-
Články
Top novinky
Reklama- Vzdělávání
- Časopisy
Top články
Nové číslo
- Témata
Top novinky
Reklama- Videa
- Podcasty
Nové podcasty
Reklama- Kariéra
Doporučené pozice
Reklama- Praxe
Top novinky
ReklamaStrengthening the Expanded Programme on Immunization in Africa: Looking beyond 2015
article has not abstract
Published in the journal: . PLoS Med 10(3): e32767. doi:10.1371/journal.pmed.1001405
Category: Policy Forum
doi: https://doi.org/10.1371/journal.pmed.1001405Summary
article has not abstract
Summary Points
-
There have been significant improvements in the performance of the Expanded Programme on Immunization (EPI) in Africa since its inception in 1974. However, there exist wide inter - and intra-country differences.
-
Successes such as the introduction of hepatitis B (HepB), Haemophilus influenzae type B (Hib), and meningococcal group A vaccines across the continent are milestones indicating growth and development in the right direction. Conversely polio and measles outbreaks, as well as high vaccine drop-out rates across the continent, indicate failures within the EPI system that require evidence-informed corrective interventions.
-
With the 2015 deadline for the Millennium Development Goals (MDGs) approaching, it is necessary for Africa to take stock, critically assess its position, take ownership of the regional and country-specific problems, and develop precise strategies to overcome the challenges identified.
-
There is need for increased immunisation systems strengthening, as many are plagued by weak infrastructure and shortage of skilled human resources. More affordable and adapted vaccines need to be made available.
-
Increased political and financial commitments from African governments are key factors for both maintaining current achievements and making additional progress for EPI in Africa.
Immunisation is amongst the most cost-effective public health interventions for reducing global child morbidity and mortality [1],[2]. The global effort to use vaccination as a public health intervention began when the World Health Organization (WHO) launched the Expanded Programme on Immunization (EPI) in 1974. Over the years there have been several international efforts to increase EPI coverage, including Universal Childhood Immunisation [3]; the Global Alliance for Vaccines and Immunisation (GAVI) [4]; Millennium Development Goals (MDGs) [5]; the Global Immunisation Vision and Strategy (GIVS) [6]; and most recently, the Global Vaccine Action Plan (GVAP) [7]. These initiatives, coupled with specific regional efforts such as the WHO African Region's EPI strategic plans of action for the periods 2001–2005 and 2006–2009 [8], and the Reach Every District (RED) approach [9], as well as the efforts of national EPIs, have seen global coverage with three doses of the diphtheria-tetanus-pertussis vaccine by 12 months of age (DTP3) rise from 5% in 1974 to 85% in 2010 [10],[11]. However, sub-Saharan Africa reached only 77% DTP3 coverage in 2010 [10]. Although DTP3 is an acknowledged indicator of EPI performance, it is important to understand other EPI indicators in Africa. Here, we assess immunisation systems strengthening, accelerated disease control efforts, and the introduction of new and underutilised vaccines across Africa.
Performance of Childhood Immunisation Programmes in Africa
Immunisation Systems Strengthening
Over the past four decades, extraordinary progress has been made in improving vaccination coverage in Africa (53 countries). According to WHO and the United Nations Children's Fund (UNICEF) coverage estimates, the number of countries with national DTP3 coverage of at least 80% increased from one (2%) in 1980, through 22 (42%) in 1990 and 17 (32%) in 2000, to 35 (67%) in 2010 (Figure 1) [10]. While 35 (67%) countries reported 80% national DTP3 coverage in 2010, only 16 (30%) countries reported at least 80% DTP3 coverage in 80% of their districts [10]. The DTP drop-out rate [((DTP1–DTP3)/DTP1)×100%] is also used for measuring EPI performance, where a DTP drop-out of less than 10% is considered good. Improvement in the proportion of countries having a DTP drop-out rate less than 10% was observed from 1974 till 1990, stagnating between 1990 and 2000, and then significantly increasing from 28% in 2000 to 60% in 2010 (p = 0.0013) [10].
Fig. 1. Colour-coded maps of Africa showing national coverage with the third dose of the diphtheria-tetanus-pertussis vaccine (DTP3) at the end of each decade since 1974. 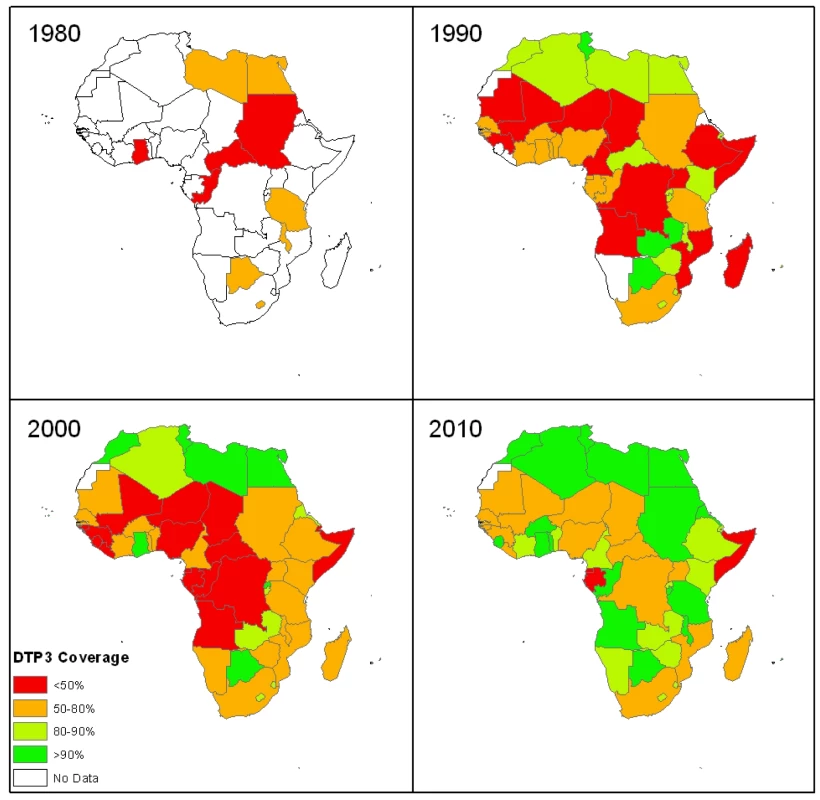
(Source of data: World Health Organization [10].) In 2010, one-fifth of African countries were yet to implement use of auto-disable syringes as well as adequate safety and waste disposal measures [10],[12]. Cold chain management in resource-poor settings, where electricity is non-existent or erratic, coupled with a lack of adequate trained staff to administer vaccines present major challenges in most African countries [13]. Furthermore, of those children who do receive the vaccines, many receive them late or at inappropriate timing and likely receive sub-optimal disease protection [14]–[16].
Improvements in immunisation spending in most African countries have predominantly been due to donor funds. In 2005, 49% (26/53) of countries reported that at least half of the costs of their routine vaccines were funded by government [10]. However, of those that established line items in their national budgets for rountine vaccines, over a third of them did not fund them, and those that had drawn financial plans did not utilise them to the degree expected [17]. Only 15% (8/53) of African countries reported on routine vaccines funded by government in 2010 [10].
The quality of immunisation data in many African countries is questionable. Various external evaluations have identified many inconsistencies in reported data suggesting that immunisation data monitoring remains weak in most African countries [18]–[20].
Accelerated Disease Control
Poliomyelitis, measles, yellow fever, and neonatal tetanus remain at the forefront of disease control efforts in Africa. By 2010, 81% (27/33) of the countries at risk for yellow fever had introduced the vaccination into their EPI schedules [21], compared to 27% (9/33) in 2000 [10].
Between 2000 and 2002, the number of African countries endemic with the wild poliovirus (WPV) decreased from 12 to two, and new WPV cases declined by 89% from 1,863 to 208 [17],[22]. However, following the cessation of polio immunisation for 12 months in the northern Nigerian state of Kano beginning in September 2003, WPV was imported into 29 previously polio-free African countries [23]. Religious and political leaders urged parents not to immunise their children as they believed the vaccine was contaminated with anti-fertility, HIV, and cancerous agents [24]. Since 2010, intensified efforts around the continent have resulted in WPV cases in Africa dropping by 47% from 657 in 2010 to 350 in 2011 [25]. Despite these efforts, in 2011, Nigeria remained endemic, transmission had re-established in Angola, Chad, and the Democratic Republic of the Congo (DRC), and ten other countries reported importations [26].
While routine measles vaccination had been established in most African countries by 1980, low coverage and outbreaks resulted in the initiation of catch-up and follow-up supplementary immunisation activities (SIAs) and case-based surveillance in the 1990s. A total of 24 million children in seven African countries were first reached during SIAs between 1996 and 2000 [27]. Between 2000 and 2010, all except four African countries conducted at least one catch-up SIA for children aged 9 months to 15 years, leading to a 92% reduction in measles mortality in sub-Saharan Africa between 2000 and 2008 [28]–[30]. Thereafter, due to low measles-containing vaccine (MCV) coverage and suboptimal follow-up SIAs, 27 countries had confirmed measles outbreaks between 2009 and 2011 [31].
In 2000, two-thirds (18/27) of the countries accounting for 90% of global neonatal tetanus cases were in Africa [32]. Thereafter, neonatal tetanus elimination was validated in 20 (38%) African countries in 2005, increasing to 27 (51%) in 2010 [10].
New and Underutilised Vaccines
There has been significant but slow progress in the introduction of new and underutilised vaccines in Africa. HepB and Hib vaccines were first licensed in the United States in 1981 and 1985, respectively. By 2005, 20 years later, the proportion of African countries having introduced HepB (70%) and Hib (26%) highlight the need to address underutilisation of available vaccines on the continent [10].
Although pneumonia and diarrhoea remain leading causes of child death [33], only seven African countries had introduced the rotavirus and/or pneumococcal conjugate (PCV) vaccines by 2010. These are “new vaccines” on the market that are costly and largely unaffordable for most African countries. Some progress is anticipated with an additional 16 countries and nine countries planning to introduce PCV and rotavirus vaccines, respectively, by 2013, with GAVI funding [10]. The Meningitis Vaccine Project (MVP) is a modern vaccine success story that saw the development of a new vaccine against meningococcal group A (the predominant cause of epidemic meningitis in the “meningitis belt”) being developed within 10 years. Negotiations between the MVP and partners around the world allowed for the development of this conjugate vaccine (MenAfriVac) in a low - and middle-income country (LMIC), India, at a cost of less than US$0.50/dose [34]. Within 2 years of licensure, six of the 25 countries at risk have already introduced MenAfriVac with GAVI support [33].
What Are the Implications for African Countries?
It is estimated that 1.5 million children died globally from vaccine-preventable diseases (VPDs) for which there were available WHO pre-qualified vaccines in 2010 [35]. Approximately 19.3 million children did not receive DTP3 worldwide in 2010, with more than one-third of these children living in Africa [36]. While Africa has made remarkable improvements in immunisation services, this agenda remains largely unfinished with large numbers of children remaining unreached, unvaccinated, under-vaccinated, and still dying from VPDs. While many countries have introduced HepB and Hib vaccines, the majority have not yet introduced PCV and rotavirus vaccines, and will not have done so by 2015. This continued failure to meet agreed targets thus far suggests that general and country-specific challenges with regards to immunisation programmes in Africa have not been fully identified, understood, and/or addressed effectively [37].
Paving the Way forward for an Improved EPI in Africa
With the 2015 deadline for the MDGs fast approaching [5], it is necessary for Africa to take stock, critically assess its position, take ownership of the regional and country-specific problems, and develop precise strategies to overcome the challenges identified. The annual cost per live birth for immunisation in LMICs is estimated to have increased from an average of US$6.00 in 2000 to US$25.00 in 2008 (due to HepB and Hib vaccines) and is likely to increase to US$58.00 if PCV and rotavirus vaccines are included [3]. Even with continued support from donors, political will as well as financial planning and commitment from African governments will be key factors for successful introduction and sustainability of new vaccines in EPI schedules in Africa. Issues of immunisation awareness, demand for immunisation, level of trust in health system, adequate human resources, access, timeliness of vaccinations, service delivery, poor infrastructure, and immunisation monitoring are among the many challenges faced by most African countries, all requiring evidence-based interventions [37]–[39]. Rwashana and colleagues from Uganda provide a good example of understanding the specific challenges and dynamics faced by an individual immunisation programme in the African context [40]. Identification of suitable and effective interventions to address identified problems within immunisation programmes is then of great importance to ensure best use of the limited resources available [41],[42]. Vaccine procurement and pricing strategies, vaccine adaptation to suit LMICs, as well as the establishment of vaccine production in LMICs remain essential components of helping to strengthen immunisation systems across Africa [13]. The polio boycott in northern Nigeria highlights the need for adequate communication about vaccines across Africa, the consequences of not urgently addressing concerns about perceived vaccine safety, as well as the need for prompt high-quality outbreak investigations [22]–[26].
We believe that in order for Africa to take advantage of the new decade of vaccines and extend the full benefits of immunisation to its citizens by 2020 and beyond, a critical assessment is a fundamental first step. The recently introduced GVAP is guided by six principles: country ownership, shared responsibility and partnership, equity, integration, sustainability, and innovation [7]. While this provides generalised strategies for attaining outlined goals, it is absolutely necessary for complementary tailor-made African approaches accompanied by robust monitoring and accountability frameworks.
Conclusion
African countries must be commended for giant steps made in EPI performance. However, there exist wide inter - and intra-country differences, with large numbers of African children remaining unreached, unvaccinated, under-vaccinated, and still dying from VPDs. Immunisation systems strengthening is essential, as most are under-staffed with inadequate resources to function efficiently. Issues of vaccine supply, financing, and sustainability in Africa require urgent attention. Increased political and financial commitment from governments as well as coordinated national and continental evidence-informed efforts by all immunisation stakeholders are needed to both maintain current achievements and make additional progress for EPI in Africa. African leaders must be held accountable for meeting agreed country targets and honouring international commitments made.
Zdroje
1. Centers for Disease Control and Prevention (2006) Vaccine preventable deaths and the Global Immunization Strategy, 2006–2015. MMWR Morb Mortal Wkly Rep 55 : 511–515.
2. BloomD (2011) The value of vaccination. Adv Exp Med Biol 697 : 1–8.
3. Okwo-BeleJM (2011) Cherian (2011) The Expanded Programme on Immunization: a lasting legacy of smallpox eradication. Vaccine (Suppl 1): D74–D79.
4. WittetS (2000) Introducing GAVI and the Global Fund for Children's Vaccines. Vaccine 19 : 385–386.
5. United Nations (2008) Millennium Development Goals: official list of MDG indicators. Available: http://unstats.un.org/unsd/mdg/Resources/Attach/Indicators/OfficialList2008.pdf. Accessed 8 February 2013.
6. BilousJ, EggersR, GasseF, JarrettS, LydonP, et al. (2006) A new global immunisation vision and strategy. Lancet 367 : 1464–1466.
7. Decade of Vaccines (DoV) Collaboration: draft global vaccine action plan. Available: http://www.dovcollaboration.org/action-plan/. Accessed 8 February 2013.
8. World Health Organization Regional Office for Africa. Immunization and vaccines development. Available: http://www.afro.who.int/en/clusters-a-programmes/ard/immunization-and-vaccines-development.html. Accessed 8 February 2013.
9. RymanT, MacauleyR, NshimirimanaD, TaylorP, ShimpL, et al. (2009) Reaching every district (RED) approach to strengthen routine immunization services: evaluation in the African region, 2005. J Public Health 32(1): 18–25.
10. World Health Organization. WHO Vaccine Preventable Diseases Monitoring System http://apps.who.int/immunization_monitoring/en/globalsummary/countryprofileselect.cfm. Accessed 8 February 2013. (Data as of July 2011.)
11. WiysongeCS, WaggieZ, RhodaL, HusseyG (2009) Vaccines for Africa (VACFA) website – an innovative immunisation advocacy tool. SAMJ 99(5): 275.
12. WHO, UNICEF, and UNFPA (2003) Safety of infections; WHO-UNICEF-UNFPA joint statement on the use of auto-disable syringes in immunization services. Available: http://www.who.int/vaccines-documents/DocsPDF99/www9948.pdf.
13. Medecins Sans Frontieres (2012) The right shot: extending the reach of affordable and adapted vaccines. Available: http://www.msfaccess.org/content/rightshot. Accessed 8 February 2013.
14. FadnesLT, NankabirwaV, SommerfeltH, TylleskarT, TumwineJK, et al. (2011) Is vaccination coverage a good indicator of age-appropriate vaccination? A prospective study from Uganda. Vaccine 29(19): 3564–3570.
15. BabiryeJN, EngebretsenIM, MakumbiF, FadnesLT, WamaniH, et al. (2012) Timeliness of childhood vaccinations in Kampala Uganda: a community-based cross-sectional study. PLoS ONE 7(4): e35432 doi:10.1371/journal.pone.0035432.
16. ClarkA, SandersonC (2009) Timing of children's vaccinations in 45 low-income and middle-income countries: an analysis of survey data. Lancet 373(9674): 1543–1549.
17. ArevshatianL, ClementsCJ, LwangaSK, MisoreAO, NdumbeP, et al. (2007) An evaluation of infant immunization in Africa: Is a transformation in progress? Bull World Health Organ 85 : 449–457.
18. RonveauxO, RickertD, HadlerS, GroomH, LloydJ, et al. (2005) The immunization data quality audit: verifying the quality and consistency of immunization monitoring systems. Bull World Health Organ 83(7): 503–510.
19. WiysongeCS, OfalJ (2009) Assessment of childhood immunisation coverage. Lancet 373(9673): 1427–1428.
20. Bosch-CapblanchX, RonveauxO, DoyleV, RemediosV, BchirA (2009) Accuracy and quality of immunization information systems in forty-one low income countries. Trop Med Int Health 14(1): 2–10.
21. Vaccine Preventable Diseases Unit WHO/African Region (2003) Yellow fever control in Africa: progress, issues and challenges. Vaccine Preventable Diseases Bulletin WHO/AFRO. January 2003, N° 031.
22. Global Polio Eradication Initiative (GPEI). Infected countries. Available: http://www.polioeradication.org/Infectedcountries.aspx. Accessed 27 August 2012.
23. Centers for Disease Control and Prevention (2012) Progress toward global polio eradication – Africa, 2011. MMWR Morb Mortal Wkly Rep 61(11): 190–194.
24. JegedeAS (2007) What led to the Nigerian Boycott of the Polio Vaccination Campaign? PLoS Med 4(3): e73 doi:10.1371/journal.pmed.0040073.
25. World Health Organization (2012) Tracking progress towards global polio eradication, 2010–2011. Wkly Epidemiol Rec 87 : 153–160.
26. World Health Organization Regional Office for Africa (2012) Eradicating polio in the African region: 2011 annual report. Available: http://www.afro.who.int/en/clusters-a-programmes/ard/immunization-and-vaccines-development/features/3619-eradicating-polio-in-the-african-region-2011-annual-report.html. Accessed 8 February 2013.
27. BiellikR, MademaS, TaoleA, KutsulukutaA, AlliesE, et al. (2002) First 5 years of elimination in southern Africa: 1996–2000. Lancet 359 : 1564–68.
28. Centers for Disease Control and Prevention (2009) Progress toward measles control – African region, 2001–2008. MMWR Morb Mortal Wkly Rep 58 : 1036–1041.
29. Centers for Disease Control and Prevention (2008) Progress toward measles mortality reduction and elimination – Eastern Mediterranean region, 1997–2007. MMWR Morb Mortal Wkly Rep 57 : 262–67.
30. MareshaB, FallA, EshetuM, SoslerS, AllemanM, et al. (2011) Measles mortality reduction and pre-elimination in the African region, 2001–2009. JID (Suppl 1): S198.
31. Centers for Disease Control and Prevention (2012) Progress in global measles control, 2000–2010. MMWR Morb Mortal Wkly Rep 61 : 73–78.
32. UNICEF, WHO, and UNFPA (2000) Maternal and neonatal tetanus elimination by 2005 – strategies for achieving and maintaining elimination. Available: http://www.unicef.org/health/files/MNTE_strategy_paper.pdf. Accessed 8 February 2013.
33. GAVI Alliance. New and underused vaccine support. Available: http://www.gavialliance.org/support/nvs/. Accessed 8 February 2013.
34. Meningitis Vaccine Project. Developing a meningococcal A conjugate vaccine. Available: http://www.meningvax.org/developing-conjugate-vaccine.php. Accessed 8 February 2013.
35. World Health Organization and UNICEF (2012) Global immunization data. Available: http://www.who.int/immunization_monitoring/Global_Immunization_Data.pdf. Accessed 8 February 2013.
36. WHO and UNICEF. Progress towards global immunization goals – 2011. Available: http://www.who.int/immunization_monitoring/data/SlidesGlobalImmunization.pdf. Accessed 8 February 2013.
37. WiysongeCS, UthmanOA, NdumbePM, HusseyGD (2012) Individual and contextual factors associated with low childhood immunisation coverage in sub-Saharan Africa: a multilevel analysis. PLoS ONE 7(5): e37905 doi:10.1371/journal.pone.0037905.
38. RaineyJ, WatkinsM, RymanT, SandhuP, BoA, BanerjeeK (2011) Reasons related to non-vaccination and under-vaccination of children in low and middle income countries: Findings from a systematic review of the published literature 1999-2009. Vaccine 29 : 8215–8221.
39. FavinM, SteinglassR, FieldsR, BanerjeeK, SawhneyM (2012) Why children are not vaccinated: a review of the grey literature. International Health 4 : 229–238 doi:10.1016/j.inhe.2012.07.004.
40. RwashanaAS, WilliamsDW, NeemaS (2009) System dynamics approach to immunization healthcare issues in developing countries: a case study of Uganda. Health Informatics J 15(2): 95–107.
41. Oyo-Ita A, Nwachukwu CE, Oringanje C, Meremikwi MM (2011) Interventions for improving coverage of child immunisation in low - and middle-income countries (Review). Cochrane Database of Systematic Reviews. Issue 7. Art. No.: CD008145. doi:10.1002/14651858.CD008145.pub2.
42. WiysongeCS, NgcoboNJ, JeenaPM, MadhiS, SchoubB, et al. (2012) Advances in childhood immunisation in South Africa: where to now? Programme managers' views and evidence from systematic reviews. BMC Public Health 12 : 578 doi:10.1186/1471-2458-12-578.
Štítky
Interní lékařství
Článek vyšel v časopisePLOS Medicine
Nejčtenější tento týden
2013 Číslo 3- Berberin: přírodní hypolipidemikum se slibnými výsledky
- Léčba bolesti u seniorů
- Příznivý vliv Armolipidu Plus na hladinu cholesterolu a zánětlivé parametry u pacientů s chronickým subklinickým zánětem
- Jak postupovat při výběru betablokátoru − doporučení z kardiologické praxe
- Červená fermentovaná rýže účinně snižuje hladinu LDL cholesterolu jako vhodná alternativa ke statinové terapii
-
Všechny články tohoto čísla
- Malaria Burden and Artemisinin Resistance in the Mobile and Migrant Population on the Thai–Myanmar Border, 1999–2011: An Observational Study
- Getting Closer to a Fully Correctable and Connected Research Literature
- Surveillance Programme of IN-patients and Epidemiology (SPINE): Implementation of an Electronic Data Collection Tool within a Large Hospital in Malawi
- Using Routine Surveillance Data to Estimate the Epidemic Potential of Emerging Zoonoses: Application to the Emergence of US Swine Origin Influenza A H3N2v Virus
- Adapting Standards: Ethical Oversight of Participant-Led Health Research
- Strengthening the Expanded Programme on Immunization in Africa: Looking beyond 2015
- Changing Patterns in Place of Cancer Death in England: A Population-Based Study
- Policies and Initiatives Aimed at Addressing Research Misconduct in High-Income Countries
- Young Children's Probability of Dying Before and After Their Mother's Death: A Rural South African Population-Based Surveillance Study
- Research Misconduct in Low- and Middle-Income Countries
- Dissemination of Research Findings to Research Participants Living with HIV in Rural Uganda: Challenges and Rewards
- The Cost and Impact of Scaling Up Pre-exposure Prophylaxis for HIV Prevention: A Systematic Review of Cost-Effectiveness Modelling Studies
- Adjunctive Atypical Antipsychotic Treatment for Major Depressive Disorder: A Meta-Analysis of Depression, Quality of Life, and Safety Outcomes
- Number of Patients Studied Prior to Approval of New Medicines: A Database Analysis
- PLOS Medicine
- Archiv čísel
- Aktuální číslo
- Informace o časopisu
Nejčtenější v tomto čísle- Surveillance Programme of IN-patients and Epidemiology (SPINE): Implementation of an Electronic Data Collection Tool within a Large Hospital in Malawi
- Adjunctive Atypical Antipsychotic Treatment for Major Depressive Disorder: A Meta-Analysis of Depression, Quality of Life, and Safety Outcomes
- Strengthening the Expanded Programme on Immunization in Africa: Looking beyond 2015
- The Cost and Impact of Scaling Up Pre-exposure Prophylaxis for HIV Prevention: A Systematic Review of Cost-Effectiveness Modelling Studies
Kurzy
Zvyšte si kvalifikaci online z pohodlí domova
Současné možnosti léčby obezity
nový kurzAutoři: MUDr. Martin Hrubý
Všechny kurzyPřihlášení#ADS_BOTTOM_SCRIPTS#Zapomenuté hesloZadejte e-mailovou adresu, se kterou jste vytvářel(a) účet, budou Vám na ni zaslány informace k nastavení nového hesla.
- Vzdělávání



