-
Články
Top novinky
Reklama- Vzdělávání
- Časopisy
Top články
Nové číslo
- Témata
Top novinky
Reklama- Videa
- Podcasty
Nové podcasty
Reklama- Kariéra
Doporučené pozice
Reklama- Praxe
Top novinky
ReklamaElimination of HIV in South Africa through Expanded Access to Antiretroviral Therapy: A Model Comparison Study
Background:
Expanded access to antiretroviral therapy (ART) using universal test and treat (UTT) has been suggested as a strategy to eliminate HIV in South Africa within 7 y based on an influential mathematical modeling study. However, the underlying deterministic model was criticized widely, and other modeling studies did not always confirm the study's finding. The objective of our study is to better understand the implications of different model structures and assumptions, so as to arrive at the best possible predictions of the long-term impact of UTT and the possibility of elimination of HIV.Methods and Findings:
We developed nine structurally different mathematical models of the South African HIV epidemic in a stepwise approach of increasing complexity and realism. The simplest model resembles the initial deterministic model, while the most comprehensive model is the stochastic microsimulation model STDSIM, which includes sexual networks and HIV stages with different degrees of infectiousness. We defined UTT as annual screening and immediate ART for all HIV-infected adults, starting at 13% in January 2012 and scaled up to 90% coverage by January 2019. All models predict elimination, yet those that capture more processes underlying the HIV transmission dynamics predict elimination at a later point in time, after 20 to 25 y. Importantly, the most comprehensive model predicts that the current strategy of ART at CD4 count ≤350 cells/µl will also lead to elimination, albeit 10 y later compared to UTT. Still, UTT remains cost-effective, as many additional life-years would be saved. The study's major limitations are that elimination was defined as incidence below 1/1,000 person-years rather than 0% prevalence, and drug resistance was not modeled.Conclusions:
Our results confirm previous predictions that the HIV epidemic in South Africa can be eliminated through universal testing and immediate treatment at 90% coverage. However, more realistic models show that elimination is likely to occur at a much later point in time than the initial model suggested. Also, UTT is a cost-effective intervention, but less cost-effective than previously predicted because the current South African ART treatment policy alone could already drive HIV into elimination.
Please see later in the article for the Editors' Summary
Published in the journal: . PLoS Med 10(10): e32767. doi:10.1371/journal.pmed.1001534
Category: Research Article
doi: https://doi.org/10.1371/journal.pmed.1001534Summary
Background:
Expanded access to antiretroviral therapy (ART) using universal test and treat (UTT) has been suggested as a strategy to eliminate HIV in South Africa within 7 y based on an influential mathematical modeling study. However, the underlying deterministic model was criticized widely, and other modeling studies did not always confirm the study's finding. The objective of our study is to better understand the implications of different model structures and assumptions, so as to arrive at the best possible predictions of the long-term impact of UTT and the possibility of elimination of HIV.Methods and Findings:
We developed nine structurally different mathematical models of the South African HIV epidemic in a stepwise approach of increasing complexity and realism. The simplest model resembles the initial deterministic model, while the most comprehensive model is the stochastic microsimulation model STDSIM, which includes sexual networks and HIV stages with different degrees of infectiousness. We defined UTT as annual screening and immediate ART for all HIV-infected adults, starting at 13% in January 2012 and scaled up to 90% coverage by January 2019. All models predict elimination, yet those that capture more processes underlying the HIV transmission dynamics predict elimination at a later point in time, after 20 to 25 y. Importantly, the most comprehensive model predicts that the current strategy of ART at CD4 count ≤350 cells/µl will also lead to elimination, albeit 10 y later compared to UTT. Still, UTT remains cost-effective, as many additional life-years would be saved. The study's major limitations are that elimination was defined as incidence below 1/1,000 person-years rather than 0% prevalence, and drug resistance was not modeled.Conclusions:
Our results confirm previous predictions that the HIV epidemic in South Africa can be eliminated through universal testing and immediate treatment at 90% coverage. However, more realistic models show that elimination is likely to occur at a much later point in time than the initial model suggested. Also, UTT is a cost-effective intervention, but less cost-effective than previously predicted because the current South African ART treatment policy alone could already drive HIV into elimination.
Please see later in the article for the Editors' SummaryIntroduction
South Africa is home to the largest population of HIV-infected individuals worldwide, with nearly 6 million people living with HIV in 2010 [1]. Although extensive efforts to curb the epidemic may have resulted in some decline in the number of new HIV infections among young adults in the past few years [2],[3], incidence levels remain considerable. The proof of concept that antiretroviral therapy (ART) can be used to prevent onward transmission [4],[5], created renewed excitement that a turning point in the ever-growing HIV epidemic could be achieved by expanding access to treatment. “Treatment as prevention” (treatment of all HIV-infected individuals with ART, regardless of CD4 cell count, in order to reduce transmission)—a hypothesized HIV prevention intervention that is currently being tested in community randomized trials [6]—was conceptually designed by mathematical models [7]–[13]. In 2009, Granich et al. suggested that the HIV epidemic in South Africa could be driven into an elimination phase (defined as an incidence of below one new infection per 1,000 person-years) after just 7 y of annual HIV screening for individuals aged 15 y and older and immediate ART for all HIV-infected patients (universal test and treat [UTT]) [9].
In response to these results, other modeling studies also examined the potential impact of a UTT intervention in various settings [14]–[19]. But there are as many different conclusions as there are models that investigated the issue. As models are profoundly different in many aspects—structure, parameterization, and assumptions about the intervention—it is difficult to determine which factors are responsible for the differences in the model predictions [20]. There are several obvious reasons for these discrepancies, such as differences in the time horizon of the analysis [14], less or more optimistic assumptions regarding programmatic efficacy [14],[18], or different assumptions about HIV natural history, heterogeneity in transmission, and ART effectiveness in reducing infectiousness [17]. For example, Granich et al. assumed a 99.4% reduction in infectiousness of those on ART [9], but later studies suggested that this reduction is likely to be too optimistic [4],[21]–[23]. The HPTN 052 trial showed a reduction of 96% [4] with trial participants completely adhering to treatment, which is unlikely in large-scale interventions. A Cochrane review including all observational studies and the HPTN 052 trial reported a reduction in transmission of about 86% [21]. Also, the ongoing treatment rollout following the 2010 World Health Organization (WHO) treatment guidelines of ART at CD4 cell counts of ≤350 cells/µl [24] will already have a profound impact on the HIV epidemic [25],[26], making it important to compare the impact of UTT with the current treatment scale-up. Nevertheless, these obvious differences explain only part of the variation between model predictions [20]. As modeling remains essential to further inform public health decision-making, it is vital to better understand the reasons for the discrepancies between models.
We examined the impact of model structure and parameterization on the estimated impact of UTT in South Africa in a highly controlled experiment as follows: we developed nine structurally different models of the South African HIV epidemic with a standardized core set of assumptions but with gradated degrees of model complexity and realism that span from the very simplest to one of the most comprehensive representations of HIV epidemics (Figure 1). In all models, we examined the impact of the UTT intervention suggested by Granich et al. [9] and related this to a baseline of no UTT (i.e., no ART in the simplest models, and rollout of ART at CD4 count ≤350 cells/µl as currently applied in South Africa in the most detailed model).
Fig. 1. Stepwise approach of developing nine structurally different models with increasing complexity and realism. 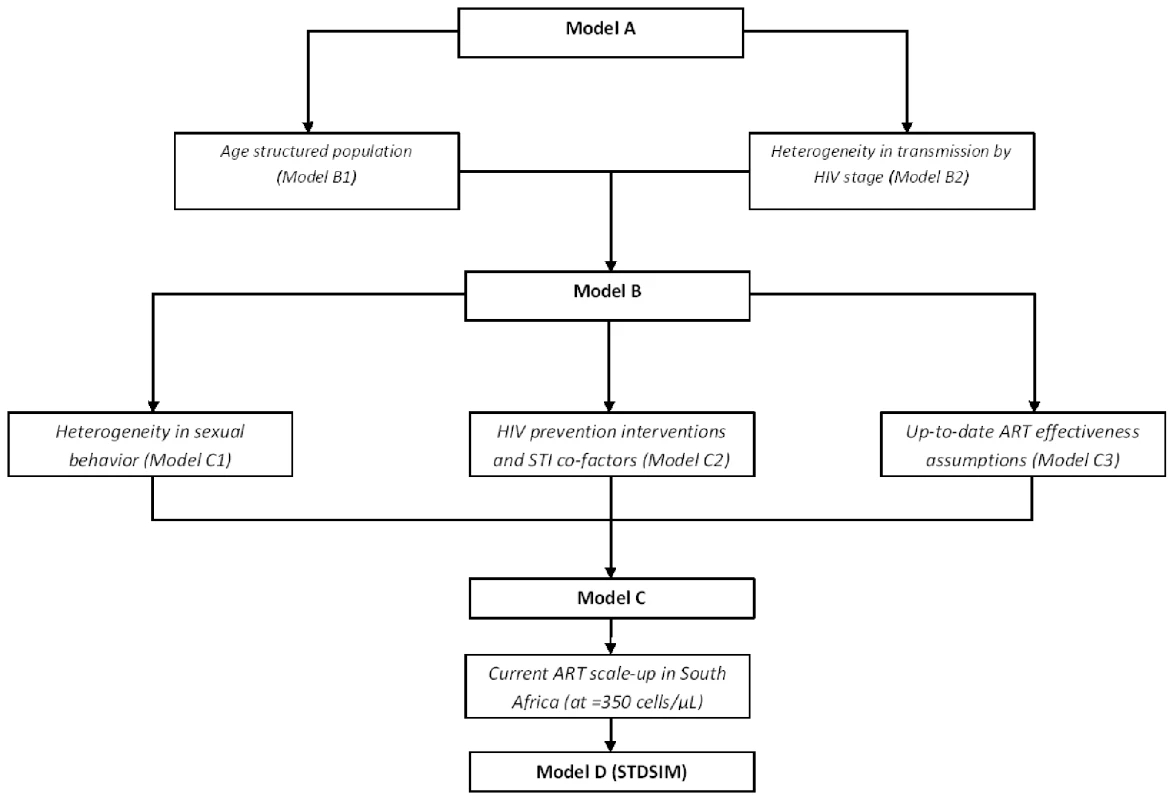
Model A resembles the deterministic model used by Granich et al. [9], now simulated using an event-driven approach. Models A and B are fitted to predict UNAIDS prevalence levels for South Africa by tuning the HIV transmission probabilities and year of HIV introduction. In addition, similar to Granich et al. [9], models A and B use a prevalence density function to explain the steady-state HIV prevalence observed in South Africa. Models C and D are fitted to represent UNAIDS-predicted HIV prevalence by adjusting overall partner change rates and the year of HIV introduction. A prevalence density function is no longer used, and the scaling-up of condom use in the late 1990s/early 2000s—introduced in model C2 and consistent with observations [2],[3]—is now used to explain the steady-state HIV prevalence in South Africa. Finally, models C and D allow for more realistic assumptions on the effectiveness of ART in reducing infectiousness (infectiousness reduction of 90% [20]–[22] instead of 99.4%; survival twice as high [26]). Methods
We developed four structurally different main models (models A, B, C, and D) and five sub-models (sub-models B1, B2, C1, C2, and C3) of the South African HIV epidemic through a stepwise approach of increasing complexity and realism (Figure 1; Table 1). With all models, we compare the impact of UTT to a no-UTT counterfactual (i.e., no ART in models A to C, and rollout of ART at CD4 count ≤350 cells/µl as currently applied in South Africa in model D). We used the STDSIM framework as a basis for all nine models. STDSIM is a stochastic microsimulation model that simulates the life course of individuals in a dynamic network of sexual contacts [27]. Events like partnership formation and the acquisition of infection are the result of random processes, determined by probability distributions. Therefore, the results are subject to stochastic variation, and the results in our study are based on the average of 1,000 runs.
Tab. 1. Overview of successive addition of components and structures to each of the nine models. 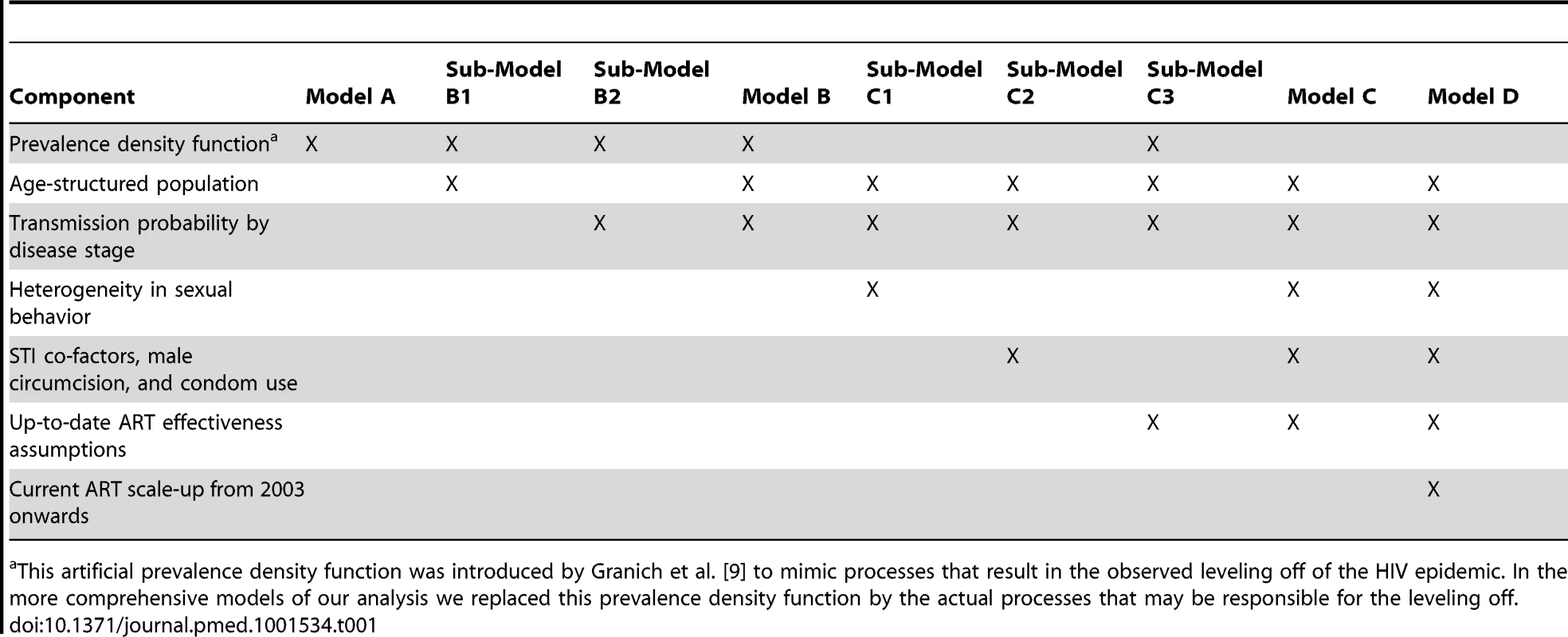
This artificial prevalence density function was introduced by Granich et al. [9] to mimic processes that result in the observed leveling off of the HIV epidemic. In the more comprehensive models of our analysis we replaced this prevalence density function by the actual processes that may be responsible for the leveling off. The STDSIM model consists of four modules: demography, sexual behavior, transmission and natural history, and interventions. The demography module covers the processes of birth, death, and migration. Processes for initiation and dissolution of sexual relationships, mixing according to age preference, sexual contacts within relationships, and sexual contacts between female sex workers (FSWs) and their male clients are defined in the sexual behavior module. In the transmission and natural history module, transmission probabilities per sexual contact are specified for HIV and five other sexually transmitted infections (STIs): chancroid, chlamydia, gonorrhea, syphilis, and herpes simplex virus 2. The interventions module specifies the timing and effectiveness of control measures in curbing transmission (e.g., condom use) or enhancing survival (e.g., ART). STDSIM has been extensively used to evaluate behavioral interventions [28]–[31], syndromic treatment for STIs [32],[33], male circumcision [34], different HIV epidemics in sub-Saharan Africa [35], and, more recently, the impact of ART on HIV epidemics [25],[36]–[38]. STDSIM can be used in various levels of complexity by adding or removing components from the model. We exploit this flexibility to evaluate the test and treat strategy with alternative model structures.
Model A
Model A fully resembles the deterministic model developed by Granich et al. [9], but now simulated using an event-driven stochastic approach. All individuals in the model constitute a homogeneous mixture of people in which HIV spreads from person to person. Individuals are assumed to have a one-off sexual contact with a random individual of the opposite sex every 8.5 d. We simulate a population aged 15–65 y with a constant background mortality rate of 0.025 per year. HIV is modeled in four consecutive stages with equal duration (30 mo) and transmission probabilities, and is introduced in the model by randomly “infecting” ten men and ten women. ART is assumed to decrease infectiousness by 99%, and the duration of the HIV stages for patients on ART is twice the duration of the stages for ART-naïve individuals [9]. In addition, as in the Granich model, transmission rates are further reduced by 40% because of simultaneous scale-up of other prevention interventions [9]. In accordance with Granich et al., we adjust transmission rates according to HIV prevalence through a prevalence density function to arrive at the observed steady state in HIV prevalence [9]: p(t1) = p(t0)×e−xP; where p = HIV transmission probability and P = HIV prevalence.
Model B
To arrive at model B, we extended model A by adding the age-specific fertility and background mortality rates of South Africa (sub-model B1), and different stages of HIV disease progression (acute infection, asymptomatic infection, symptomatic infection, and AIDS—sub-model B2). Births are assigned randomly to sexually active women between the ages 15 and 49 y, and the probability of having a child depends on the age of the woman. We parameterized the model with Unite Nations–reported data on age-specific fertility rates for South Africa (Table S1) [39]. The resulting initial total fertility rate (defined as the expected lifetime number of births per woman) equals 4.9 births per woman. We reduced all age-specific fertility rates with equal factors in order to capture declines in fertility rates as observed in South Africa (Figure S1A) [39]. At birth, the age at (non-HIV) death of each individual is drawn from predefined sex-specific survival curves. In order to obtain background mortality rates in the absence of HIV for South Africa, we corrected the age - and sex-specific mortality rates for South Africa reported by WHO [40] using the cause-specific mortality estimates from WHO burden of disease estimates [41]. The resulting survival curve is shown in Figure S1B.
In sub-model B2, we added the following HIV disease progression: (i) early/acute infection with a median duration of 3 mo, (ii) asymptomatic infection with a median duration of 5 y, (iii) symptomatic infection with a median duration of 4 y, and (iv) AIDS with a median duration of 8 mo. All stages are exponentially distributed, and the resulting overall survival distribution has a median of 10 y and an interquartile range of 8 to 13 y, consistent with observations [42],[43]. Relative to asymptomatic infection (second stage), transmission probabilities are increased by a factor 15 during early/acute infection, a factor three during symptomatic infection, and a factor 7.5 during the AIDS stage [35],[44]. In addition, we assumed that the sexual activity of HIV-infected patients in the AIDS stage (last 40 wk of life) is reduced by 50% because of ill health [45].
Model C
We extended model B with three components to arrive at model C. We added heterogeneity in sexual behavior (sub-model C1) by including different kinds of relationships. We use the same patterns of mixing as recently used by Hontelez et al. for a rural South African setting (the Hlabisa sub-district of KwaZulu-Natal) [25],[36],[37]. The model contains three types of sexual relationships: steady relationships, casual relationships, and commercial sex. The formation of partnerships occurs according to a supply-and-demand-based mechanism. People become available for a sexual relationship at an “age of sexual debut” that is randomly drawn at birth from a uniform distribution (Table S2). Each time the partnership status of a person changes (e.g., a partnership is formed or ended), a new duration until the person becomes available for a new relationship (“time until availability”) is drawn from a predefined exponential distribution with μ being the mean time until availability defined as: μ = τs,r/(rs,a×p), with τs,r = time interval by person's sex (s) and relationship status (r), rs,a = specific promiscuity factor by sex (s) and age (a), and p = personal promiscuity factor. The personal promiscuity factor (p) reflects the heterogeneity between individuals in the tendency to form partnerships, and is given by a gamma distribution with an average value (pm) of 1.0, and a shape parameter of 1.5 [35].
The duration of the availability period of an individual is given by an exponential distribution, with mean time to find (κ) defined as: , where the value of δ is 0.25 y for men and 2.25 y for women (Table S2) [30]. rs,a and p are explained above. When a person is available for a new relationship, he/she can be selected by an individual of the opposite sex who is at the end of his/her availability period. If a person has not been selected by the end of his/her availability period, he/she will select a partner from the pool of available persons of the opposite sex. The type of relationship (steady or casual) that is formed when a partner is selected depends on the age of the male partner, and is defined as the probability of a steady relationship (Table S2). The probability of a new relationship being a casual relationship is given by one minus the probability of a steady relationship. A relationship starts with a sexual contact. After each contact, the time until a new sexual contact q within the relationship is drawn from an exponential distribution with a mean frequency of sexual contact depending on relationship type and the age of the male partner (Table S2). Finally, the duration of a new relationship is drawn from an exponential distribution, where the average relationship duration depends on the relationship type (Table S2).
Partner selection at the end of the time to find κ is guided through an age preference matrix (Table S3), which defines the probability of selecting a partner from a certain age class. When there is no partner available in the preferred age class, immediate resampling is done of a new preferred age class using the remaining age groups with a probability larger than 0. If no partner can be found in any of the age classes, a new κ value is drawn from the above described equation. Probabilities in the age preference matrix are chosen to have men prefer slightly younger women. Preference matrices for both sexes are given in Table S3.
In the model, men can have sexual contacts with FSWs. A man's frequency of sexual contacts with a FSW is determined by defining frequency classes (in this study 0, 1, and 12 times per year [25],[35]). For each class, the proportion of men with and without a steady relationship falling in that category can be specified. A personal “prostitute-visiting inclination,” assigned to each male at birth, determines which individual men are assigned to which frequency classes. At sexual debut and at each sexual contact with a FSW, the next sexual contact with a FSW is scheduled according to an exponential distribution, with the mean duration until next contact based on the FSW contact frequency class of the individual.
The number of FSWs in the model results from male demand. New FSWs are recruited from sexually active women with a defined age range. The number of available FSWs and their predefined number of clients per week is checked each year and matched with the number of male contacts with FSWs. If the number FSWs is too low, new FSWs are recruited. If the number is too high, a random selection of FSWs terminate their career. For this study, we used the same values for number of FSWs and number of male contacts with FSWs as previously used for KwaZulu-Natal, South Africa [25] (Table S4).
In model C2, we added male circumcision (prevalence = 35% [46],[47]; reduces the risk of HIV acquisition by 50% [48]–[50]) and STIs that act as co-factors for HIV transmission (chlamydia, gonorrhea, chancroid, syphilis, and herpes simplex virus 2). Natural history and transmission assumptions for all STIs are described in Table S5. In addition, the model allows for increasing rates of condom use in the late 1990s/early 2000s, consistent with observations [2],[3], to replace the prevalence density function used in models A and B.
Sub-model C3 uses more up-to-date assumptions regarding the effectiveness of ART in reducing HIV transmission and enhancing survival. Granich et al. assumed that ART reduces infectiousness by 99% [9]. However, recent observational studies and a randomized controlled trial showed that effectiveness is likely to be lower [21]–[23]. A meta-analysis of observational studies found an average reduction of 92% [22], which was later also reported by Donnell et al. [23]. The HPTN 052 trial showed a reduction of 96% [4]; however, the participants in the trial were completely adherent to treatment, which is unlikely in large-scale interventions. A Cochrane review including all observational studies and the HPTN 052 trial reported a reduction in transmission as a result of ART of about 86% [21]. Here, we assume a 90% efficacy in reducing transmission, implicitly allowing for imperfect adherence. In addition, Granich et al. assumed that ART increases survival of HIV-infected patients by a factor of two relative to their remaining life expectancy without HIV treatment. We assume the survival benefit of ART to be twice as high as assumed by Granich et al. (i.e., a factor four increase), consistent with observations [51].
Model D
Model D resembles the full STDSIM model [25],[35]–[38], consisting of all of the features in model C but with two important additions: CD4 cell count decline during disease progression and the ART rollout in South Africa for the period 2004–2011. Based on data from Orange Farm, South Africa, we assumed that the initial (HIV-negative) CD4 cell count in the population follows a lognormal distribution with median 7.02 (equivalent to 1,116 cells/µl) [52]. CD4 cell counts decline by 25% during acute infection, and decline linearly over the other stages until the CD4 cell count reaches 0.5% of its initial value, after which an individual dies of AIDS [9],[25],[52]. Therefore, based on average HIV-negative CD4 cell counts and duration of HIV infection, an individual will, on average, reach a CD4 cell count of ≤350 cells/µl about 6 y following infection, and at that point will have a remaining life expectancy of about 4 y.
In the model, ART coverage is the result of two components: (i) an individual's demand for ART as a function of HIV disease stage, and (ii) the capacity of the health system to meet this demand. ART coverage in our model is the ART demand met by the capacity of the health system. We assumed the ART demand function to be the same as previously estimated for the Hlabisa sub-district of KwaZulu-Natal, South Africa [25], in which about 30% of all infected individuals first seek care for HIV well after their CD4 cell count has dropped below 200 cells/µl. We fitted the model predictions to observed ART coverage levels over the period July 2004–July 2010 by performing a grid search on three parameters: start year of ART scale-up, rate of ART scale-up, and ART scale-up function (three options: linear, square-root, or quadratic). We optimized predicted ART coverage by calculating the mean squared error of predicted ART coverage in the model compared to coverage data reported by WHO [53]. We assumed that eligibility criteria changed from ART at CD4 count ≤200 cells/µl to ART at CD4 count ≤350 cells/µl in August 2011, and that ART scale-up continued according to the estimated scale-up pattern for the years 2012–2050 in the baseline.
Model Fitting and Parameter Uncertainty
We fitted all models to replicate the observed HIV prevalence in South Africa as reported by the Joint United Nations Programme on HIV/AIDS (UNAIDS) [1]. For each model, we used the parameters of three aspects that link directly to three different characteristics of the HIV epidemic in South Africa: (i) the start of the epidemic, (ii) the growth of the epidemic over the 1990s, and (iii) leveling off of the epidemic in the early 2000s. We obtained the best fit by minimizing the squared errors of predicted and reported HIV prevalence over the period 1990–2010.
We used the following parameters to fit the models/sub-models A, B1, B2, B, and C3: (i) year of HIV introduction, (ii) transmission probabilities in men with asymptomatic HIV; (iii) the x parameter in the prevalence density function. We fitted sub-model C1 in 2 parts: (i) the initial growth of the epidemic in the 1990s, and (ii) the leveling off of the epidemic in the 2000s. For step 1, we fitted three parameters: year of HIV introduction, HIV transmission probabilities in individuals with asymptomatic HIV, and relative partner change rates (multiplying all values of sex - and age-specific promiscuity—see above—by a certain factor). For step 2, we assumed changes in the observed leveling off of the HIV epidemic to be the result of behavior change—defined as changes in relative partner change rates—and used three parameters: year of start of behavior change, rate of change in behavior change, and end year of behavior. The sexual behavior pattern resulting from the best fit by sex and age for the year 1990 (start of the epidemic) is given in Figure S2, and for the year 2003 (after above described reduction in risk behavior) in Figure S3. We used the following parameters to fit sub-model C2 to observed HIV prevalence levels: (i) year of introduction of HIV, (ii) transmission probabilities in individuals with asymptomatic HIV, and (iii) scale-up of condom use over time. We assume a stepwise linear increase of condom use over time, and estimate the start year, slope, and end year of the scale-up that results in the best-fitting HIV prevalence. For models C and D, we fixed the HIV transmission probability in individuals with asymptomatic HIV at 0.001 for men and 0.0005 for women [12]. In order to start the epidemic, we introduced HIV in six FSWs. We used the following parameters to fit the model: (i) year of HIV introduction, (ii) relative partner change rates, and (iii) start year, rate, and end year of condom use scale-up in casual relations and commercial sex. The best fit for model D resulted in a 30% condom use rate in casual relationships, which is comparable to data [54].
We calculated a range around the baseline estimates reflecting the uncertainty in the parameters that were used to fit all nine models. We developed uniform distributions with intervals wide enough to capture all possible parameter values that could produce a good fit (defined as a predicted HIV prevalence within the uncertainty interval provided by UNAIDS for the period 1995 to 2010 [1]), and randomly drew values from these distributions to serve as model input. We ran the model with these parameter values, and accepted parameter value combinations only when they produced a good fit. For all parameter value combinations for which this was the case, we recalculated all the outcomes of the study.
For model D (the most comprehensive model in our analysis) we repeated this procedure until we arrived at 120 alternative parameter values that were accepted based on the above mentioned criterion, and calculated all main outcomes of this study with these alternative parameter settings. We developed ranges reflecting parameter uncertainty by discarding the three highest and lowest values for each outcome. For all other models and sub-models, we repeated the procedure until we arrived at 40 alternative parameter values that were accepted, and discarded only the single highest and lowest outcome values in order to crudely arrive at the interval. We incorporated the intervals resulting from this parameter uncertainty analysis as bars and ranges in graphs and tables. A visual representation of all parameter combinations that were used to calculate uncertainty ranges, including the combinations that produced the highest and lowest values that were later discarded, is given in Figure S4.
Scenarios and Outcomes
For all nine models we predicted the impact of a hypothetical UTT intervention with annual screening of individuals aged 15+ y and immediate ART for those who are infected with HIV, as modeled by Granich et al., i.e., the intervention is scaled up linearly to 90% coverage in seven years' time (2012–2019), and there is a dropout rate of 8.5% in the first year of treatment and 1.5% in subsequent years [9]. We assume no further scale-up of other prevention interventions (e.g., condom use, circumcision) after 2012 in all models. Following Granich et al. we defined the “elimination phase” of HIV to start when HIV incidence drops below 1 new infection per 1,000 person-years [9].
Furthermore, we calculated the cumulative number of life-years saved and cumulative net costs of UTT compared to continued scale-up of ART at CD4 count ≤350 cells/µl in model D, the only model that incorporates enough detail to be able to adequately represent the current scale-up of ART at CD4 count ≤350 cells/µl in South Africa as the baseline of no UTT. We analyzed costs from the health care sector perspective, and assumed ART costs similar to those in Hontelez et al. [25]—where annual ART costs were stratified by CD4 cell count at initiation and thereafter dependent on the number of years on treatment (Table 2)—which were derived from ART programs in Cape Town, South Africa [55],[56]. Costs include costs for ART provision, treatment of opportunistic infections, outpatient visits, and inpatient days. Costs were stratified by CD4 cell count at initiation since those initiating treatment at late stages (low CD4 cell count) are more likely to have opportunistic infections and other complications, thus requiring more additional care. This difference disappears after subsequent years of successful treatment. We assumed annual ART costs for those initiating ART at CD4 cell counts of >350 cells/µl to be similar to the costs for those who initiated at 200–350 cells/µl and were on treatment for more than 2 y. For the UTT scenario, in which treatment initiation is not guided by CD4 cell count, we lowered all cost input values in the first year of treatment by US$104 to subtract the cost of a CD4 cell count test [25]. We discounted future costs and life-years saved by 3% annually [57].
Tab. 2. Cost input values used in this study. 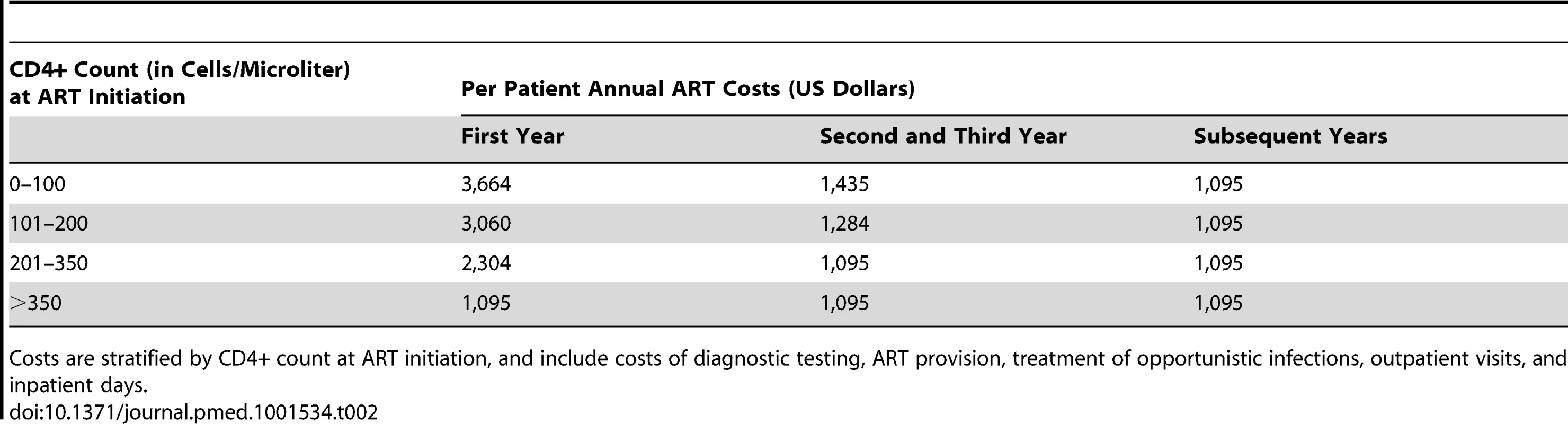
Costs are stratified by CD4+ count at ART initiation, and include costs of diagnostic testing, ART provision, treatment of opportunistic infections, outpatient visits, and inpatient days. Finally, we performed a sensitivity analysis on all the results from model D by varying parameters of HIV natural history, heterogeneity in HIV transmission, the state of the HIV epidemic in South Africa, more and less optimistic UTT intervention outcomes, and the assumptions on overall cost and scale effects. Details on the sensitivity analysis can be found in Text S1.
Results
Figure 2 (left panels) shows the fit of all models to the HIV prevalence in South Africa as reported by UNAIDS [1], together with the projected impact of annual screening of individuals aged 15+ y and immediate ART for all HIV-infected patients at 90% coverage. All models replicate the HIV prevalence in South Africa in the period 1990–2010. However, as a result of the difference in underlying processes in the structurally different models, the corresponding HIV incidence levels are substantially different (Figure 2, right panels). For example, the predicted incidence in 2011 for model A was 2.0/100 person-years, while for model D this was only 1.0/100 person-years (right panels of Figure 2). Also, projections regarding the future course of the HIV epidemic in the absence of UTT differ substantially. Future incidence and prevalence in the absence of treatment reach a steady state in models A and B, as indicated by the dashed lines. In model C, the incidence and prevalence of HIV already decline in the no-intervention scenario because of the increase in condom use in the early 2000s. Such a decline is even more profound in model D, where current ART scale-up in South Africa is included.
Fig. 2. Predicted impact of universal testing and immediate ART for all HIV-infected patients (UTT) on HIV prevalence and incidence in adults (aged 15+ y) for four main models of the South African HIV epidemic over the period 1990–2050. 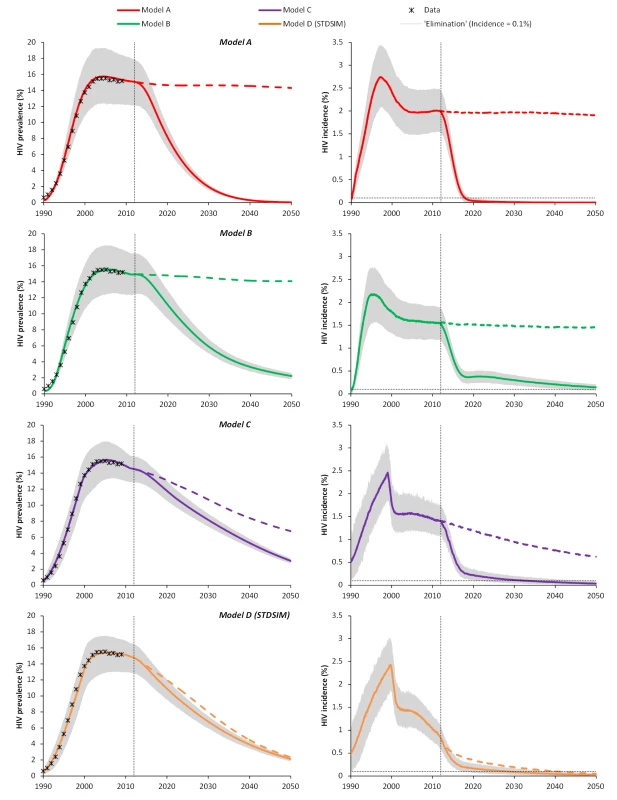
Left panels: HIV prevalence; right panels: HIV incidence. All models are structurally different. Solid lines represent the impact of the UTT intervention; the dashed lines represent the no-UTT counterfactual. Colored lines are the average result of 1,000 simulations, and the gray areas represent the probability intervals illustrating 95% of the stochastic variation around the baseline estimate. UTT is implemented as annual screening of the adult population (aged 15+ y), and immediate ART for all HIV-infected patients. The intervention is scaled up linearly, starting in 2012 and reaching 90% coverage in 2019 (similar to Granich et al. [9]). The vertical dotted lines give the timing of the start of the intervention. The horizontal dotted lines in the right panels indicate the elimination phase, defined as incidence below 1/1,000 person-years. Structures and components of the different models are explained in Figure 1. All models are consistent in predicting that HIV will eventually be eliminated by UTT. However, the timing of elimination significantly differs between the models (Figure 2; Table 3). In model A, the HIV epidemic is driven into an elimination phase after 7 y (range: 6; 9), while in models B, C, and D the elimination phase is reached only after 39 (range: 30; 49), 21 (range: 19; 30), and 17 (range: 15; 23) y, respectively. For model D, the HIV incidence is even projected to reach the elimination phase in 2041 (range: 2037; 2047) without the full UTT intervention, because of the impact of the current scale-up of ART at CD4 cell counts of ≤350 cells/µl.
Tab. 3. Year of HIV elimination (incidence <1/1,000 person-years) under universal testing and immediate ART for all HIV-infected patients (UTT) and number of life-years saved through UTT compared to the baseline of no UTT. 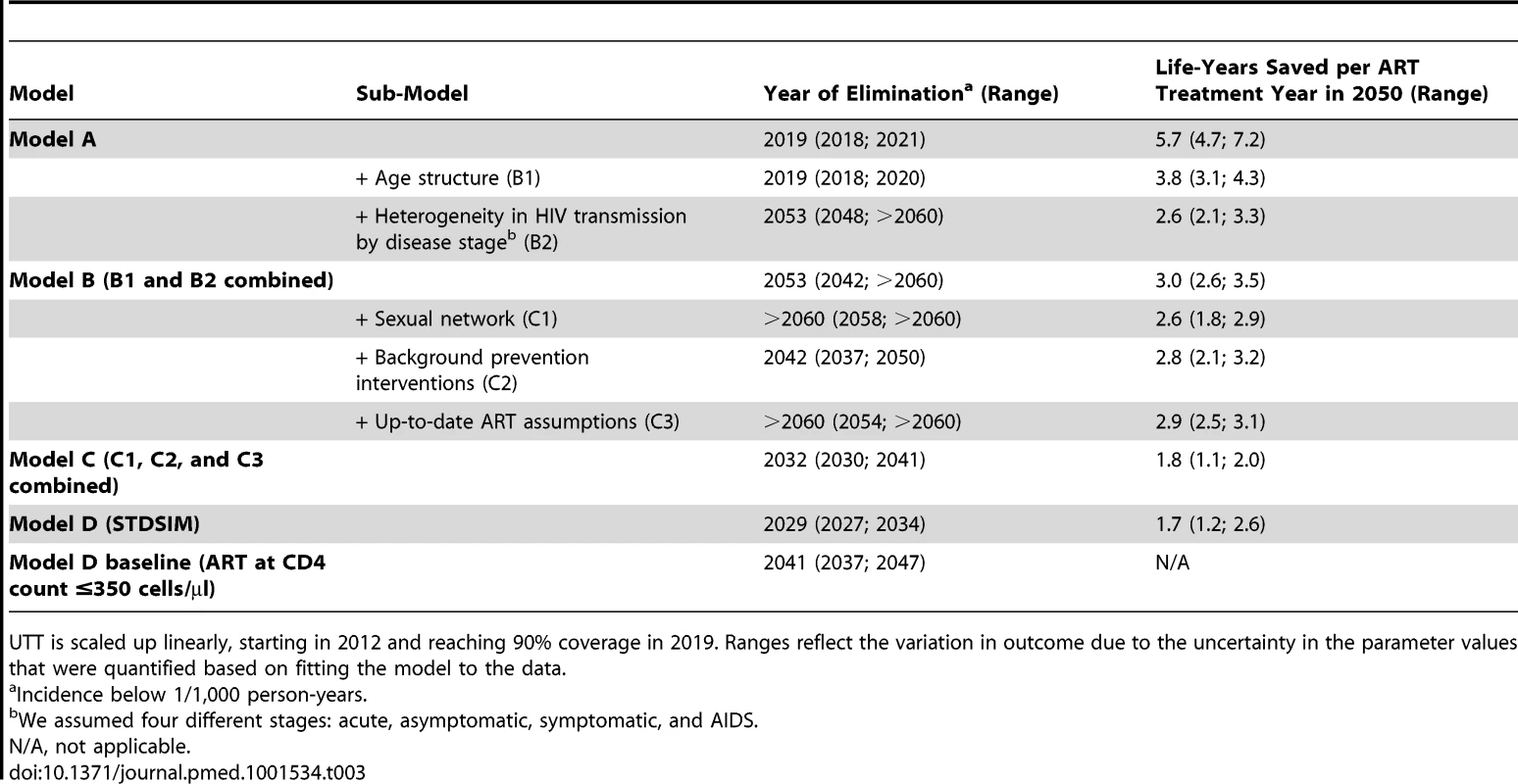
UTT is scaled up linearly, starting in 2012 and reaching 90% coverage in 2019. Ranges reflect the variation in outcome due to the uncertainty in the parameter values that were quantified based on fitting the model to the data. The sub-models B2, C1, and C3 do not predict elimination of HIV by 2050 (Table 3; Figure S5). The combination of a high background mortality and heterogeneity in HIV transmission (model B2) results in a disproportionate contribution of acute infection to the overall epidemic (as many HIV-infected patients die because of other causes), thereby limiting the potential impact of UTT. Heterogeneity in sexual behavior also prolongs the predicted time to elimination (sub-model C1), as it accounts for high-risk individuals who continue to spread HIV even in the presence of ART. Finally, it is obvious that more up-to-date assumptions on ART effectiveness result in a lower predicted impact of UTT (sub-model C3), as the reduction in infectiousness is lower (90% versus 99.4%) and survival is higher (twice as high compared to Granich et al. [9]). On the other hand, explicitly modeling background prevention interventions and STI co-factors (sub-model C2) instead of using a simple prevalence density function shortens the time until elimination, as the interventions scaled up before 2012 affect the dynamics of the epidemic in the long run, reducing incidence even without UTT or further scale-up of other interventions (dashed line for model C in Figure 2).
There are substantial differences in the impact of UTT compared to the no-UTT baseline in the different models, which has important consequences for the effectiveness of the intervention. By 2050, a cumulative total of 1,800 new infections per 100,000 person-years (range: 1,600; 2,500) would be averted in model A, while this value is only 100 (range: 83; 150) in model D (Figure 3A). Consequently, the predicted efficiency of ART in saving lives also differs substantially between models (Figure 3B). Model A predicts about 5.7 cumulative life-years saved per treatment year by 2050 (range: 4.7; 7.2), while in model D this value is only 1.7 (range: 1.2; 2.6), almost four times lower.
Fig. 3. Number of infections averted per 100,000 person-years and cumulative number of life-years saved per ART treatment year for universal testing and immediate ART for all HIV-infected patients (UTT) in South Africa over the period 2010–2050. 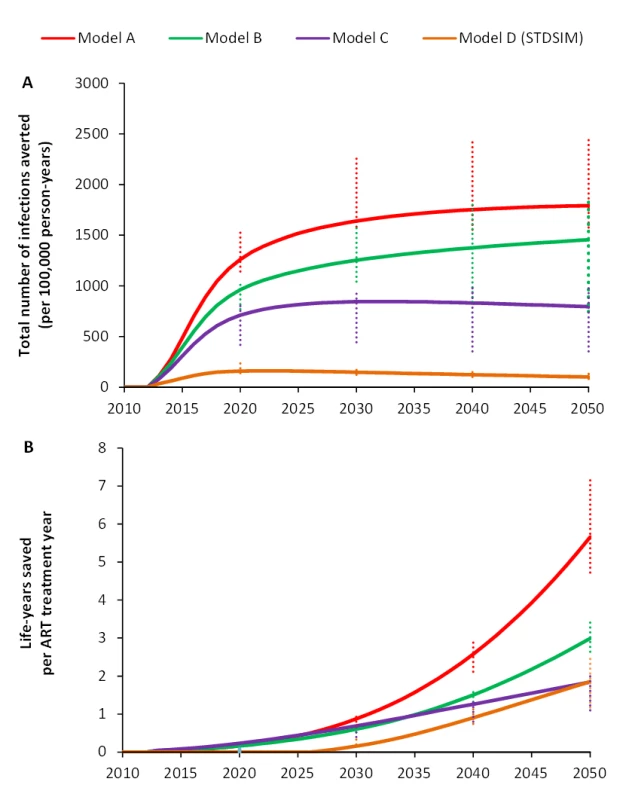
The intervention consists of annual screening of the adult population (aged 15+ y), and immediate ART for all HIV-infected patients. Intervention is scaled up linearly starting in 2012 and reaching 90% coverage in 2019. (A) Difference between cumulative numbers of new infections per 100,000 person-years in the UTT intervention scenario versus the baseline (for models A, B, and C, the baseline is no ART; for model D, the baseline is ART at CD4 count ≤350 cells/µl). (B) Cumulative number of life-years saved per person-year on ART treatment in the UTT intervention compared to the baseline (for models A, B, and C, the baseline is no ART; for model D, the baseline is ART at CD4 count ≤350 cells/µl). Error bars reflect ranges due to the uncertainty in the parameter values that were quantified based on fitting the model to the data. Model D shows that cumulative net costs peak at US$3.8 billion (range: 3.1 billion; 4.7 billion) at around 2020, and decline thereafter as the impact of UTT on HIV incidence is translated into a lower number of patients on treatment (Figure 4A). Cumulative net costs reach about US$1.8 billion in 2050 (range: 0.25 billion; 3.5 billion). The effects of UTT will become apparent only around the year 2020, when the prevented infections translate into life-years saved (Figure 4B), and life-years saved increase linearly to 10.4 million by 2050 (range: 5.6 million; 16.1 million). The resulting incremental cost-effectiveness ratio is US$170/life-year saved (range: 19; 406) (Table 4). All results are robust to alternative assumptions and parameterizations (see sensitivity analysis in Text S1 and Tables S6, S7, S8).
Fig. 4. Cumulative net costs and cumulative number of life-years saved of universal testing and immediate ART for all HIV-infected patients (UTT) compared to the current rollout in South Africa of ART at CD4 count ≤350 cells/µl, as predicted with model D. 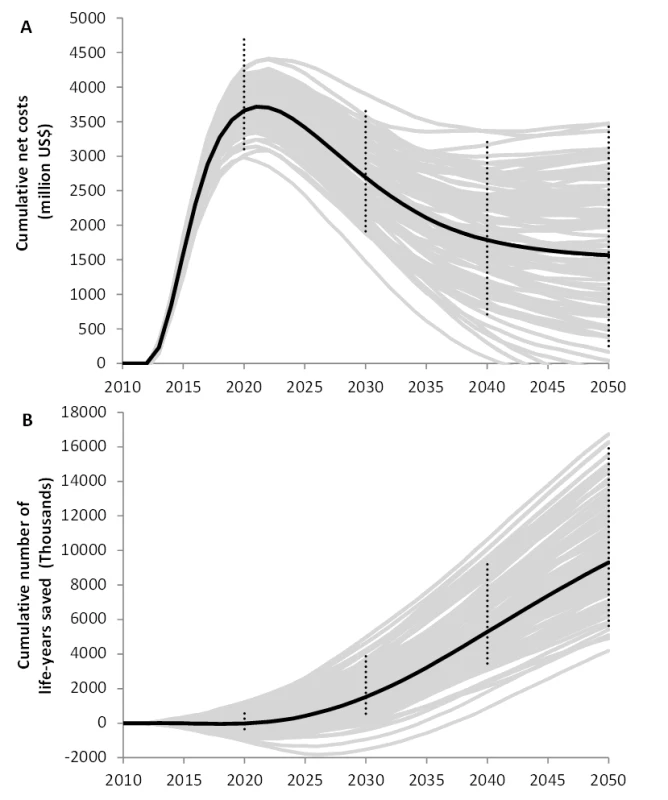
(A) Cumulative net costs; (B) cumulative number of life-years saved. Grey lines represent 100 individual model runs illustrating stochastic variation; black lines are averages over 1,000 model runs. Error bars reflect ranges due to uncertainty in the parameter values that were quantified based on fitting the model to data. Costs and life-years saved were discounted at an annual rate of 3%. Tab. 4. Effects, cost, and cost-effectiveness of universal test and treat versus continued scale-up of ART at CD4 count ≤350 cells/µl in South Africa over the period 2012–2050 (Model D). 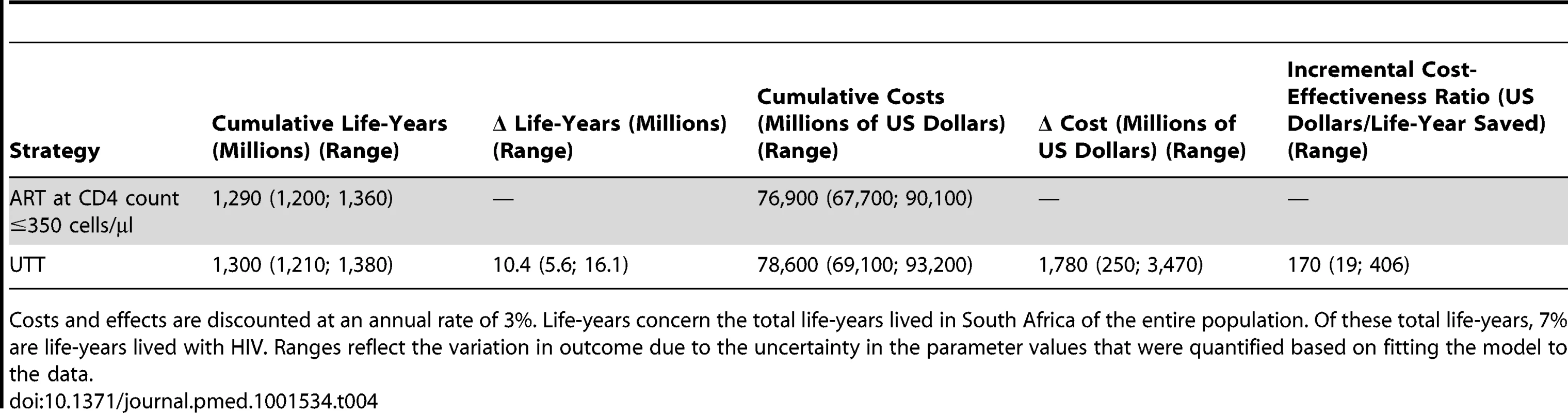
Costs and effects are discounted at an annual rate of 3%. Life-years concern the total life-years lived in South Africa of the entire population. Of these total life-years, 7% are life-years lived with HIV. Ranges reflect the variation in outcome due to the uncertainty in the parameter values that were quantified based on fitting the model to the data. Discussion
Our study confirms previous reports that an intervention of universal voluntary counseling and testing for individuals aged 15+ y and immediate ART for all HIV-infected individuals (UTT) at 90% coverage will eventually result in the elimination of HIV, even in a highly endemic setting such as South Africa and with realistic assumptions about the efficacy of ART in reducing HIV transmission and enhancing survival. However, the predicted timing of the elimination of HIV (defined as an incidence of below one new infection per 1,000 person-years) differs substantially for the different models in our study, and HIV elimination is likely to take three times longer than the mere 7 y predicted by Granich et al. [9]. In addition, the relative impact of the UTT intervention compared to the baseline differs substantially. Whereas 1,800 infections are averted per 100,000 person-years (range: 1,600; 2,500) in the simplest model, this value is only 100 (range: 83; 150) in the most comprehensive model. In fact, the latter model shows that the current scale-up of ART for patients with CD4 cell counts of ≤350 cells/µl already leads to elimination of HIV without the additional UTT intervention. However, the considerable number of life-years saved makes UTT at 90% coverage still a highly cost-effective intervention, with an incremental cost-effectiveness ratio of US$170/life-year saved (range: 19; 406).
Our sub-model analysis shows that choices in model structure and assumptions have an important impact on the predicted impact of UTT. It makes sense that more up-to-date assumptions on the overall efficacy of ART in reducing infectiousness (90% versus 99.4%) lead to delayed HIV elimination. Also, incorporating high infectiousness during the acute stage results in a less profound impact of UTT, since relatively many transmission events will then occur during this short period of high infectiousness, which is difficult to target in UTT interventions [17],[58]. Adding heterogeneity in sexual behavior and sexual networks to the model also increases the time until elimination—this is because the relative force of infection of HIV is high in certain high-risk groups (e.g., FSWs) and therefore the impact of UTT is less profound in these subgroups. Finally, explicitly modeling male circumcision, condom use, and STI co-factors, and using increases in condom use to quantify the HIV epidemic in South Africa [2],[3], decreases the time until HIV elimination, since the counterfactual of no UTT already shows a substantial decline in incidence, despite the fact that these interventions are not further scaled up in the model after 2012. A model that relies on implicit modeling of these interventions to capture the steady state (e.g., through a prevalence density function, as was used by Granich et al. [9]) will therefore overestimate the impact of UTT. Finally, it appears vital to incorporate the current ART rollout in the counterfactual scenario. The availability of ART in South Africa and many other African countries is now a fact of life, and the rollout that generally started in 2003–2004 is already affecting the epidemics through increased survival and decreased transmission [2].
Given that the stepwise inclusion of model components appeared to change the predicted impact of a UTT intervention, the model that incorporates all these components (model D) gives the most accurate prediction of the impact. In addition, although all models were able to accurately replicate the UNAIDS-reported HIV prevalence in South Africa, model D was the only model that was also able to capture the observed decline in incidence over the past decade [2],[3]. In model D, incidence in the population aged 15–49 y declined from 1.9/100 person-years in 2002 to 1.3/100 person-years in 2008, which is nearly the same as the observed reduction from 2.0/100 person-years in 2002–2005 to 1.3/100 person-years in 2005–2008, as reported by Rehle et al. [3]. Incidence rates in the other models remained constant over the same period (models A to C). In addition, model D was able to replicate data on demographic structure, age-specific HIV prevalence, sexual behavior, STI prevalence, and ART coverage in South Africa (Figure S7; Text S2). Finally, previous studies with STDSIM have shown that the model is capable of reproducing HIV prevalence (overall and age - and sex-specific), incidence, and mortality data from a population-based HIV and demographic surveillance site in KwaZulu-Natal, South Africa [25],[36],[37],[59],[60]. The simulated impact of ART in this highly endemic area of South Africa [25] was very similar to what was recently observed by Tanser et al. [5], providing reassurance that our model predictions are accurate.
To our knowledge, this is the first study that shows that the current rollout of ART for all HIV-infected patients with CD4 cell counts of ≤350 cells/µl will eventually eliminate HIV. This raises questions about the value for money of the additional investments required to implement UTT. Although we show that the UTT intervention proposed by Granich et al. [9] is highly cost-effective, the required number of health workers and financial resources for such a strategy far exceeds the current availability in South Africa [61]. Also, the assumed rates of HIV testing, ART uptake, retention in care, and treatment adherence are rather optimistic [62],[63]. Adherence and retention are likely to decrease when treatment is initiated at higher CD4 cell counts [64], while the number of patients lost to follow-up increases when treatment programs are scaled up [65]. Both these issues are especially important in UTT strategies, where patient numbers increase substantially, and many patients initiate ART at high CD4 cell counts. In addition, maintaining screening coverage levels at 90% for 40+ y seems not very plausible. It is likely that test refusal will be substantially higher than the 10% assumed in our analyses [66], increase over time [67], and be more common among people with HIV [67], resulting in a lower and declining screening coverage over time. Still, our sensitivity analysis shows that UTT would remain a cost-effective strategy, even with coverage rates of only 60%. A recent study on the cost-effectiveness of ART provision in South Africa showed that cost savings will be achieved after just 5 y of UTT at 90% coverage [68], while our modeling indicates that there will be no net savings from this UTT intervention in South Africa. The underlying compartmental transmission model in that study [68] is essentially the same as that previously used by Granich et al. [9],[68], and thus resembles our model A. We show that these types of models, which ignore sexual networks and background prevention interventions underlying the current South African epidemic, predict a far more optimistic impact of UTT compared to the baseline. Cost-effectiveness and economic impact studies based on such models should therefore be interpreted with caution. More research with comprehensive models of the impact of more modest UTT interventions is necessary in order to determine whether universal treatment for HIV really is a cost-effective intervention.
Our study has a number of limitations. We defined elimination as incidence below 1/1,000 person-years. However, real elimination is achieved when both incidence and prevalence reach 0%. Microsimulation allows for such an analysis, and we found that in a model population of about 35,000 people, by 2080, 99% of all model runs predict that HIV prevalence reaches 0% in model A (Figure S5). In model D this point is reached only in year 2116 for the UTT scenario, and in year 2164 for continued scale-up of ART at CD4 count ≤350 cells/µl (Figure S5). In addition, we did not model the development and transmission of drug-resistant strains. Both acquired resistance (development of resistance within an individual on treatment) and transmitted resistance (spread of drug-resistant strains) will have an impact on the effectiveness of treatment programs, and will consequently result in a less profound effect of the current ART scale-up or UTT in South Africa. It is currently unclear, however, to what extent the fears of rapidly spreading drug resistance expressed at the start of the ART scale-up were justified [69]. The prevalence of drug resistance remains low in South Africa after nearly 10 y of scaling up ART [70],[71]. In addition, adherence to treatment is as high as in many high-income countries [72], and survival of patients on treatment in sub-Saharan Africa approaches general life expectancy [73], suggesting that resistance may not become a major problem in South Africa in the near future.
Elimination of HIV in South Africa will have huge implications for public health and socioeconomic development in the country. The current ART rollout is already resulting in a substantial increase in the life expectancy of the general population [74] and in the employment rates of HIV-infected people [75]. Finally, elimination of HIV will also substantially reduce the tuberculosis burden in South Africa, given the close link between the two epidemics [76].
In conclusion, our results from a series of structurally different models support the main message from previous studies that HIV in South Africa can be eliminated through a strategy of annual screening of individuals aged 15+ y and immediate ART for all HIV-infected patients at 90% coverage, but elimination will occur substantially later than previously predicted. Importantly, the most comprehensive model suggests that HIV incidence in South Africa can reach the elimination phase even if the current treatment scale-up of ART at CD4 count ≤350 cells/µl continues without the addition of a UTT intervention. Results from upcoming community randomized trials of treatment as prevention will need to be evaluated with models that allow for sufficient detail in assumptions in order to adequately project the population-level impact and overall cost-effectiveness of the UTT intervention.
Supporting Information
Zdroje
1. Joint United Nations Programme on HIV/AIDS (2012) Report on the global AIDS epidemic 2012. Geneva: Joint United Nations Programme on HIV/AIDS.
2. JohnsonLF, HallettTB, RehleTM, DorringtonRE (2012) The effect of changes in condom usage and antiretroviral treatment coverage on human immunodeficiency virus incidence in South Africa: a model-based analysis. J R Soc Interface 9 : 1544–1554.
3. RehleTM, HallettTB, ShisanaO, Pillay-van WykV, ZumaK, et al. (2010) A decline in new HIV infections in South Africa: estimating HIV incidence from three national HIV surveys in 2002, 2005 and 2008. PLoS ONE 5: e11094 doi:10.1371/journal.pone.0011094
4. CohenMS, ChenYQ, McCauleyM, GambleT, HosseinipourMC, et al. (2011) Prevention of HIV-1 infection with early antiretroviral therapy. N Engl J Med 365 : 493–505.
5. TanserF, BärnighausenT, GrapsaE, ZaidiJ, NewellML (2013) High coverage of ART associated with decline in risk of HIV acquisition in rural KwaZulu-Natal, South Africa. Science 339 : 966–971.
6. DabisF, NewellML, HirschelB (2010) HIV drugs for treatment, and for prevention. Lancet 375 : 2056–2057.
7. BaggaleyRF, FergusonNM, GarnettGP (2005) The epidemiological impact of antiretroviral use predicted by mathematical models: a review. Emerg Themes Epidemiol 2 : 9.
8. BaggaleyRF, GarnettGP, FergusonNM (2006) Modelling the impact of antiretroviral use in resource-poor settings. PLoS Med 3: e124 doi:10.1371/journal.pmed.0030124
9. GranichRM, GilksCF, DyeC, De CockKM, WilliamsBG (2009) Universal voluntary HIV testing with immediate antiretroviral therapy as a strategy for elimination of HIV transmission: a mathematical model. Lancet 373 : 48–57.
10. MontanerJS, HoggR, WoodE, KerrT, TyndallM, et al. (2006) The case for expanding access to highly active antiretroviral therapy to curb the growth of the HIV epidemic. Lancet 368 : 531–536.
11. SalomonJA, HoganDR, StoverJ, StaneckiKA, WalkerN, et al. (2005) Integrating HIV prevention and treatment: from slogans to impact. PLoS Med 2: e16 doi:10.1371/journal.pmed.0020016
12. StoverJ, WalkerN, GarnettGP, SalomonJA, StaneckiKA, et al. (2002) Can we reverse the HIV/AIDS pandemic with an expanded response? Lancet 360 : 73–77.
13. Velasco-HernandezJX, GershengornHB, BlowerSM (2002) Could widespread use of combination antiretroviral therapy eradicate HIV epidemics? Lancet Infect Dis 2 : 487–493.
14. BendavidE, BrandeauML, WoodR, OwensDK (2010) Comparative effectiveness of HIV testing and treatment in highly endemic regions. Arch Intern Med 170 : 1347–1354.
15. DoddPJ, GarnettGP, HallettTB (2010) Examining the promise of HIV elimination by ‘test and treat’ in hyperendemic settings. AIDS 24 : 729–735.
16. KretzschmarME, van der LoeffMF, CoutinhoRA (2012) Elimination of HIV by test and treat: a phantom of wishful thinking? AIDS 26 : 247–248.
17. PowersKA, GhaniAC, MillerWC, HoffmanIF, PettiforAE, et al. (2011) The role of acute and early HIV infection in the spread of HIV and implications for transmission prevention strategies in Lilongwe, Malawi: a modelling study. Lancet 378 : 256–268.
18. WagnerBG, KahnJS, BlowerS (2010) Should we try to eliminate HIV epidemics by using a ‘test and treat’ strategy? AIDS 24 : 775–776.
19. WalenskyRP, PaltielAD, LosinaE, MorrisBL, ScottCA, et al. (2010) Test and treat DC: forecasting the impact of a comprehensive HIV strategy in Washington DC. Clin Infect Dis 51 : 392–400.
20. EatonJW, JohnsonLF, SalomonJA, BärnighausenT, BendavidE, et al. (2012) HIV treatment as prevention: systematic comparison of mathematical models of the potential impact of antiretroviral therapy on HIV incidence in South Africa. PLoS Med 9: e1001245 doi:10.1371/journal.pmed.1001245
21. AnglemyerA, RutherfordGW, BaggaleyRC, EggerM, SiegfriedN (2011) Antiretroviral therapy for prevention of HIV transmission in HIV-discordant couples. Cochrane Database Syst Rev 2011: CD009153.
22. AttiaS, EggerM, MullerM, ZwahlenM, LowN (2009) Sexual transmission of HIV according to viral load and antiretroviral therapy: systematic review and meta-analysis. AIDS 23 : 1397–1404.
23. DonnellD, BaetenJM, KiarieJ, ThomasKK, StevensW, et al. (2010) Heterosexual HIV-1 transmission after initiation of antiretroviral therapy: a prospective cohort analysis. Lancet 375 : 2092–2098.
24. World Health Organization (2009) Rapid advice: antiretroviral therapy for HIV infected in adults and adolescents. Geneva: World Health Organization.
25. HontelezJA, de VlasSJ, TanserF, BakkerR, BärnighausenT, et al. (2011) The impact of the new WHO antiretroviral treatment guidelines on HIV epidemic dynamics and cost in South Africa. PLoS ONE 6: e21919 doi:10.1371/journal.pone.0021919
26. MontanerJS, LimaVD, BarriosR, YipB, WoodE, et al. (2010) Association of highly active antiretroviral therapy coverage, population viral load, and yearly new HIV diagnoses in British Columbia, Canada: a population-based study. Lancet 376 : 532–539.
27. van der PloegCPB, Van VlietC, De VlasSJ, Ndinya-AcholaJO, FransenL, et al. (1998) STDSIM: a microsimulation model for decision support in STD control. Interfaces 28 : 84–100.
28. KorenrompEL, BakkerR, De VlasSJ, RobinsonNJ, HayesR, et al. (2002) Can behavior change explain increases in the proportion of genital ulcers attributable to herpes in sub-Saharan Africa? A simulation modeling study. Sex Transm Dis 29 : 228–238.
29. KorenrompEL, BakkerR, GrayR, WawerMJ, SerwaddaD, et al. (2002) The effect of HIV, behavioural change, and STD syndromic management on STD epidemiology in sub-Saharan Africa: simulations of Uganda. Sex Transm Infect 78 (Suppl 1) i55–i63.
30. KorenrompEL, Van VlietC, BakkerR, De VlasSJ, HabbemaJD (2000) HIV spread and partnership reduction for different patterns of sexual behavior—a study with the microsimulation model STDSIM. Math Pop Studies 8 : 135–173.
31. van VlietC, MeesterEI, KorenrompEL, SingerB, BakkerR, et al. (2001) Focusing strategies of condom use against HIV in different behavioural settings: an evaluation based on a simulation model. Bull World Health Organ 79 : 442–454.
32. KorenrompEL, Van VlietC, GrosskurthH, GavyoleA, Van der PloegCP, et al. (2000) Model-based evaluation of single-round mass treatment of sexually transmitted diseases for HIV control in a rural African population. AIDS 14 : 573–593.
33. WhiteRG, FreemanEE, OrrothKK, BakkerR, WeissHA, et al. (2008) Population-level effect of HSV-2 therapy on the incidence of HIV in sub-Saharan Africa. Sex Transm Infect 84 (Suppl 2) ii12–ii18.
34. WhiteRG, GlynnJR, OrrothKK, FreemanEE, BakkerR, et al. (2008) Male circumcision for HIV prevention in sub-Saharan Africa: who, what and when? AIDS 22 : 1841–1850.
35. OrrothKK, FreemanEE, BakkerR, BuveA, GlynnJR, et al. (2007) Understanding the differences between contrasting HIV epidemics in east and west Africa: results from a simulation model of the Four Cities Study. Sex Transm Infect 83 (Suppl 1) i5–i16.
36. HontelezJA, LurieMN, NewellML, BakkerR, TanserF, et al. (2011) Ageing with HIV in South Africa. AIDS 25 : 1665–1667.
37. HontelezJA, NagelkerkeN, BärnighausenT, BakkerR, TanserF, et al. (2011) The potential impact of RV144-like vaccines in rural South Africa: a study using the STDSIM microsimulation model. Vaccine 29 : 6100–6106.
38. HontelezJAC, De VlasSJ, BaltussenR, NewellM, BakkerR, et al. (2012) The impact of antiretroviral treatment on the age composition of the HIV epidemic in sub-Saharan Africa. AIDS 26 (Suppl 1) S19–S30.
39. United Nations Population Division Fertility and Family Planning Section (2008) World fertility data 2008 [database]. New York: United Nations Population Division Fertility and Family Planning Section.
40. World Health Organization (2011) Life tables for WHO member States. Geneva: World Health Organization.
41. World Health Organization (2008) The global burden of disease: 2004 update. Geneva: World Health Organization.
42. JaffarS, GrantAD, WhitworthJ, SmithPG, WhittleH (2004) The natural history of HIV-1 and HIV-2 infections in adults in Africa: a literature review. Bull World Health Organ 82 : 462–469.
43. MorganD, MaheC, MayanjaB, OkongoJM, LubegaR, et al. (2002) HIV-1 infection in rural Africa: is there a difference in median time to AIDS and survival compared with that in industrialized countries? AIDS 16 : 597–603.
44. BoilyMC, BaggaleyRF, WangL, MasseB, WhiteRG, et al. (2009) Heterosexual risk of HIV-1 infection per sexual act: systematic review and meta-analysis of observational studies. Lancet Infect Dis 9 : 118–129.
45. HollingsworthTD, AndersonRM, FraserC (2008) HIV-1 transmission, by stage of infection. J Infect Dis 198 : 687–693.
46. South Africa Department of Health (2003) Demographic and Health Survey of South Africa. Pretoria: South Africa Department of Health.
47. WilliamsBG, Lloyd-SmithJO, GouwsE, HankinsC, GetzWM, et al. (2006) The potential impact of male circumcision on HIV in sub-Saharan Africa. PLoS Med 3: e262 doi:10.1371/journal.pmed.0030262
48. AuvertB, TaljaardD, LagardeE, Sobngwi-TambekouJ, SittaR, et al. (2005) Randomized, controlled intervention trial of male circumcision for reduction of HIV infection risk: the ANRS 1265 Trial. PLoS Med 2: e298 doi:10.1371/journal.pmed.0020298
49. BaileyRC, MosesS, ParkerCB, AgotK, MacleanI, et al. (2007) Male circumcision for HIV prevention in young men in Kisumu, Kenya: a randomised controlled trial. Lancet 369 : 643–656.
50. GrayRH, KigoziG, SerwaddaD, MakumbiF, WatyaS, et al. (2007) Male circumcision for HIV prevention in men in Rakai, Uganda: a randomised trial. Lancet 369 : 657–666.
51. MutevedziPC, LessellsRJ, RodgerAJ, NewellML (2011) Association of age with mortality and virological and immunological response to antiretroviral therapy in rural South African adults. PLoS ONE 6: e21795 doi:10.1371/journal.pone.0021795
52. WilliamsBG, KorenrompEL, GouwsE, SchmidGP, AuvertB, et al. (2006) HIV infection, antiretroviral therapy, and CD4+ cell count distributions in African populations. J Infect Dis 194 : 1450–1458.
53. World Health Organization (2010) Towards universal access: scaling up priority HIV/AIDS interventions in the health sector: progress report 2010. Geneva: World Health Organization.
54. HargreavesJR, BonellCP, MorisonLA, KimJC, PhetlaG, et al. (2007) Explaining continued high HIV prevalence in South Africa: socioeconomic factors, HIV incidence and sexual behaviour change among a rural cohort, 2001–2004. AIDS 21 (Suppl 7) S39–S48.
55. BadriM, MaartensG, MandaliaS, BekkerLG, PenrodJR, et al. (2006) Cost-effectiveness of highly active antiretroviral therapy in South Africa. PLoS Med 3: e4 doi:10.1371/journal.pmed.0030004
56. HarlingG, WoodR (2007) The evolving cost of HIV in South Africa: changes in health care cost with duration on antiretroviral therapy for public sector patients. J Acquir Immune Defic Syndr 45 : 348–354.
57. World Health Organization (2003) Making choices in health: WHO guide to cost-effectiveness analysis. Geneva: World Health Organization.
58. CohenMS, ShawGM, McMichaelAJ, HaynesBF (2011) Acute HIV-1 infection. N Engl J Med 364 : 1943–1954.
59. TanserF, HosegoodV, BärnighausenT, HerbstK, NyirendaM, et al. (2008) Cohort profile: Africa Centre Demographic Information System (ACDIS) and population-based HIV survey. Int J Epidemiol 37 : 956–962.
60. HerbstAJ, CookeGS, BärnighausenT, KanyKanyA, TanserF, et al. (2009) Adult mortality and antiretroviral treatment roll-out in rural KwaZulu-Natal, South Africa. Bull World Health Organ 87 : 754–762.
61. HontelezJA, NewellML, BlandRM, MunnellyK, LessellsRJ, et al. (2012) Human resources needs for universal access to antiretroviral therapy in South Africa: a time and motion study. Hum Resour Health 10 : 39.
62. BärnighausenT (2010) The role of the health system in HIV treatment-as-prevention. AIDS 24 : 2741–2742.
63. BärnighausenT, TanserF, DabisF, NewellML (2012) Interventions to improve the performance of HIV health systems for treatment-as-prevention in sub-Saharan Africa: the experimental evidence. Curr Opin HIV AIDS 7 : 140–150.
64. KranzerK, LewisJJ, FordN, ZeineckerJ, OrrellC, et al. (2010) Treatment interruption in a primary care antiretroviral therapy program in South Africa: cohort analysis of trends and risk factors. J Acquir Immune Defic Syndr 55: e17–e23.
65. CornellM, GrimsrudA, FairallL, FoxMP, van CutsemG, et al. (2010) Temporal changes in programme outcomes among adult patients initiating antiretroviral therapy across South Africa, 2002–2007. AIDS 24 : 2263–2270.
66. Garcia-CallejaJM, GouwsE, GhysPD (2006) National population based HIV prevalence surveys in sub-Saharan Africa: results and implications for HIV and AIDS estimates. Sex Transm Infect 82 (Suppl 3) iii64–iii70.
67. NyirendaM, ZabaB, BärnighausenT, HosegoodV, NewellML (2010) Adjusting HIV prevalence for survey non-response using mortality rates: an application of the method using surveillance data from rural South Africa. PLoS ONE 5: e12370 doi:10.1371/journal.pone.0012370
68. GranichR, KahnJG, BennettR, HolmesCB, GargN, et al. (2012) Expanding ART for treatment and prevention of HIV in South Africa: estimated cost and cost-effectiveness 2011–2050. PLoS ONE 7: e30216 doi:10.1371/journal.pone.0030216
69. NagelkerkeNJ, JhaP, de VlasSJ, KorenrompEL, MosesS, et al. (2002) Modelling HIV/AIDS epidemics in Botswana and India: impact of interventions to prevent transmission. Bull World Health Organ 80 : 89–96.
70. HamersRL, WallisCL, KityoC, SiwaleM, MandaliyaK, et al. (2011) HIV-1 drug resistance in antiretroviral-naive individuals in sub-Saharan Africa after rollout of antiretroviral therapy: a multicentre observational study. Lancet Infect Dis 11 : 750–759.
71. ManasaJ, KatzensteinD, CassolS, NewellML, de OliveiraT (2012) Primary drug resistance in South Africa—data from 10 years of surveys. AIDS Res Hum Retroviruses 28 : 558–565.
72. NachegaJB, MillsEJ, SchechterM (2010) Antiretroviral therapy adherence and retention in care in middle-income and low-income countries: current status of knowledge and research priorities. Curr Opin HIV AIDS 5 : 70–77.
73. MillsEJ, BakandaC, BirungiJ, MwesigwaR, ChanK, et al. (2011) Mortality by baseline CD4 cell count among HIV patients initiating antiretroviral therapy: evidence from a large cohort in Uganda. AIDS 25 : 851–855.
74. BorJ, HerbstAJ, NewellML, BärnighausenT (2013) Increases in adult life expectancy in rural South Africa: valuing the scale-up of HIV treatment. Science 339 : 961–965.
75. BorJ, TanserF, NewellML, BärnighausenT (2012) In a study of a population cohort in South Africa, HIV patients on antiretrovirals had nearly full recovery of employment. Health Aff (Millwood) 31 : 1459–1469.
76. Abdool KarimSS, ChurchyardGJ, KarimQA, LawnSD (2009) HIV infection and tuberculosis in South Africa: an urgent need to escalate the public health response. Lancet 374 : 921–933.
77. United Nations Population Division (2010) World population prospects: the 2010 revision. New York: United Nations Population Division.
78. Shisana O, Rehle T, Simbayi L, Parker W, Zuma K, et al.. (2005) South African national HIV prevalence, behavioural risks and communication survey, 2005. Cape Town: HSRC Press.
79. JohnsonLF, AlkemaL, DorringtonRE (2010) A Bayesian approach to uncertainty analysis of sexually transmitted infection models. Sex Transm Infect 86 : 169–174.
80. HoulihanCF, BlandR, MutevedziP, LessellsRJ, NdiranguJ, et al. (2011) Cohort profile: Hlabisa HIV treatment and care programme. Int J Epidemiol 40 : 318–326.
81. WilliamsBG, GranichR, DyeC (2011) Role of acute infection in HIV transmission. Lancet 378 : 1913.
82. BärnighausenT, TanserF, NewellML (2009) Lack of a decline in HIV incidence in a rural community with high HIV prevalence in South Africa, 2003–2007. AIDS Res Hum Retroviruses 25 : 405–409.
83. KumaranayakeL (2008) The economics of scaling up: cost estimation for HIV/AIDS interventions. AIDS 22 (Suppl 1) S23–S33.
84. JohnsonLF, DorringtonRE, BradshawD, Pallay-Van WykV, RehleT (2009) Sexual behaviour patterns in South Africa and their association with the spread of HIV: insights from a mathematical model. Demogr Res 21 : 289–340.
85. CaraelM, ClelandJ, AdeokunL (1991) Overview and selected findings of sexual behaviour surveys. AIDS 5 (Suppl 1) S65–S74.
86. NnkoS, BoermaJT, UrassaM, MwalukoG, ZabaB (2004) Secretive females or swaggering males? An assessment of the quality of sexual partnership reporting in rural Tanzania. Soc Sci Med 59 : 299–310.
87. WeinhardtLS, ForsythAD, CareyMP, JaworskiBC, DurantLE (1998) Reliability and validity of self-report measures of HIV-related sexual behavior: progress since 1990 and recommendations for research and practice. Arch Sex Behav 27 : 155–180.
Štítky
Interní lékařství
Článek vyšel v časopisePLOS Medicine
Nejčtenější tento týden
2013 Číslo 10- Berberin: přírodní hypolipidemikum se slibnými výsledky
- Léčba bolesti u seniorů
- Příznivý vliv Armolipidu Plus na hladinu cholesterolu a zánětlivé parametry u pacientů s chronickým subklinickým zánětem
- Jak postupovat při výběru betablokátoru − doporučení z kardiologické praxe
- Červená fermentovaná rýže účinně snižuje hladinu LDL cholesterolu jako vhodná alternativa ke statinové terapii
-
Všechny články tohoto čísla
- Modelling the Strategic Use of Antiretroviral Therapy for the Treatment and Prevention of HIV
- Psychosocial Interventions for Perinatal Common Mental Disorders Delivered by Providers Who Are Not Mental Health Specialists in Low- and Middle-Income Countries: A Systematic Review and Meta-Analysis
- Predicting Patterns of Long-Term CD4 Reconstitution in HIV-Infected Children Starting Antiretroviral Therapy in Sub-Saharan Africa: A Cohort-Based Modelling Study
- Use of Expert Panels to Define the Reference Standard in Diagnostic Research: A Systematic Review of Published Methods and Reporting
- Elimination of HIV in South Africa through Expanded Access to Antiretroviral Therapy: A Model Comparison Study
- A Transcriptional Signature for Active TB: Have We Found the Needle in the Haystack?
- Poor Health in Rich Countries: A Role for Open Access Journals
- The 2003 Iraq War and Avoidable Death Toll
- Completeness of Reporting of Patient-Relevant Clinical Trial Outcomes: Comparison of Unpublished Clinical Study Reports with Publicly Available Data
- The Final Push for Polio Eradication: Addressing the Challenge of Violence in Afghanistan, Pakistan, and Nigeria
- Saving Lives in Health: Global Estimates and Country Measurement
- Complexity in Mathematical Models of Public Health Policies: A Guide for Consumers of Models
- Mortality in Iraq Associated with the 2003–2011 War and Occupation: Findings from a National Cluster Sample Survey by the University Collaborative Iraq Mortality Study
- Why We Must Provide Better Support for Pakistan's Female Frontline Health Workers
- Effect on Postpartum Hemorrhage of Prophylactic Oxytocin (10 IU) by Injection by Community Health Officers in Ghana: A Community-Based, Cluster-Randomized Trial
- The Prevention of Postpartum Hemorrhage in the Community
- Pregnancy Weight Gain and Childhood Body Weight: A Within-Family Comparison
- Detection of Tuberculosis in HIV-Infected and -Uninfected African Adults Using Whole Blood RNA Expression Signatures: A Case-Control Study
- A New Approach to Psychiatric Drug Approval in Europe
- Utility of the Xpert MTB/RIF Assay for Diagnosis of Tuberculous Meningitis
- Methodological and Policy Limitations of Quantifying the Saving of Lives: A Case Study of the Global Fund's Approach
- Diagnostic Accuracy of Quantitative PCR (Xpert MTB/RIF) for Tuberculous Meningitis in a High Burden Setting: A Prospective Study
- Assessing Optimal Target Populations for Influenza Vaccination Programmes: An Evidence Synthesis and Modelling Study
- PLOS Medicine
- Archiv čísel
- Aktuální číslo
- Informace o časopisu
Nejčtenější v tomto čísle- Effect on Postpartum Hemorrhage of Prophylactic Oxytocin (10 IU) by Injection by Community Health Officers in Ghana: A Community-Based, Cluster-Randomized Trial
- Utility of the Xpert MTB/RIF Assay for Diagnosis of Tuberculous Meningitis
- Modelling the Strategic Use of Antiretroviral Therapy for the Treatment and Prevention of HIV
- Diagnostic Accuracy of Quantitative PCR (Xpert MTB/RIF) for Tuberculous Meningitis in a High Burden Setting: A Prospective Study
Kurzy
Zvyšte si kvalifikaci online z pohodlí domova
Současné možnosti léčby obezity
nový kurzAutoři: MUDr. Martin Hrubý
Všechny kurzyPřihlášení#ADS_BOTTOM_SCRIPTS#Zapomenuté hesloZadejte e-mailovou adresu, se kterou jste vytvářel(a) účet, budou Vám na ni zaslány informace k nastavení nového hesla.
- Vzdělávání



