-
Články
Top novinky
Reklama- Vzdělávání
- Časopisy
Top články
Nové číslo
- Témata
Top novinky
Reklama- Videa
- Podcasty
Nové podcasty
Reklama- Kariéra
Doporučené pozice
Reklama- Praxe
Top novinky
ReklamaMonitoring and Evaluating Progress towards Universal Health Coverage in Tanzania
article has not abstract
Published in the journal: . PLoS Med 11(9): e32767. doi:10.1371/journal.pmed.1001698
Category: Collection Review
doi: https://doi.org/10.1371/journal.pmed.1001698Summary
article has not abstract
This paper is part of the PLOS Universal Health Coverage Collection. This is the summary of the Tanzania country case study. The full paper is available as Supporting Information file Text S1.
Background
Achieving universal health coverage (UHC)—defined as access to needed health services to all and protection against financial risks arising from paying for health services [1]—is among the top priorities of reform agendas across many countries. Provision of health services should be determined by individuals' need rather than their ability to pay and, at the same time, utilization of services by those seeking health care should not impose the risk of financial catastrophe [2],[3]. In addition, paying for health care should be administered in an equitable manner whereby individuals with a higher ability to pay contribute a relatively higher share of their income to health financing compared to those individuals with a lower ability to pay [3]. Tanzania has been making efforts towards UHC starting with the abolition of user fees soon after independence in 1967, before their reintroduction in the early 1990s, and the introduction of health insurance schemes in early 2000.
Universal Health Coverage: The Policy Context
Immediately after independence in 1961, Tanzania adopted a free health care policy that lasted until the early 1990s when user fees were reintroduced, accompanied by exemptions and waivers for the poor [4]. In 1999 the National Health Insurance Fund (NHIF) for formal public sector employees was introduced [5], followed by the community health fund (CHF) enacted in 2001 to cover the informal sector of the population (such as farmers, unregistered business owners, and the unemployed) [6]. In 2007 the country adopted a ten year (2007–2017) primary health care development program (PHCDP), whose main objective is improvement of the primary health care delivery system by increasing the number of health facilities, especially in rural areas [7]. Currently the government is in the process of developing its first National Health Financing Strategy (HFS), which stipulates the intention of developing a health financing system that will guarantee access to needed care for all and provide financial protection against payments for health care.
Monitoring and Evaluation for Universal Health Coverage
The assessment of progress in financial protection used data from the National Household Budget Survey 2007, the Strategies for Health Insurance for Equities in Less Developed Countries (SHIELD) survey 2008, and the National Panel Survey (NPS) 2010/2011. Access indicators were derived from the analytical report prepared for medium term review of the health sector strategic plan 2009–2015. Indicators were selected on the basis of availability of data, their priorities in the health sector strategic plans, and the degree to which the indicator addresses a critical health system problem in Tanzania (e.g., availability of human resources for health). The study uses the framework presented in Figure 1 to assess progress towards UHC. The analysis starts by evaluating the extent to which needed services are accessible to the wider population; and then assesses the degree to which financial protection is guaranteed. The extent to which access and financial protection translate into improvement in health outcomes (e.g., morbidity and mortality) is also explored.
Fig. 1. Universal health coverage assessment framework. 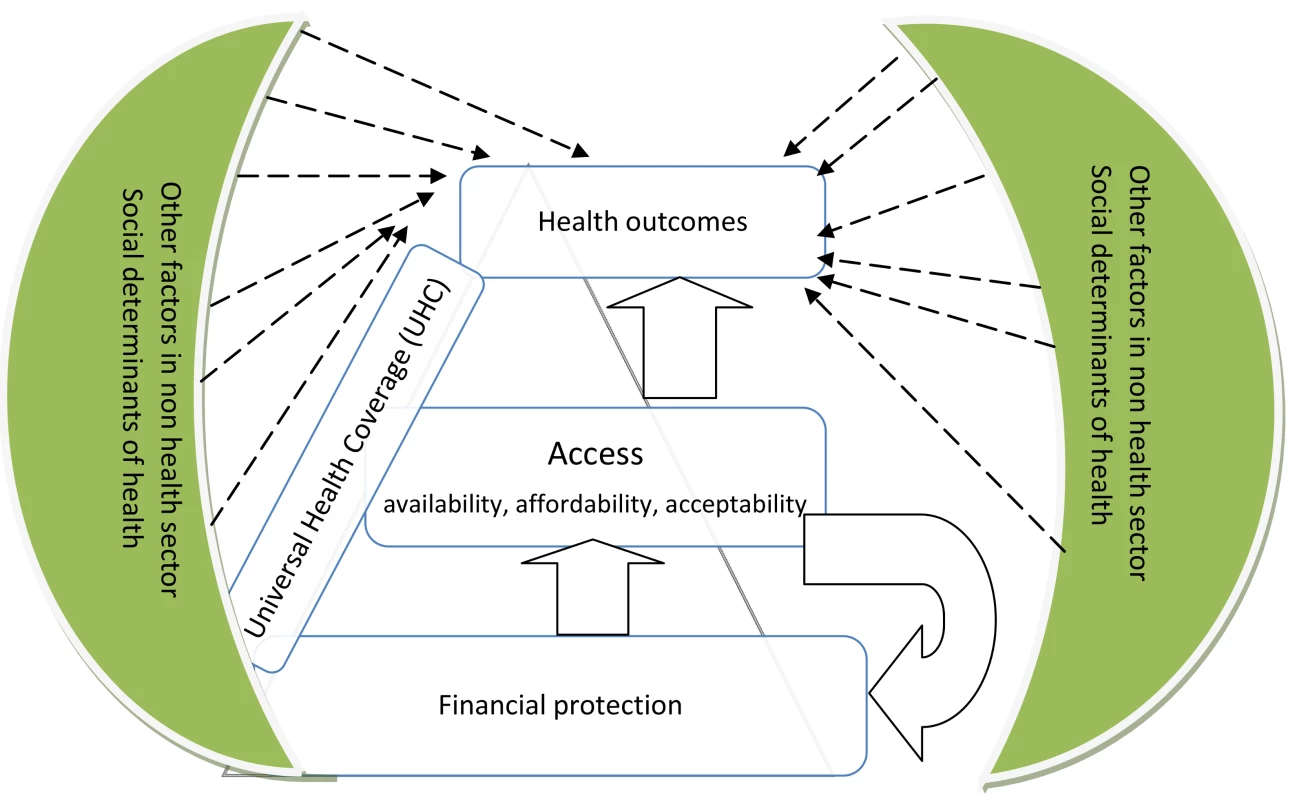
Progress towards Universal Health Coverage in Tanzania
Out-of-pocket (OOP) payments account for about 2% of people's income. About 2% of the population incurs catastrophic health care expenditures and 1% becomes impoverished because of OOP payments. Although the observed levels of incidences of catastrophic events and impoverishment are still low in Tanzania compared to other low - and middle-income countries [8],[9], they are still unacceptable because the main purpose of UHC is to protect every individual seeking health care against the hardships and impoverishing consequences of OOP payments.
The burden of OOP payments is significantly large among the poorest segment of the population as indicated by the negative Kakwani index (see Text S1, Table S3). The Kakwani index is a measure of how health care payments deviate from proportionality. The index is negative if the financing source is regressive, positive if it is progressive, and equal to zero if it is proportional. Only 15% of the population is covered by health insurance schemes. About 40% of total health sector financing is from external sources while OOP payments account for about 30% of total health sector resources. The contribution of prepayment health insurance schemes in total financing is insignificant.
Nearly every child has access to immunization services in Tanzania (Text S1, Table S4). Challenges remain in improving access to maternal services, especially in antenatal care visits and skilled birth deliveries, as these levels are still very low. Work is also needed in ensuring that health facilities have sufficient human resources and essential drugs and medical supplies.
The country has achieved significant improvements in infant and under-five mortality. Under-five mortality decreased from 112 deaths per 1,000 live births in 2005 to 81 deaths in 2010. Infant mortality decreased from 68 deaths to 51 deaths during the same period. A challenge remains in reducing maternal mortality following a small decrease from 578 deaths in 2005 to 468 deaths in 2010. HIV prevalence is about 6% and, with the current interventions to control the spread of this disease, there are high prospects of achieving the United Nations Millennium Development Goal (MDG) targets by 2015. Although the proportion of households owning insecticide treated nets is large, malaria prevalence among outpatients is still high at 34% (see Text S1, Table S5).
Conclusions and Recommendations
To achieve the goal of UHC, it is important for Tanzania to expand health insurance coverage through mandatory contributions to health insurance pools. Expansion of health insurance coverage will enhance financial protection among those who use services and also increase access to needed services, thereby translating into improved health status.
Supporting Information
Zdroje
1. WHO (2010) World health report. Geneva: WHO.
2. World Health Organization (2005) Social health insurance: sustainable health financing, universal coverage and social health insurance; 2005 16–25 May; Geneva: WHO.
3. World Health Organization (2005) Resolutions and decisions; 2005 16–25 May; Geneva: WHO.
4. MubyaziG (2004) The Tanzanian policy on health-care fee waivers and exemptions in practice as compared with other developing countries: evidence from recent local studies and international literature. East African Journal of Public Health 1 : 1–10.
5. United Republic of Tanzania (1999) The National Health Insurance Fund Act. The United Republic of Tanzania
6. United Republic of Tanzania (2001) The Community Health Fund Act. Dar es Salaam: United Republic of Tanzania.
7. Ministry of Health and Social Welfare (2007) Primary Health Services Development Program-MMAM 2007–2017. Dar es Salaam: Ministry of Health and Social Welfare.
8. Van DoorslaerE, O'DonnellO, Rannan-EliyaRP, SomanathanA, AdhikariSR, et al. (2007) Catastrophic payments for health care in Asia. Health Economics 16 : 1159–1184.
9. van DoorslaerE, O'DonnellO, Rannan-EliyaRP, SomanathanA, AdhikariSR, et al. (2006) Effect of payments for health care on poverty estimates in 11 countries in Asia: an analysis of household survey data. Lancet 368 : 1357–1364.
Štítky
Interní lékařství
Článek vyšel v časopisePLOS Medicine
Nejčtenější tento týden
2014 Číslo 9- Berberin: přírodní hypolipidemikum se slibnými výsledky
- Léčba bolesti u seniorů
- Příznivý vliv Armolipidu Plus na hladinu cholesterolu a zánětlivé parametry u pacientů s chronickým subklinickým zánětem
- Jak postupovat při výběru betablokátoru − doporučení z kardiologické praxe
- Červená fermentovaná rýže účinně snižuje hladinu LDL cholesterolu jako vhodná alternativa ke statinové terapii
-
Všechny články tohoto čísla
- Monitoring and Evaluating Progress towards Universal Health Coverage in Ghana
- Sorting Reality from What We Think We Know About Breast Cancer in Africa
- The PLOS “Monitoring Universal Health Coverage” Collection: Managing Expectations
- Monitoring and Evaluating Progress towards Universal Health Coverage in India
- Monitoring and Evaluating Progress towards Universal Health Coverage in Tanzania
- Monitoring and Evaluating Progress towards Universal Health Coverage in Brazil
- Monitoring and Evaluating Progress towards Universal Health Coverage in Thailand
- Monitoring and Evaluating Progress towards Universal Health Coverage in Estonia
- Monitoring and Evaluating Progress towards Universal Health Coverage in Chile
- Prioritizing Pregnant Women for Long-Lasting Insecticide Treated Nets through Antenatal Care Clinics
- Financial Risk Protection and Universal Health Coverage: Evidence and Measurement Challenges
- Convergence of Mortality Rates among Patients on Antiretroviral Therapy in South Africa and North America
- Malaria Prevention during Pregnancy—Is There a Next Step Forward?
- Beyond UHC: Monitoring Health and Social Protection Coverage in the Context of Tuberculosis Care and Prevention
- Intimate Partner Violence and Reproductive Coercion: Global Barriers to Women's Reproductive Control
- Genetic Predisposition to Increased Blood Cholesterol and Triglyceride Lipid Levels and Risk of Alzheimer Disease: A Mendelian Randomization Analysis
- Readmissions after Hospitalization for Heart Failure, Acute Myocardial Infarction, or Pneumonia among Young and Middle-Aged Adults: A Retrospective Observational Cohort Study
- Intermittent Preventive Treatment of Malaria in Pregnancy with Mefloquine in HIV-Infected Women Receiving Cotrimoxazole Prophylaxis: A Multicenter Randomized Placebo-Controlled Trial
- Equity-Oriented Monitoring in the Context of Universal Health Coverage
- The Clinical and Economic Impact of Point-of-Care CD4 Testing in Mozambique and Other Resource-Limited Settings: A Cost-Effectiveness Analysis
- Effective Coverage: A Metric for Monitoring Universal Health Coverage
- Mortality in Patients with HIV-1 Infection Starting Antiretroviral Therapy in South Africa, Europe, or North America: A Collaborative Analysis of Prospective Studies
- Global Financing and Long-Term Technical Assistance for Multidrug-Resistant Tuberculosis: Scaling Up Access to Treatment
- Oral Cholera Vaccine Development and Use in Vietnam
- Monitoring and Evaluating Progress towards Universal Health Coverage in Bangladesh
- Monitoring and Evaluating Progress towards Universal Health Coverage in South Africa
- Monitoring and Evaluating Progress towards Universal Health Coverage in Ethiopia
- Preventing Acute Malnutrition in Young Children: Improving the Evidence for Current and Future Practice
- Monitoring and Evaluating Progress towards Universal Health Coverage in Singapore
- Monitoring and Evaluating Progress towards Universal Health Coverage in China
- Monitoring and Evaluating Progress towards Universal Health Coverage in Tunisia
- Receptor-Defined Subtypes of Breast Cancer in Indigenous Populations in Africa: A Systematic Review and Meta-Analysis
- WHO Essential Medicines Policies and Use in Developing and Transitional Countries: An Analysis of Reported Policy Implementation and Medicines Use Surveys
- Intermittent Preventive Treatment of Malaria in Pregnancy with Mefloquine in HIV-Negative Women: A Multicentre Randomized Controlled Trial
- Preventing Acute Malnutrition among Young Children in Crises: A Prospective Intervention Study in Niger
- Monitoring Progress towards Universal Health Coverage at Country and Global Levels
- Monitoring Intervention Coverage in the Context of Universal Health Coverage
- Regular Breakfast Consumption and Type 2 Diabetes Risk Markers in 9- to 10-Year-Old Children in the Child Heart and Health Study in England (CHASE): A Cross-Sectional Analysis
- Proton Pump Inhibitors and Hospitalization with Hypomagnesemia: A Population-Based Case-Control Study
- PLOS Medicine
- Archiv čísel
- Aktuální číslo
- Informace o časopisu
Nejčtenější v tomto čísle- Proton Pump Inhibitors and Hospitalization with Hypomagnesemia: A Population-Based Case-Control Study
- Monitoring and Evaluating Progress towards Universal Health Coverage in Chile
- Malaria Prevention during Pregnancy—Is There a Next Step Forward?
- Financial Risk Protection and Universal Health Coverage: Evidence and Measurement Challenges
Kurzy
Zvyšte si kvalifikaci online z pohodlí domova
Současné možnosti léčby obezity
nový kurzAutoři: MUDr. Martin Hrubý
Všechny kurzyPřihlášení#ADS_BOTTOM_SCRIPTS#Zapomenuté hesloZadejte e-mailovou adresu, se kterou jste vytvářel(a) účet, budou Vám na ni zaslány informace k nastavení nového hesla.
- Vzdělávání



