-
Články
Top novinky
Reklama- Vzdělávání
- Časopisy
Top články
Nové číslo
- Témata
Top novinky
Reklama- Videa
- Podcasty
Nové podcasty
Reklama- Kariéra
Doporučené pozice
Reklama- Praxe
Top novinky
ReklamaBuilding the Field of Health Policy and Systems Research: An Agenda for Action
article has not abstract
Published in the journal: . PLoS Med 8(8): e32767. doi:10.1371/journal.pmed.1001081
Category: Policy Forum
doi: https://doi.org/10.1371/journal.pmed.1001081Summary
article has not abstract
PLoS Medicine Series on HPSR
Following the First Global Symposium on Health Systems Research in Montreux in November 2010, PLoS Medicine commissioned three articles on the state-of-the-art in Health Policy and Systems Research (HPSR). Three Policy Forum articles, authored by a diverse group of global health academics, critically examine the current challenges to the field and lay out what is needed to build capacity in HPSR and support local policy development and health systems strengthening, especially in low and middle income countries.
Paper 1. Kabir Sheikh and colleagues. Building the Field of Health Policy and Systems Research: Framing the Questions.
Paper 2. Lucy Gilson and colleagues. Building the Field of Health Policy and Systems Research: Social Science Matters
Paper 3. Sara Bennett and colleagues. Building the Field of Health Policy and Systems Research: An Agenda for Action
Summary Points
-
There is an urgent need to build the Health Policy and Systems Research (HPSR) field and in particular to develop understanding across different disciplinary boundaries.
-
The development of HPSR is impeded by a cluster of related issues, namely (i) a heavy reliance on international funding for HPSR, (ii) an excessive focus on the direct utility of HPSR findings from specific studies, and (iii) a tendency to under-value contributions to HPSR from social sciences.
-
Innovations in funding HPSR are needed so that local actors, including policy-makers, civil society, and researchers, have a greater say in determining the nature of HPSR conducted.
-
Strategic investment should be made in promoting a greater shared understanding of theoretical frames and methodological approaches for HPSR including, for example, the development of HPSR journals, methodological workshops, and shared HPSR teaching curricula.
-
Dedicated and supportive homes for HPSR need to be found within universities, and also be developed as independent research institutes.
Introduction
The lack of clarity and shared understanding regarding the scientific foundations of Health Policy and Systems Research (HPSR) [1] potentially has very negative consequences for the field [2]. Disagreement over the value of different types of theoretical frameworks and research methods can lead to inappropriate evaluations of research proposals, contradictory reviews of the same paper, and delays in publication. Excessive time may be spent communicating broad frameworks to other researchers within HPSR, inhibiting progression to more detailed and specific conversations. Communication barriers may discourage inter-disciplinary collaboration, driving researchers back to their disciplinary safety zones, and creating potential for conflict that may discourage younger researchers who may be less secure in their career from staying in the field. As the second paper in this series concluded [1], there is an urgent need to build understanding across disciplinary boundaries. This final paper in the “Building the Field of HPSR” series turns to practical questions concerning how to remove structural barriers that currently inhibit the development of the HPSR field and thus unlock HPSR capacities.
HPSR suffers from many of the same problems as other branches of health research in low - and middle-income countries (LMICs): major imbalances between the resources available in high - versus low - and middle-income contexts [3], acute shortages of skilled researchers (especially senior ones), and relatively few organizations that house HPSR expertise [4]. Historically, low levels of funding for HPSR compared to clinical or biomedical research have compounded these problems. Many papers provide relevant recommendations to address health research capacity issues in LMICs [5]–[8]. However, there is also a nexus of issues specific to HPSR that currently constrains development of the field. This paper builds on the analysis of the previous papers in this series [1],[9] to investigate the practical problems faced and then develops an agenda for building the HPSR field.
Unpacking the Problem
The development of HPSR is affected by a series of interconnected problems:
-
a heavy reliance on international funding for HPSR;
-
an excessive focus on the direct utility of HPSR findings from specific studies;
-
a tendency to under-value contributions to HPSR from social sciences.
While the first of these problems may not be unique to HSPR, its significance is: HPSR—unlike clinical or biomedical research—should be driven by understanding of local contexts. At all stages of the research endeavor, from prioritization of research questions, to conceptualization and conduct of the research, to interpretation of and communication of findings, HPSR will benefit from being embedded within a particular context and close engagement with local actors.
In LMICs (particularly low-income countries), current funding for HPSR comes predominantly from external sources, notably international and bilateral agencies, but also via sub-contracts through larger research consortia typically led by Northern researchers [10]. A further important source of funding for “HPSR-type” analysis (though rarely undertaken with the rigor of research) comes from short-term consulting contracts. Consultancies commissioned by aid agencies may crowd out HPSR that is responsive to local needs [11].
Global funding for HPSR is frequently focused on programmatic or operational questions with a primary concern of how to expedite the scale up of priority services [10]. It is less likely to address deeper, more structural questions (such as how to promote accountability in health systems) or to support action research that actively engages stakeholders in improving health systems. In part, this is due to the nature of new funding agencies in the field who are frequently focused on achieving global targets, and thus prioritize research that leads to generalizable conclusions supporting decision-making and service scale up, across LMIC contexts. It is unclear to what extent local actors in LMIC health systems would frame their research concerns in the same way as global stakeholders.
One of the strengths of HPSR is that it is frequently of direct instrumental value, leading to changes in policy and practice. But research findings can also be influential in less direct ways, for example, by shifting the framing of health policy debates, and gradually influencing the nature of dialogue [12],[13]. These indirect influences of research can be more significant than direct ones. Frequently, direct use of research addresses marginal changes or technical questions such as “Should immunization services be delivered through campaigns or fixed health centers?” or “What salary increase would incentivize health workers to stay in rural areas?” In contrast, research evidence that shapes understanding of the complexity of a problem may ultimately lead to more substantial reforms and greater impacts—but through longer and more circuitous routes [14]. This kind of game-changing research often challenges assumptions and established ways of working, and for this reason it may be neglected or actively resisted by powerful global and national actors [9]. Further, by narrowing the focus of HSPR to specific, short-term questions, opportunities are missed to engage in long-term blue-sky thinking that may address the health systems challenges of tomorrow.
The belief that HPSR should have direct impacts upon policy has led to an emphasis on the more direct forms of knowledge translation such as the development of policy briefs, and hosting of workshops to disseminate research findings. While such activities are important, there is a danger that the less visible, structural factors that critically influence the policy/research interface and involve, for example, the development of long-term relationships between researchers and policy-makers built upon mutual trust and familiarity with the contexts within which each other works, are neglected [15].
The phenomena identified above also contribute to the third concern, the relative neglect of social science within HPSR. The perspectives of new funders to the HPSR field are informed by the type of research (frequently positivist and biomedical) that they are accustomed to funding as well as by their perception of current priority research questions. Relativist perspectives often provide nuanced insights into how to implement a policy or why a policy is ineffective, but rarely offer discrete interventions as policy solutions. Building on the user fee example from the second paper in this series (Gilson et al. [1]), Table 1 illustrates the nuanced policy lessons that relativist perspectives may provide compared to the more direct policy lessons sometimes offered by positivist investigations.
Tab. 1. Possible policy implications of alternative types of research on user fees. 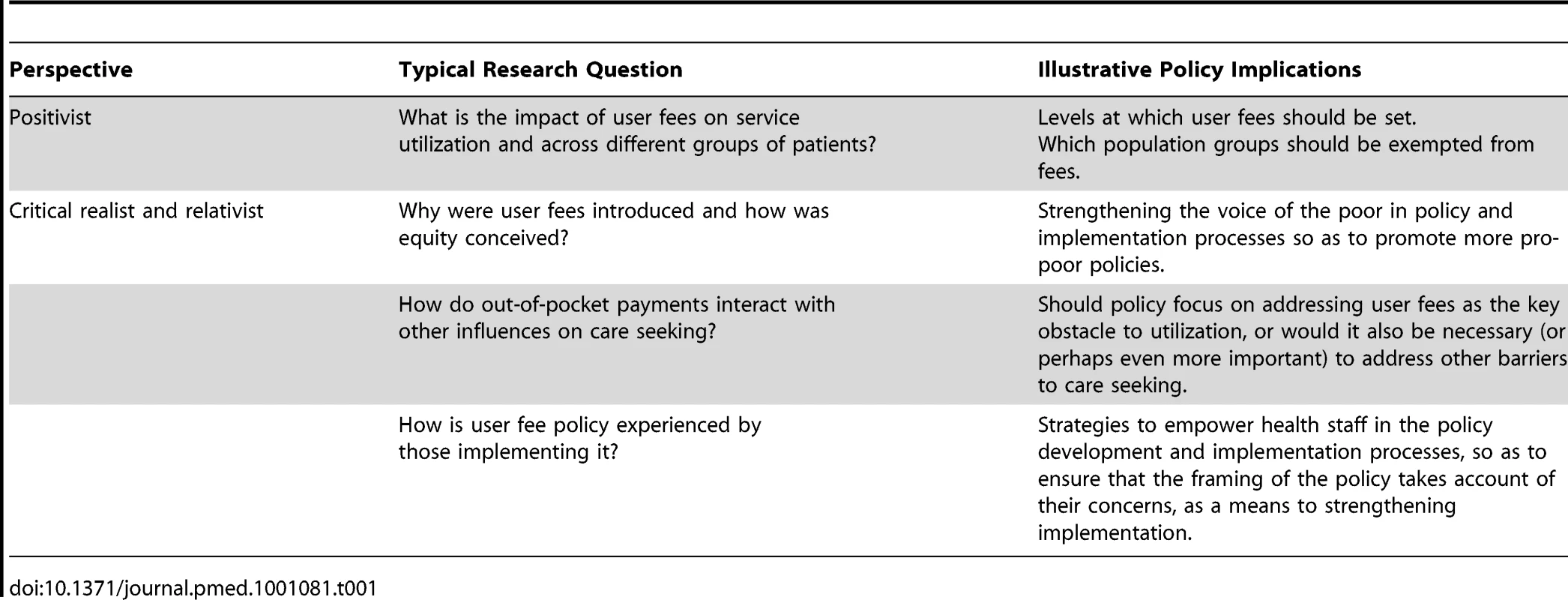
Building Capacity for the Field
So, given these problems, what can be done to take advantage of the growing momentum to develop capacities in the field?
Approaches to capacity development often conceive of capacity as a hierarchy starting from broad systems and structural issues and working up to specific individual skills and competencies. We use a similar approach to describe what needs to be done in the HPSR field (Figure 1).
Fig. 1. Dimensions of capacity in the HPSR field. 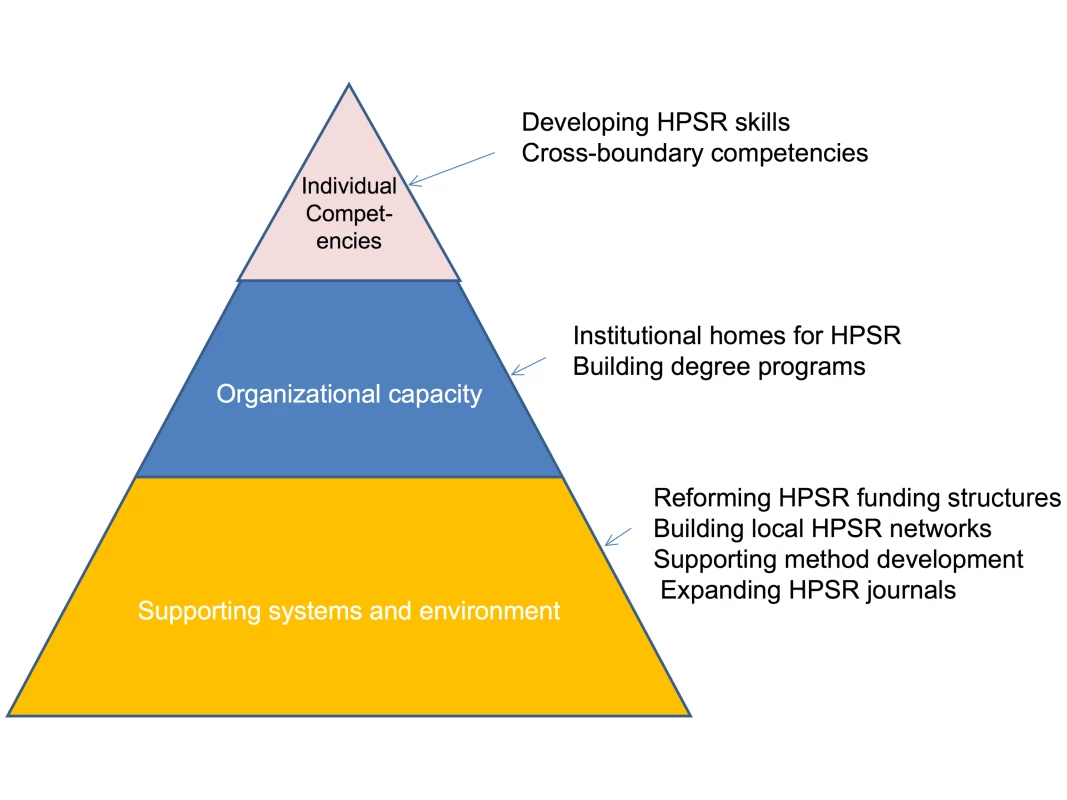
Supporting Systems and the Research Environment
HPSR needs to be driven by local actors who have an intimate understanding of their own health systems and the challenges that they face. Reforming systems for funding HPSR appears crucial in this respect. Despite repeated international commitments to increasing domestic resources for health research, in most LMICs extremely limited national resources are applied to HPSR. Increases in domestic commitments are important, although likely to be difficult to achieve without stronger policy-maker demand for HPSR. In addition, measures that pool a proportion of international research resources at the country level and develop local systems and capacities to allocate these resources in an informed manner need to be explored. The widespread use of consultants could be addressed through dedicating a proportion of consultancy funding to local research departments and organizations as core funding, thus both reducing the temptation for researchers to chase short-term projects, and enabling greater responsiveness to local policy-makers than project funding allows.
The emphasis on international funding and research consortia means that networks between researchers within a country are often neglected. Strengthening national research networks can help achieve multiple goals: strengthening the focus on national research priorities, enhancing capacity through bringing together researchers with differing disciplinary skills, and facilitating longer-term trust-based networks. Developing closer ties between health care providers and managers, policy-makers, and health systems researchers can help promote an organizational culture of evidence-informed decision-making across the health sector, facilitate access to research sites for researchers, and generate a stronger focus on locally identified research questions.
Greater shared understanding of the theoretical frames and methodological approaches that drive the field is also needed. HPSR journals with a focus on LMICs publish primarily empirical papers. Greater opportunities for conceptual work and methodological dialogue are needed, including journal papers, online resources and exchange, and methodological tracks within HPSR conferences. The work of the United States-based Health Services Research Methods Council of AcademyHealth provides one possible approach, providing online and in person methods seminars, and a library of online research resources among other things (see http://www.academyhealth.org/Training/ResourceDetail.cfm?ItemNumber=2418). The Alliance for Health Policy and Systems Research, as the only multilateral agency with a mandate focused on HPSR, has a natural leadership position in supporting such activities, although this should be done in partnership with others. Comparing the evolution of health services research in high-income countries with HPSR in LMICs may also be instructive—while the two fields have developed in parallel, there are surely shared lessons.
Relatively few journals focus on publishing HPSR relevant to LMICs, and there are very few regional or country-specific journals of this nature. As a consequence, researchers try to publish in journals that do not understand the field well—whether social science disciplinary journals or broader public health or biomedical journals—and may receive poorly informed reviews, or have papers rejected outright for either being “too applied” or not applying the kind of research methods that are recognized by the biomedical sciences. Some papers of considerable national or regional policy interest remain unpublished as they do not fit well with priorities of international journals. Expectations regarding paper length and structure also limit HPSR publishing opportunities. Biomedical journals typically expect short papers (3,000–3,500 words in length) with findings presented in tabular formats; for qualitative and mixed-methods studies this is inappropriate. Reduced to short papers for publication, HPSR studies may lose richness and nuance. Mixed-method studies may be split into qualitative and quantitative components and published separately with consequent loss of the synergies between these approaches.
The lack of appropriate outlets for publication creates indirect problems too. Difficulties in publishing may undermine the career development of HPS researchers, and the lack of country and regional journals reinforces the financial incentives for researchers to focus on global HPSR priorities rather than national ones. New HPSR journals, particularly those focused on specific countries or regions, are needed, and general health journals should review their policies in terms of reviewer identification and article length if they seriously wish to accommodate HPSR papers.
Organizational Capacity
HPSR often occupies a tenuous home within universities and academic departments. While much HPSR takes place within schools of public health, few schools have departments dedicated to health policy and systems; instead, HPSR may be housed in departments of epidemiology, community/public health, or health management. Alternatively, HPS researchers may be located in discipline-specific departments (such as economics departments) that may not fully appreciate the applied or inter-disciplinary nature of the field. In such contexts, HPS researchers may struggle for due recognition of their work and be pressured to adopt particular types of research paradigms and methods. For HPSR to develop as a field, dedicated and supportive homes within universities are required and research leadership may need to be educated about the inter-disciplinary nature and contemporary relevance of HPSR. Positioning HPSR as being at the cutting edge of current efforts to work across the boundaries of social and biological sciences [1] may help stimulate enthusiasm and support.
Given the policy-relevant and question-focused nature of HPSR, it is also important to support think tanks and other types of research institutes that can provide stable institutional environments for HPSR as well as offer opportunities for close engagement with policy processes. Case studies of such institutes have highlighted the importance of secure funding, such as endowments, as well as strong links to policy-makers in the success of these institutes [16].
Training curricula for HPSR are lacking and relatively few courses teach HPSR methods relevant to LMICs; instead, HPSR is typically a minor component of the material covered. To generate greater shared understanding of methods, HPSR curricula need to be developed that promote a greater degree of shared perspectives, methodological understandings, and language among those who work in the field. A common approach to categorizing, organizing, and teaching the multiple theoretical frames and methods for HPSR should be developed, as should guidance to help researchers select which type of approach will work best for different types of HPSR questions. Training curricula need to provide a solid orientation to the paradigmatic differences described in the second paper of this series. Two recently funded European Union projects are addressing these issues (CHEPSAA the Consortium for Health Policy and Systems Analysis in Africa and ARCADE, the African Regional Capacity Development for Health Services and Systems Research grant), but the discussions ultimately need to engage the whole of the HPSR community.
Individual Competencies
People come to HPSR with varied backgrounds and needs: some may be trained social scientists who have little understanding of the health sector but wish to apply their skills to health systems questions. Many come from broad public health backgrounds, perhaps with experience in disease control programs. Others are clinical practitioners or researchers who usually have very limited exposure to social sciences. Given the diversity of individuals entering the field, training programs need to be tailored to the needs of different types of entrants, while still ensuring a common basic training in HPSR concepts, approaches, and terminology.
For the inter-disciplinary health systems researcher, a post-graduate training in HPSR is desirable. Much support to research capacity development for HPSR to date has taken the form of short course training [4]. Short courses appear to scale up capacity rapidly to conduct HPSR, but their utility in producing rounded, inter-disciplinary health systems researchers is doubtful. It would be better to invest in graduate training programs and scholarship funding, as student support remains a problem for many HPSR academic programs. Short courses may have a limited role to play in orienting social scientists coming from different fields to HPSR, keeping qualified researchers up-to-date in new developments in the field, or in helping policy - and other decision-makers gain an appreciation of the HPSR field.
The skills needed to be effective in inter-disciplinary research are often compared to cultural competencies: the ability to listen to other points of view, respect different positions, and communicate ideas effectively without resort to jargon and disciplinary-specific terminology [17]. Other competencies that support work across boundaries include an ability to see the big picture and a strong ethical orientation [18]. HPS researchers need to be consummate boundary crossers, traversing disciplines, organizations, and professions. Training programs should reinforce such competencies, encouraging diverse students to work together. Innovative approaches to structuring academic programs can also promote work across traditional boundaries through interspersing didactic training with practicums or internships, and promoting interaction with practitioners.
Particularly in light of the hostile organizational environments in which some HPS researchers work, mentorship may be key to sustaining interest and skill development. Very few mentorship programs exist and their development requires careful planning to motivate and support overstretched senior researchers who could act as mentors. Given the challenges in developing mentorship schemes, efforts to build communities of practice among HPS researchers within countries and at regional levels may also be helpful.
Conclusions
HPSR is currently at a tipping point. As a new scientific field develops there are likely to be struggles over ideas, resources, and paradigmatic dominance [19]. As HPS researchers we have all spent time repeatedly explaining and justifying what we do, and why we use the methods we do. In its emergent phase HPSR has been characterized by fluidity and sometimes a lack of clarity: the first paper in this series described how HPSR has emerged from questions bubbling up from the field [9].
With increased recognition of the important role that HPSR needs to play in achieving health goals there is a healthy intensification of questions regarding the nature of the field. Given the rush of new blood and interest in HPSR, we urgently need to move beyond individual explanations of what we do. Instead, we need to take advantage of the current interest to develop the programs and structures of a fully-fledged scientific field with core curricula, text books, scientific meetings, communities of practice, academic departments, and journals. Through investment in the range of activities described in this paper (see also Box 1), HPSR can develop into a more crystalline form, underpinned by shared and inter-disciplinary understandings. Only with this consolidated intellectual development can the field of HPSR realize its full potential to contribute new knowledge for health systems strengthening.
Box 1. An Agenda for Action
-
Reform systems for funding HPSR so as to create stronger national ownership
-
Build capacity and understanding of HPSR to enable country level policy - and decision-makers and managers to effectively “manage” the ownership
-
Develop stronger HPSR networks at the national and sub-national levels
-
Build opportunities for methodological dialogue and exchange
-
Develop more HPSR journals, especially at country and regional levels
-
Identify and build sustainable institutions for HPSR in universities and in independent research institutes
-
Focus training on post-graduate courses and develop core training curricula for HPSR
-
Build inter-disciplinary competencies among HPS researchers
Zdroje
1. GilsonLHansonKSheikhKAgyepongIASsengoobaF 2011 Building the field of Health Policy and Systems Research: social science matters. PLoS Med 8 e1001079 doi:10.1371/journal.pmed.1001079
2. PfefferJ 1993 Barriers to the advance of organizational science: paradigm development as a dependent variable. The Academy of Management Review 18 4 599 620
3. NchindaTC 2002 Research capacity strengthening in the South. Soc Sci Med 54 11 1699 1711
4. BennettSPainaLKimCAgyepongIChunharasS 2010 What must be done to enhance capacity for health systems research? Background paper for the First Global Symposium on Health Systems Research, 16–19 November 2010, Montreux, Switzerland
5. WHO 2004 The Mexico Statement on health research: knowledge for better health: strengthening health systems Geneva WHO
6. WHO 2004 World report on knowledge for better health Geneva World Health Organization
7. LansangMADennisR 2004 Building capacity in health research in the developing world. Bull World Health Organ 82 10 764 770
8. NuyensY 2005 No Development without Research: a challenge for research capacity strengthening Geneva Global Forum for Health Research
9. SheikhKGilsonLAgyepongIAHansonKSsengoobaFBennettS 2011 Building the field of Health Policy and Systems Research: framing the questions. PLoS Med 8 e1001073 doi:10.1371/journal.pmed.1001073
10. BennettSAdamTZarowskyCTangcharoensathienVRansonK 2008 From Mexico to Mali: progress in health policy and systems research. Lancet 372 9649 1571 1578
11. ActionAid 2006 Real aid 2: making technical assistance work Johannesburg Action Aid
12. WaltG 1994 How far does research influence policy? European Journal of Public Health 4 4 233 235
13. KuruvillaSMaysNWaltG 2007 Describing the impact of health services and policy research. J Health Serv Res Policy 12 Suppl 1 S1-23 31
14. LewisS 2011 Health services research: rethinking the quest to be useful. J Health Serv Res Policy 16 1 59 61
15. InnvaerSVistGTrommaldMOxmanA 2002 Health policy-makers' perception of their use of evidence: a systematic review. J Health Serv Res Policy 7 4 239 244
16. BennettSCorlukaADohertyJTangcharoensathienVPatcharanarumolW 2011 Influencing policy change: the experience of health think tanks in low and middle income countries. Health Policy Plan E-pub ahead of print 10 May 2011
17. ReichSMReichJA 2006 Cultural competence in interdisciplinary collaborations: a method for respecting diversity in research partnerships. Am J Community Psychol 38 1–2 51 62
18. WilliamsP 2002 The competent boundary spanner. Public Administration 80 1 103 124
19. KuhnTS 1970 The structure of scientific revolutions Chicago Chicago University Press
Štítky
Interní lékařství
Článek vyšel v časopisePLOS Medicine
Nejčtenější tento týden
2011 Číslo 8- Berberin: přírodní hypolipidemikum se slibnými výsledky
- Léčba bolesti u seniorů
- Příznivý vliv Armolipidu Plus na hladinu cholesterolu a zánětlivé parametry u pacientů s chronickým subklinickým zánětem
- Červená fermentovaná rýže účinně snižuje hladinu LDL cholesterolu jako vhodná alternativa ke statinové terapii
- Jak postupovat při výběru betablokátoru − doporučení z kardiologické praxe
-
Všechny články tohoto čísla
- Are HIV Epidemics among Men Who Have Sex with Men Emerging in the Middle East and North Africa?: A Systematic Review and Data Synthesis
- Commercial Serological Tests for the Diagnosis of Active Pulmonary and Extrapulmonary Tuberculosis: An Updated Systematic Review and Meta-Analysis
- How Industry Uses the ICMJE Guidelines to Manipulate Authorship—And How They Should Be Revised
- Ghostwriting Revisited: New Perspectives but Few Solutions in Sight
- Legal Remedies for Medical Ghostwriting: Imposing Fraud Liability on Guest Authors of Ghostwritten Articles
- Can Mobile Phone Data Improve Emergency Response to Natural Disasters?
- Government Inaction on Ratings and Government Subsidies to the US Film Industry Help Promote Youth Smoking
- Building the Field of Health Policy and Systems Research: Framing the Questions
- Building the Field of Health Policy and Systems Research: Social Science Matters
- Building the Field of Health Policy and Systems Research: An Agenda for Action
- Corporate Social Responsibility and Access to Policy Élites: An Analysis of Tobacco Industry Documents
- Improved Response to Disasters and Outbreaks by Tracking Population Movements with Mobile Phone Network Data: A Post-Earthquake Geospatial Study in Haiti
- Changes in Drug Utilization during a Gap in Insurance Coverage: An Examination of the Medicare Part D Coverage Gap
- Serological Testing Versus Other Strategies for Diagnosis of Active Tuberculosis in India: A Cost-Effectiveness Analysis
- Neonatal Mortality Levels for 193 Countries in 2009 with Trends since 1990: A Systematic Analysis of Progress, Projections, and Priorities
- Reporting Guidelines for Survey Research: An Analysis of Published Guidance and Reporting Practices
- Four Arguments against the Adult-Rating of Movies with Smoking Scenes
- Being the Ghost in the Machine: A Medical Ghostwriter's Personal View
- Population Density, Water Supply, and the Risk of Dengue Fever in Vietnam: Cohort Study and Spatial Analysis
- PLOS Medicine
- Archiv čísel
- Aktuální číslo
- Informace o časopisu
Nejčtenější v tomto čísle- Commercial Serological Tests for the Diagnosis of Active Pulmonary and Extrapulmonary Tuberculosis: An Updated Systematic Review and Meta-Analysis
- Are HIV Epidemics among Men Who Have Sex with Men Emerging in the Middle East and North Africa?: A Systematic Review and Data Synthesis
- Government Inaction on Ratings and Government Subsidies to the US Film Industry Help Promote Youth Smoking
- Serological Testing Versus Other Strategies for Diagnosis of Active Tuberculosis in India: A Cost-Effectiveness Analysis
Kurzy
Zvyšte si kvalifikaci online z pohodlí domova
Současné možnosti léčby obezity
nový kurzAutoři: MUDr. Martin Hrubý
Všechny kurzyPřihlášení#ADS_BOTTOM_SCRIPTS#Zapomenuté hesloZadejte e-mailovou adresu, se kterou jste vytvářel(a) účet, budou Vám na ni zaslány informace k nastavení nového hesla.
- Vzdělávání



