-
Články
Top novinky
Reklama- Vzdělávání
- Časopisy
Top články
Nové číslo
- Témata
Top novinky
Reklama- Videa
- Podcasty
Nové podcasty
Reklama- Kariéra
Doporučené pozice
Reklama- Praxe
Top novinky
ReklamaTrends in traumatic brain injury mortality in China, 2006–2013: A population-based longitudinal study
In a population-based cohort study, Guoqing Hu and colleagues examine trends in traumatic brain injury mortality in China, 2006–2013.
Published in the journal: . PLoS Med 14(7): e32767. doi:10.1371/journal.pmed.1002332
Category: Research Article
doi: https://doi.org/10.1371/journal.pmed.1002332Summary
In a population-based cohort study, Guoqing Hu and colleagues examine trends in traumatic brain injury mortality in China, 2006–2013.
Introduction
Traumatic brain injury (TBI) is defined as an alteration of brain function or evidence of brain pathology caused by an external force [1]. It is a serious public health problem worldwide. Each year, TBI causes a substantial number of deaths and temporary and permanent disabilities [2–5]. In the United States, for example, a total of approximately 2.5 million emergency department visits, 282,000 hospitalizations, and 56,000 deaths occurred due to TBI in 2013 [6]. In Europe, Majdan et al. [7] report that TBI caused about 82,000 deaths and was recorded in 2.1 million hospital discharges in 2012.
Understanding the patterns, causes, and trends of TBI is critical for quantifying the severity of the problem, identifying risk factors, developing prevention solutions, and evaluating interventions and policies at local, national, and global levels. Unfortunately, few publications have addressed the epidemiological characteristics of TBI morbidity and mortality, and most available data are from high-income countries (HICs) [8–12]. Rigorous national epidemiological studies are particularly scarce for TBI in most low - and middle-income countries (LMICs). For China, the only available epidemiological studies on TBI that have been published in international or domestic academic journals were conducted among outpatients and/or inpatients at local hospitals, and the results cannot be generalized to the national population [13–15].
The absence of high-quality research evidence from LMICs like China not only prevents the public and policy-makers from recognizing the scope, severity, and urgency of TBI, and therefore taking actions to curb the threat, but also substantially undermines the reliability and validity of the estimation of global TBI burden, which depends greatly on the availability and quality of research evidence from LMICs at the national and local levels [16,17].
To address these research gaps, we used mortality data from the nationally representative Disease Surveillance Points (DSPs) system in China to investigate TBI mortality and differences in mortality based on location (urban/rural), sex, age group, and external cause of TBI from 2006 to 2013 in China.
Methods
Ethics concerns
This secondary analysis was approved by the ethics committee of Xiangya School of Public Health, Central South University. Data were de-identified, and informed consent was not required.
Design
We conducted a population-based longitudinal analysis to examine trends in TBI mortality and differences based on location (urban/rural), sex, age group, and external cause of TBI from 1 January 2006 through 31 December 2013. RECORD guidelines (S1 RECORD Checklist) were adhered to in reporting this study.
This study was part of a larger study focusing on the fatality burden from several major causes of injury, including TBI, in China using the DSPs data. Ideas were conceived in August 2016, and a research plan was prepared, listing the key points of secondary data analysis, including research questions, study population, data sources, definitions of primary injuries, cause classifications, related International Classification of Diseases–10th Revision (ICD-10) codes, primary outcome measures, explanatory factors (location, sex, age group, and year), statistical analyses, and ethical reviews (S1 Protocol). In mid-October 2016, we completed the extraction and collation of data from the DSPs system. We then analyzed the data using the preexisting data analysis plan.
Data sources
Mortality rates were derived from the DSPs dataset. Mortality data for this study can be accessed by contacting the Division of Vital Registration and Cause of Death Surveillance, National Center for Chronic and Noncommunicable Disease Control and Prevention, Chinese Center for Disease Control and Prevention (CDC) (contact email: crvsdata@chinacdc.cn). The DSPs system was first established by the Chinese central government in 1978, and data are collected under the direction of the China CDC [18]. Each surveillance point represents a single district (urban area) or county (rural area), and all residents of that geographic area are covered by the DSPs system [19]. In 2004–2006, an important improvement was made, raising the number of surveillance points to 161 (64 urban, 97 rural) across all 31 Chinese provinces and creating a dataset that is demographically representative of the full country [19–21]. Starting in 2008, the Chinese government introduced a web-based approach to report death cases using the DSPs system [22,23], and the timeliness of data reporting has improved remarkably. In 2013, the number of surveillance points was increased to 605 points [24], but we used data only from the 161 points available beginning in 2006 for this analysis to avoid potential impact on our research from the DSPs update in 2013.
All causes of death in DSPs are determined according to a standard protocol by trained coders located in hospitals or local CDC offices. Since 2004, coding has been conducted using ICD-10 codes. Duplicate deaths are identified and eliminated as part of routine processing operations at the provincial and county levels. An internal procedural check system evaluates timeliness, completeness, and accuracy of data reporting, and statistical measures (e.g., the standard United Nations Age–Sex Accuracy Index) are employed to monitor data quality [18]. Further, a fixed national sample survey is conducted at all DSPs locations every 3 years to obtain extra information that permits adjustment for underreporting [25]. Previous studies indicate that the DSPs data are generally reliable, valid, and nationally representative [18,25].
Definition of traumatic brain injury
TBI-induced deaths were identified according to the ICD-10 codes recommended by the US CDC [26,27], based on the following diagnosis codes: S01.0–S01.9, S02.0, S02.1, S02.3, S02.7–S02.9, S04.0, S06.0–S06.9, S07.0, S07.1, S07.8, S07.9, S09.7−S09.9, T01.0, T02.0, T04.0, T06.0, T90.1, T90.2, T90.4, T90.5, T90.8, and T90.9. Based on published studies and ICD-10 codes of external cause of injury [8,28], we classified the underlying external causes of TBI deaths into 4 categories: motor vehicle crashes (V30–V79 [.4–.9], V81.1, V82.1, V83–V86 [.0–.3], V20–V28 [.3–.9], V29 [.4–.9], V12–V14 [.3–.9], V19 [.4–.6], V02–V04 [.1, .9], V09.2, V80 [.3–.5], V87 [.0–.8], V89.2, X82, Y03, Y32), falls (W00–W19, X80, Y01, Y30), struck by and against (W20–W22, W50–W52, X79, Y00, Y04, Y29, Y35.3), and all others (remaining ICD-10 codes for all other causes). To detail the subgroups of TBI deaths from motor vehicle crashes, we report the results by road user category. Road users were classified into 5 categories according to the ICD-10 injury matrix recommended by the US CDC [29]: vehicle occupant (V30−V79 [.4−.9], V81.1, V82.1, V83−V86 [.0−.3]), motorcyclist (V20−V28 [.3−.9], V29 [.4−.9]), pedal cyclist (V12−V14 [.3−.9], V19 [.4−.6]), pedestrian (V02−V04 [.1, .9], V09.2), and all others (V80 [.3−.5], V87 [.0−.8], V89.2).
Statistical analyses
The DSPs database underwent several changes in its sampling methods during the 1990s, mid-2000s, and recently. To eliminate bias from these changes, we analyzed mortality data from the same 161 surveillance points from 2006 to 2013, in this study. We calculated the overall and cause-specific age-standardized mortality over that time period. The direct standardization method was adopted to adjust for the impact of the population structure. The census population in 2010 was used as the reference population. The 95% confidence intervals of mortality rates were calculated.
Because substantial age variations in TBI morbidity and mortality have been reported in previous publications [8,26], we created 7 age groups: 0–4 years, 5–14 years, 15–24 years, 25–44 years, 45–64 years, 65–74 years, and 75 years and older. We calculated sex-, age-, location-, and cause-specific death rates to inform policy-making priorities. Pearson chi-square tests were used to test differences in mortality rates between subgroups. When the assumption for the chi-square test was violated, Fisher’s exact test was used.
The Cochran–Armitage trend test was used to examine the significance of trends in mortality. Subgroup analysis was conducted by strata of location (urban/rural), sex, age group, and external cause of TBI. Because of the overdispersion of TBI-induced deaths, we used negative binomial models to explore the associations of deaths with socio-demographic factors including location (urban/rural), sex, age group, and year [30,31]. Mortality rate ratios (MRRs) and corresponding 95% CIs quantified the extent of associations. Following strategies in a previous report [32], we tested the significance of the interaction of age group × year by comparing negative binomial models with and without multiplicative interaction terms using the likelihood ratio test.
All statistical analyses were conducted using Stata statistical software version 12.1. Differences were considered statistically significant in 2-tailed tests if p-values were less than 0.05.
Results
Surveillance sample characteristics of disease surveillance points
Between 2006 and 2013, the population covered by the 161 included surveillance points in the DSPs database increased from 76 million to 83 million, accounting, respectively, for 5.8% and 6.3% of the total population of China (S1 Table). Across the study time period, males generally represented 50.3%–51.1% of the surveillance sample, the proportion of urban residents rose from 37.4% to 43.5%, and older age groups represented a gradually growing portion of the whole population. All of these trends are consistent with national demographical statistics in China over the same years.
Overall traumatic-brain-injury-induced mortality and trends
In total, 93,793 TBI-induced deaths were captured by the DSPs between 1 January 2006 and 31 December 2013. Age-adjusted TBI mortality first increased from 13.23 per 100,000 population in 2006 to 17.06 per 100,000 population in 2008, and then started to fall gradually. In 2013, age-adjusted TBI mortality was 12.99 per 100,000 population (SE = 0.13) (Table 1). After adjusting for location (urban/rural), sex, and age group, TBI mortality from 2007 to 2011 was increased, respectively, by 17%, 31%, 15%, 27%, and 19% compared with 2006, and then remained at a similar level from 2012 to 2013 (Table 2).
Tab. 1. Mortality rates of traumatic brain injury per 100,000 population by location, sex, age group, and external cause of injury in China, 2006–2013. 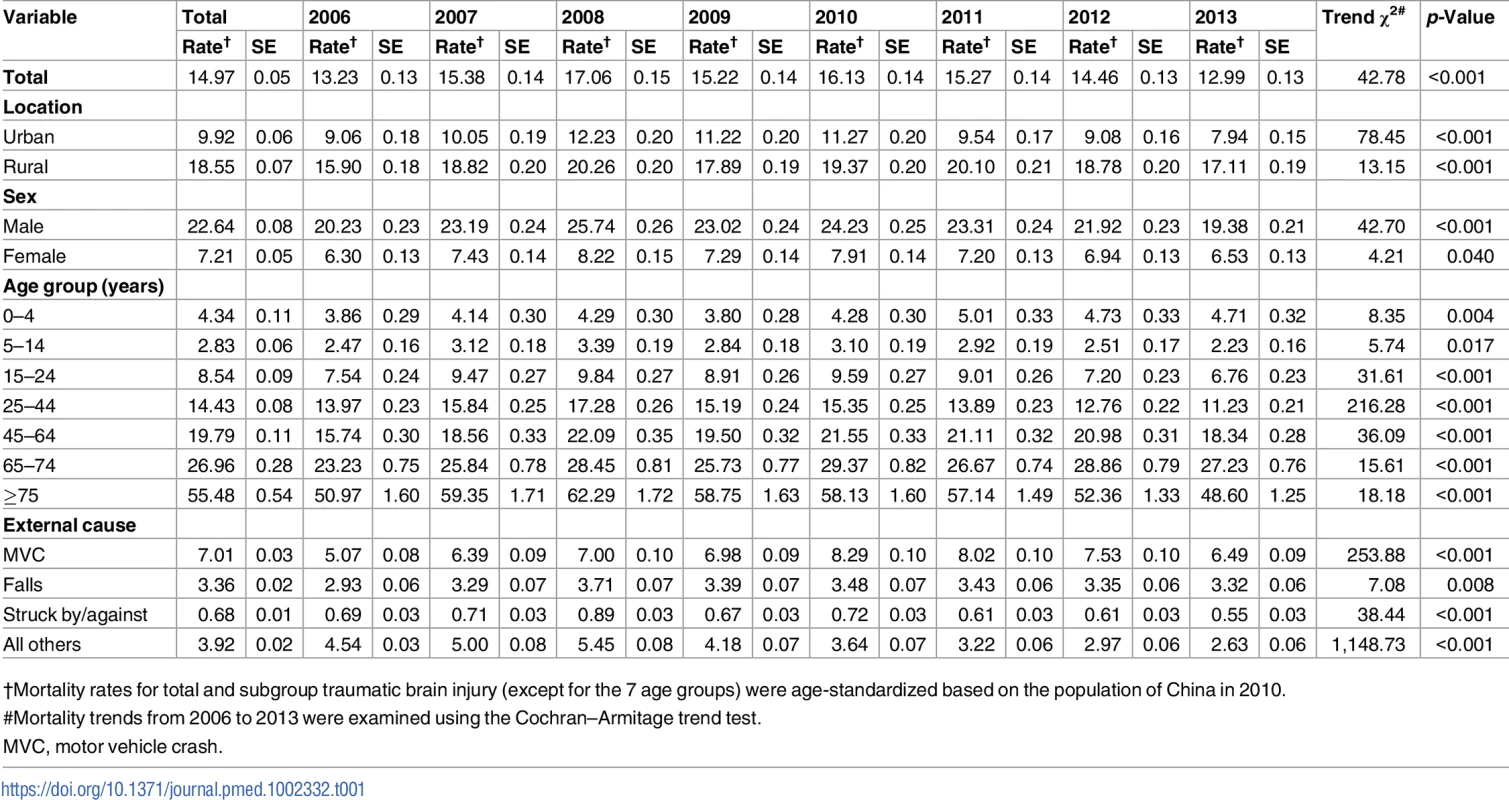
†Mortality rates for total and subgroup traumatic brain injury (except for the 7 age groups) were age-standardized based on the population of China in 2010. Tab. 2. Associations of traumatic brain injury mortality with socio-demographic variables from multivariate negative binomial regression (China, 2006–2013). 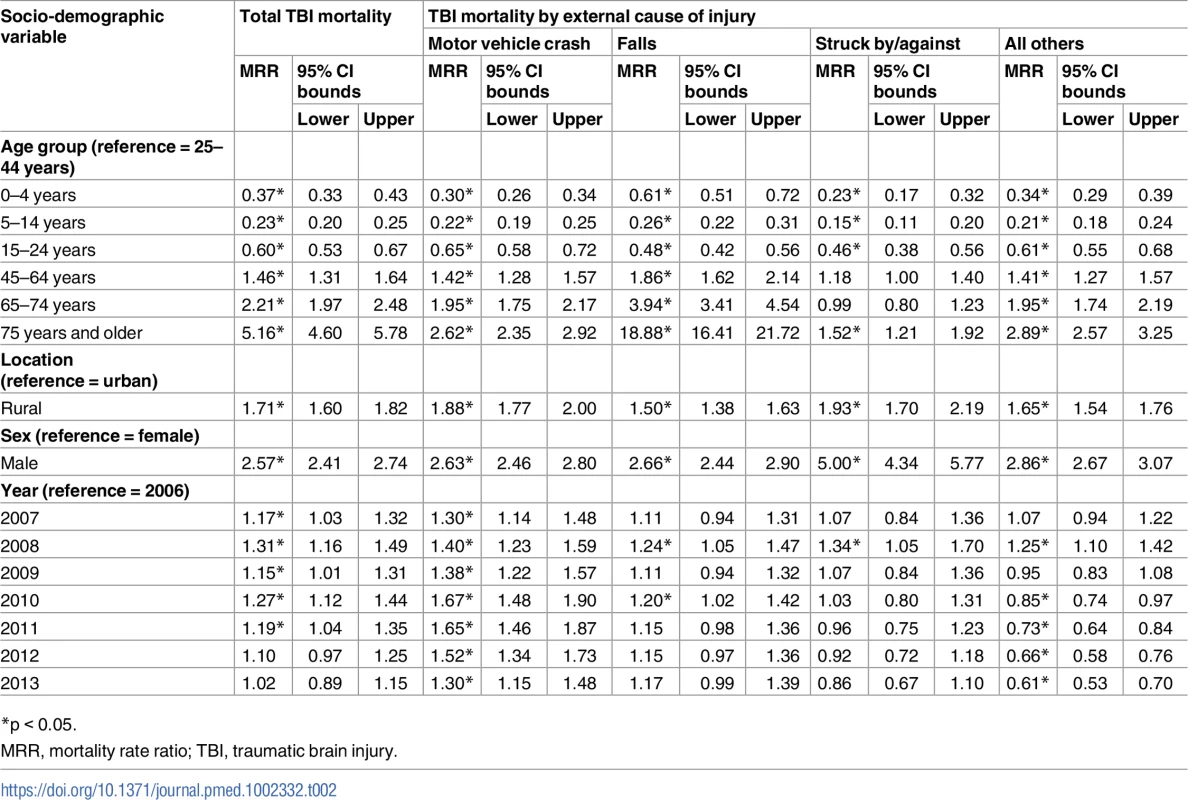
*p < 0.05. Urban–rural difference
Rural residents had much higher TBI mortality rates between 2006 and 2013 than urban residents (age-standardized mortality ratio ranging from 1.6 to 2.2) (S2 Table; Fig 1A). After adjusting for sex, age group, and year, rural residents were at greater risk of dying from TBI than urban residents (MRR for overall TBI: 1.71, 95% CI 1.60–1.82; for motor vehicle crashes: 1.88, 95% CI 1.77–2.00; for falls: 1.50, 95% CI 1.38–1.63; for struck by/against: 1.93, 95% CI 1.70–2.19; Table 2). TBI mortality rates followed similar patterns for both urban and rural residents from 2006 to 2013 (Fig 1A).
Fig. 1. Mortality rates from traumatic brain injury by location (urban/rural), sex, and age group in China, 2006–2013. 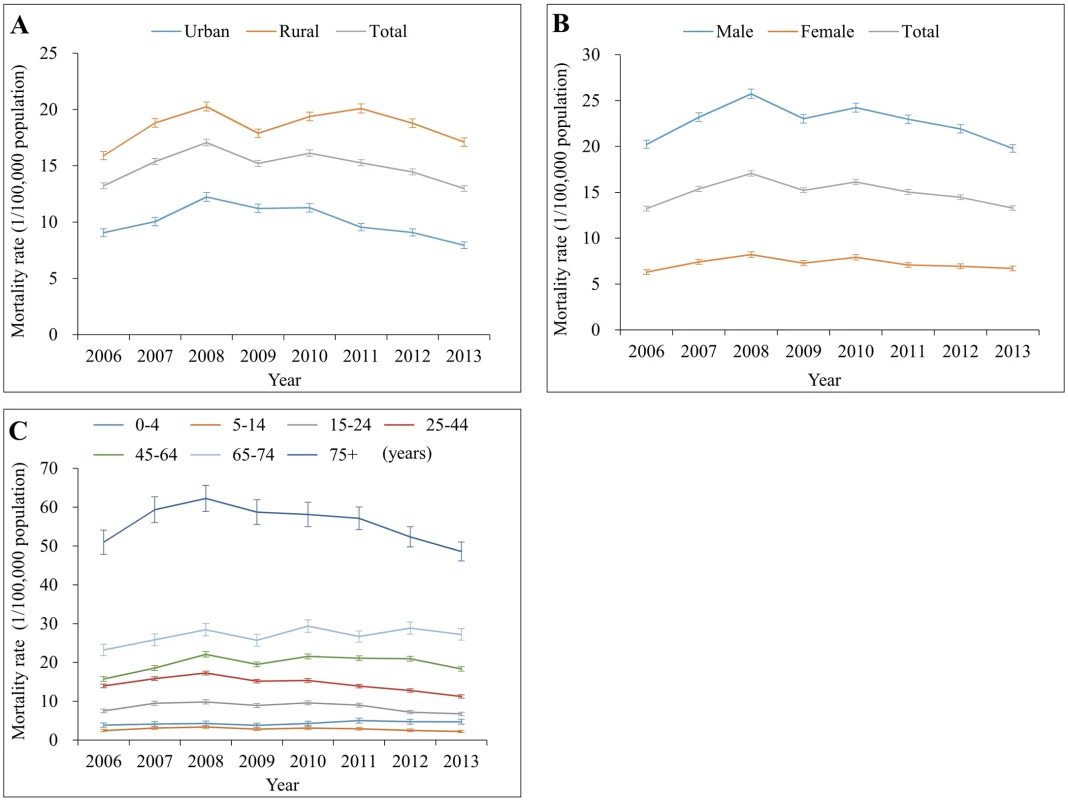
(A) By location; (B) by sex; (C) by age group. Mortality rates in (A) and (B) were age-standardized based on the population of China in 2010. Sex difference
Compared to females, males had about a 3-fold greater risk of dying from TBI during 2006–2013 (S3 Table; Fig 1B). TBI mortality for both males and females showed a similar pattern of change over time in the study period. After adjusting for location (urban/rural), age group, and year, males had 2.57 times the risk of dying from TBI compared to females. The adjusted male–female MRR was 2.63 for TBI from motor vehicle crashes and 2.66 for TBI from falls, but was up to 5.00 for TBI from struck by/against (Table 2).
Variations across age groups
Large TBI mortality variations were observed between age groups for all years (Fig 1C). For persons aged 5 years and older, TBI mortality increased substantially as age increased. In 2013, children aged 5–14 years had the lowest mortality (2.33 per 100,000 population), while adults aged 75 years and older had the highest mortality (48.60 per 100,000 population) (Table 1); the overall TBI-induced mortality rates by 5-year age group and year are listed in S4 Table.
Trends in TBI mortality between 2006 and 2013 varied with age group. All 7 age groups showed a rising tendency for TBI deaths from 2006 to 2008, but 3 age groups (15–24 years, 25–44 years, and ≥75 years) showed a gradual and substantial decrease in TBI mortality after 2008. The age group 0–4 years showed a slight increase, and the other 3 groups remained nearly unchanged, between 2008 and 2013 (Fig 1C).
Similar and large TBI mortality variations remained between age groups after adjusting for location (urban/rural), sex, and year, but the pattern was different for external cause of TBI (Tables 2 and 3). For example, the adjusted MRR for adults aged 75 years and older compared to adults aged 25–44 years old was 18.88 for falls (95% CI 16.41–21.72) but was far lower than 10 for all other external causes.
Tab. 3. Associations of traumatic brain injury mortality from motor vehicle crashes with socio-demographic variables from multivariate negative binomial regression (China, 2006–2013). 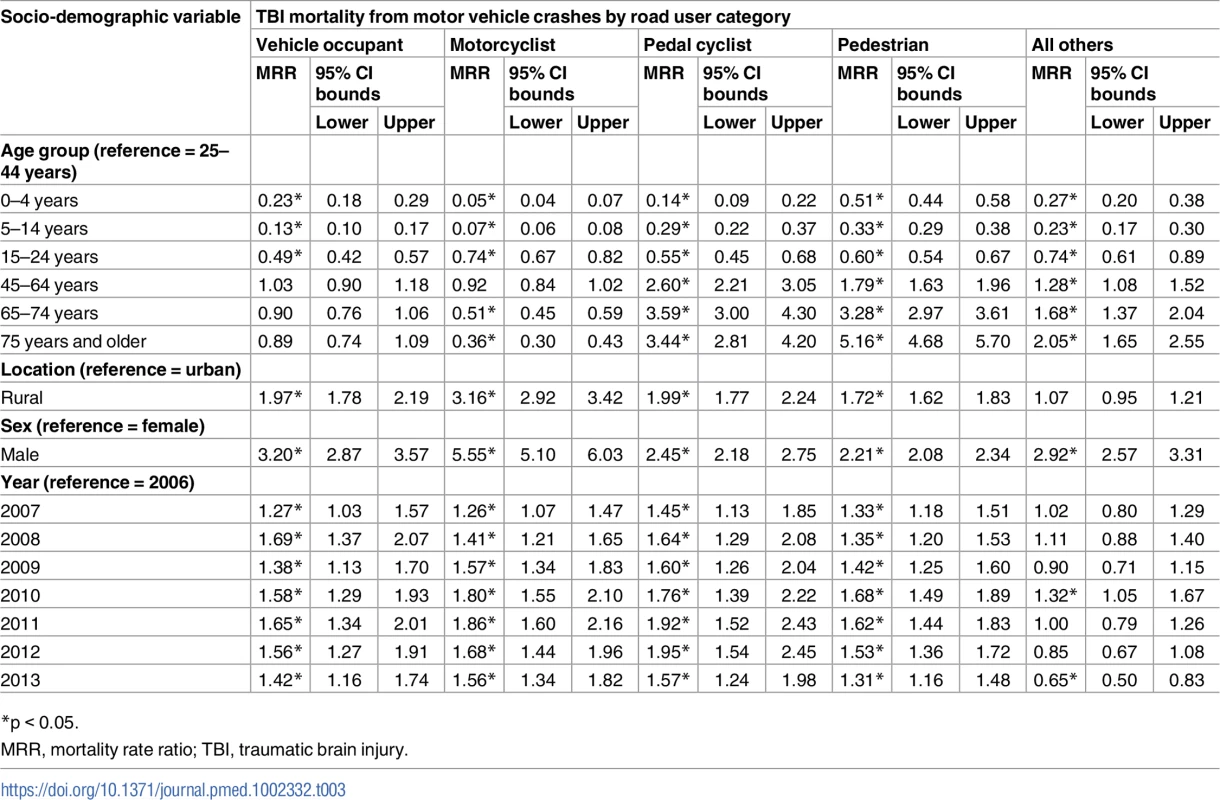
*p < 0.05. The interaction of age group × year was statistically insignificant in all models (all p-values for the interaction > 0.05; see Tables 2 and 3) except for the model of the TBI-induced mortality rate for motorcyclists (υ = 42, likelihood ratio = 76.60, p-value for the interaction < 0.05).
External cause of TBI-induced deaths
From 2006–2013, motor vehicle crashes and falls were consistently the 2 leading causes of TBI mortality for both urban and rural residents, and for both males and females (Fig 2). Just as large differences were observed in overall TBI mortality, large urban–rural and male–female gaps also occurred in cause-specific TBI mortality. Strikingly, TBI mortality from motor vehicle crashes generally increased from 2006 to 2010 but began to decrease gradually after 2010 in both urban and rural areas. The reduction since 2010 was greater in urban areas than in rural areas.
Fig. 2. Mortality rates from traumatic brain injury by urban/rural location, sex, and external cause of injury (China, 2006–2013). 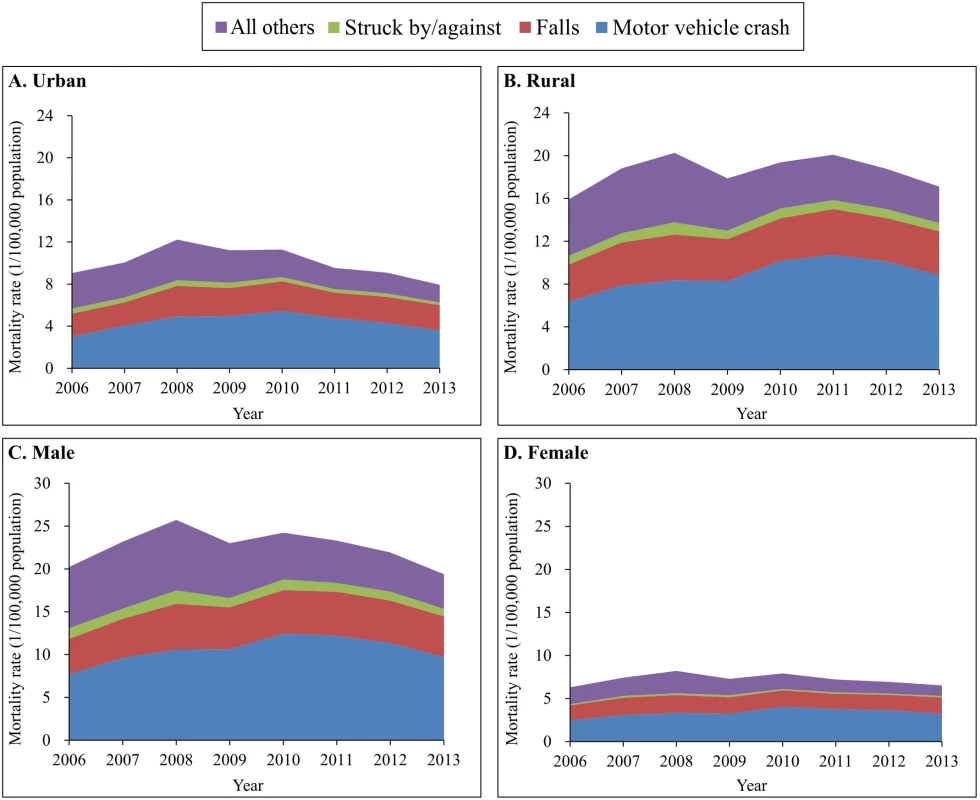
(A) Urban areas; (B) rural areas; (C) male; (D) female. Mortality rates were age-standardized based on the population of China in 2010. The spectrum of the causes of TBI deaths varied somewhat across age groups. For all 6 age groups less than 75 years, the leading cause of TBI mortality was motor vehicle crashes, but for adults aged 75 years and older, the leading cause was falls (Fig 3). After age 15 years, falls began to contribute more and more to total TBI mortality as age increased.
Fig. 3. Mortality rates from traumatic brain injury by age group and external cause of injury (China, 2006–2013). 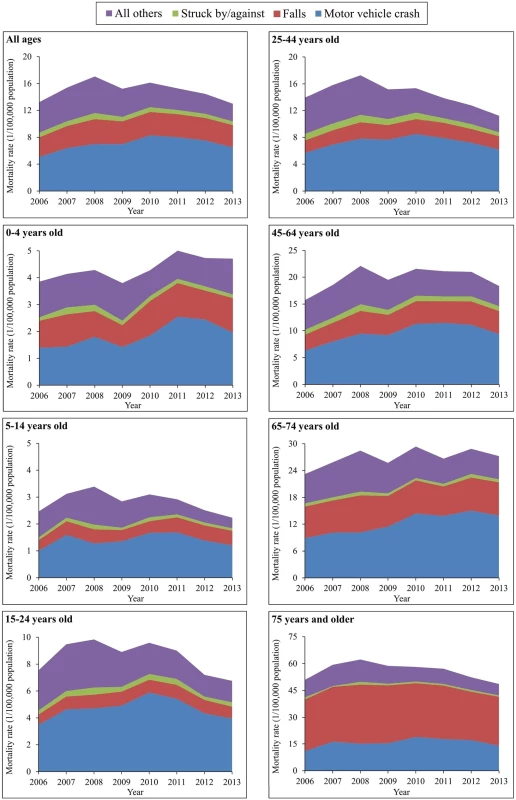
The external causes of TBI mortality changed greatly between 2006 and 2013 across age groups. All 7 groups showed significant increases in TBI mortality attributed to motor vehicle crashes, with the largest increase occurring in the age group 65–74 years (from 8.89 to 13.95 per 100,000 population) (S5 Table).
Pedestrians were the most vulnerable road users for TBI deaths attributed to motor vehicle crashes in both urban and rural areas and for both sexes (Fig 4). Notably, the age-adjusted TBI mortality for motorcyclists increased 54% for rural residents (from 1.70 to 2.61 per 100,000 population) and 35% for males (from 2.16 to 2.91 per 100,000 population) between 2006 and 2013. Similarly, TBI mortality for pedal cyclists rose by 91% in rural areas, 41% in males, and 100% in females between 2006 and 2013 (S6 and S7 Tables).
Fig. 4. Mortality rates from traumatic brain injury due to motor vehicle crashes by urban/rural location, sex, and road user category (China, 2006–2013). 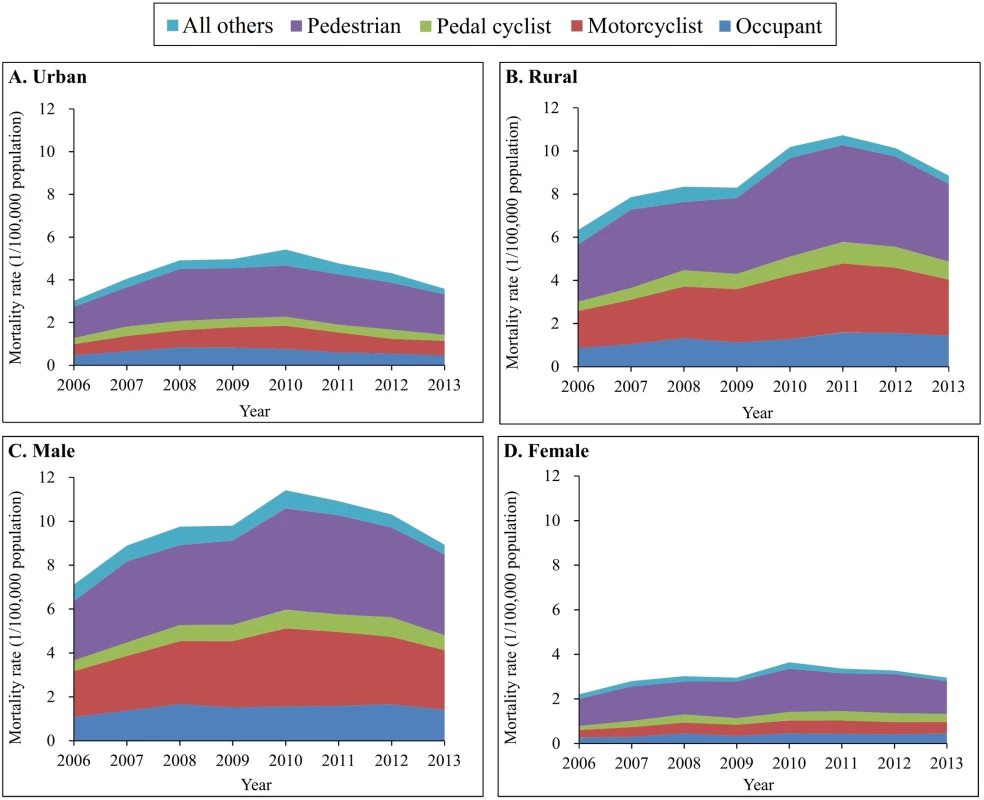
(A) Urban areas; (B) rural areas; (C) male; (D) female. Mortality rates were age-standardized based on the population of China in 2010. The spectrum of road use for TBI mortality attributed to motor vehicle crashes varied across age groups. For children aged 0–4 and 5–14 years and for adults aged 65 years and older, pedestrian deaths constituted over 60% of total TBI deaths from motor vehicle crashes (Fig 5). For the age groups 15–24, 25–44, and 45–64 years, motorcyclist deaths emerged as the first or second leading cause of TBI mortality from motor vehicle crashes, explaining 50% of total TBI deaths due to motor vehicle crashes in 2013; the contribution of motorcyclist deaths to TBI mortality caused by motor vehicle crashes was 59% in the age group 15–24 years (Fig 5).
Fig. 5. Mortality rates from traumatic brain injury due to motor vehicle crashes by age group and road user category (China, 2006–2013). 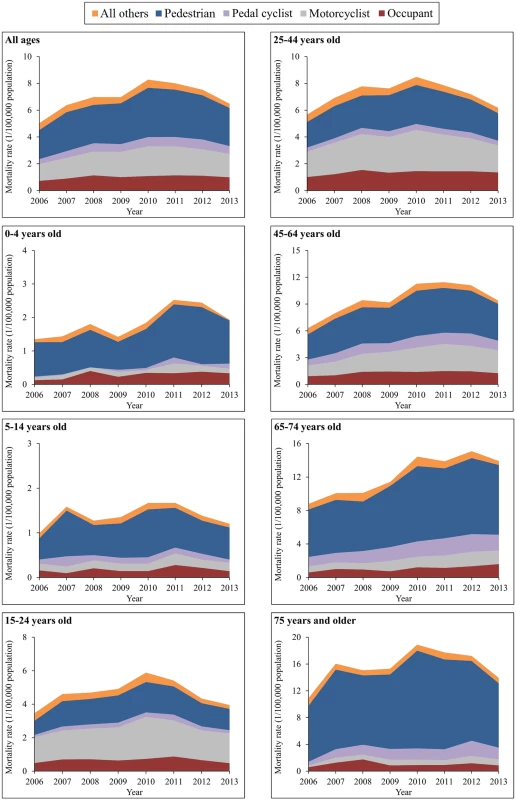
Across all ages, TBI mortality increased by 38% for vehicle occupants, 39% for motorcyclists, and 31% for pedestrians between 2006 and 2013 (S8 Table). Notable age-specific TBI mortality changes over the study time period included the following: a 166% increase for occupants in the age group 65–74 years, an increase of over 110% for motorcyclists in the age groups ≥ 45 years combined, a 626% rise for pedal cyclists in the age group 0–4 years but a 26% decrease in the age group 5–14 years, and increases for pedestrians in all age groups, especially in the age groups 15–24 years, 45–64 years, and 65–74 years (increased 50%, 46%, and 47%, respectively) (S8 Table).
Discussion
Summary of findings
To our knowledge, this is the first published national study to report socio-demographic patterns, trends, and external causes of TBI mortality in a low - or middle-income country like China. Five key findings are summarized as follows: (1) overall TBI mortality remained relatively stable and high (12.99–17.06 per 100,000 population) from 2006 to 2013; (2) there were great variations in TBI rates across locations (urban/rural), sex, and age groups that persisted across the study time period for both overall and cause-specific TBI mortality rates; (3) motor vehicle crashes were the leading cause of TBI mortality for Chinese residents under 75 years, but falls were the leading cause of TBI deaths for adults aged 75 years and older; (4) pedestrians were the most common type of road user in TBI deaths from motor vehicle crashes in children aged 0–14 years and adults aged 65 years and older, but motorcyclists were as vulnerable as pedestrians among residents 15–64 years; and (5) notable TBI mortality increases occurred in persons aged 45–74 years for vulnerable road users (pedestrians, motorcyclists, and pedal cyclists).
Potential influence of disease surveillance points system updates
As described above, the DSPs have experienced 2 major updates in history. First, there were adjustments made to the surveillance points in 1989 and in 2004–2006. In both cases, the aim was to improve the coverage and representativeness of the surveillance samples for the total population [19–21]. By 2006, the number of surveillance points was raised to 161 points, including 64 urban points and 97 rural points, across 31 provinces [19]. We initiated our study timeline in 2006, after the changes had been implemented, and therefore we assume the changes in surveillance points would not have had a substantial impact on our results.
The second major update to DSPs was the introduction of web-based reporting in 2008 [33]. Since then, all death cases have been reported by the web-based National Death Registration Management System of Chinese CDC. The change in data reporting approach may have caused some problems in practice and may have had an unexpected impact on reported mortality rates. For example, many local employees who were responsible for DSPs data reporting needed time to familiarize themselves with the web-based reporting system (although they had received specific training before the web-based reporting system was introduced nationwide). In addition, the quality control office needed time to develop new methods to assess and guarantee the quality of web-based reporting. Consequently, the introduction of the web-based reporting system in 2008 may have caused unexpected fluctuations in mortality rates in the initial stages after the change. Our results show a notable and consistent fluctuation in overall and location-, sex-, age-, and cause-specific TBI mortality rates between 2007 and 2009. Similar fluctuations are reported in previous publications that used DSPs data from the same period to assess trends in mortality from cardiovascular diseases [22], tuberculosis [23], and road traffic crashes [34,35]. These fluctuations may reflect the effect of the introduction of the web-based reporting system in all DSPs surveillance points in 2008.
Interpretation of findings
The overall TBI mortality rate in China (12.99 per 100,000 population in 2013 and slightly higher in previous years) approximates that in the US (17.0 per 100,000 population) [6], Europe (11.7 per 100,000 population) [7], and Germany (11.5 per 100,000 population) [36]. Given potential differences across the studies—including aspects of the study methodology, population structure and culture, data acquisition, and definition of TBI [37,38]—differences in TBI mortality observed across countries and regions should be interpreted with caution. However, the data clearly indicate that TBI should be regarded as a significant public health problem in China, as TBI mortality rates remained fairly stable and high from 2006 to 2013.
The slight decrease in TBI mortality since 2010 in China may reflect improvements in pre-hospital aids and hospital treatment, as well as fragmented efforts for injury prevention in China [39–41]. An analysis of pre-hospital aid data from Fangshan District, Beijing, for example, showed that the median time from receiving an emergency call to the arrival of an ambulance decreased significantly between 2009 and 2012 [42]. Based on data from the Chinese Health Statistics Yearbook [43,44], the number of hospital beds per 1,000 population increased from 2.72 beds in 2006 to 4.55 beds in 2013.
Corresponding to results from previous epidemiological studies [3,8] and literature reviews [2,37,45] from HICs, our results showed high TBI mortality risk in Chinese males, rural residents, and older adults. Greater TBI mortality risk in males may primarily reflect more risk-taking behaviors among men than among women, including risks such as distracted driving from cell phone use (68% versus 56%) [46], driving without helmets (62% versus 46%) and seatbelts (27% versus 25%) [47], use of weapons (incidence rate ratio = 2.74) [48], higher alcohol consumption (both in frequency and quantity) [49], and driving under the influence of alcohol (odds ratio: 2.78) [50]. Our finding of increased risk among rural residents also replicates results from previous studies [51–54]. Higher risk among rural residents may be attributed to more law violations and high-risk behaviors of rural residents, plus underdeveloped injury prevention and medical care in rural areas. Finally, our study reproduces findings from HICs [28,36,55] that older adults have higher TBI mortality risk. Such a finding is likely the result of the natural aging process. As adults age, they are at increased risk of having multiple chronic diseases such as hypertension, hyperlipidemia, and glaucoma, which result in balance impairments, vision disorders, and/or cognitive impairment and raise the risk of TBI injury. According to the Global Burden of Disease Study 2013, the number of individuals with several morbidities rapidly increases with age: in elderly adults aged 80 years and older, 10.3% had 1 to 4 sequelae, 64.6% had 5 to 9 sequelae, and 25.1% had 10 or more sequelae in 2013 [56].
One finding differs substantially from reports in other countries. In China, motor vehicle crashes were the most common cause of TBI mortality for all age groups under 75 years, in contrast to cause patterns in the United States, where firearm-related wounds are the leading cause of TBI mortality in the age groups 20–24 and ≥75 years [28], and in contrast to many European countries, including Austria, Finland, Germany, Switzerland, and the United Kingdom, where about 50% of TBI mortalities are caused by falls [7]. Our finding represents the heavy burden caused by road traffic crashes to Chinese residents, and the urgent need for motor vehicle safety efforts. These results concord with those from published domestic epidemiological studies for overall road traffic mortality in China [34,35,57,58].
Within the motor vehicle crash category, our detailed analysis by road user category reveals important findings. Chinese children aged 0–4 and 5–14 years, as well as adults aged 65 years and older, were most vulnerable to TBI death as pedestrians. In the middle years of life (ages 15–64 years), motorcyclists emerged as the road users with the highest rate of TBI death. These results correspond with all-mortality data among road users in other LMICs but differ from data from HICs [45]. They likely reflect the patterns of road use in China across different age groups, and the distinctions in road use and motorcycle operation between LMICs and HICs. In addition, we also observed distinct urban–rural differences in TBI mortality patterns, which were mainly driven by urban–rural differences in mortality from motor vehicle crashes. These results agree with the analysis for total road traffic mortality [54].
Implications
Our findings have 2 major implications. First, the detailed analysis quantifies the severity of TBI as a public health problem in China. It describes high-risk populations and the major causes of TBI mortality, providing rigorous empirical evidence for decision-makers to tackle this problem and offering valuable data to estimate global TBI burdens. The results also highlight the urgency of improving injury prevention, pre-hospital aid, hospital treatment, and recovery after experiencing a TBI.
The primary and urgent strategic goal for enhancing injury prevention is to assign a single government agency to coordinate injury prevention efforts that presently span multiple government departments and partners [39–41]. From the perspective of immediate action, some prevention measures that have been demonstrated effective in HICs should be introduced and tailored culturally to ensure their acceptability, feasibility, and efficacy. Examples include helmet use for bicyclists and motorcyclists, child restraint (car seat and booster seat) use for child passengers, seatbelt use for all vehicle passengers, use of shock-absorbing materials in the surface of children’s playgrounds, and periodic review of vision, medication, and home environment assessments and modifications [59–62] to reduce fall-induced injury, especially among older adults. Additionally, government policies to improve the safety of hospitals and nursing facilities and to enhance the pension policy and system for the older people, especially elderly individuals in rural areas, have potential to play a meaningful role in reducing the morbidity and mortality of TBI caused by falls [63]. Unfortunately, many proven interventions to prevent major causes of unintentional child injuries are underrepresented in Chinese laws and regulations, and the associated implementation responsibilities are poorly defined [64]. Basic prerequisites to implement proven prevention interventions should be implemented by the government of China.
In addition, effective interventions to improve pre-hospital aid, hospital treatment, and rehabilitation services for TBI patients are needed [65–67]. These may include developing a pre-hospital trauma care system with reference to successful programs in HICs, quality improvement programs, speeding up rescue efforts to ensure individuals receive life-sustaining care within a few minutes of injury, and teaching individuals how to react at the scene of an injury. These programs can prevent TBI-related death and disability and should be introduced and disseminated nationwide. Of course, necessary tailoring and modifications may be incorporated to respect China’s healthcare system and culture.
Second, our results provide valuable data to guide etiological studies exploring causal and modifiable factors leading to high TBI mortality rates particularly in Chinese populations, including vulnerable and high-risk populations (males, rural residents, and older adults). Our study also offers data concerning significant rises in TBI mortality among specific groups, such as vulnerable road users in the age group ≥75 years. In addition, effective, easy-to-implement interventions should be applied in practice to protect high-risk populations. Such interventions could include encouraging vulnerable pedestrians to wear light-colored clothing and reflective materials, construction of sidewalks and raised crossings, reducing legal speed limits, and construction of refuge islands and raised platforms at bus stops [68,69].
Study limitations
This study has several limitations. First, the DSPs dataset does not cover confounding factors that influence TBI mortality and may influence TBI mortality trends. Such factors include individual differences and behaviors, environmental factors, and pre-hospital and hospital care. Second, TBI morbidity data were not available. Morbidity data may reveal different trends, patterns, and cause spectrums compared with mortality data and are needed within LMICs. Third, TBI deaths may be seriously underestimated in the DSPs mortality data because of many missing S - or T-codes in injury-related deaths. A TBI death in the DSPs system is defined only with the coexistence of an external cause of injury code (E-code) and a nature of injury code (N-code, namely S - or T-code). Supplemental analysis shows that up to 46% of injury deaths of 2006–2013 did not have an S - or -T-code on the death certificate, a proportion that is far higher than that in the US (0.6%) [70]. This strongly suggests that TBI deaths may be underestimated in our analysis. Further, we found that the proportion of missing S - or T-codes increased slightly between 2009 and 2013, which may have led to an apparent decrease of TBI mortality rates and influenced TBI mortality trends to a small extent. Finally, our results may be affected by the completeness of reporting, including the accuracy of coding of cause of death in the DSPs system. The final data were rigorously checked and corrected through various methods including routine national survey sampling every 3 years at all surveillance points [71,72], but minor flaws may remain.
Conclusion
In conclusion, TBI mortality has remained high and stable for many years in China, constituting a significant threat to the health of the Chinese population. Males and rural residents are at particularly high risk of dying from TBI compared to females and urban residents. TBI mortality risk rises dramatically as individuals age. Future research should explore reasons for the particularly high risk of TBI mortality among particular populations, as well as for recent increases in certain subgroups. In particular, evidence-based prevention, response, and treatment interventions for TBI, as recommended by the World Health Organization and other agencies, should be translated to Chinese culture and implemented nationwide. Examples of such programs include efforts to reduce injury risk from motor vehicle crashes (helmet use, car seat and booster seat use, lower speed limits, improved drunk driving laws, and alcohol ignition interlock use) and falls (exercise, home modification, and multifaceted interventions).
Supporting Information
Zdroje
1. Menon DK, Schwab K, Wright DW, Maas AI. Position statement: definition of traumatic brain injury. Arch Phys Med Rehabil. 2010;91 : 1637–40. doi: 10.1016/j.apmr.2010.05.017 21044706
2. Peeters W, van den Brande R, Polinder S, Brazinova A, Steyerberg EW, Lingsma HF, et al. Epidemiology of traumatic brain injury in Europe. Acta Neurochir (Wien). 2015;157 : 1683–96.
3. Coronado VG, Mcguire LC, Sarmiento K, Bell J, Lionbarger MR, Jones CD, et al. Trends in traumatic brain injury in the U.S. and the public health response: 1995–2009. J Safety Res. 2012;43 : 299–307. doi: 10.1016/j.jsr.2012.08.011 23127680
4. Zaloshnja E, Miller T, Langlois JA, Selassie AW. Prevalence of long-term disability from traumatic brain injury in the civilian population of the United States, 2005. J Head Trauma Rehabil. 2008;23 : 394–400. doi: 10.1097/01.HTR.0000341435.52004.ac 19033832
5. Traumatic brain injury: time to end the silence. Lancet Neurol. 2010;9 : 331. doi: 10.1016/S1474-4422(10)70069-7 20298955
6. Taylor CA, Bell JM, Breiding MJ, Xu L. Traumatic brain injury-related emergency department visits, hospitalizations, and deaths—United States, 2007 and 2013. MMWR Surveill Summ. 2017;66(9):1–16. doi: 10.15585/mmwr.ss6609a1 28301451
7. Majdan M, Plancikova D, Brazinova A, Rusnak M, Nieboer D, Feigin V, et al. Epidemiology of traumatic brain injuries in Europe: a cross-sectional analysis. Lancet Public Health. 2016;1(2):e76–83.
8. Feigin VL, Theadom A, Barker-Collo S, Starkey NJ, McPherson K, Kahan M, et al. Incidence of traumatic brain injury in New Zealand: a population-based study. Lancet Neurol. 2013;12 : 53–64. doi: 10.1016/S1474-4422(12)70262-4 23177532
9. MRC CRASH Trial Collaborators, Perel P, Arango M, Clayton T, Edwards P, Komolafe E, et al. Predicting outcome after traumatic brain injury: practical prognostic models based on large cohort of international patients. BMJ. 2008;336 : 425–9. doi: 10.1136/bmj.39461.643438.25 18270239
10. Fazel S, Wolf A, Pillas D, Lichtenstein P, Långström N. Suicide, fatal injuries, and other causes of premature mortality in patients with traumatic brain injury: a 41-year Swedish population study. JAMA Psychiatry. 2014;71 : 326–33. doi: 10.1001/jamapsychiatry.2013.3935 24430827
11. Scholten AC, Haagsma JA, Panneman MJ, van Beeck EF, Polinder S. Traumatic brain injury in the Netherlands: incidence, costs and disability-adjusted life years. PLoS ONE. 2014;9:e110905. doi: 10.1371/journal.pone.0110905 25343447
12. Vaaramo K, Puljula J, Tetri S, Juvela S, Hillbom M. Head trauma with or without mild brain injury increases the risk of future traumatic death: a controlled prospective 15-year follow-up study. J Neurotrauma. 2015;32 : 1579–83. doi: 10.1089/neu.2014.3757 25584928
13. Zhan H, Wu X, Hu J, Chen L, Wu X, Sun Y, et al. Analysis of epidemiological investigation on the brain injury of elderly inpatients and strategy of medical care to deal with from 2005 to 2015. Chin J Emerg Med. 2016;25 : 779–83.
14. Zhang Y, Qiu J, Wang H, Xu L, Zhou J, Xu M. Analysis of epidemiological characteristics of 338,083 cases of traumatic brain injury. J Trauma Surg. 2016;18 : 328–30.
15. Zhang Y, Qiu J, Zhou J, Xu L, Xu M. Epidemiological study of traffic accidents-related traumatic brain injury in 159,242 cases. Chin J Trauma. 2014;30 : 1215–8.
16. GBD 2015 Mortality and Causes of Death Collaborators. Global, regional, and national life expectancy, all-cause mortality, and cause-specific mortality for 249 causes of death, 1980–2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet. 2016;388 : 1459–544. doi: 10.1016/S0140-6736(16)31012-1 27733281
17. GBD 2015 Disease and Injury Incidence and Prevalence Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990–2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet. 2016;388 : 1545–602. doi: 10.1016/S0140-6736(16)31678-6 27733282
18. Yang G, Hu J, Rao KQ, Ma J, Rao C, Lopez AD. Mortality registration and surveillance in China: history, current situation and challenges. Popul Health Metr. 2005;3 : 3. doi: 10.1186/1478-7954-3-3 15769298
19. Zhou M, Jiang Y, Huang Z, Wu F. Adjustment and representativeness evaluation of national disease surveillance points system. Dis Surveill. 2010;25 : 239–44.
20. Yang G, Zhen X, Zeng G, Wang L, Chen Y, Chen A, et al. Selection of DSP points in second stage and their presentation. Zhonghua Liu Xing Bing Xue Za Zhi. 1992;13 : 197–201. 1301261
21. Mooney P. Counting the dead in China. Bull World Health Organ. 2006;84 : 168–9. doi: /S0042-96862006000300007 16583071
22. Liu MB, Wang W, Zhou MG. Trend analysis on the mortality of cardiovascular diseases from 2004 to 2010 in China. Zhonghua Liu Xing Bing Xue Za Zhi. 2013;34 : 985–8. 24377992
23. Zhang H, Huang F, Chen W, Du X, Zhou MG, Hu J, et al. Estimates of tuberculosis mortality rates in China using the Disease Surveillance Point System, 2004–2010. Biomed Environ Sci. 2012;25 : 483–8. doi: 10.3967/0895-3988.2012.04.015 23026530
24. Chinese Center for Disease Control and Prevention National Center for Chronic and Noncommunicable Disease Control and Prevention. Data sets of death cause surveillance in disease surveillance points system, 2013. Beijing: Popular Science Press; 2015.
25. Wang L, Wang LJ, Cai Y, Ma LM, Zhou MG. Analysis of under-reporting of mortality surveillance from 2006 to 2008 in China. Zhonghua Yu Fang Yi Xue Za Zhi. 2011;45 : 1061–4. 22336336
26. Faul M, Xu L, Wald MM, Coronado VG. Traumatic brain injury in the United States: emergency department visits, hospitalizations and deaths 2002–2006. Atlanta: US Centers for Disease Control and Prevention; 2010.
27. Thurman DJ, Sniezek JE, Johnson D, Greenspan A, Smith SM. Guidelines for surveillance of central nervous system injury. Washington (DC): US Department of Health and Human Services; 1995.
28. Coronado VG, Xu L, Basavaraju SV, McGuire LC, Wald MM, Faul MD, et al. Surveillance for traumatic brain injury-related deaths—United States, 1997–2007. MMWR Surveill Summ. 2011;60 : 1–32.
29. US Centers for Disease Control and Prevention. External cause of injury mortality matrix for ICD-10. Available from: https://www.cdc.gov/nchs/data/ice/icd10_transcode.pdf. Accessed 2017 Mar 28.
30. Adams RS, Larson MJ, Corrigan JD, Ritter GA, Williams TV. Traumatic brain injury among U.S. active duty military personnel and negative drinking-related consequences. Subst Use Misuse. 2013;48 : 821–36. doi: 10.3109/10826084.2013.797995 23869456
31. Statistical Consulting Group. Negative binomial regression: Stata annotated output. Available from: https://stats.idre.ucla.edu/stata/output/negative-binomial-regression/. Accessed 2017 Jun 1.
32. Nicodemus KK, Marenco S, Batten AJ, Vakkalanka R, Egan MF, Straub RE, et al. Serious obstetric complications interact with hypoxia-regulated/vascular-expression genes to influence schizophrenia risk. Mol Psychiatry. 2008;13(9):873–7. doi: 10.1038/sj.mp.4002153 18195713
33. Chinese Center for Disease Control and Prevention National Center for Chronic and Noncommunicable Disease Control and Prevention. Data sets of death cause surveillance in disease surveillance points system, 2008. Beijing: People’s Medical Publishing House Press; 2010.
34. Ning P, Schwebel DC, Huang H, Li L, Li J, Hu G. Global progress in road injury mortality since 2010. PLoS ONE. 2016;11:e0164560. doi: 10.1371/journal.pone.0164560 27727318
35. Huang H, Yin Q, Schwebel DC, Li L, Hu G. Examining road traffic mortality status in China: a simulation study. PLoS ONE. 2016;11:e0153251. doi: 10.1371/journal.pone.0153251 27071008
36. Firsching R, Woischneck D. Present status of neurosurgical trauma in Germany. World J Surg. 2001;25 : 1221–3. 11571961
37. Hyder AA, Wunderlich CA, Puvanachandra P, Gururaj G, Kobusingye OC. The impact of traumatic brain injuries: a global perspective. Neurorehabilitation. 2007;22 : 341–53. 18162698
38. Nguyen R, Fiest KM, Mcchesney J, Kwon CS, Jette N, Frolkis AD, et al. the international incidence of traumatic brain injury: a systematic review and meta-analysis. Can J Neurol Sci. 2016;43 : 774–85. doi: 10.1017/cjn.2016.290 27670907
39. Ning P, Schwebel DC, Hu G. Healthy China 2030: a missed opportunity for injury control. Inj Prev. 2017 Feb 23. doi: doi: 10.1136/injuryprev-2017-042314 28232400
40. Hu G, Baker TD, Baker SP. Injury control in China: priorities and actions. Lancet. 2009;373 : 214.
41. Hu G, Baker TD, Li G, Baker SP. Injury control: an opportunity for China. Inj Prev. 2008;14 : 129–30. doi: 10.1136/ip.2007.017822 18388234
42. Yang D, Wang X, Hu W, Lv Z. Analysis of response ability of prehospital emergency from 2009 to 2012 in Fangshan, Beijing. Chin J Crit Care Med. 2013;33(12):1130–3.
43. National Health and Family Planning Commission of the People’s Republic of China. Chinese health statistics yearbook 2007. Beijing: Peking Union Medical College Press; 2007.
44. National Health and Family Planning Commission of the People’s Republic of China. Chinese health statistics yearbook 2014. Beijing: Peking Union Medical College Press; 2014.
45. Roozenbeek B, Maas AI, Menon DK. Changing patterns in the epidemiology of traumatic brain injury. Nat Rev Neurol. 2013;9 : 231–6. doi: 10.1038/nrneurol.2013.22 23443846
46. Barr GC Jr, Kane KE, Barraco RD, Rayburg T, Demers L, Kraus CK, et al. Gender differences in perceptions and self-reported driving behaviors among teenagers. J Emerg Med. 2015;48 : 366–70.e3. doi: 10.1016/j.jemermed.2014.09.055 25497842
47. Riesch SK, Kedrowski K, Brown RL, Temkin BM, Wang K, Henriques J, et al. Health-risk behaviors among a sample of US pre-adolescents: types, frequency, and predictive factors. Int J Nurs Stud. 2013;50 : 1067–79. doi: 10.1016/j.ijnurstu.2012.10.012 23177901
48. Reidy DE, Berke DS, Gentile B, Zeichner A. Masculine discrepancy stress, substance use, assault and injury in a survey of US men. Inj Prev. 2016;22 : 370–4. doi: 10.1136/injuryprev-2015-041599 26303670
49. Kessaram T, McKenzie J, Girin N, Roth A, Vivil P, Williams G, et al. Alcohol use in the Pacific region: results from the STEPwise approach to surveillance, Global School-Based Student Health Survey and Youth Risk Behavior Surveillance System. Drug Alcohol Rev. 2016;35 : 412–23. doi: 10.1111/dar.12328 26358376
50. Asbridge M, Payne E, Cartwright J, Mann R. Driving under the influence of alcohol: examining ethno-specific rates and the mediating effects of psychological distress and harmful and problematic drinking. Accid Anal Prev. 2010;42 : 1408–15. doi: 10.1016/j.aap.2010.03.005 20441859
51. Hu G, Baker SP, Baker TD. Urban–rural disparities in injury mortality in China, 2006. J Rural Health. 2010;26 : 73–7. doi: 10.1111/j.1748-0361.2009.00255.x 20105271
52. D’Souza AJ, Blakely TA, Woodward A. The effect of eradicating poverty on childhood unintentional injury mortality in New Zealand: a cohort study with counterfactual modelling. J Epidemiol Community Health. 2008;62 : 899–904. doi: 10.1136/jech.2007.068072 18413434
53. Tian D, Sun L, Zhang L, Zhang L, Zhang W, Li L, et al. Large urban-rural disparity in the severity of two-week illness: updated results based on the first health service survey of Hunan Province, China. Int J Equity health. 2016;15 : 37. doi: 10.1186/s12939-016-0330-z 26926446
54. Huang Y, Tian D, Gao L, Li L, Deng X, Mamady K, et al. Neglected increases in rural road traffic mortality in China: findings based on health data from 2005 to 2010. BMC Public Health. 2013;13 : 1111. doi: 10.1186/1471-2458-13-1111 24289458
55. Song SY, Lee SK, Eom KS, KNTDB Investigators. Analysis of mortality and epidemiology in 2617 cases of traumatic brain injury: Korean Neuro-Trauma Data Bank System 2010–2014. J Korean Neurosurg Soc. 2016;59 : 485–91. doi: 10.3340/jkns.2016.59.5.485 27651867
56. Global Burden of Disease Study 2013 Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 301 acute and chronic diseases and injuries in 188 countries, 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2015;386 : 743–800. doi: 10.1016/S0140-6736(15)60692-4 26063472
57. Hu G, Baker T, Baker SP. Comparing road traffic mortality rates from police-reported data and death registration data in China. Bull World Health Organ. 2011;89 : 41–5. doi: 10.2471/BLT.10.080317 21346889
58. Alcorn T. Uncertainty clouds China’s road-traffic fatality data. Lancet. 2011;378 : 305–6. 21789786
59. Judge JO, Lindsey C, Underwood M, Winsemius D. Balance improvements in older women: effects of exercise training. Phys Ther. 1993;73 : 254–62. 8456144
60. Lord SR, Caplan GA, Ward JA. Balance, reaction time, and muscle strength in exercising older women: a pilot study. Arch Phys Med Rehabil. 1993;74 : 837–9. 8347068
61. Campbell AJ, Robertson MC, Gardner MM, Norton RN, Buchner DM. Falls prevention over 2 years: a randomized controlled trial in women 80 years and older. Age Ageing. 1999;28 : 513–8. 10604501
62. Mack MG, Sacks JJ, Thompson D. Testing the impact attenuation of loose fill playground surfaces. Inj Prev. 2000;6 : 141–4. doi: 10.1136/ip.6.2.141 10875672
63. World Health Organization. WHO global report on falls prevention in older age. Geneva: World Health Organization; 2007.
64. Li L, Scherpbier R, Wu J, Zhu X, Zhang W, Zhang L, et al. Legislation coverage for child injury prevention in China. Bull World Health Organ. 2015;93 : 169–75. doi: 10.2471/BLT.14.139998 25838612
65. Sasser SM, Varghese M, Joshipura M, Kellermann A. Preventing death and disability through the timely provision of prehospital trauma care. Bull World Health Organ. 2006;84(7):507. 16878215
66. Sasser S, Varghese M, Kellermann A, Lormand JD. Pre-hospital trauma care systems. Geneva: World Health Organization; 2005.
67. Michael YL, Whitlock EP, Lin JS, Fu R, O’Connor EA, Gold R. Primary care-relevant interventions to prevent falling in older adults: a systematic evidence review for the U.S. Preventive Services Task Force. Ann Intern Med. 2010;153(12):815–25. doi: 10.7326/0003-4819-153-12-201012210-00008 21173416
68. World Health Organization. Pedestrian safety: a road safety manual for decision-makers and practitioners. Geneva: World Health Organization; 2013.
69. World Health Organization. Make walking safe: a brief overview of pedestrian safety around the world. Geneva: World Health Organization; 2013.
70. US Centers for Disease Control and Prevention. CDC WONDER. Available from: http://wonder.cdc.gov/. Accessed 2017 Apr 2.
71. Zhou MG, Wang YY, Ge H, Wang LJ, Ma JQ, Yang GH. Study on the quality of death-case-reporting-system in county and above levels’ medical institutions in 2004. Zhonghua Liu Xing Bing Xue Za Zhi. 2006;27 : 328–32. 16875538
72. Wang LJ, Ma JQ, Zhou MG, Wang YY, Ge H, Yang GH. Study on the evaluation of underreporting and the quality of death cases reporting system, from medical institutions at county level and above, in 2005. Zhonghua Liu Xing Bing Xue Za Zhi. 2007;28 : 571–5. 17939387
Štítky
Interní lékařství
Článek vyšel v časopisePLOS Medicine
Nejčtenější tento týden
2017 Číslo 7- Berberin: přírodní hypolipidemikum se slibnými výsledky
- Léčba bolesti u seniorů
- Příznivý vliv Armolipidu Plus na hladinu cholesterolu a zánětlivé parametry u pacientů s chronickým subklinickým zánětem
- Jak postupovat při výběru betablokátoru − doporučení z kardiologické praxe
- Červená fermentovaná rýže účinně snižuje hladinu LDL cholesterolu jako vhodná alternativa ke statinové terapii
-
Všechny články tohoto čísla
- Time for trauma immunology
- Translational approaches to coagulopathy after trauma: Towards targeted treatment
- The new survivors and a new era for trauma research
- Research questions in pre-hospital trauma care
- Major scientific lessons learned in the trauma field over the last two decades
- The science of rapid start—From the when to the how of antiretroviral initiation
- Reducing undiagnosed HIV infection among adolescents in sub-Saharan Africa: Provider-initiated and opt-out testing are not enough
- Community and health system intervention to reduce disrespect and abuse during childbirth in Tanga Region, Tanzania: A comparative before-and-after study
- Prescription medicine use by pedestrians and the risk of injurious road traffic crashes: A case-crossover study
- Trauma care: Finding a better way
- Risk of surgical site infection, acute kidney injury, and infection following antibiotic prophylaxis with vancomycin plus a beta-lactam versus either drug alone: A national propensity-score-adjusted retrospective cohort study
- Ammonium tetrathiomolybdate following ischemia/reperfusion injury: Chemistry, pharmacology, and impact of a new class of sulfide donor in preclinical injury models
- Years of life lost due to traumatic brain injury in Europe: A cross-sectional analysis of 16 countries
- Antimicrobial resistance in : Global surveillance and a call for international collaborative action
- Signatures of inflammation and impending multiple organ dysfunction in the hyperacute phase of trauma: A prospective cohort study
- Cellular therapies in trauma and critical care medicine: Looking towards the future
- Leveraging peer-based support to facilitate HIV care in Kenya
- Trends in traumatic brain injury mortality in China, 2006–2013: A population-based longitudinal study
- Temporal profile of intracranial pressure and cerebrovascular reactivity in severe traumatic brain injury and association with fatal outcome: An observational study
- Community health promotion and medical provision for neonatal health—CHAMPION cluster randomised trial in Nagarkurnool district, Telangana (formerly Andhra Pradesh), India
- A comparison of Selective Aortic Arch Perfusion and Resuscitative Endovascular Balloon Occlusion of the Aorta for the management of hemorrhage-induced traumatic cardiac arrest: A translational model in large swine
- Risk of hospitalization with neurodegenerative disease after moderate-to-severe traumatic brain injury in the working-age population: A retrospective cohort study using the Finnish national health registries
- Ultrasound non-invasive measurement of intracranial pressure in neurointensive care: A prospective observational study
- Cancer trials in sub-Saharan Africa: Aligning research and care
- Prehospital immune responses and development of multiple organ dysfunction syndrome following traumatic injury: A prospective cohort study
- Patient-reported outcomes and survival in multiple sclerosis: A 10-year retrospective cohort study using the Multiple Sclerosis Impact Scale–29
- Cerebrovascular pressure reactivity monitoring using wavelet analysis in traumatic brain injury patients: A retrospective study
- Validation of the sensitivity of the National Emergency X-Radiography Utilization Study (NEXUS) Head computed tomographic (CT) decision instrument for selective imaging of blunt head injury patients: An observational study
- Same-day HIV testing with initiation of antiretroviral therapy versus standard care for persons living with HIV: A randomized unblinded trial
- Community burden of undiagnosed HIV infection among adolescents in Zimbabwe following primary healthcare-based provider-initiated HIV testing and counselling: A cross-sectional survey
- Timing of femoral shaft fracture fixation following major trauma: A retrospective cohort study of United States trauma centers
- IL33-mediated ILC2 activation and neutrophil IL5 production in the lung response after severe trauma: A reverse translation study from a human cohort to a mouse trauma model
- Long-term health status and trajectories of seriously injured patients: A population-based longitudinal study
- Multidrug-resistant gonorrhea: A research and development roadmap to discover new medicines
- PLOS Medicine
- Archiv čísel
- Aktuální číslo
- Informace o časopisu
Nejčtenější v tomto čísle- Signatures of inflammation and impending multiple organ dysfunction in the hyperacute phase of trauma: A prospective cohort study
- Multidrug-resistant gonorrhea: A research and development roadmap to discover new medicines
- Patient-reported outcomes and survival in multiple sclerosis: A 10-year retrospective cohort study using the Multiple Sclerosis Impact Scale–29
- Ammonium tetrathiomolybdate following ischemia/reperfusion injury: Chemistry, pharmacology, and impact of a new class of sulfide donor in preclinical injury models
Kurzy
Zvyšte si kvalifikaci online z pohodlí domova
Současné možnosti léčby obezity
nový kurzAutoři: MUDr. Martin Hrubý
Všechny kurzyPřihlášení#ADS_BOTTOM_SCRIPTS#Zapomenuté hesloZadejte e-mailovou adresu, se kterou jste vytvářel(a) účet, budou Vám na ni zaslány informace k nastavení nového hesla.
- Vzdělávání



