-
Články
Top novinky
Reklama- Vzdělávání
- Časopisy
Top články
Nové číslo
- Témata
Top novinky
Reklama- Videa
- Podcasty
Nové podcasty
Reklama- Kariéra
Doporučené pozice
Reklama- Praxe
Top novinky
ReklamaThe Effectiveness of Mobile-Health Technology-Based Health Behaviour Change or Disease Management Interventions for Health Care Consumers: A Systematic Review
Background:
Mobile technologies could be a powerful media for providing individual level support to health care consumers. We conducted a systematic review to assess the effectiveness of mobile technology interventions delivered to health care consumers.Methods and Findings:
We searched for all controlled trials of mobile technology-based health interventions delivered to health care consumers using MEDLINE, EMBASE, PsycINFO, Global Health, Web of Science, Cochrane Library, UK NHS HTA (Jan 1990–Sept 2010). Two authors extracted data on allocation concealment, allocation sequence, blinding, completeness of follow-up, and measures of effect. We calculated effect estimates and used random effects meta-analysis. We identified 75 trials. Fifty-nine trials investigated the use of mobile technologies to improve disease management and 26 trials investigated their use to change health behaviours. Nearly all trials were conducted in high-income countries. Four trials had a low risk of bias. Two trials of disease management had low risk of bias; in one, antiretroviral (ART) adherence, use of text messages reduced high viral load (>400 copies), with a relative risk (RR) of 0.85 (95% CI 0.72–0.99), but no statistically significant benefit on mortality (RR 0.79 [95% CI 0.47–1.32]). In a second, a PDA based intervention increased scores for perceived self care agency in lung transplant patients. Two trials of health behaviour management had low risk of bias. The pooled effect of text messaging smoking cessation support on biochemically verified smoking cessation was (RR 2.16 [95% CI 1.77–2.62]). Interventions for other conditions showed suggestive benefits in some cases, but the results were not consistent. No evidence of publication bias was demonstrated on visual or statistical examination of the funnel plots for either disease management or health behaviours. To address the limitation of the older search, we also reviewed more recent literature.Conclusions:
Text messaging interventions increased adherence to ART and smoking cessation and should be considered for inclusion in services. Although there is suggestive evidence of benefit in some other areas, high quality adequately powered trials of optimised interventions are required to evaluate effects on objective outcomes.
Please see later in the article for the Editors' Summary
Published in the journal: . PLoS Med 10(1): e32767. doi:10.1371/journal.pmed.1001362
Category: Research Article
doi: https://doi.org/10.1371/journal.pmed.1001362Summary
Background:
Mobile technologies could be a powerful media for providing individual level support to health care consumers. We conducted a systematic review to assess the effectiveness of mobile technology interventions delivered to health care consumers.Methods and Findings:
We searched for all controlled trials of mobile technology-based health interventions delivered to health care consumers using MEDLINE, EMBASE, PsycINFO, Global Health, Web of Science, Cochrane Library, UK NHS HTA (Jan 1990–Sept 2010). Two authors extracted data on allocation concealment, allocation sequence, blinding, completeness of follow-up, and measures of effect. We calculated effect estimates and used random effects meta-analysis. We identified 75 trials. Fifty-nine trials investigated the use of mobile technologies to improve disease management and 26 trials investigated their use to change health behaviours. Nearly all trials were conducted in high-income countries. Four trials had a low risk of bias. Two trials of disease management had low risk of bias; in one, antiretroviral (ART) adherence, use of text messages reduced high viral load (>400 copies), with a relative risk (RR) of 0.85 (95% CI 0.72–0.99), but no statistically significant benefit on mortality (RR 0.79 [95% CI 0.47–1.32]). In a second, a PDA based intervention increased scores for perceived self care agency in lung transplant patients. Two trials of health behaviour management had low risk of bias. The pooled effect of text messaging smoking cessation support on biochemically verified smoking cessation was (RR 2.16 [95% CI 1.77–2.62]). Interventions for other conditions showed suggestive benefits in some cases, but the results were not consistent. No evidence of publication bias was demonstrated on visual or statistical examination of the funnel plots for either disease management or health behaviours. To address the limitation of the older search, we also reviewed more recent literature.Conclusions:
Text messaging interventions increased adherence to ART and smoking cessation and should be considered for inclusion in services. Although there is suggestive evidence of benefit in some other areas, high quality adequately powered trials of optimised interventions are required to evaluate effects on objective outcomes.
Please see later in the article for the Editors' SummaryIntroduction
Each year, worldwide, over 22 million people die from diseases such as cardiovascular disease, chronic obstructive pulmonary disease, HIV, lung cancer, and diabetes mellitus [1]. The majority of deaths (83%) occur in low - and middle-income countries; however, these are also important causes of mortality in high-income countries, accounting for about 39% of deaths [1].
Health care consumers adopting healthy behaviours can prevent the onset of many of these leading causes of mortality. Ten years after stopping smoking, the risk of lung cancer is half of that of those continuing smoking and 15 y after stopping smoking the risk of cardiovascular disease is similar to that of those who never smoked [2]. HIV can be prevented by adopting safer sexual practices [3]. In people who are overweight, weight loss can reduce the incidence of diabetes [4].
Optimal treatment of existing diseases can also reduce mortality and morbidity. In patients with existing coronary heart disease long term anti-platelet therapy reduces major vascular events (myocardial infarction, stroke, or vascular mortality) by about a quarter [5], ACE inhibitors reduce cardiovascular mortality by just under a fifth [6], beta blockers reduce mortality by almost a quarter [7], and lipid lowering therapy reduces coronary mortality by about a fifth [8]. Antiretroviral medication delays the progression of HIV infection [9]. Good control of diabetes reduces the onset of retinopathy by half and reduces the onset of nephropathy by two-thirds [10].
Optimal treatment of existing diseases requires the involvement of health care consumers in managing aspects of their disease. Health care consumers decide whether to adhere to prescribed medication and determine when they seek health care [11]. Involving health care consumers in self-management of diseases such as in monitoring their health/disease status and adjusting their medication dosage (e.g., insulin or asthma medications) can improve health outcomes [12]–[14].
An important function of health care services is therefore to encourage and support health care consumers to adopt healthy behaviours and to self-manage chronic diseases. However, the amount of information, encouragement, and support that can be conveyed during consultations, within existing service infrastructures or through other traditional media (such as leaflets), is limited.
Mobile technologies are a means for providing individual level support to health care consumers. Mobile health interventions for health care consumers have been designed to increase healthy behaviour (for example, to increase smoking cessation or activity levels) or improve disease management (for example, by increasing adherence to prescribed medication, improving management of diabetes or asthma, or delivering therapeutic interventions).
Mobile technologies include mobile phones; personal digital assistants (PDAs) and PDA phones (e.g., BlackBerry, Palm Pilot); smartphones (e.g., iPhone); enterprise digital assistants (EDAs); portable media players (i.e., MP3-players, MP4-players, e.g., ipod); handheld video-game consoles (e.g., Playstation Portable [PSP], Nintendo DS); handheld and ultra-portable computers such as tablet PCs (e.g., iPad), and Smartbooks.
These devices have a range of functions from mobile cellular communication using text messages (SMS), photos and video (MMS), telephone, and World Wide Web access, to multi-media playback and software application support. Technological advances and improved computer processing power mean that single mobile devices such as smart phones and PDA phones are increasingly capable of high level performance in many or all of these functions.
The features of mobile technologies that may make them particularly appropriate for providing individual level support to health care consumers relate to their popularity, their mobility, and their technological capabilities. The popularity of mobile technologies has led to high and increasing ownership of mobile technologies, which means interventions can be delivered to large numbers of people. In 2009, more than two-thirds of the world's population owned a mobile phone and 4.2 trillion text messages were sent [15]. In many high-income countries, the number of mobile phone subscriptions outstrips the population [16]. In low-income countries, mobile communication technology is the fastest growing sector of the communications industry and geographical coverage is high [17]–[20].
Mobile technologies are mobile and popular, such that many people carry their mobile phone with them wherever they go. This allows temporal synchronisation of the intervention delivery and allows the intervention to claim people's attention when it is most relevant. For example, health care consumers can be sent messages designed to sustain their motivation to quit smoking throughout the day. Temporal synchronisation of the intervention delivery also allows interventions to be accessed or delivered within the relevant context, i.e., the intervention can be delivered at any time and extra support can be requested wherever and whenever it is needed. For example smokers trying to quit can send text messages requesting extra support while they are experiencing cravings due to withdrawal from nicotine, or those with asthma can access advice regarding how to increase the use of inhalers during an exacerbation of asthma.
The technological capabilities of mobile technologies are continuing to advance at a high pace. Current technological capabilities allow low cost interventions. There are potential economies of scale as it is technically easy to deliver interventions to large populations (for example, mobile technology applications can easily be downloaded and automated systems can deliver text messages to large numbers of people at low cost). The technological functions that have been utilised for health care consumers include text messages (SMS), software applications, and multiple media (SMS, photos) interventions. The technology supports interactivity, which allows people to obtain extra help when needed [21],[22]. Motivational messages, monitoring, and behaviour change tools used in face-to-face support can be modified for delivery via mobile phones. Interventions can be personalised with the content tailored to the age, sex, and ethnic group of the participant or to the issues they face [21],[22].
Existing systematic reviews of M-health interventions focus on the application of specific devices (e.g., mobile phones [23]–[27], specific mobile technology functions (e.g., text messaging [28]–[30]), or individual diseases or types of illness (e.g., diabetes care or chronic disease management [26],[30],[31]). These reviews require updating. Some types of interventions for health care consumers targeting healthy behaviour or disease management have not been covered by previous reviews. A comprehensive review of interventions delivered to health care consumers is lacking and provides a valuable overview of the existing evidence.
This systematic review aimed to quantify the effectiveness of mobile technology-based interventions delivered to health care consumers for health behaviour change and management of diseases.
Methods
We adhered to our published plan of investigation as outlined in the study protocol [32].
Participants were men and women of any age. We included all controlled trials employing any mobile technology interventions (mobile phones; PDAs and PDA phones [e.g., BlackBerry, Palm Pilot]; smartphones [e.g., iphone]; enterprise digital assistants [EDAs]; portable media players [i.e., MP3-players and MP4-players, e.g., ipod]; handheld video-game consoles [e.g., Playstation Portable (PSP), Nintendo DS]; handheld and ultra-portable computers such as tablet PCs [e.g., ipad and Smartbooks]) to improve or promote health or health service use or quality. Trials were included regardless of publication status or language.
We included studies in which the intervention delivered by mobile technology was the primary intervention component under evaluation. We excluded studies evaluating either mixed mobile technology and non-mobile technology based interventions in which the treatment and control group both received the mobile technology-based component or interventions in which treatments between the treatment and control groups differed in additional ways besides the components delivered by mobile technology, such as interventions involving face-to-face counselling with a text message intervention compared to a control group receiving information only. We included trials of immunisation reminders; trials of general appointment reminders are reported elsewhere [33].
The interventions in trials meeting the inclusion criteria and targeting health behaviour change or disease management interventions for health care consumers are reported here. Other trials identified targeted data collection or health care delivery processes, such as those directed to health care providers (e.g., for diagnosis and management) or those involving communication between health care services and health care consumers (e.g., appointment reminders, test result notification). These are reported in two separate articles [33]. No trial was excluded from the review based on the type of health or health care service targeted.
Primary outcomes were defined as any objective measure of health or health service delivery or use. Secondary outcomes were defined as the following: self-reported outcomes related to health behaviours, disease management, health service delivery or use, and cognitive outcomes. Outcomes reported for any length of follow-up were included.
We searched the following electronic bibliographic databases MEDLINE, EMBASE, PsycINFO, Global Health, The Cochrane Library (Cochrane Database of Systematic Reviews, Cochrane Central Register of Controlled Trials [CENTRAL], Cochrane Methodology Register), NHS Health Technology Assessment Database, and Web of Science (science and social science citation index) from 1990 to Sept 2010 and the reference lists of included trials. The list of subheadings (MeSH) and textwords used in the search strategy can be found in Text S3. All of these terms were combined with the Cochrane Library MEDLINE filter for controlled trials of interventions.
Two reviewers independently scanned the electronic records to identify potentially eligible trials.
Two reviewers independently extracted data on number of randomised participants, intervention, intervention components, mobile devices employed, mobile technology functions used, sequence generation, allocation concealment, blinding of outcome assessors, completeness of follow-up, evidence of selective outcome reporting, any other potential sources of bias, and measures of effect using a standardised data extraction form. The authors were not blinded to authorship, journal of publication, or the trial results. All discrepancies were agreed by discussion with a third reviewer. The behaviour change techniques used in behaviour change interventions were classified according to Abraham and Michie's taxonomy of behaviour change techniques [34]. Risk of bias was assessed according to the criteria outlined by the International Cochrane Collaboration [35]. We assessed blinding of outcome assessors and data analysts and we used a cut off of 90% complete follow-up for low risk of bias for completeness of follow-up. We contacted study authors for additional information about the included studies, or for clarification of the study methods as required.
All analyses were conducted in STATA v 11. We calculated risk ratios and standard mean differences. We used random effects meta-analysis to give pooled estimates where there were two or more trials using the same mobile technology function (e.g., SMS messages) and targeting the same disease (e.g., diabetes control) or behaviour (e.g., activity) and reporting the same outcome. We examined heterogeneity visually by examining the forest plots and statistically using both the χ2 test and the I2 statistic. We assessed evidence of publication bias using Funnel plots.
Results
The combined search strategies identified 26,221 electronic records, which were screened for eligibility (Figure 1). The full texts of 334 potentially eligible reports were obtained for further assessment. Out of the 334 potentially eligible reports, 75 met the study inclusion criteria and were trials delivered to health care consumers; 26 interventions aimed to increase healthy behaviours, such as stopping smoking or increasing activity, which can prevent the onset or progression of disease (health behaviour change interventions); and 49 targeted disease management, including interventions designed to improve self-management of diseases like diabetes, and therapeutic interventions, such as interventions providing psychological support.
Fig. 1. PRISMA 2009 flow diagram. 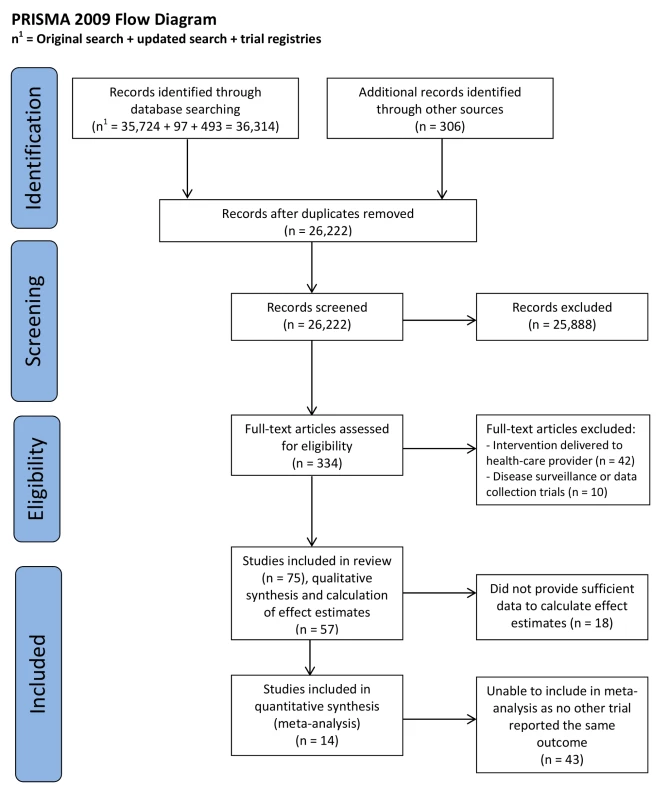
Characteristics of Studies
Health behaviour change
The health behaviour change trials included 10,706 participants. Sample sizes ranged from 17 to 5,800. There were 26 randomised controlled trials with parallel groups, and one non-randomised controlled trial. There were five trials aiming to increase smoking cessation (Table 1), seven trials aimed to increase physical activity (Table 2), three trials aimed to reduce calorie intake (Table 2), seven trials aimed to increase physical activity and reduce calorie intake (Table 2), three trials aimed to increase safer sexual behaviour (Table 3), and one trial aimed to reduce alcohol consumption (Table 3).
Tab. 1. Description of trials of smoking cessation interventions. Health behaviour change: smoking-related studies. 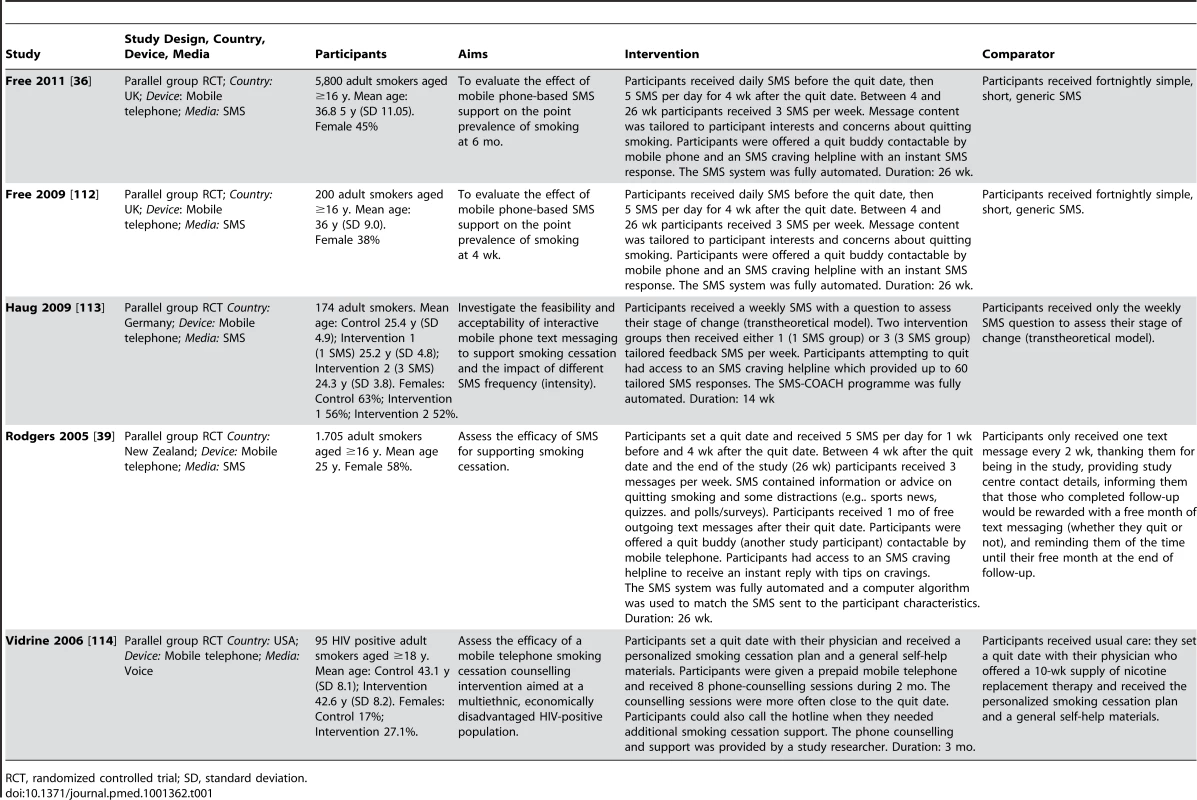
RCT, randomized controlled trial; SD, standard deviation. Tab. 2. Description of trials of interventions targeting physical activity, diet, and physical activity and diet combined. 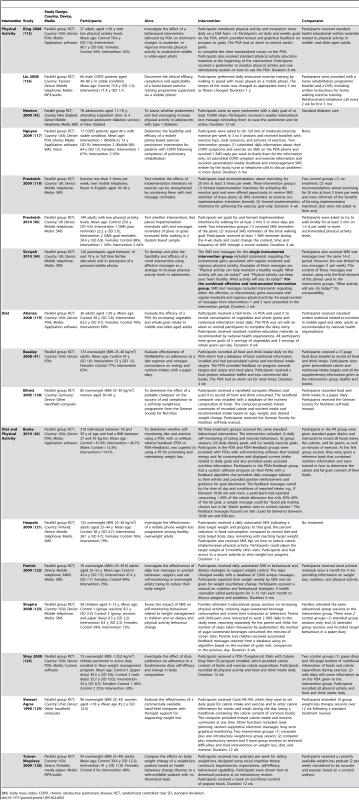
BMI, body mass index; COPD, chronic obstructive pulmonary disease; RCT, randomized controlled trial; SD, standard deviation. Tab. 3. Description of trials of sexual health and alcohol reduction interventions. 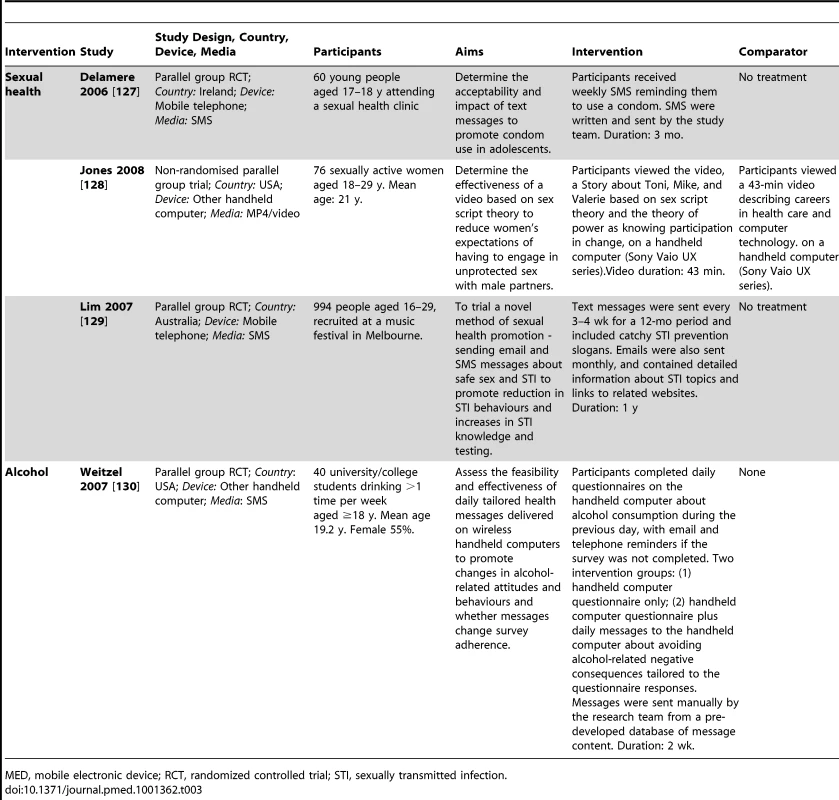
MED, mobile electronic device; RCT, randomized controlled trial; STI, sexually transmitted infection. All trials were conducted in high-income countries.
Disease management
The 49 disease management trials recruited 6,832 participants with sample sizes ranging from 16 to 273 participants. Thirty-four were randomised controlled trials with parallel groups, three were cluster randomised controlled trials, five were crossover trials, and seven were non-randomised parallel group trials. Nine trials aimed to improve the management of illnesses presenting acutely. Of these nine trials, seven provided cardiopulmonary resuscitation instruction (Table 4), one provided the information required by a lay-helper to manage an emergency, and one provided accident and emergency department discharge information for sprains and lacerations. For chronic conditions six trials aimed to increase adherence to medication (Table 5). Thirteen trials aimed to improve diabetes control (Table 6), six aimed to improve asthma control (Table 7), and two aimed to improve hypertension control (Table 8). Seven interventions provided psychological support (Table 9). One trial aimed to increase self-care behaviours in patients following a lung transplant, one trial aimed to improve monitoring and provide appropriate advice regarding chemotherapy-related toxicity symptoms, one trial aimed to monitor vital parameters (e.g., blood pressure, heart rate, weight) and provide appropriate advice to people with heart failure, one trial aimed to monitor home care blood transfusions in people with severe haemophilia so the clinic could be alerted regarding “significant” bleeds. One trial aimed to improve the recall of rehabilitation goals in people with acquired head injury by sending text messages regarding their goals. These varied trials are described in Table 10.
Tab. 4. Description of trials of cardiopulmonary resuscitation interventions. 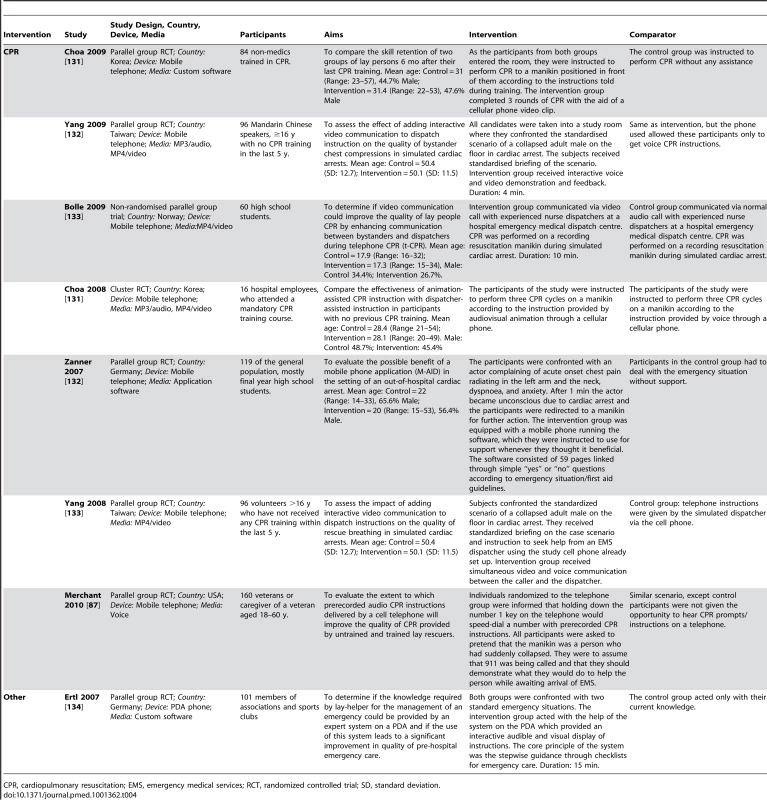
CPR, cardiopulmonary resuscitation; EMS, emergency medical services; RCT, randomized controlled trial; SD, standard deviation. Tab. 5. Description of trials targeting medication adherence. 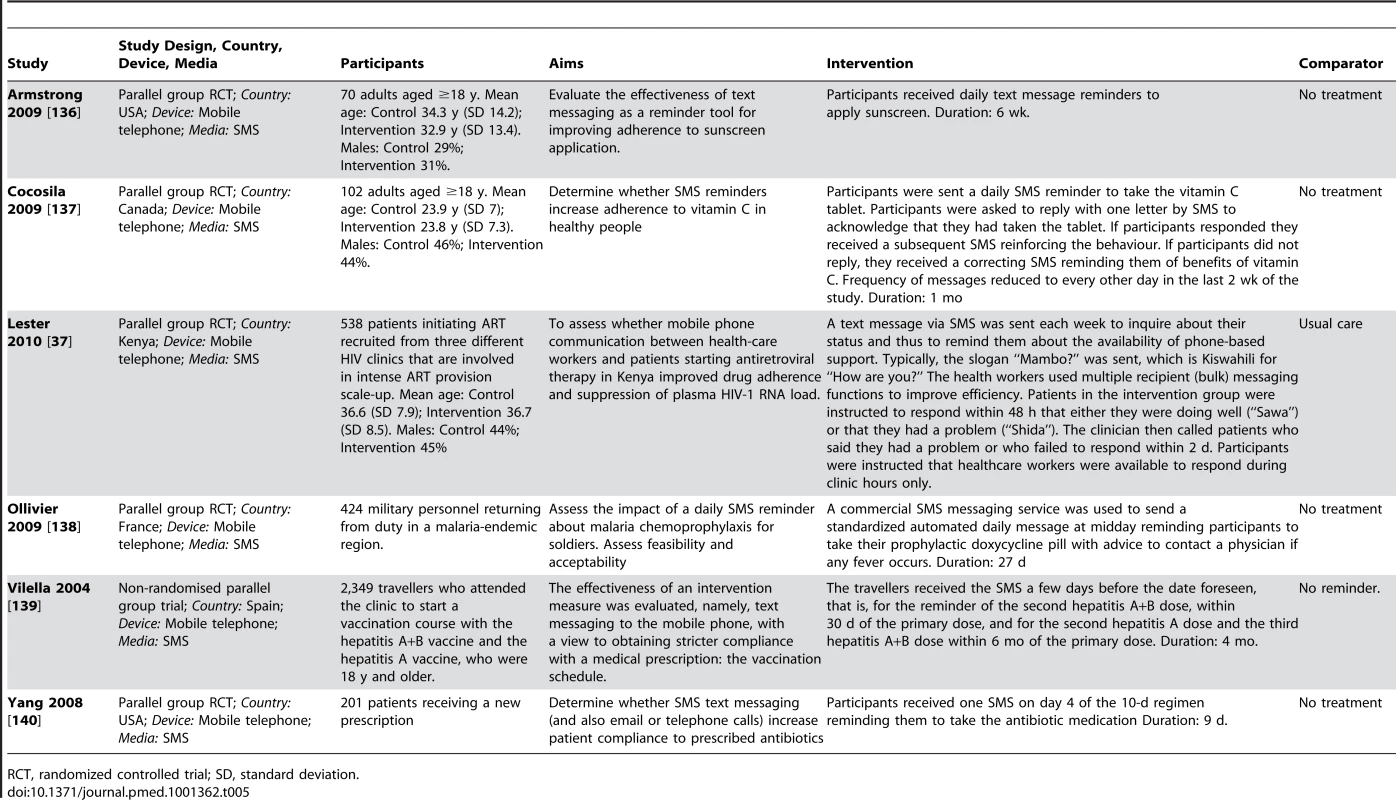
RCT, randomized controlled trial; SD, standard deviation. Tab. 6. Description of trials of diabetes management interventions. 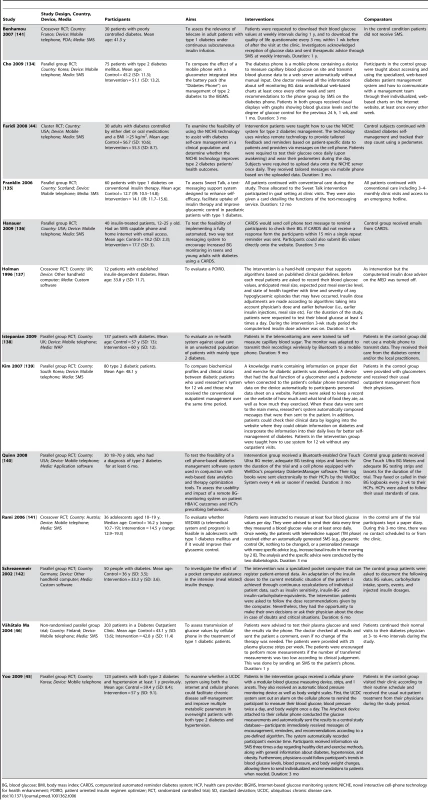
BG, blood glucose; BMI, body mass index; CARDS, computerized automated reminder diabetes system; HCP, health care provider; IBGMS, Internet-based glucose monitoring system; NICHE, novel interactive cell-phone technology for health enhancement; POIRO, patient oriented insulin regimen optimizer; RCT, randomized controlled trial; SD, standard deviation; UCDC, ubiquitous chronic disease care. Tab. 7. Description of trials of asthma and chronic obstructive pulmonary disease interventions. 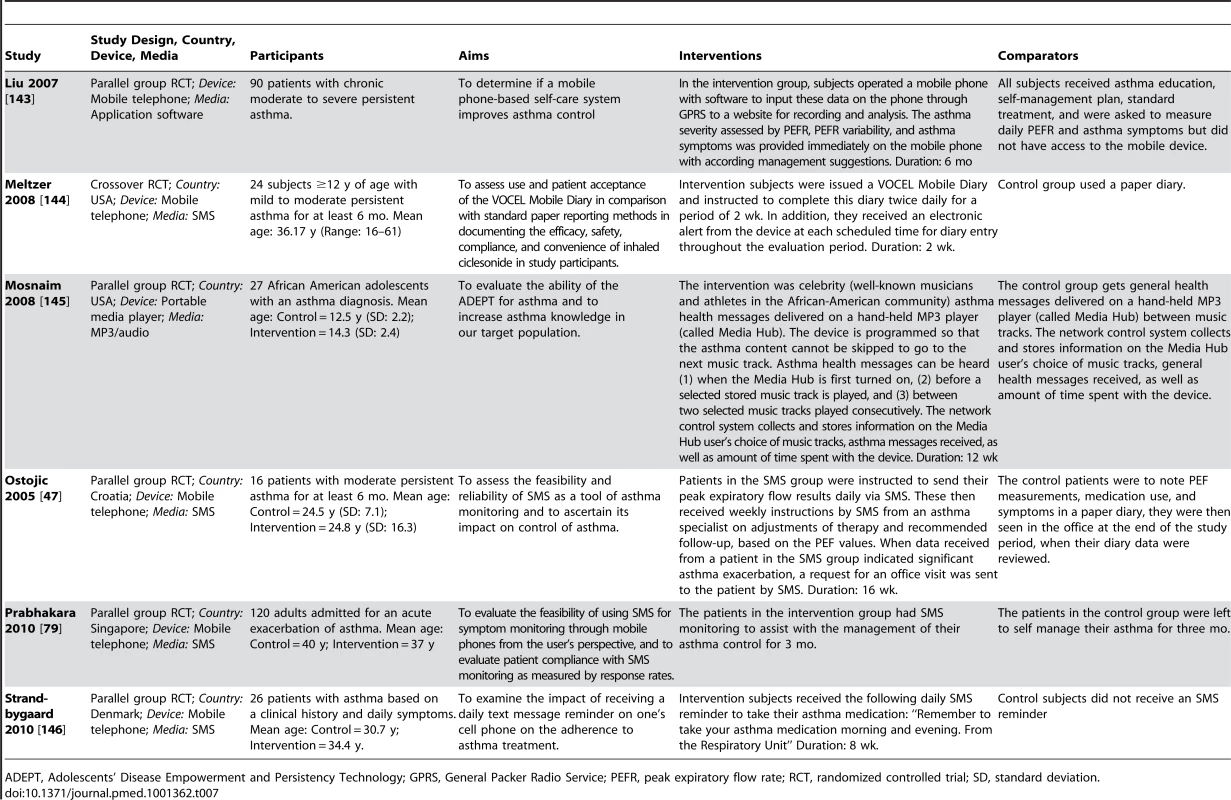
ADEPT, Adolescents' Disease Empowerment and Persistency Technology; GPRS, General Packer Radio Service; PEFR, peak expiratory flow rate; RCT, randomized controlled trial; SD, standard deviation. Tab. 8. Description of trials targeting hypertension. 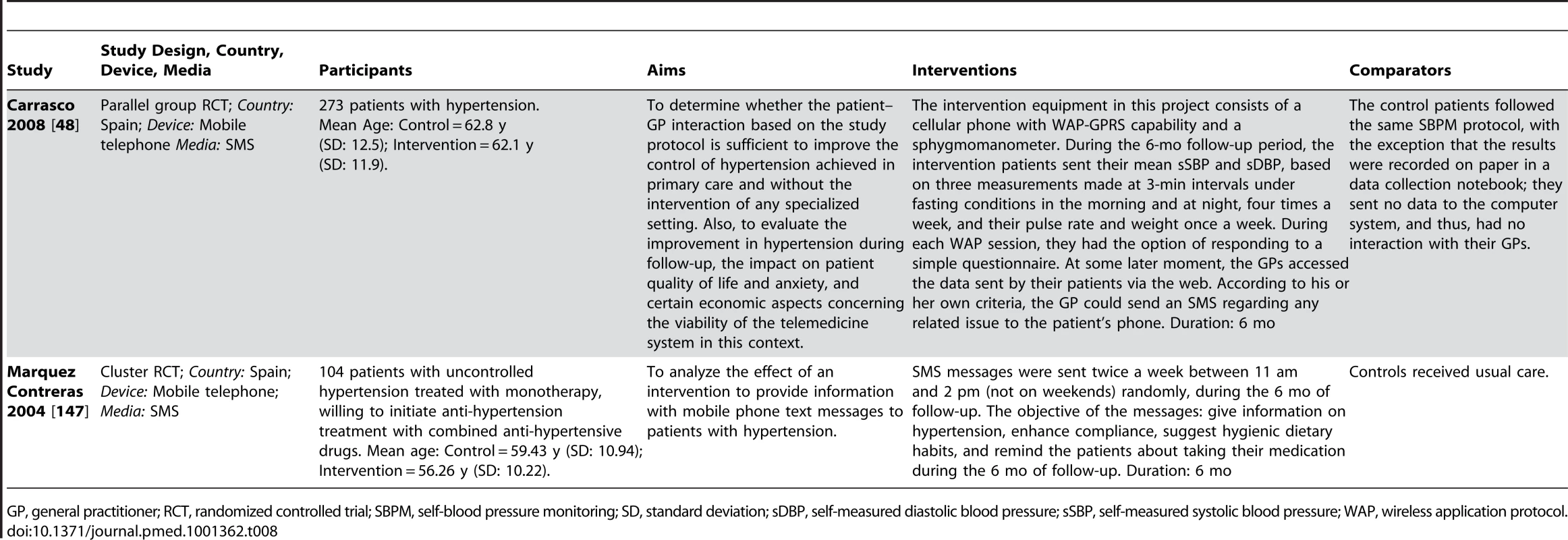
GP, general practitioner; RCT, randomized controlled trial; SBPM, self-blood pressure monitoring; SD, standard deviation; sDBP, self-measured diastolic blood pressure; sSBP, self-measured systolic blood pressure; WAP, wireless application protocol. Tab. 9. Description of trials of psychological support interventions. 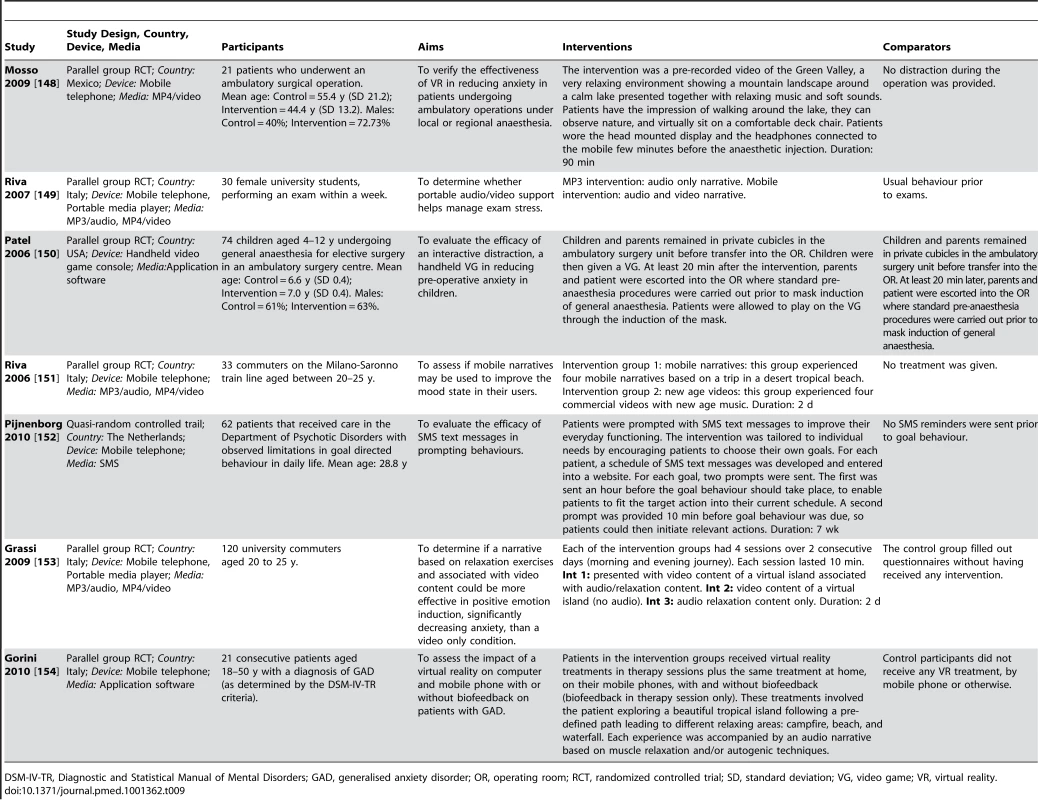
DSM-IV-TR, Diagnostic and Statistical Manual of Mental Disorders; GAD, generalised anxiety disorder; OR, operating room; RCT, randomized controlled trial; SD, standard deviation; VG, video game; VR, virtual reality. Tab. 10. Description of trials of other disease management interventions. 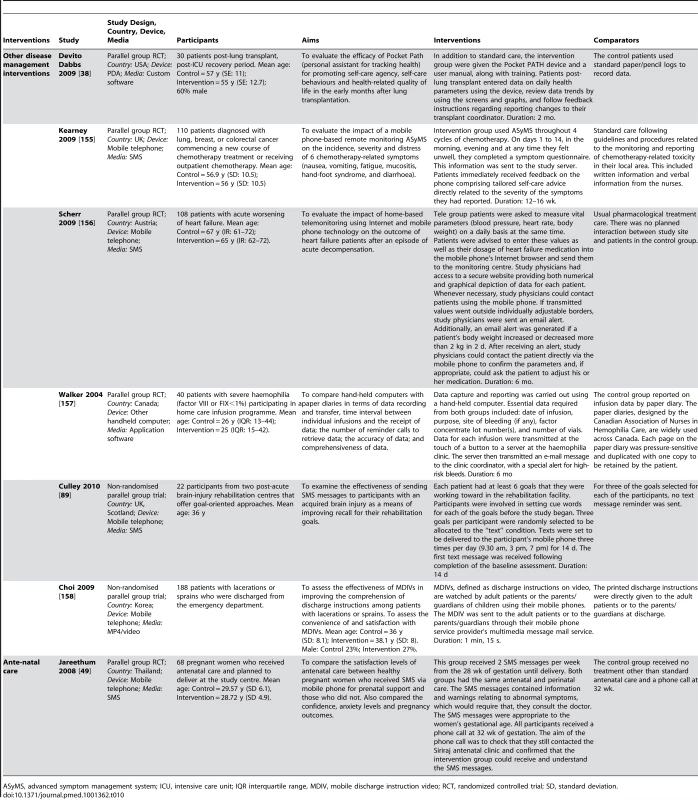
ASyMS, advanced symptom management system; ICU, intensive care unit; IQR interquartile range, MDIV, mobile discharge instruction video; RCT, randomized controlled trial; SD, standard deviation. One disease management trial was conducted in a low-income country (Kenya), and two were conducted in middle-income countries (Mexico, Thailand). All other trials were conducted in high-income countries.
Interventions
We describe the interventions according to the device (mobile phone, PDA, etc.) and functions used (SMS, multi-media messaging service MMS, software application, video). Behaviour change interventions are described according to the study authors' descriptions of the behavioural change theory underpinning the intervention and behaviour change techniques employed. Further details of each intervention, as described by authors, are provided in Tables 1–10.
Health behaviour change
Sixteen of the health behaviour change interventions used mobile phones, of which 13 used the SMS function, one used the MP3 function, one used the MP4 function, and one used the telephone function. One intervention was delivered using a PDA phone using application software, SMS, and telephone functions. Five interventions were delivered using PDAs using application software, two used hand held computers employing application software or MP4/video functions, one used the audio functions provided by a MP3 audio players.
Of the 26 studies, seven reported using behavioural theories to underpin their intervention. The maximum number of techniques reported by any intervention description was 18 [21],[22],[36] and the median number was six. The most commonly used behaviour change techniques were the following: provide feedback on performance (13 interventions), goal setting (12 interventions), provide information on the consequences of behaviour generally (11 interventions), tailoring (11 interventions), prompt self-monitoring of behaviour (10 interventions), and identify barriers to behaviour/problem solving/identify ways of overcoming barriers (eight interventions). The behavioural theories and behaviour change techniques reported in the description of interventions in the trial reports are found in Tables 11 and 12.
Tab. 11. Techniques employed in behaviour change interventions. 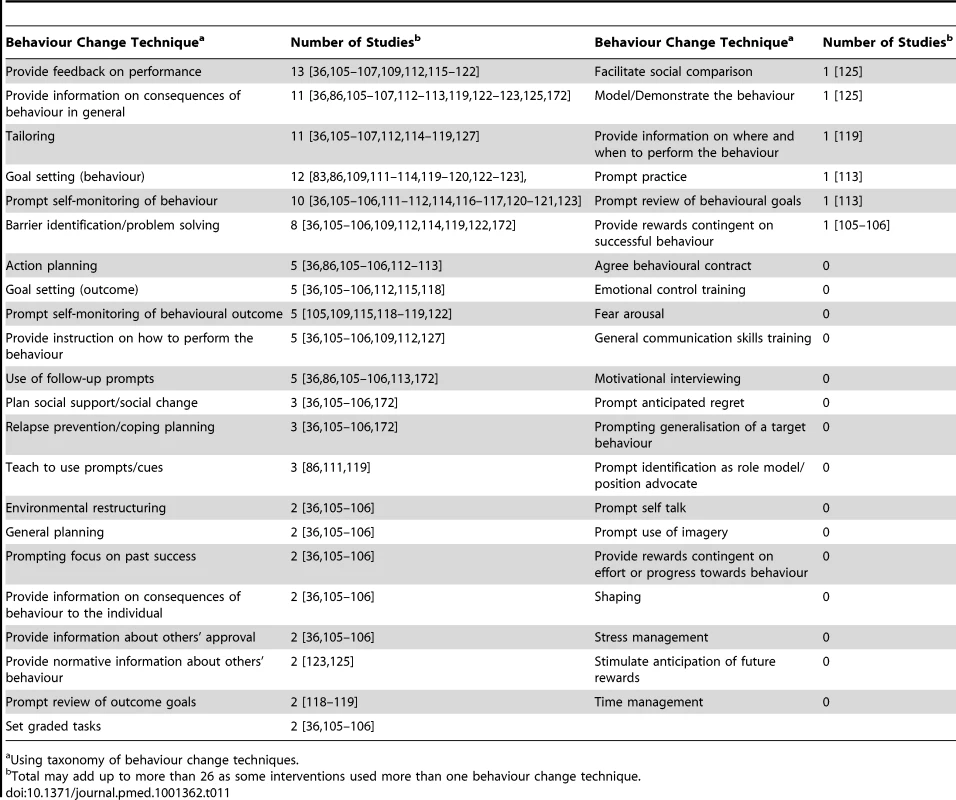
Using taxonomy of behaviour change techniques. Tab. 12. Frequency of reported use of behaviour change theories. 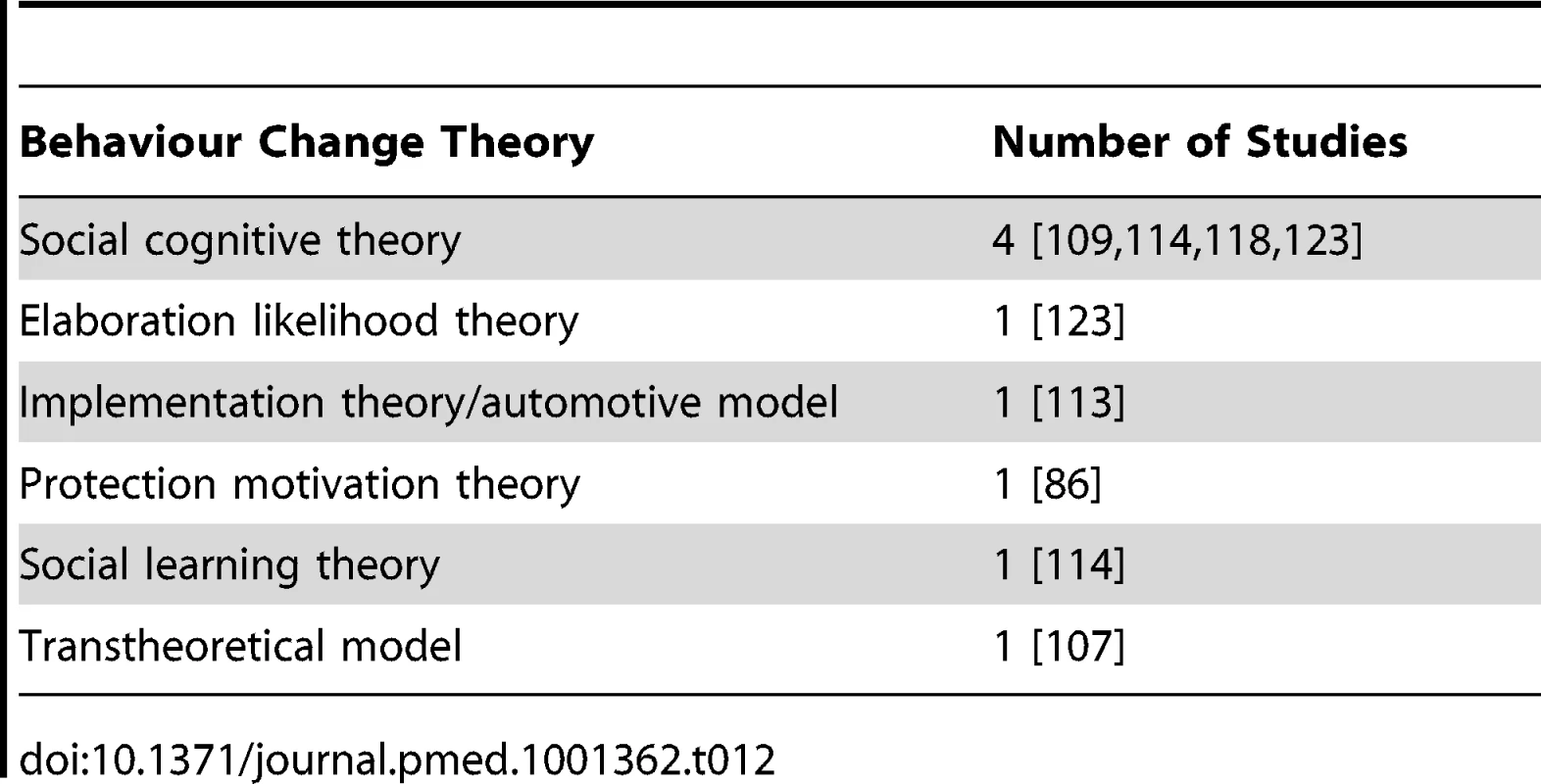
Disease management
Forty-two of the 49 disease management interventions were delivered by mobile phone or PDA mobile phone with 27 using the SMS function, three using MP4 video functions, four using MP3 audio and MP4 video functions, six using application software, one using WAP for data transfer, and one using telephone functions. Two interventions were delivered via PDA, three used hand held computers, one used a video console all of which employed application software. One used a portable media player/MP3 employing audio functions.
Outcomes
Health behaviour change
The health behaviour change trials reported between one and 23 outcomes. Primary outcomes were as follows: Four trials reported four different medical outcomes such as HBA1C (n = 1), blood pressure (n = 1), and deaths (n = 1). Fourteen trials reported seven different anthropometric outcomes (e.g., height, weight). Eight trials reported four different objective measures of behaviour.
Secondary outcomes were as follows: Thirteen trials reported 38 different self-reported behaviour outcomes and four trials reported seven different knowledge, cognitive, or other mediator outcomes.
Disease management
The disease management trials reported between one and 25 outcomes. Primary outcomes were as follows: Seventeen trials measured 28 different medical outcomes. Three trials measured four different anthropometric outcomes. Secondary outcomes were as follows: Thirty trials reported 125 different medical, disease control, or medical process outcomes such as hospitalization, cardiopulmonary resuscitation (CPR) skills, adherence to treatment, and self-monitoring of disease. Eleven cognitive mediator or other mediator outcomes were reported (such as knowledge and attitudes).
Study Quality
Health behaviour change
The assessment of study quality is reported in Table 13 and the Cochrane risk of bias summary is reported in Figure 2. Two trials were at low risk of bias for all quality criteria [21],[36]. No evidence of publication bias was demonstrated on visual or statistical examination of the funnel plots.
Fig. 2. Cochrane summary risk of bias for health behaviour change trials. 
Tab. 13. Methodological quality summary for health behaviour change interventions. 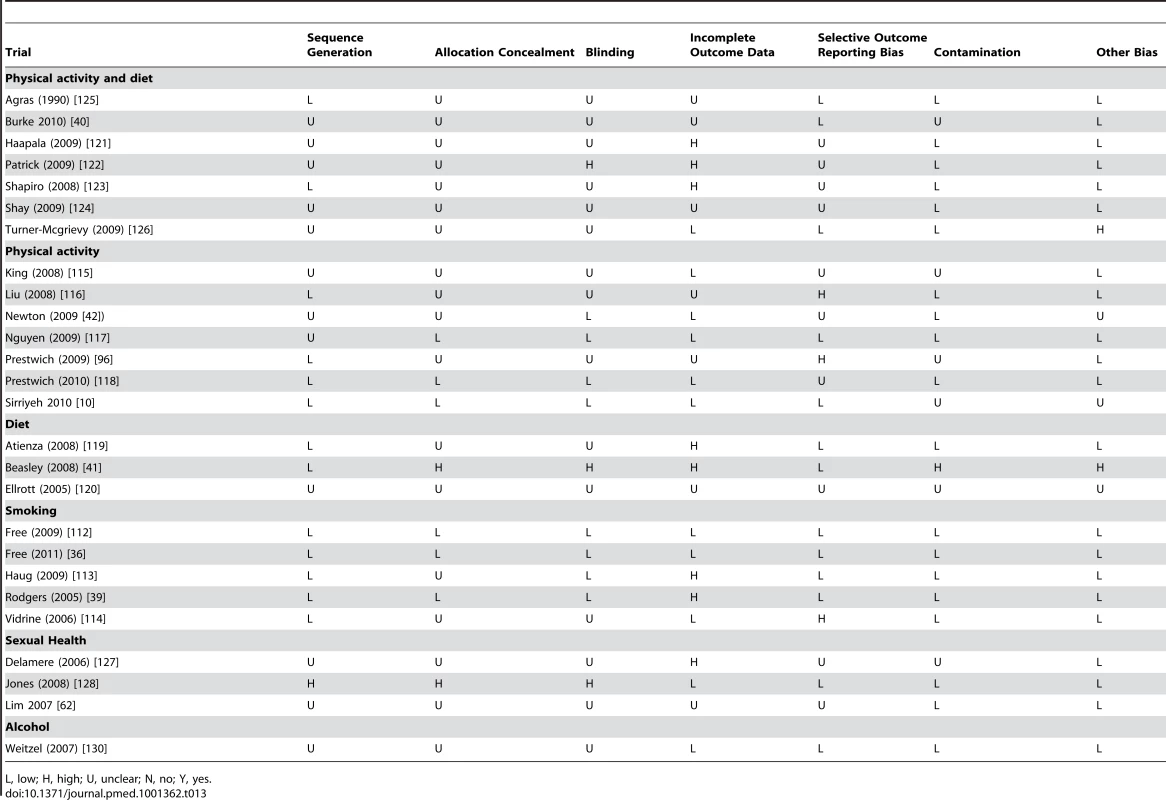
L, low; H, high; U, unclear; N, no; Y, yes. Disease management
The assessment of study quality is reported in Table 14 and the Cochrane risk of bias summary is reported in Figure 3. Two trials were low risk of bias in all areas assessed [37],[38]. No evidence of publication bias was demonstrated on visual or statistical examination of the funnel plots.
Fig. 3. Cochrane risk of bias summary for emergency care by lay people and self management of diseases. 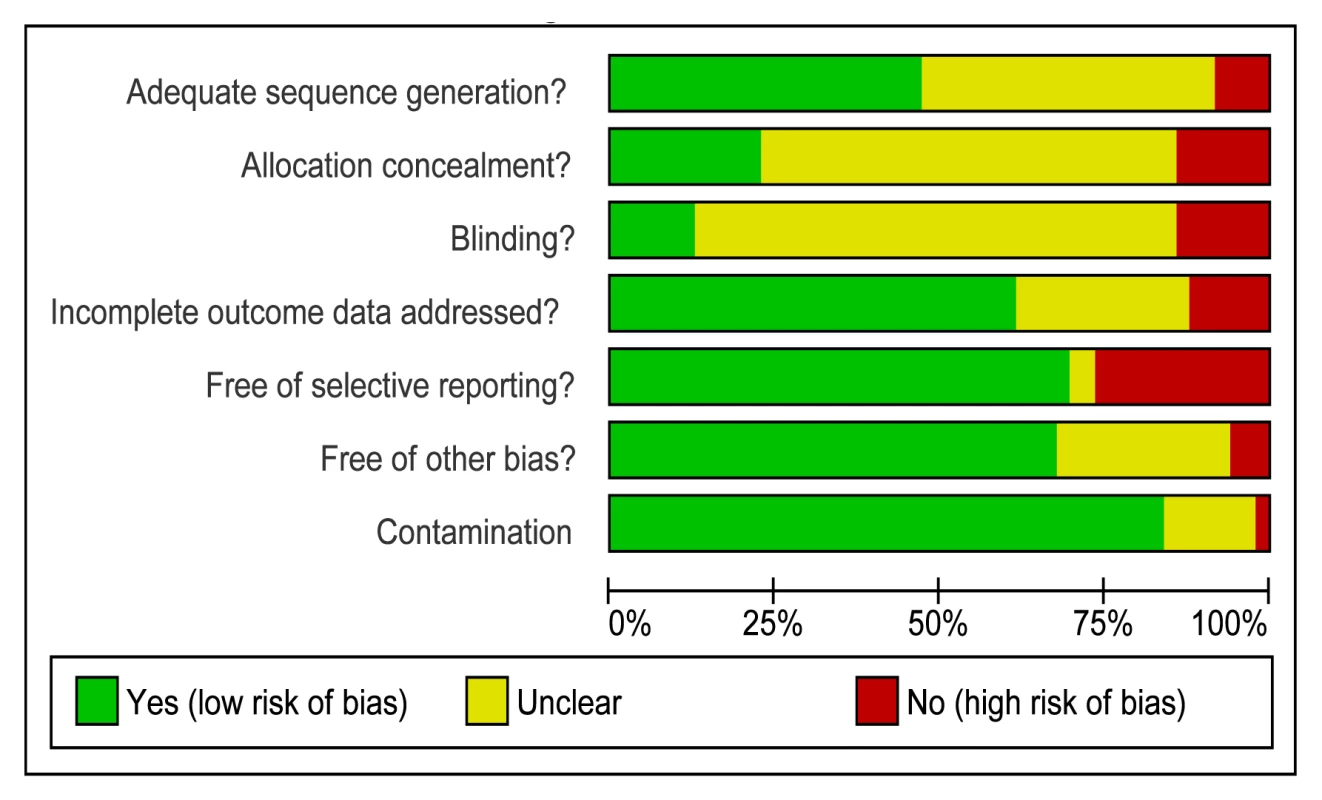
Tab. 14. Cochrane risk of bias summary for emergency care delivered by lay people and self-management of diseases. 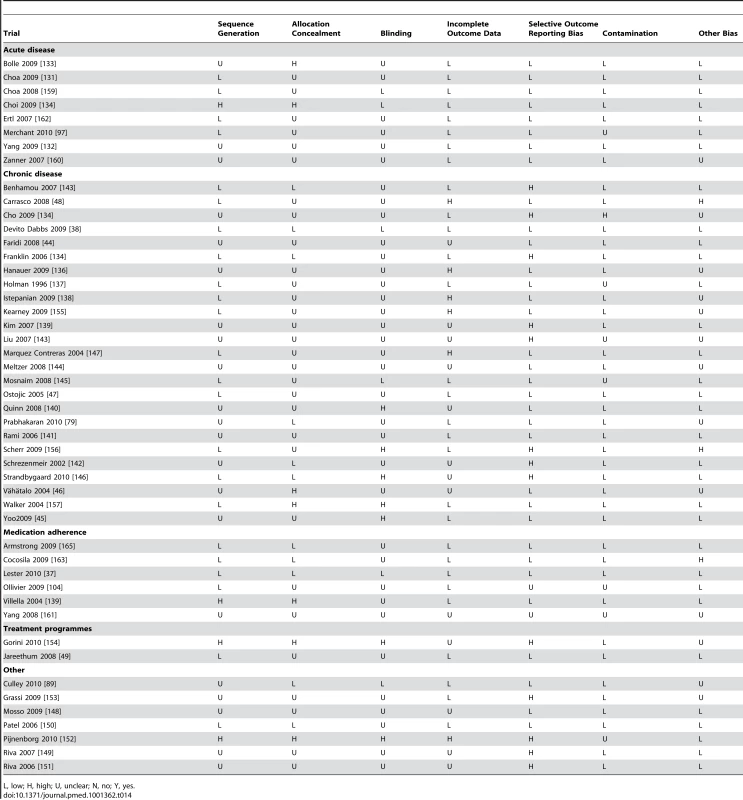
L, low; H, high; U, unclear; N, no; Y, yes. Effects
For each type of intervention we report primary outcomes and a summary of secondary outcomes. Full details of the secondary outcomes are available in Tables 15–17.
Tab. 15. Secondary outcomes health behaviour change interventions. 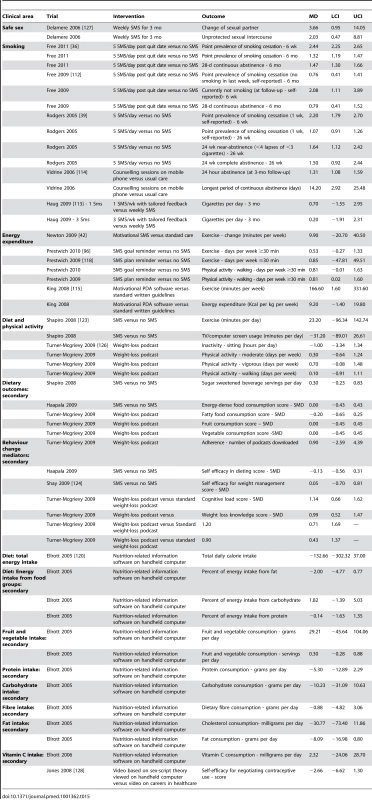
Tab. 16. Secondary outcomes for emergencies. 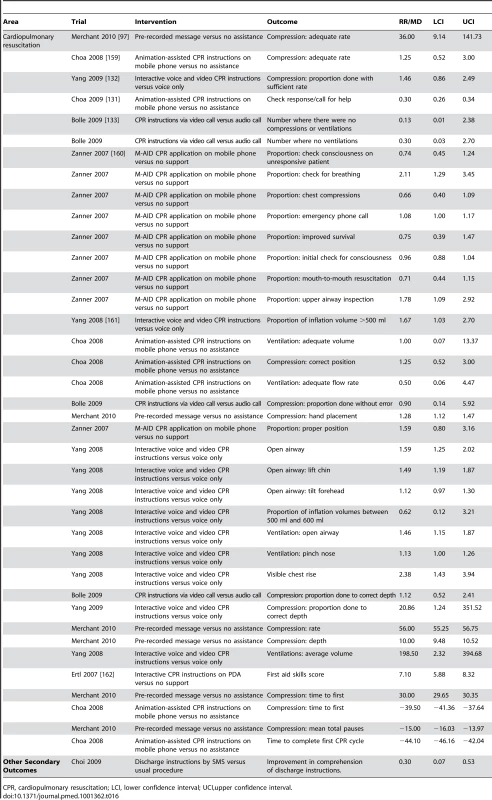
CPR, cardiopulmonary resuscitation; LCI, lower confidence interval; UCI,upper confidence interval. Tab. 17. Secondary outcomes for chronic disease management trials. 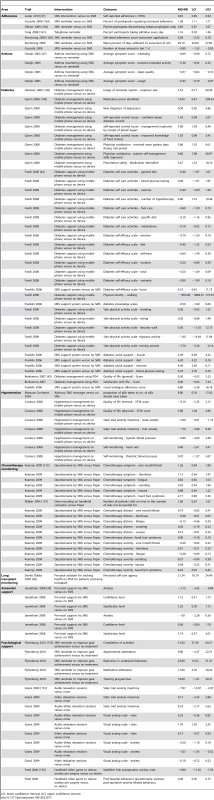
LCI, lower confidence interval; UCI, upper confidence interval. Health Behaviour Change
Pooled effects for health behaviour change are reported in Figure 4 and outcomes are reported in Table 18.
Fig. 4. Health behavior change interventions. 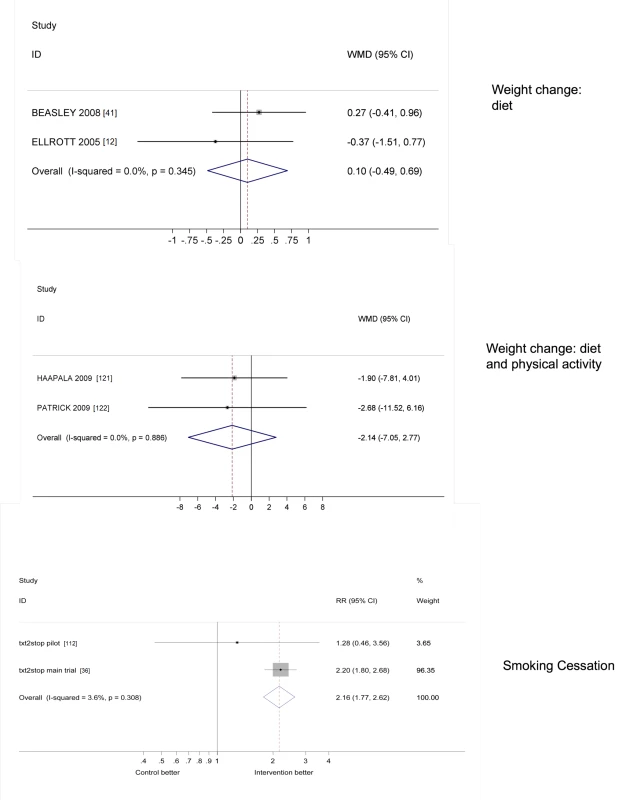
Tab. 18. Primary outcomes for health behaviour change interventions. 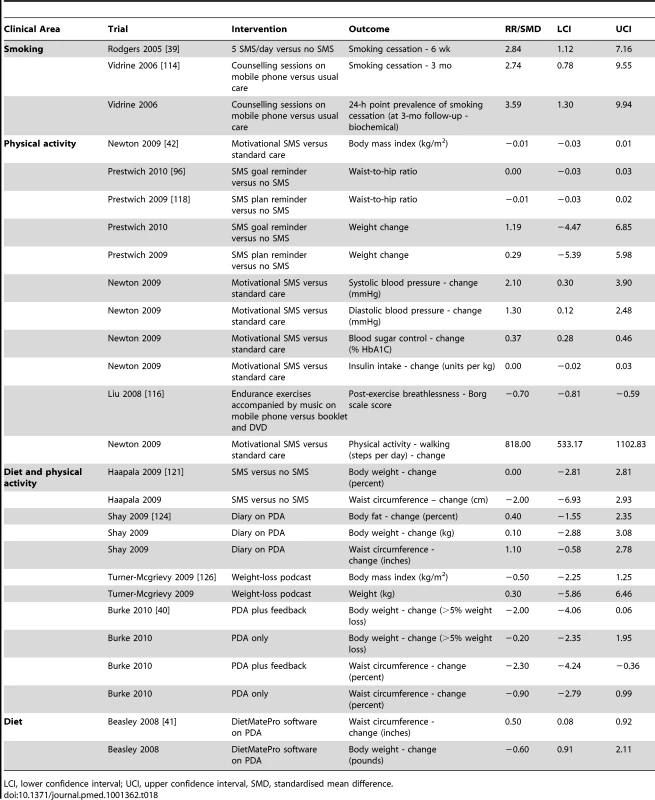
LCI, lower confidence interval; UCI, upper confidence interval, SMD, standardised mean difference. Primary objective outcomes
Two health behaviour change trial had low risk of bias. SMS-based smoking cessation interventions more than doubled biochemically-verified smoking cessation at 6 months [21],[36] (pooled effect estimate relative risk [RR] 2.16 [95% CI 1.77–2.62, p<0.0001]).
For other trials, of three smoking cessation trials reporting biochemicallyverified smoking cessation outcomes, two showed statistically significant improvement [36],[39]. There were no statistically or clinically significant changes in weight for trials using SMS messages to reduce calorie intake and increase physical activity (standard mean difference [SMD] −2.14 [95% CI −7.05 to 2.77] kg) or for trials using application software to reduce calorie intake (SMD −0.10 [95% CI −0.49 to 0.69] kg). One trial of a diet and physical activity intervention and one other trial of an intervention targeting diet only showed statistically significant reductions in waist circumference [40],[41]. The other 13 anthropometric outcomes for trials targeting physical activity only, diet only, or diet and physical activity showed no statistically significant effects (Table 18). One trial [42] targeting physical activity reported four disease control outcomes: one showed a statistically significant benefit in diabetes control (HBA1C) [42], one showed no effect on insulin requirements [42], and two showed no change in systolic and diastolic blood pressure. One objective measure of physical activity showed a statistically significant increase in the number of steps taken per day as assessed by a pedometer. There were no primary outcomes reported for sexual health or alcohol consumption [42].
Secondary outcomes
Table 15 shows the effect estimates for secondary outcomes for health behaviour change interventions. For smoking cessation support, eight of the 14 self-reported smoking outcomes showed statistically significant benefits and none showed statistically significant harms. For physical activity, diet, and diet and physical activity trials, seven of the 14 self-reported physical activity outcomes reported showed statistically significant benefits and none showed statistically significant harms. None of the 17 dietary intake outcomes reported showed statistically significant effects. There were six reported outcomes regarding cognitive mediators of behaviour change. Of these, three showed statistically significant benefits and none showed statistically significant harms. For the trial targeting safer sexual behaviour, the cognitive mediator of behaviour change (self-efficacy regarding condom use) reported showed a statistically significant benefit.
Disease Management
Primary outcomes
Pooled effects are reported in Figure 5 and outcomes are reported in Table 19.
Fig. 5. Self-management of disease. 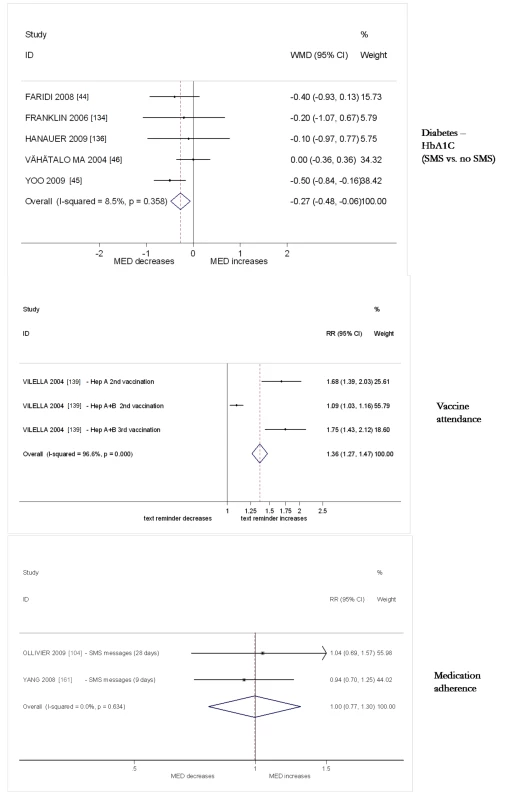
Tab. 19. Primary outcomes for disease management. 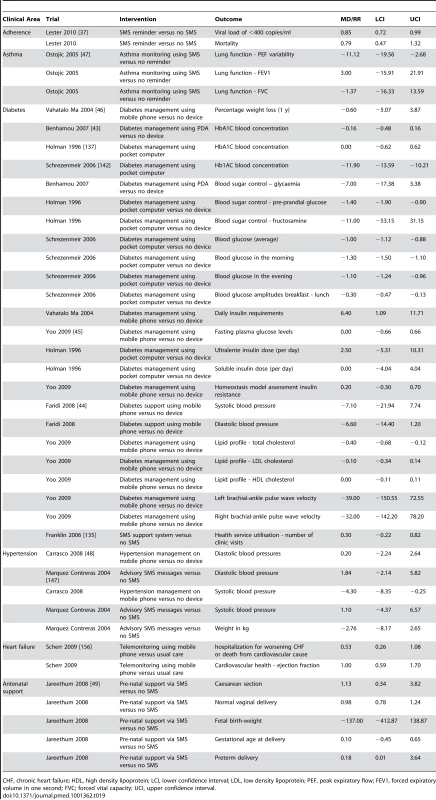
CHF, chronic heart failure; HDL, high density lipoprotein; LCI, lower confidence interval; LDL, low density lipoprotein; PEF, peak expiratory flow; FEV1, forced expiratory volume in one second; FVC; forced vital capacity; UCI, upper confidence interval. A trial with low risk of bias dealt with adherence to prescribed medication, in which an intervention that used text messages to maintain contact, monitor, and respond to medication issues in patients on antiretrovirals statistically significantly reduced HIV viral load <400 copies (RR 0.85 [95% CI 0.72–0.99]) [37] but did not reduce mortality (RR 0.79 [95% CI 0.47 to 1.32]). The other trial with low risk of bias did not report any primary outcomes [38].
Diabetes self-management intervention reduced HBA1C (pooled mean difference [MD] −0.27% [95% CI −0.48 to −0.06]) [43]. For 12 other diabetes control outcomes, six showed statistically significant benefits. Two trials [44] reported two blood pressure outcomes; neither showed reductions that were statistically significant. One trial reported three lipid profile outcomes, of which one showed a statistically significant reduction [45]. One trial reported no effect on weight loss [46]. No trials reported outcomes of hypoglycaemia.
For patients with asthma, one trial [47]reported three lung function outcomes, of which one showed a statistically significant improvement and none showed statistically significant negative effects. For patients with hypertension, of four blood pressure outcomes reported in two trials, one showed a statistically significant reduction [48] and none showed statistically significant negative effects. There were no statistically significant effects reported for a trial for monitoring of heart failure. For antenatal support there were no statistically significant effects reported for five outcomes reported in one trial [49].
Secondary outcomes
Secondary outcomes are reported in Tables 16 and 17.
One trial at low risk of bias was an adherence intervention that reduced self-reported non adherence to antiretroviral medication (RR 0.80 [95% CI 0.69–0.94]).The other trial with low risk of bias reported an increase in self care agency in patients with lung transplants [38].
Other trials included SMS reminders that had no effect on the percentage of pills taken daily in two trials (RR 1.00 [95% CI 0.77–1.30]) with I2 = 0%. Of six other adherence outcomes reported by four trials, three showed statistically significant benefits and none showed statistically significant harms. In one trial, the pooled effect of SMS reminders on attendance for vaccination at different time points was RR 1.19 (95% CI 1.15–1.23) with I2 = 99.7% (p>0.001). For cardiopulmonary resuscitation (CPR), of 37 outcomes reported in nine trials, 18 showed statistically significant benefits and none showed statistically significant reductions in the quality of CPR. For diabetes self-management interventions, of 26 medical process outcomes reported, five showed statistically significant benefits and two showed statistically significant reductions in beneficial medical processes. Of 11 cognitive or mediator outcomes, five showed statistically significant benefits and none showed statistically significant harms. For hypertension, of three self-monitoring outcomes, none had statistically significant effects and one of two quality of life outcomes showed a statistically significant benefit. One of two anxiety outcomes showed a statistically significant benefit and there was no effect on self-reported adherence to hypertension medication. There were no statistically significant effects on 19 outcomes relating to chemotherapy symptom monitoring. One lung transplant monitoring intervention reported a statistically significant increase in perceived self-care agency. For one trial of ante-natal support, four of the six outcomes regarding anxiety, confidence, and satisfaction showed statistically significant benefits and none showed statistically significant harms. For psychological support interventions, three of the seven anxiety outcomes showed statistically significant reductions in anxiety and five of the nine other outcomes showed statistically significant benefits. There were no statistically significant reductions reported in psychological health outcomes.
Discussion
Key Findings
This review of randomised controlled trials for mobile technology interventions delivered to health care consumers found 59 trials that investigated the use of mobile technologies to improve disease management and 26 trials that investigated their use to change health behaviours. The trial demonstrated mixed evidence regarding the benefits of interventions, and nearly all trials were conducted in high-income countries. Four trials had a low risk of bias. One trial with low risk of bias reported clinically important reductions in viral load from an intervention that used text messages to maintain contact, monitor, and respond to medication issues with patients prescribed antiretrovirals in Kenya [37]. Trials demonstrate that automated multifaceted smoking cessation support delivered by text message more than doubles biochemically verified smoking cessation [21],[36]. However, our meta-analyses show that, to date, mobile technology-based interventions for diabetes control that have statistically significant effects are small and of borderline clinical importance. Simple medication reminders delivered by SMS message show no benefits. The effect estimates for diet and diet with physical activity interventions on weight were consistent with no or small benefits. There is suggestive evidence of benefit for reminders for vaccine appointment attendance and cardiopulmonary resuscitation training. There is suggestive evidence of short-term benefits for interventions for asthma control, physical activity, and psychological support interventions, which could be clinically important if these effects were demonstrated in the long term. Our review found that few trials were at low risk of bias in all areas assessed. Few trials were conducted in low - or middle-income countries.
Strengths and weaknesses of the systematic review in relation to other systematic reviews
To our knowledge, this is the first systematic review of all mobile technology interventions delivered to health care consumers. Our review updates earlier reviews and expands them either by using a more exhaustive search strategy, by presenting effect estimates and 95% confidence intervals for all reported outcomes [28],[29],[31], or by conducting meta-analysis, where sufficient trials report similar outcomes [28],[29],[31]. Nineteen trials (25%) did not provide sufficient data to calculate effect estimates and authors did not respond to requests for data; this could have resulted in bias in the systematic review findings. It was beyond the scope of our review to review all internet or video-based interventions, which in principal can be viewed on many modern mobile phones. Our review aimed to examine the effects of interventions delivered by mobile technologies alone, so we excluded interventions combining mobile technologies with other interventions such as face-to-face counselling. These interventions could be subject to a separate systematic review. A wide range of factors could influence the effectiveness of mobile technology interventions including trial quality [50]; participant factors such as demographics (gender/age) or disease status (disease management/disease prevention interventions); the setting (low-/middle - or high-income country), intervention factors such as components, intensity, timing, type of mobile device (e.g., PDA or mobile phone); or the mobile technology function used (e.g., SMS, video, application software). It was not possible to explore the factors influencing heterogeneity statistically, as there were few trials of similar interventions reporting the same outcomes, resulting in limited power for such analyses. The examination of funnel plots in exploring publication bias was limited. as few trials contributed to some pooled analyses.
We used Abraham and Michie's typology [34] of behaviour change tools to code the intervention content according to author descriptions in the papers or protocols. The typology could be improved by modifying it for mobile technology-based interventions and specific behavioural domains, as has been done for smoking cessation [51]. We coded the authors' descriptions of the interventions as reported in the papers, which varied in the level of detail provided. The coding of intervention content would have been more complete and accurate if the text message and other intervention content was obtained and directly coded, as has been done for the txt2stop intervention [51]. There was inadequate power to explore the impact of different behaviour change tools in specific behavioural domains on effect estimates.
Systematic review findings in relation to findings from trials published since our search was completed
On 1 November 2012, we re-ran our search to identify new trials published since the search conducted for the systematic review was completed.
Health Behaviour Change
We identified 14 new trials of health behaviour change interventions. Primary outcomes were as follows: One trial reported increases in smoking cessation at 1 wk for mobile phone-based telephone counselling intervention [52]. A trial involving video-based smoking cessation support showed no benefits [53]. Three trials reported no statistically significant effects on weight of a diary-plus-mobile-phone daily feedback messages compared to a diary [54], a text message based intervention [55], and a twitter, podcast, and mobile phone application based intervention [56]. A mobile phone-based counselling intervention had no effect on postponing subsequent pregnancies on teen mothers [57]. There was no effect on plaque score of text message based oral health education [58].
Secondary outcomes were as follows: One trial reported pregnant smokers receiving text messages were more likely to set a quit date [59]. One trial reported a reduction in portion sizes for a mobile phone and web based planning intervention designed to reduce weight [60]. One trial reported an increase in testing for HIV in those receiving a text message intervention involving ten or more messages [61]. One trial reported increases in sexually transmitted infection testing amongst those receiving text message based sexual health interventions (odds ratio [OR] 2.51 [95% CI 1.11–5.69]) [62]. One factorial trial reported a reduction in sexual partners in participants receiving safer sex text messages, but no effects of sun protection messages on hat wearing [63]. One trial reported an increase in condom use with “risky partners such as sex workers or with other men” [64]. One trial reported a reduction in self-reported heavy drinking days in young people allocated to a text messages-based intervention [65].
Disease Management
We identified 37 new trials of disease management interventions. Primary outcomes were as follows: One trial with unclear risk of bias reported improved cure rates for tuberculosis in those receiving medication reminders [66]. One trial employing text messages increased the proportion of urban women delivering with a skilled attendant (OR 5.73 [95% CI 1.51–21.81]); the risk of bias in this trial was unclear [67]. One small trial reported a statistically and clinically important >1% absolute reduction in HBA1C in the intervention group compared to control group [68].Four trials of a diabetes care intervention, three involving text messages and the other involving video messages, reported statistically significant decreases in HBA1C, which were of borderline clinical significance [69]–[73]. One trial with unclear risk of bias reported increases in receipt of vaccinations in those allocated to receive text messages reminders [74]. One trial found no effect of a detailed text message compared to a simple text message inviting women for mammography screening [75]. One trial with unclear/high risk of bias reported an improvement in cardiovascular risk profiles for patients receiving telemonitoring via mobile phone with text message-based advice (RR = 1.4; 95% CI 1.1–1.7). The intervention increased the proportion of patients achieving blood pressure <140/90 (RR 1.4 [1.1–1.9]) and increased the proportion of patients achieving HBA1C of <7% (RR 1.16 [1.6–2.4]), but there were no statistically significant differences in LDL cholesterol or smoking [76]. One trial with unclear risk of bias reported a statistically significant reduction in systolic and diastolic blood pressure compared to baseline in an intervention group receiving monitoring of salt excretion but no statistically significant change in the control group [77]. Two trials reported no statistically significant beneficial effects of either a text message-based intervention or a mobile phone-based monitoring and feedback intervention on asthma control [78],[79]. A trial providing asthma patients with alerts regarding health risk weather forecast had no statistically significant benefits on reducing exacerbations of asthma [80].
Secondary outcomes were as follows: Three trials reported statistically significant increases in adherence to antiretroviral medication with text message reminders [81]–[83], and one trial reported increases in adherence that were not statistically significant [84]. One trial has demonstrated improved quality of life for patients with heart failure receiving a mobile phone based telemonitoring intervention [85]. Two trials reported increases in emotional self-awareness in young people receiving risk assessment and management of youth mental health problems: one reported benefits in mild depressive symptoms [86],[87], and another reported that delivering cognitive behavioural therapy messages by mobile phone was feasible and acceptable [88]. One trial reported improved recall of goals in a trials delivering text messages to patients undergoing brain rehabilitation [89]. One trial reported that an educational package of text messages increased continuation of the combined oral contraceptive pill [90], but simple daily reminders regarding taking the combined oral contraceptive has no effect in another trials [91]. One trial reported an increase in self-efficacy for self-managing cystic fibrosis [92]. A mobile phone-based map did not shorten the time taken to retrieve an automated external defibrillator in out-of-hospital cardiac arrest victims [93]. Three trials reported short term increases in physical activity in those receiving a text message-based intervention designed to increase activity [94]–[96]. Four trials reported benefits in cardiopulmonary resuscitation processes with mobile phone-based audio instructions [97], video instruction [98], and a feedback application [99]. One trial reported improved quality of life with a mobile phone-based asthma self-care system [100], and another reported increases in self-reported adherence to asthma medication [101].
In summary, while interventions using mobile technologies for patients are a fast-moving field, the findings of many trials published since the search for the systematic review was completed are generally consistent with the reported results of trials in the systematic review, particularly for primary outcomes. Trials report benefits in adherence to antiretroviral medication and smoking cessation; one small trial reported a significant reduction in HBA1c for a diabetes control intervention, and there were no or small effects of interventions on weight and no reported benefits of daily medication reminders. There is suggestive evidence of benefit for attendance for vaccination and cardiopulmonary resuscitation interventions. There are short term benefits for physical activity interventions and psychological support interventions that could be clinically significant if sustained.
Novel trial findings published since our search for the systematic review was completed suggest that text messages can increase the proportion of women receiving skilled delivery in urban areas in Kenya. There are now mixed results for asthma control interventions, with some trials reporting benefits. There is suggestive evidence that multifaceted adherence interventions can increase adherence to the combined oral contraceptive pill and TB medication resulting in increased TB cure rates. There is suggestive evidence that a heart failure intervention can improve quality of life and that tele-monitoring data sent by mobile combined with text message advice can reduce blood pressure and HBA1C. There is suggestive evidence that sexual health interventions can increase testing for HIV and sexually transmitted infections.
Implications of the Study for Health Care Delivery
Multifaceted adherence interventions demonstrate an increase in adherence to anti-retrovirals and a decrease in viral load when evaluated in Kenya [37]. An automated texting intervention for smoking cessation support was effective when evaluated in the UK. Both interventions may require some adaptation as well as translation for use in other countries. Health services should consider implementing similar interventions in similar settings.
The finding that simple SMS reminders for adherence to medication have at best small effects is consistent with the findings from existing adherence research, which has previously demonstrated that uni-faceted interventions have very modest benefits [102]–[104]. Likewise, it is unsurprising that interventions delivered by mobile technologies appear to have small effects on weight, given the paucity of effective behavioural change interventions for obesity [105],[106].
There is currently insufficient high quality evidence of beneficial effects on clinical outcomes to warrant implementation of interventions for other areas of health behaviour change or self-management of diseases.
Unanswered Questions and Future Research
The benefits of text message support on adherence to antiiretrovirals and smoking cessation should be established in high-, middle-, and low-income countries. The cost-effectiveness of antiretroviral adherence interventions should be established. A cost-effectiveness analysis of mobile phone text messaging interventions for smoking cessation showed that the intervention is cost-effective [107]. Further high quality trials should robustly establish the effects of multifaceted text messaging interventions on medication adherence in other areas, TB cure rates, and on the proportion of births with a skilled attendant at delivery in urban areas in low - and middle-income countries. Adequately powered high quality trials of optimised interventions are required in areas of health behaviour change and self-management of diseases where there is currently suggestive evidence of benefit.
In areas where, to date, interventions have shown small benefits of borderline or no clinical importance future research should focus on improving interventions, drawing on existing guidance for the development of complex interventions, prior to considering further evaluation by randomised controlled trial [108]. There is a considerable body of existing research regarding effective face-to-face interventions for self-management of diseases, and much of this literature suggests multifaceted interventions are required [104],[109]–[111]. Mobile technology-based interventions for health care consume rs developed to date may not be optimal; some are uni-faceted and may need to incorporate additional components found in other effective interventions for self-management of diseases, but modified for delivery by mobile technologies. For health behaviour change interventions, further research is required to elucidate the effects of different behaviour change tools on behaviours and to explore if interventions, which include a wider range of behaviour change tools, have greater effects.
A range of questions regarding the effects of mobile technologies remain open to question including which functions are most effective (SMS, video, oral instruction, application software), which behaviour change techniques are effective, and whether the effectiveness of interventions is influenced by setting or participant demographics.
The majority of the research to date has been conducted in high-income countries, so trials of interventions in low - and middle-income countries are required, particularly in view of the high coverage of mobile technologies in these settings.
Conclusion
Multifaceted mobile technology text messaging interventions have been shown to increase adherence to antiretroviral medication in a low-income setting and increase smoking cessation in a high-income setting; these interventions should be considered for inclusion in services in similar settings. Their effects in other settings should be established. For other mobile technology health interventions delivered to health care consumers. the effects of optimised interventions on long term, clinically important outcomes must be robustly established in randomised controlled trials.
Supporting Information
Zdroje
1. World Health Organisation (2011) World Health Statistics, 2011. Geneva: WHO.
2. DollR, PetoR, WheatleyK, GrayR, SutherlandI (1994) Mortality in relation to smoking: 40 years' observations on male British doctors. BMJ 309 : 901–911.
3. UNAIDS (2003) AIDS Epidemic update.
4. HammanRF, WingRR, EdelsteinSL, LachinJM, BrayGA, et al. (2006) Effect of weight loss with lifestyle intervention on risk of diabetes. DIABETES CARE 29 : 2102–2107.
5. Trialists'CollaborationA (2002) Collaborative meta-analysis of randomised trials of antiplatelet therapy for prevention of death, myocardial infarction, and stroke in high risk patients. Bmj 324 : 71–86.
6. Al-MallahMH, TleyjehIM, Abdel-LatifAA, WeaverWD (2006) Angiotensin-converting enzyme inhibitors in coronary artery disease and preserved left ventricular systolic function: a systematic review and meta-analysis of randomized controlled trials. Journal of the American College of Cardiology 47 : 1576–1583.
7. FreemantleN, ClelandJ, YoungP, MasonJ, HarrisonJ (1999) β Blockade after myocardial infarction: systematic review and meta regression analysis. Bmj 318 : 1730–1737.
8. BaigentC (2005) Cholesterol Treatment Trialists'(CTT) Collaborators, Efficacy and safety of cholesterol-lowering treatment: prospective meta-analysis of data from 90,056 participants in 14 randomised trials of statins. Lancet 366 : 1267–1278.
9. HarindraV (1997) British HIV Association guidelines for antiretroviral treatment of HIV Seropositive individuals. Lancet 349 : 1838.
10. WangPH (1993) Tight glucose control and diabetic complications. Lancet 342 : 129.
11. NewbyLK, LaPointeNM, ChenAY, KramerJM, HammillBG, et al. (2006) Long-term adherence to evidence-based secondary prevention therapies in coronary artery disease. Circulation 113 : 203–212.
12. OlivariusNF, Beck-NielsenH, AndreasenAH, HorderM, PedersenPA (2001) Randomised controlled trial of structured personal care of type 2 diabetes mellitus. BMJ 323 : 970–975.
13. RothmanRL, MaloneR, BryantB, ShintaniAK, CriglerB, et al. (2005) A randomized trial of a primary care-based disease management program to improve cardiovascular risk factors and glycated hemoglobin levels in patients with diabetes. Am J Med 118 : 276–284.
14. EffingT, MonninkhofE, van der ValkP, ZielhuisG, WaltersH, et al. (2009) Self-management education for patients with chronic obstructive pulmonary disease. Cochrane Database Syst Rev
15. Union IT (2010) The world in 2010: ICT facts and figures. International Telecommunication Union.
16. Ofcom (2009) The Consumer Experience: Telecoms, Internet and Digital Broadcasting 2009. Evaluation Report.
17. Feldmann V (2003) Mobile overtakes fixed: Implications for policy and regulation. Geneva: ITU.
18. Sciadas G, Guiguère P, Adarn L (2005) From the digital divide to digital opportunities: Measuring infostates for development: Orbicom International Secretariat.
19. Banks K, Burge R (2004) Mobile phones: an appropriate tool for conservation and development: by Fauna & Flora International, Cambridge, UK.
20. DonnerJ (2008) Research approaches to mobile use in the developing world: A review of the literature. The Information Society 24 : 140–159.
21. FreeC, WhittakerR, KnightR, AbramskyT, RodgersA, et al. (2009) Txt2stop: a pilot randomised controlled trial of mobile phone-based smoking cessation support. Tob Control 18 : 88–91.
22. RodgersA, CorbettT, BramleyD, RiddellT, WillsM, et al. (2005) Do u smoke after txt? Results of a randomised trial of smoking cessation using mobile phone text messaging. Tob Control 14 : 255–261.
23. DaleO, HagenKB (2007) Despite technical problems personal digital assistants outperform pen and paper when collecting patient diary data. Journal of clinical epidemiology 60 : 8.
24. KhoA, HendersonLE, DresslerDD, KripalaniS (2006) Use of handheld computers in medical education. A systematic review. J Gen Intern Med 21 : 531–537.
25. KrishnaS, BorenSA, BalasEA (2009) Healthcare via cell phones: a systematic review. Telemedicine Journal & E-Health 15 : 231–240.
26. LaneSJ, HeddleNM, ArnoldE, WalkerI (2006) A review of randomized controlled trials comparing the effectiveness of hand held computers with paper methods for data collection. BMC Medical Informatics & Decision Making 6 : 23.
27. Whittaker R, Borland R, Bullen C, Lin Ruey B, McRobbie H, et al.. (2009) Mobile phone-based interventions for smoking cessation. Cochrane Database of Systematic Reviews.
28. Cole-LewisH, KershawT (2010) Text Messaging as a Tool for Behavior Change in Disease Prevention and Management. Epidemiol Rev 32 : 56–69.
29. FjeldsoeBS, MarshallAL, MillerYD (2009) Behavior change interventions delivered by mobile telephone short-message service. Am J Prev Med 36 : 165–173.
30. LimMS, HockingJS, HellardME, AitkenCK (2008) SMS STI: a review of the uses of mobile phone text messaging in sexual health. Int J STD AIDS 19 : 287–290.
31. HeronKE, SmythJM (2010) Ecological momentary interventions: Incorporating mobile technology into psychosocial and health behaviour treatments. Br J Health Psychol 15 : 1–39.
32. FreeC, PhillipsG, FelixL, GalliL, PatelV, et al. (2010) The effectiveness of M-health technologies for improving health and health services: a systematic review protocol. BMC Res Notes 3 : 250.
33. FreeCPG, WatsonL, GalliL, FelixL, EdwardsP, PatelV, HainesA (2013) The effectiveness of M-health technologies to improve health care service delivery processes: a systematic review and meta-analysis. PLoS Med 10: e1001363 doi:10.1371/journal.pmed.1001363.
34. AbrahamC, MichieS (2008) A taxonomy of behavior change techniques used in interventions. Health Psychol 27 : 379–387.
35. Higgins JPT, Green S (2008) Cochrane Handbook for Systematic Reviews of Interventions Version 5.0.0: The Cochrane Collaboration.
36. FreeC, KnightR, RobertsonS, WhittakerR, EdwardsP, et al. (2011) Smoking cessation support delivered via mobile phone text messaging (txt2stop): a single-blind, randomised trial. Lancet 378 : 49–55.
37. LesterRT, RitvoP, MillsEJ, KaririA, KaranjaS, et al. (2010) Effects of a mobile phone short message service on antiretroviral treatment adherence in Kenya (WelTel Kenya1): a randomised trial. Lancet 376 : 1838–1845.
38. DeVito DabbsA, DewMA, MyersB, BegeyA, HawkinsR, et al. (2009) Evaluation of a hand-held, computer-based intervention to promote early self-care behaviors after lung transplant. Clinical Transplantation 23 : 537–545.
39. RodgersA, CorbettT, BramleyD, RiddellT, WillsM, et al. (2005) Do u smoke after txt? Results of a randomised trial of smoking cessation using mobile phone text messaging. Tob Control 14 : 255–261.
40. BurkeLE, ConroyMB, SereikaSM, ElciOU, StynMA, et al. (2010) The Effect of Electronic Self-Monitoring on Weight Loss and Dietary Intake: A Randomized Behavioral Weight Loss Trial. Obesity
41. BeasleyJM, RileyWT, DavisA, SinghJ (2008) Evaluation of a PDA-based dietary assessment and intervention program: a randomized controlled trial. J American Coll Nutr 27 : 280–286.
42. NewtonKH, WiltshireEJ, ElleyCR (2009) Pedometers and text messaging to increase physical activity: randomized controlled trial of adolescents with type 1 diabetes. Diabetes Care 32 : 813–815.
43. BenhamouPY, MelkiV, BoizelR, PerrealF, QuesadaJL, et al. (2007) One-year efficacy and safety of Web-based follow-up using cellular phone in type 1 diabetic patients under insulin pump therapy: the PumpNet study. Diabetes & Metabolism 33 : 220–226.
44. FaridiZ, LibertiL, ShuvalK, NorthrupV, AliA, et al. (2008) Evaluating the impact of mobile telephone technology on type 2 diabetic patients' self-management: the NICHE pilot study. Journal of Evaluation in Clinical Practice 14 : 465–469.
45. YooHJ, ParkMS, KimTN, YangSJ, ChoGJ, et al. (2009) A Ubiquitous Chronic Disease Care system using cellular phones and the internet. Diabetic Medicine 26 : 628–635.
46. VähätaloM, VirtamoH, ViikariJ, RönnemaaT (2004) Cellular phone transferred self blood glucose monitoring: prerequisites for positive outcome. Practical Diabetes International 21 : 192–194.
47. OstojicV, CvoriscecB, OstojicSB, ReznikoffD, Stipic-MarkovicA, et al. (2005) Improving asthma control through telemedicine: a study of short-message service. Telemedicine Journal & E-Health 11 : 28–35.
48. Carrasco MP, Salvador CH, Sagredo PG, Márquez-Montes J, González de Mingo MA, et al.. (2008) Impact of patient-general practitioner short-messages-based interaction on the control of hypertension in a follow-up service for low-to-medium risk hypertensive patients: a randomized controlled trial. IEEE transactions on information technology in biomedicine: a publication of the IEEE Engineering in Medicine and Biology Society. pp. 780–791.
49. JareethumR, TitapantV, ChantraT, SommaiV, ChuenwattanaP, et al. (2008) Satisfaction of healthy pregnant women receiving short message service via mobile phone for prenatal support: A randomized controlled trial. Journal of the Medical Association of Thailand 91 : 458–463.
50. JuniP, AltmanDG, EggerM (2001) Systematic reviews in health care: Assessing the quality of controlled clinical trials. BMJ 323 : 42–46.
51. Michie WF, C., Development and application of a reliable system for coding the content of text messages for smoking cessation.
52. VidrineDJ, MarksRM, ArduinoRC, GritzER (2012) Efficacy of Cell Phone-Delivered Smoking Cessation Counseling for Persons Living With HIV/AIDS: 3-Month Outcomes. Nicotine & Tobacco Research 14 : 106–110.
53. WhittakerR, DoreyE, BramleyD, BullenC, DennyS, et al. (2011) A Theory-Based Video Messaging Mobile Phone Intervention for Smoking Cessation: Randomized Controlled Trial. Journal of Medical Internet Research 13 : 58–69.
54. BurkeLE, StynMA, SereikaSM, ConroyMB, YeL, et al. (2012) Using mHealth Technology to Enhance Self-Monitoring for Weight Loss A Randomized Trial. American Journal of Preventive Medicine 43 : 20–26.
55. de NietJ, TimmanR, BauerS, van den AkkerE, de KlerkC, et al. (2012) Short Message Service Reduces Dropout in Childhood Obesity Treatment: A Randomized Controlled Trial. Health Psychol
56. Turner-McGrievyG, TateD (2011) Tweets, Apps, and Pods: Results of the 6-month Mobile Pounds Off Digitally (Mobile POD) randomized weight-loss intervention among adults. J Med Internet Res 13: e120.
57. KatzKS, RodanM, MilliganR, TanS, CourtneyL, et al. (2011) Efficacy of a randomized cell phone-based counseling intervention in postponing subsequent pregnancy among teen mothers. Matern Child Health J 15 Suppl 1: S42–53.
58. SharmaR, HebbalM, AnkolaAV, MurugabupathyV (2011) Mobile-phone text messaging (SMS) for providing oral health education to mothers of preschool children in Belgaum City. J Telemed Telecare 17 : 432–436.
59. NaughtonF, PrevostAT, GilbertH, SuttonS (2012) Randomized Controlled Trial Evaluation of a Tailored Leaflet and SMS Text Message Self-help Intervention for Pregnant Smokers (MiQuit). Nicotine & Tobacco Research 14 : 569–577.
60. SouretiA, MurrayP, CobainM, ChinapawM, van MechelenW, et al. (2011) Exploratory study of web-based planning and mobile text reminders in an overweight population. J Med Internet Res 13: e118.
61. de TollyK, SkinnerD, NembawareV, BenjaminP (2012) Investigation into the use of short message services to expand uptake of human immunodeficiency virus testing, and whether content and dosage have impact. Telemedicine Journal & E-Health 18 : 18–23.
62. LimMS, HockingJS, AitkenCK, FairleyCK, JordanL, et al. (2012) Impact of text and email messaging on the sexual health of young people: a randomised controlled trial. J Epidemiol Community Health 66 : 69–74.
63. GoldJ, LimMSC, HellardME, HockingJS, KeoghL (2010) What's in a message? Delivering sexual health promotion to young people in Australia via text messaging. BMC Public Health 10.
64. KaoaiemH, TaneepanichskulS, SomrongthongR, SaengdidthaB, LertmaharitS (2012) The effect of squad leader mentors through short message services for mobile phones in promoting safe sex among first (central) army area conscripts of Thailand. Journal of the Medical Association of Thailand 95 : 249–256.
65. SuffolettoB, CallawayC, KristanJ, KraemerK, ClarkD (2012) Text-message-based drinking assessments and brief interventions for young adults discharged from the emergency department. Alcohol Clin Exp Res 36 : 552–560.
66. KunawararakP, PongpanichS, ChantawongS, PokaewP, TraisathitP, et al. (2011) Tuberculosis treatment with mobile-phone medication reminders in northern Thailand. Southeast Asian J Trop Med Public Health 42 : 1444–1451.
67. LundS, HemedM, NielsenBB, SaidA, SaidK, et al. (2012) Mobile phones as a health communication tool to improve skilled attendance at delivery in Zanzibar: a cluster-randomised controlled trial. BJOG 119 : 1256–1264.
68. HusseinWI, HasanK, JaradatAA (2011) Effectiveness of mobile phone short message service on diabetes mellitus management; the SMS-DM study. Diabetes Research and Clinical Practice 94: E24–E26.
69. BellAM, FondaSJ, WalkerMS, SchmidtV, VigerskyRA (2012) Mobile phone-based video messages for diabetes self-care support. J Diabetes Sci Technol 6 : 310–319.
70. ShettyAS, ChamukuttanS, NandithaA, RajRK, RamachandranA (2011) Reinforcement of adherence to prescription recommendations in Asian Indian diabetes patients using short message service (SMS)–a pilot study. J Assoc Physicians India 59 : 711–714.
71. QuinnCC, ShardellMD, TerrinML, BarrEA, BallewSH, et al. (2011) Cluster-randomized trial of a mobile phone personalized behavioral intervention for blood glucose control. DIABETES CARE 34 : 1934–1942.
72. ZolfaghariM, MousavifarSA, PedramS, HaghaniH (2012) The impact of nurse short message services and telephone follow-ups on diabetic adherence: which one is more effective? J Clin Nurs 21 : 1922–1931.
73. LimS, KangSM, ShinH, LeeHJ, Won YoonJ, et al. (2011) Improved glycemic control without hypoglycemia in elderly diabetic patients using the ubiquitous healthcare service, a new medical information system. DIABETES CARE 34 : 308–313.
74. StockwellMS, KharbandaEO, MartinezRA, VargasCY, VawdreyDK, et al. (2012) Effect of a text messaging intervention on influenza vaccination in an urban, low-income pediatric and adolescent population: a randomized controlled trial. JAMA 307 : 1702–1708.
75. LakkisNA, AtfehAM, El-ZeinYR, MahmassaniDM, HamadehGN (2011) The effect of two types of sms-texts on the uptake of screening mammogram: a randomized controlled trial. Preventive Medicine 53 : 325–327.
76. BlascoA, CarmonaM, Fernandez-LozanoI, SalvadorCH, PascualM, et al. (2012) Evaluation of a telemedicine service for the secondary prevention of coronary artery disease. J Cardiopulm Rehabil Prev 32 : 25–31.
77. MorikawaN, YamasueK, TochikuboO, MizushimaS (2011) Effect of salt reduction intervention program using an electronic salt sensor and cellular phone on blood pressure among hypertensive workers. Clin Exp Hypertens 33 : 216–222.
78. RyanD, PriceD, MusgraveSD, MalhotraS, LeeAJ, et al. (2012) Clinical and cost effectiveness of mobile phone supported self monitoring of asthma: multicentre randomised controlled trial. BMJ 344: e1756.
79. PrabhakaranL, CheeWY, ChuaKC, AbisheganadenJ, WongWM (2010) The use of text messaging to improve asthma control: a pilot study using the mobile phone short messaging service (SMS). Journal of Telemedicine and Telecare 16 : 286–290.
80. HalpinDMG, Laing-MortonT, SpeddingS, LevyML, CoyleP, et al. (2011) A randomised controlled trial of the effect of automated interactive calling combined with a health risk forecast on frequency and severity of exacerbations of COPD assessed clinically and using EXACT PRO. Primary Care Respiratory Journal 20 : 324–331.
81. KalichmanSC, KalichmanMO, CherryC, SwetzesC, AmaralCM, et al. (2011) Brief behavioral self-regulation counseling for HIV treatment adherence delivered by cell phone: an initial test of concept trial. AIDS Patient Care STDS 25 : 303–310.
82. Pop-ElechesC, ThirumurthyH, HabyarimanaJP, ZivinJG, GoldsteinMP, et al. (2011) Mobile phone technologies improve adherence to antiretroviral treatment in a resource-limited setting: a randomized controlled trial of text message reminders. AIDS 25 : 825–834.
83. HardyH, KumarV, DorosG, FarmerE, DrainoniML, et al. (2011) Randomized Controlled Trial of a Personalized Cellular Phone Reminder System to Enhance Adherence to Antiretroviral Therapy. Aids Patient Care and Stds 25 : 153–161.
84. da CostaTM, BarbosaBJP, CostaDAGE, SigulemD, MarinHD, et al. (2012) Results of a randomized controlled trial to assess the effects of a mobile SMS-based intervention on treatment adherence in HIV/AIDS-infected Brazilian women and impressions and satisfaction with respect to incoming messages. International Journal of Medical Informatics 81 : 257–269.
85. SetoE, LeonardKJ, CafazzoJA, BarnsleyJ, MasinoC, et al. (2012) Mobile Phone-Based Telemonitoring for Heart Failure Management: A Randomized Controlled Trial. Journal of Medical Internet Research 14.
86. ReidSC, KauerSD, KhorAS, HearpsSJC, SanciLA, et al. (2012) Using a mobile phone application in youth mental health An evaluation study. Australian Family Physician 41 : 711–714.
87. KauerSD, ReidSC, CrookeAHD, KhorA, HearpsSJC, et al. (2012) Self-monitoring Using Mobile Phones in the Early Stages of Adolescent Depression: Randomized Controlled Trial. Journal of Medical Internet Research 14 : 15–31.
88. WhittakerR, MerryS, StasiakK, McDowellH, DohertyI, et al. (2012) MEMO-A Mobile Phone Depression Prevention Intervention for Adolescents: Development Process and Postprogram Findings on Acceptability From a Randomized Controlled Trial. Journal of Medical Internet Research 14.
89. CulleyC, EvansJJ (2010) SMS text messaging as a means of increasing recall of therapy goals in brain injury rehabilitation: a single-blind within-subjects trial. Neuropsychological Rehabilitation 20 : 103–119.
90. CastanoPM, BynumJY, AndresR, LaraM, WesthoffC (2012) Effect of Daily Text Messages on Oral Contraceptive Continuation A Randomized Controlled Trial. Obstetrics and Gynecology 119 : 14–20.
91. HouMY, HurwitzS, KavanaghE, FortinJ, GoldbergAB (2010) Using Daily Text-Message Reminders to Improve Adherence With Oral Contraceptives: A Randomized Controlled Trial (vol 116, pg 633, 2010). Obstetrics and Gynecology 116 : 1224–1224.
92. CummingsE, HauserJ, Cameron-TuckerH, FitzpatrickP, JessupM, et al. (2011) Enhancing self-efficacy for self-management in people with cystic fibrosis. Studies in Health Technology & Informatics 169 : 33–37.
93. SakaiT, IwamiT, KitamuraT, NishiyamaC, KawamuraT, et al. (2011) Effectiveness of the new ‘Mobile AED Map’ to find and retrieve an AED: A randomised controlled trial. Resuscitation 82 : 69–73.
94. SirriyehR, LawtonR, WardJ (2010) Physical activity and adolescents: an exploratory randomized controlled trial investigating the influence of affective and instrumental text messages. British Journal of Health Psychology 15 : 825–840.
95. FjeldsoeBS, MillerYD, MarshallAL (2010) MobileMums: a randomized controlled trial of an SMS-based physical activity intervention. Ann Behav Med 39 : 101–111.
96. PrestwichA, PeruginiM, HurlingR (2010) Can implementation intentions and text messages promote brisk walking? A randomized trial. Health Psychology 29 : 40–49.
97. MerchantRM, AbellaBS, AbotsiEJ, SmithTM, LongJA, et al. (2010) Cell phone cardiopulmonary resuscitation: audio instructions when needed by lay rescuers: a randomized, controlled trial. Annals of Emergency Medicine 55 : 538–543.e531.
98. LeeJS, JeonWC, AhnJH, ChoYJ, JungYS, et al. (2011) The effect of a cellular-phone video demonstration to improve the quality of dispatcher-assisted chest compression-only cardiopulmonary resuscitation as compared with audio coaching. Resuscitation 82 : 64–68.
99. SemeraroF, TaggiF, TammaroG, ImbriacoG, MarchettiL, et al. (2011) iCPR: a new application of high-quality cardiopulmonary resuscitation training. Resuscitation 82 : 436–441.
100. LiuWT, HuangCD, WangCH, LeeKY, LinSM, et al. (2011) A mobile telephone-based interactive self-care system improves asthma control. European Respiratory Journal 37 : 310–317.
101. PetrieKJ, PerryK, BroadbentE, WeinmanJ (2012) A text message programme designed to modify patients' illness and treatment beliefs improves self-reported adherence to asthma preventer medication. Br J Health Psychol 17 : 74–84.
102. SchroederK, FaheyT, EbrahimS (2008) Interventions for improving adherence to treatment in patients with high blood pressure in ambulatory settings. The Cochrane Library
103. SchedlbauerA, SchroederK, PetersT, FaheyT (2004) Interventions to improve adherence to lipid lowering medication. Cochrane Database Syst Rev 4.
104. HaynesRB, AcklooE, SahotaN, McDonaldHP, YaoX (2008) Interventions for enhancing medication adherence. Cochrane database syst Rev 2.
105. ShawK, GennatH, O'RourkeP, Del MarC (2006) Exercise for overweight or obesity. Cochrane Database Syst Rev CD003817.
106. ShawK, O'RourkeP, Del MarC, KenardyJ (2005) Psychological interventions for overweight or obesity. Cochrane Database Syst Rev CD003818.
107. Guerrierra C, Cairns J, Roberts I, Rodgers A, Whittaker R The cost effectiveness of mobile phone text messaging support for smoking cessation:txt2stop trial.
108. Medical Research Council (2000) A framework for development and evaluation of RCTs for complex interventions to improve health. London, Medical Research Council
109. DukeS, ColagiuriS, ColagiuriR (2009) Individual patient education for people with type 2 diabetes mellitus. Cochrane Database Syst Rev 1.
110. VermeireE, WensJ, Van RoyenP, BiotY, HearnshawH, et al. (2005) Interventions for improving adherence to treatment recommendations in people with type 2 diabetes mellitus. Cochrane Database Syst Rev 2.
111. GlynnLG, MurphyAW, SmithSM, SchroederK, FaheyT (2010) Self-monitoring and other non-pharmacological interventions to improve the management of hypertension in primary care: a systematic review. The British Journal of General Practice 60: e476.
112. FreeC, WhittakerR, KnightR, AbramskyT, RodgersA, et al. (2009) Txt2stop: a pilot randomised controlled trial of mobile phone-based smoking cessation support. Tob Control 18 : 88–91.
113. HaugS, MeyerC, SchorrG, BauerS, JohnU (2009) Continuous individual support of smoking cessation using text messaging: a pilot experimental study. Nicotine & Tobacco Research 11 : 915–923.
114. VidrineDJ, ArduinoRC, LazevAB, GritzER (2006) A randomized trial of a proactive cellular telephone intervention for smokers living with HIV/AIDS. AIDS 20 : 253–260.
115. KingAC, AhnDK, OliveiraBM, AtienzaAA, CastroCM, et al. (2008) Promoting physical activity through hand-held computer technology. American Journal of Preventive Medicine 34 : 138–142.
116. LiuWT, WangCH, LinHC, LinSM, LeeKY, et al. (2008) Efficacy of a cell phone-based exercise programme for COPD. European Respiratory Journal 32 : 651–659.
117. NguyenHQ, GillDP, WolpinS, SteeleBG, BendittJO (2009) Pilot study of a cell phone-based exercise persistence intervention post-rehabilitation for COPD. International Journal of Copd 4 : 301–313.
118. PrestwichA, PeruginiM, HurlingR (2009) Can the effects of implementation intentions on exercise be enhanced using text messages? Psychology & Health 24 : 677–687.
119. AtienzaAA, KingAC, OliveiraBM, AhnDK, GardnerCD (2008) Using hand-held computer technologies to improve dietary intake. American Journal of Preventive Medicine 34 : 514–518.
120. EllrottT, AustelA, RademacherC, OberritterH, BeneckeR, et al. (2005) Self-help programme for weight reduction with and without support by a handheld nutrition computer. [German]. Ernahrungs Umschau 52.
121. HaapalaI, BarengoNC, BiggsS, SurakkaL, ManninenP (2009) Weight loss by mobile phone: a 1-year effectiveness study. Public Health Nutrition 12 : 2382–2391.
122. PatrickK, RaabF, AdamsMA, DillonL, ZabinskiM, et al. (2009) A text message-based intervention for weight loss: randomized controlled trial. Journal of Medical Internet Research 11: e1.
123. ShapiroJR, BauerS, HamerRM, KordyH, WardD, et al. (2008) Use of text messaging for monitoring sugar-sweetened beverages, physical activity, and screen time in children: a pilot study. Journal of Nutrition Education & Behavior 40 : 385–391.
124. ShayLE, SeibertD, WattsD, SbroccoT, PagliaraC (2009) Adherence and weight loss outcomes associated with food-exercise diary preference in a military weight management program. Eating Behaviors 10 : 220–227.
125. Stewart AgrasW, Barr TaylorC, FeldmanDE, LoschM, BurnettKF (1990) Developing computer-assisted therapy for the treatment of obesity. Behavior Therapy 21 : 99–109.
126. Turner-McGrievyGM, CampbellMK, TateDF, TruesdaleKP, BowlingJM, et al. (2009) Pounds Off Digitally study: a randomized podcasting weight-loss intervention. American Journal of Preventive Medicine 37 : 263–269.
127. DelamereS, DooleyS, HarringtonL, KingA, MulcahyF (2006) Safer sex text messages: Evaluating a health education intervention in an adolescent population. Sexually Transmitted Infections 82: A27–A27.
128. JonesR (2008) Soap opera video on handheld computers to reduce young urban women's HIV sex risk. AIDS and Behavior 12 : 876–884.
129. LimMSC, HockingJS, AitkenCK, JordanL, FairleyCK, et al. (2007) A randomized controlled trial of the impact of email and text (SMS) messages on the sexual health of young people. Sexual Health 4 : 290–290.
130. WeitzelJA, BernhardtJM, UsdanS, MaysD, GlanzK (2007) Using wireless handheld computers and tailored text messaging to reduce negative consequences of drinking alcohol. Journal of Studies on Alcohol & Drugs 68 : 534–537.
131. ChoaM, ChoJ, ChoiYH, KimS, SungJM, et al. (2009) Animation-assisted CPRII program as a reminder tool in achieving effective one-person-CPR performance. Resuscitation 80 : 680–684.
132. YangC-W, WangH-C, ChiangW-C, HsuC-W, ChangW-T, et al. (2009) Interactive video instruction improves the quality of dispatcher-assisted chest compression-only cardiopulmonary resuscitation in simulated cardiac arrests. Critical Care Medicine 37 : 490–495.
133. BolleSR, SchollJ, GilbertM (2009) Can video mobile phones improve CPR quality when used for dispatcher assistance during simulated cardiac arrest? Acta Anaesthesiologica Scandinavica 53 : 116–120.
134. Cho JH, Lee HC, Lim DJ, Kwon HS, Yoon KH (2009) Mobile communication using a mobile phone with a glucometer for glucose control in Type 2 patients with diabetes: as effective as an Internet-based glucose monitoring system. Journal of Telemedicine and Telecare. pp. 77–82.
135. FranklinVL, WallerA, PagliariC, GreeneSA (2006) A randomized controlled trial of Sweet Talk, a text-messaging system to support young people with diabetes. Diabetic Medicine 23 : 1332–1338.
136. HanauerDA, WentzellK, LaffelN, LaffelLM (2009) Computerized Automated Reminder Diabetes System (CARDS): e-mail and SMS cell phone text messaging reminders to support diabetes management. Diabetes Technol Ther 11 : 99–106.
137. HolmanRR, SmaleAD, PembertonE, RiefflinA, NealonJL (1996) Randomized controlled pilot trial of a hand-held patient-oriented, insulin regimen optimizer. Medical Informatics 21 : 317–326.
138. Istepanian RS, Zitouni K, Harry D, Moutosammy N, Sungoor A, et al.. (2009) Evaluation of a mobile phone telemonitoring system for glycaemic control in patients with diabetes. Journal of Telemedicine and Telecare. pp. 125–128.
139. KIM Cea (2007) Internet Diabetic Patient Management Using a Short Messaging Service Automatically Produced by a Knowledge Matrix System. DIABETES CARE 30.
140. QuinnCC, CloughSS, MinorJM, LenderD, OkaforMC, et al. (2008) WellDoc mobile diabetes management randomized controlled trial: change in clinical and behavioral outcomes and patient and physician satisfaction. Diabetes Technol Ther 10 : 160–168.
141. RamiB, PopowC, HornW, WaldhoerT, SchoberE (2006) Telemedical support to improve glycemic control in adolescents with type 1 diabetes mellitus. European Journal of Pediatrics 165 : 701–705.
142. SchrezenmeirJ, DirtingK, PapazovP (2002) Controlled multicenter study on the effect of computer assistance in intensive insulin therapy of type 1 diabetics. Computer Methods & Programs in Biomedicine 69 : 97–114.
143. Liu W, Wang CH, Huang CD, Kuo HP (2007) A novel mobile phone-based self-care system improves asthma control [Abstract]. American Thoracic Society International Conference, May 18–23, 2007, San Francisco, California, USA. pp. [A93].
144. MeltzerEO, KelleyN, HovellMF (2008) Randomized, Cross-Over Evaluation of Mobile Phone vs Paper Diary in Subjects with Mild to Moderate Persistent Asthma. Open Respir Med J 2 : 72–79.
145. MosnaimGS, CohenMS, RhoadsCH, RittnerSS, PowellLH (2008) Use of MP3 players to increase asthma knowledge in inner-city African-American adolescents. International Journal of Behavioral Medicine 15 : 341–346.
146. StrandbygaardU, ThomsenSF, BackerV (2010) A daily SMS reminder increases adherence to asthma treatment: a three-month follow-up study. Respiratory Medicine 104 : 166–171.
147. Marquez ContrerasE, de la Figuera von WichmannM, Gil GuillenV, Ylla-CatalaA, FiguerasM, et al. (2004) [Effectiveness of an intervention to provide information to patients with hypertension as short text messages and reminders sent to their mobile phone (HTA-Alert)]. Atencion Primaria 34 : 399–405.
148. MossoJL, GoriniA, De La CerdaG, ObradorT, AlmazanA, et al. (2009) Virtual reality on mobile phones to reduce anxiety in outpatient surgery. Studies in Health Technology & Informatics 142 : 195–200.
149. RivaG, GrassiA, VillaniD, GaggioliA, PreziosaA (2007) Managing exam stress using UMTS phones: the advantage of portable audio/video support. Studies in Health Technology & Informatics 125 : 406–408.
150. PatelA, SchiebleT, DavidsonM, TranMCJ, SchoenbergC, et al. (2006) Distraction with a hand-held video game reduces pediatric preoperative anxiety. Paediatric Anaesthesia 16 : 1019–1027.
151. RivaG, PreziosaA, GrassiA, VillaniD (2006) Stress management using UMTS cellular phones: a controlled trial. Studies in Health Technology & Informatics 119 : 461–463.
152. PijnenborgGHM, WithaarFK, BrouwerWH, TimmermanME, van den BoschRJ, et al. (2010) The efficacy of SMS text messages to compensate for the effects of cognitive impairments in schizophrenia. British Journal of Clinical Psychology 49 : 259–274.
153. GrassiA, GaggioliA, RivaG (2009) The green valley: the use of mobile narratives for reducing stress in commuters. Cyberpsychology & Behavior 12 : 155–161.
154. GoriniA, PallaviciniF, AlgeriD, RepettoC, GaggioliA, et al. (2010) Virtual reality in the treatment of generalized anxiety disorders. Studies in Health Technology & Informatics 154 : 39–43.
155. KearneyN, McCannL, NorrieJ, TaylorL, GrayP, et al. (2009) Evaluation of a mobile phone-based, advanced symptom management system (ASyMS) in the management of chemotherapy-related toxicity. Supportive Care in Cancer 17 : 437–444.
156. ScherrD, KastnerP, KollmannA, HallasA, AuerJ, et al. (2009) Effect of home-based telemonitoring using mobile phone technology on the outcome of heart failure patients after an episode of acute decompensation: randomized controlled trial. J Med Internet Res 11: e34.
157. WalkerI, SigouinC, SekJ, AlmonteT, CarruthersJ, et al. (2004) Comparing hand-held computers and paper diaries for haemophilia home therapy: a randomized trial. Haemophilia 10 : 698–704.
158. ChoiJI, KimHB, KimMJ, LeeJS, KohYW, et al. (2011) Noncontrast chest computed tomography immediately after transarterial chemoembolization in patients with hepatocellular carcinoma: clinical benefits and effect of radiation reduction on image quality in low-dose scanning. Eur J Radiol 80: e188–194.
159. ChoaM, ParkI, ChungHS, YooSK, ShimH, et al. (2008) The effectiveness of cardiopulmonary resuscitation instruction: animation versus dispatcher through a cellular phone. Resuscitation 77 : 87–94.
160. ZannerR, WilhelmD, FeussnerH, SchneiderG (2007) Evaluation of M-AID, a first aid application for mobile phones. Resuscitation 74 : 487–494.
161. YangCW, WangHC, ChiangWC, ChangWT, YenZS, et al. (2008) Impact of adding video communication to dispatch instructions on the quality of rescue breathing in simulated cardiac arrests-A randomized controlled study. Resuscitation 78 : 327–332.
162. ErtlL, ChristF (2007) Significant improvement of the quality of bystander first aid using an expert system with a mobile multimedia device. Resuscitation 74 : 286–295.
163. CocosilaM, ArcherN, HaynesRB, YuanY (2009) Can wireless text messaging improve adherence to preventive activities? Results of a randomised controlled trial. International Journal of Medical Informatics 78 : 230–238.
164. OllivierL, RomandO, MarimoutouC, MichelR, PognantC, et al. (2009) Use of short message service (SMS) to improve malaria chemoprophylaxis compliance after returning from a malaria endemic area. Malaria Journal 8 : 236.
165. ArmstrongAW, WatsonAJ, MakredesM, FrangosJE, KimballAB, et al. (2009) Text-message reminders to improve sunscreen use: a randomized, controlled trial using electronic monitoring. Archives of Dermatology 145 : 1230–1236.
Štítky
Interní lékařství
Článek vyšel v časopisePLOS Medicine
Nejčtenější tento týden
2013 Číslo 1- Berberin: přírodní hypolipidemikum se slibnými výsledky
- Léčba bolesti u seniorů
- Příznivý vliv Armolipidu Plus na hladinu cholesterolu a zánětlivé parametry u pacientů s chronickým subklinickým zánětem
- Jak postupovat při výběru betablokátoru − doporučení z kardiologické praxe
- Červená fermentovaná rýže účinně snižuje hladinu LDL cholesterolu jako vhodná alternativa ke statinové terapii
-
Všechny články tohoto čísla
- The Effectiveness of Mobile-Health Technologies to Improve Health Care Service Delivery Processes: A Systematic Review and Meta-Analysis
- The Effectiveness of Mobile-Health Technology-Based Health Behaviour Change or Disease Management Interventions for Health Care Consumers: A Systematic Review
- More Data and Appropriate Statistical Methods Needed to Fully Measure the Displacement Effects of Development Assistance for Health
- Preventing Antiretroviral Treatment Interruptions among HIV/AIDS Patients in Africa
- Translating Coverage Gains into Health Gains for All Women and Children: The Quality Care Opportunity
- Implementation of a Mental Health Care Package for Children in Areas of Armed Conflict: A Case Study from Burundi, Indonesia, Nepal, Sri Lanka, and Sudan
- Toward an Understanding of Disengagement from HIV Treatment and Care in Sub-Saharan Africa: A Qualitative Study
- Tackling Non-Communicable Diseases In Low- and Middle-Income Countries: Is the Evidence from High-Income Countries All We Need?
- Change in the Body Mass Index Distribution for Women: Analysis of Surveys from 37 Low- and Middle-Income Countries
- Getting More Generous with the Truth: Clinical Trial Reporting in 2013 and Beyond
- Reducing Vulnerability to Climate Change in Sub-Saharan Africa: The Need for Better Evidence
- Erectile Dysfunction Severity as a Risk Marker for Cardiovascular Disease Hospitalisation and All-Cause Mortality: A Prospective Cohort Study
- Differences in Reporting of Analyses in Internal Company Documents Versus Published Trial Reports: Comparisons in Industry-Sponsored Trials in Off-Label Uses of Gabapentin
- Why Do Women Not Use Antenatal Services in Low- and Middle-Income Countries? A Meta-Synthesis of Qualitative Studies
- Considerations in Assessing the Evidence and Implications of Aid Displacement from the Health Sector
- Prioritizing Congenital Syphilis Control in South China: A Decision Analytic Model to Inform Policy Implementation
- Balancing Community and Hospital Care: A Case Study of Reforming Mental Health Services in Georgia
- PLOS Medicine
- Archiv čísel
- Aktuální číslo
- Informace o časopisu
Nejčtenější v tomto čísle- Differences in Reporting of Analyses in Internal Company Documents Versus Published Trial Reports: Comparisons in Industry-Sponsored Trials in Off-Label Uses of Gabapentin
- The Effectiveness of Mobile-Health Technologies to Improve Health Care Service Delivery Processes: A Systematic Review and Meta-Analysis
- The Effectiveness of Mobile-Health Technology-Based Health Behaviour Change or Disease Management Interventions for Health Care Consumers: A Systematic Review
- Why Do Women Not Use Antenatal Services in Low- and Middle-Income Countries? A Meta-Synthesis of Qualitative Studies
Kurzy
Zvyšte si kvalifikaci online z pohodlí domova
Současné možnosti léčby obezity
nový kurzAutoři: MUDr. Martin Hrubý
Všechny kurzyPřihlášení#ADS_BOTTOM_SCRIPTS#Zapomenuté hesloZadejte e-mailovou adresu, se kterou jste vytvářel(a) účet, budou Vám na ni zaslány informace k nastavení nového hesla.
- Vzdělávání



