-
Články
Top novinky
Reklama- Vzdělávání
- Časopisy
Top články
Nové číslo
- Témata
Top novinky
Reklama- Videa
- Podcasty
Nové podcasty
Reklama- Kariéra
Doporučené pozice
Reklama- Praxe
Top novinky
ReklamaEssential Surgery at the District Hospital: A Retrospective Descriptive Analysis in Three African Countries
Background:
Surgical conditions contribute significantly to the disease burden in sub-Saharan Africa. Yet there is an apparent neglect of surgical care as a public health intervention to counter this burden. There is increasing enthusiasm to reverse this trend, by promoting essential surgical services at the district hospital, the first point of contact for critical conditions for rural populations. This study investigated the scope of surgery conducted at district hospitals in three sub-Saharan African countries.Methods and Findings:
In a retrospective descriptive study, field data were collected from eight district hospitals in Uganda, Tanzania, and Mozambique using a standardized form and interviews with key informants. Overall, the scope of surgical procedures performed was narrow and included mainly essential and life-saving emergency procedures. Surgical output varied across hospitals from five to 45 major procedures/10,000 people. Obstetric operations were most common and included cesarean sections and uterine evacuations. Hernia repair and wound care accounted for 65% of general surgical procedures. The number of beds in the studied hospitals ranged from 0.2 to 1.0 per 1,000 population.Conclusion:
The findings of this study clearly indicate low levels of surgical care provision at the district level for the hospitals studied. The extent to which this translates into unmet need remains unknown although the very low proportions of live births in the catchment areas of these eight hospitals that are born by cesarean section suggest that there is a substantial unmet need for surgical services. The district hospital in the current health system in sub-Saharan Africa lends itself to feasible integration of essential surgery into the spectrum of comprehensive primary care services. It is therefore critical that the surgical capacity of the district hospital is significantly expanded; this will result in sustainable preventable morbidity and mortality.
: Please see later in the article for the Editors' Summary
Published in the journal: . PLoS Med 7(3): e32767. doi:10.1371/journal.pmed.1000243
Category: Research Article
doi: https://doi.org/10.1371/journal.pmed.1000243Summary
Background:
Surgical conditions contribute significantly to the disease burden in sub-Saharan Africa. Yet there is an apparent neglect of surgical care as a public health intervention to counter this burden. There is increasing enthusiasm to reverse this trend, by promoting essential surgical services at the district hospital, the first point of contact for critical conditions for rural populations. This study investigated the scope of surgery conducted at district hospitals in three sub-Saharan African countries.Methods and Findings:
In a retrospective descriptive study, field data were collected from eight district hospitals in Uganda, Tanzania, and Mozambique using a standardized form and interviews with key informants. Overall, the scope of surgical procedures performed was narrow and included mainly essential and life-saving emergency procedures. Surgical output varied across hospitals from five to 45 major procedures/10,000 people. Obstetric operations were most common and included cesarean sections and uterine evacuations. Hernia repair and wound care accounted for 65% of general surgical procedures. The number of beds in the studied hospitals ranged from 0.2 to 1.0 per 1,000 population.Conclusion:
The findings of this study clearly indicate low levels of surgical care provision at the district level for the hospitals studied. The extent to which this translates into unmet need remains unknown although the very low proportions of live births in the catchment areas of these eight hospitals that are born by cesarean section suggest that there is a substantial unmet need for surgical services. The district hospital in the current health system in sub-Saharan Africa lends itself to feasible integration of essential surgery into the spectrum of comprehensive primary care services. It is therefore critical that the surgical capacity of the district hospital is significantly expanded; this will result in sustainable preventable morbidity and mortality.
: Please see later in the article for the Editors' SummaryIntroduction
The current drive towards a health systems approach for delivering health care interventions in Africa opens an opportunity to redress long-standing neglect in the provision of surgical services [1],[2]. Health systems must be flexible enough not only to prevent and treat the high morbidity and mortality from infectious diseases and the increasing prevalence of noncommunicable conditions, but also to alleviate conditions requiring prompt surgical interventions such as obstetric emergencies and trauma cases [3]. The traditional referral-based system in which patients are provided primary health care at first-level referral facilities and referred to secondary and tertiary health care facilities for specialized care has undermined the capacity to provide timely access to essential surgical procedures. Although some surgical conditions can be postponed until the patient can gain access to specialized care, others result in death or severe disability if treatment is delayed. This situation is clearly highlighted in the case of obstetric emergencies in which it is recognized that in order to prevent maternal deaths, cesarean sections can be provided at some first referral facilities, and must be provided at district hospitals. We argue that the same basic surgical skills and equipment needed to perform emergency obstetric procedures are required to treat other surgical conditions and therefore that building surgical capacity has the potential to improve a range of health outcomes.
As funders and national policymakers consider the expansion of health systems in sub-Saharan Africa, accurate data on the current scope of surgery at district hospitals or first-level referral facilities are needed to inform programs to increase access. However, such data are limited or missing altogether. In particular, although the district hospital is the designated first-level provider of surgical services in many African countries, there is only partial information on the nature and volume of surgery performed [4]. There are no population-based studies in the sub-Saharan context that estimate the need for surgical procedures.
This article aims to contribute to the nascent literature on the role of the district hospital in providing essential surgery by describing the scope of surgery at district hospitals from three countries in eastern Africa.
Methods
Selection Criteria
We conducted a retrospective descriptive survey of eight hospitals in three African countries represented at the inaugural meeting of the Bellagio Essential Surgery Group (BESG) in Bellagio, Italy in 2007 [2]: Tanzania, Uganda, and Mozambique (see map in Figure S1). We chose at least two hospitals in three countries to assess variability in service provision. The hospitals were required to be designated district hospitals funded and operated by the government, have 50–150 beds, serve a rural catchment population, and in existence for at least 2 y. Finally, the hospitals had to have cost and utilization data available for 2006 or 2007.
Study Sites
Tanzania, Uganda, and Mozambique are of comparable size and per capita income, and have similar basic public health indicators (Table 1). The health service delivery system in these countries is regionalized and structured as a pyramid with the dispensary at the lowest level and the national referral hospital at the highest level. Health centers, district hospitals, and regional hospitals serve as intermediaries between levels.
Tab. 1. Demographic profile of three African countries under investigation, 2008 [25],[26]. ![Demographic profile of three African countries under investigation, 2008 <em class="ref">[25]</em>,<em class="ref">[26]</em>.](https://www.prolekarniky.cz/media/cache/resolve/media_object_image_small/media/image/7133fb72a5b9d30cadc7dd13719e1a36.png)
Birth rate is the ratio of total live births to total population in a specified community or area over a specified period of time. The birth rate is often expressed as the number of live births per 1,000 of the population per year. In Tanzania we studied Bagamoyo and Kasulu District Hospitals. Bagamoyo is a district hospital about 60 km from the national referral hospital in Dar es Salaam. It serves a population of 230,000 people and has five satellite health centers. Kasulu, on the other hand, is situated about 1,500 km from Dar es Salaam, in the western Tanzania region of Kigoma. It serves a population of 600,000 people and has nine satellite health centers.
In Uganda, we studied Mityana, Kiryandongo, Iganga, and Buluba District Hospitals. Mityana, Iganga, and Kiryandongo hospitals are situated astride Ugandan highways, 72 km, 110 km, and 200 km, respectively, from the capital city of Kampala. They serve suburban and rural populations. The three hospitals are officially 100-bed hospitals with catchment populations of 250,000 (for Mityana), 125,000 (for Kiryandongo), and at least 500,000 (for Iganga). Buluba and Iganga serve the same region away from Kampala.
In Mozambique, we studied Chokwe and Catandica District Hospitals. Chokwe hospital is situated in the Gaza province 150 km northeast of the capital city of Maputo. The hospital, along with its nine satellite health centers, serves a district population of 250,000 people. Catandica is situated in the Manica province, approximately 1,000 km northwest of Maputo, abutting the mountainous border with Zimbabwe. Catandica hospital serves a catchment population of approximately 100,000 people and has ten satellite clinics. Although Chokwe is well connected to nearby towns and is located 90 km from its province capital city of Xai-Xai, Catandica is situated in a remote region off the unpaved main road, 200 km from its province capital of Chimoio. Both hospitals serve primarily rural populations.
Data Collection
Data were collected from country-level censuses, administrator interviews, hospital records, and administrative records using a standard survey instrument, categorized as: district demographics, hospital characteristics including inputs (staffing, cost, functioning and nonfunctioning beds, operating rooms, etc.), and outputs (aggregate and individuals data on admissions and procedures). District population data were gathered from the most recent census in each country. The number of other hospitals and health centers in the district was obtained from local hospital administrators.
Comprehensive hospital-level information about human resources was collected: number of doctors, surgeons, dentists, mid-level health providers (MLPs) including technicians, assistant medical officers, clinical officers), nurses (including the subcategories of nurse officers, nurses' assistants, enrolled nurses, nurse midwives, public health nurses), as well as administrative and support personnel. Data on other hospital inputs (e.g., functioning and nonfunctioning beds, operating rooms, hospital operating expenditures for 2006 and/or 2007) also came from central administration records and administrator interviews in each hospital. Where 2007 data were not available (i.e., in Uganda), 2006 data were used.
Data on admissions and procedures were collected from two sources. First, we collected aggregate hospital statistics for 2007 on annual admissions, deliveries, and major surgeries from existing hospital information systems (which produce monthly statistics). Second, we collected patient-level information, including age and sex. For five hospitals the patient-level data were collected for the target months of February, June, and October, whereas for Mityana, Buluba, and Iganga hospitals, data were collected for a full 12 mo. We reviewed ward-level patient records from medical, surgical, maternity, and pediatric wards to determine patient diagnosis, age, and gender at admission. We also reviewed operating room logs for surgical procedure details. To standardize data entry and case definition, all sites used the same list of most common procedures and diagnoses on the basis of a consensus panel of physicians in the respective countries. A category “other” was only possible if none of the listed choices were appropriate. When “other” data were collected, an open-ended description was required. Ethical clearance was not required as all data were de-identified data previously collected for administrative purposes.
Data Processing and Analysis
Aggregate hospital statistics on annual surgeries were used to describe the scope of surgical procedures. Ward-level patient records for the targeted months of February, June, and October were used to describe the age and gender distribution by type of procedure. We compared the percent distribution of each procedure obtained from the annual aggregate data to that of 3-mo individual ward-level data. Few discrepancies were observed for Mityana, Buluba, and Kiryandongo, where annual individual data were available. More information about specific discrepancies is presented in Table S1. All data were entered in Microsoft Excel at each of the sites and analyzed centrally using Excel and SPSS.
Results
Catchment populations ranged from about 99,000 to 628,000 people (Table 2). Admissions ranged from 3,861 to 16,999 and deliveries from 439 to 3,607. Facilities were staffed with one to six doctors and three to 26 mid-level health providers. The number of hospital beds per 1,000 population ranged from 0.2 to 1.
Tab. 2. Characteristics, outputs, and human resources for eight district hospitals in Tanzania, Mozambique, and Uganda, 2008. 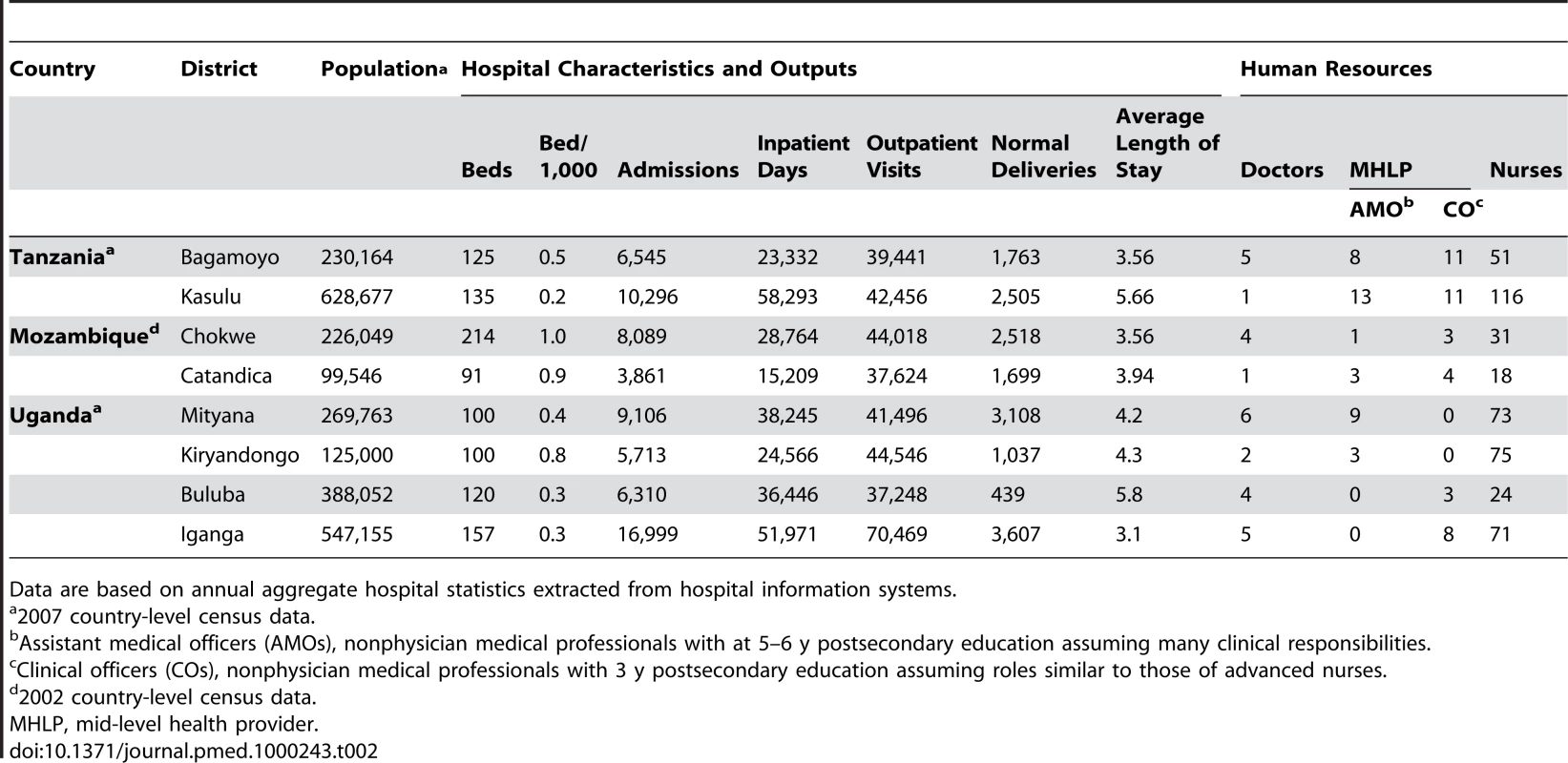
Data are based on annual aggregate hospital statistics extracted from hospital information systems. The annual aggregate number of surgical procedures performed per hospital is given in Table 3. With the exception of Kiryandongo, obstetric and nonobstetric procedures accounted for approximately 40%–60% of all procedures. In six of the eight hospitals, more than 60% of nonobstetrical procedures were major procedures.
Tab. 3. Breakdown of the annual number of surgeries performed at hospitals under investigation. 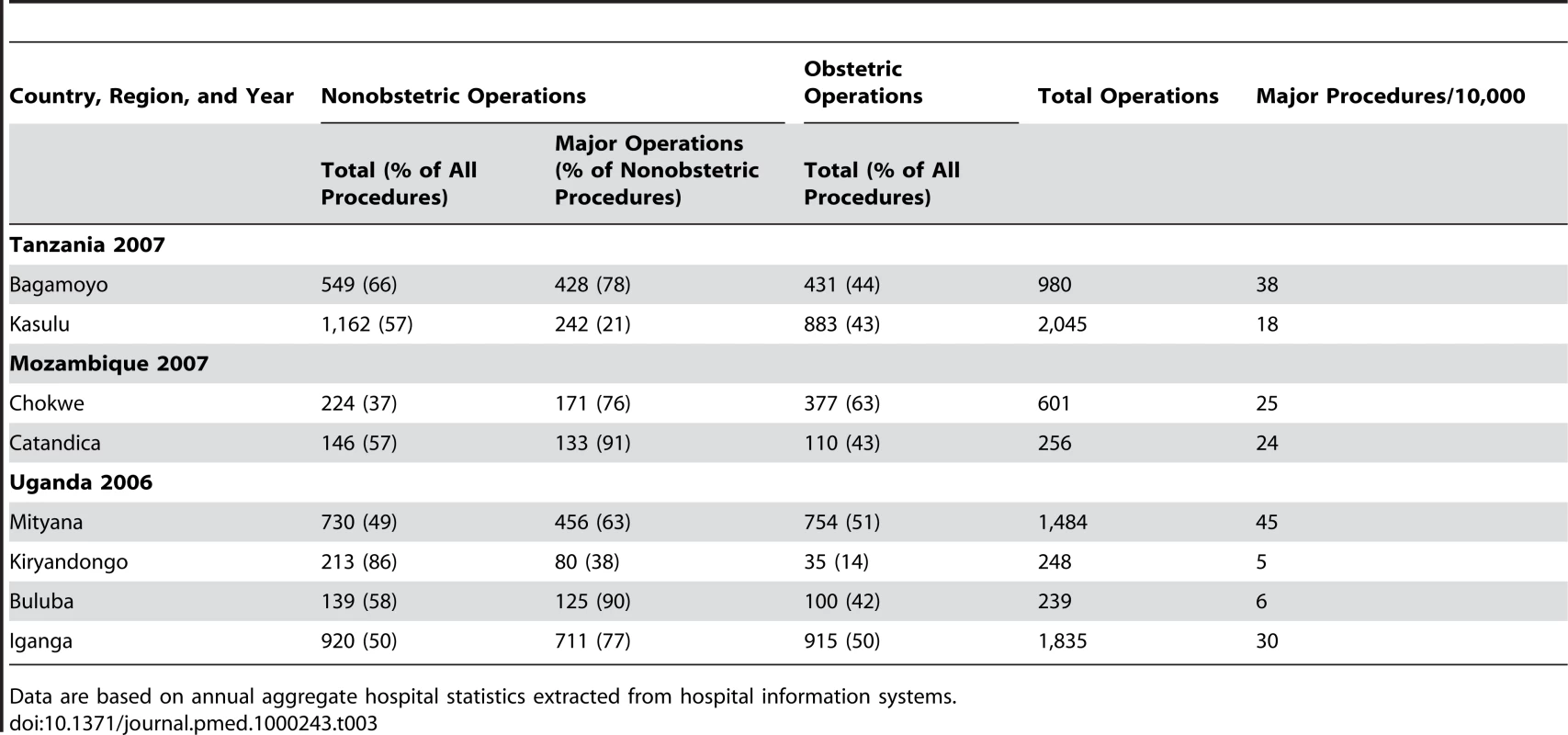
Data are based on annual aggregate hospital statistics extracted from hospital information systems. The total range of procedures when summed across all hospitals is displayed in Tables 4 and 5. Figure 1 shows the age distribution for persons receiving major, minor, and obstetric operations across all sites. Major surgery was performed across all age groups but occurred more frequently among patients aged 25 to 50 y with an average age of 40 y. Minor surgery was more common for patients under 50 y old with an average age of 24 y. The average age of patients on whom obstetric operations were performed was 26 y. Figures 1 and 2 show the age distribution for patients receiving major operations at each site, and the gender distribution for both major and minor surgeries. The differences in average ages reflect, in part, the differences in the proportions of procedures performed at each site (see Table S1).
Fig. 1. Age distribution of procedures by type of surgery across all hospitals under investigation. 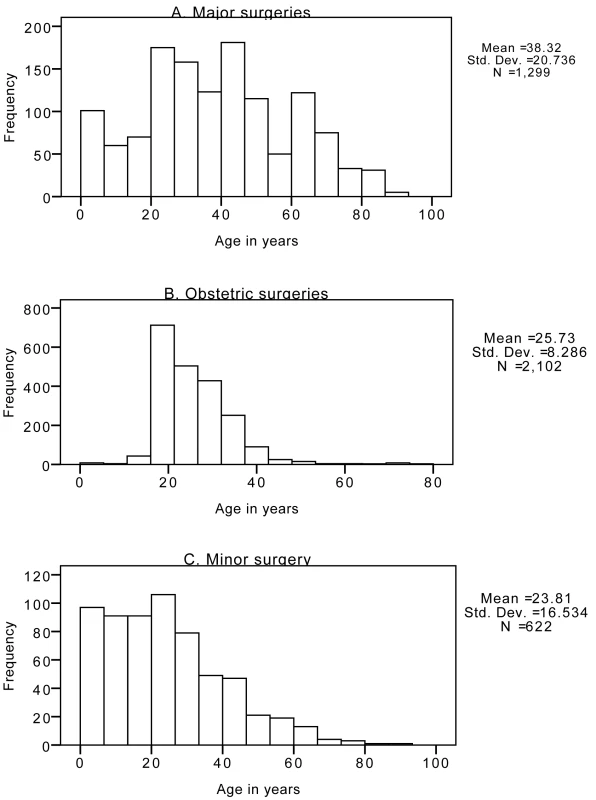
(A) Major surgeries; (B) obstetric surgeries; (C) minor surgery. Data are extracted from ward-level patient records for the targeted months of February, June, and October. Fig. 2. Type of surgery by patient sex. 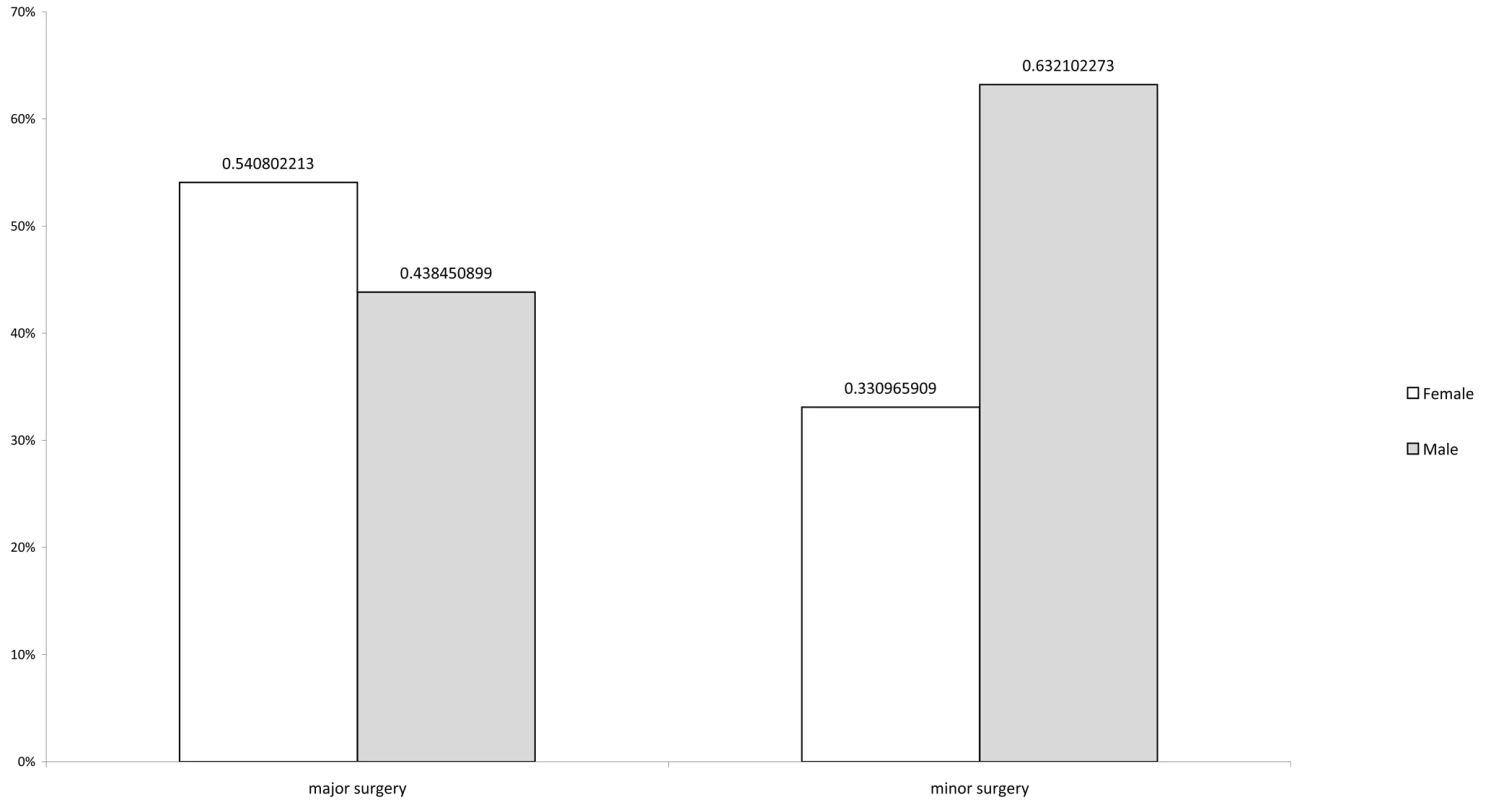
Data are extracted from ward-level patient records for the targeted months of February, June, and October; 100% of obstetric surgeries were performed in female patients; 71.9% of unspecified surgeries were in female patients versus 23.1% in males. The numbers do not add up to 100% because of missing data on sex of the patient. Tab. 4. Breakdown of major surgical procedures at hospitals under investigation. 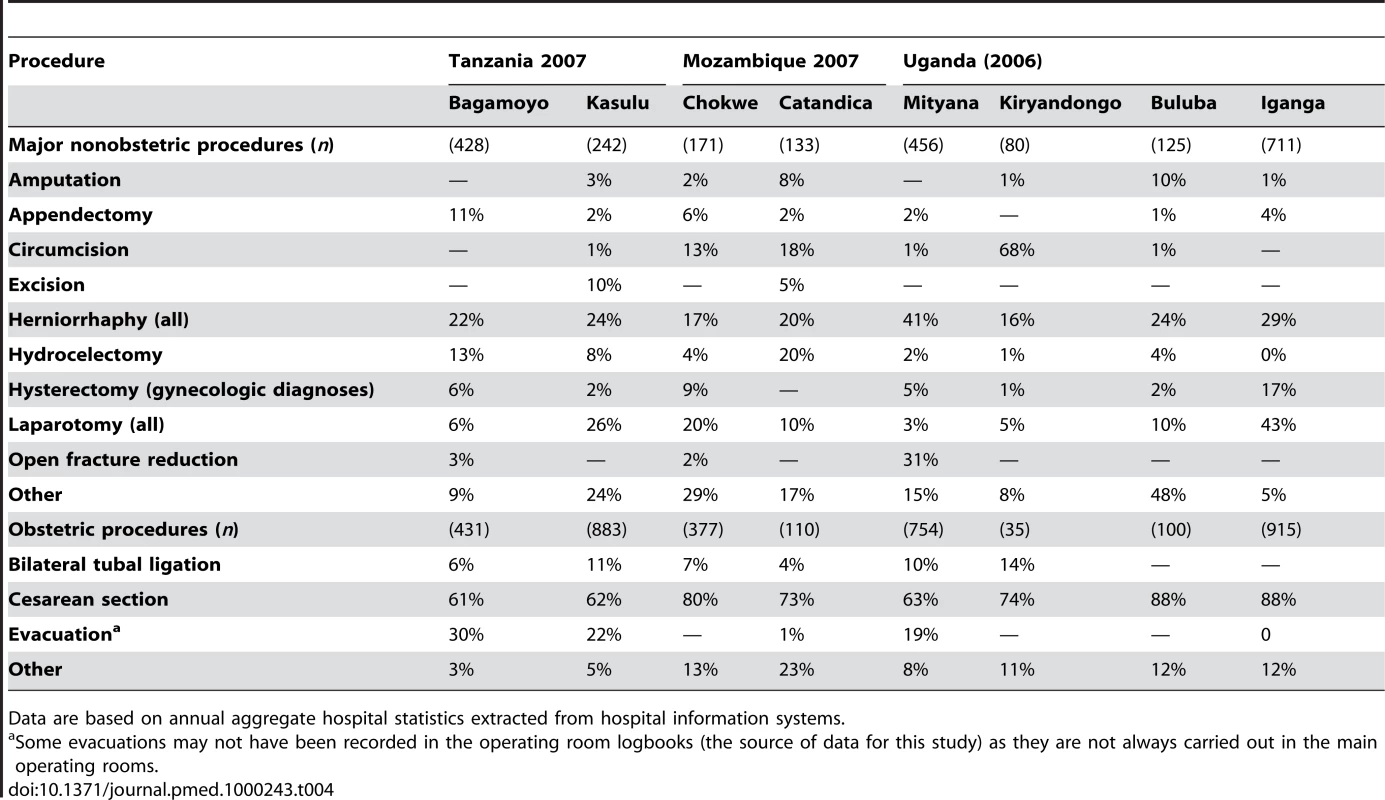
Data are based on annual aggregate hospital statistics extracted from hospital information systems. Tab. 5. Range of all procedures performed across all hospitals under investigation. 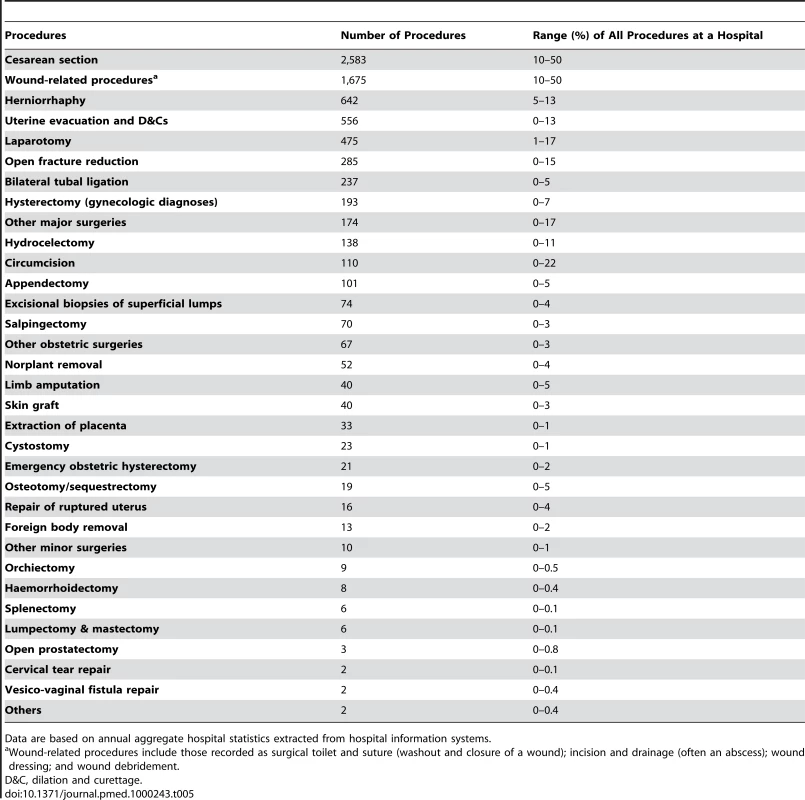
Data are based on annual aggregate hospital statistics extracted from hospital information systems. The median annual rate of major operations across the eight hospitals was 25/10,000 population (range 5–45) (Table 3). Table 6 shows that the range of cesarean sections per 1,000 deliveries in these hospitals was 25–223, whereas the range of cesarean sections/10,000 population was 1–17. Meanwhile, 0.5–7 hernia repairs were performed across the hospitals per 10,000 population. The population need for cesarean sections is debatable, but is estimated by the WHO to be 5%–15% of all deliveries [2]. Using a rate of 5% and a birth rate of 35/1,000 (estimated for Tanzania in Table 1), we calculated the annual need of cesarean sections for the catchment populations (given in Table 2) of Bagamoyo and Kasulu to be 400 and 1,100 cesarean sections, respectively. These calculations imply that the unmet need for cesarean section in Bagomoyo was 65%, whereas for Kasulu it was 47%.
Tab. 6. Annual rates of hernia operations and cesarean operations/10,000 population. 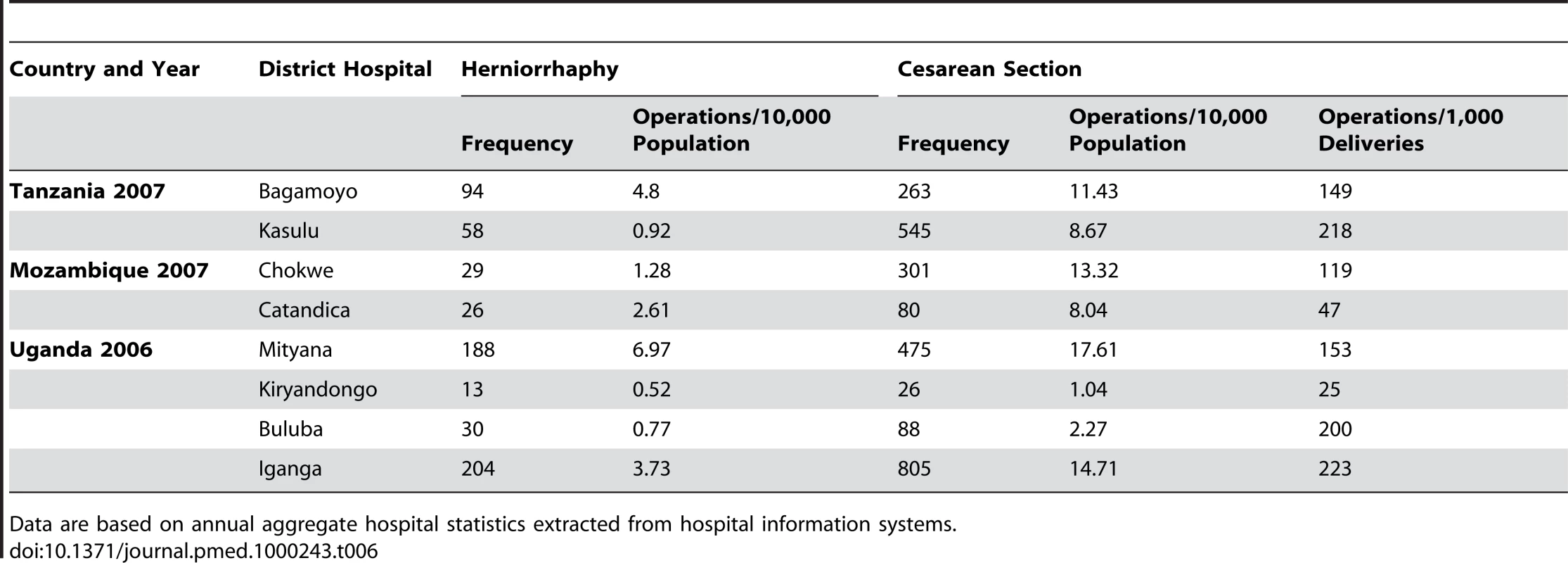
Data are based on annual aggregate hospital statistics extracted from hospital information systems. Discussion
We found relatively low rates of major surgery at district hospitals in East Africa, ranging from 50 to 450 surgical procedures per 100,000 population. Although lack of data on the population need for surgery precludes conclusions about the magnitude of unmet need, this confirms that there are barriers to access to essential surgery in at least some rural districts in Uganda, Tanzania, and Mozambique. This is reinforced by our finding that the majority of nonobstetric surgery was for emergency rather than elective conditions, suggesting that district residents do not receive surgical care for common surgical conditions (e.g., inguinal hernia repair) in local hospitals.
Global data also point to limited access to essential surgery in most low-income countries, with only 26% of 234 million estimated surgical procedures performed in poor and lower health expenditure countries that account for 70% of the world's population [4]. Nonetheless, very little is known about the incidence and prevalence of surgical conditions, even the number of basic surgical conditions such as hernia. Prior facility-based reports of surgical procedures in low-income countries have focused on individual institutions or countries, but there have not been cross-country comparisons using a common template [4]–[9]. In many of the sites investigated the number of public hospital district beds have remained the same for decades, while the population on average has doubled over the period [10]. This has meant, in effect, a decline in hospital beds per population over time.
At the first meeting of the BESG, participants drafted a list of the highest-priority surgical procedures that could be carried out at the level of the district hospital (first-level health facility) in Africa [11]. These procedures heavily overlap with the set of procedures defined by the World Health Organization [2]. These highest priority procedures primarily address health emergencies such as injuries and obstetric complications. A recent estimate suggests that injuries account for the greatest mortality and morbidity from surgical conditions in Africa (15 disability-adjusted life years [DALYs] lost per 1,000 population) [12]. At the same time prior work in similar settings has suggested that only one-third of injured patients reach a health facility [12].
Our data suggest but do not definitively confirm that the volume of surgical procedures to treat traumatic injury was relatively low in the study hospitals. For example, while some of the laparotomies performed were likely due to trauma, they were not clearly classified as such, and may have been performed for other causes of acute abdomen such as bowel obstruction or intestinal perforation. Open fracture reduction, which might also be considered a proxy for trauma when treated at a district hospital, was recorded at only two of the eight hospitals (Bagamoyo and Mityana). Similarly, there were no burns recorded and very few skin grafts, though burns in rural areas are a well-documented serious public health issue, especially in children [13]. Life-saving interventions such as airway management, tube thoracostomy for chest trauma, and resuscitation with intravenous fluids were not recorded, as the data do not include bedside and some accident and emergency procedures. The difficulties we encountered in obtaining data on trauma suggest the need for new data collection approaches. Trauma registries have been piloted in several countries in the region and other groups have called for greater facility-based and population-level surveillance of injuries to improve knowledge of trauma care [14]–[16]. The few existing population-based surveys of injuries have pointed to a high incidence of untreated injuries [12],[17].
In terms of obstetric surgery it is notable that cesarean section births, while still insufficient to meet the population need, far outnumbered instrumental deliveries (e.g., vacuum extraction), which were extremely rare in the study hospitals. This finding raises a concern for the quality of obstetric care as instrumental delivery poses lower risk to the mother and the fetus, particularly in the context of weak infection control practices and high rates of repeat childbearing for women [18]. There also appeared to be a gap in the provision of surgical family planning. No vasectomies were recorded across the study hospitals. The tubal ligation rate in the hospitals translates to 90 per million compared to 1,150 per million in the US [19]MLHP By reducing the rate of unwanted pregnancy, surgical and nonsurgical family planning methods can reduce the need for surgical interventions for birth complications [20]. Similarly very few cancer-related procedures were done in the study hospitals. It is unclear from these data if these limitations are due to a lack of capacity at the district hospital, to referral to higher-level facilities, or to low health-seeking behavior. There were no accessible records to establish what kinds of conditions were referred to higher-level hospitals over the study period. The same is true for other elective conditions known to be prevalent in the region such as vesico-vaginal fistula [21]. Another possibility discussed under limitations is that the data for these procedures were not captured in the operating room logs.
In seven of the eight studied hospitals the surgeries performed were evenly divided between obstetric and nonobstetric procedures. This finding is in contrast to a recent survey of 21 district hospitals in Malawi that found considerably more obstetric procedures followed by surgical toilet and suture and fracture manipulation [9]. In our study, wound-related procedures were the second most commonly performed operation after cesarean sections, followed by herniorrhaphies. While the ratio of cesarean sections to laparotomies was 13∶1 in the Malawi study, it was 5∶1 in our study. More laparotomies were performed in central hospitals in Malawi, perhaps reflecting different patterns of practice and referral.
All of the figures on surgical provision should be interpreted in the context of the population need for surgery. However, while it is possible to estimate unmet need for emergency obstetric care (see Results section), it remains difficult to estimate the expected need for general surgery in sub-Saharan Africa. For one, we have limited information on the population served by each hospital and there may be other facilities that provide services or patients may travel to other hospitals. In the absence of estimates of unmet need, we compared our findings with surgical rates per population obtained in other countries. We found that surgical rates/catchment population in this study (60–450/100,000) were comparable to prior estimates in the region (263/100,000 in Kenya; 166/100,000 in Uganda; 369/100,000 in Malawi) [4]–[9].
Kiryandongo hospital in northern Uganda was an outlier with very low surgical output. According to on-site interviews the hospital had deficits in staffing of essential cadres for surgical services such anesthetic and medical officers. In addition, the population in the catchment area includes several large camps of refuges from Southern Sudan and a native Ugandan population, some of whom seek care in another regional hospital where a different local dialect is spoken.
The age distribution from these data, especially for major procedures, indicates that the young productive workforce receives the majority of surgeries (Table 1). There are few procedures recorded in the pediatric age group. This finding may suggest a significant unmet need for pediatric surgery given that up to half the population is less than 15 y of age in many of these countries, and that children are more prone to injuries and congenital anomalies. One study estimated that up to 85% of children living in an urban areas of the Gambia are likely to need a surgical procedure by age 15 y, generally minor surgery [3].
Most of the recorded procedures were for emergency surgical conditions, suggesting significant potential mortality and morbidity averted through the provision of surgical care. However, this finding leads to the question of why numbers of elective procedures were low. The one exception is hernia surgery, which was relatively common. Again, it is not known how many of the herniorrhaphies performed were for strangulated hernia, an emergency condition, as this was not recorded in all hospitals. Whether patients with less acute surgical conditions do not seek care at all or are referred to higher-level facilities requires further investigation.
The limitations of this study include the usual limitations of using retrospective hospital records, for example the low number of minor operations observed may be because they were recorded as outpatient procedures not in the theatre logbooks. This practice may account for the absence of evacuations of remnants of pregnancy in the records as these may have been treated outside the theatre. In addition our study lacked information on outcomes of operations. The limited evidence available suggests that perioperative morbidity and mortality from procedures are significant in these settings and makes the case that anesthesia services and safety measures must also be stressed [22]–[24]. In addition, accurate estimates of patient referrals to higher-level facilities for conditions that exceeded the capacity of the district hospitals could not be assessed through this study. This absence may result in overestimates of unmet need as these estimates were made assuming that all cesarean sections required in the district population were done at the index hospitals. The estimate of unmet need for cesarean sections may have been inflated by some operations that were performed for convenience rather than need. Also, there may have been misclassification of operations as there is no standardized way that operations are recorded. For example, “surgical toilet” could mean a major complicated dirty wound or a simple laceration. This misclassification could be addressed by future prospective facility-based data collection. Finally, the age and gender distribution of the surgeries should be interpreted in light of the discrepancies observed between the 12-mo aggregate data and the 3-mo individual data used to estimate patient demographics.
Although the scope of surgical procedures done in these first-level referral facilities in Tanzania, Mozambique, and Uganda is narrow, emergency and essential procedures were the primary procedures performed. This study did not formally assess deficiencies in infrastructure and equipment, but qualitative interviews and the experience of the authors confirm that these procedures are performed under very challenging circumstances. Many procedures designated as high priority by the World Health Organization and other groups are performed in low volume or not at all. In particular, there is a low volume of essential trauma care such as fracture management, and of management of procedures for cancer, and for vesico-vaginal fistula repair.
This study suggests the need for urgent new research into the provision of essential surgery at the district level. Our results are limited as they are based on retrospectively collected data but are useful in pointing to the need for carefully designed prospective studies. The unmet need for surgical care could be estimated by population-based surveys and measurement of surgical need should be included in such surveys. Outcomes of care and referral patterns could be better assessed by prospective studies of first - and referral-level facilities. The district hospital is well positioned in the health service delivery hierarchy to integrate surgery and primary health care. The surgical capacity of the district hospital therefore must be strengthened to avert morbidity and mortality from surgical conditions. Greater emphasis must be paid to the role of surgical care in the global health research agenda and in plans to improve health care for vulnerable rural populations in sub-Saharan Africa.
Supporting Information
Zdroje
1. BicklerSW
SpiegelDA
2008 Global surgery–defining a research agenda. Lancet 372 90 92
2. LubogaS
MacfarlaneSB
von SchreebJ
KrukME
CherianMN
2009 Increasing access to surgical services in sub-saharan Africa: priorities for national and international agencies recommended by the Bellagio Essential Surgery Group. PLoS Med 6 e1000200 doi:10.1371/journal.pmed.1000200
3. BicklerSW
TelferML
Sanno-DuandaB
2003 Need for paediatric surgery care in an urban area of The Gambia. Trop Doct 33 91 94
4. WeiserTG
RegenbogenSE
ThompsonKD
HaynesAB
LipsitzSR
2008 An estimation of the global volume of surgery: a modelling strategy based on available data. Lancet 372 139 144
5. NabembeziJS
NordbergE
2001 Surgical output in Kibaale district, Uganda. East Afr Med J 78 379 381
6. NordbergE
MwobobiaI
MuniuE
2002 Major and minor surgery output at district level in Kenya: review and issues in need of further research. Afr J Health Sci 9 17 25
7. NordbergEM
1984 Incidence and estimated need of caesarean section, inguinal hernia repair, and operation for strangulated hernia in rural Africa. Br Med J (Clin Res Ed) 289 92 93
8. BlanchardRJ
BlanchardME
ToussignantP
AhmedM
SmytheCM
1987 The epidemiology and spectrum of surgical care in district hospitals of Pakistan. Am J Public Health 77 1439 1445
9. LavyC
TindallA
SteinlechnerC
MkandawireN
ChimangeniS
2007 Surgery in Malawi - a national survey of activity in rural and urban hospitals. Ann R Coll Surg Engl 89 722 724
10. OzgedizD
GalukandeM
MabweijanoJ
KijjambuS
MijumbiC
2008 The neglect of the global surgical workforce: experience and evidence from Uganda. World J Surg 32 1208 1215
11. Ouro-Bang'na MamanAF
KaboreRA
ZoumenouE
GnassingbeK
ChobliM
2009 Anesthesia for children in Sub-Saharan Africa–a description of settings, common presenting conditions, techniques and outcomes. Paediatr Anaesth 19 5 11
12. MockCN
nii-Amon-KoteiD
MaierRV
1997 Low utilization of formal medical services by injured persons in a developing nation: health service data underestimate the importance of trauma. J Trauma 42 504 511; discussion 511–503
13. Justin-TemuM
RimoyG
PremjiZ
MatemuG
2008 Causes, magnitude and management of burns in under-fives in district hospitals in Dar es Salaam, Tanzania. East Afr J Public Health 5 38 42
14. TayeM
MunieT
2003 Trauma registry in Tikur Anbessa Hospital, Addis Ababa, Ethiopia. Ethiop Med J 41 221 226
15. KobusingyeOC
LettRR
2000 Hospital-based trauma registries in Uganda. J Trauma 48 498 502
16. MockC
LormandJ
GoosenJ
JoshipuraM
PedenM
2004 Guidelines for essential trauma care. Geneva World Health Organization
17. KobusingyeO
GuwatuddeD
LettR
2001 Injury patterns in rural and urban Uganda. Inj Prev 7 46 50
18. HofmeyrGJ
2004 Obstructed labor: using better technologies to reduce mortality. Int J Gynaecol Obstet 85 S62 S72
19. PetersonHB
2008 Sterilization. Obstet Gynecol 111 189 203
20. ClelandJ
BernsteinS
EzehA
FaundesA
GlasierA
2006 Family planning: the unfinished agenda. Lancet 368 1810 1827
21. WallLL
2006 Obstetric vesicovaginal fistula as an international public-health problem. Lancet 368 1201 1209
22. FentonPM
WhittyCJ
ReynoldsF
2003 Caesarean section in Malawi: prospective study of early maternal and perinatal mortality. BMJ 327 587
23. WalkerIA
MortonNS
2009 Pediatric healthcare–the role for anesthesia and critical care services in the developing world. Paediatr Anaesth 19 1 4
24. HaynesAB
WeiserTG
BerryWR
LipsitzSR
BreizatAH
2009 A surgical safety checklist to reduce morbidity and mortality in a global population. N Engl J Med 360 491 499
25. US Central Intelligence Agency (CIA) 2008 The World Factbook online. Washington (D.C) CIA Available: https://www.cia.gov/library/publications/the-world-factbook/
26. WHO 2008 World Health Organization Statistical Information System: Core Health Indicators. Available: http://www3.who.int/whosis/core/core_select_process.cfm
Štítky
Interní lékařství
Článek vyšel v časopisePLOS Medicine
Nejčtenější tento týden
2010 Číslo 3- Berberin: přírodní hypolipidemikum se slibnými výsledky
- Příznivý vliv Armolipidu Plus na hladinu cholesterolu a zánětlivé parametry u pacientů s chronickým subklinickým zánětem
- Červená fermentovaná rýže účinně snižuje hladinu LDL cholesterolu jako vhodná alternativa ke statinové terapii
- Léčba bolesti u seniorů
- Jak postupovat při výběru betablokátoru − doporučení z kardiologické praxe
-
Všechny články tohoto čísla
- CONSORT 2010 Statement: Updated Guidelines for Reporting Parallel Group Randomised Trials
- BMI and Risk of Serious Upper Body Injury Following Motor Vehicle Crashes: Concordance of Real-World and Computer-Simulated Observations
- Preventing Road Deaths—Time for Data
- Essential Surgery at the District Hospital: A Retrospective Descriptive Analysis in Three African Countries
- Drivers of Inequality in Millennium Development Goal Progress: A Statistical Analysis
- Where Will the Next Generation of Stroke Treatments Come From?
- Unravelling the Genetics of Ischaemic Stroke
- Chronic Obstructive Pulmonary Disease: Effects beyond the Lungs
- The Promise of Prevention: The Effects of Four Preventable Risk Factors on National Life Expectancy and Life Expectancy Disparities by Race and County in the United States
- Can Animal Models of Disease Reliably Inform Human Studies?
- New Approaches to Preventing, Diagnosing, and Treating Neonatal Sepsis
- Protecting Vulnerable Road Users from Injury
- Providing Alcohol-Related Screening and Brief Interventions to Adolescents through Health Care Systems: Obstacles and Solutions
- Effects on Coronary Heart Disease of Increasing Polyunsaturated Fat in Place of Saturated Fat: A Systematic Review and Meta-Analysis of Randomized Controlled Trials
- Accelerating Policy Decisions to Adopt Type b Vaccine: A Global, Multivariable Analysis
- Human Resource and Funding Constraints for Essential Surgery in District Hospitals in Africa: A Retrospective Cross-Sectional Survey
- PLOS Medicine
- Archiv čísel
- Aktuální číslo
- Informace o časopisu
Nejčtenější v tomto čísle- BMI and Risk of Serious Upper Body Injury Following Motor Vehicle Crashes: Concordance of Real-World and Computer-Simulated Observations
- Unravelling the Genetics of Ischaemic Stroke
- Providing Alcohol-Related Screening and Brief Interventions to Adolescents through Health Care Systems: Obstacles and Solutions
- Human Resource and Funding Constraints for Essential Surgery in District Hospitals in Africa: A Retrospective Cross-Sectional Survey
Kurzy
Zvyšte si kvalifikaci online z pohodlí domova
Současné možnosti léčby obezity
nový kurzAutoři: MUDr. Martin Hrubý
Všechny kurzyPřihlášení#ADS_BOTTOM_SCRIPTS#Zapomenuté hesloZadejte e-mailovou adresu, se kterou jste vytvářel(a) účet, budou Vám na ni zaslány informace k nastavení nového hesla.
- Vzdělávání



