-
Články
Top novinky
Reklama- Vzdělávání
- Časopisy
Top články
Nové číslo
- Témata
Top novinky
Reklama- Videa
- Podcasty
Nové podcasty
Reklama- Kariéra
Doporučené pozice
Reklama- Praxe
Top novinky
ReklamaThe Health System and Population Health Implications of Large-Scale Diabetes Screening in India: A Microsimulation Model of Alternative Approaches
Sanjay Basu and colleagues estimate the benefits and costs of scaling up survey - or glucometer-based diabetes screening across India’s diverse populations.
Published in the journal: . PLoS Med 12(5): e32767. doi:10.1371/journal.pmed.1001827
Category: Research Article
doi: https://doi.org/10.1371/journal.pmed.1001827Summary
Sanjay Basu and colleagues estimate the benefits and costs of scaling up survey - or glucometer-based diabetes screening across India’s diverse populations.
Introduction
Type 2 diabetes has increased in prevalence at an alarming rate in rapidly developing countries such as India and China [1–4]. Most people with diabetes in these countries are undiagnosed; hence, community-based screening of adults for diabetes has been suggested [5–8]. In India, for example, a recently initiated program has already screened as many as 53 million adults in both urban and rural communities, using either survey-based instruments (i.e., risk-scoring questionnaires) or random (i.e., not necessarily fasting) blood glucose testing [9]. Individuals identified as high risk through these screening strategies are typically referred for fasting blood glucose tests to confirm the diagnosis. The Indian government plans to continue expanding this large-scale screening program in coming years. However, despite its potentially large impact, essentially no data have been collected to track the performance of the screening program [10].
Large-scale screening for diabetes, like population-wide screening for any disease, must fulfill several key criteria: (i) that a reliably sensitive and specific screening instrument is available, (ii) that facilities for diagnosis and treatment are available to those screened in order to initiate early therapy, (iii) that there is an agreed-upon policy on whom to treat among those screened, (iv) that the total cost of finding a case is included in estimating the impact of screening on medical expenditure as a whole, and (v) that beneficial early therapy delivered to those individuals newly diagnosed provides significant health advantages over the status quo [11]. In India, numerous survey-based screening instruments have been constructed to identify persons with a high risk of having undiagnosed diabetes among select sub-national Indian populations [6–8], yet these have not been tested more widely among diverse populations given the absence of large, nationally representative cohorts. The various risk factors incorporated into different instruments vary in prevalence among demographic populations and have very different associations with diabetes prevalence among urban and rural populations (e.g., [12]). Hence, screening instruments developed among some subpopulations may not be optimal for a standardized, national program. Furthermore, it remains unclear how many resources must be devoted to confirmatory testing and subsequent treatment to deliver population health benefits. In high-income countries, additional screening for high-risk, asymptomatic patients has not resulted in a significant reduction in all-cause, cardiovascular, or diabetes-related mortality, or in rates of diabetes-related microvascular complications such as blindness or renal failure [13,14].
We therefore constructed a microsimulation model to determine the implications of using alternative proposed screening instruments to identify persons with a high risk of having undiagnosed type 2 diabetes across diverse populations in India. We compared the three major survey-based screening instruments proposed for use in India [6–8], as well as a random glucometer-based screening approach that has been initiated by some government offices [15], to identify how different populations of people with diabetes in India would be detected through these alternative screening strategies. Both the questionnaire-based screening instruments and random glucometer-based screening are typically implemented through health “camps” that adopt a “come one, come all” strategy, whereby any members of the public can potentially be screened. We estimated rates of true - and false-positive and true - and false-negative screens, the associated need for confirmatory testing, and the implications of therapy among those found through the alternative screening approaches. We then calculated the number needed to screen and treat (NNST) to prevent the incidence of one complication, since this is the ultimate goal of early detection and treatment of type 2 diabetes; understanding the magnitude of benefit in reduction of complication risk is an essential component of WHO screening criteria. We also examined the costs of screening, including programmatic costs. We quantified the degree of sensitivity and uncertainty in all of these calculations, identifying the extent to which information available in currently available datasets could inform policy decisions despite continued uncertainty about type 2 diabetes pathogenesis and prevalence in India.
Methods
Ethics committee approval for the Indian Migration Study (IMS) that was used to inform the model was obtained from the All India Institute of Medical Sciences Ethics Committee, reference number A-60/4/8/2004; for the overall modeling research, ethics committee approval was obtained from the Stanford University Institutional Review Board, reference number eP-28811.
Model Overview
The modeling proceeded in three stages (see Fig 1). Full details of the modeling process, including all input parameters, are provided in S1 Text, in accordance with international model reporting guidelines [16]. Here, we provide an overview of the input data and calculation approach.
Fig. 1. Model diagram. Individuals in the simulated population are assigned demographic characteristics based on the joint probabilities of being in each age, sex, location, and income group given population demographic estimates for India. 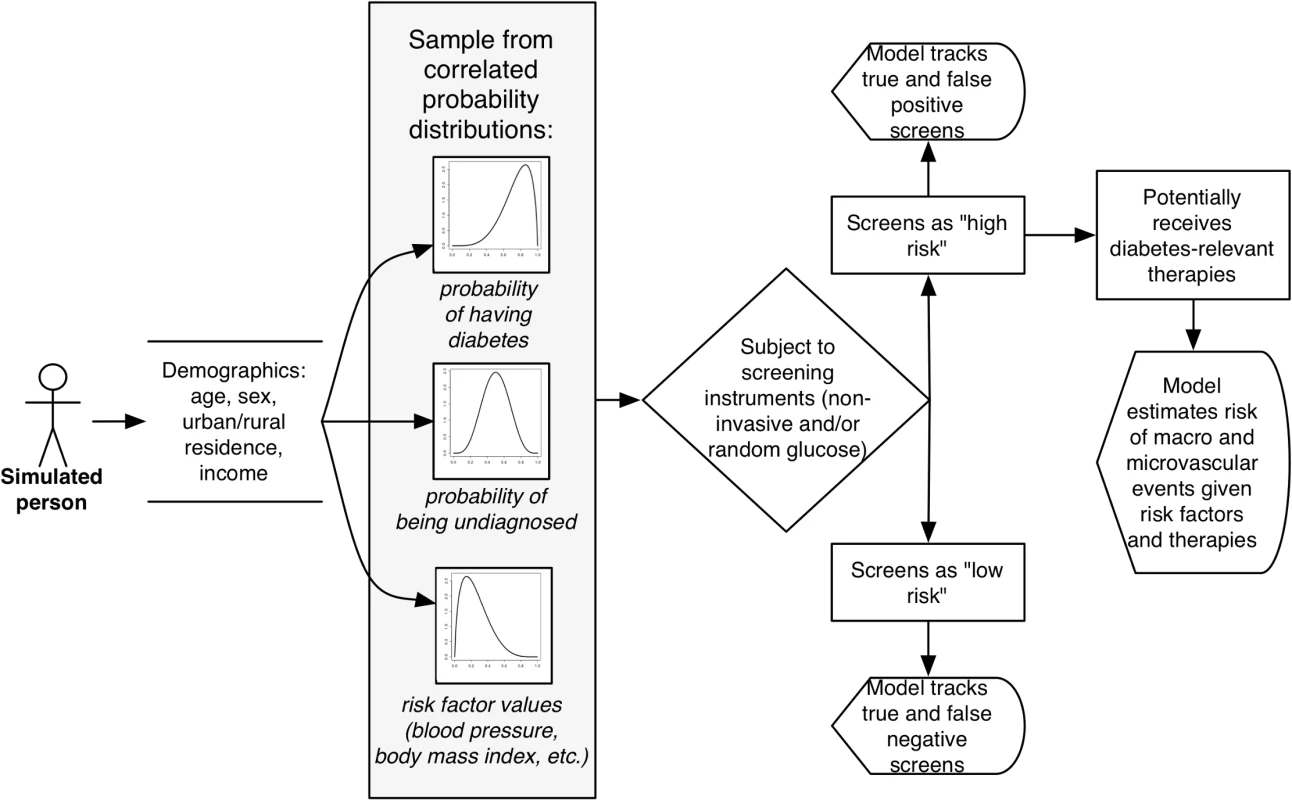
They are then assigned a probability of having diabetes, either diagnosed or undiagnosed, and having various associated co-morbid risk factors, based on the joint probabilities of these prevalence rates and factors listed in S2 Table and illustrated in S1 Fig based on prior population estimates for India. Individuals are then subject to the screening instruments listed in Table 1, from which the model estimates positive and negative test results and subsequent diabetes complications with and without treatment. Tab. 1. Alternative risk factors included in survey-based screening instruments proposed for detecting undiagnosed diabetes in India [6–8]. ![Alternative risk factors included in survey-based screening instruments proposed for detecting undiagnosed diabetes in India [<em class="ref">6</em>–<em class="ref">8</em>].](https://www.prolekarniky.cz/media/cache/resolve/media_object_image_small/media/image/4c5cd5e3eb78f49e84c143ec2f63336e.png)
The model subjects each simulated individual to each of the listed screening instruments to identify how many people would test positive or negative by each instrument. First, we constructed a synthetic, nationally representative Indian population from a series of sub-national cohort studies. We estimated the probability of having diabetes, the probability of being diagnosed, and the correlated distribution between these probabilities and key diabetes risk factors and co-morbidities (see Table 1 and S1 Fig) by age, sex, location, and income, using mixed-effects meta-regression.
Second, we subjected each member of the synthetic population to each of three survey-based screening instruments advocated for the detection of people with undiagnosed diabetes in India (see Table 1) [6–8], implemented as an alternative to or in combination with random glucose testing [15]. We tracked the number of people with previously undiagnosed diabetes who would be detected through screening (true positives) or would be missed (false negatives), and the number of people without diabetes who would be false positives or true negatives upon screening, given the distribution of risk factors among these groups and the different risk factors incorporated into each instrument (Table 1).
Disease Burden
To estimate the burden of diabetes in India, we constructed a synthetic, nationally representative population for our model. We used United Nations estimates of India’s demographics for the year 2015 [17], dividing a simulated population of India into cohorts defined by age (25–44 y old and 45–65 y old—the age groups among whom screening efforts are focused and risk equations for complications have been validated [18,19]), sex, location (urban or rural), and income (tertiles of the standard of living index, the standard metric of wealth in India [20]). The lower-bound age cutoff was chosen based on the extremely small prevalence rates of type 2 diabetes below age 25 y in India, such that screening performance always worsens when including persons below this age; the upper-bound age cutoff was chosen based on the cutoff commonly used in current screening efforts [10] and the absence of clinical trial data for the effects of glycemic control beyond this age [21].
We adopted a microsimulation approach, which means each member of the population was simulated as an individual, and assigned a probability of having diabetes, a probability of being undiagnosed if having diabetes, and a set of risk factor values and co-morbidities (itemized in Table 1) correlated to these two probabilities. The advantage of this technique over older Markov modeling approaches is that microsimulation can capture complex individual screening experiences and co-morbid disease histories, providing an estimate of heterogeneous effects in a population as opposed to a simple population average among a given cohort. To assign individuals a diabetes disease status, determine whether they were likely to have been diagnosed if they had diabetes, and provide them with associated risk factor values, we performed Monte Carlo sampling from joint probability distributions of each of these probabilities and risk factors specific to their age, sex, income, and location group, estimated from a meta-regression on 58 cohort studies of diabetes published in India (n = 447,481; S1 Table). The cohort studies describe the prevalence of previously diagnosed diabetes (via self-report), the prevalence of previously undiagnosed diabetes (established through testing of the cohort populations per WHO diagnostic criteria [22,23]), and the correlated frequency of the risk factors and co-morbid conditions listed in Table 1. The overall probability distributions for diabetes disease, diabetes diagnosis, and associated risk factors were estimated through mixed-effects meta-regression accounting for changes in both disease prevalence and the probability of diagnosis over time. This is a method to infer a population metric from a group of studies rather than a single cohort, accounting for variations in sampling among studies. Specifically, the model applied to the total diabetes prevalence, the probability of being previously undiagnosed, and the risk factor value/co-morbidity prevalence observations y among the j studies was specified as [24]
where x1i denotes the value of the first moderator variable (e.g., percent of population in the first age category, 25–44 y old) in the ith study, and so on through all moderator classes of age, sex, income, and location, and uj and εj are error terms referring to the amount of variability in the true value of the outcome that is not accounted for by the moderators included in the model and sample variances. The model was fitted with weights using a standard “inverse-variance” method, with Monte Carlo sampling of estimates specific to the age, sex, income, and location groups drawn from the probability distributions of the β coefficients in the fitted model. Model details and outputs are provided in S1 Text and S2 Table. To assess the face validity of our estimates, we compared them against three independent estimates from the Global Burden of Metabolic Risk Factors of Chronic Diseases Collaborating Group [25], the WHO Study on Global Ageing and Adult Health [26], and the International Diabetes Federation Diabetes Atlas [4].Screening Simulations
By applying each of the three screening instruments shown in Table 1 to the synthetic population, we estimated how each screening instrument would perform in terms of sensitivity, specificity, positive predictive value, and negative predictive value. We then calculated the number needed to screen (NNS) to detect one previously undiagnosed diabetes case, and computed the overall number of persons deemed high risk, who would be referred for confirmatory testing in both urban and rural locations, thereby providing an estimate of the burden of screening on the healthcare system. Note that waist circumference is commonly used in the screening instruments, given its superior performance compared to BMI in predicting type 2 diabetes risk among South Asians [27–29]; however, BMI is included in one screening instrument, adopting a lower cut point than the international obesity cut point, given that diabetes risk in South Asians increases at a lower BMI, according to prior analyses [30,31].
The survey-based screening instruments listed in Table 1 were also compared to random glucometer testing, for which a previous trial in rural India found that the optimal threshold for screening by ROC curve analysis was ≥6.1 mmol/l [15]. We estimated how many people would exceed this threshold, incorporating the variation in blood glucose levels among both persons with undiagnosed diabetes and persons without diabetes (S1 Fig) and the degree to which the measures of random glucose via handheld glucometers in the Indian field trial differed from laboratory venous blood glucose test results (a standard deviation of 0.9 in Bland-Altman analysis) [15]. In all cases, the screening instruments were followed by laboratory-based fasting blood glucose testing for diagnosis because other methods (i.e., hemoglobin A1c) are not widely available in India or other low - and middle-income countries at present. We additionally determined what proportion of screened patients would be expected to be positive for additional co-morbidities such as hypertension and obesity by noting the prevalence of these conditions among the screen-positive patients (based on the joint distributions of co-morbidities illustrated in S1 Fig). We also combined the survey-based instruments and random glucometer testing to evaluate the sensitivity and specificity of both serial and parallel screening scenarios, specifically simulating every possible combination of screening questionnaires and random glucose testing in which either one test is followed by another in any order (and both tests need to be positive for referral to confirmatory testing) or both tests are performed simultaneously (and either test needs to be positive to proceed to confirmatory testing). We applied the instruments selectively to sub-populations defined by age, sex, urban/rural location, and income status to examine variations in sensitivity and specificity.
Cost Analysis
To provide a sense of the typical costs associated with a screening program, we tabulated the costs of both questionnaire-based and glucometer-based screening. We used World Health Organization CHOICE (CHOosing Interventions that are Cost-Effective) data [32], which provide the unit costs for personnel, operations, and materials for screening (itemized in S3 Table). Total costs including overhead expenditures were tabulated in 2014 US dollars for each screening strategy over a 10-y implementation horizon at a standard 3% annual discount rate, and were subjected to the sensitivity and uncertainty analyses described below.
Diabetes Complication Rates
To estimate the health benefits of screening, we used a mathematical model, the United Kingdom Prospective Diabetes Study (UKPDS) Outcomes Model 2, which includes South Asian–specific disease progression parameters that have been validated among South Asians in both the UK and India [33,34]. The risk equations in this model provide estimates of disease progression rates with and without treatment, including 20-y probabilities of heart disease events (including ischemic heart disease, myocardial infarction, and heart failure), stroke, blindness, diabetic ulcer (from peripheral arterial disease or neuropathy), and renal failure (see S1 Text for endpoint definitions) [18,19,33]. We drew relevant biomarker values for individuals found through screening using Monte Carlo sampling from the distribution of biomarkers among people with previously undiagnosed diabetes in the IMS, in which the biomarkers were assessed across India by age, sex, income, and location (see S1 Fig) [35]. We then estimated the minimum NNST to prevent each of the diabetes complications, using the most optimistic and aggressive targets for treatment (those set by the American Diabetes Association) to provide a minimum floor estimate of the NNST [21]. These targets include lowering systolic blood pressure to ≤140 mm Hg, low-density lipoprotein (LDL) to ≤2.6 mmol/l in those with no cardiovascular disease history (or ≤1.8 mmol/l in those with a history of cardiovascular disease), and hemoglobin A1c to ≤7%. We additionally simulated the observed impact of behavioral risk factor modification (i.e., lifestyle interventions) to reduce diabetes complications; although these have not been found effective for cardiovascular endpoints, they potentially reduce the risk of intermediate microvascular endpoints, which may translate into eventual reductions in blindness and end-stage renal failure [36,37]. To estimate the minimum NNST values (i.e., the most optimistic case), we simulated full reversal of risk, as per the UKPDS risk equations, and simulated the case of universal treatment adherence by both providers and patients. This approach provides the best-case scenario for treatment outcomes. We also simulated treatment of currently diagnosed patients with diabetes, similarly assigned biomarkers through Monte Carlo sampling from their distribution of risk factors in the IMS [35]. We validated our estimates against previously published example calculations to ensure correct application of the model equations [18,19,33].
Sensitivity and Uncertainty Analyses
First, we estimated the minimum NNS to find one previously undiagnosed diabetes case if people eligible for screening were subjected directly to fasting venous blood glucose testing rather than the survey-based screening or random glucometer screening.
Second, we determined whether alternative thresholds for classifying persons as high risk for each instrument would maximize the performance (i.e., increase the product of the sensitivity and specificity) of the instrument among the national population in the model, as compared to the existing instrument cut points published previously based on sub-national studies (Table 1). We constructed ROC curves on all tested instruments to identify optimal cut points in the national population.
Finally, for uncertainty analysis, we ran our model 10,000 times while using Monte Carlo sampling from the probability distributions of all input parameters to estimate stable 95% credible interval estimates around all model outcomes.
The model was programmed and implemented in R (v. 3.1.0, The R Foundation for Statistical Computing, Vienna).
Results
Disease Burden
Among the 586 million people anticipated to be aged 25–65 y old in India in the year 2015, the mean diabetes prevalence rate was estimated as 12.0% in our model (95% CI: 8.4%–15.6%), such that an estimated 70 million (95% CI: 50 million–91 million) people in this age group are thought to have diabetes. In the simulated population, diabetes prevalence was slightly but not significantly higher among men (12.3%, 95% CI: 9.4%–15.2%) than women (11.7%, 95% CI: 7.5%–16.0%), and higher among urban (18.6%, 95% CI: 13.1%–24.1%) than rural (8.7%, 95% CI: 6.1%–11.2%) populations. An estimated 51 million of the 70 million persons with diabetes are expected to be undiagnosed before the screening program (73.3%, 95% CI: 69.9%–76.7%), with particularly high probabilities of being undiagnosed among women (83.1%, 95% CI: 81.3%–84.9%), low-income individuals (86.3%, 95% CI: 83.3%–89.3%), and rural populations (80.0%, 95% CI: 77.2%–82.8%). Fully disaggregated estimates by demographic group are provided in S2 Table.
We compared our modeled estimates of diagnosed and total diabetes prevalence to three independent estimates [4,25,26]. As shown in S4 Table, the model closely matched the independent estimates (<1.6% absolute difference) among all demographic categories and across all years for which estimates are available from 2000 through 2014.
Screening Simulation
Table 2 summarizes the estimated sensitivity, specificity, positive predictive value, and negative predictive value of each instrument, as well as the estimated NNS to find one undiagnosed diabetes case. The Chaturvedi risk score had the highest sensitivity (72.8%, versus 50.8% and 64.9% for the other two risk scores) and intermediate specificity (58.0%, versus 64.0% and 47.1%), and has the lowest NNS to find one undiagnosed diabetes case (15.2, versus 21.7 and 17.0).
Tab. 2. Comparison of instrument performance in published sub-national populations versus synthetic national population [6–8,15]. ![Comparison of instrument performance in published sub-national populations versus synthetic national population [<em class="ref">6</em>–<em class="ref">8</em>,<em class="ref">15</em>].](https://www.prolekarniky.cz/media/cache/resolve/media_object_image_small/media/image/16d2ab9a3bd6fcef531589f9aafbc0c1.png)
95% credible intervals are shown in parentheses. In all cases, the screening instrument is the first-stage test, and individuals testing positive are then subject to fasting blood glucose testing for diagnostic confirmation. By comparison with these survey-based screening instruments, random glucometer testing offered greater specificity and therefore fewer false-positive results (see Table 2). Random glucometer testing would be expected to have 62.6% sensitivity (95% CI: 61.1%–64.2%) and 75.5% specificity (95% CI: 75.2%–75.8%), requiring 17.6 persons (95% CI: 8.0–27.3) to be screened to find one undiagnosed diabetes case.
When projected to the population level (Fig 2; Table 3), we estimated that among 567 million Indians aged 25–65 y eligible for screening, between 158 and 306 million people (27.9%–53.9%) would screen positive and need referral for confirmatory testing. Between 26 and 37 million of the 51 million people with undiagnosed diabetes would be detected through any of the screening instruments (50.9%–72.8% of the undiagnosed population), while between 14 and 25 million people with undiagnosed diabetes would be missed by the screening instruments (27.2%–49.1% of those undiagnosed). Because of the lack of specificity of the survey-based screening instruments, between 186 and 273 million people without diabetes (36.0%–52.8% of those without diabetes screened) would be identified as false positives after confirmatory testing. For comparison, using a coin flip to refer people for confirmatory testing would detect 50% of undiagnosed diabetes (25.5 million people) and refer about 258 million people without diabetes to confirmatory testing. In the case of using random glucometer testing as an alternative screening approach, the number of false-positive screens would be expected to be reduced to 126 million (24.5% of those without diabetes screened). In other words, the ratio of false to true positives would range from 3.9 (in the case of random glucometer testing) to 8.2 (in the case of the Ramachandran risk score). S5 Table provides a complete sensitivity analysis of screening outcomes if screening were targeted to certain demographic groups and locations, revealing a consistently high ratio of false to true positives across targeted screening approaches.
Fig. 2. Population-level implications of large-scale screening for diabetes in India. FBG, fasting blood glucose. 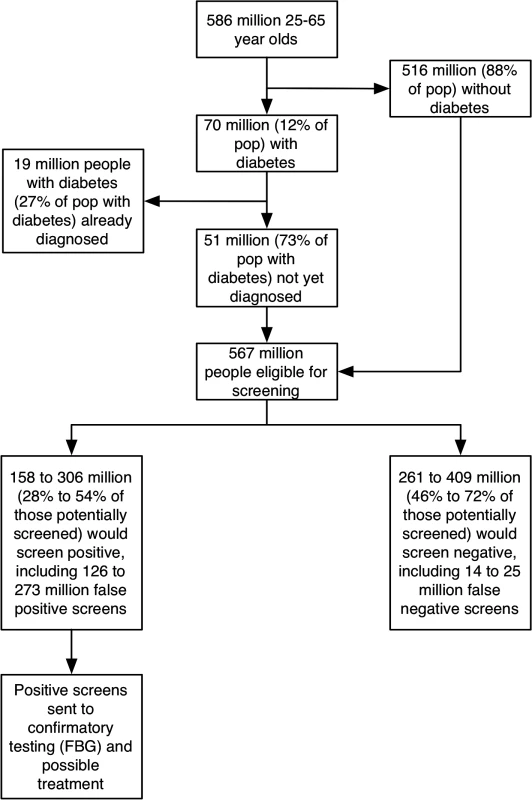
Tab. 3. Health system burden associated with alternative diabetes screening approaches. 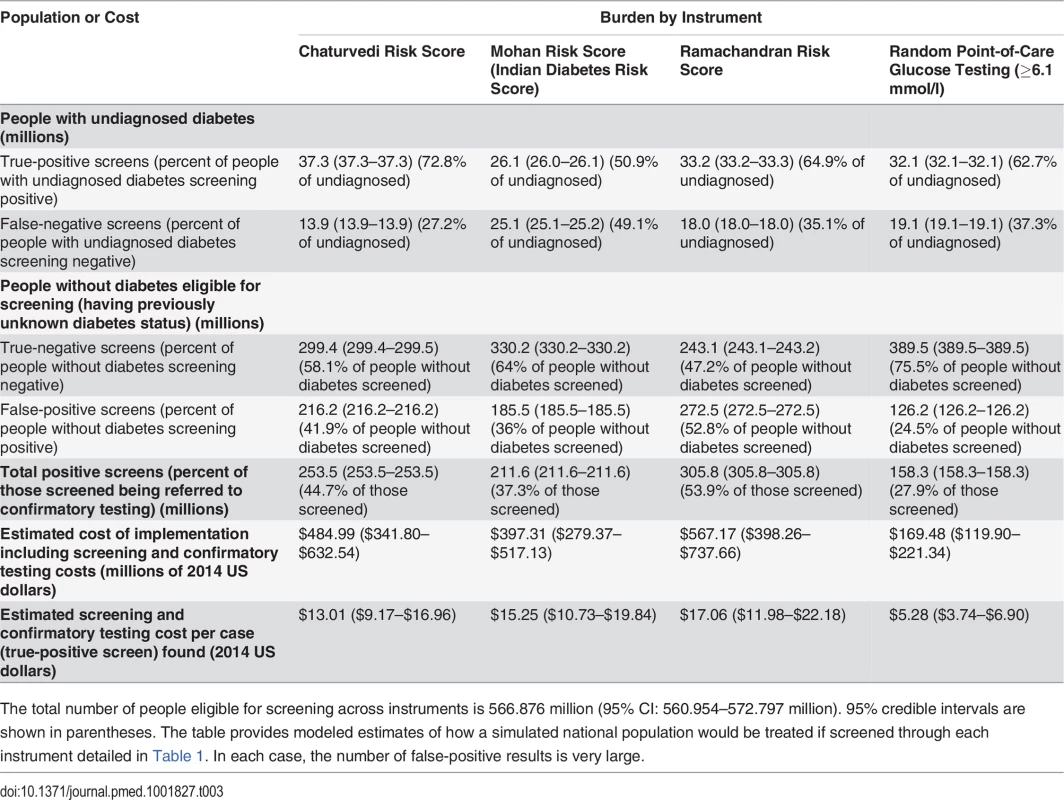
The total number of people eligible for screening across instruments is 566.876 million (95% CI: 560.954–572.797 million). 95% credible intervals are shown in parentheses. The table provides modeled estimates of how a simulated national population would be treated if screened through each instrument detailed in Table 1. In each case, the number of false-positive results is very large. Of note, the diabetes screening strategies would also serve to detect co-morbid diseases (S1 Fig). Of the proportion of persons screening positive through each instrument, between 23% (Mohan risk score) and 79% (random glucometer testing) would also be expected to have hypertension, and between 13% (Mohan risk score) and 56% (random glucometer testing) would also be expected to meet the criterion for obesity (BMI ≥ 30 kg/m2).
We compared both serial and parallel screening scenarios, that is, when one instrument would be followed by another in any order (and both tests would need to be positive for referral to confirmatory testing) or both tests would be performed simultaneously (and either test would need to be positive for referral to confirmatory testing), respectively. All of the parallel screening scenarios had worse screening performance than the serial testing scenarios, because of extremely high false - to true-positive ratios (S6 Table). Performing serial testing with survey-based instruments after random glucometer testing also failed to improve screening performance. The best screening performance, by contrast, was achieved through serial testing when survey-based instruments were used first, followed by random glucose testing of a blood sample with a handheld glucometer. This did not produce a significant improvement in sensitivity over and above using random glucose testing alone, but the specificity of the screening could be improved to as much as 86% (reducing the number of false positives to 30 million, but not significantly lowering the false - to true-positive ratio; S6 Table). Fig 3 illustrates the ROC points for each screening instrument in isolation and when followed by random glucose testing.
Fig. 3. Comparison of each instrument in isolation, or when followed by random blood glucose testing (point-of-care capillary blood glucometer test). 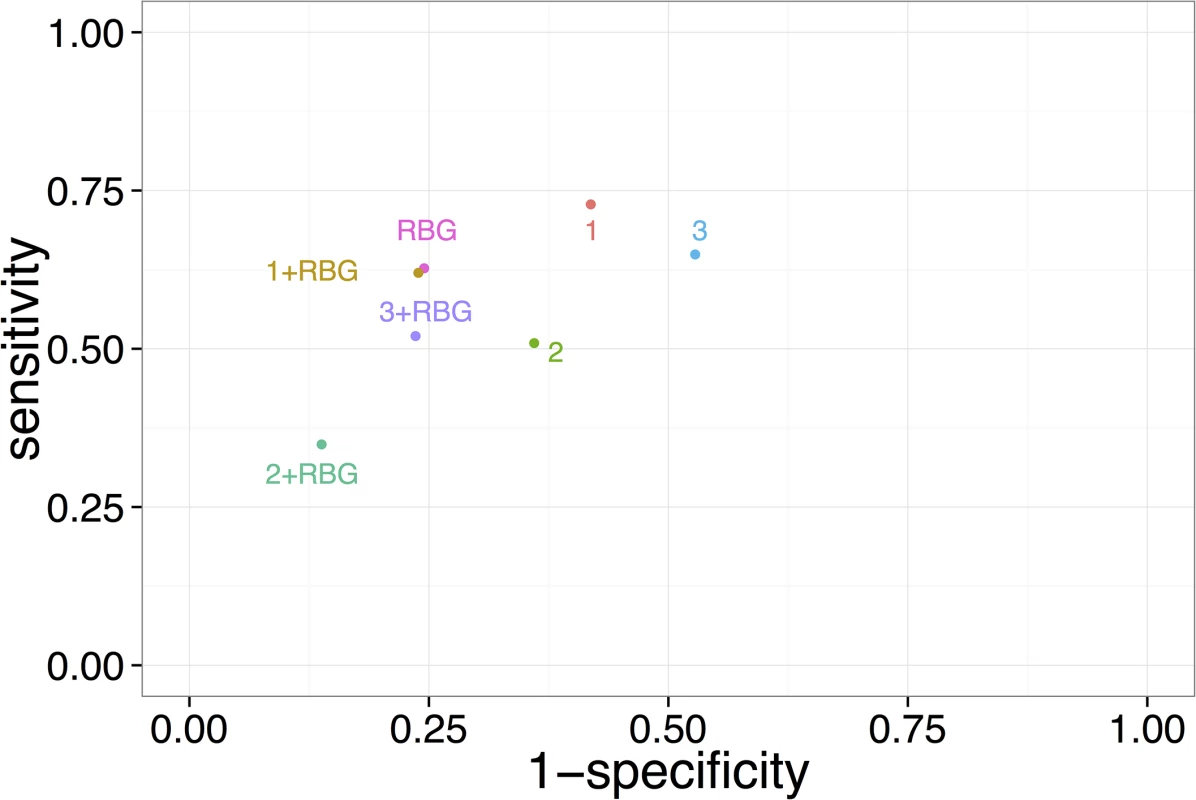
Numbers refer to screening instruments: 1, Chaturvedi risk score; 2, Mohan risk score; 3, Ramachandran risk score; RBG refers to random blood glucose testing. This plot displays the instrument performance using the cut points for positivity that were published in the literature previously to maximize the area under the ROC curve upon testing of the instruments among sub-national populations [6–8,15]. We also compared the performance of the instruments when recalibrated to the synthetic nationally representative population (S2 Fig). Cost Analysis
Table 3 summarizes the overall costs of each screening strategy, including estimated personnel, operations, and material costs anticipated from each screening strategy. We found that although the screening questionnaire costs were smaller than the costs of glucometer testing, this cost differential is more than outweighed by the high cost of confirmatory testing for the larger number of people who falsely screen positive by the questionnaire-based instruments. Overall discounted costs for screening varied from a low-end estimate of US$169 million for random glucometer testing (95% CI: US$120–US$221 million) to a high-end estimate of US$567 million for the Ramachandran risk score (95% CI: US$398–US$737 million), which corresponds to a price per case found of between US$5.28 (95% CI: US$3.74–US$6.90) for random glucometer testing and US$17.06 (95% CI: US$11.98–US$22.18) for the Ramachandran risk score.
Diabetes Complication Rates
In order to provide a sense of the order-of-magnitude difference in potential benefits of treatment among those with diabetes newly detected through screening versus those already diagnosed, S7 Table summarizes the model-based estimates of complication rates among the newly screened population. As shown in the table, in the best-case treatment scenario the NNST among those diagnosed through the community-based screening program was very high: on the order of 789 people (95% CI: 225–2,213). Tallying the individual complications averted through therapy, we found that 6.8% of the population newly diagnosed due to the screening program (95% CI: 2.3%-28.6%) would be expected to avoid a diabetes complication over 20 y in this best-case scenario. This corresponds to a median screening cost per case with complication prevented (i.e., excluding treatment costs) of US$1,908.17 (95% CI: US$562.00–US$7,015.81) in the best-case scenario.
Sensitivity and Uncertainty Analyses
We also estimated the minimum NNS to find one previously undiagnosed diabetes case if people eligible for screening were subjected to fasting venous blood glucose testing, bypassing the survey-based screening instruments or random glucometer screening to skip directly to the confirmatory testing phase. The NNS through this approach to find one previously undiagnosed diabetes case was estimated to be 11.1 (95% CI: 8.6–15.6), as compared to between 15.2 and 21.7 for the alternative screening instruments (Table 2).
We found that recalibrating each screening instrument to the synthetic nationally representative population (S2 Fig), rather than using the standard cut points established in the sub-national cohort studies (Table 1), would allow us to improve the specificity of some of the instruments (S8 Table). Here, the recalibration involved choosing the cut point that maximized the product of sensitivity and specificity (i.e., the point at the top - and left-most corner of the ROC curves). This recalibration did not significantly change the NNS (Table 2, cf. S8 Table), and the number of false positives would still remain between 40 million and 116 million, for a false - to true-positive ratio of between 1.2 and 4.4.
Discussion
Our study finds that large-scale, population-wide screening for type 2 diabetes among adults in India is unlikely to meet established criteria for implementing screening programs, which specify that such screening should utilize a reliably sensitive and specific instrument, and offer significant therapeutic benefits to those individuals diagnosed through screening [11].
Our investigation adds several important findings to the existing literature. First, we found that not all instruments tested previously in nonrepresentative subpopulations would be expected to work well in a nationally standardized large-scale screening program. For instance, the popular Indian Diabetes Risk Score (the Mohan risk score) was found to have a sensitivity no better than chance on average when extended to population-representative data, as opposed to the data from the single city in which it was previously evaluated [8]. Recalibrating the instruments to a nationally representative population did not significantly impact the NNS to detect one undiagnosed diabetes case. Second, among the instruments and approaches tested, we found that very large numbers of false-positive screens would be expected. At a minimum, 126 million people who do not have diabetes would be labeled as high risk and referred for confirmatory testing, and as many as 273 million false positives would be expected to be referred if applying some currently proposed screening instruments. When including both false - and true-positive screens, the burden on the health system would be expected to range from 158 to 306 million people referred to confirmatory testing, in order to detect an estimated 26 to 37 million people with currently undiagnosed diabetes. Third, among the screening options available, skipping the survey-based or random glucometer testing to proceed directly to fasting venous blood glucose appeared to significantly lower the NNS to find one previously undiagnosed diabetes case, from between 15 and 22 persons down to 11 persons. It may be argued that adopting such a measure requires laboratory infrastructure, and thereby limits the population reached through screening; conversely, the question remains how meaningful and safe glucose-lowering therapy would be delivered to those individuals newly diagnosed in settings without such capacity, given that screening processes must follow basic principles of non-maleficence (i.e., “first do no harm”) [11].
The microsimulation results imply that the benefits of population-based diabetes screening may be just as limited in India as in higher-income countries, where such screening has been shown not to produce a significant reduction in all-cause, cardiovascular, or diabetes-related mortality, or in rates of end-stage diabetes-related microvascular compilations such as blindness or renal failure. The studies in higher-income countries have involved cardiovascular risk reduction measures among screen-detected diabetes patients, and target-based treatment among diabetes patients detected through screening in high-risk populations [13,14]. In countries such as India where the burden of disease is rising in the context of healthcare system capacity limitations, a large-scale screening program bears the burden of demonstrating that the system can handle the effort required to provide confirmatory testing and significantly beneficial treatment among those screening positive and testing positive, respectively. Our assessment calls into question the ability for this to be achieved in India, given the poor performance of current screening instruments and the modest impact of early therapy for diabetes.
There are several strengths and some limitations of the present study. We conducted a comprehensive analysis that incorporates the most optimistic screening scenarios and iteratively varies screening instruments across all plausible approaches. We additionally sampled among diverse Indian populations to construct a nationally representative population for study. Yet, as with all assessments of potential public health interventions, our model is based on important assumptions. First, we used existing published cohort studies of diabetes prevalence. While our assessment generated diabetes prevalence estimates matching independent estimates, the cohort studies are still unlikely fully to capture the poorest and most rural areas of the country, which are thought to have the lowest diabetes prevalence. This limitation would tend to overstate the positive impacts of screening in our model. We additionally derived estimates of treatment effects based on a model primarily developed among South Asians in the UK, and using effect size estimates largely derived from clinical trials in higher-income populations. Further, to provide best-case estimates, we assumed that aggressive treatment goals (systolic blood pressure < 140 mm Hg, hemoglobin A1c < 7%, and LDL < 100 mg/dl) would be reached, though these goals are rarely achieved even in developed countries and are clearly not reflective of current treatment patterns in India [38]. We performed these calculations to provide relative magnitude estimates of treatment impact among newly screened versus previously diagnosed patients, not to provide precise forecasts for cost-effectiveness analysis. Furthermore, we focused exclusively on type 2 diabetes, which is believed to comprise the vast majority of diabetes cases in India; the screening approaches here are not valid for type 1 diabetes, which would typically manifest among much younger age groups. Finally, we attached cost estimates based on currently available data on cost, but cost variations over space and time would be expected to generate differences between expected and realized costs in practice.
Our findings have several implications for further research. In particular, we did not compare alternative guidelines that are being advocated for treatment strategies among those newly diagnosed with diabetes. The American Diabetes Association, World Health Organization, and International Diabetes Federation guidelines all slightly differ in their suggested management strategies for diabetes among adults, and would likely have different implications for patient risk, safety, and system-level resource requirements [21,39,40]. A formal comparative effectiveness assessment to tabulate the risks and benefits of each guideline-based treatment strategy is needed. Furthermore, we found that a significant number of persons screening as high risk for diabetes would also likely screen positive for untreated hypertension. While the mass screening for asymptomatic diabetes may not produce significant treatment benefits given the limited impact of early glycemic control for asymptomatic diabetes, further evaluation of mass screening approaches for hypertension, with secondary screening of hypertensive individuals for diabetes risk, may be a prudent approach. This is particularly important given that the major cause of morbidity and mortality among people with type 2 diabetes in India and other low - and middle-income countries is cardiovascular disease, and the major all-cause mortality risk reduction benefit from diabetes treatment is from antihypertensive therapy rather than glycemic control [41,42]. An alternative to disease-specific screening may be an approach that focuses not on detection of individual risk factors, but on global cardiovascular risk assessment, based on a constellation of observed co-morbid risk factors ranging from diabetes to hypertension to tobacco smoking [43,44]. However, the benefit of cardiovascular risk assessment programs has been questioned, and their feasibility and cost-effectiveness in low - and middle-income countries need to be carefully considered [45].
Despite the need for future research as suggested above, our current analysis suggests that the existing and expanding large-scale diabetes screening program in India, which parallels the programs being suggested for implementation in numerous low - and middle-income countries [5,46], may have difficulties fulfilling basic criteria considered essential for effective large-scale screening. The current analysis suggests that no population-based mass diabetes screening option can truly be recommended at present because of the vast expected number of false-positive results. Hence, given our results, an approach that focuses on symptom-based screening, with attendant treatment improvement among already-diagnosed persons, may be more sensible than community-based mass screening. Improving instruments to reduce false-positive screens, preparing the health system for very substantial confirmatory testing demands, and identifying how to deliver efficacious treatment, are three priority areas that require urgent attention before countries experiencing rapid increases in diabetes prevalence implement large-scale community-based diabetes screening programs.
Supporting Information
Zdroje
1. Wild S, Roglic G, Green A, Sicree R, King H (2004) Global prevalence of diabetes estimates for the year 2000 and projections for 2030. Diabetes Care 27 : 1047–1053. 15111519
2. Shaw JE, Sicree RA, Zimmet PZ (2010) Global estimates of the prevalence of diabetes for 2010 and 2030. Diabetes Res Clin Pract 87 : 4–14. doi: 10.1016/j.diabres.2009.10.007 19896746
3. Lozano R, Naghavi M, Foreman K, Lim S, Shibuya K, et al. (2013) Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet 380 : 2095–2128.
4. International Diabetes Federation (2013) Diabetes atlas, 6th edition. Brussels: International Diabetes Federation.
5. Narayan KMV, Echouffo-Tcheugui JB, Mohan V, Ali MK (2012) Global prevention and control of type 2 diabetes will require paradigm shifts in policies within and among countries. Health Aff (Millwood) 31 : 84–92.
6. Chaturvedi V, Reddy KS, Prabhakaran D, Jeemon P, Ramakrishnan L, et al. (2008) Development of a clinical risk score in predicting undiagnosed diabetes in urban Asian Indian adults: a population-based study. CVD Prev Control 3 : 141–151.
7. Ramachandran A, Snehalatha C, Vijay V, Wareham NJ, Colagiuri S (2005) Derivation and validation of diabetes risk score for urban Asian Indians. Diabetes Res Clin Pract 70 : 63–70. 16126124
8. Mohan V, Deepa R, Deepa M, Somannavar S, Datta M (2005) A simplified Indian Diabetes Risk Score for screening for undiagnosed diabetic subjects. J Assoc Physicians India 53 : 759–763. 16334618
9. Ministry of Health and Family Welfare (2014) National Programme for Prevention and Control of Cancer, Diabetes, Cardiovascular Diseases and Stroke. Delhi: Government of India.
10. National Health Mission, Ministry of Health and Family Welfare (2013) Guidelines for the National Programme for Prevention and Control of Cancer, Diabetes, Cardiovascular Diseases and Stroke. Delhi: Government of India.
11. Wilson JMG, Jungner G (1968) Principles and practice of screening for disease. Geneva: World Health Organization. http://apps.who.int/iris/bitstream/10665/37650/1/WHO_PHP_34.pdf?ua=1. Accessed 16 April 2015.
12. Ramachandran A, Snehalatha C, Dharmaraj D, Viswanathan M (1992) Prevalence of glucose intolerance in Asian Indians: urban-rural difference and significance of upper body adiposity. Diabetes Care 15 : 1348–1355. 1425100
13. Griffin SJ, Borch-Johnsen K, Davies MJ, Khunti K, Rutten GEHM, et al. (2011) Effect of early intensive multifactorial therapy on 5-year cardiovascular outcomes in individuals with type 2 diabetes detected by screening (ADDITION-Europe): a cluster-randomised trial. Lancet 378 : 156–167. doi: 10.1016/S0140-6736(11)60698-3 21705063
14. Simmons RK, Echouffo-Tcheugui JB, Sharp SJ, Sargeant LA, Williams KM, et al. (2012) Screening for type 2 diabetes and population mortality over 10 years (ADDITION-Cambridge): a cluster-randomised controlled trial. Lancet 380 : 1741–1748. doi: 10.1016/S0140-6736(12)61422-6 23040422
15. Ritchie GE, Kengne AP, Joshi R, Chow C, Neal B, et al. (2011) Comparison of near-patient capillary glucose measurement and a risk assessment questionnaire in screening for type 2 diabetes in a high-risk population in rural India. Diabetes Care 34 : 44–49. doi: 10.2337/dc10-1270 21193620
16. Caro JJ, Briggs AH, Siebert U, Kuntz KM (2012) Modeling good research practices—overview: a report of the ISPOR-SMDM Modeling Good Research Practices Task Force–1. Med Decis Making 32 : 667–677. 22990082
17. United Nations (2013) World population prospects: the 2012 revision. Geneva: United Nations.
18. Stevens RJ, Kothari V, Adler AI, Stratton IM, Holman RR, et al. (2001) The UKPDS risk engine: a model for the risk of coronary heart disease in type II diabetes (UKPDS 56). Clin Sci 101 : 671–679. 11724655
19. Kothari V, Stevens RJ, Adler AI, Stratton IM, Manley SE, et al. (2002) UKPDS 60: risk of stroke in type 2 diabetes estimated by the UK Prospective Diabetes Study risk engine. Stroke 33 : 1776–1781. 12105351
20. International Institute for Population Sciences (2008) National Family Health Survey, India 2005–06. Bombay: International Institute for Population Sciences.
21. American Diabetes Association (2014) Standards of medical care in diabetes—2014. Diabetes Care 37: S14–S80. doi: 10.2337/dc14-S014 24357209
22. World Health Organization (2011) Use of glycated haemoglobin (HbA1c) in the diagnosis of diabetes mellitus. Geneva: World Health Organization.
23. World Health Organization (2006) Definition and diagnosis of diabetes mellitus and intermediate hyperglycemia: report of a WHO/IDF consultation. Geneva: World Health Organization.
24. Stanley TD, Doucouliagos H (2012) Meta-regression analysis in economics and business [Internet]. New York: Routledge.
25. Danaei G, Finucane MM, Lu Y, Singh GM, Cowan MJ, et al. (2011) National, regional, and global trends in fasting plasma glucose and diabetes prevalence since 1980: systematic analysis of health examination surveys and epidemiological studies with 370 country-years and 2.7 million participants. Lancet 378 : 31–40. doi: 10.1016/S0140-6736(11)60679-X 21705069
26. Vellakkal S, Subramania SV, Millett C, Basu S, Stuckler D, et al. (2013) Socioeconomic inequalities in non-communicable diseases prevalence in India: disparities between self-reported diagnoses and standardized measures. PLoS ONE 8: e68219. doi: 10.1371/journal.pone.0068219 23869213
27. McKeigue PM, Shah B, Marmot MG (1991) Relation of central obesity and insulin resistance with high diabetes prevalence and cardiovascular risk in South Asians. Lancet 337 : 382–386. 1671422
28. McKeigue PM, Pierpoint T, Ferrie JE, Marmot MG (1992) Relationship of glucose intolerance and hyperinsulinaemia to body fat pattern in south Asians and Europeans. Diabetologia 35 : 785–791. 1511807
29. Forouhi NG, Jenkinson G, Thomas EL, Mullick S, Mierisova S, et al. (1999) Relation of triglyceride stores in skeletal muscle cells to central obesity and insulin sensitivity in European and South Asian men. Diabetologia 42 : 932–935. 10491752
30. Chiu M, Austin PC, Manuel DG, Shah BR, Tu JV (2011) Deriving ethnic-specific BMI cutoff points for assessing diabetes risk. Diabetes Care 34 : 1741–1748. doi: 10.2337/dc10-2300 21680722
31. Ntuk UE, Gill JMR, Mackay DF, Sattar N, Pell JP (2014) Ethnic-specific obesity cutoffs for diabetes risk: cross-sectional study of 490,288 UK biobank participants. Diabetes Care 37 : 2500–2507. doi: 10.2337/dc13-2966 24974975
32. World Health Organization (2014) Cost effectiveness and strategic planning (WHO-CHOICE). http://www.who.int/choice/cost-effectiveness/en/. Accessed 16 April 2015.
33. Hayes AJ, Leal J, Gray AM, Holman RR, Clarke PM (2013) UKPDS outcomes model 2: a new version of a model to simulate lifetime health outcomes of patients with type 2 diabetes mellitus using data from the 30 year United Kingdom Prospective Diabetes Study: UKPDS 82. Diabetologia 56 : 1925–1933. doi: 10.1007/s00125-013-2940-y 23793713
34. Ghosh P, Kandhare AD, Raygude KS, Kumar VS, Rajmane AR, et al. (2012) Determination of the long term diabetes related complications and cardiovascular events using UKPDS risk engine and UKPDS outcomes model in a representative western Indian population. Asian Pac J Trop Dis 2 (Suppl 2): S642–S650.
35. Ebrahim S, Kinra S, Bowen L, Andersen E, Ben-Shlomo Y, et al. (2010) The effect of rural-to-urban migration on obesity and diabetes in India: a cross-sectional study. PLoS Med 7: e1000268. doi: 10.1371/journal.pmed.1000268 20436961
36. Knowler W (2013) Impact of a lifestyle intervention on diabetes control and microvascular complications. 73rd Scientific Sessions; 21–25 Jun 2013; Chicago, Illinois, US.
37. Look AHEAD Research Group, Wing RR, Bolin P, Brancati FL, Bray GA, et al. (2013) Cardiovascular effects of intensive lifestyle intervention in type 2 diabetes. N Engl J Med 369 : 145–154. doi: 10.1056/NEJMoa1212914 23796131
38. Casagrande SS, Fradkin JE, Saydah SH, Rust KF, Cowie CC (2013) The prevalence of meeting A1C, blood pressure, and LDL goals among people with diabetes, 1988–2010. Diabetes Care 36 : 2271–2279. doi: 10.2337/dc12-2258 23418368
39. World Health Organization (2012) Guidelines for primary health care in low-resource settings. Geneva: World Health Organization.
40. International Diabetes Federation (2012) Global guideline for type 2 diabetes. http://www.idf.org/sites/default/files/IDF-Guideline-for-Type-2-Diabetes.pdf. Accessed 16 April 2015.
41. UK Prospective Diabetes Study Group (1998) Tight blood pressure control and risk of macrovascular and microvascular complications in type 2 diabetes: UKPDS 38. BMJ 317 : 703–713. 9732337
42. Zoungas S, Chalmers J, Neal B, Billot L, Li Q, et al. (2014) Follow-up of blood-pressure lowering and glucose control in type 2 diabetes. N Engl J Med 371 : 1392–1406. doi: 10.1056/NEJMoa1407963 25234206
43. Vijan S, Sussman JB, Yudkin JS, Hayward RA (2014) Effect of patients’ risks and preferences on health gains with plasma glucose level lowering in type 2 diabetes mellitus. JAMA Intern Med 174 : 1227–1234. doi: 10.1001/jamainternmed.2014.2894 24979148
44. Sussman J, Vijan S, Hayward R (2013) Using benefit-based tailored treatment to improve the use of antihypertensive medications. Circulation 128 : 2309–2317. doi: 10.1161/CIRCULATIONAHA.113.002290 24190955
45. Capewell S (2008) Will screening individuals at high risk of cardiovascular events deliver large benefits? No. BMJ 337: a1395. doi: 10.1136/bmj.a1395 18755771
46. Narayan KMV, Chan J, Mohan V (2011) Early identification of type 2 diabetes policy should be aligned with health systems strengthening. Diabetes Care 34 : 244–246. doi: 10.2337/dc10-1952 21193623
Štítky
Interní lékařství
Článek vyšel v časopisePLOS Medicine
Nejčtenější tento týden
2015 Číslo 5- Berberin: přírodní hypolipidemikum se slibnými výsledky
- Příznivý vliv Armolipidu Plus na hladinu cholesterolu a zánětlivé parametry u pacientů s chronickým subklinickým zánětem
- Léčba bolesti u seniorů
- Jak postupovat při výběru betablokátoru − doporučení z kardiologické praxe
- Hydrofilní gel na bázi medu v terapii chronických a infikovaných ran
-
Všechny články tohoto čísla
- The Tobacco Endgame: Is It Possible?
- Screening and Treating UN Peacekeepers to Prevent the Introduction of Artemisinin-Resistant Malaria into Africa
- The Health System and Population Health Implications of Large-Scale Diabetes Screening in India: A Microsimulation Model of Alternative Approaches
- Seasonal Influenza Vaccination for Children in Thailand: A Cost-Effectiveness Analysis
- Healthy Eating and Risks of Total and Cause-Specific Death among Low-Income Populations of African-Americans and Other Adults in the Southeastern United States: A Prospective Cohort Study
- An Unsupported Preference for Intravenous Antibiotics
- Use of Fixed Dose Combination (FDC) Drugs in India: Central Regulatory Approval and Sales of FDCs Containing Non-Steroidal Anti-Inflammatory Drugs (NSAIDs), Metformin, or Psychotropic Drugs
- A Global Biomedical R&D Fund and Mechanism for Innovations of Public Health Importance
- Setting International Standards for the Management of Public Health Pesticides
- How Has the Age-Related Process of Overweight or Obesity Development Changed over Time? Co-ordinated Analyses of Individual Participant Data from Five United Kingdom Birth Cohorts
- PLOS Medicine
- Archiv čísel
- Aktuální číslo
- Informace o časopisu
Nejčtenější v tomto čísle- Use of Fixed Dose Combination (FDC) Drugs in India: Central Regulatory Approval and Sales of FDCs Containing Non-Steroidal Anti-Inflammatory Drugs (NSAIDs), Metformin, or Psychotropic Drugs
- How Has the Age-Related Process of Overweight or Obesity Development Changed over Time? Co-ordinated Analyses of Individual Participant Data from Five United Kingdom Birth Cohorts
- A Global Biomedical R&D Fund and Mechanism for Innovations of Public Health Importance
- An Unsupported Preference for Intravenous Antibiotics
Kurzy
Zvyšte si kvalifikaci online z pohodlí domova
Současné možnosti léčby obezity
nový kurzAutoři: MUDr. Martin Hrubý
Všechny kurzyPřihlášení#ADS_BOTTOM_SCRIPTS#Zapomenuté hesloZadejte e-mailovou adresu, se kterou jste vytvářel(a) účet, budou Vám na ni zaslány informace k nastavení nového hesla.
- Vzdělávání




