-
Články
Top novinky
Reklama- Vzdělávání
- Časopisy
Top články
Nové číslo
- Témata
Top novinky
Reklama- Videa
- Podcasty
Nové podcasty
Reklama- Kariéra
Doporučené pozice
Reklama- Praxe
Top novinky
ReklamaAnalysing Recent Socioeconomic Trends in Coronary Heart Disease Mortality in England, 2000–2007: A Population Modelling Study
Background:
Coronary heart disease (CHD) mortality in England fell by approximately 6% every year between 2000 and 2007. However, rates fell differentially between social groups with inequalities actually widening. We sought to describe the extent to which this reduction in CHD mortality was attributable to changes in either levels of risk factors or treatment uptake, both across and within socioeconomic groups.Methods and Findings:
A widely used and replicated epidemiological model was used to synthesise estimates stratified by age, gender, and area deprivation quintiles for the English population aged 25 and older between 2000 and 2007. Mortality rates fell, with approximately 38,000 fewer CHD deaths in 2007. The model explained about 86% (95% uncertainty interval: 65%–107%) of this mortality fall. Decreases in major cardiovascular risk factors contributed approximately 34% (21%–47%) to the overall decline in CHD mortality: ranging from about 44% (31%–61%) in the most deprived to 29% (16%–42%) in the most affluent quintile. The biggest contribution came from a substantial fall in systolic blood pressure in the population not on hypertension medication (29%; 18%–40%); more so in deprived (37%) than in affluent (25%) areas. Other risk factor contributions were relatively modest across all social groups: total cholesterol (6%), smoking (3%), and physical activity (2%). Furthermore, these benefits were partly negated by mortality increases attributable to rises in body mass index and diabetes (−9%; −17% to −3%), particularly in more deprived quintiles. Treatments accounted for approximately 52% (40%–70%) of the mortality decline, equitably distributed across all social groups. Lipid reduction (14%), chronic angina treatment (13%), and secondary prevention (11%) made the largest medical contributions.Conclusions:
The model suggests that approximately half the recent CHD mortality fall in England was attributable to improved treatment uptake. This benefit occurred evenly across all social groups. However, opposing trends in major risk factors meant that their net contribution amounted to just over a third of the CHD deaths averted; these also varied substantially by socioeconomic group. Powerful and equitable evidence-based population-wide policy interventions exist; these should now be urgently implemented to effectively tackle persistent inequalities.
: Please see later in the article for the Editors' Summary
Published in the journal: . PLoS Med 9(6): e32767. doi:10.1371/journal.pmed.1001237
Category: Research Article
doi: https://doi.org/10.1371/journal.pmed.1001237Summary
Background:
Coronary heart disease (CHD) mortality in England fell by approximately 6% every year between 2000 and 2007. However, rates fell differentially between social groups with inequalities actually widening. We sought to describe the extent to which this reduction in CHD mortality was attributable to changes in either levels of risk factors or treatment uptake, both across and within socioeconomic groups.Methods and Findings:
A widely used and replicated epidemiological model was used to synthesise estimates stratified by age, gender, and area deprivation quintiles for the English population aged 25 and older between 2000 and 2007. Mortality rates fell, with approximately 38,000 fewer CHD deaths in 2007. The model explained about 86% (95% uncertainty interval: 65%–107%) of this mortality fall. Decreases in major cardiovascular risk factors contributed approximately 34% (21%–47%) to the overall decline in CHD mortality: ranging from about 44% (31%–61%) in the most deprived to 29% (16%–42%) in the most affluent quintile. The biggest contribution came from a substantial fall in systolic blood pressure in the population not on hypertension medication (29%; 18%–40%); more so in deprived (37%) than in affluent (25%) areas. Other risk factor contributions were relatively modest across all social groups: total cholesterol (6%), smoking (3%), and physical activity (2%). Furthermore, these benefits were partly negated by mortality increases attributable to rises in body mass index and diabetes (−9%; −17% to −3%), particularly in more deprived quintiles. Treatments accounted for approximately 52% (40%–70%) of the mortality decline, equitably distributed across all social groups. Lipid reduction (14%), chronic angina treatment (13%), and secondary prevention (11%) made the largest medical contributions.Conclusions:
The model suggests that approximately half the recent CHD mortality fall in England was attributable to improved treatment uptake. This benefit occurred evenly across all social groups. However, opposing trends in major risk factors meant that their net contribution amounted to just over a third of the CHD deaths averted; these also varied substantially by socioeconomic group. Powerful and equitable evidence-based population-wide policy interventions exist; these should now be urgently implemented to effectively tackle persistent inequalities.
: Please see later in the article for the Editors' SummaryIntroduction
Since the 1970s, coronary heart disease (CHD) mortality in England has fallen by a remarkable 60%, with accelerated reductions in annual death rates since 2000 [1]. However, CHD remains the leading cause of mortality and is a major contributor to social inequalities in premature mortality in England, as in the USA [2],[3]. Moreover, UK death rates have fallen faster in the most socially advantaged groups compared to the most deprived [1]. Thus, whilst absolute inequalities in mortality have fallen, relative inequalities have increased over the last decade. Previous country-level analyses have shown that about 50%–70% of the dramatic falls in CHD mortality between 1980 and 2000 were explained by improvements in modifiable risk factors (mainly smoking, total cholesterol and blood pressure), with the remaining 30%–50% attributable to improved uptake of evidence-based treatments [4]–[6]. However, so far no study has examined the specific contribution of risk factors and medical treatments to the underlying social differentials in CHD mortality falls.
The most recent study in the UK modelled CHD mortality change in England and Wales between 1981 and 2000 [4]. Since then several initiatives have been rolled out to improve the delivery of health care in England. Notable among them include the National Service Framework for CHD (2000) and the Qualities and Outcome Framework (2004), which aim to monitor and incentivise improvements in the quality of services provided for CHD prevention, diagnosis, treatment, and rehabilitation [7],[8]. In addition, important population-wide public health measures to reduce risk factors across the entire population were introduced. These measures included the ban on tobacco advertising (2003); comprehensive smoke-free legislation (2007), and voluntary agreements to reduce salt and artificial trans-fats in processed food [9],[10]. Reducing health inequalities was at the heart of New Labour's health agenda when it came to office in 1997. However, the target to reduce the inequality gap in life expectancy by 2010 was not met [11]. Furthermore, the potential effect of population-wide interventions on reducing inequalities in CHD mortality (when compared with individual treatments) remains unclear [12].
Thus although our analysis covers a relatively short period of time, the period included a raft of measures specifically aimed to improve outcomes and reduce social inequalities. We have quantified the variation by socioeconomic circumstances (SEC) in the relative contributions of modifiable population-level risk factors and evidence-based individual treatments to the fall in CHD mortality during the period 2000 to 2007. To do this we have used the widely used and replicated IMPACT model, substantially extending the model to capture socioeconomic inequalities concealed within the overall national trends.
Methods
IMPACTSEC Model and Data Sources
IMPACT is an epidemiological model used to explain the contributions of population-level risk factor changes (incidence reduction) and uptake of evidence-based treatments (case fatality reduction) to the change in CHD deaths between two points in time. This deterministic, cell-based model has been described in detail elsewhere [4],[5]. The extended IMPACTSEC model included all the major risk factors for CHD: smoking, systolic blood pressure, total cholesterol, body mass index (BMI), diabetes, physical inactivity, along with fruit and vegetable consumption; plus all 45 medical and surgical treatments currently in use in nine patient groups. The model included the total population of England aged 25 y and over in 2000 and 2007.
Data sources specific to the England population were used to construct the IMPACTSEC model. When several sources were available, we chose the most up-to-date, representative dataset that we could link to a small-area deprivation index. Population estimates and CHD death counts (2000: ICD9 410–414; 2007: ICD10 I20–I25) by sex, 5-y age bands to age 85+, and deprivation quintile were obtained from the Office for National Statistics. Emergency admissions for acute myocardial infarction were extracted from Hospital Episode Statistics and supplemented with data from the Myocardial Ischaemia National Audit Project to disaggregate ST-elevated acute myocardial infarction and non–ST-elevated acute coronary syndrome, and to apportion treatment uptake to each group. For heart failure admissions, the National Health Service (NHS) Heart Failure Survey was used to estimate in-hospital treatment uptake. The General Practice Research Database and the Health Survey for England provided data on treatment uptake in the community. Risk factor trend data came from the Health Survey for England.
Detailed information on the IMPACTSEC model, calculation methods, and data sources are provided as supporting information in Text S1.
Stratifying Data according to Socioeconomic Circumstances
Only the Health Survey for England consistently recorded individual socioeconomic position; but all data sources recorded individual's postcode of residence. We therefore used a measure of relative area deprivation as a proxy indicator of the SECs of individuals living in small areas (n = 32,482; average population of 1,500). We used the Index of Multiple Deprivation 2007 [13] to rank all lower super output areas in England in ascending order of increasing deprivation and grouped them into equal quintiles. Although scoring low on the deprivation index does not necessarily equate to affluence, to assist readability we refer to quintile one as “most affluent” and quintile five as “most deprived.” On the basis of postcode of residence, the data providers matched CHD deaths and treated patients to their corresponding deprivation quintile before releasing the data to us.
Deaths Prevented or Postponed
The total number of deaths prevented or postponed (DPPs) for each deprivation quintile were calculated as the difference between observed deaths in 2007 and expected deaths had age-, sex-, and quintile - specific CHD mortality rates in 2000 remained unchanged. DPPs explained by the model could be positive (i.e., deaths averted) or negative (i.e., additional deaths in 2007 relative to 2000). Any shortfalls between the DPPs explained by the model and the total DPPs for each SEC quintile were assumed to reflect either imprecision in our model parameters or omission of other, unmeasured risk factors.
Mortality Reductions Attributable to Treatment Uptake
The treatment component of IMPACTSEC included nine mutually exclusive CHD patient groups: ST-elevation myocardial infarction; non–ST-elevation acute coronary syndrome; secondary prevention post myocardial infarction; secondary prevention post revascularisation; chronic stable coronary artery disease; heart failure patients admitted to hospital; heart failure patients resident in the community; persons in the community taking blood pressure lowering medication; and persons in the community taking lipid lowering treatment. A total of 45 patient-treatment pairings were generated. To avoid double counting of patients treated for two or more conditions within the year (e.g., heart failure develops within 1 y after myocardial infarction in approximately 30% of survivors), we quantified overlaps between different groups and made appropriate adjustments to construct distinct, non-overlapping CHD patient subgroups (Text S1, Table N).
The numbers eligible for treatment, uptake of specific treatment, 1-y case fatality rates, and relative risk reduction due to treatment, all stratified by age, sex, and CHD patient subgroups, were extracted from relevant data sources (Text S1, Tables A, B, F, G, I, J). Disease prevalence and treatment uptake were further stratified by deprivation quintiles.
The estimates of medication uptake in the community recorded in our primary data sources were adjusted to reflect ordinary clinical practice. We assumed that medication adherence (i.e., the proportion of eligible patients actually taking therapeutically effective levels of medication) was 100% among hospitalised patients, 70% among symptomatic patients in the community, and 50% among asymptomatic patients in the community [5]. The scale of the downward adjustment of uptake was assumed to reasonably represent the combined effects of lower rates of adherence in community settings and reduced population effectiveness in routine health care settings compared to optimal clinical trial conditions. Uncertainty in both of these input variables—the actual uptake rates and the adjustment factor—were included in the stochastic sensitivity analysis reported below.
Deaths prevented by each intervention were then calculated by multiplying the numbers of patients in each diagnostic group by the (adherence-adjusted) proportion of those patients who received the treatment, the baseline case fatality rate, and the relative risk reduction of that treatment. To estimate the cumulative effect of relative risk reduction for patients on a combination of drug therapies, we used the Mant and Hicks correction [14].
Many of the treatments were already widely used in 2000. The net benefit of an intervention in 2007 was therefore calculated by subtracting the expected number of deaths prevented if 2000 uptake rates had remained unchanged from the deaths prevented using 2007 treatment uptake rates.
Mortality Reductions Attributable to Risk Factor Changes
We included seven risk factors in the model; both behavioural—smoking, physical inactivity, fruit and vegetable consumption, BMI—and physiological markers including systolic blood pressure, total serum cholesterol, and diagnosed diabetes. To quantify the mortality benefits of an absolute change in each specific risk factor between 2000 and 2007, we used two approaches: a regression-based approach for factors measured on a continuous scale (e.g., total blood cholesterol); and, a population-attributable risk fraction approach for dichotomous variables such as diagnosed diabetes. The independent regression coefficients of mortality benefit for a unit change in mean risk factor were obtained from published multivariate analyses (Text S1, Table I). Hence, the contribution of each risk factor to deaths averted was then calculated as the product of the deaths in 2000 (the base year), the absolute change in risk factor, and the associated relative risk reduction. For binary variables, we used relative risks from the most recent meta-analyses and population cohort studies (Text S1, Table J).
CHD deaths are usually caused by multiple risk factors acting simultaneously. It is therefore recommended that enumerating mortality benefits from risk factor reductions should not use a simple additive approach. Instead, the effects of risk factor changes should be jointly estimated using the cumulative risk-reduction approach. This can be stated in the equation:The cumulative effect of change in all risk factors over the study period was calculated by age, sex, and deprivation quintile (see Text S1, Section 1.3). The ratio of the cumulative effect to the corresponding additive effect was then calculated, yielding 70 adjustment factors (Text S1, Table D). These adjustment factors were used to scale down the additive DPPs for each risk factor. These adjusted DPPs, summed over all seven risk factors, then equalled the estimated total combined DPPs, capturing the multiplicative net impact of positive and adverse changes in risk factors. All risk factor DPPs quoted in the results tables refer to the adjusted DPPs.
We assumed that there was no further synergy between the treatment and risk-factor components of the model. Lag times between the change in cardiovascular risk factor levels and change in CHD mortality rates were assumed to be relatively rapid [15] and were therefore not specifically modelled. Similar to economic evaluation studies in health [16], 95% uncertainty intervals around the model output (i.e., DPPs) were calculated using Monte Carlo simulation. This calculation involved replacing all fixed input parameters used in the model by appropriate probability distributions, and repeatedly recalculating the model output with values sampled from the defined input distributions (Text S1, Table M). We used the EXCEL add-in Ersatz software (www.epigear.com) to perform 1,000 runs to determine the 95% uncertainty intervals of the DPPs (2.5th and 97.5th percentile values corresponding to the lower and upper limits).
Results
Between 2000 and 2007, the age-standardised CHD mortality rate in adults aged 25 y and over fell from 229 to 147 deaths per 100,000; a decline of 36% overall or 6.1% per year (Table 1). In 2007, there were 74,174 CHD deaths, 56% of these were in men. Both death rates and the number of deaths were lowest in the most affluent quintile and the pace of fall was also faster: decreasing by 6.7% per year compared to just 4.9% in the most deprived quintile. Differentials in the rates of fall therefore widened relative inequalities over the period.
Tab. 1. Observed coronary heart disease deaths, age-standardised rates 2000 and 2007 and deaths prevented or postponed in England and stratified by deprivation quintiles. 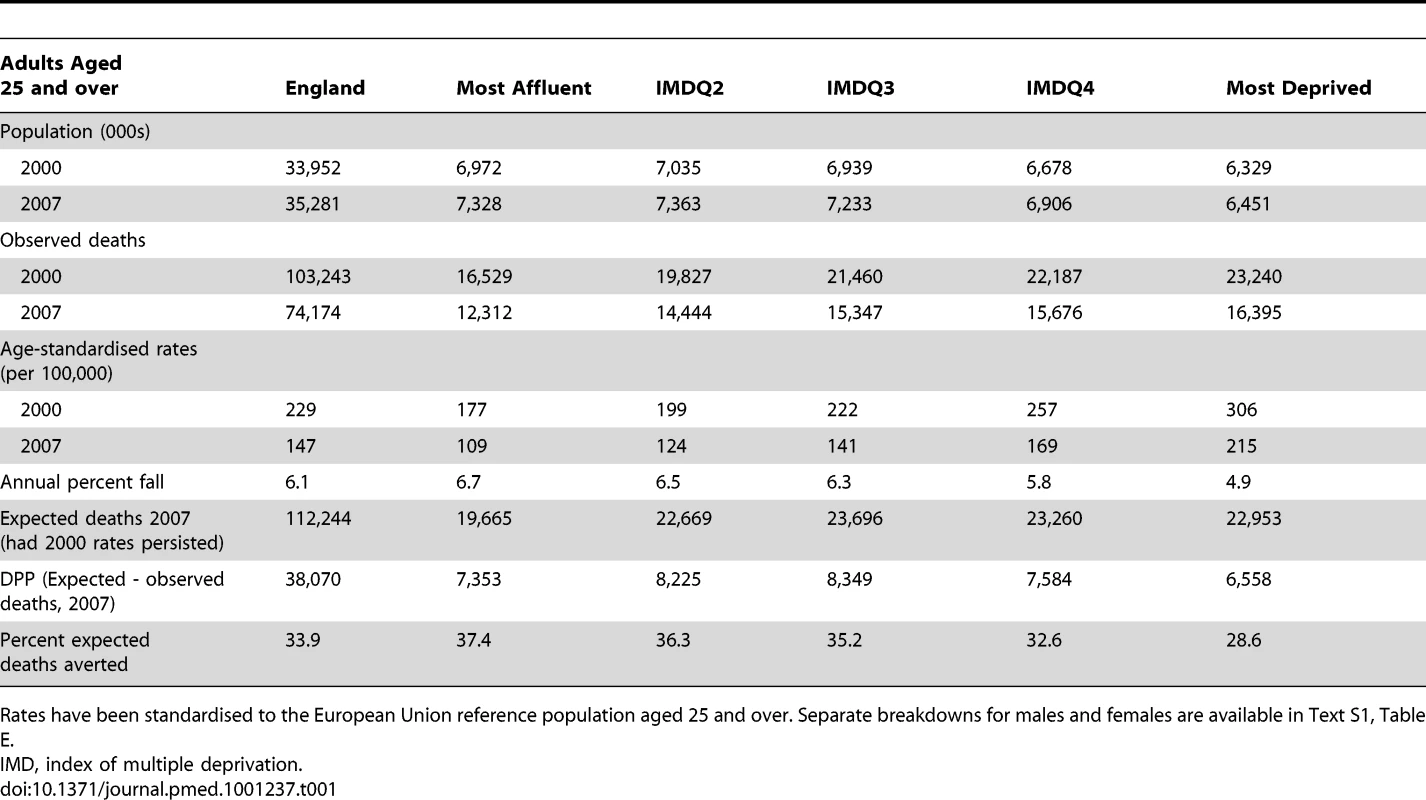
Rates have been standardised to the European Union reference population aged 25 and over. Separate breakdowns for males and females are available in Text S1, Table E. Nationally, there were 38,070 fewer CHD deaths in 2007 than if 2000 mortality rates had persisted, representing the “total” DPPs. Despite the slower annual rates of fall in the most deprived quintile, their higher CHD mortality rates in the base year meant that the number of DPPs by 2007 were fairly equally distributed: about 6,560 fewer deaths in the most deprived quintile versus 7,355 in the most affluent (Table 1).
Overall, approximately half of the total CHD mortality fall (19,780 fewer deaths or 52%; 95% uncertainly interval ranging from 40% to 70%) was attributable to improvements in uptake of medical and surgical treatments (Table 2). In contrast, population-level risk factor changes accounted for approximately 12,990 (34%; 21%–47%) fewer deaths (Table 3). The model could not explain some 14% of the overall mortality fall (i.e., a shortfall of 5,300 deaths) (Figure 1; Table 3). The contribution of medical treatments to the deaths averted was very similar across all quintiles, ranging from 50% in the most affluent quintile to 53% in the most deprived (Table 4). But risk factor changes explained a smaller proportion of deaths prevented in the most affluent quintile compared with the most deprived (approximately 29% versus 44%, respectively). As a result, about 21% of CHD deaths prevented could not be explained by the model in the most affluent quintile. The proportion not explained fell successively with increasing deprivation to 3% of CHD deaths (190 deaths) not explained in the most deprived quintile.
Fig. 1. Proportion of coronary heart disease mortality decline attributable to treatment or risk factor changes, 2000–2007. 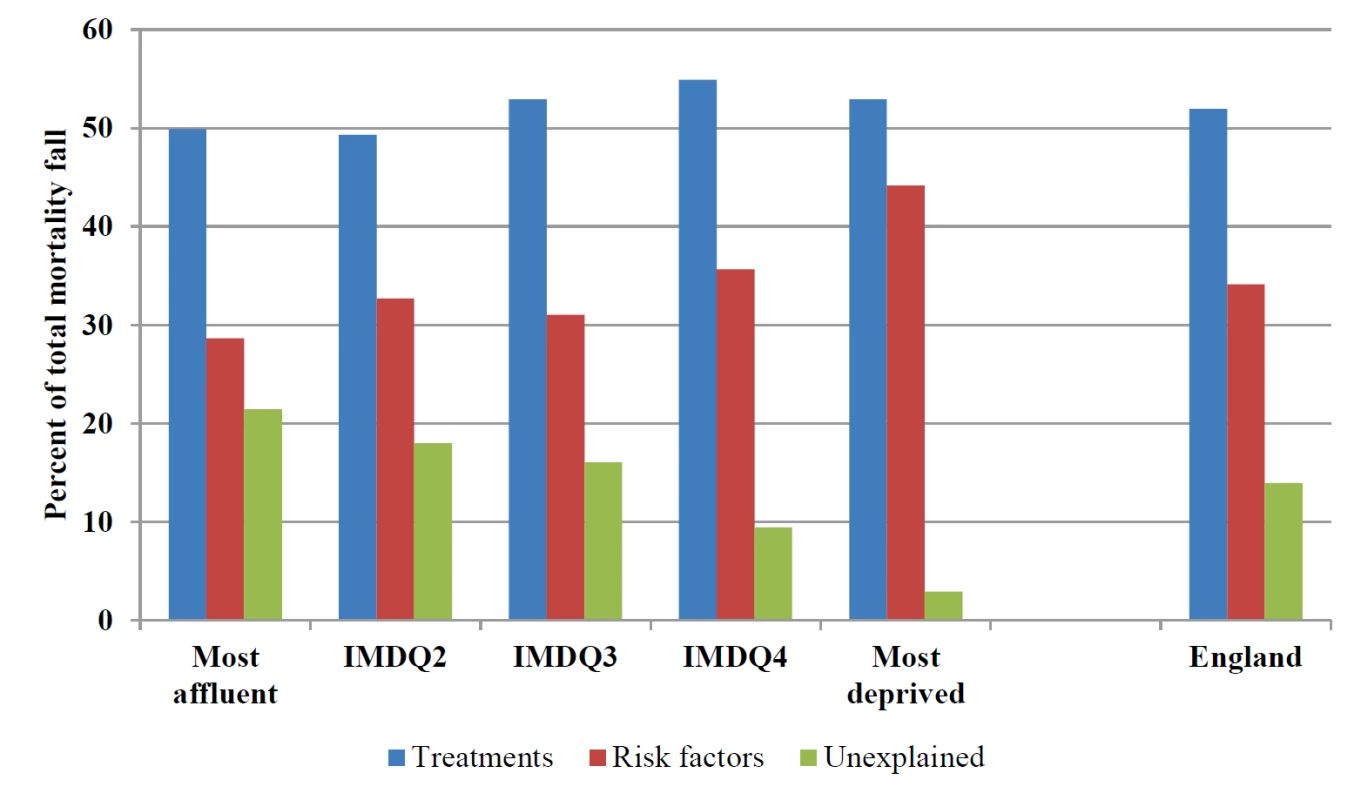
England overall and by socioeconomic quintile. Tab. 2. Coronary heart disease deaths prevented or postponed due to changes in treatment uptake between 2000 and 2007 in England and stratified by deprivation quintiles. 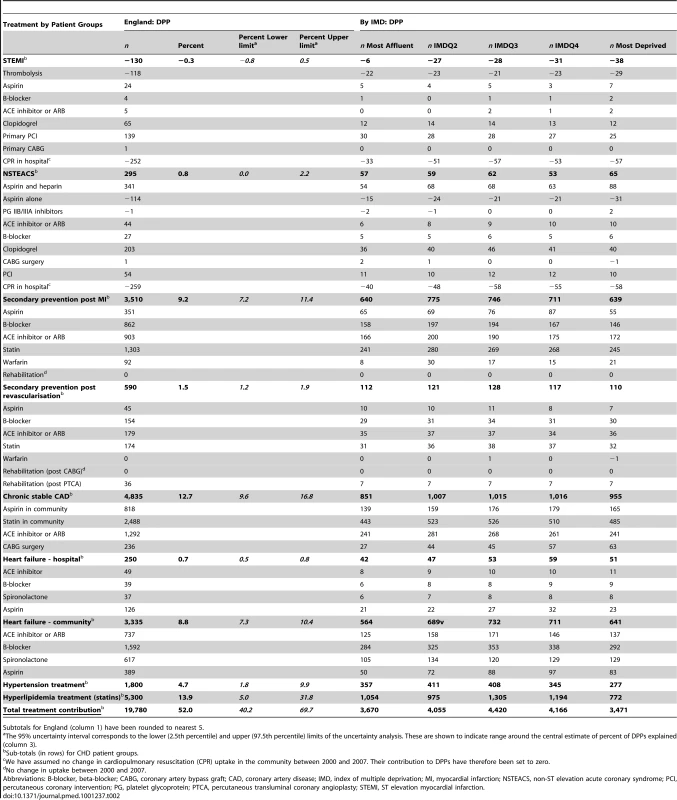
Subtotals for England (column 1) have been rounded to nearest 5. Tab. 3. CHD deaths prevented or postponed due to changes in risk factor prevalence between 2000 and 2007 in England and stratified by deprivation quintiles. 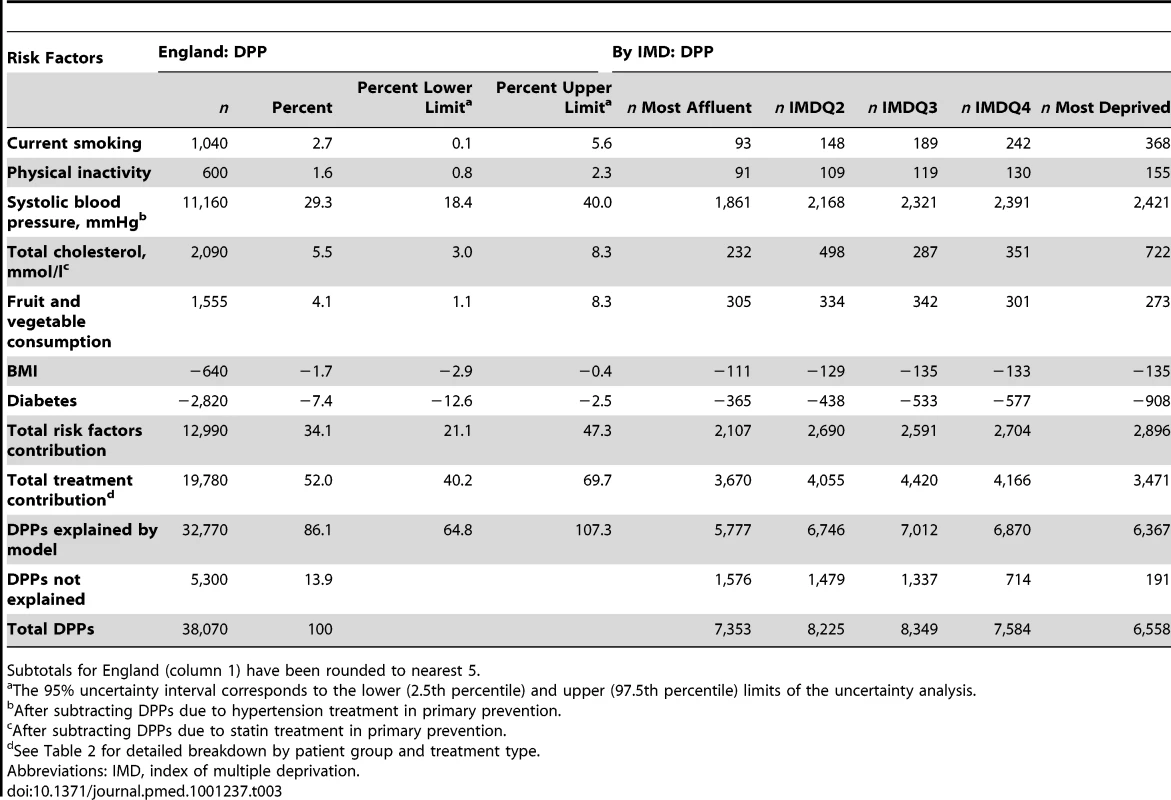
Subtotals for England (column 1) have been rounded to nearest 5. Tab. 4. Percentage distribution of deaths prevented of postponed by deprivation quintile. 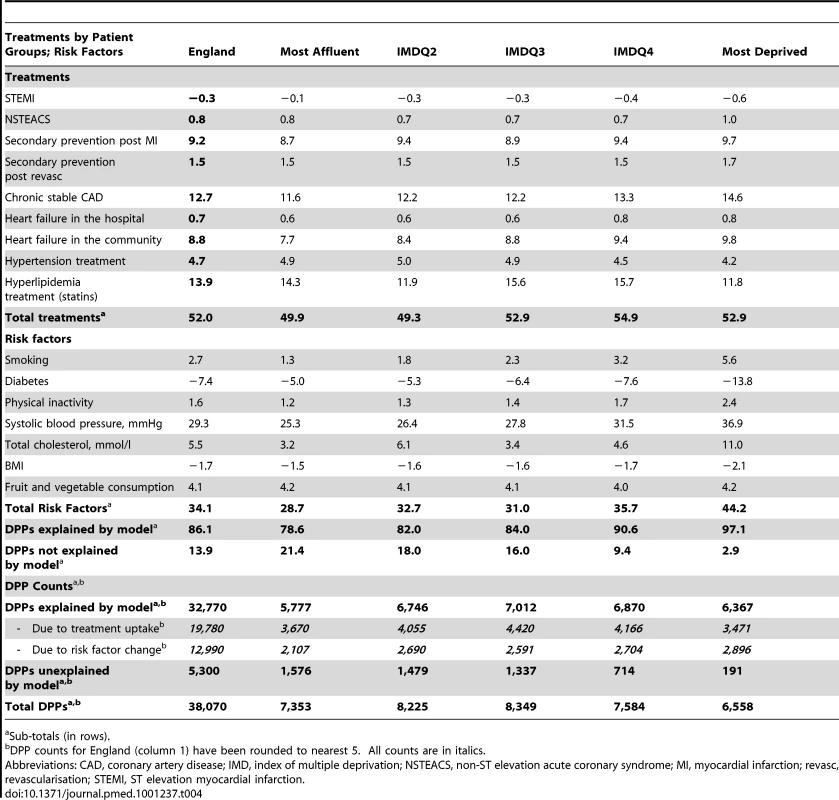
Sub-totals (in rows). The most substantial contribution to deaths prevented by treatments came from statin treatment for hyperlipidemia (14% of the total mortality reduction, 5%–32%), management of chronic stable coronary artery disease (13%; 10%–17%), and secondary prevention following myocardial infarction or revascularisation (11%; 8%–13%) (Table 2). Uptake rates of statins and angiotensin-converting enzyme inhibitors (ACE inhibitors) or angiotensin receptor blockers (ARB) more than doubled for secondary prevention and the management of stable coronary artery disease (Table 5). These two therapies together contributed some 6,340 DPPs (17%). In contrast, deaths averted due to changes in treatment uptake in hospital-based patient groups were relatively modest: contributing just 165 fewer deaths (0.5%; −1% to 3%) amongst emergency admissions for infarction and unstable angina (ST elevation myocardial infarction [STEMI] and non-ST elevation acute coronary syndrome [NSTEACS], respectively). Improved heart failure treatments in the community resulted in approximately 3,335 fewer deaths (9%; 7%–10%), with relatively modest gains (250 fewer deaths) in hospitalised patients. Furthermore, there were essentially no gradients in treatment uptake across deprivation quintiles for either hospital treatment or drugs prescribed in the community for secondary prevention and heart failure (Table 5).
Tab. 5. Percentage treatment uptake rates 2000 and 2007 for England and stratified by deprivation quintiles. 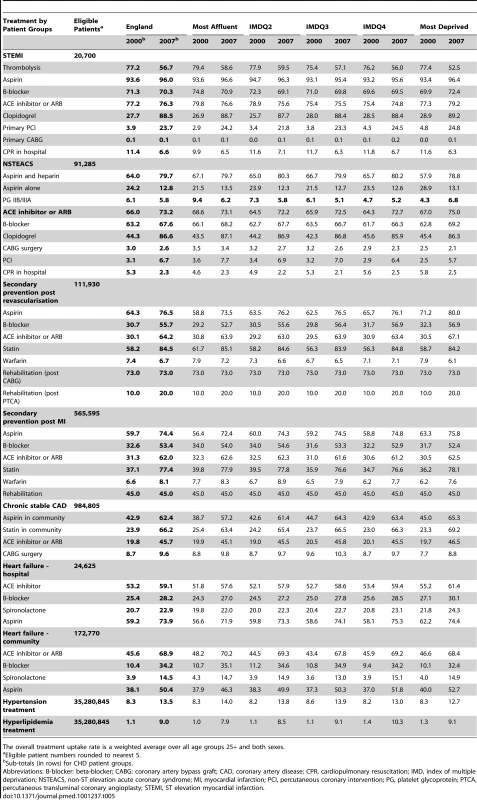
The overall treatment uptake rate is a weighted average over all age groups 25+ and both sexes. Of the deaths prevented due to population-level risk factor changes, the largest contribution came from the fall in systolic blood pressure amongst those not on hypertensive medications (11,160 fewer deaths, or 29%; 18%–40%) (Table 3). On the other hand, gains from hypertensive medication were modest (approximately 1,800 fewer deaths [5%; 2%–10%]) (Table 2). Blood pressure falls were twice as high in women (5.4 mmHg versus 2.5 mmHg in men) but were of a similar magnitude across all deprivation quintiles (Table 6). Both in terms of absolute numbers and proportions, more deaths were prevented because of blood pressure falls in the most deprived quintile than in the most affluent (Tables 3 and 4).
Tab. 6. Absolute change in risk factor levels between 2000 and 2007 for England and stratified by deprivation quintiles and sex. 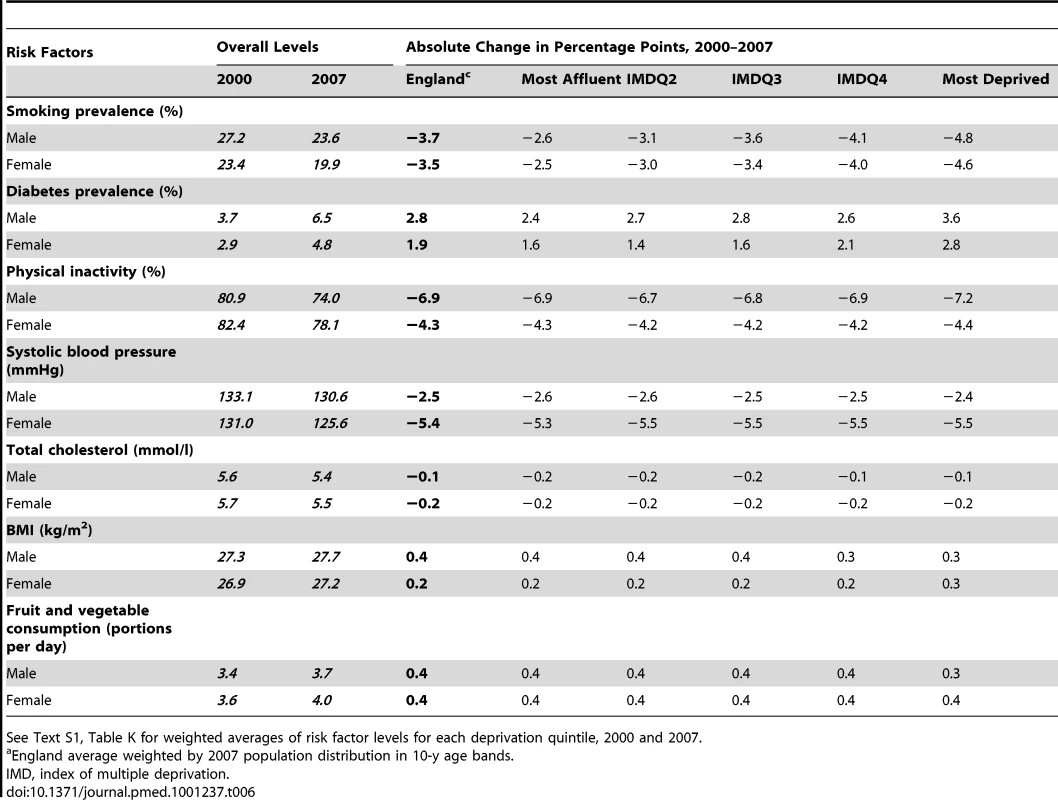
See Text S1, Table K for weighted averages of risk factor levels for each deprivation quintile, 2000 and 2007. In contrast, the benefits attributable to statin lowering of total cholesterol levels were double those attributable to the fall in cholesterol levels in the population not on treatment (approximately 5,300 versus 2,090 fewer deaths, respectively). Between 2000 and 2007, hyperlipidemia treatment increased nine-fold across all social groups from 1% to 9% (Table 5). Total cholesterol levels fell marginally more in women than men and by a similar magnitude across deprivation quintiles (Table 6). Thus, while the proportionate fall in deaths attributable to cholesterol reduction in the general population was similar across quintiles, in absolute terms more deaths were prevented in the most deprived quintiles (Table 3).
Favourable trends in smoking, fruit and vegetable consumption, and physical activity were modest; together only contributing about 3,195 fewer deaths, or 8% (2%–18%) of the overall mortality fall (Table 2). Smoking prevalence declined in men and women by a similar amount (4%); however, there was a clear social gradient with larger absolute falls in smoking prevalence in more deprived quintiles (Table 6). Furthermore, levels of smoking still remained twice as high in the most deprived compared to affluent groups (Text S1, Table K). Physical inactivity fell more in men (7%) than women (4%) across all deprivation quintiles; however, three in four adults remained classed as inactive in every quintile.
Mortality gains due to positive trends in smoking, fruit and vegetable consumption, and physical activity risk factors were negated by increases in BMI and diabetes (together contributing 3,460 additional deaths, equivalent to an 9% increase in mortality (−17% to −3%) (Table 3). Even over the relatively short period of this analysis, the social gradient in diabetes became more pronounced resulting in three times as many additional diabetes-related deaths in the most deprived quintile compared with the most affluent.
Model Fit
The percentage unexplained by the model varied by age, sex, and SECs. The model fit was generally good overall and in women and men living in the most deprived areas (Text S1, Table L.3). However, the fit was least good in affluent quintiles, with the 95% uncertainty limits around the DPPs explained by the model (5,777; 4,134–7,420) just overlapping with the number of observed DPPs (7,353). Model fit was also better for women than men (see Text S1, Figure L.1).
Discussion
Between 2000 and 2007, English CHD mortality rates fell by an impressive 36%, resulting in approximately 38,000 fewer CHD deaths in 2007. However the relative mortality inequalities between rich and poor persisted and even increased slightly over this period. This study is the first, to our knowledge, to analyse the socioeconomic components concealed within the overall mortality reductions attributable specifically to risk factor trends and to evidence-based treatments. By using deprivation scores for area of residence as a unified marker of SECs across all relevant large databases of population health and health service use in England, the study had adequate statistical size to quantify the impact of changes in risk factors and treatments within socioeconomic groups, even over a relatively short period of 7 y. Understanding these recent trends, and their socially divergent trajectories, will be crucial to planning the most effective and equitable future strategies to prevent cardiovascular disease and reduce inequalities.
Main Findings
Approximately half the fall in CHD mortality was attributable to increased medical therapies. These benefits largely reflected a doubling of drug use for community patients with chronic disease (who represent the largest CHD burden). In contrast, the contribution of medical interventions in hospital was relatively modest. Firstly, because the numbers of patients admitted to hospital with acute disease were much smaller. Secondly, because few new treatments were introduced after 2000 other than clopidogrel and primary angioplasty. And thirdly, the uptake rates for existing hospital-based treatments were already close to maximum levels in 2000. The age-specific prevalence of CHD is socially graded. With similar levels of uptake of treatments across socioeconomic quintiles in both base and final years, this meant that the benefits of increased treatment were distributed remarkably evenly across social groups, which suggests a fairly equitable distribution of therapies across the NHS.
Reductions in major cardiovascular risk factors explained over two-fifths of the fall in CHD mortality (43%). However, the net benefit was much smaller (approximately 34%) because adverse trends in BMI and diabetes potentially increased mortality by some 9%.
The single largest contribution to the overall CHD mortality decrease came from population falls in blood pressure [17] with relatively small gains from hypertension therapies. Furthermore, reductions were similar across social groups. This is therefore entirely consistent with recent UK population-wide reductions in salt intake [18], and with recent encouraging trends in other wealthy counties [19].
Small increases in fruit and vegetable consumption and physical activity were seen across all social groups. Furthermore, moderate declines in smoking levels were actually greater in deprived areas. This may reflect the benefit of cumulative tobacco control policies since 2000, reinforced by the targeting of cessation services in deprived areas [20].
However, after excluding the effect of statin therapy, the decline in cholesterol levels in the wider population was modest. This finding may well reflect a failure to implement more effective dietary policies [21]. Particularly worrying was the approximately 3,500 additional deaths attributable to the continuing rises in diabetes and BMI. This number is consistent with recent Foresight analyses and represents a further warning to policy makers [22].
The absolute gap in CHD mortality between the most affluent and most deprived groups narrowed over the period of our study, however relative inequalities widened. This was unlikely to be due to differential treatment of diagnosed patients because levels of uptake of evidence-based therapies were similar for all groups. The pace of fall in mortality in the most affluent groups was faster; but changes in risk factor levels could not explain about 20% of this fall. By contrast, in the most deprived quintile, changes in risk factor levels explained almost all of the remaining CHD mortality fall after accounting for deaths averted due to increase in treatment uptake rates. Perhaps the most likely explanation for this difference is a social gradient in effect modification. Thus, the current model assumed that the mortality decrease per unit change in risk factor was similar across deprivation quintiles. However, the benefits of a specific decrease in blood pressure or cholesterol may be disproportionately higher in more affluent groups, perhaps reflecting synergy with other positive trends [23]. A recent cohort analysis found that even if four classic risk factors—blood pressure, cholesterol, smoking, and diabetes—were to be completely eliminated in middle-aged men, relative inequalities in CHD mortality between those in low and high employment grades would persist despite a 70% reduction in absolute mortality differences [24]. Furthermore we do not have many estimates of the cumulative benefit associated with a lifetime of low risk. For example, the Finnish Public Sector Study found that a marked socioeconomic gradient in absolute risk of CHD mortality persisted even in a low-risk subgroup that had never smoked, were not obese or physically inactive, and who consumed moderate amounts of alcohol [25].
Alternative explanations for the fraction of the mortality fall unexplained by the model include the possible omission of more “upstream” risks such as psychosocial stress, which might differentially benefit affluent groups [23],[26]. Differential levels of adherence to prescribed medications may also play a role; however, this is a relatively under-researched area without clear-cut evidence to support or refute the existence of systematic social gradients [27]–[29]. We also tested the impact of varying adherence rates differentially on the DPPs explained. However, varying adherence rates in this way had a limited effect on reducing the gradient in the proportion unexplained. Finally, measurement error may contribute; Health Survey estimates of risk factor trends by deprivation quintiles may lack precision because of small samples and differential response rates.
Comparisons with Other UK and International Studies
Compared with previous IMPACT analyses from a baseline of the 1980s [4],[5],[30]–[33], models of more recent changes, for example in Ontario [6], demonstrate the growing relative contribution from improved treatments to reductions in CHD mortality. However, country-specific proportions attributable to risk factors or treatments are relative to the scale of the decline, and hence potentially misleading. Thus, although Nordic countries possess uniformly good health services, their larger absolute falls in coronary mortality mainly reflect particularly impressive decreases in major risk factors, mainly cholesterol, blood pressure and smoking, and smaller increases in obesity and diabetes [33],[34].
Strengths and Limitations of This Study
The IMPACT model has been replicated and validated in diverse national populations. This is the first IMPACT study to quantify the socioeconomic components of the contributions of changes in treatment and risk factors to falls in coronary mortality. The main datasets used are reasonably representative of the socioeconomic distribution of the English population and large enough for reasonably accurate estimates of socioeconomic change.
However, a number of limitations should also be acknowledged. These include the use of area-level categorisation of SECs. However, area deprivation correlates well with individual socioeconomic position and may also help to capture the contextual effects of living conditions [35],[36].
Approximately 14% of the CHD mortality fall was not explained by the model and the uncertainty analysis also produced wide limits in the percentage explained (86%; 65%–107%). The model fit was also less good in men in affluent areas, as discussed earlier. However, the model fit was generally good overall and in women and in men living in the most deprived areas. As with all models attempting to capture complex and interacting changes, it remains possible that there were additional (unquantifiable) sources of error not captured by the uncertainty analysis.
Conclusions and Implications for Future Prevention Policies and Strategies
Approximately half of the recent substantial CHD mortality fall in England was attributable to medical therapies. Benefits were relatively even across social groups. These findings are consistent with equitable service delivery across the NHS. Treatment uptake in hospitals was close to maximum levels over the entire period, while follow-up treatment of cardiovascular patients in the community substantially improved and was equitable. This suggests the Qualities and Outcome Framework that was being implemented in general practice during the study period was an effective incentive for improving uptake overall [37].
However, the net gains from risk factor improvements were small, reflecting modest recent decreases in powerful cardiovascular risk factors such as smoking and cholesterol, and further eroded by continuing rises in BMI and diabetes. This throws a spotlight on recent UK policies for salt reduction and tobacco control (relatively effective) and healthier diets (relatively neglected). Elsewhere, the successful introduction of effective, powerful, rapid, and cost-saving policy interventions have achieved substantial reductions in the saturated fat, trans-fats, sugars, and calories hidden in processed food, takeaways, and sweetened drinks [21],[37],[38]. Mandatory interventions involving legislation, regulation, taxation, or subsidies consistently appear more effective and cost saving than voluntary schemes [19],[39],[40]. They also tend to be equitable [12] and surprisingly rapid [15],[38]. The UK now has an equally pressing need for population-wide policy interventions to effectively tackle persistent inequalities in cardiovascular mortality.
Supporting Information
Zdroje
1. BajekalMScholesSO'FlahertyMRaineRNormanP 2010 Trends in CHD mortality by socioeconomic circumstances, England 1982–2006. J Epidemiol Community Health 64Suppl 1 p.A2
2. The Marmot Review 2010 Fair society, healthy lives: strategic review of health inequalities in England post-2010. London: The Marmot Review, Available: http://www.instituteofhealthequity.org/projects/fair-society-healthy-lives-the-marmot-review
3. LeylandAH 2004 Increasing inequalities in premature mortality in Great Britain. J Epidemiol Community Health 58 296 302
4. UnalBCritchleyJACapewellS 2004 Explaining the decline in coronary heart disease mortality in England and Wales between 1981 and 2000. Circulation 109 1101 1107
5. FordESAjaniUACroftJBCritchleyJALabartheDR 2007 Explaining the decrease in US deaths from coronary disease, 1980–2000. N Engl J Med 356 2388 2398 Detailed technical appendix of model available available: http://www.nejm.org/doi/suppl/10.1056/NEJMsa053935/suppl_file/nejm_ford_2388sa1.pdf
6. WijeysunderaHCMachadoMFarahatiFWangXWittemanW 2010 Association of temporal trends in risk factors and treatment uptake with coronary heart disease mortality, 1994–2005. JAMA 303 1841 1847
7. Department of Health 2000 National service framework for coronary heart disease Crown Copyright, London Department of Health
8. The NHS Information Centre for Health and Social Care 2004 Quality and outcomes framework: Introduction to QOF. Available: http://www.ic.nhs.uk/statistics-and-data-collections/supporting-information/audits-and-performance/the-quality-and-outcomes-framework/qof-information/introduction-to-qof. Accessed 8 May 2012
9. UK Food Standards Agency 2006 New salt reduction targets published as part of FSA campaign to reduce salt in our diets. Available: http://webarchive.nationalarchives.gov.uk/20120206100416/http://food.gov.uk/news/pressreleases/2006/mar/targets. Accessed 8 May 2012
10. UK Food Standards Agency 2007 FSA Board recommends voluntary approach to trans fats in food. Available: http://webarchive.nationalarchives.gov.uk/20120206100416/http://food.gov.uk/news/newsarchive/2007/dec/trans. Accessed 8 May 2012
11. House of Commons Committee of Public Accounts 2010 Tackling inequalities in life expectancy in areas with the worst health and deprivation. House of Commons London: The Stationery Office Limited. Available: http://www.publications.parliament.uk/pa/cm201011/cmselect/cmpubacc/470/470.pdf. Accessed 8 May 2012
12. CapewellSGrahamH 2010 Will cardiovascular disease prevention widen health inequalities? PLoS Med 7 e10000320 doi:10.1371/journal.pmed.1000320
13. Department for Communities and Local Government 2007 The English indices of deprivation 2007. Available www.communities.gov.uk/publications/communities/indicesdeprivation07. Accessed 8 May 2012
14. MantJHicksN 1995 Detecting differences in quality of care - the sensitivity of measures of process and outcome in treating acute myocardial infarction. BMJ 311 793 796
15. KuulasmaaKTunstall-PedoeHDobsonAFortmannSSansS 2000 Estimation of contribution of changes in classic risk factors to trends in coronary-event rates across the WHO MONICA project populations. Lancet 355 675 687
16. BarendregtJJ 2010 The effect size in uncertainty analysis. Value in Health 13 388 391
17. Tunstall-PedoeHConnaghanJWoodwardMTolonenHKuulasmaaK 2006 Pattern of declining blood pressure across replicate population surveys of the WHO MONICA project, mid-1980s to mid-1990s, and the role of medication. BMJ 332 629 632
18. UK Food Standards Agency 2008 An assessment of dietary sodium levels among adults (aged 19–64) in the UK general population in 2008, based on analysis of dietary sodium in 24 hour urine samples. London: National Centre for Social Research. Available: http://www.food.gov.uk/multimedia/pdfs/08sodiumreport.pdf. Accessed 8 May 2012
19. DanaeiGFinucaneMMLinJKSinghGMPaciorekCJ 2011 National, regional, and global trends in systolic blood pressure since 1980: systematic analysis of health examination surveys and epidemiological studies with 786 country-years and 5·4 million participants. Lancet 377 568 577
20. BauldLJudgeKPlattS 2007 Assessing the impact of smoking cessation services on reducing health inequalities in England: observational study. Tob Control 16 400 404
21. National Institute of Health and Clinical Excellence 2010 Prevention of cardiovascular disease at population level. Available: http://guidance.nice.org.uk/PH25/. Accessed 8 May 2012
22. Foresight 2007 Tackling obesities: future choices. UK Government Office of Science. Available: http://www.bis.gov.uk/foresight/our-work/projects/published-projects/tackling-obesities/reports-and-publications
23. YusufSHawkenSOunpuuSDansTAvezumA 2004 Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): case-control study. Lancet 364 937 952
24. KivimäkiMShipleyMJFerrieJESingh-ManouxABattyGD 2008 Best-practice interventions to reduce socioeconomic inequalities of coronary heart disease mortality in UK: a prospective occupational cohort study. Lancet 372 1648 1654
25. KivimäkiMLawlorDADavey SmithGKouvonenAVirtanenM 2007 Socioeconomic position, co-occurrence of behavior-related risk factors, and coronary heart disease: the Finnish Public Sector study. Am J Public Health 97 874 879
26. HaraldKKoskinenSJousilahtiPTorppaJVartiainenE 2008 Changes in traditional risk factors no longer explain time trends in cardiovascular mortality and its socioeconomic differences. J Epidemiol Community Health 62 251 257
27. National Co-ordinating Centre for NHS Service Delivery and Organisation R&D 2005 Concordance, adherence and compliance in medicine taking. Available: http://www.medslearning.leeds.ac.uk/pages/documents/useful_docs/76-final-report%5B1%5D.pdf. Accessed 8 May 2012
28. OckeneJMaYZapkaJPbertLValentine GoinsK 2002 Spontaneous cessation of smoking and alcohol use among low-income pregnant women. Am J Prev Med 23 150 159
29. SchüzBMarxCWurmSWarnerLMZiegelmannJP 2011 Medication beliefs predict medication adherence in older adults with multiple illnesses J Psychosom Res 70 179 187
30. CapewellSMorrisonCEMcMurrayJJ 1999 Contribution of modern cardiovascular treatment and risk factor changes to the decline in coronary heart disease mortality in Scotland between 1975 and 1994. Heart 81 380 386
31. CapewellSBeagleholeRSeddonMMcMurrayJ 2000 Explanation for the decline in coronary heart disease mortality rates in Auckland, New Zealand, between 1982 and 1993. Circulation 102 1511 1516
32. PalmieriLBennettKGiampaoliSCapewellS 2010 Explaining the decrease in coronary heart disease mortality in Italy between 1980 and 2000. Am J Public Health 100 684 692
33. AspelundTGudnasonVMagnusdottirBTAndersenKSigurdssonG 2010 Analysing the large decline in coronary heart disease mortality in the Icelandic population aged 25–74 between the years 1981 and 2006. PloS One 5 e13957 doi:10.1371/journal.pone.0013957
34. LeylandAH 2005 Socioeconomic gradients in the prevalence of cardiovascular disease in Scotland: the roles of composition and context. J Epidemiol Community Health 59 799 803
35. LaatikainenTCritchleyJVartiainenESalomaaVKetonenM 2005 Explaining the decline in coronary heart disease mortality in Finland between 1982 and 1997. Am J Epidemiol 162 764 773
36. Davey SmithGHartCWattGHoleDHawthorneV 1998 Individual social class, area-based deprivation,cardiovascular disease risk factors, and mortality: the Renfrew and Paisley study. J Epidemiol Community Health 52 399 405
37. DoranTKontopantelisEValderasJMCampbellSRolandM 2011 Effect of financial incentives on incentivised and non-incentivised clinical activities: longitudinal analysis of data from the UK Quality and Outcomes Framework. BMJ 342 d3590 doi:10.1136/bmj.d3590
38. ZatonskiWAWillettW 2005 Changes in dietary fat and declining coronary heart disease in Poland: population based study. BMJ 331 187 188
39. CobiacLJVosTVeermanJL 2010 Cost-effectiveness of interventions to reduce dietary salt intake. Heart 96 1920 1925
40. GlantzSGonzalezM 2012 Effective tobacco control is key to rapid progress in reduction of non-communicable diseases. Lancet 379 1269 1271
Štítky
Interní lékařství
Článek vyšel v časopisePLOS Medicine
Nejčtenější tento týden
2012 Číslo 6- Berberin: přírodní hypolipidemikum se slibnými výsledky
- Léčba bolesti u seniorů
- Příznivý vliv Armolipidu Plus na hladinu cholesterolu a zánětlivé parametry u pacientů s chronickým subklinickým zánětem
- Červená fermentovaná rýže účinně snižuje hladinu LDL cholesterolu jako vhodná alternativa ke statinové terapii
- Jak postupovat při výběru betablokátoru − doporučení z kardiologické praxe
-
Všechny články tohoto čísla
- Point-of-Care Tests to Strengthen Health Systems and Save Newborn Lives: The Case of Syphilis
- Tobacco Industry Manipulation of Tobacco Excise and Tobacco Advertising Policies in the Czech Republic: An Analysis of Tobacco Industry Documents
- Global Health Governance and the Commercial Sector: A Documentary Analysis of Tobacco Company Strategies to Influence the WHO Framework Convention on Tobacco Control
- Why Human Health and Health Ethics Must Be Central to Climate Change Deliberations
- Connecting the Global Climate Change and Public Health Agendas
- Protecting Clinical Trial Participants and Protecting Data Integrity: Are We Meeting the Challenges?
- Food Sovereignty: Power, Gender, and the Right to Food
- Clinical Trials Have Gone Global: Is This a Good Thing?
- Analysing Recent Socioeconomic Trends in Coronary Heart Disease Mortality in England, 2000–2007: A Population Modelling Study
- Soda and Tobacco Industry Corporate Social Responsibility Campaigns: How Do They Compare?
- Series on Big Food: The Food Industry Is Ripe for Scrutiny
- Big Food, Food Systems, and Global Health
- Manufacturing Epidemics: The Role of Global Producers in Increased Consumption of Unhealthy Commodities Including Processed Foods, Alcohol, and Tobacco
- A Multifaceted Intervention to Improve the Quality of Care of Children in District Hospitals in Kenya: A Cost-Effectiveness Analysis
- Reproductive Outcomes Following Ectopic Pregnancy: Register-Based Retrospective Cohort Study
- Nevirapine- Versus Lopinavir/Ritonavir-Based Initial Therapy for HIV-1 Infection among Women in Africa: A Randomized Trial
- Long-Term Risk of Incident Type 2 Diabetes and Measures of Overall and Regional Obesity: The EPIC-InterAct Case-Cohort Study
- Comparative Performance of Private and Public Healthcare Systems in Low- and Middle-Income Countries: A Systematic Review
- Bacterial Vaginosis Associated with Increased Risk of Female-to-Male HIV-1 Transmission: A Prospective Cohort Analysis among African Couples
- PLOS Medicine
- Archiv čísel
- Aktuální číslo
- Informace o časopisu
Nejčtenější v tomto čísle- Tobacco Industry Manipulation of Tobacco Excise and Tobacco Advertising Policies in the Czech Republic: An Analysis of Tobacco Industry Documents
- Why Human Health and Health Ethics Must Be Central to Climate Change Deliberations
- Clinical Trials Have Gone Global: Is This a Good Thing?
- Point-of-Care Tests to Strengthen Health Systems and Save Newborn Lives: The Case of Syphilis
Kurzy
Zvyšte si kvalifikaci online z pohodlí domova
Současné možnosti léčby obezity
nový kurzAutoři: MUDr. Martin Hrubý
Všechny kurzyPřihlášení#ADS_BOTTOM_SCRIPTS#Zapomenuté hesloZadejte e-mailovou adresu, se kterou jste vytvářel(a) účet, budou Vám na ni zaslány informace k nastavení nového hesla.
- Vzdělávání



