEABeroLA
2000
Assessing faculty financial relationships with industry: a case study.
JAMA
284
2209
2214
12. LexchinJBeroLADjulbegovicBClarkO
2003
Pharmaceutical industry sponsorship and research outcome and quality: systematic review.
BMJ
326
1167
1176
13. MoncrieffJHopkerSThomasP
2005
Psychiatry and the pharmaceutical industry: who pays the piper.
Psych Bull
29
84
85
14. PerlisRHPerlisCSWuYHwangCJosephM
2005
Industry sponsorship and financial conflict of interest in the reporting of clinical trials in psychiatry.
Am J Psychiatry
162
1957
1960
15. WagerE
2003
How to dance with porcupines: rules and guidelines on doctors' relations with drug companies.
BMJ
326
1196
1198
16. GøtzschePCHróbjartssonAJohansenHKHaahrMTAltmanDG
2007
Ghost authorship in industry-initiated randomised trials.
PLoS Med
4
e19
doi:10.1371/journal.pmed.0040019
17. MenkesDB
2006
Psychiatrist subscribing preferences and attitudes toward promotion.
Inaugural Conference on Disease-Mongering; 11–13 April 2006; Newcastle, Australia
18. AshmoreRCarverN
2001
The pharmaceutical industry and mental health nursing.
Br J Nurs
10
1396
1402
19. MahonS
2006
Impact of direct-to-consumer advertising on healthcare providers and consumers.
Clin J Oncol Nurs
10
417
420
20. VialePH
2003
What nurse practitioners should know about direct-to-consumer advertising of prescription medications.
J Am Acad Nurse Pract
15
297
304
21. InlanderC
1991
A hard pill to swallow. Advertising prescription drugs directly to the consumer.
Nurs Econ
9
343
347
22. GruberWLlewelynJArrasCLionS
1995
The role of the pharmaceutical industry in promoting patient education.
Patient Educ Couns
26
245
249
23. VialePH
2002
Direct-to-consumer advertising of prescription medications: implications for patients with cancer.
Oncol Nurs Forum
29
505
513
24. VialePHYamamotoDS
2004
The attitudes and beliefs of oncology nurse practitioners regarding direct-to-consumer advertising of prescription medications.
Oncol Nurs Forum
31
777
783
25. BowronA
2006
Bridging the information gap in primary care.
Community Pract
79
242
26. DaviesJHemingwayS
2006
Pharmaceutical influences: nurse prescribers: eyes wide open.
Nurse Prescr
1
e42
27. DeSiletsLD
2006
Commercial support for professional development.
J Contin Educ Nurs
37
52
53
28. EdmundsM
2004
Confusing ethical guidelines dampen pharmaceutical support.
Nurse Pract
29
16
29. FlewellMN
2006
Pharmaceutical sales reps: Value beyond samples.
Adv Nurse Pract
14
18
30. HallJCantrillJNoyceP
2003
The information sources used by community nurse prescribers.
Br J Nurs
12
810
818
31. KessenichCRWestbrookMH
1999
Pharmaceutical companies and the prescriptive practices of nurse practitioners.
J Am Acad Nurse Pract
11
533
538
32. MonaghanMSGaltKATurnerPDHoughtonBLRichEC
2003
Student understanding of the relationship between the health professions and the pharmaceutical industry.
Teaching and learning in medicine
15
14
20
33. NolanPCarrNDoranM
2004
Nurse prescribing: The experiences of psychiatric nurses in the United States.
Nurs Stand
18
33
38
34. YoungM
2006
They are more than just pretty people handing out cool pens.
Dermatol Nurs
18
323
324
35. KleinCA
2006
Dispensing pharmaceutical samples: A few reminders.
Nurse Pract
31
15
36. Alexander-BanysB
2002
Pharmaceutical company advertising practices: Call to arms.
J Pediatr Health Care
16
49
50
37. SidiqiSEdmundsM
2003
Pharmaceutical influence.
Nurse Pract
28
6
7
38. EdmundsM
2003
Response to Sidiqi.
Nurse Pract
28
7
39. O'MalleyP
2006
Pharmaceutical advertising and clinical nurse specialist practice.
Clin Nurse Spec
20
13
15
40. AshmoreRCarverNBanksD
2007
Mental health nursing students' relationships with the pharmaceutical industry.
Nurse Educ Today
27
551
560
41. WillisJ
1997
The drug squad.
Nurs Times
93
36
38
42. DayL
2006
Industry gifts to healthcare providers: are the concerns serious.
Am J Crit Care
5
510
513
43. LieferD
1997
Warning over drug courses.
Nurs Stand
11
9
44. KmietowiczZ
2004
Drug company influence extends to nurses, pharmacists and patient groups.
BMJ
329
1206
45. CriggerNJBennisonJW
2006
Unethical marketing or business as usual.
Adv Nurse Pract
15
61
68
46. HemingwayS
2003
Mental health nursing and the pharmaceutical industry.
Ment Health Pract
7
22
23
47. CastledineG
2003
Nurses must be immune to product promotions.
Br J Nurs
12
827
48. StokamerCI
2003
Pharmaceutical gift giving: Analysis of an ethical dilemma.
J Nurs Adm
33
48
51
49. CriggerNJ
2005
Pharmaceutical promotions and conflict of interest in nurse practitioner's decision making: The undiscovered country.
J Am Acad Nurse Pract
17
207
212
50. International Committee of Medical Journal Editors
2007
Uniform requirements for manuscripts submitted to biomedical journals: Writing and editing for biomedical publication.
Available: http://www.icmje.org/index.html. Accessed 27 December 2007
51. MansfieldPRLexchinJWenLSGrandoriLMcCoyCP
2006
Educating health professionals about drug and device promotion: Advocates' recommendations.
PLoS Med
3
e451
doi:10.1371/journal.pmed.0030451
52. MenkesDB
2006
Calling the piper's tune.
Prim Care Clin Psychiatry
11
147
149
53. CardarelliRLicciardoneJCTaylorLG
2006
A cross-sectional evidence-based review of pharmaceutical promotional marketing brochures and their underlying studies: is what they tell us important and true.
BMC Fam Pract
7
13
54. ZieglerMLewPSingerB
1995
The accuracy of drug information from pharmaceutical sales representatives.
JAMA
273
1296
1298
55. CooperRJSchrigerDLWallaceRCMikulichVJWilkesMS
2003
The quantity and quality of scientific graphs in pharmaceutical advertisements.
J Gen Intern Med
18
294
297
56. KaphingstKADeJongW
2004
Market watch: The educational potential of direct-to-consumer prescription drug advertising.
Health Aff
23
143
150
57. MadhavanSAmonkarMMElliotDBurkeKGoreP
1997
The gift relationship between pharmaceutical companies and physicians: an exploratory survey of physicians.
J Clin Pharm Ther
22
207
215
58. SteinmanMShlipakMMcPheeSJ
2001
Of principles and pens; attitudes and practices of medicine house staff toward pharmaceutical industry promotions.
Am J Med
551
557
59. WatkinsRSKimberlyJJr
2004
What residents don't know about physician-pharmaceutical industry interactions.
Acad Med
79
432
437
60. EmanuelEJEmanuelLL
1992
Four models of the physician-patient relationship.
JAMA
267
2221
2226
61. MansfieldPR
2007
Is it insulting to suggest that health professionals are influenced by drug companies.
Available: http://www.healthyskepticism.org/news/2007/May.php. Accessed 27 December 2007
62. Stanford University
2006
Policy and guidelines for interactions between the Stanford University School of Medicine, the Stanford Hospital and Clinics and Lucile Packard Children's Hospital with the pharmaceutical, bioetch, medical device, and hospital and research and supplies industries (“Industry”).
Available: http://med.stanford.edu/coi/siip/documents/siip_policy_aug06. pdf. Accessed 27 December 2007
63. JonesM
2004
Case Report. Nurse prescribing, a case study in policy influence.
Journal of nursing management
12
266
272
64. MittmanDEYackerenTFHendrixPMirotznikHG
1994
Sales reps recognize value of nurse practitioners.
Med Mark Media
29
52
54
65. ArnoldM
2004
The hidden prescribers.
Med Mark Media
39
44
52
66. WhileAEBiggsKS
2004
Benefits and challenges of nurse prescribing.
J Adv Nurs
45
559
567
Štítky
Interní lékařství
Článek vyšel v časopisePLOS Medicine
Nejčtenější tento týden
2008 Číslo 2- Berberin: přírodní hypolipidemikum se slibnými výsledky
- Léčba bolesti u seniorů
- Příznivý vliv Armolipidu Plus na hladinu cholesterolu a zánětlivé parametry u pacientů s chronickým subklinickým zánětem
- Červená fermentovaná rýže účinně snižuje hladinu LDL cholesterolu jako vhodná alternativa ke statinové terapii
- Jak postupovat při výběru betablokátoru − doporučení z kardiologické praxe
-
Všechny články tohoto čísla
- Antiretroviral Therapy for Prevention of HIV Infection: New Clues From an Animal Model
- A Collaborative Epidemiological Investigation into the Criminal Fake Artesunate Trade in South East Asia
- Does Preventing Obesity Lead to Reduced Health-Care Costs?
- Solving the Mystery of Myelodysplasia
- The Evolution of Norovirus, the “Gastric Flu”
- Maternal Death, Autopsy Studies, and Lessons from Pathology
- Soft Targets: Nurses and the Pharmaceutical Industry
- Eliminating Human African Trypanosomiasis: Where Do We Stand and What Comes Next?
- Should Data from Demographic Surveillance Systems Be Made More Widely Available to Researchers?
- New Formulation of Paraquat: A Step Forward but in the Wrong Direction?
- The Neglected Diseases Section in : Moving Beyond Tropical Infections
- PLOS Medicine
- Archiv čísel
- Aktuální číslo
- Informace o časopisu
Nejčtenější v tomto čísle- Eliminating Human African Trypanosomiasis: Where Do We Stand and What Comes Next?
- Solving the Mystery of Myelodysplasia
- The Neglected Diseases Section in : Moving Beyond Tropical Infections
- Should Data from Demographic Surveillance Systems Be Made More Widely Available to Researchers?
Kurzy
Zvyšte si kvalifikaci online z pohodlí domova
Současné možnosti léčby obezity
nový kurzAutoři: MUDr. Martin Hrubý
Všechny kurzyPřihlášení#ADS_BOTTOM_SCRIPTS#Zapomenuté hesloZadejte e-mailovou adresu, se kterou jste vytvářel(a) účet, budou Vám na ni zaslány informace k nastavení nového hesla.
- Vzdělávání



