-
Články
Top novinky
Reklama- Vzdělávání
- Časopisy
Top články
Nové číslo
- Témata
Top novinky
Reklama- Videa
- Podcasty
Nové podcasty
Reklama- Kariéra
Doporučené pozice
Reklama- Praxe
Top novinky
ReklamaSocioeconomic Inequalities in Lung Cancer Treatment: Systematic Review and Meta-Analysis
Background:
Intervention-generated inequalities are unintended variations in outcome that result from the organisation and delivery of health interventions. Socioeconomic inequalities in treatment may occur for some common cancers. Although the incidence and outcome of lung cancer varies with socioeconomic position (SEP), it is not known whether socioeconomic inequalities in treatment occur and how these might affect mortality. We conducted a systematic review and meta-analysis of existing research on socioeconomic inequalities in receipt of treatment for lung cancer.Methods and Findings:
MEDLINE, EMBASE, and Scopus were searched up to September 2012 for cohort studies of participants with a primary diagnosis of lung cancer (ICD10 C33 or C34), where the outcome was receipt of treatment (rates or odds of receiving treatment) and where the outcome was reported by a measure of SEP. Forty-six papers met the inclusion criteria, and 23 of these papers were included in meta-analysis. Socioeconomic inequalities in receipt of lung cancer treatment were observed. Lower SEP was associated with a reduced likelihood of receiving any treatment (odds ratio [OR] = 0.79 [95% CI 0.73 to 0.86], p<0.001), surgery (OR = 0.68 [CI 0.63 to 0.75], p<0.001) and chemotherapy (OR = 0.82 [95% CI 0.72 to 0.93], p = 0.003), but not radiotherapy (OR = 0.99 [95% CI 0.86 to 1.14], p = 0.89), for lung cancer. The association remained when stage was taken into account for receipt of surgery, and was found in both universal and non-universal health care systems.Conclusions:
Patients with lung cancer living in more socioeconomically deprived circumstances are less likely to receive any type of treatment, surgery, and chemotherapy. These inequalities cannot be accounted for by socioeconomic differences in stage at presentation or by differences in health care system. Further investigation is required to determine the patient, tumour, clinician, and system factors that may contribute to socioeconomic inequalities in receipt of lung cancer treatment.
Please see later in the article for the Editors' Summary
Published in the journal: . PLoS Med 10(2): e32767. doi:10.1371/journal.pmed.1001376
Category: Research Article
doi: https://doi.org/10.1371/journal.pmed.1001376Summary
Background:
Intervention-generated inequalities are unintended variations in outcome that result from the organisation and delivery of health interventions. Socioeconomic inequalities in treatment may occur for some common cancers. Although the incidence and outcome of lung cancer varies with socioeconomic position (SEP), it is not known whether socioeconomic inequalities in treatment occur and how these might affect mortality. We conducted a systematic review and meta-analysis of existing research on socioeconomic inequalities in receipt of treatment for lung cancer.Methods and Findings:
MEDLINE, EMBASE, and Scopus were searched up to September 2012 for cohort studies of participants with a primary diagnosis of lung cancer (ICD10 C33 or C34), where the outcome was receipt of treatment (rates or odds of receiving treatment) and where the outcome was reported by a measure of SEP. Forty-six papers met the inclusion criteria, and 23 of these papers were included in meta-analysis. Socioeconomic inequalities in receipt of lung cancer treatment were observed. Lower SEP was associated with a reduced likelihood of receiving any treatment (odds ratio [OR] = 0.79 [95% CI 0.73 to 0.86], p<0.001), surgery (OR = 0.68 [CI 0.63 to 0.75], p<0.001) and chemotherapy (OR = 0.82 [95% CI 0.72 to 0.93], p = 0.003), but not radiotherapy (OR = 0.99 [95% CI 0.86 to 1.14], p = 0.89), for lung cancer. The association remained when stage was taken into account for receipt of surgery, and was found in both universal and non-universal health care systems.Conclusions:
Patients with lung cancer living in more socioeconomically deprived circumstances are less likely to receive any type of treatment, surgery, and chemotherapy. These inequalities cannot be accounted for by socioeconomic differences in stage at presentation or by differences in health care system. Further investigation is required to determine the patient, tumour, clinician, and system factors that may contribute to socioeconomic inequalities in receipt of lung cancer treatment.
Please see later in the article for the Editors' SummaryIntroduction
Lung cancer is the most commonly occurring cancer worldwide. In the USA and the UK it is the second most incident cancer [1],[2], as well as the most common cause of cancer mortality [2],[3]. Survival differs internationally. In the UK, fewer than 10% of those diagnosed with lung cancer survive for 5 years [3],[4], with higher survival rates found in Nordic countries [4],[5], the USA [2],[5], Australia, and Canada [4].
Lung cancers are classified into small cell (SCLC) and non-small cell (NSCLC) lung cancers. NSCLC is more common than SCLC and has a better survival rate [6]. National Institute for Health and Clinical Excellence (NICE) guidelines recommend radical surgery for stage I or II NSCLC [6]. Chemotherapy and radiotherapy are recommended for later-stage NSCLC patients and are the treatments of choice for SCLC [6]. Treatment intervention with surgery, chemotherapy, or radiotherapy has been shown to improve lung cancer survival [6].
Socioeconomic inequalities in incidence of, and survival from, the majority of cancers have been reported [1],[3],[7]. A recent non-systematic review revealed socioeconomic inequalities in receipt of treatment for colorectal cancer [8], and it has been suggested that socioeconomic differences in access to treatment might at least partially explain socioeconomic differences in survival [9]. Unintended variations in outcome that result from the way that health interventions are organised and delivered have been described as intervention-generated inequalities [10].
Incidence of lung cancer is higher [1],[11], and survival poorer [7], in the most deprived patient groups. However, it is not known whether socioeconomic inequalities in receipt of treatment exist for lung cancer and, if so, what contribution they make to overall socioeconomic inequalities in outcome. In order to explore the first of these questions, we undertook a systematic review and meta-analysis of cohort studies examining the association between socioeconomic position (SEP) and receipt of lung cancer treatment.
Methods
A protocol (see Text S2) was developed and systematic methods were used to identify relevant studies, assess study eligibility for inclusion, and evaluate study quality. The review is reported according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [12] (see Text S1 for PRISMA checklist).
Literature Search
The online databases of MEDLINE and EMBASE were searched up to September 2012 (see Table S1 for full search strategies). No language restriction was applied. A search of Scopus uncovered no further papers. Additional studies were identified by reviewing the reference lists of all included studies and by using a forward citation search to identify more recent studies that had cited included studies. EndNote X5 software was used to manage the references.
Study Eligibility
Studies that met the following criteria were included in the review: primary, cohort studies of participants with a primary diagnosis of lung cancer (ICD10 C33 or C34) reported separately from other cancers; published in a peer-reviewed journal; where at least one reported outcome was receipt of treatment (measured by rates or odds of receiving treatment); and where receipt of this outcome was reported by a measure of SEP. Any curative or palliative treatment for lung cancer including surgery, chemotherapy, and radiotherapy was included.
Studies where SEP was included as a descriptive variable or confounder, but where outcomes for receipt of treatment by SEP were not presented, were not eligible for inclusion, but the authors were contacted to determine whether relevant data were available that might allow for inclusion in the review.
Studies where multivariable analysis was conducted (and included control for a minimum of age and sex as confounders); receipt of treatment was compared to not receiving treatment; odds ratios (ORs) and 95% confidence intervals (CIs) of receipt of treatment in low compared to high SEP were calculated; and SEP was not further stratified by another variable, were considered suitable for inclusion in meta-analysis.
Acceptable measures of SEP were: area-based indices of deprivation (e.g., Index of Multiple Deprivation [IMD], Townsend Score, Carstairs Index); and area or individual measures of income, poverty, or education level.
Multiple papers using the same or overlapping study data were included. Sensitivity analyses were conducted including all eligible papers and using different combinations of included papers, but only data from the better quality or more detailed paper in each overlapping study group were included in the final meta-analyses. Sensitivity meta-analyses are included in the supplemental material.
Study Selection and Data Extraction
Studies obtained from the database searches were independently assessed by two researchers (LFF and HW) in three phases: title, abstract, and full paper screening. Any disagreements at any of the screening stages were resolved by discussion between the two researchers in the first instance and with a third reviewer (JA) if agreement could not be reached. Data extraction was carried out by LFF using an Access database pro-forma developed for this purpose, and double-checked by HW.
There is evidence to suggest that health insurance status is an important factor relating to access to lung cancer care in countries such as the USA that rely on insurance-based health care systems [13]. Insurance status is less relevant and rarely measured in most other countries. Therefore, three analytical categories were developed a priori: studies conducted in a universal health care system (UHCS), free at the point of access (similar to the UK); studies conducted in countries with primarily private insurance health care systems (non-UHCS, similar to the USA) [14]; and studies conducted in countries with social insurance health care systems (similar to many European countries). No studies were identified that fell into the third category.
Study Quality
A study quality tool, adapted from existing quality tools [15],[16], was used to divide studies into six quality categories, with 1 being the lowest, and 6 the highest, quality (see Text S3). Quality assessment was carried out by LFF and checked by HW.
Cohort studies reporting only univariable analysis are of lower quality in terms of their ability to control for confounding. Only studies conducting multivariable analysis (quality scores 3–6) were included in the meta-analysis. All studies that met the inclusion criteria were analysed in the narrative synthesis.
Statistical Analysis
Trends in receipt of treatment across SEP groups were described in the narrative analysis of all studies that met the inclusion criteria.
Meta-analysis of eligible studies was undertaken using Cochrane Collaboration Review Manager 5.1. Natural logs of the ORs and their standard errors (SEs) were calculated for use in forest plots. Random-effects meta-analysis of the odds of treatment in the lowest compared to the highest SEP group was conducted. Where a study reported the most deprived class as the comparator, reverse ORs were calculated. Studies that presented a single OR as either an OR for a one unit increase in deprivation score or incremental quintile increase in income were not included.
Subgroup analyses by treatment type and health care system were conducted. In meta-analyses where a “substantial” percentage [17] of the variability appeared to be due to the heterogeneity of the studies rather than to chance, further subgroup analyses by stage, histology, and quality score were conducted, where appropriate, in order to examine potential sources of heterogeneity. A funnel plot was used to assess potential publication bias.
Results
Included Papers/Studies
A total of 46 papers met the inclusion criteria and were included in the review (see the PRISMA flow diagram [Figure 1]). Twenty-eight papers were from UHCS countries (Tables 1 and 2). Of these, 19 UK papers examined 13 study populations, although as these included national and regional populations from different sources, there was some further population overlap. One UK paper also compared treatment in Scotland and Canada [18]. A further nine papers from Canada (2), Sweden (1), Australia (1), Italy (1), France (1), and New Zealand (3) were included. The three New Zealand papers all examined the same population.
Fig. 1. Flow diagram of study selection and exclusion. 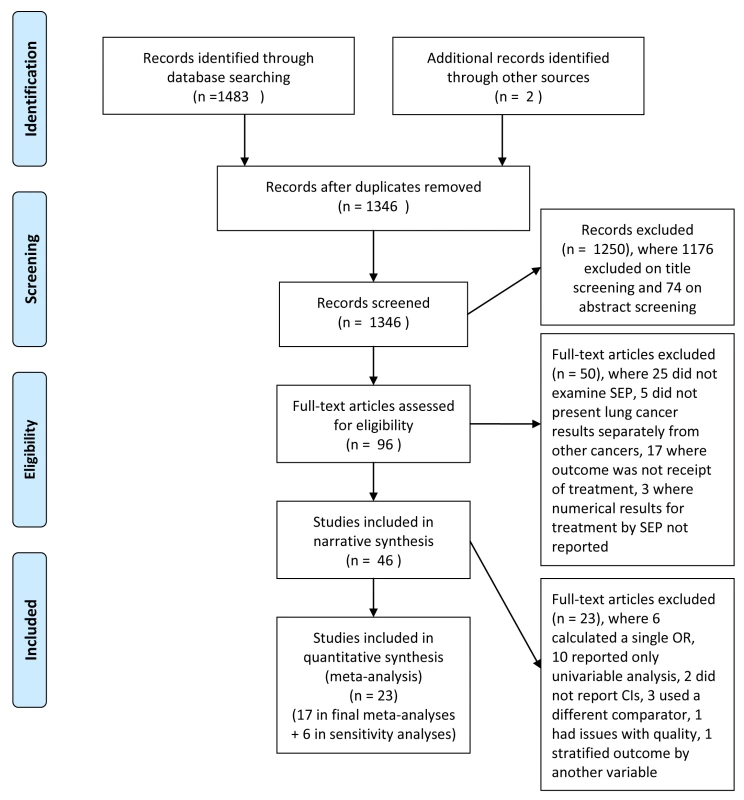
CI, confidence interval; SEP, socioeconomic position. Tab. 1. Characteristics of included studies potentially suitable for meta-analysis (universal health care systems). 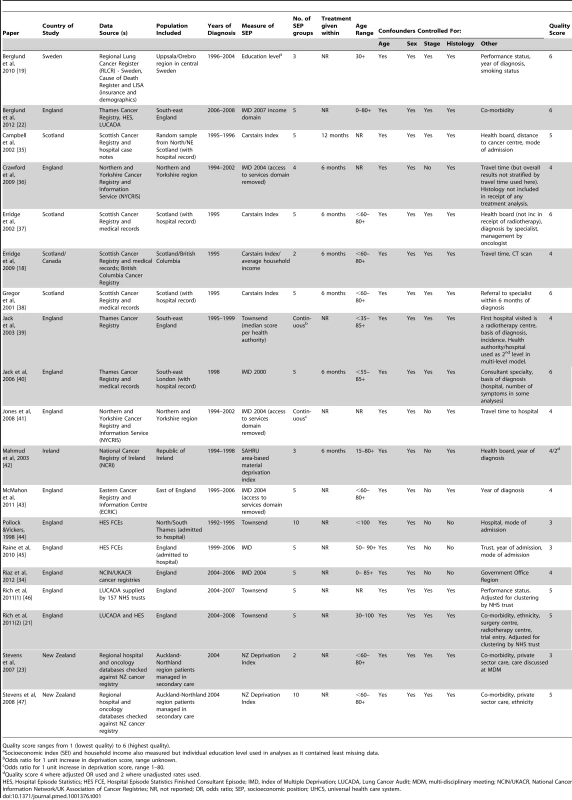
Quality score ranges from 1 (lowest quality) to 6 (highest quality). Tab. 2. Characteristics of included studies not suitable for meta-analysis (universal health care systems). 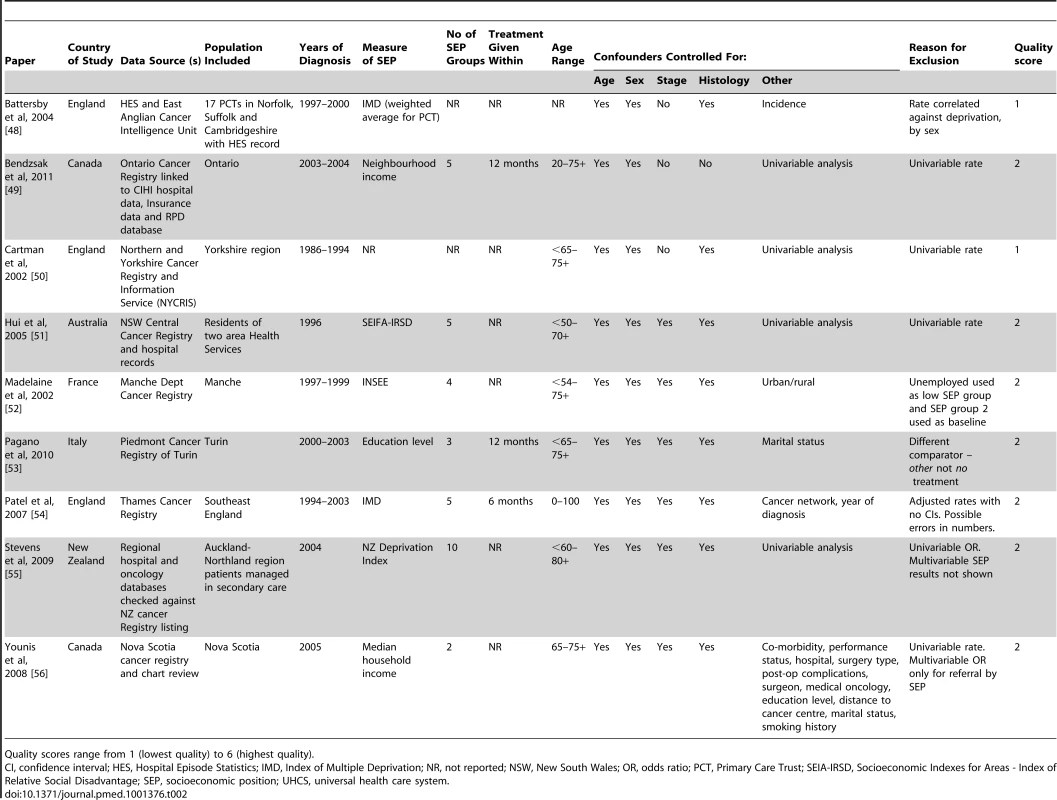
Quality scores range from 1 (lowest quality) to 6 (highest quality). Eighteen papers were from non-UHCSs, all of which were from the USA (Tables 3 and 4). The majority of non-UHCS papers used sub-groups of the National Cancer Institute's Surveillance, Epidemiology and End Results (SEER) database population and, again, some population overlap was found.
Tab. 3. Characteristics of included studies potentially suitable for meta-analysis (non-universal health care systems). 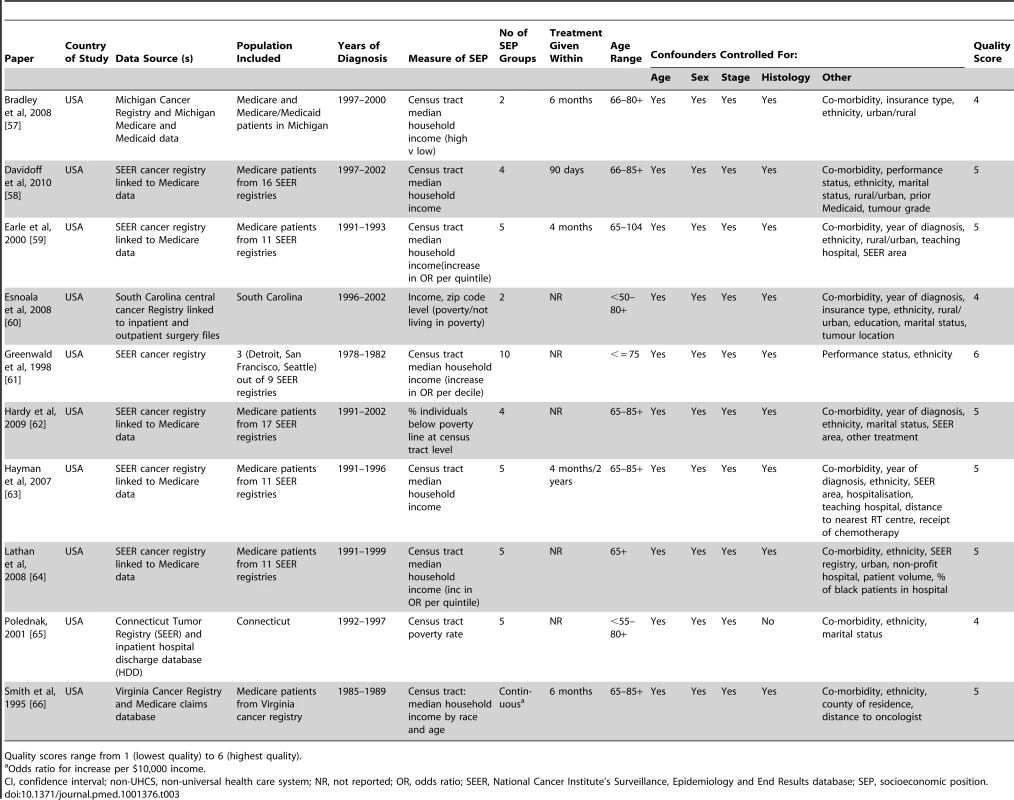
Quality scores range from 1 (lowest quality) to 6 (highest quality). Tab. 4. Characteristics of included studies not suitable for meta-analysis (non-universal health care systems). 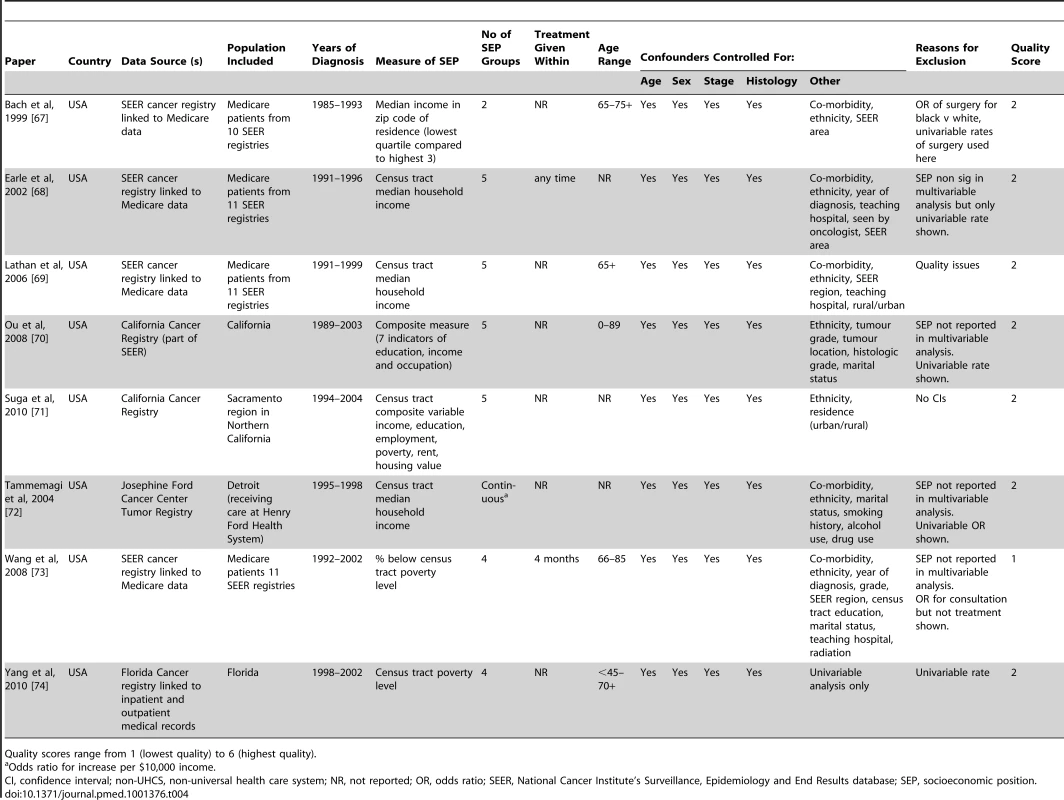
Quality scores range from 1 (lowest quality) to 6 (highest quality). An individual measure of SEP (education level) was used in one study [19]. All other studies used area-level measures of deprivation, income, poverty, or education level.
In terms of quality, the non-UHCS studies that carried out multivariable analyses had better control for confounding than did UHCS studies, as they tended to stratify by stage and histology. However, half of the non-UHCS papers used a Medicare-only population aged over 65, and so were more restrictive in population terms than the UHCS studies.
Twenty-nine papers met the criteria for meta-analysis—19 from UHCSs and 10 from non-UHCSs. However, six studies that examined receipt of treatment in low compared to high SEP presented the results as a single OR and so could not be included in the meta-analyses. Seventeen studies were included in the final meta-analyses and a further six in the sensitivity meta-analyses.
Surgery
Thirty-one papers (29 study populations) included receipt of surgery as an outcome—18 UHCS papers (15 study populations) and 13 non-UHCS papers (14 study populations) (Tables 5 and 6). Of the papers that reported measures of significance (CIs or p-values), 20 out of 27 (74%) reported that lower SEP was significantly associated with lower likelihood of surgery when comparing the lowest with the highest SEP group, although three of these 20 papers did not find a significant trend across groups.
Tab. 5. Likelihood of receipt of surgery by SEP group (universal health care systems). 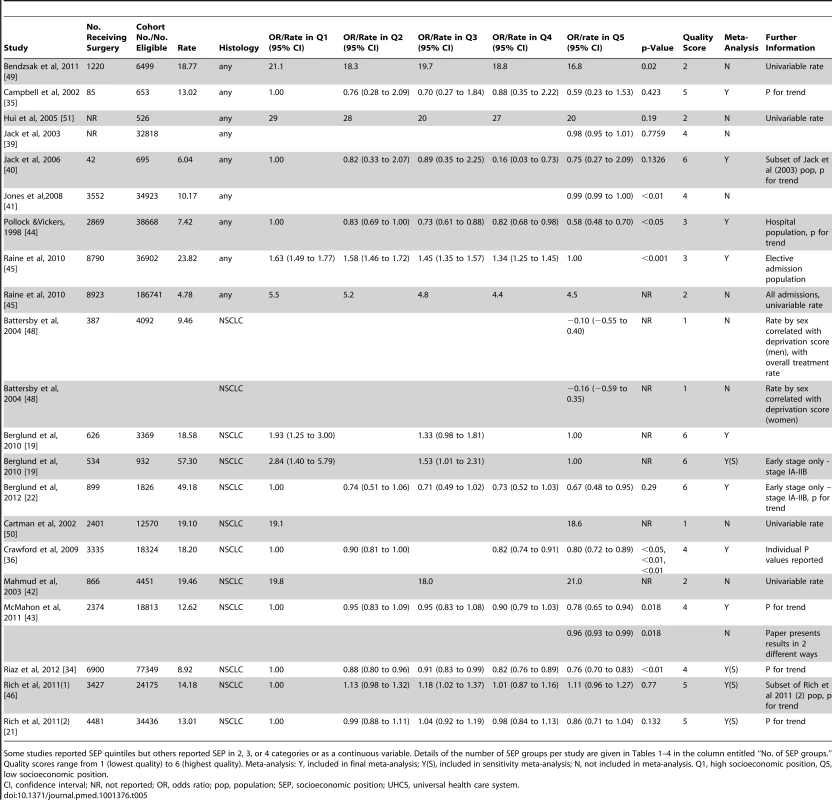
Some studies reported SEP quintiles but others reported SEP in 2, 3, or 4 categories or as a continuous variable. Details of the number of SEP groups per study are given in Tables 1–4 in the column entitled “No. of SEP groups.” Quality scores range from 1 (lowest quality) to 6 (highest quality). Meta-analysis: Y, included in final meta-analysis; Y(S), included in sensitivity meta-analysis; N, not included in meta-analysis. Q1, high socioeconomic position, Q5, low socioeconomic position. Tab. 6. Likelihood of receipt of surgery by SEP group (non-universal health care systems). 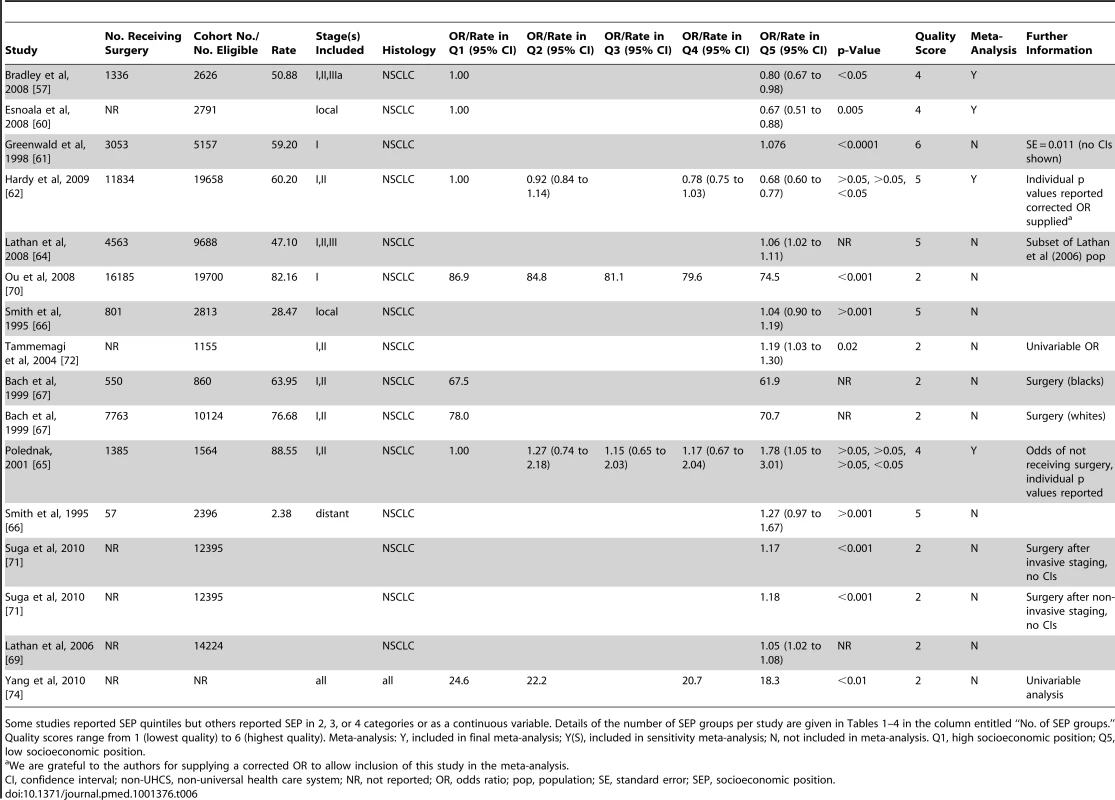
Some studies reported SEP quintiles but others reported SEP in 2, 3, or 4 categories or as a continuous variable. Details of the number of SEP groups per study are given in Tables 1–4 in the column entitled “No. of SEP groups.” Quality scores range from 1 (lowest quality) to 6 (highest quality). Meta-analysis: Y, included in final meta-analysis; Y(S), included in sensitivity meta-analysis; N, not included in meta-analysis. Q1, high socioeconomic position; Q5, low socioeconomic position. Meta-analysis of all 16 populations that were suitable for inclusion showed a significant negative effect of lower SEP on the likelihood of receiving surgery: OR = 0.72 (95% CI 0.65 to 0.80), p<0.001, I2 = 80% (Figure S1). Including only non-overlapping study populations (n = 12) gave a similar result: OR = 0.68 (95% CI 0.63 to 0.75), p<0.001, I2 = 53% (Figure 2). Similar results were also seen for the subgroup of eight papers including NSCLC patients only (OR = 0.73 [95% CI 0.68 to 0.80] p<0.001, I2 = 24%) (Figure S2) and with further stratification by health care system; NSCLC (UHCS): OR = 0.75 (95% CI 0.66 to 0.85), p<0.001, I2 = 29%; NSCLC (non-UHCS, early stage only, co-morbidity included): OR = 0.71 (95% CI 0.64 to 0.78) p<0.001; I2 = 2% (Figure 2).
Fig. 2. Meta-analysis of odds of receipt of surgery in low versus high SEP. 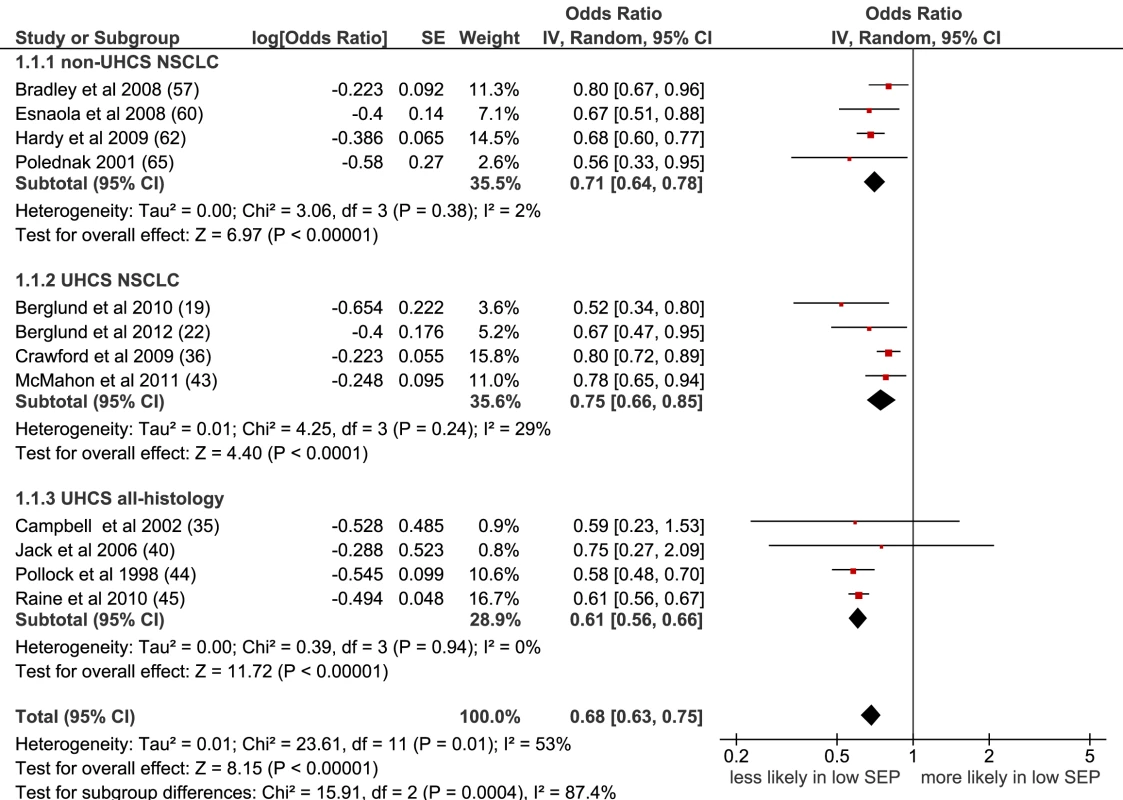
CI, confidence interval; non-UHCS, non-universal health care system; NSCLC, non-small cell lung cancer; OR, odds ratio; SE, standard error; SEP, socioeconomic position; UHCS, universal health care system. Lower SEP was associated with a lower likelihood of receiving lung cancer surgery, in both types of health care system, and in studies where histology and stage at diagnosis were taken into account.
Chemotherapy
Twenty-three papers included chemotherapy as an outcome—14 UHCS papers (12 populations) and nine non-UHCS papers (10 populations) (Tables 7 and 8). Of the 21 papers that reported measures of significance, 15 (71%) reported that lower SEP was significantly associated with lower likelihood of receipt of chemotherapy.
Tab. 7. Likelihood of receipt of chemotherapy by SEP group (universal health care systems). 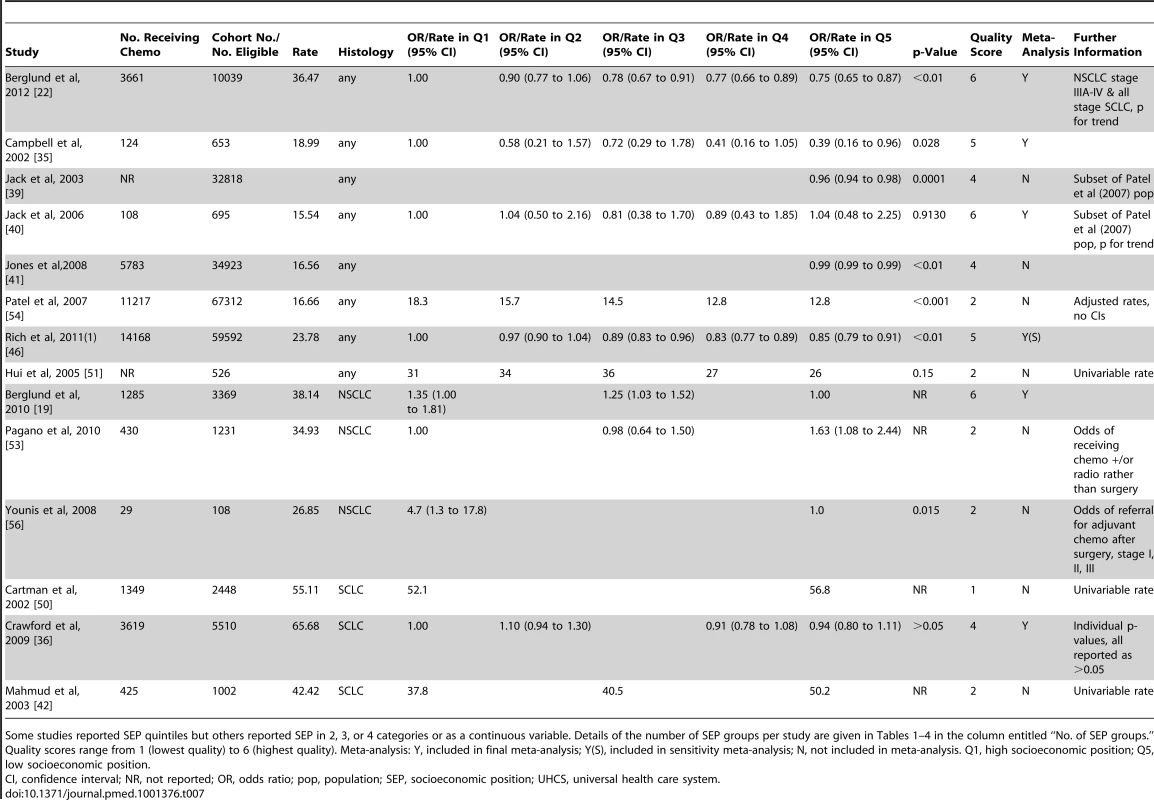
Some studies reported SEP quintiles but others reported SEP in 2, 3, or 4 categories or as a continuous variable. Details of the number of SEP groups per study are given in Tables 1–4 in the column entitled “No. of SEP groups.” Quality scores range from 1 (lowest quality) to 6 (highest quality). Meta-analysis: Y, included in final meta-analysis; Y(S), included in sensitivity meta-analysis; N, not included in meta-analysis. Q1, high socioeconomic position; Q5, low socioeconomic position. Tab. 8. Likelihood of receipt of chemotherapy by SEP group (non-universal health care systems). 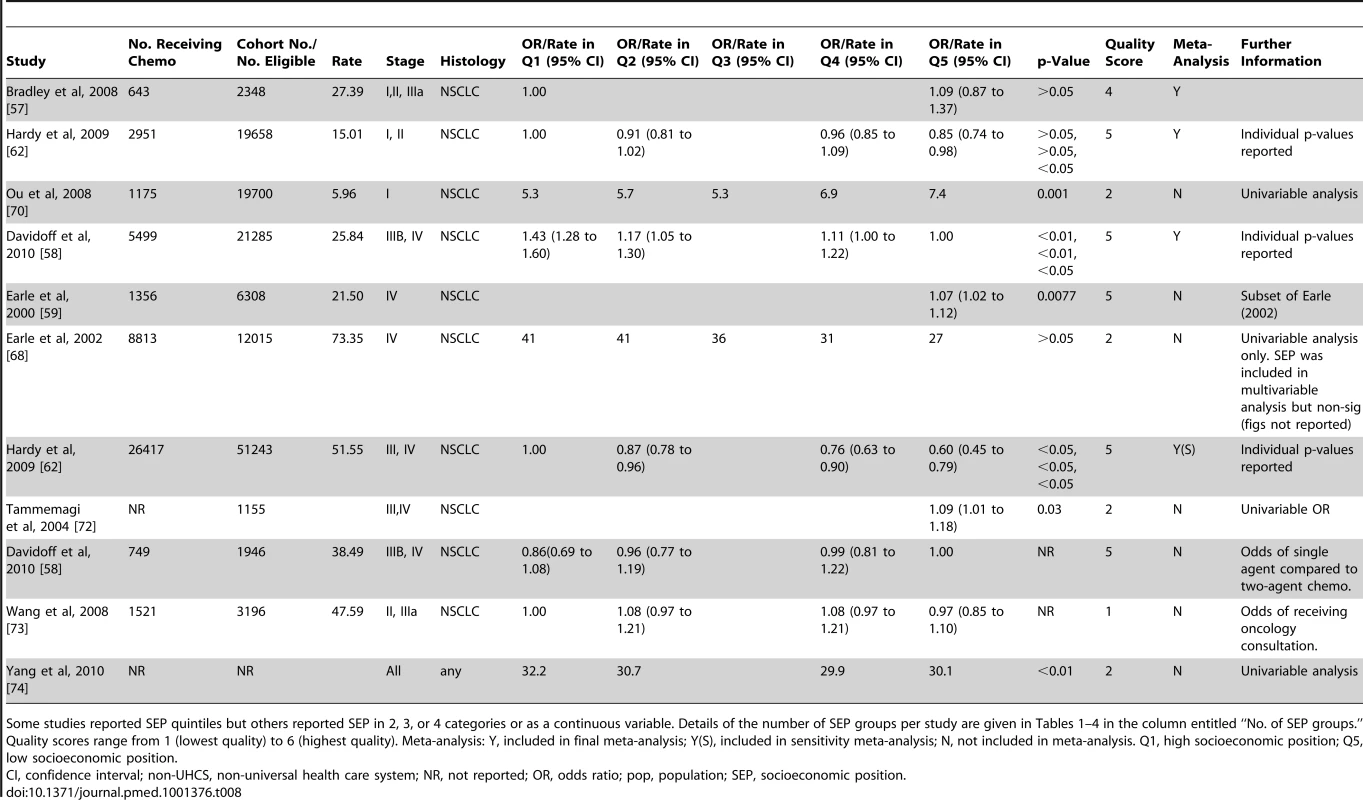
Some studies reported SEP quintiles but others reported SEP in 2, 3, or 4 categories or as a continuous variable. Details of the number of SEP groups per study are given in Tables 1–4 in the column entitled “No. of SEP groups.” Quality scores range from 1 (lowest quality) to 6 (highest quality). Meta-analysis: Y, included in final meta-analysis; Y(S), included in sensitivity meta-analysis; N, not included in meta-analysis. Q1, high socioeconomic position; Q5, low socioeconomic position. Meta-analysis of the ten populations that were suitable for inclusion found a significant negative effect of lower SEP on the likelihood of receiving chemotherapy: OR = 0.81 (95% CI 0.73 to 0.89), p<0.001, I2 = 68% (Figure S3). Similarly, in a meta-analysis of the eight papers containing non-overlapping populations that were selected for inclusion, the odds of receiving chemotherapy were significantly lower for those with low SEP compared to those with high SEP (OR = 0.82 [95% CI 0.72 to 0.93], p = 0.003, I2 = 67%), overall. A similar pattern was found in UHCS (OR = 0.80 [95% CI 0.68 to 0.95], p = 0.01, I2 = 46%); and in non-UHCS settings (OR = 0.85 [95% CI 0.68 to 1.07], p = 0.16, I2 = 85%), although this did not reach significance (Figure 3).
Fig. 3. Meta-analysis of odds of receipt of chemotherapy in low versus high SEP. 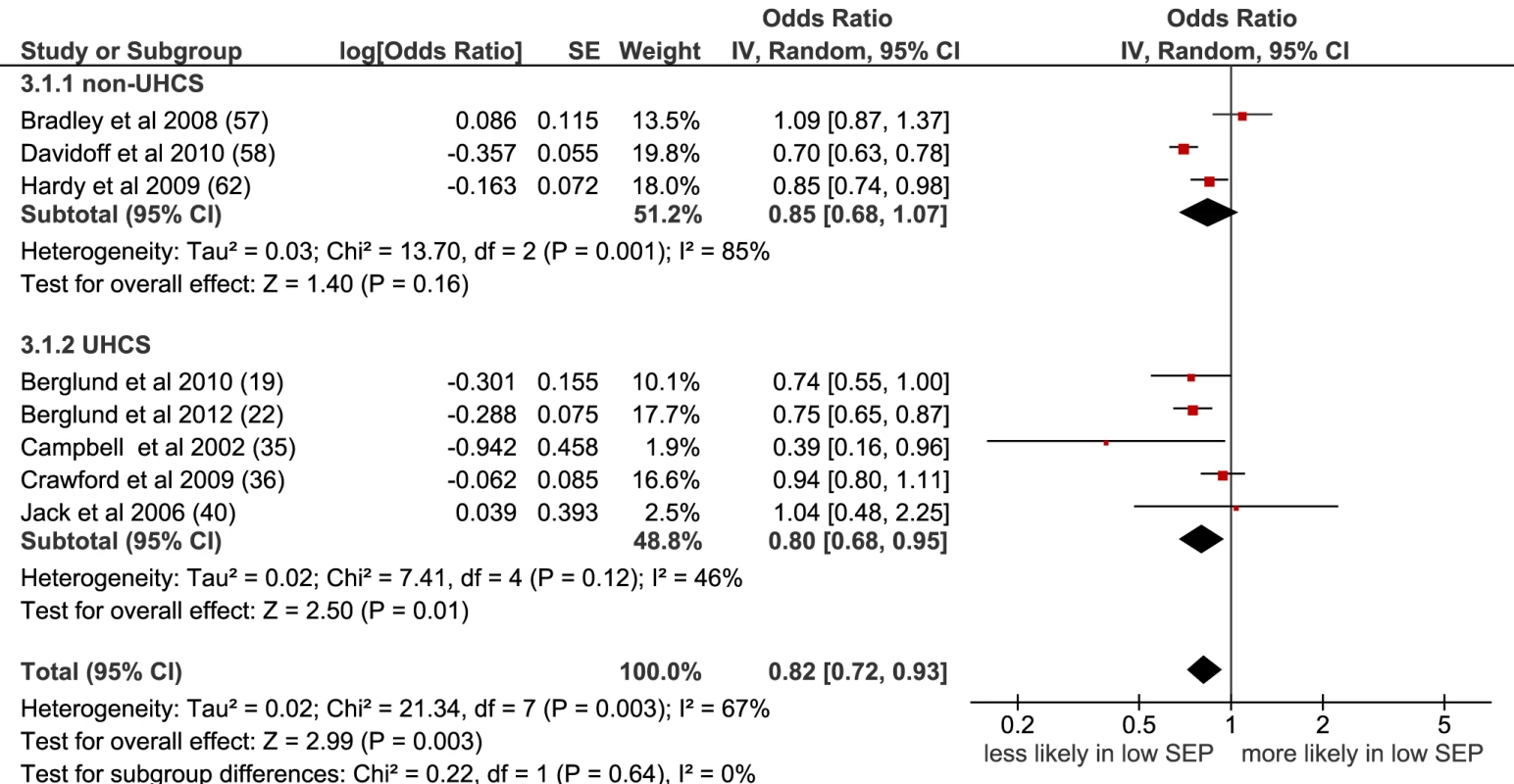
CI, confidence interval; non-UHCS, non-universal health care system; OR, odds ratio; SE, standard error; SEP, socioeconomic position; UHCS, universal health care system. Radiotherapy
Eighteen papers (18 populations) examined receipt of radiotherapy for lung cancer—12 in UHCS settings (11 populations) and six in non-UHCS settings (seven populations) (Tables 9 and 10). Only one UHCS study found an association between SEP and receipt of radiotherapy. The non-UHCS studies had very heterogeneous outcomes.
Tab. 9. Likelihood of receipt of radiotherapy by SEP group (universal health care systems). 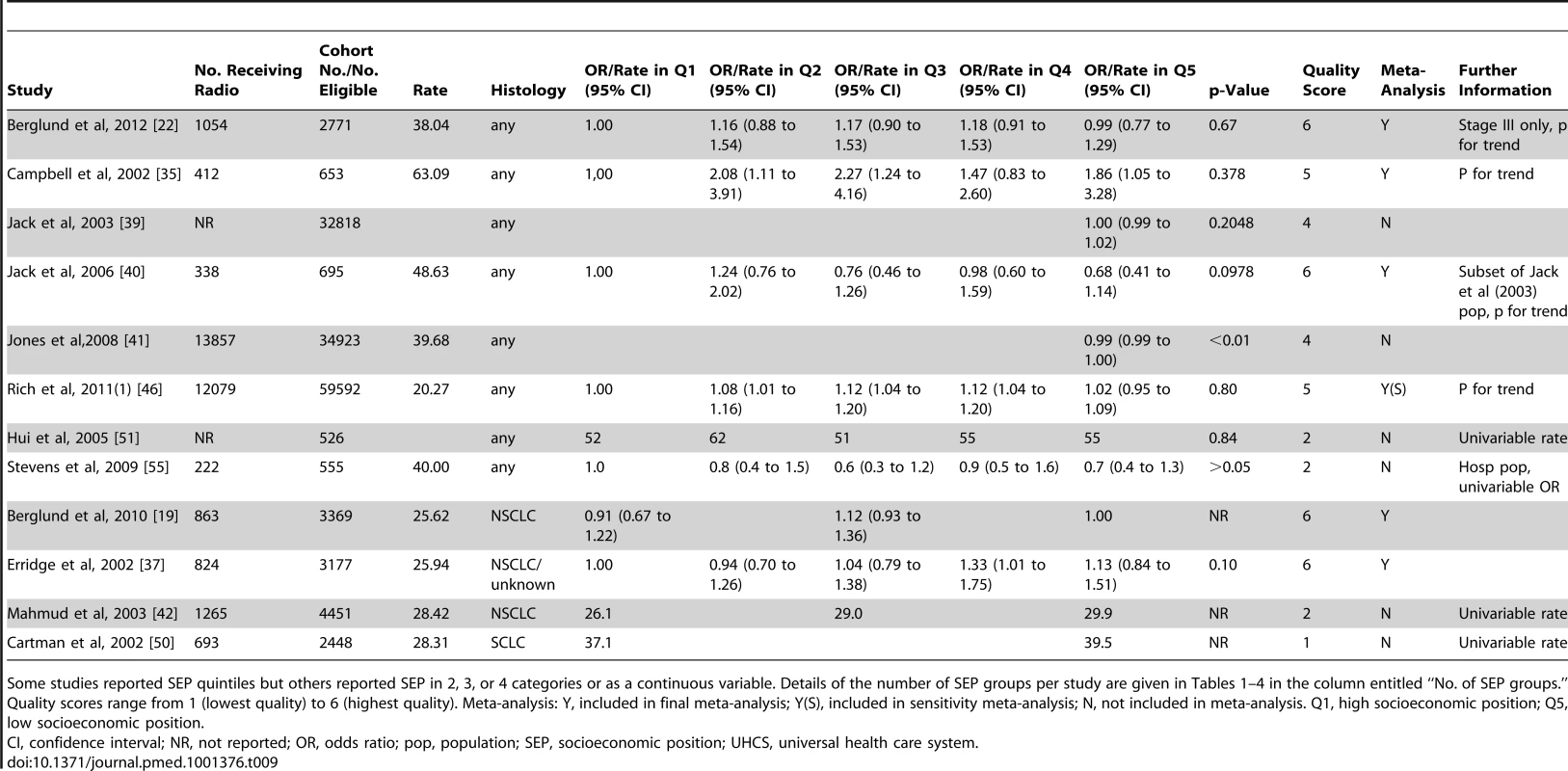
Some studies reported SEP quintiles but others reported SEP in 2, 3, or 4 categories or as a continuous variable. Details of the number of SEP groups per study are given in Tables 1–4 in the column entitled “No. of SEP groups.” Quality scores range from 1 (lowest quality) to 6 (highest quality). Meta-analysis: Y, included in final meta-analysis; Y(S), included in sensitivity meta-analysis; N, not included in meta-analysis. Q1, high socioeconomic position; Q5, low socioeconomic position. Tab. 10. Likelihood of receipt of radiotherapy by SEP group (non-universal health care systems). 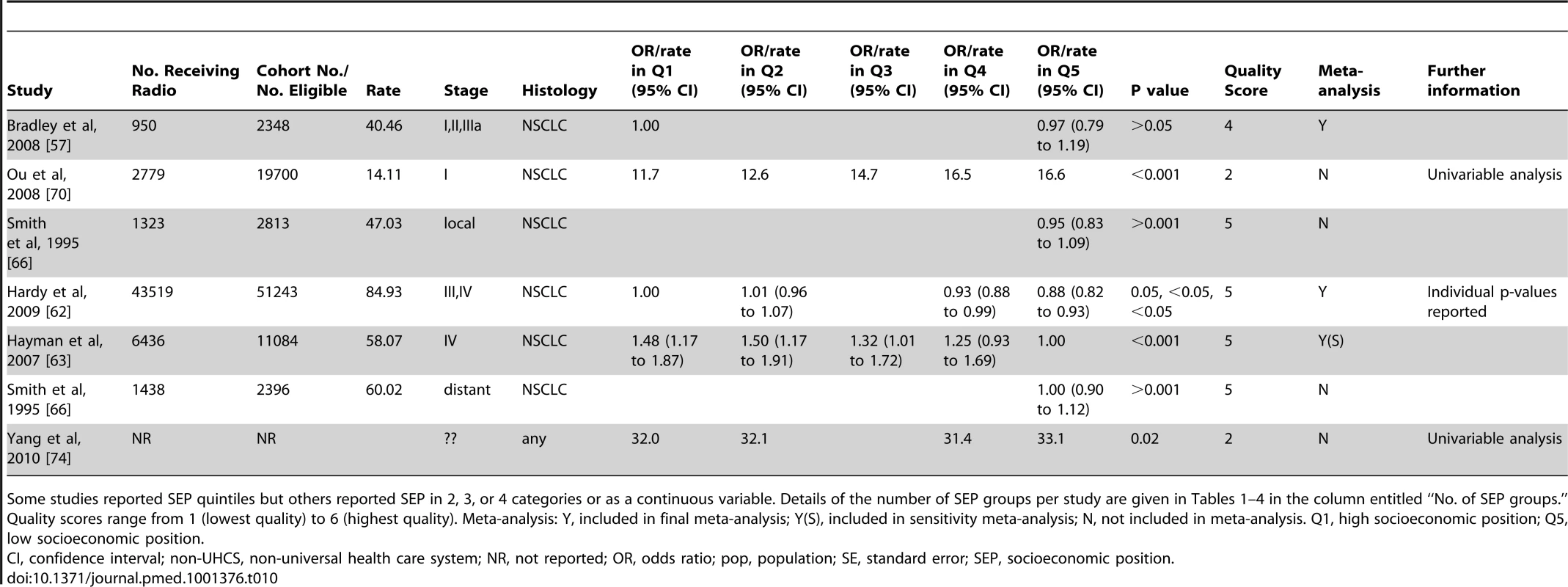
Some studies reported SEP quintiles but others reported SEP in 2, 3, or 4 categories or as a continuous variable. Details of the number of SEP groups per study are given in Tables 1–4 in the column entitled “No. of SEP groups.” Quality scores range from 1 (lowest quality) to 6 (highest quality). Meta-analysis: Y, included in final meta-analysis; Y(S), included in sensitivity meta-analysis; N, not included in meta-analysis. Q1, high socioeconomic position; Q5, low socioeconomic position. Overall, no association between SEP and receipt of radiotherapy was seen in the meta-analysis of the seven studies with non-overlapping populations selected for inclusion (OR = 0.99 [95% CI 0.86 to 1.14], p = 0.89, I2 = 54%) (Figure 4), or when all nine studies were included (OR = 0.95 [95% CI 0.85 to 1.06], p = 0.40, I2 = 71%) (Figure S4). A significant association was seen for non-UHCS studies but only two studies were included here, each looking at different stage patients.
Fig. 4. Meta-analysis of odds of receipt of radiotherapy in low versus high SEP. 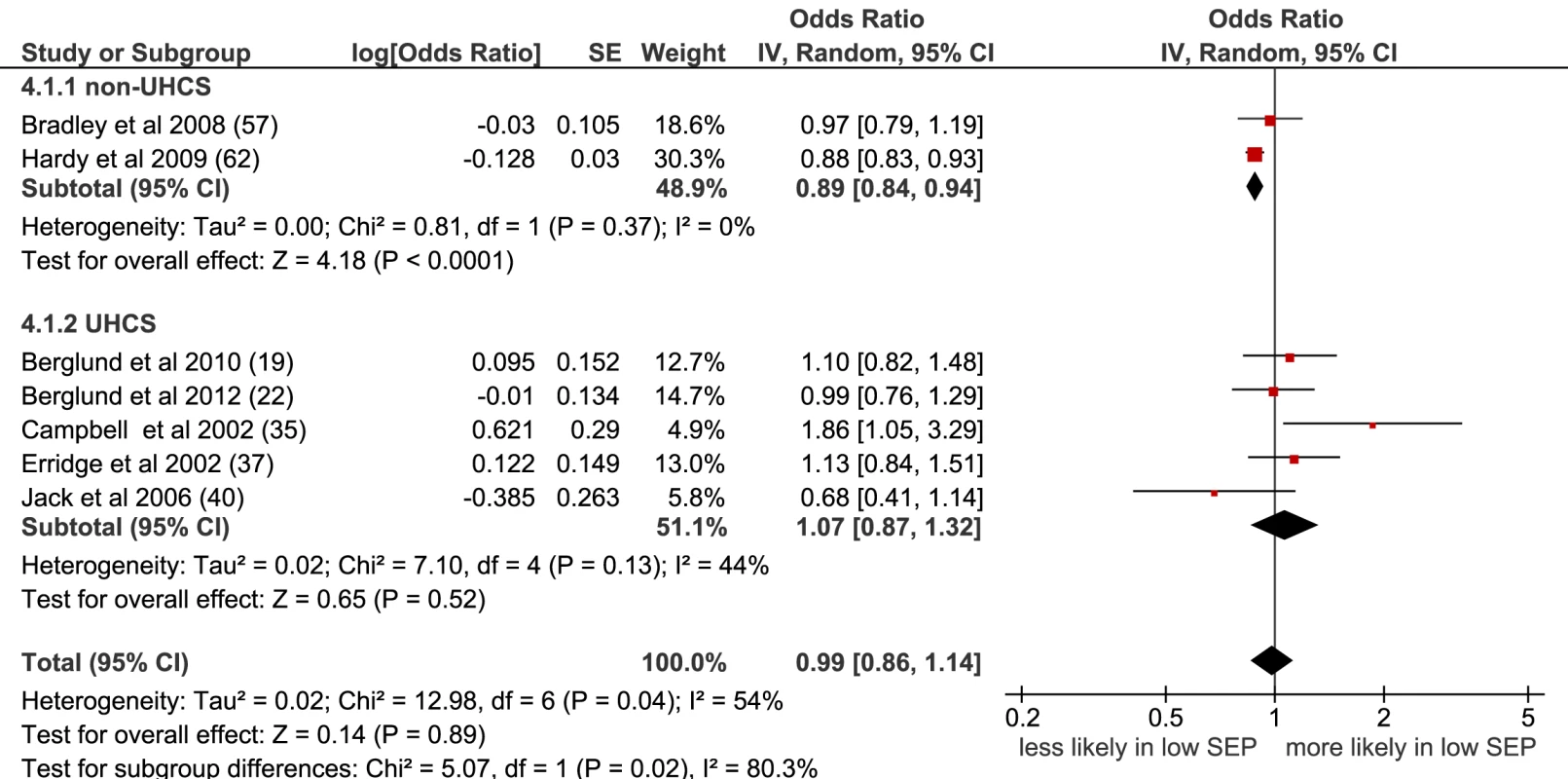
CI, confidence interval; non-UHCS, non-universal health care system; OR, odds ratio; SE, standard error; SEP, socioeconomic position; UHCS, universal health care system. Treatment Type not Specified
Seven papers (eight study populations) examined receipt of unspecified treatment, and three papers considered receipt of unspecified curative treatment in three populations (Tables 11–13). In the meta-analysis of five non-overlapping studies, low SEP was associated with a lower likelihood of receiving unspecified treatment (OR = 0.78 [95% CI 0.74 to 0.83], p<0.001, I2 = 0) (Figure 5). This was also seen when studies with overlapping populations were included (OR = 0.80 [95% CI 0.77 to 0.84], p<0.001, I2 = 17%) (Figure S5).
Fig. 5. Meta-analysis of odds of receipt of unspecified treatment in low versus high SEP. 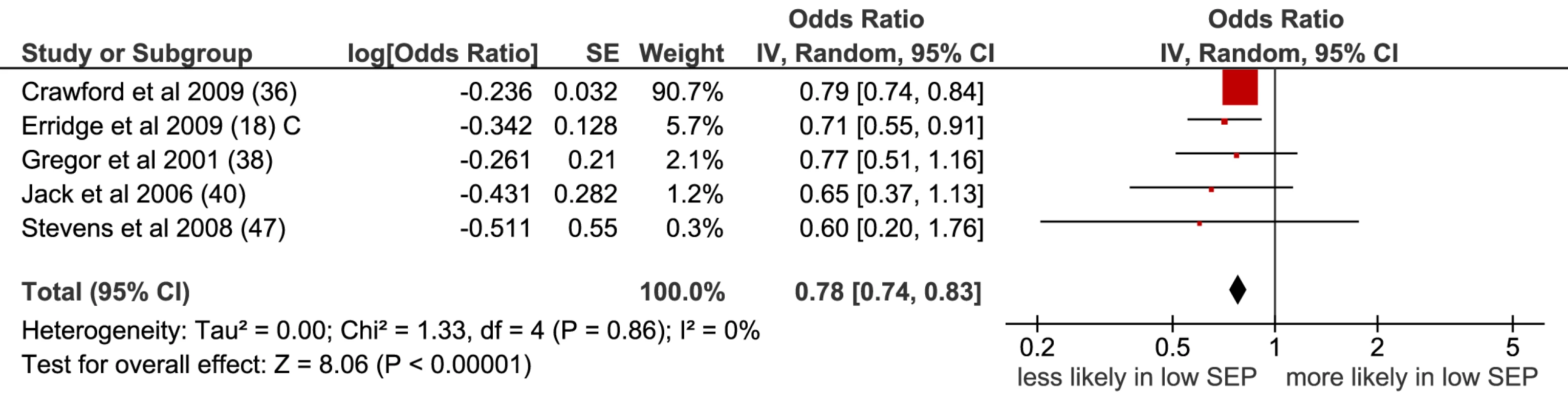
CI, confidence interval; OR, odds ratio; SE, standard error; SEP, socioeconomic position. Tab. 11. Likelihood of receipt of any type of unspecified treatment by SEP group (universal health care systems). 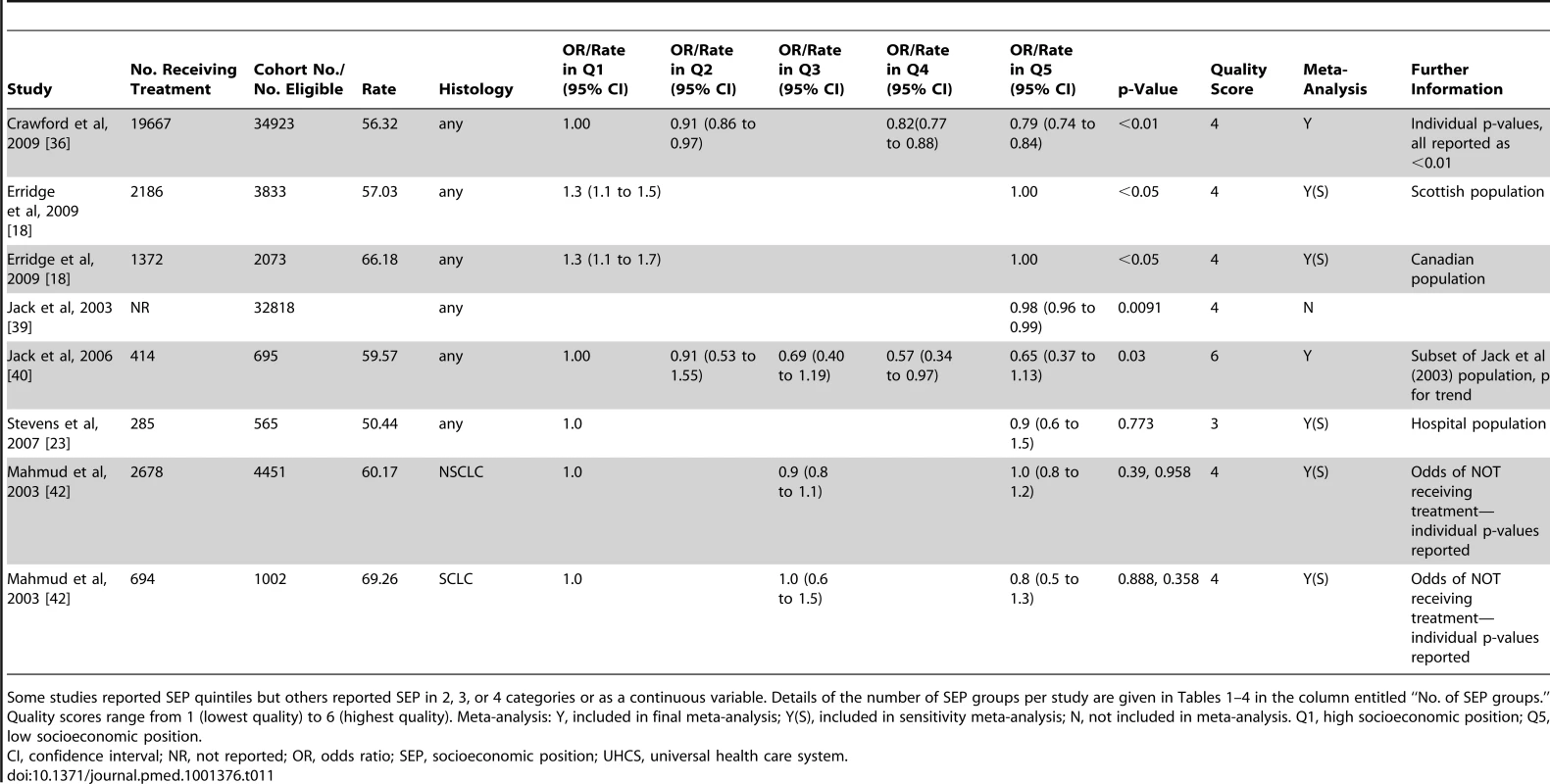
Some studies reported SEP quintiles but others reported SEP in 2, 3, or 4 categories or as a continuous variable. Details of the number of SEP groups per study are given in Tables 1–4 in the column entitled “No. of SEP groups.” Quality scores range from 1 (lowest quality) to 6 (highest quality). Meta-analysis: Y, included in final meta-analysis; Y(S), included in sensitivity meta-analysis; N, not included in meta-analysis. Q1, high socioeconomic position; Q5, low socioeconomic position. Tab. 12. Likelihood of receipt of any type of unspecified treatment by SEP group (non-universal health care systems). 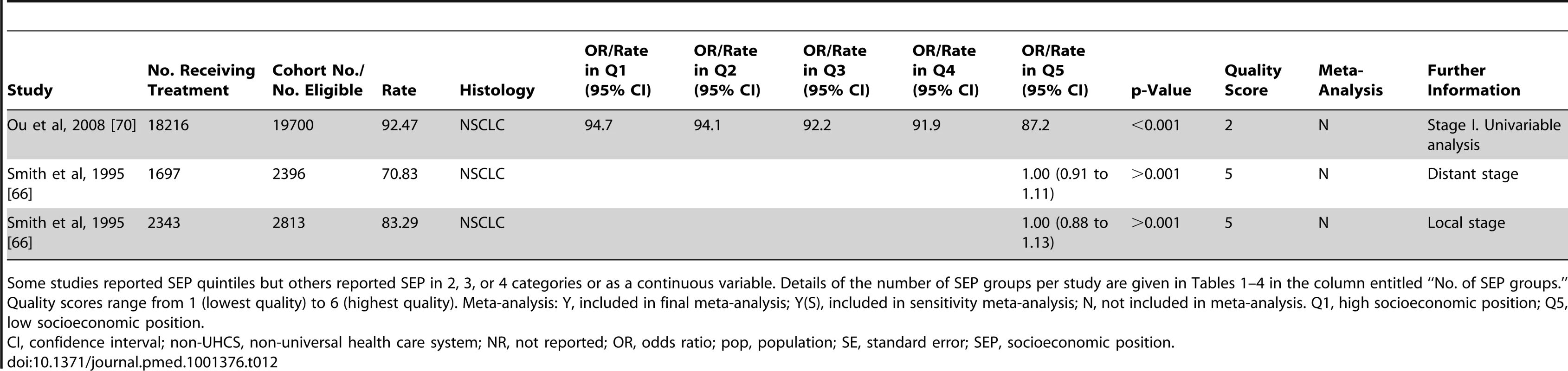
Some studies reported SEP quintiles but others reported SEP in 2, 3, or 4 categories or as a continuous variable. Details of the number of SEP groups per study are given in Tables 1–4 in the column entitled “No. of SEP groups.” Quality scores range from 1 (lowest quality) to 6 (highest quality). Meta-analysis: Y, included in final meta-analysis; Y(S), included in sensitivity meta-analysis; N, not included in meta-analysis. Q1, high socioeconomic position; Q5, low socioeconomic position. Tab. 13. Likelihood of receipt of any type of unspecified curative treatment by SEP group (universal health care systems). 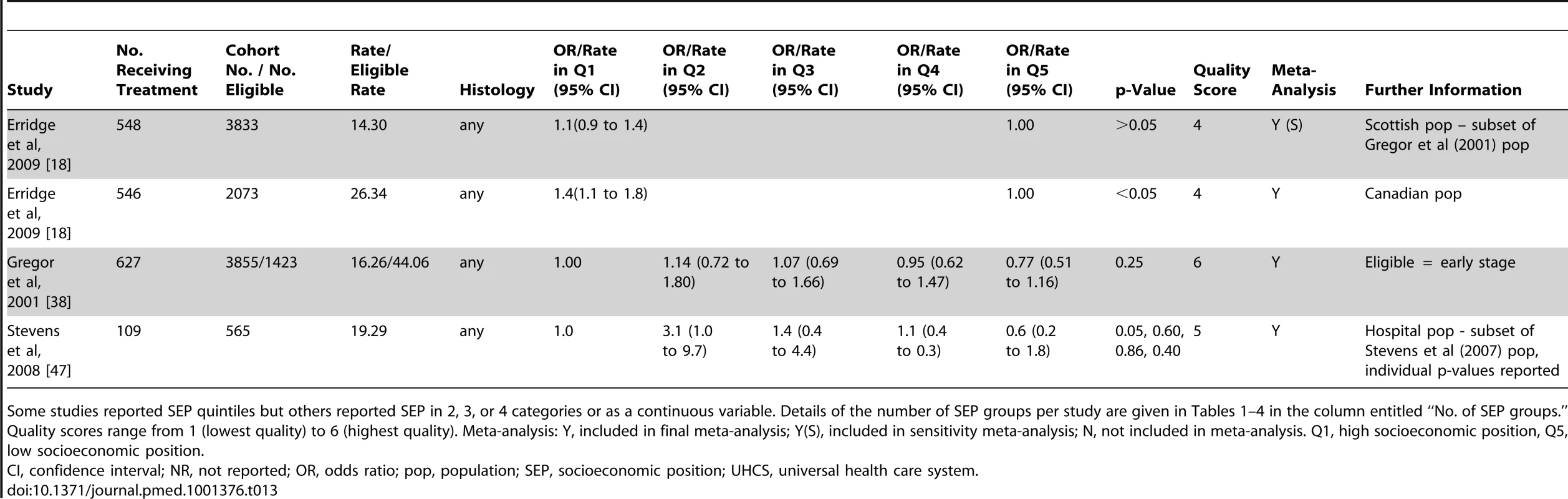
Some studies reported SEP quintiles but others reported SEP in 2, 3, or 4 categories or as a continuous variable. Details of the number of SEP groups per study are given in Tables 1–4 in the column entitled “No. of SEP groups.” Quality scores range from 1 (lowest quality) to 6 (highest quality). Meta-analysis: Y, included in final meta-analysis; Y(S), included in sensitivity meta-analysis; N, not included in meta-analysis. Q1, high socioeconomic position, Q5, low socioeconomic position. When the surgery, chemotherapy, and radiotherapy papers included in the separate treatment meta-analyses in this systematic review were analysed together to produce an overall summary effect meta-analysis OR, a similar result was seen, with low SEP associated with a lower likelihood of receiving any type of treatment. This was found when including only studies with non-overlapping populations (OR = 0.79 [95% CI 0.73 to 0.86], p<0.001, I2 = 77%) (Figure S6) and when including all eligible studies (OR = 0.80 [95% CI 0.75 to 0.86], p<0.001, I2 = 82%) (Figure S7).
Discussion
Principal Findings
To our knowledge, this is the first systematic review and meta-analysis examining socioeconomic inequalities in receipt of lung cancer treatment. It shows an association between low SEP and reduced likelihood of receipt of any type of treatment, surgery, and chemotherapy. The results were generally consistent across different health care systems.
Interpretation of Results
Surgery is suitable only for patients with early-stage NSCLC, and it has been suggested that patients with cancer in a lower SEP are more likely to present later and with later-stage disease [20]. This may help explain why socioeconomic inequalities in receipt of surgery are observed in some studies. However, presentation with later-stage cancer in lower SEP patients has not been consistently observed [19]. In this review, when receipt of treatment was examined in studies of early-stage patients only (from non-UHCS studies), low SEP remained associated with reduced likelihood of surgery. Thus, the association between SEP and receipt of surgery appears to be independent of stage. Similar results were seen for NSCLC studies in both health care systems.
Receipt of treatment may also be influenced by clinical suitability for treatment, and socioeconomic differences in the number of co-morbidities present may explain socioeconomic inequalities in treatment. In the three UHCS studies that took co-morbidity into account, SEP was not associated with receipt of surgery [21],[22] or of any treatment [23] when the trend across SEP groups was examined, suggesting that co-morbidity may be a potential mediator of socioeconomic inequalities in treatment in UHCSs. However, most of the non-UHCS studies did include co-morbidity as a confounder, and socioeconomic inequalities in treatment were still observed, suggesting that there may be differences between health care systems here.
Strengths and Weaknesses of the Review and of the Available Evidence
This is one of the first equity reviews published [24],[25], the first systematic review of the literature on intervention-generated inequalities in lung cancer treatment to our knowledge, and the first cancer equity review to include a meta-analysis. Extensive searches were carried out to identify studies. However, it is possible that not all relevant studies were obtained.
The included studies reported observational data only. The suitability of meta-analysis for observational studies has been questioned, as it may produce precise but spurious results [26]. Examining the possible sources of heterogeneity by conducting sensitivity analyses across different sub-groups may be less prone to bias than calculating an overall summary effect [26]. Here, although an overall summary effect OR was calculated, heterogeneity was taken into account. Separate analyses by type of treatment were carried out, with further stratification by stage and histology. Universal and non-UHCSs were examined separately and random effects rather than fixed effects meta-analyses were conducted. These precautions did not change the overall pattern of results seen.
Significant heterogeneity remained in some cases, which could be considered a limitation, although this is not surprising because of the characteristics of the studies included. For studies examining receipt of chemotherapy and radiotherapy it was generally not possible to differentiate between curative and palliative treatment and, if patterns of care differ for these by SEP, this might explain the high degree of heterogeneity seen. However, although there is some suggestion that heterogeneity can be considered high at >50% [17], when confidence intervals were calculated these were wide, so it was difficult to be confident about the degree of heterogeneity present [27].
Results for receipt of radiotherapy differed in the non-UHCS sub-group compared to overall but, as only two studies were included in this sub-group, it is difficult to be sure that different patterns of receipt of radiotherapy by SEP are due to differences in health care system.
Many of the non-UHCS studies used overlapping population sub-groups from the SEER database. There was also population overlap between some UHCS datasets. We attempted to include only substantially non-overlapping datasets within the final meta-analyses to ensure independence of results. A judgement had to be made as to which was the best-quality and most appropriate paper to include, but sensitivity analyses using different inclusion combinations (Figure S8) did not change the overall findings, nor did including all suitable studies regardless of population overlap (Figures S1, S3, S4, S5, S7).
Included papers contained data for patients diagnosed between 1978 and 2008. As treatment guidance has changed over time, older studies may be less applicable to current clinical practice. However, the majority of included studies were published within the last five years, and sensitivity analyses excluding studies published prior to 2000 did not change the overall findings.
Various measures of SEP were used, and these were categorised differently—an acknowledged problem in equity reviews [28]. All but one study measured SEP at the area level. This is a further limitation, as area-based measures of SEP are unlikely to be accurate markers of individual-level circumstances and access to resources [29]. Area-based measures of SEP can be calculated using address, making them easy to add to disease registers, such as those used in many of the studies synthesised here. However, the reliance on area-based markers of SEP may underestimate the strength of the true association between SEP and receipt of treatment.
Not all studies reported details of stage and histology—both of which influence treatment type—and very few UHCS studies took co-morbidity into account. Thus, the ORs used in the meta-analyses were not consistently adjusted for the same covariates. However, we attempted to take these factors into account in the quality scores and by conducting subgroup sensitivity analyses. Examining only high-quality studies did not alter our findings nor did sensitivity analyses, although consequent reduction in numbers did result in loss of significance in some analyses, potentially due to lack of power to detect differences.
In order to conduct meta-analysis it is necessary to compare the odds of treatment in the lowest-SEP group with the odds in the highest, which simplifies what may be a complex relationship across SEP groups. However, studies that reported a change in odds ratios across the SEP categories, and thus explored trends in receipt of treatment, generally supported the overall findings of the review.
A number of existing tools suitable for assessing cohort study quality were considered [15],[16]. However, none of these tools was entirely appropriate for the type of studies included and, as has been done in previous reviews [13],[30], we devised a unique tool, adapting and utilising aspects of other available tools. This approach has the benefit of producing a quality tool that is highly specific for the type of studies examined.
As with any systematic review, we are unable to exclude the possibility of publication bias. Studies reporting null findings are less likely to be published or, if they are published, not to report numerical outcomes [17]. A funnel plot to assess potential publication bias did not show obvious bias (Figure S9). However, a number of papers recovered in the search included SEP in the description of the study population but did not report receipt of treatment by SEP [31]–[34]. Study authors were contacted and asked to provide further information, but only one supplied the requested data [34]. It is likely that SEP was not significantly associated with receipt of treatment in the other studies, but this was not always clearly reported. However, publication bias is thought to be less important than other sources of bias, such as confounding, in meta-analyses of observational studies [26].
Implications for Policy and Practice
Socioeconomic inequalities in receipt of treatment may exacerbate socioeconomic inequalities in incidence of lung cancer, which is strongly associated with higher smoking rates in more deprived populations, so may further contribute to the poorer outcomes in lower SEP groups.
Socioeconomic inequalities in treatment may be due to differences in access to care. Within a non-UHCS it might be expected that socioeconomic differences in receipt of treatment would be observed due to income-related differences in health insurance status. Patients with lung cancer in the USA who do not have insurance have been shown to have more limited access to care [13]. However, as socioeconomic inequalities in receipt of lung cancer treatment were also observed in UHCSs that do not depend on ability to pay and in non-UHCS studies where insurance type was taken into account, this would suggest that other system factors may be contributing to this inequality. The extent to which receipt of treatment is influenced by factors such as patient choice is not known.
Variability at the patient, tumour, system, and individual clinician levels needs to be investigated before clear recommendations for changes to policy and practice can be made.
Future Research
This review has demonstrated a clear association between lower SEP and reduced likelihood of receiving surgery, chemotherapy, and any type of unspecified treatment for lung cancer. The reasons for these inequalities need to be more thoroughly investigated. Better-quality UHCS studies, including statistical control for co-morbidity and stratification by stage and histology—so that only those patients eligible for a particular treatment are included in the population-denominator—are required. It would also be useful to be able to distinguish between curative and palliative intent of treatment. In non-UHCS, studies in younger populations, examining a range of insurance providers, are required.
Further investigation into the system and patient factors that might contribute to socioeconomic inequalities in receipt of lung cancer care is necessary, to help develop interventions that ensure equitable receipt of appropriate treatment. This should include a quantitative exploration of inequalities at each stage of the care pathway as well as qualitative work exploring reasons for inequality. Inequalities in receipt of treatment may contribute to inequalities in cancer survival and so cohort survival analyses are warranted in order to investigate intervention-generated inequalities in lung cancer outcomes.
Supporting Information
Zdroje
1. Cancer Research UK Cancer incidence: UK statistics. Available: http://info.cancerresearchuk.org/cancerstats/incidence/. Accessed 09 January 2013.
2. Howlader N, Noone AM, Krapcho M, Neyman N, Aminou R, et al.. (eds). SEER Cancer Statistics Review, 1975–2009 (Vintage 2009 Populations), National Cancer Institute. Bethesda, MD. Based on November 2011 SEER data submission, posted to the SEER web site, April 2012. Available: http://seer.cancer.gov/csr/1975_2009_pops09/. Accessed 09 January 2012.
3. Cancer Research UK Common cancers - UK mortality statistics. Available: http://info.cancerresearchuk.org/cancerstats/mortality/cancerdeaths/. Accessed 09 January 2013.
4. ColemanMP, FormanD, BryantH, ButlerJ, RachetB, et al. (2011) Cancer survival in Australia, Canada, Denmark, Norway, Sweden, and the UK, 1995–2007 (the International Cancer Benchmarking Partnership): an analysis of population-based cancer registry data. Lancet 377 : 127–138.
5. VerdecchiaA, FrancisciS, BrennerH, GattaG, MicheliA, et al. (2007) Recent cancer survival in Europe: a 2000–02 period analysis of EUROCARE-4 data. Lancet Oncol 8 : 784–796.
6. NICE (2005) Clinical Guideline 24. Lung Cancer: the diagnosis and treatment of lung cancer. London: NICE.
7. RachetB, EllisL, MaringeC, ChuT, NurU, et al. (2010) Socioeconomic inequalities in cancer survival in England after the NHS cancer plan. Br J Cancer 103 : 446–453.
8. AartsMJ, LemmensVEPP, LouwmanMWJ, KunstAE, CoeberghJWW (2010) Socioeconomic status and changing inequalities in colorectal cancer? A review of the associations with risk, treatment and outcome. Eur J Cancer 46 : 2681–2695.
9. WoodsLM, RachetB, ColemanMP (2006) Origins of socio-economic inequalities in cancer survival: a review. Ann Oncol 17 : 5–19.
10. White M, Adams J, Heywood P (2009) How and why do interventions that increase health overall widen inequalities within populations? In: Babones S, editor. Health, inequality and society. Bristol: Policy Press.
11. SidorchukA, AgardhE, AremuO, HallqvistJ, AllebeckP, et al. (2009) Socioeconomic differences in lung cancer incidence: a systematic review and meta-analysis. Cancer Causes Control 20 : 459–471.
12. MoherD, LiberatiA, TetzlaffJ, AltmanDG (2009) The PRISMA Group (2009) Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. PLoS Med 6(7): e1000097 doi:10.1371/journal.pmed.1000097.
13. SlatoreCG, AuDH, GouldMK (2010) on behalf of the American Thoracic Society Disparities in Healthcare G (2010) An Official American Thoracic Society Systematic Review: Insurance Status and Disparities in Lung Cancer Practices and Outcomes. Am J Respir Crit Care Med 182 : 1195–1205.
14. Donaldson C, Gerard K (2005) Health care financing reforms: moving into the new millenium. Economics of Health Care Financing: The Visible Hand. Basingstoke: Palgrave Macmillan.
15. SIGN (2011) SIGN 50: A Guideline Developer's Handbook. Methodology Checklist 3: Cohort studies. Edinburgh: SIGN.
16. VandenbrouckeJP, von ElmE, AltmanDG, GøtzschePC, MulrowCD, et al. (2007) Strengthening the Reporting of Observational Studies in Epidemiology (STROBE): Explanation and Elaboration. PLoS Med 4(10): e297 doi:10.1371/journal.pmed.0040297.
17. The Cochrane Collaboration (2008) Cochrane Handbook for Systematic Reviews of Interventions. Version 5.0.2. Higgins J, Green S, editors.
18. ErridgeSC, MurrayB, WilliamsL, BrewsterD, BlackR, et al. (2009) Improved survival from lung cancer in British Columbia compared to Scotland-Are different treatment rates the whole story? Lung Cancer 64 : 358–366.
19. BerglundA, HolmbergL, TishelmanC, WageniusG, EakerS, et al. (2010) Social inequalities in non-small cell lung cancer management and survival: a population-based study in central Sweden. Thorax 65 : 327–333.
20. DaltonSO, FrederiksenBL, JacobsenE, Steding-JessenM, OsterlindK, et al. (2011) Socioeconomic position, stage of lung cancer and time between referral and diagnosis in Denmark, 2001–2008. Br J Cancer 105 : 1042–1048.
21. RichAL, TataLJ, FreeCM, StanleyRA, PeakeMD, et al. (2011) Inequalities in outcomes for non-small cell lung cancer: the influence of clinical characteristics and features of the local lung cancer service. Thorax 66 : 1078–1084.
22. BerglundA, LambeM, LüchtenborgM, LinklaterK, PeakeMD, et al. (2012) Social differences in lung cancer management and survival in South East England: a cohort study. BMJ Open 2 doi:10.1136/bmjopen-2012-001048.
23. StevensW, StevensG, KolbeJ, CoxB (2007) Lung cancer in New Zealand: Patterns of secondary care and implications for survival. J Thorac Oncol 2 : 481–493.
24. WelchV, PetticrewM, UeffingE, Benkhalti JanduM, BrandK, et al. (2012) Does Consideration and Assessment of Effects on Health Equity Affect the Conclusions of Systematic Reviews? A Methodology Study. PLoS ONE 7(3): e31360 doi:10.1371/journal.pone.0031360.
25. ThomasS, FayterD, MissoK, OgilvieD, PetticrewM, et al. (2008) Population tobacco control interventions and their effects on social inequalities in smoking: systematic review. Tob Control 17 : 230–237.
26. EggerM, SchneiderM, SmithGD (1998) Meta-analysis Spurious precision? Meta-analysis of observational studies. BMJ 316 : 140–144.
27. IoannidisJ, PatsopoulosN, EvangelouE (2007) Uncertainty in heterogeneity estimates in meta-analyses. BMJ 335 : 914–916.
28. OgilvieD, FayterD, PetticrewM, SowdenA, ThomasS, et al. (2008) The harvest plot: A method for synthesising evidence about the differential effects of interventions. BMC Med Res Methodol 8 : 8.
29. AdamsJ, RyanV, WhiteM (2005) How accurate are Townsend Deprivation Scores as predictors of self-reported health? A comparison with individual level data. J Public Health 27 : 101–106.
30. OlssonJK, SchultzEM, GouldMK (2009) Timeliness of care in patients with lung cancer: a systematic review. Thorax 64 : 749–756.
31. GroseD, DevereuxG, BrownL, JonesR, SharmaD, et al. (2011) Variation in comorbidity and clinical management in patients newly diagnosed with lung cancer in four Scottish centers. J Thorac Oncol 6 : 500–509.
32. HallSE, BulsaraCE, BulsaraMK, LeahyTG, CulbongMR, et al. (2004) Treatment patterns for cancer in Western Australia: Does being indigenous make a difference? Med J Aust 181 : 191–194.
33. McCannJ, ArtinianV, DuhaimeL, LewisJW, KvalePA, et al. (2005) Evaluation of the Causes for Racial Disparity in Surgical Treatment of Early Stage Lung Cancer. Chest 128 : 3440–3446.
34. RiazSP, LüchtenborgM, JackRH, CouplandVH, LinklaterKM, et al. (2012) Variation in surgical resection for lung cancer in relation to survival: Population-based study in England 2004–2006. Eur J Cancer 48 : 54–60.
35. CampbellNC, ElliottAM, SharpL, RitchieLD, CassidyJ, et al. (2002) Impact of deprivation and rural residence on treatment of colorectal and lung cancer. Br J Cancer 87 : 585–590.
36. CrawfordSM, SauerzapfV, HaynesR, ZhaoH, FormanD, et al. (2009) Social and geographical factors affecting access to treatment of lung cancer. Br J Cancer 101 : 897–901.
37. ErridgeSC, ThomsonCS, DavidsonJ, JonesRD, PriceA (2002) Factors Influencing the Use of Thoracic Radiotherapy in Lung Cancer;an Analysis of the 1995 Scottish Lung Cancer Audit. Clin Oncol 14 : 219–227.
38. GregorA, ThomsonCS, BrewsterDH, StronerPL, DavidsonJ, et al. (2001) Management and survival of patients with lung cancer in Scotland diagnosed in 1995: results of a national population based study. Thorax 56 : 212–217.
39. JackRH, GullifordMC, FergusonJ, MollerH (2003) Geographical inequalities in lung cancer management and survival in South East England: evidence of variation in access to oncology services? Br J Cancer 88 : 1025–1031.
40. JackRH, GullifordMC, FergusonJ, MøllerH (2006) Explaining inequalities in access to treatment in lung cancer. J Eval Clin Pract 12 : 573–582.
41. JonesAP, HaynesR, SauerzapfV, CrawfordSM, ZhaoH, et al. (2008) Travel time to hospital and treatment for breast, colon, rectum, lung, ovary and prostate cancer. Eur J Cancer 44 : 992–999.
42. MahmudSM, ReillyM, ComberH (2003) Patterns of initial management of lung cancer in the Republic of Ireland: a population-based observational study. Lung Cancer 41 : 57–64.
43. McMahonM, BarbiereJM, GreenbergDC, WrightKA, LyratzopoulosG (2011) Population-based trends in use of surgery for non-small cell lung cancer in a UK region, 1995–2006. Thorax 66 : 453–455.
44. PollockAM, VickersN (1998) Deprivation and emergency admissions for cancers of colorectum, lung, and breast in south east England: ecological study. BMJ 317 : 245–252.
45. RaineR, WongW, ScholesS, AshtonC, ObichereA, et al. (2010) Social variations in access to hospital care for patients with colorectal, breast, and lung cancer between 1999 and 2006: retrospective analysis of hospital episode statistics. BMJ 340.
46. RichAL, TataLJ, StanleyRA, FreeCM, PeakeMD, et al. (2011) Lung cancer in England: Information from the National Lung Cancer Audit (LUCADA). Lung Cancer 72 : 16–22.
47. StevensW, StevensG, KolbeJ, CoxB (2008) Ethnic differences in the management of lung cancer in New Zealand. J Thorac Oncol 3(3): 237–244.
48. BattersbyJ, FlowersJ, HarveyI (2004) An alternative approach to quantifying and addressing inequity in healthcare provision: access to surgery for lung cancer in the east of England. J Epidemiol Community Health 58 : 623–625.
49. BendzsakA, NenshiR, DarlingG, SchultzSE, GunrajN, et al. (2011) Overview of Lung Cancer Surgery in Ontario. Ann Thorac Surg 91 : 361–366.
50. CartmanML, HatfieldAC, MuersMF, PeakeMD, HawardRA, et al. (2002) Lung cancer: district active treatment rates affect survival. J Epidemiol Community Health 56 : 424–429.
51. HuiAC, VinodSK, JalaludinBB, YuileP, DelaneyGP, et al. (2005) Socio-economic status and patterns of care in lung cancer. Aust N Z J Public Health 29 : 372–377.
52. MadelaineJ, GuizardAV, LefevreH, LecarpentierMM, LaunoyG (2002) [Diagnosis, treatment, and prognosis of lung cancer in the Manche (France) (1997–1999) according to patients socioeconomic characteristics]. Revue d Epidemiologie et de Sante Publique 50 : 383–392.
53. PaganoE, FilippiniC, Di CuonzoD, RuffiniE, ZanettiR, et al. (2010) Factors affecting pattern of care and survival in a population-based cohort of non-small-cell lung cancer incident cases. Cancer Epidemiol 34 : 483–489.
54. PatelN, AdatiaR, MellemgaardA, JackR, MollerH (2007) Variation in the use of chemotherapy in lung cancer. Br J Cancer 96 : 886–890.
55. StevensG, StevensW, PurchuriS, KolbeJ, CoxB (2009) Radiotherapy utilisation in lung cancer in New Zealand: Disparities with optimal rates explained. N Z Med J 122(1306): 43–54.
56. YounisT, Al-FayeaT, VirikK, MorzyckiW, Saint-JacquesN (2008) Adjuvant chemotherapy uptake in non-small cell lung cancer. J Thorac Oncol 3 : 1272–1278.
57. BradleyCJ, DahmanB, GivenCW (2008) Treatment and Survival Differences in Older Medicare Patients With Lung Cancer as Compared With Those Who Are Dually Eligible for Medicare and Medicaid. J Clin Oncol 26 : 5067–5073.
58. DavidoffAJ, TangM, SealB, EdelmanMJ (2010) Chemotherapy and Survival Benefit in Elderly Patients With Advanced Non–Small-Cell Lung Cancer. J Clin Oncol 28 : 2191–2197.
59. EarleCC, VendittiLN, NeumannPJ, GelberRD, WeinsteinMC, et al. (2000) Who Gets Chemotherapy for Metastatic Lung Cancer?. Chest 117 : 1239–1246.
60. EsnaolaNF, GebregziabherM, KnottK, FinneyC, SilvestriGA, et al. (2008) Underuse of Surgical Resection for Localized, Non-Small Cell Lung Cancer Among Whites and African Americans in South Carolina. Ann Thorac Surg 86 : 220–227.
61. GreenwaldHP, PolissarNL, BorgattaEF, McCorkleR, GoodmanG (1998) Social Factors, Treatment, and Survival in Early-Stage Non-Small Cell Lung Cancer. Am J Public Health 88 : 1681–1684.
62. HardyD, LiuC-C, XiaR, CormierJN, ChanW, et al. (2009) Racial disparities and treatment trends in a large cohort of elderly black and white patients with nonsmall cell lung cancer. Cancer 115 : 2199–2211.
63. HaymanJA, AbrahamsePH, LakhaniI, EarleCC, KatzSJ (2007) Use of Palliative Radiotherapy Among Patients With Metastatic Non-Small-Cell Lung Cancer. Int J Radiation Oncology Biol Phys 69 : 1001–1007.
64. LathanCS, NevilleBA, EarleCC (2008) Racial composition of hospitals: Effects on surgery for early-stage non-small-cell lung cancer. J Clin Oncol 26(26): 4347–4352.
65. PolednakAP (2001) Disaparities in surgical treatment of early-stage non-small-cell lung cancer. Yale J Biol Med 74 : 309–314.
66. SmithTJ, PenberthyL, DeschCE, WhittemoreM, NewschafferC, et al. (1995) Differences in initial treatment patterns and outcomes of lung cancer in the elderly. Lung Cancer 13 : 235–252.
67. BachPB, CramerLD, WarrenJL, BeggCB (1999) Racial differences in the treatment of early-stage lung cancer. N Engl J Med 341 : 1198–1205.
68. EarleCC, NeumannPJ, GelberRD, WeinsteinMC, WeeksJC (2002) Impact of Referral Patterns on the Use of Chemotherapy for Lung Cancer. J Clin Oncol 20 : 1786–1792.
69. LathanCS, NevilleBA, EarleCC (2006) The effect of race on invasive staging and surgery in non-small-cell lung cancer. J Clin Oncol 24 : 413–418.
70. OuSHI, ZellJA, ZiogasA, Anton-CulverH (2008) Low socioeconomic status is a poor prognostic factor for survival in stage I nonsmall cell lung cancer and is independent of surgical treatment, race, and marital status. Cancer 112 : 2011–2020.
71. SugaJM, NguyenDV, MohammedSM, BrownM, CalhounR, et al. (2010) Racial disparities on the use of invasive and noninvasive staging in patients with non-small cell lung cancer. J Thorac Oncol 5 : 1772–1778.
72. TammemagiCM, Neslund-DudasC, SimoffM, KvaleP (2004) In lung cancer patients, age, race-ethnicity, gender and smoking predict adverse comorbidity, which in turn predicts treatment and survival. J Clin Epidemiol 57 : 597–609.
73. WangJ, KuoY, FreemanJ, GoodwinJ (2008) Increasing access to medical oncology consultation in older patients with stage II-IIIA non-small-cell lung cancer. Med Oncol 25 : 125–132.
74. YangR, CheungMC, ByrneMM, HuangY, NguyenD, et al. (2010) Do racial or socioeconomic disparities exist in lung cancer treatment? Cancer 116 : 2437–2447.
Štítky
Interní lékařství
Článek vyšel v časopisePLOS Medicine
Nejčtenější tento týden
2013 Číslo 2- Berberin: přírodní hypolipidemikum se slibnými výsledky
- Léčba bolesti u seniorů
- Příznivý vliv Armolipidu Plus na hladinu cholesterolu a zánětlivé parametry u pacientů s chronickým subklinickým zánětem
- Jak postupovat při výběru betablokátoru − doporučení z kardiologické praxe
- Červená fermentovaná rýže účinně snižuje hladinu LDL cholesterolu jako vhodná alternativa ke statinové terapii
-
Všechny články tohoto čísla
- Prevalence of Age-Related Macular Degeneration in Nakuru, Kenya: A Cross-Sectional Population-Based Study
- Socioeconomic Inequalities in Lung Cancer Treatment: Systematic Review and Meta-Analysis
- Cardiovascular Risk of NSAIDs: Time to Translate Knowledge into Practice
- Prognosis Research Strategy (PROGRESS) 3: Prognostic Model Research
- Who Should Pay for Global Health, and How Much?
- Global Estimates of Syphilis in Pregnancy and Associated Adverse Outcomes: Analysis of Multinational Antenatal Surveillance Data
- Prehospital Lactated Ringer's Solution Treatment and Survival in Out-of-Hospital Cardiac Arrest: A Prospective Cohort Analysis
- Causal Relationship between Obesity and Vitamin D Status: Bi-Directional Mendelian Randomization Analysis of Multiple Cohorts
- A Reality Checkpoint for Mobile Health: Three Challenges to Overcome
- Use of Non-Steroidal Anti-Inflammatory Drugs That Elevate Cardiovascular Risk: An Examination of Sales and Essential Medicines Lists in Low-, Middle-, and High-Income Countries
- Scaling Up mHealth: Where Is the Evidence?
- Prognosis Research Strategy (PROGRESS) 2: Prognostic Factor Research
- Whole Genome Sequencing versus Traditional Genotyping for Investigation of a Outbreak: A Longitudinal Molecular Epidemiological Study
- PLOS Medicine
- Archiv čísel
- Aktuální číslo
- Informace o časopisu
Nejčtenější v tomto čísle- Prognosis Research Strategy (PROGRESS) 3: Prognostic Model Research
- Prognosis Research Strategy (PROGRESS) 2: Prognostic Factor Research
- Whole Genome Sequencing versus Traditional Genotyping for Investigation of a Outbreak: A Longitudinal Molecular Epidemiological Study
- Prevalence of Age-Related Macular Degeneration in Nakuru, Kenya: A Cross-Sectional Population-Based Study
Kurzy
Zvyšte si kvalifikaci online z pohodlí domova
Současné možnosti léčby obezity
nový kurzAutoři: MUDr. Martin Hrubý
Všechny kurzyPřihlášení#ADS_BOTTOM_SCRIPTS#Zapomenuté hesloZadejte e-mailovou adresu, se kterou jste vytvářel(a) účet, budou Vám na ni zaslány informace k nastavení nového hesla.
- Vzdělávání



