-
Články
Top novinky
Reklama- Vzdělávání
- Časopisy
Top články
Nové číslo
- Témata
Top novinky
Reklama- Videa
- Podcasty
Nové podcasty
Reklama- Kariéra
Doporučené pozice
Reklama- Praxe
Top novinky
ReklamaThe Cost and Impact of Scaling Up Pre-exposure Prophylaxis for HIV Prevention: A Systematic Review of Cost-Effectiveness Modelling Studies
Background:
Cost-effectiveness studies inform resource allocation, strategy, and policy development. However, due to their complexity, dependence on assumptions made, and inherent uncertainty, synthesising, and generalising the results can be difficult. We assess cost-effectiveness models evaluating expected health gains and costs of HIV pre-exposure prophylaxis (PrEP) interventions.Methods and Findings:
We conducted a systematic review comparing epidemiological and economic assumptions of cost-effectiveness studies using various modelling approaches. The following databases were searched (until January 2013): PubMed/Medline, ISI Web of Knowledge, Centre for Reviews and Dissemination databases, EconLIT, and region-specific databases. We included modelling studies reporting both cost and expected impact of a PrEP roll-out. We explored five issues: prioritisation strategies, adherence, behaviour change, toxicity, and resistance. Of 961 studies retrieved, 13 were included. Studies modelled populations (heterosexual couples, men who have sex with men, people who inject drugs) in generalised and concentrated epidemics from Southern Africa (including South Africa), Ukraine, USA, and Peru. PrEP was found to have the potential to be a cost-effective addition to HIV prevention programmes in specific settings. The extent of the impact of PrEP depended upon assumptions made concerning cost, epidemic context, programme coverage, prioritisation strategies, and individual-level adherence. Delivery of PrEP to key populations at highest risk of HIV exposure appears the most cost-effective strategy. Limitations of this review include the partial geographical coverage, our inability to perform a meta-analysis, and the paucity of information available exploring trade-offs between early treatment and PrEP.Conclusions:
Our review identifies the main considerations to address in assessing cost-effectiveness analyses of a PrEP intervention—cost, epidemic context, individual adherence level, PrEP programme coverage, and prioritisation strategy. Cost-effectiveness studies indicating where resources can be applied for greatest impact are essential to guide resource allocation decisions; however, the results of such analyses must be considered within the context of the underlying assumptions made.
Please see later in the article for the Editors' Summary
Published in the journal: . PLoS Med 10(3): e32767. doi:10.1371/journal.pmed.1001401
Category: Research Article
doi: https://doi.org/10.1371/journal.pmed.1001401Summary
Background:
Cost-effectiveness studies inform resource allocation, strategy, and policy development. However, due to their complexity, dependence on assumptions made, and inherent uncertainty, synthesising, and generalising the results can be difficult. We assess cost-effectiveness models evaluating expected health gains and costs of HIV pre-exposure prophylaxis (PrEP) interventions.Methods and Findings:
We conducted a systematic review comparing epidemiological and economic assumptions of cost-effectiveness studies using various modelling approaches. The following databases were searched (until January 2013): PubMed/Medline, ISI Web of Knowledge, Centre for Reviews and Dissemination databases, EconLIT, and region-specific databases. We included modelling studies reporting both cost and expected impact of a PrEP roll-out. We explored five issues: prioritisation strategies, adherence, behaviour change, toxicity, and resistance. Of 961 studies retrieved, 13 were included. Studies modelled populations (heterosexual couples, men who have sex with men, people who inject drugs) in generalised and concentrated epidemics from Southern Africa (including South Africa), Ukraine, USA, and Peru. PrEP was found to have the potential to be a cost-effective addition to HIV prevention programmes in specific settings. The extent of the impact of PrEP depended upon assumptions made concerning cost, epidemic context, programme coverage, prioritisation strategies, and individual-level adherence. Delivery of PrEP to key populations at highest risk of HIV exposure appears the most cost-effective strategy. Limitations of this review include the partial geographical coverage, our inability to perform a meta-analysis, and the paucity of information available exploring trade-offs between early treatment and PrEP.Conclusions:
Our review identifies the main considerations to address in assessing cost-effectiveness analyses of a PrEP intervention—cost, epidemic context, individual adherence level, PrEP programme coverage, and prioritisation strategy. Cost-effectiveness studies indicating where resources can be applied for greatest impact are essential to guide resource allocation decisions; however, the results of such analyses must be considered within the context of the underlying assumptions made.
Please see later in the article for the Editors' SummaryIntroduction
Since the announcement of the results of HIV pre-exposure prophylaxis (PrEP) trials and the HPTN052 early treatment for prevention trial, there have been crucial policy discussions about the use of antiretroviral (ARV) drugs to prevent HIV acquisition or transmission. With regards to PrEP, encouraging results were first reported for men and transgender women who have sex with men in the iPrEX trial [1], which showed a 44% (95% CI 15–63) reduction in HIV acquisition with a daily dose of tenofovir/emtricitabine (TDF/FTC). In two large trials, the Partners PrEP [2] and TDF2 [3] studies, PrEP was found to be effective in reducing the risk of heterosexual HIV transmission using either TDF or TDF/FTC daily (Partners PrEP) and TDF/FTC daily (TDF2). However, FEM-PrEP [4], a trial recruiting heterosexual women in South Africa, Tanzania, and Kenya for daily TDF/FTC was closed prematurely in 2011 for futility as was the oral TDF arm of the VOICE trial [5] in women in South Africa, Uganda, and Zimbabwe. Two topical PrEP trials have tested the efficacy of 1% TDF gel and a third, FACTS001 [6], is currently recruiting women in South Africa. The CAPRISA 004 trial [7] in Kwa Zulu-Natal found that pre - and post-coital vaginal TDF gel reduced women's acquisition risk by 39% (95% CI 6–60) but the VOICE trial stopped its gel arm when it became evident that daily gel use was safe but not effective [8].
Clinical guidance on oral PrEP has already been offered by the US Centers for Disease Control and Prevention, the Southern African HIV Clinicians Society, World Health Organization (WHO), and the British Association for Sexual Health and HIV [9]–[13]. An advisory panel to the US Food and Drug Administration recently recommended oral TDF/FTC for preventive use among people at higher risk of HIV exposure [14]. As PrEP emerges as an option for inclusion in the HIV prevention toolbox, it is important for national policy and decision makers to identify where PrEP may fit best within already established HIV prevention programming (and budgets) and the potential implications of introducing such policy changes. In particular, decision makers need information translating the trial results into potential population-level impact and cost-effectiveness to ensure that any additional investment will have the maximum possible effect on the epidemic.
Economic and mathematical models provide a framework to integrate information on efficacy, effectiveness, costs, and patient outcomes to support decision making and resource allocation [15]. However, due to their complexity, dependence on assumptions made, and inherent uncertainties, generalising results from these models can be difficult. In this review, we aim to assess published cost-effectiveness models that have evaluated the expected health gains and costs of PrEP interventions. Specifically, our objectives are: (1) to describe modelling approaches of cost-effectiveness analyses of PrEP; (2) to compare the effects of epidemiological and cost assumptions on cost-effectiveness results; and (3) to explore the potential impact on cost-effectiveness estimates of five issues raised by policy makers [16]–[18] when considering PrEP implementation: prioritisation, adherence, behaviour change, toxicity, and resistance.
Methods
We performed a systematic review of the published literature following the protocol available in Text S2 and adhering to the PRISMA guidelines for reporting of systematic reviews (Text S1: PRISMA checklist) [19] and guidelines for appraisal of economic evaluations [20].
Search Strategy, Inclusion Criteria, and Study Selection
A broad strategy using both MeSH headings and free text, with no language limitations, was used to search PubMed/Medline, ISI Web of Knowledge (including Web of Science, Current Contents Connect, Derwent Innovations Index, CABI: CAB Abstracts, and Journal Citation Reports), Centre for Reviews and Dissemination databases (including DARE - Database of Abstracts of Reviews of Effects, NHS EED - NHS Economic Evaluation Database, and HTA database - health technology assessments), EconLIT, and region-specific databases (African Index Medicus, Eastern Mediterranean Literature (WHO), Index Medicus for South-East Asia Region, LILACS for Latin America). Our searches covered all published research up to the last search performed 14 January 2013 with no limitations on publication date. The following keywords were used: “cost” AND “tenofovir OR pre-exposure prophylaxis OR chemoprophylaxis OR PrEP” AND “HIV.” Citations and bibliographies of full text reports retrieved were reviewed for additional relevant articles. Abstracts from international conferences identified in the searches were also reviewed, as was the website of the International AIDS Economic Network. Experts were consulted for additional studies. We included all modelling studies reporting both cost and impact of a potential roll-out of a PrEP programme. We excluded those studies where costs were not assessed. No restrictions were made on the type of model, geography, mode of transmission, or impact (effectiveness) metric chosen. We included studies looking at both topical and systemic PrEP products. Full published papers were eligible, as well as abstracts from conferences providing sufficient information. Two authors (GBG and AB) screened titles and abstracts to identify potentially relevant articles. Full text reports of these articles were assessed independently for inclusion.
Data Extraction and Analysis
Data were extracted from selected studies by one reviewer (GBG) into prepared data sheets and independently cross-checked by a second assessor (AB). For conference abstracts selected for inclusion, we contacted the first author listed for further information. Extracted information on the study design included the type of study, viewpoint of analysis, timeframe, setting and population, background HIV prevalence or incidence, mode of HIV transmission, and a detailed description of alternative programmes compared in the studies (baseline scenario and PrEP scenario). We also tabulated data on the impact including risk heterogeneity, efficacy or effectiveness of PrEP, adherence (to programme or individual), behavioural change expected after introduction of PrEP, resistance, toxicity due to PrEP use, and disability-adjusted life year (DALY)/quality-adjusted life year (QALY) assumptions. A description of economic assumptions includes expected drug cost, other service costs, costs above service level, downstream antiretroviral treatment (ART) costs averted, discount rates, and, finally, cost-effectiveness results by metric and the conclusions presented in each publication. Prioritised scenarios were defined as those scenarios where PrEP was offered to specific sub-populations within the population modelled. While providing a critical assessment and narrative review of the studies included, we did not attempt to perform a meta-analysis due to the variability across the studies in reporting outcomes. Therefore, we adjusted estimates of cost-effectiveness for inflation to US$2012 to be able to compare studies from different years [21]. For those studies reporting cost/DALY averted, cost/QALY averted, or cost/life-year saved (LYS), we compared the estimates to a benchmark for cost-effectiveness [22] of one times the gross domestic product per capita (GDP/capita) per DALY averted, per QALY gained, or per LYS, depending on the unit of outcome used by each study. While DALYs, QALYs, and LYS are not equivalent, and decision rules vary by setting, this gives a broad indication of potential cost-effectiveness. The values for current GDP/capita were sourced from the World Bank databank for each country [23]. There is much controversy around decision rules [24], and while the comparison against GDP is the conventional approach, it should be noted that this may not represent the true opportunity cost in countries where less cost-effective health interventions are not being implemented at scale.
Results
We screened 961 titles and abstracts retrieved from 14 electronic databases. After performing web searches and consulting experts in the field, 36 full text articles were evaluated. We also reviewed the reference lists and citations of these articles. Of these 36, 13 studies were included in the review [25]–[37]: 11 peer-reviewed publications and two peer-reviewed conference abstracts (Figure 1). Articles excluded are listed in Table S1 and a summary of conclusions of the articles included are presented in Table S2.
Fig. 1. Flow diagram of study selection. 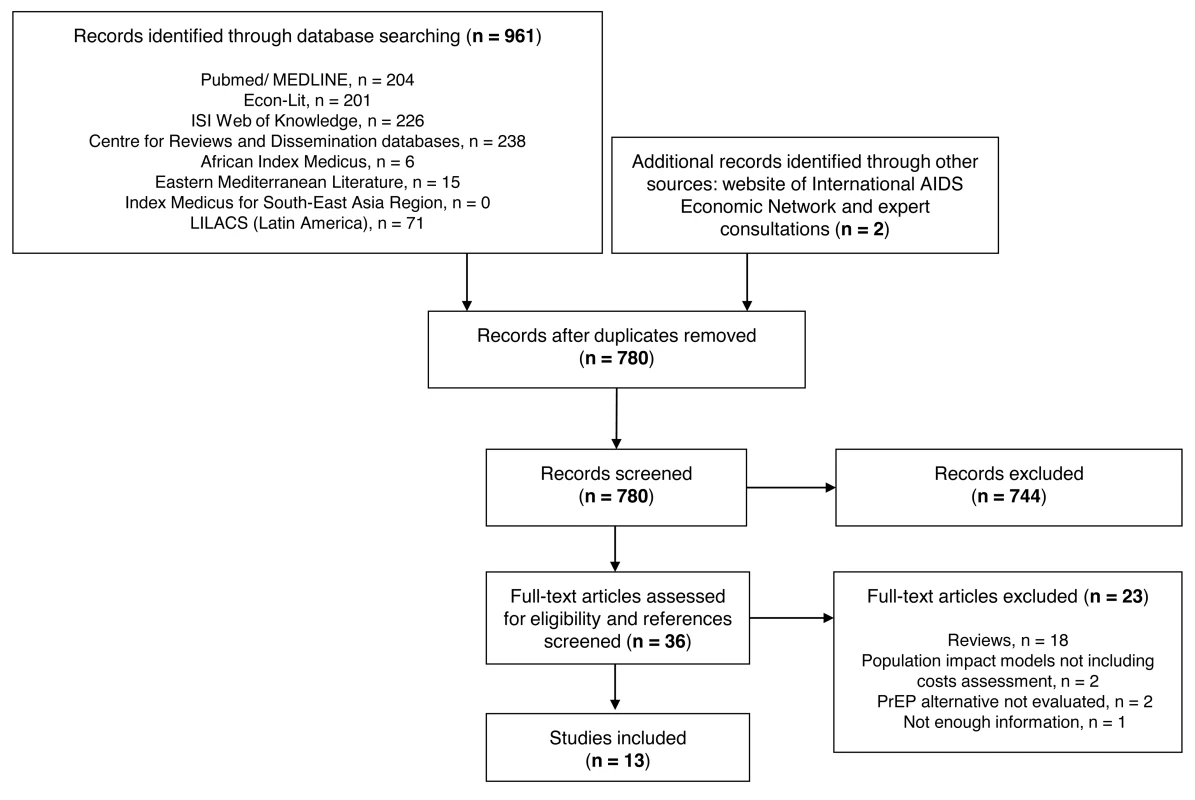
Region-specific databases can be accessed as follows: African Index Medicus, http://indexmedicus.afro.who.int/; Eastern Mediterranean Literature, http://www.emro.who.int/; Index Medicus for South-East Asia Region, http://www.hellis.org/; LILACS, Latin America, http://www.bireme.br/iah2/homepagei.htm. We present in Tables 1 to 4 the data extracted from the studies reviewed by study design, description of alternative programmes compared, impact, and cost assumptions. All studies were published between 2007 and 2013 and modelled the impact and cost, from a health care provider perspective, of PrEP scale-up in diverse settings. These settings included: heterosexual transmission in generalised epidemics in sub-Saharan Africa—the Southern Africa region [25], South Africa [28],[30],[31],[32],[36],[37]), and other modes of transmission in concentrated epidemics—among people who inject drugs (PWID) in Ukraine [33]; and men who have sex with men (MSM) in the USA [26],[29],[34],[35] and in Peru [27]. Timeframes varied from 5 to 20 y. All studies focused the models on high prevalence/incidence populations (Table 1).
Tab. 1. Study design. 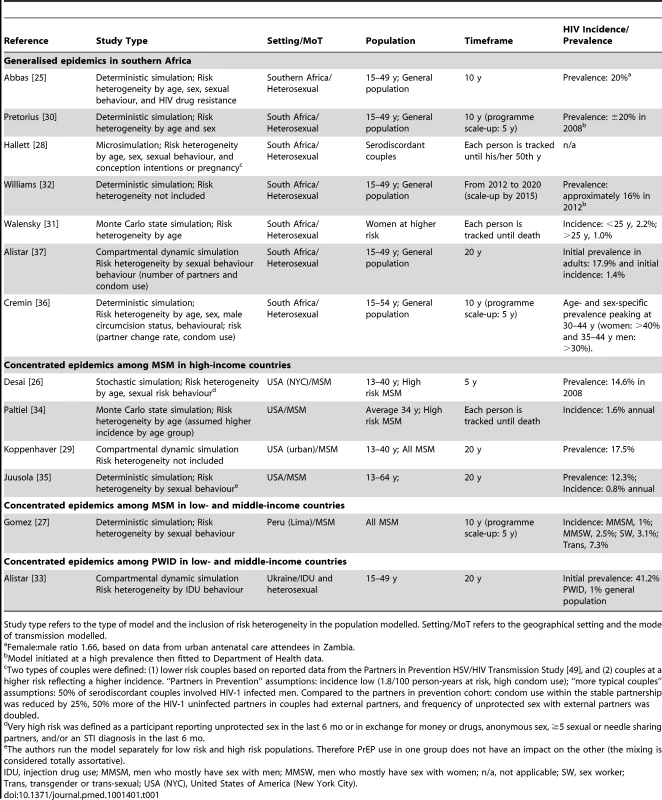
Study type refers to the type of model and the inclusion of risk heterogeneity in the population modelled. Setting/MoT refers to the geographical setting and the mode of transmission modelled. Tab. 2. Alternative programmes compared. 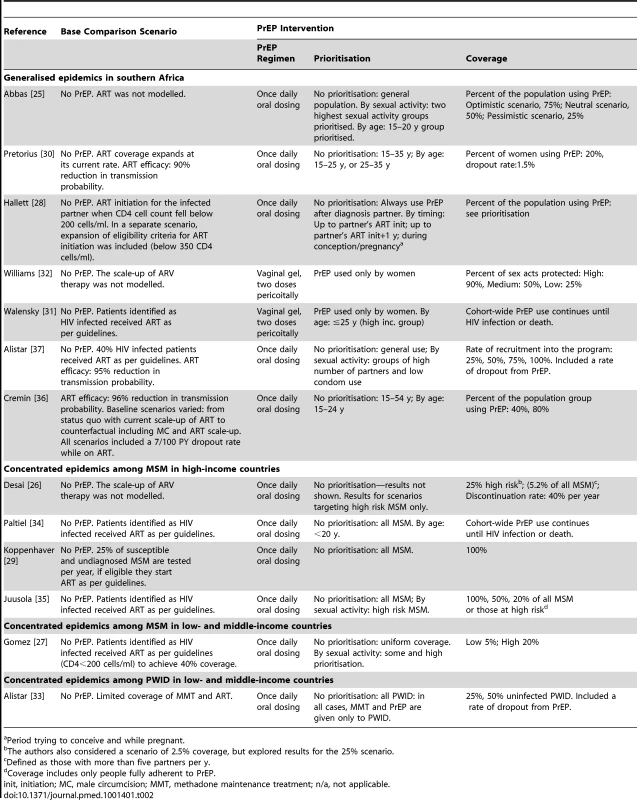
Period trying to conceive and while pregnant. Tab. 3. Impact: assumptions. 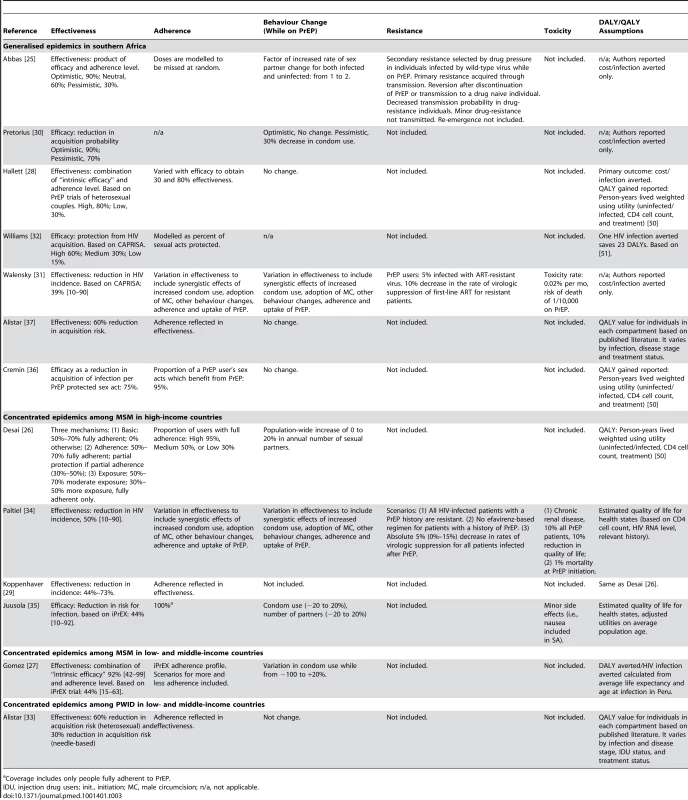
Coverage includes only people fully adherent to PrEP. Tab. 4. Cost: assumptions (US$ in publication). 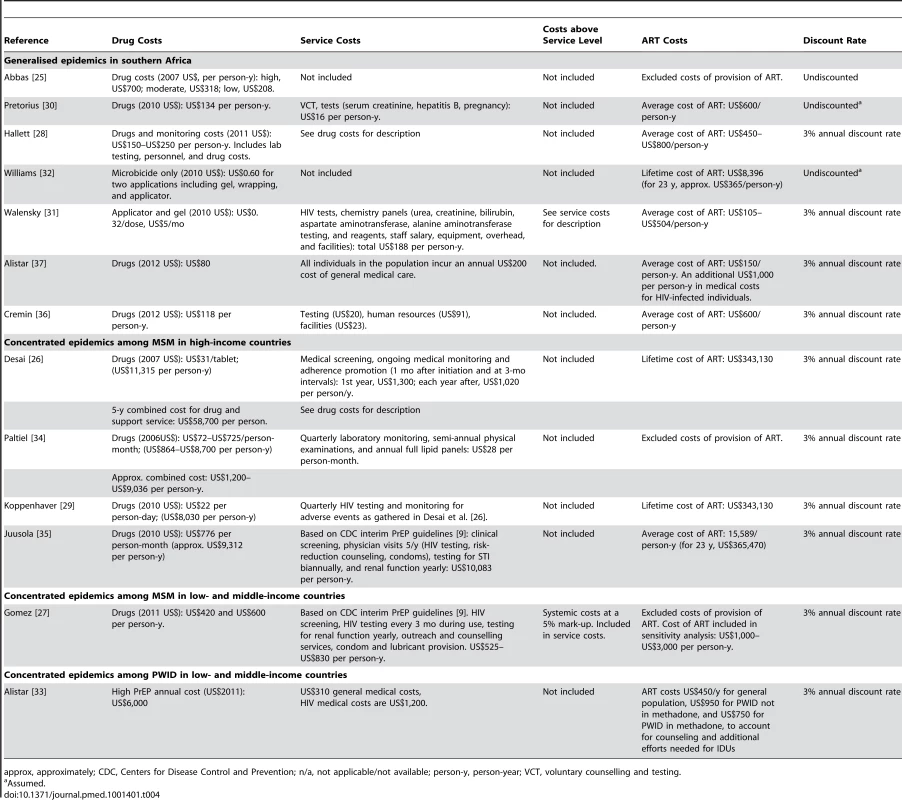
approx, approximately; CDC, Centers for Disease Control and Prevention; n/a, not applicable/not available; person-y, person-year; VCT, voluntary counselling and testing. In all models, the comparison scenario did not include PrEP and assumptions varied regarding current treatment scale-up: from no ART programme included [25],[26],[32] to ART coverage remaining stable at a current level [27],[29],[31],[34],[35] or an ongoing ART programme coverage expansion [28],[30],[33],[36],[37]. While most of the studies looked at systemic PrEP (daily oral dosing), two studies in South Africa looked at vaginal gels [31],[32]. Coverage assumptions were stated as scenarios. The criteria used to characterise priority populations varied among the studies, including high risk of acquisition (defined by sexual activity, condom use, or HIV incidence) [25]–[27],[35],[37], age [25],[30],[31],[34],[36], and timing of PrEP use [28] in relation to users' life events (Table 2).
All models were transmission models, except for two Markov simulations [31],[34]. Efficacy and effectiveness estimates varied from estimated ranges that were assumed prior to the results from clinical trials and had wide ranges (from 10% to 90%) [25],[26],[30],[33],[34] to estimates available directly from clinical trials [27]–[29],[31],[32],[35]–[37]. Several authors interpreted effectiveness as being dependent on the product efficacy and the individual-level adherence, specifically modelling this interaction [25]–[29],[32],[36]. Adherence assumptions varied from random [25] to profiles based on observations from published trials [27]–[29],[32]. Potential behaviour change following the introduction of a PrEP programme was included in the models as an increase in the number of sexual partners [25],[26], changes in condom use [27],[30], or both [35]. Drug resistance associated with PrEP use was explicitly modelled in one study [25], while in two further studies it was represented as a decrease in the rate of virologic suppression while on subsequent treatment [31],[34]. The studies did not assume any reduction in the quality of life or disability weights due to PrEP use, with the exception of three studies where toxicity to PrEP was addressed through a reduction in the quality of life and/or an excess fatality rate among PrEP users (Table 3) [31],[34],[35].
The majority of studies presented costs for PrEP programmes including drugs and monitoring costs, except for two studies that included drug costs only [25],[32]. Costs above service level were only included in two studies, as overheads [31] or a mark-up percentage of 5% [27]. Overall PrEP programme costs were consistent among studies by setting and ranged from high in the USA (between US$8,000 and US$12,000 per person-year) to low in South Africa (between US$80 to US$250). All cost estimates were driven by the cost of drugs. Three studies in the USA [26],[29],[35] and six in South Africa [28],[30]–[32],[36],[37] included averted ART costs. Ranges of estimated cost of ART were consistent among studies and context-specific (<US$1,000 per person-year in South Africa to >US$15,000 per person-year in the USA) (Table 4).
We present all cost-effectiveness estimates in Table 5 by epidemiological context and scenario modelled.
Tab. 5. Cost-effectiveness estimates by scenario. 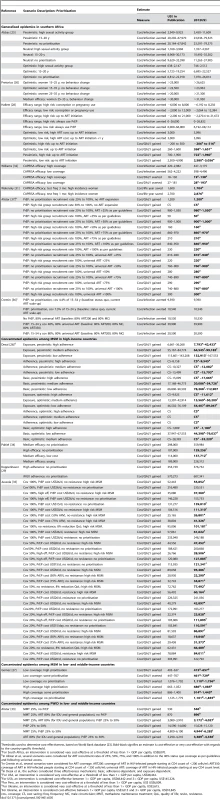
Thresholds used to determine cost-effectiveness, based on World Bank database [23]. Bold-black signifies an estimate is cost-effective or very cost-effective with regards to the country-specific threshold. Generalised Epidemics in Southern Africa (n = 7)
Studies on topical PrEP and two studies on oral PrEP suggest the intervention to be cost-effective (topical PrEP: <200 US$/DALY [32], <3,000 US$/LYS [31]; oral PrEP: <5,000 US$/QALY [28], <2,800 US$/QALY [37]) using benchmarks for cost-effectiveness specific to South Africa [22]. Three studies reported cost/infection averted only, estimates ranging from US$1,000 to 39,900 [25],[30],[36].
For topical PrEP, the two studies presented different estimates of cost-effectiveness: less cost-effective in Walensky et al. [31] (<US$1,600–US$2,700/life year saved) than in Williams et al. [32] (<US$18–US$181/DALY averted) due to a more comprehensive set of assumptions in the former (i.e., inclusion of the above service level costs of providing PrEP, adverse outcomes, topical PrEP toxicity, and resistance as well as a lifelong use of PrEP and discounting) [31],[32]. Prioritisation to high-risk key populations (high incidence groups, such as young women in South Africa) and improvements in adherence maximised the effectiveness of a topical PrEP programme [31],[32].
For oral PrEP, the impact was estimated to be higher if PrEP was prioritised for use among people at higher risk of HIV acquisition compared to no prioritisation strategy in four of the five studies included (i.e., higher sexual activity groups in Abbas et al. [25], couples at higher risk in Hallett et al. [28], people with high number of partners and low condom use in Alistar et al. [37], and younger women in Pretorius et al. [30]). In Cremin et al. [36], the authors compared PrEP prioritised to 15 to 24 years old to no prioritisation (PrEP available to the total adult population: 15 to 54 years old) and found the impact of the two strategies was very similar. However, the group prioritised (15 to 24 years old) did not present the highest risk of infection in this population. The impact of prioritising by age may be more evident when the intervention is aimed at age groups where incidence peaks (in this case among the 25 - to 34-year age group).
Four studies analysed the interactions between oral PrEP and an expanding ART programme. Pretorius et al. found oral PrEP cost-effectiveness and its impact at population level to be considerably reduced if PrEP is added to the expanding ART programme [30]. Accordingly, Alistar et al. and Cremin et al. found that expanding ART coverage in this setting will be the more attractive strategy than investing in oral PrEP [36],[37]. However, Alistar et al. found PrEP to be cost saving, when delivered to individuals at greater risk of infection with no ART expansion [37]. Cremin et al. [36] found that a PrEP intervention was not cost-saving when implemented on top of a base case that included an 80% coverage of ART for people with CD4 counts of less than 200 cells/ml and male circumcision to be scaled up to 80%. Hallett et al. compared early ART to PrEP in HIV-serodiscordant couples, finding that if higher risk couples change their behaviour (for example through risk reduction counselling), earlier initiation of ART might become a cost-effective alternative to oral PrEP [28]. Assumptions about behavioural change (an increase in the number of partners) was a key driver of cost-effectiveness in Abbas et al. [25], while Pretorius et al. [30] found a lesser impact on cost-effectiveness following changes in condom use. This might be explained by the inclusion in Pretorius et al. of a background decrease in condom use with age, with older women tending to have less condom use. Hallett et al. did not include changes in behaviour due to oral PrEP introduction in their analyses. Resistance and toxicity levels did not significantly affect cost-effectiveness estimates [25],[31].
Concentrated Epidemics among MSM in the USA (n = 4)
Pre-iPrEX modelling studies estimated cost-effectiveness of PrEP interventions among MSM with mixed results in the USA. The cost per QALY gained presented by Paltiel et al. [34] was considerably higher (US$298,000/QALY gained) than that presented by Desai et al. [26] (from cost saving to a maximum of US$143,208/QALY gained). This difference is primarily due to the inclusion of benefits from reduced onward transmission in the latter. The authors of post-iPrEX studies are in agreement that PrEP use among populations of MSM in the USA could have a significant impact on the domestic HIV epidemic. However, Koppenhaver et al., while exploring only scenarios with no prioritisation, found a PrEP intervention not to be cost-effective [29]. Juusola et al. found PrEP to be cost-effective under certain assumptions (i.e., prioritisation scenarios and no prioritisation scenarios including high product effectiveness or low drug costs [US$15/day for oral PrEP to the equivalent of 50% or 75% the cost of ART]) [35]. Both studies concluded that a PrEP programme might not be affordable due to the high cost of drugs used for PrEP (US$8,000 to US$9,300 per person-years for PrEP drugs only) [29],[35]. In this setting, the benefits of PrEP were expected to be offset by relatively small increases in the number of partners in one study [26]. Conversely, resistance was not found to have a strong impact on cost-effectiveness estimates [34],[35]. Varying levels of toxicity to PrEP had the potential to counterbalance PrEP benefits in two studies [34],[35].
Concentrated Epidemics among MSM in Peru (n = 1)
PrEP could be a cost-effective addition to current prevention programmes in Peru for MSM populations (up to US$1,702/DALY averted) using benchmarks for cost-effectiveness specific to Peru [22]. However, even if PrEP drugs are expected to cost less than in settings such as the USA, a PrEP programme in this middle-income country might well require significant expenditure [27]. Behaviour change was not estimated to significantly affect cost-effectiveness estimates. It would result in detrimental effects (increases in the number of infections) only if PrEP efficacy and adherence were both assumed to be low [27]. The effect of prioritisation appears to be less pronounced in those scenarios with high coverage levels where saturation of coverage of those at highest risk occurs early during implementation and higher levels of coverage of lower-risk populations is achieved [27].
Concentrated Epidemics among People Who Inject Drugs in Ukraine (n = 1)
Alistar et al. [33] found PrEP not to be a cost-effective intervention in isolation from other HIV control interventions for use among populations of PWID (US$14,590–US$14,680/QALY gained) using benchmarks for cost-effectiveness specific to Ukraine [22]. PrEP is considerably less attractive when compared to the expansion of either methadone maintenance therapy (US$530/QALY gained) or to the combination of methadone maintenance therapy and ART for those in need (US$870/QALY gained) [33].
Discussion
This systematic review included 13 modelling studies estimating the cost and potential population-level impact of introducing a PrEP programme in generalised and concentrated epidemic settings. Our findings show that PrEP is estimated to have the potential to be a cost-effective addition to HIV prevention programmes in some settings. However, the cost-effectiveness of PrEP is likely to depend on considerations such as cost, the epidemic context, PrEP programme coverage and prioritisation strategies, as well as individual adherence levels and PrEP efficacy estimates.
To prevent heterosexual transmission in the generalised epidemics of southern Africa, PrEP is potentially a cost-effective intervention. Topical PrEP, in particular, could have a significant impact in South Africa, providing a much-needed female-initiated prevention option. However, it should be noted that funding PrEP while other potentially more cost-effective HIV prevention interventions remain under-funded may have high opportunity costs. In concentrated epidemics, such as MSM-driven epidemics both in Peru and in the USA, PrEP could have a substantial impact on the epidemic but may not be affordable at current drug prices. In Ukraine, expansion of ART coverage and methadone maintenance treatment programmes for PWID should be a first priority, with PrEP potentially added on within a combination prevention framework. However, evidence to date shows PrEP might not be cost-effective in this setting at current drug prices. Nevertheless, findings from the phase III Bangkok Tenofovir Study of PrEP among PWID will shed light on the efficacy estimates of PrEP in this population and inform future model estimates in similar epidemic contexts [38].
In all settings, the price of drugs is a limiting factor in terms of affordability of PrEP programmes as has been previously suggested [39],[40], and is key to determining cost-effectiveness. Moreover, the findings above predominately exclude important service and above service costs of providing PrEP (i.e., regular HIV testing and blood chemistry panels; the costs of possible adverse outcomes, including PrEP-related toxicity and potential drug resistance attributable to PrEP; and system-wide costs of implementing a PrEP programme). All of these should be considered to improve the validity and utility of estimates. Another key limitation among the studies is that the majority did not include savings in treatment and hospitalisation due to secondary infections averted. Although carrying significant uncertainties, the inclusion of these benefits allows a more informed consideration of potential PrEP benefits within broader programmatic planning for HIV prevention and care.
In the models reviewed, several prioritisation strategies were explored. Prioritisation by sexual activity characteristics to deliver PrEP to those populations at highest risk of HIV exposure improved the cost-effectiveness estimates. However, the extent to which prioritising populations at higher risk improves cost-effectiveness results in the models depends largely on the assumptions made about sexual mixing and risk heterogeneity. Extra costs related to the identification and engagement of priority populations were not included in any of the studies, neither were considerations in terms of economies of scale. Furthermore, as results from the enrolment phase of iPrEX Ole show (65% of trial participants decided to continue taking PrEP), not all individuals at higher risk are willing to use PrEP [41]. Identifying and meaningfully engaging those at highest risk in tailored HIV prevention strategies represents a significant challenge for decision makers, health care providers, and prevention advocates.
Prioritisation by age was a strategy advanced in several studies. In the studies reviewed, prioritisation by age group resulted in a lower cost-effectiveness benefit compared to prioritisation strategies based on self-reported risk behaviour [25],[30],[31],[34]. However, the former has the advantage of being straightforward to implement compared to a selection of potential PrEP users based on self-reported risk behaviour. In contexts such as South Africa and the USA, age prioritisation clearly would focus on those populations at higher risk of HIV acquisition. Another prioritisation strategy analysed in one study was the delivery of PrEP depending on the stage in users' lives. In reality, PrEP use will not need to be sustained throughout an individual's lifetime but may vary as his or her risk situation changes over time. People may opt to use PrEP during specific higher risk life periods, such as during periods of active sex work or when serodiscordant couples are trying to conceive a child [42],[43]. Understanding potential scenarios of PrEP use over the life cycle is essential for decision makers to be able to evaluate the possible impact of PrEP programmes in their local contexts. An additional consideration concerns intermittent PrEP. The first report of safety and adherence to an intermittent PrEP regimen in Kenya showed that among MSM and female sex workers adherence was lower than for daily dosing [44]. Results from two phase II trials underway in France [45] and the USA [46] will help inform adherence requirements and, should intermittent pre - and post-exposure dosing be proven effective, help tailor PrEP programmes to consumer demand [47].
Behavioural change due to PrEP use and adherence to PrEP were estimated to have potentially significant impacts on programme effectiveness. While the emergence of drug resistance due to PrEP programme scale-up and PrEP-related toxicity assumptions did not significantly affect cost-effectiveness estimates, improvement of drug resistance surveillance systems as well as effective adherence counselling will be essential components of PrEP programme implementation, in addition to behavioural counselling.
This review has several limitations. The geographical coverage of the studies reviewed is partial and both the impact and cost evaluations are highly setting-specific, limiting the generalisability of the findings. We were unable to perform a meta-analysis due to the variability across studies in reporting outcomes. Nevertheless, in order to compare cost-effectiveness estimates across settings, we used the thresholds proposed by the WHO-CHOICE Project and the Commission on Macroeconomics as a benchmark [22]. These standards are based on the GDP per capita, assuming that a society is willing to pay the equivalent of up to one GDP per capita (for highly cost-effective interventions) or between one and three times the GDP per capita (for a cost-effective intervention for a DALY averted, QALY saved, or LYS). This is a normative selection of cost-effectiveness thresholds, albeit regarded as useful from a decision analytic perspective [24].
It is worth noting that, with the exception of four studies in South Africa [28],[30],[36],[37], research comparing the potential trade-offs of earlier treatment for prevention versus PrEP remains an important gap in the literature that should be addressed, especially in concentrated epidemics. Cost-effectiveness studies that demonstrate where resources applied can have the greatest impact will help inform this complicated decision-making, but these are not the only considerations. The decision to include a PrEP option within the combination prevention package requires input from all strata of society. For instance, in contexts where universal access to ART for patients in need has not been achieved, PrEP programme planning processes will be challenged by concerns about social justice, equity, and affordability. This is in addition to the hurdles of overcoming the marginalisation, stigmatisation, and criminalisation of many of the populations that would most benefit from tailored HIV prevention programming that includes the choice of PrEP. Disentangling these issues will be critical for effective decision-making, as will the consideration of potential synergies between an expanded testing and treatment programme and a PrEP programme.
While the interest of donors for modelling studies that compare the cost-effectiveness of different HIV prevention methods is expected to increase [48], current evidence is already available to aid policy makers in assessing PrEP as a new prevention option. In this context, our review sheds light on the main considerations that decision makers need to address when judging the relevance of cost-effectiveness estimates of a potential PrEP programme and the potential gaps in the modelling evidence. Given that our review shows that setting and target population are critical drivers of cost-effectiveness, the next step is to conduct context-specific demonstration studies, including comprehensive cost analyses, of different prioritisation and adherence promotion strategies to ensure that the maximum benefit from the introduction of PrEP is realised within combination HIV prevention programmes.
Supporting Information
Zdroje
1. GrantRM, LamaJR, AndersonPL, McMahanV, LiuAY, et al. (2010) Preexposure chemoprophylaxis for HIV prevention in men who have sex with men. N Engl J Med 363 : 2587–2599.
2. BaetenJM, DonnellD, NdaseP, MugoNR, CampbellJD, et al. (2012) Antiretroviral prophylaxis for HIV prevention in heterosexual men and women. N Engl J Med 367 : 399–410.
3. ThigpenMC, KebaabetswePM, PaxtonLA, SmithDK, RoseCE, et al. (2012) Antiretroviral preexposure prophylaxis for heterosexual HIV transmission in Botswana. N Engl J Med 367 : 423–434.
4. Van DammeL, CorneliA, AhmedK, AgotK, LombaardJ, et al. (2012) Preexposure prophylaxis for HIV infection among African women. N Engl J Med 367 : 411–422.
5. NIH (2011) NIH modifies ‘VOICE’ HIV prevention study in women: oral tenofovir discontinued in clinical trial. Available: http://www.nih.gov/news/health/sep2011/niaid-28.htm). Bethesda: National Institute of Allergy and Infectious Diseases. Accessed 11 February 2013.
6. Facts Consortium (2013) FACTS001 Available: http://www.facts-consortium.co.za/. Accessed 11 February 2013.
7. Abdool KarimQ, Abdool KarimSS, FrohlichJA, GroblerAC, BaxterC, et al. (2010) Effectiveness and safety of tenofovir gel, an antiretroviral microbicide, for the prevention of HIV infection in women. Science 329 : 1168–1174.
8. MTN (2011) MTN statement on decision to discontinue use of tenofovir gel in VOICE, major prevention study in women. Available: http://www.mtnstopshiv.org/node/3909). Pittsburgh: Microbicide Trials Network. Accessed 11 February 2013.
9. CDC (2011) Interim guidance: preexposure prophylaxis for the prevention of hiv infection in men who have sex with men. MMWR Morb Mortal Wkly Rep 60 : 65–68.
10. McCormackS, FidlerS, FisherM (2012) The British HIV Association/British Association for Sexual Health and HIV Position Statement on pre-exposure prophylaxis in the UK. Int J STD AIDS 23 : 1–4.
11. The Consensus Committee SAHCS (2012) Southern African guidelines for the safe use of pre-exposure prophylaxis in men who have sex with men who are at risk for HIV infection. S Afr J HIV Med 13 : 40–55.
12. WHO (2012) Guidance on oral pre-exposure prophylaxis (PrEP) for serodiscordant couples, men and transgender women who have sex with men at high risk of HIV: recommendations for use in the context of demonstration projects. Available: http://www.who.int/hiv/pub/guidance_prep/en/index.html). Geneva. Accessed 11 February 2013.
13. CDC (2012) Interim guidance for clinicians considering the use of preexposure prophylaxis for the prevention of HIV infection in heterosexually active adults. MMWR Morb Mortal Wkly Rep 61 : 586–589.
14. Morgan D (2012) FDA panel backs Gilead's Truvada to prevent HIV. Washington (D.C.): Reuters: http://www.reuters.com/article/2012/05/11/us-usa-aids-truvada-idUSBRE84A00C20120511. Accessed 11 February 2013.
15. SchwartlanderB, StoverJ, HallettT, AtunR, AvilaC, et al. (2011) Towards an improved investment approach for an effective response to HIV/AIDS. Lancet 377 : 2031–2041.
16. WheelockA, EisingerichAB, GomezGB, GrayE, DybulMR, et al. (2012) Views of policymakers, healthcare workers and NGOs on HIV pre-exposure prophylaxis (PrEP): a multinational qualitative study. BMJ Open 2: e001234.
17. KrakowerD, MayerKH (2012) Engaging healthcare providers to implement HIV pre-exposure prophylaxis. Curr Opin HIV AIDS 7 : 593–599.
18. ArnoldEA, HazeltonP, LaneT, ChristopoulosKA, GalindoGR, et al. (2012) A qualitative study of provider thoughts on implementing pre-exposure prophylaxis (PrEP) in clinical settings to prevent HIV infection. PLoS One 7: e40603 doi:10.1371/journal.pone.0040603.
19. MoherD, LiberatiA, TetzlaffJ, AltmanDG (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 6: e1000097 doi:10.1371/journal.pmed.1000097.
20. DrummondMF, JeffersonTO (1996) Guidelines for authors and peer reviewers of economic submissions to the BMJ. The BMJ Economic Evaluation Working Party. BMJ 313 : 275–283.
21. KumaranayakeL (2000) The real and the nominal? Making inflationary adjustments to cost and other economic data. Health Policy Plan 15 : 230–234.
22. WHO-CHOICE (2012) Cost effectiveness thresholds: http://www.who.int/choice/costs/CER_thresholds/en/index.html. Accessed 11 February 2013.
23. World Bank (2012) GDP per capita (current US$). Available: http://data.worldbank.org/indicator/NY.GDP.PCAP.CD.
24. ShillcuttSD, WalkerDG, GoodmanCA, MillsAJ (2009) Cost effectiveness in low - and middle-income countries: a review of the debates surrounding decision rules. Pharmacoeconomics 27 : 903–917.
25. AbbasUL, AndersonRM, MellorsJW (2007) Potential impact of antiretroviral chemoprophylaxis on HIV-1 transmission in resource-limited settings. PLoS One 2: e875 doi:10.1371/journal.pone.0000875.
26. DesaiK, SansomSL, AckersML, StewartSR, HallHI, et al. (2008) Modeling the impact of HIV chemoprophylaxis strategies among men who have sex with men in the United States: HIV infections prevented and cost-effectiveness. AIDS 22 : 1829–1839.
27. GomezGB, BorquezA, CaceresCF, SeguraER, GrantRM, et al. (2012) The potential impact of pre-exposure prophylaxis for HIV prevention among men who have sex with men in Lima, Peru. PLoS Med 9: e1001323 doi:10.1371/journal.pmed.1001323.
28. HallettTB, BaetenJM, HeffronR, BarnabasR, de BruynG, et al. (2011) Optimal uses of antiretrovirals for prevention in HIV-1 serodiscordant heterosexual couples in South Africa: a modelling study. PLoS Med 8: e1001123 doi:10.1371/journal.pmed.1001123.
29. KoppenhaverRT, SorensenSW, FarnhamPG, SansomSL (2011) The cost-effectiveness of pre-exposure prophylaxis in men who have sex with men in the United States: an epidemic model. J Acquir Immune Defic Syndr 58: e51–e52.
30. PretoriusC, StoverJ, BollingerL, BacaerN, WilliamsB (2010) Evaluating the cost-effectiveness of pre-exposure prophylaxis (PrEP) and its impact on HIV-1 transmission in South Africa. PLoS One 5: e13646 doi:10.1371/journal.pone.0013646.
31. WalenskyRP, ParkJE, WoodR, FreedbergKA, ScottCA, et al. (2012) The cost-effectiveness of pre-exposure prophylaxis for HIV infection in South African women. Clin Infect Dis 54 : 1504–1513.
32. WilliamsBG, Abdool KarimSS, KarimQA, GouwsE (2011) Epidemiological impact of tenofovir gel on the HIV epidemic in South Africa. J Acquir Immune Defic Syndr 58 : 207–210.
33. Alistar SS (2011) TR2-2: Effectiveness and cost-effectiveness of oral pre-exposure prophylaxis for injection drug users in mixed HIV epidemics. Available: http://smdm.confex.com/smdm/2011ch/webprogram/Paper6553.html). 33rd Annual Meeting of the Society for Medical Decision Making, Hillsborough, USA. Accessed 11 February 2013.
34. PaltielAD, FreedbergKA, ScottCA, SchackmanBR, LosinaE, et al. (2009) HIV preexposure prophylaxis in the United States: impact on lifetime infection risk, clinical outcomes, and cost-effectiveness. Clin Infect Dis 48 : 806–815.
35. JuusolaJL, BrandeauML, OwensDK, BendavidE (2012) The cost-effectiveness of preexposure prophylaxis for HIV prevention in the United States in men who have sex with men. Ann Intern Med 156 : 541–550.
36. CreminI, AlsallaqR, DybulM, PiotP, GarnettG, et al. (2013) The new role of antiretrovirals in combination HIV prevention: a mathematical modelling analysis. Aids 27 : 447–458.
37. Alistar SS, Grant P, Bendavid E (2012) Paper #1081 - An economic analysis of ART and PrEP for HIV prevention: South Africa. Available: http://www.retroconference.org/2012b/Abstracts/44724.htm). 19th Conference on Retroviruses and Opportunistic Infections. Seattle. Accessed 11 February 2013.
38. MartinM, VanichseniS, SuntharasamaiP, SangkumU, ChuachoowongR, et al. (2011) Enrollment characteristics and risk behaviors of injection drug users participating in the Bangkok Tenofovir Study, Thailand. PLoS One 6: e25127 doi:10.1371/journal.pone.0025127.
39. KellerSB, SmithDM (2011) The price of tenofovir-emtricitabine undermines the cost-effectiveness and advancement of pre-exposure prophylaxis. Aids 25 : 2308–2310.
40. LeeDH, VielemeyerO (2011) Preexposure chemoprophylaxis for HIV prevention. N Engl J Med 364 : 1372–1373 author reply 1374-1375.
41. iPrEXOle (2012) Press release. Available: http://www.iprexnews.com/pdfswhatisnew/closedenrollment/iPrEx%20OLE%20Fully%20Enrolled%20-%2001JUL12.pdf. Accessed 11 February 2013.
42. VernazzaPL, GrafI, Sonnenberg-SchwanU, GeitM, MeurerA (2011) Preexposure prophylaxis and timed intercourse for HIV-discordant couples willing to conceive a child. Aids 25 : 2005–2008.
43. MatthewsLT, BaetenJM, CelumC, BangsbergDR (2010) Periconception pre-exposure prophylaxis to prevent HIV transmission: benefits, risks, and challenges to implementation. Aids 24 : 1975–1982.
44. MutuaG, SandersE, MugoP, AnzalaO, HabererJE, et al. (2012) Safety and adherence to intermittent pre-exposure prophylaxis (PrEP) for HIV-1 in African men who have sex with men and female sex workers. PLoS One 7: e33103 doi:10.1371/journal.pone.0033103.
45. IPERGAY: un essai ANRS (2013) ANRS Intervention Preventive de l'Exposition aux Risques avec et pour les GAYS. Available: http://www.ipergay.fr/. Accessed 11 February 2013.
46. HPTN (2013) HPTN 067: ADAPT study, a phase II, randomized, open-label, pharmacokinetic and behavioral study of the use of intermittent oral emtricitabine/tenofovir disoproxil fumarate pre-exposure prophylaxis (PrEP). http://www.hptn.org/research_studies/hptn067.asp. Accessed 11 February 2013.
47. EisingerichAB, WheelockA, GomezGB, GarnettGP, DybulMR, et al. (2012) Attitudes and acceptance of oral and parenteral HIV preexposure prophylaxis among potential user groups: a multinational study. PLoS One 7: e28238 doi:10.1371/journal.pone.0028238.
48. SimpsonKN (2010) Economic modeling of HIV treatments. Curr Opin HIV AIDS 5 : 242–248.
49. LingappaJR, KahleE, MugoN, MujugiraA, MagaretA, et al. (2009) Characteristics of HIV-1 discordant couples enrolled in a trial of HSV-2 suppression to reduce HIV-1 transmission: the partners study. PLoS One 4: e5272 doi:10.1371/journal.pone.0005272.
50. TengsTO, LinTH (2002) A meta-analysis of utility estimates for HIV/AIDS. Med Decis Making 22 : 475–481.
51. VerguetS, WalshJA (2010) Vaginal microbicides save money: a model of cost-effectiveness in South Africa and the USA. Sex Transm Infect 86 : 212–216.
Štítky
Interní lékařství
Článek vyšel v časopisePLOS Medicine
Nejčtenější tento týden
2013 Číslo 3- Berberin: přírodní hypolipidemikum se slibnými výsledky
- Léčba bolesti u seniorů
- Příznivý vliv Armolipidu Plus na hladinu cholesterolu a zánětlivé parametry u pacientů s chronickým subklinickým zánětem
- Červená fermentovaná rýže účinně snižuje hladinu LDL cholesterolu jako vhodná alternativa ke statinové terapii
- Jak postupovat při výběru betablokátoru − doporučení z kardiologické praxe
-
Všechny články tohoto čísla
- Malaria Burden and Artemisinin Resistance in the Mobile and Migrant Population on the Thai–Myanmar Border, 1999–2011: An Observational Study
- Getting Closer to a Fully Correctable and Connected Research Literature
- Surveillance Programme of IN-patients and Epidemiology (SPINE): Implementation of an Electronic Data Collection Tool within a Large Hospital in Malawi
- Using Routine Surveillance Data to Estimate the Epidemic Potential of Emerging Zoonoses: Application to the Emergence of US Swine Origin Influenza A H3N2v Virus
- Adapting Standards: Ethical Oversight of Participant-Led Health Research
- Strengthening the Expanded Programme on Immunization in Africa: Looking beyond 2015
- Changing Patterns in Place of Cancer Death in England: A Population-Based Study
- Policies and Initiatives Aimed at Addressing Research Misconduct in High-Income Countries
- Young Children's Probability of Dying Before and After Their Mother's Death: A Rural South African Population-Based Surveillance Study
- Research Misconduct in Low- and Middle-Income Countries
- Dissemination of Research Findings to Research Participants Living with HIV in Rural Uganda: Challenges and Rewards
- The Cost and Impact of Scaling Up Pre-exposure Prophylaxis for HIV Prevention: A Systematic Review of Cost-Effectiveness Modelling Studies
- Adjunctive Atypical Antipsychotic Treatment for Major Depressive Disorder: A Meta-Analysis of Depression, Quality of Life, and Safety Outcomes
- Number of Patients Studied Prior to Approval of New Medicines: A Database Analysis
- PLOS Medicine
- Archiv čísel
- Aktuální číslo
- Informace o časopisu
Nejčtenější v tomto čísle- Surveillance Programme of IN-patients and Epidemiology (SPINE): Implementation of an Electronic Data Collection Tool within a Large Hospital in Malawi
- Adjunctive Atypical Antipsychotic Treatment for Major Depressive Disorder: A Meta-Analysis of Depression, Quality of Life, and Safety Outcomes
- Strengthening the Expanded Programme on Immunization in Africa: Looking beyond 2015
- The Cost and Impact of Scaling Up Pre-exposure Prophylaxis for HIV Prevention: A Systematic Review of Cost-Effectiveness Modelling Studies
Kurzy
Zvyšte si kvalifikaci online z pohodlí domova
Současné možnosti léčby obezity
nový kurzAutoři: MUDr. Martin Hrubý
Všechny kurzyPřihlášení#ADS_BOTTOM_SCRIPTS#Zapomenuté hesloZadejte e-mailovou adresu, se kterou jste vytvářel(a) účet, budou Vám na ni zaslány informace k nastavení nového hesla.
- Vzdělávání



