-
Články
Top novinky
Reklama- Vzdělávání
- Časopisy
Top články
Nové číslo
- Témata
Top novinky
Reklama- Videa
- Podcasty
Nové podcasty
Reklama- Kariéra
Doporučené pozice
Reklama- Praxe
Top novinky
ReklamaA 50-Year-Old Woman with Recurrent Generalised Seizures
article has not abstract
Published in the journal: . PLoS Med 5(9): e186. doi:10.1371/journal.pmed.0050186
Category: Learning Forum
doi: https://doi.org/10.1371/journal.pmed.0050186Summary
article has not abstract
Description of Case
50-year-old woman presented in May 2006 with recurrent generalised convulsions. She had a history of hypertension treated with indapamide, but was otherwise well. Her older sister and mother were known to have thyroid disease. She did not have any history of chronic alcohol use nor any recent history of head injury. The patient had never lived outside of Hong Kong. Prior to admission, she was taken to her general practitioner by her family for gradual onset of decreased alertness, cognitive decline, and reduced verbal communication, which worsened over the course of one week. She was found to have hypothyroidism with TSH (thyroid stimulating hormone) 52.3 mIU/l (normal range 0.47–4.68 mIU/l) and free T4 4.2 pmol/l (normal range 10.0–28.2 pmol/l), and was started on thyroxine replacement. Four days later, she developed two generalised seizures within three days and was admitted into hospital. She was afebrile and had no focal neurological signs on examination. Baseline investigations, including electrolytes, liver function tests, calcium, and phosphate, were normal. Random plasma glucose was 5.7 mmol/l. Magnetic resonance imaging (MRI) of brain was unremarkable. She was subsequently transferred to our hospital for further management.
On admission, she was afebrile and had a series of seizures over a period of five hours without regaining full consciousness in between seizures. The patient was given intravenous diazepam and phenytoin, and was intubated and transferred to the intensive care unit.
What Was Our Differential Diagnosis at This Stage?
The patient presented with several days' history of decreased consciousness, followed by acute symptomatic seizures. The differential diagnosis of someone with a subacute encephalopathy is wide, and possible causes are listed in Box 1. These include metabolic derangements such as hyponatraemia, as well as infections, central nervous system (CNS) disorders, drugs and toxins, systemic conditions such as hepatic encephalopathy, and psychiatric conditions. The patient was at risk of hyponatraemia in view of her use of indapamide, but her serum electrolytes were normal. She was afebrile and had no neck stiffness, though CNS infection would still need to be excluded. There was no known history of neurological or psychiatric conditions, though this would not preclude her from suffering from such conditions. Although there was no easily identifiable drug or toxic cause, these remained distinct possibilities and a toxicology screen was indicated.
Box 1. Common Causes of Subacute Encephalopathy
-
A. Metabolic derangements
Electrolyte disturbances
Hyponatraemia or hypernatraemia
Hypocalcaemia or hypercalcaemia
Hypomagnesaemia or hypermagnesaemia
Hypophosphataemia or hyperphosphataemia
Endocrine disturbances
Hypothyroidism (rarely thyrotoxicosis)
Hyperparathyroidism or hypoparathyroidism
Insulinoma
Pituitary insufficiency
Adrenal insufficiency or Cushing's syndrome
Hypoxia
Hyperglycaemia or hypoglycaemia
Carbon dioxide
Inborn errors of metabolism
Porphyria
Wilson disease
Nutritional deficiencies
Vitamin B12 deficiency
Wernicke encephalopathy
-
B. Infections
Sepsis
Systemic infections
CNS infections (see below)
-
C. Neurological
CNS infections
Encephalitis
Meningitis
Brain abscess
Epilepsy
Complex partial seizures
Non-convulsive status epilepticus
Head injury
Hypertensive encephalopathy
Carcinomatous meningitis
Paraneoplastic encephalitis
Limbic encephalitis associated with anti voltage gated potassium channel antibodies
-
D. Drugs
Alcohol-related
Alcohol intoxication
Alcohol withdrawal
Recreational drugs
Narcotics
Cocaine
Lysergic acid diethylamide (LSD)
3,4-methylenedioxymethamphetamine (MDMA, ecstasy)
Phencyclidine
Ketamine
Poisons
Methanol
Ethylene glycol
Insecticides
Carbon monoxide poisoning
Prescription medications
-
E. Systemic conditions
Hepatic encephalopathy
Respiratory failure
Renal failure
Severe burns
Hyperthermia or hypothermia
-
F. Psychiatric disease
What Was the Most Likely Diagnosis?
Although the patient had been diagnosed with hypothyroidism shortly prior to her presentation, the abnormal thyroid function tests could not fully explain her neurological state. Repeat serum electrolytes, liver function tests, and calcium and magnesium levels were all normal. Repeat TSH was 11 mIU/l. Computed tomography (CT) of the brain on admission was normal. A lumbar puncture was performed, which showed raised cerebrospinal fluid (CSF) protein 1.5 g/l. The paired CSF–plasma glucose levels were 7.0 mmol/l and 7.1 mmol/l. The CSF cell count, microscopy, and Ziehl-Neelson stain were all normal. The opening pressure was 13 cmH20. Polymerase chain reaction of the CSF was later found to be negative for herpes simplex, enterovirus, and varicella zoster virus DNA. Toxicology screen was negative. Her clinical seizures persisted, and intravenous infusion of propofol/thiopentone was commenced. Over the subsequent four days, upon withdrawal of propofol and thiopental, the patient still demonstrated altered mental state. The electroencephalogram (EEG) monitoring showed repetitive focal spikes or sharps of less than three per second, which may be abolished by combination anti-epileptic therapy with phenytoin and sodium valproate, pointing towards non-convulsive status epilepticus (Figures 1 and 2).
Fig. 1. Electroencephalogram Showing Repetitive Focal Spikes or Sharps Less Than Three per Second 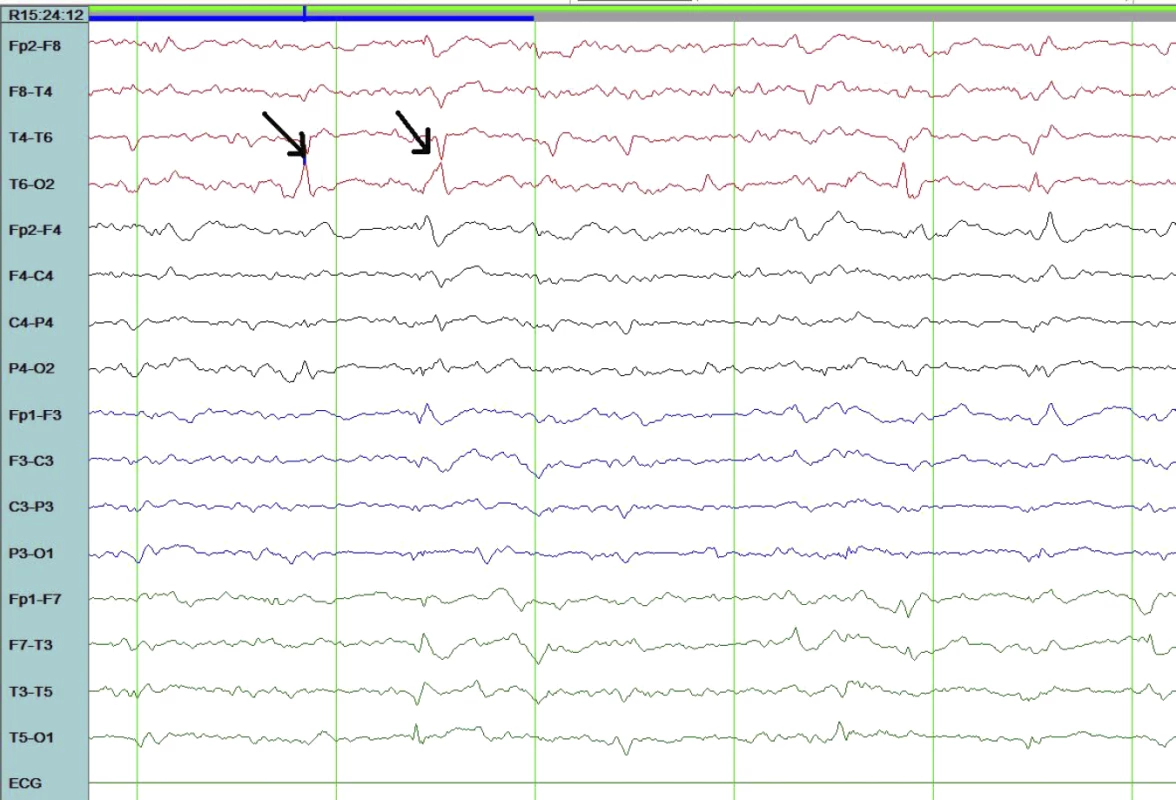
Fig. 2. Electroencephalogram after Combination Anti-Epileptic Therapy with the Focal Spikes Abolished 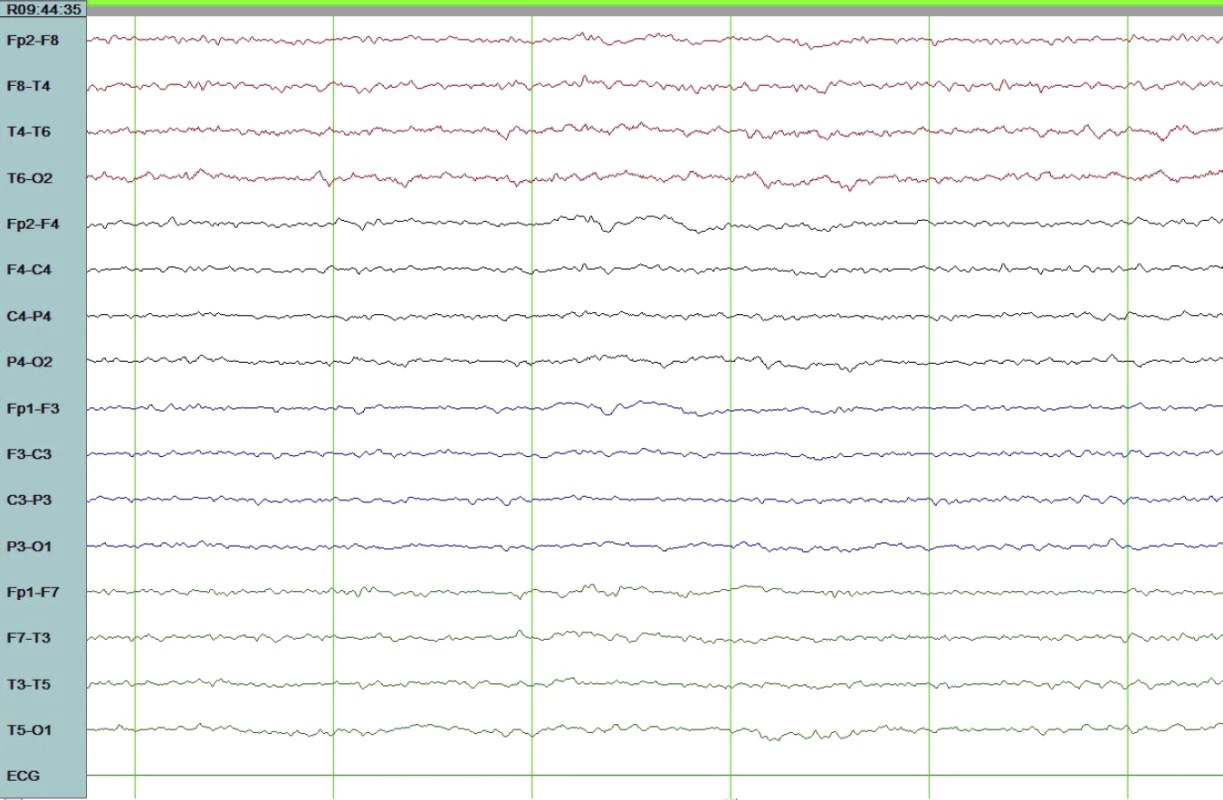
Ten days after successful treatment, occasional interictal discharges within a normal background were observed. Some conditions associated with multiple seizures are listed in Box 2. Structural brain lesions were not likely in our case, given the initial normal MRI imaging. Nevertheless, repeat imaging was warranted if the patient's condition continued to deteriorate. Repeat CT brain performed three days after admission was normal. Results of our investigations did not support metabolic or toxic causes. Sporadic Creutzfeldt-Jakob disease (CJD) can present with a similar clinical picture including dementia, myoclonus, ataxia, personality change, psychotic phenomenon, or even recurrent seizures [1,2]. However, the EEG of our patient did not reveal the periodic sharp wave complexes typical of CJD. Detection of the 14-3-3 protein in the CSF would also support a diagnosis of CJD, though this test was not available in our hospital. Once infectious causes were excluded, other causes of a subacute encephalopathy, such as an autoimmune or inflammatory process, including paraneoplastic encephalitis, need to be considered.
Box 2. Causes of Acute Symptomatic Seizures with Multiple Seizures upon Presentation
-
A. Withdrawal of benzodiazepines, barbiturates, alcohol
-
B. Acute structural injury
a. Tumour or cerebral metastases
b. Encephalitis/meningitis
c. Brain abscess
d. Stroke
e. Head injury
f. Subarachnoid haemorrhage/intra-cerebral haemorrhage/subdural haematoma
g. Cerebral hypoxia
h. Cerebral arteriovenous malformations
i. Posterior reversible encephalopathy syndrome
j. Systemic lupus erythematosus
k. Sagittal sinus thrombosis
-
C. Metabolic disturbances
a. Hypoglycaemia
b. Hyponatraemia
c. Hypocalcaemia
d. Hypomagnesaemia
e. Hepatic encephalopathy
f. Uraemia
g. Hashimoto encephalopathy
-
D. Drugs (particularly overdose) and other toxins
a. Theophylline
b. Ciprofloxacin
c. Tricyclic antidepressants
d. Lithium
e. Flumazenil
f. Cyclosporine
g. Lidocaine
h. Metronidazole
What Tests Would Now Be Helpful?
As there was no other organic pathology to explain her recurrent seizures and subacute encephalopathy, a diagnosis of Hashimoto encephalopathy was considered in view of the recent diagnosis of hypothyroidism. Anti-microsomal and anti-thyroglobulin antibodies titres were 1 in 25,600 and 1 in 400 respectively, supporting a diagnosis of autoimmune thyroid disease. Anti-nuclear antibodies, anti-DNA, anti-extractable nuclear antigen, and anti-cardiolipin antibodies were all negative. The patient's erythrocyte sedimentation rate and C-reactive protein were mildly elevated at 41 mm/h (normal <20 mm/h) and 39.5 mg/l (normal <9.9 mg/l), respectively, with complement C3 of 0.84 g/l (normal range 0.62–1.87 g/l) and C4 of 0.18 g/l (normal range 0.20–0.59 g/l).
What Was the Next Step in Her Management?
The patient was started on a trial of intravenous hydrocortisone 400 mg/day. Her neurological condition gradually stabilised, and a repeat EEG ten days after admission showed normal background with occasional interictal activities consisting of frontal predominant sharpish discharges. She was eventually taken off glucocorticoids after 18 days. The patient was fully orientated and able to walk unaided when discharged from hospital five weeks after admission, on maintenance phenytoin and valproate.
Progress
Six months after discharge, her anti-microsomal antibodies titre was reduced to 1 in 6,400, and anti-thyroglobulin antibodies were undetectable. She remained seizure-free six months after discharge, and the anti-convulsants were gradually tapered off. When last seen in January 2008, she was well and biochemically euthyroid on thyroxine 0.1 mg daily and had not had any further seizures. She gave written consent for this case to be published.
Discussion
Hashimoto Encephalopathy
The association of Hashimoto disease with an encephalopathy was first described by Lord Brain in 1966 [3]. Hashimoto encephalopathy (HE) is characterised by an encephalopathy with acute or subacute onset, accompanied by seizures, tremor, myoclonus, ataxia, psychosis, or stroke-like episodes, with a relapsing/remitting or progressive course. The prevalence is estimated to be 2.1 per 100,000 [4], although the condition is often under-recognised. Women are more commonly affected than men. In a recent series, the mean age at onset was 56 years, with the most frequent presenting features being tremor, transient aphasia, myoclonus, gait ataxia, cognitive impairment, seizures, and sleep abnormalities. Misdiagnosis at presentation was common, with most cases misdiagnosed as viral encephalitis, Creutzfeldt-Jakob disease, dementia, or psychiatric disorders [5]. Recurrent seizures are a recognised presentation of this condition [6]. Other causes of acute symptomatic seizures with multiple seizures upon presentation are listed in Box 2.
Making the Correct Diagnosis
The diagnosis of HE is based on presence of elevated antithyroid antibodies in patients with a compatible clinical presentation and exclusion of other causes of encephalopathy or acute confusional state (Box 1). Diagnosis requires presence of high titres of anti-thyroid peroxidase and/or anti-thyroglobulin antibodies, although this is not specific and there is no clear correlation between antibody titres and the severity of neurological symptoms [7]. The presence of anti-thyroid antibodies can sometimes be detected in normal individuals, though usually at lower titres. In some cases, presence of anti-neuronal antibodies has been noted [8]. Most patients have overt or subclinical hypothyroidism at the time of presentation, but can also be euthyroid at the time of diagnosis. Erythrocyte sedimentation rate and C-reactive protein are elevated in some patients [5]. In some aspects, Hashimoto encephalopathy resembles a heterogenous group of conditions, including Sjögren syndrome and systemic lupus erythematosus-associated meningoencephalitis, which are characterised by the association with underlying autoimmune conditions as well as the unifying feature of steroid responsiveness [5,9].
CSF analysis is abnormal in around 80% of cases of HE, often with elevated protein concentrations, and less often, a lymphocytic pleocytosis [7]. MRI is usually normal. Non-specific EEG abnormalities are often seen in the absence of seizures, with slowing of background activity that correlates with the clinical severity of the underlying encephalopathy. Other EEG findings reported include triphasic waves, epileptiform abnormalities, photomyogenic response, and photoparoxysmal response. The EEG abnormalities often paralleled the clinical course, showing improvement with the clinical condition. In one series, myoclonic jerks were recorded during the EEG study of about half the patients [10]. Patients with sporadic CJD may have clinical features identical to that of Hashimoto encephalopathy, when steroid responsiveness may be the only differentiating feature [1,9]. In addition, diffusion-weighted MRI imaging may also help differentiate between the two conditions, with hyper-intense abnormalities involving cortex and deep gray matter being highly sensitive and specific for sporadic CJD.
Treatment Approach
In addition to supportive measures, use of high-dose glucocorticoids is usually associated with marked clinical improvement, as well as improvement in EEG findings. In a review of 85 cases, the majority of patients who received glucocorticoids improved with treatment [11]. In some cases, additional short courses of glucocorticoids or other immunomodulatory therapy may be required to treat relapses [5]. In more severe cases, intravenous immunoglobulins and plasmapheresis may also be helpful [12]. Treatment of seizures with anti-convulsant medications may be necessary as a temporary measure, though in some cases seizures do not respond to anti-epileptic drugs but may respond to steroid therapy. Thus, considering HE in the differential diagnosis is of paramount importance. Whilst thyroid hormone replacement is indicated in patients with biochemical evidence of overt hypothyroidism, there is no correlation between neurological improvement and thyroxine replacement. The treatment of subclinical hypothyroidism, on the other hand, remains controversial [13].
As illustrated by our case, recognition of this form of autoimmune encephalopathy and its varied presentation is important, as it is readily treatable. Presence of a personal or family history of thyroid disorder should alert clinicians to the possibility of Hashimoto encephalopathy in patients with an otherwise unexplained subacute encephalopathy. Measurements of thyroid function and thyroid antibodies will be helpful in this setting.
Key Learning Points
Autoimmune thyroid disease may be associated with an encephalopathy (HE) with acute or subacute onset, accompanied by seizures, tremor, myoclonus, ataxia, psychosis, or stroke-like episodes, with a relapsing/remitting or progressive course.
A diagnosis of HE should be considered in patients with unexplained delirium, encephalopathy, or seizures. The diagnosis is based on exclusion of other causes of delirium, and is supported by the finding of elevated titres of anti-thyroid antibodies.
Other autoimmune conditions such as Sjögren syndrome and systemic lupus erythematosus may also be associated with a steroid-responsive meningoencephalitis and a similar clinical presentation to HE.
Treatment is supportive, though use of intravenous glucocorticoids is associated with improvement in neurological features as well as EEG abnormalities.
Thyroid hormone replacement is indicated in patients with biochemical evidence of overt hypothyroidism, though there is no correlation between neurological improvement and thyroxine replacement.
Zdroje
1. SeipeltMZerrINauRMollenhauerBKroppS
1999
Hashimoto's encephalitis as a differential diagnosis of Creutzfeldt-Jakob disease.
J Neurol Neurosurg Psychiatry
66
172
176
2. ReesJHSmithSJKullmannDMHirschNPHowardRS
1999
Creutzfeldt-Jakob disease presenting as complex partial status epilepticus: A report of two cases.
J Neurol Neurosurg Psychiatry
66
406
407
3. BrainLJellinekEHBallK
1966
Hashimoto's disease and encephalopathy.
Lancet
2
512
514
4. FerracciFBertiatoGMorettoG
2004
Hashimoto's encephalopathy: Epidemiologic data and pathogenetic considerations.
J Neurol Sci
217
165
168
5. CastilloPWoodruffBCaselliRVerninoSLucchinettiC
2006
Steroid-responsive encephalopathy associated with autoimmune thyroiditis.
Arch Neurol
63
197
202
6. FerlazzoERaffaeleMMazzuIPisaniF
2006
Recurrent status epilepticus as the main feature of Hashimoto's encephalopathy.
Epilepsy Behav
8
328
330
7. Kothbauer-MargreiterISturzeneggerMKomorJBaumgartnerRHessCW
1996
Encephalopathy associated with Hashimoto thyroiditis: Diagnosis and treatment.
J Neurol
243
585
593
8. OideTTokudaTYazakiMWataraiMMitsuhashiS
2004
Anti-neuronal autoantibody in Hashimoto's encephalopathy: Neuropathological, immunohistochemical, and biochemical analysis of two patients.
J Neurol Sci
217
7
12
9. ChongJYRowlandLP
2006
What's in a NAIM? Hashimoto encephalopathy, steroid-responsive encephalopathy associated with autoimmune thyroiditis, or nonvasculitic autoimmune meningoencephalitis.
Arch Neurol
63
175
176
10. SchaubleBCastilloPRBoeveBFWestmorelandBF
2003
EEG findings in steroid-responsive encephalopathy associated with autoimmune thyroiditis.
Clin Neurophysiol
114
32
37
11. ChongJYRowlandLPUtigerRD
2003
Hashimoto encephalopathy: Syndrome or myth.
Arch Neurol
60
164
171
12. MocellinRWalterfangMVelakoulisD
2007
Hashimoto's encephalopathy : Epidemiology, pathogenesis and management.
CNS Drugs
21
799
811
13. GharibH
2008
Review: Available evidence does not support a benefit for thyroid hormone replacement in adults with subclinical hypothyroidism.
Evid Based Med
13
22
Štítky
Interní lékařství
Článek vyšel v časopisePLOS Medicine
Nejčtenější tento týden
2008 Číslo 9- Berberin: přírodní hypolipidemikum se slibnými výsledky
- Léčba bolesti u seniorů
- Příznivý vliv Armolipidu Plus na hladinu cholesterolu a zánětlivé parametry u pacientů s chronickým subklinickým zánětem
- Jak postupovat při výběru betablokátoru − doporučení z kardiologické praxe
- Červená fermentovaná rýže účinně snižuje hladinu LDL cholesterolu jako vhodná alternativa ke statinové terapii
-
Všechny články tohoto čísla
- Towards a Data Sharing Culture: Recommendations for Leadership from Academic Health Centers
- A 50-Year-Old Woman with Recurrent Generalised Seizures
- Tobacco Control Yields Clear Dividends for Health and Wealth
- Ethical and Practical Issues Associated with Aggregating Databases
- Publication of Clinical Trials Supporting Successful New Drug Applications: A Literature Analysis
- Informed Consent in the Genomics Era
- Birth Size and the Pathogenesis of Breast Cancer
- Animal Models of Inflammatory Bowel Disease at the Dawn of the New Genetics Era
- Making Sense of Non-Financial Competing Interests
- PLOS Medicine
- Archiv čísel
- Aktuální číslo
- Informace o časopisu
Nejčtenější v tomto čísle- Informed Consent in the Genomics Era
- Publication of Clinical Trials Supporting Successful New Drug Applications: A Literature Analysis
- A 50-Year-Old Woman with Recurrent Generalised Seizures
- Ethical and Practical Issues Associated with Aggregating Databases
Kurzy
Zvyšte si kvalifikaci online z pohodlí domova
Současné možnosti léčby obezity
nový kurzAutoři: MUDr. Martin Hrubý
Všechny kurzyPřihlášení#ADS_BOTTOM_SCRIPTS#Zapomenuté hesloZadejte e-mailovou adresu, se kterou jste vytvářel(a) účet, budou Vám na ni zaslány informace k nastavení nového hesla.
- Vzdělávání



