-
Články
Top novinky
Reklama- Vzdělávání
- Časopisy
Top články
Nové číslo
- Témata
Top novinky
Reklama- Videa
- Podcasty
Nové podcasty
Reklama- Kariéra
Doporučené pozice
Reklama- Praxe
Top novinky
ReklamaPsychosocial Factors That Shape Patient and Carer Experiences of Dementia Diagnosis and Treatment: A Systematic Review of Qualitative Studies
Background:
Early diagnosis and intervention for people with dementia is increasingly considered a priority, but practitioners are concerned with the effects of earlier diagnosis and interventions on patients and caregivers. This systematic review evaluates the qualitative evidence about how people accommodate and adapt to the diagnosis of dementia and its immediate consequences, to guide practice.Methods and Findings:
We systematically reviewed qualitative studies exploring experiences of community-dwelling individuals with dementia, and their carers, around diagnosis and the transition to becoming a person with dementia. We searched PubMed, PsychINFO, Embase, CINAHL, and the British Nursing Index (all searched in May 2010 with no date restrictions; PubMed search updated in February 2012), checked reference lists, and undertook citation searches in PubMed and Google Scholar (ongoing to September 2011). We used thematic synthesis to identify key themes, commonalities, barriers to earlier diagnosis, and support identified as helpful. We identified 126 papers reporting 102 studies including a total of 3,095 participants. Three overarching themes emerged from our analysis: (1) pathways through diagnosis, including its impact on identity, roles, and relationships; (2) resolving conflicts to accommodate a diagnosis, including the acceptability of support, focusing on the present or the future, and the use or avoidance of knowledge; and (3) strategies and support to minimise the impact of dementia. Consistent barriers to diagnosis include stigma, normalisation of symptoms, and lack of knowledge. Studies report a lack of specialist support particularly post-diagnosis.Conclusions:
There is an extensive body of qualitative literature on the experiences of community-dwelling individuals with dementia on receiving and adapting to a diagnosis of dementia. We present a thematic analysis that could be useful to professionals working with people with dementia. We suggest that research emphasis should shift towards the development and evaluation of interventions, particularly those providing support after diagnosis.
Please see later in the article for the Editors' Summary.
Published in the journal: . PLoS Med 9(10): e32767. doi:10.1371/journal.pmed.1001331
Category: Research Article
doi: https://doi.org/10.1371/journal.pmed.1001331Summary
Background:
Early diagnosis and intervention for people with dementia is increasingly considered a priority, but practitioners are concerned with the effects of earlier diagnosis and interventions on patients and caregivers. This systematic review evaluates the qualitative evidence about how people accommodate and adapt to the diagnosis of dementia and its immediate consequences, to guide practice.Methods and Findings:
We systematically reviewed qualitative studies exploring experiences of community-dwelling individuals with dementia, and their carers, around diagnosis and the transition to becoming a person with dementia. We searched PubMed, PsychINFO, Embase, CINAHL, and the British Nursing Index (all searched in May 2010 with no date restrictions; PubMed search updated in February 2012), checked reference lists, and undertook citation searches in PubMed and Google Scholar (ongoing to September 2011). We used thematic synthesis to identify key themes, commonalities, barriers to earlier diagnosis, and support identified as helpful. We identified 126 papers reporting 102 studies including a total of 3,095 participants. Three overarching themes emerged from our analysis: (1) pathways through diagnosis, including its impact on identity, roles, and relationships; (2) resolving conflicts to accommodate a diagnosis, including the acceptability of support, focusing on the present or the future, and the use or avoidance of knowledge; and (3) strategies and support to minimise the impact of dementia. Consistent barriers to diagnosis include stigma, normalisation of symptoms, and lack of knowledge. Studies report a lack of specialist support particularly post-diagnosis.Conclusions:
There is an extensive body of qualitative literature on the experiences of community-dwelling individuals with dementia on receiving and adapting to a diagnosis of dementia. We present a thematic analysis that could be useful to professionals working with people with dementia. We suggest that research emphasis should shift towards the development and evaluation of interventions, particularly those providing support after diagnosis.
Please see later in the article for the Editors' Summary.Introduction
Dementia affects one in 20 people over the age of 65 and one in five over the age of 80. World-wide there are an estimated 35.6 million people with dementia. By 2050 this number will rise to over 115 million [1]. In 2010 the total estimated worldwide costs of dementia were US$604 billion, with 70% of the costs occurring in western Europe and North America [2]. There is evidence that many patients who meet the criteria for dementia never receive a formal diagnosis [3]–[6] or receive a diagnosis only late in the disease trajectory [7]. There remains wide variability in current practice and attitudes to diagnostic disclosure [8], with some professionals worried about the possible harm of early diagnosis of a condition widely seen as untreatable and life-changing [9]. There is, however, growing support for early diagnosis [10]–[12], as it may improve quality of life for patients and carers, delay or prevent care home admissions [13],[14], and facilitate referral to specialist services and treatment [11],[15].
There is increasing recognition of the importance of systematically reviewing qualitative research [16], as it allows the development of in-depth understanding of persistent themes, explores transferability, and prevents unnecessary duplication of research. Previous reviews have looked at patient and carer experiences of dementia [17],[18] and disclosure of diagnosis [8],[19],[20], but none, to our knowledge, has performed a comprehensive thematic synthesis of qualitative studies exploring the experiences of people with dementia and their family members of receiving and adapting to a diagnosis, and of service delivery. Our aim was to inform the debate about early diagnosis and service provision by systematically reviewing qualitative literature on the psychosocial factors that shape patient and carer experiences of diagnosis and early treatment. We aimed to identify the following: key themes, commonalities, and differences across groups; barriers to early diagnosis; and which support services individuals newly diagnosed with dementia and their carers perceive as helpful.
Methods
Selection Criteria
We included qualitative studies that explored patient and carer experiences around diagnosis and treatment of dementia or mild cognitive impairment (MCI). This included studies from any established qualitative tradition and using any recognised qualitative methodology. Mixed method studies were included if they had a qualitative element, but only the qualitative data were used in the analysis. The main outcomes of interest were patient and carer attitudes, beliefs, and feelings around becoming or caring for an individual with dementia. In particular we searched for data on responses to early signs of dementia, receiving and adapting to a diagnosis, and experiences of post-diagnosis support. We focused on community-dwelling participants and excluded studies in long-term care settings or published in languages other than English. The reporting of the review follows PRISMA guidance (Text S1), and the methods for the review were pre-specified in a protocol (Text S2).
Search Strategy
We searched for all potentially relevant published and unpublished literature, with no date restrictions, and regardless of country of origin. Studies were identified by computerised searches of PubMed (1950–2012), PsychINFO (Ovid) (1806–2010), Embase (Ovid) (1980–2010), CINAHL (EBSCO Publishing) (1980–2010), and the British Nursing Index (NHS Evidence) (1985–2010). An example search query is given in Box 1. In addition, we employed extensive lateral search techniques (ongoing March 2010–September 2011), such as checking reference lists, performing key word searches in Google Scholar, contacting experts, and using the “cited by” option in Google Scholar and the “related articles” option in PubMed. Such lateral search strategies have been shown to be particularly important for identifying non-randomised studies [21]. The original electronic database searches were conducted between March and May 2010, with the PubMed search updated in February 2012.
Box 1. Example Search Query
The following search query was used for the PubMed searches* (May 2010, updated February 2012):
(disability OR disablement OR aware OR awareness OR self OR fear OR emotions OR “self concept” OR self assessment OR “self care” OR adaptation OR stress OR autonomy OR denial OR sick role OR coping OR cope OR patient participation OR self disclosure OR life [ti] OR live [ti] or living [ti]) AND (confusion OR memory loss OR “early dementia” OR “mild dementia” OR “moderate dementia” OR alzheimers OR mild cognitive disorder OR (MCI (cognition disorder AND (mild OR moderate OR early)))) AND (caregivers OR social support OR self-help groups OR relatives OR carers OR health care staff OR spouses OR dyadic OR partner OR communication OR nursing)
*Search terms were adapted for other databases.
Data Extraction and Critical Appraisal
Two reviewers independently screened titles and abstracts identified by the electronic search, applied the selection criteria to potentially relevant papers, and extracted data using a standardised checklist. Where results of a study were reported in more than one publication, we grouped reports together and marked the publication with the most complete data as the primary reference; the other papers describing the same study were classified as associated papers. We collected data on study design (including theoretical framework), aims, methods, participant characteristics, areas covered (e.g., symptom recognition, receiving a diagnosis, adjusting to a diagnosis, and issues relating to service delivery), and common themes.
Two reviewers independently assessed study quality using a checklist based on Spencer et al.'s framework for assessing quality in qualitative research [22]. This framework has been adapted by one of the authors and used in previous work [23],[24]. In addition, the overall reliability and usefulness of the study to the research questions was graded as low, medium, or high. Reliability related to the quality of the study, and usefulness to the relevancy of a paper in the context of our review. The core quality assessment principles are summarised in Table 1. Data compiled by the two reviewers were compared for agreement, and any discrepancies were resolved by discussion or by consultation with a third researcher. As there is no consensus or empirically tested method for excluding qualitative studies from reviews on the basis of quality, we included all studies regardless of their quality.
Tab. 1. Core principles of study quality assessment. 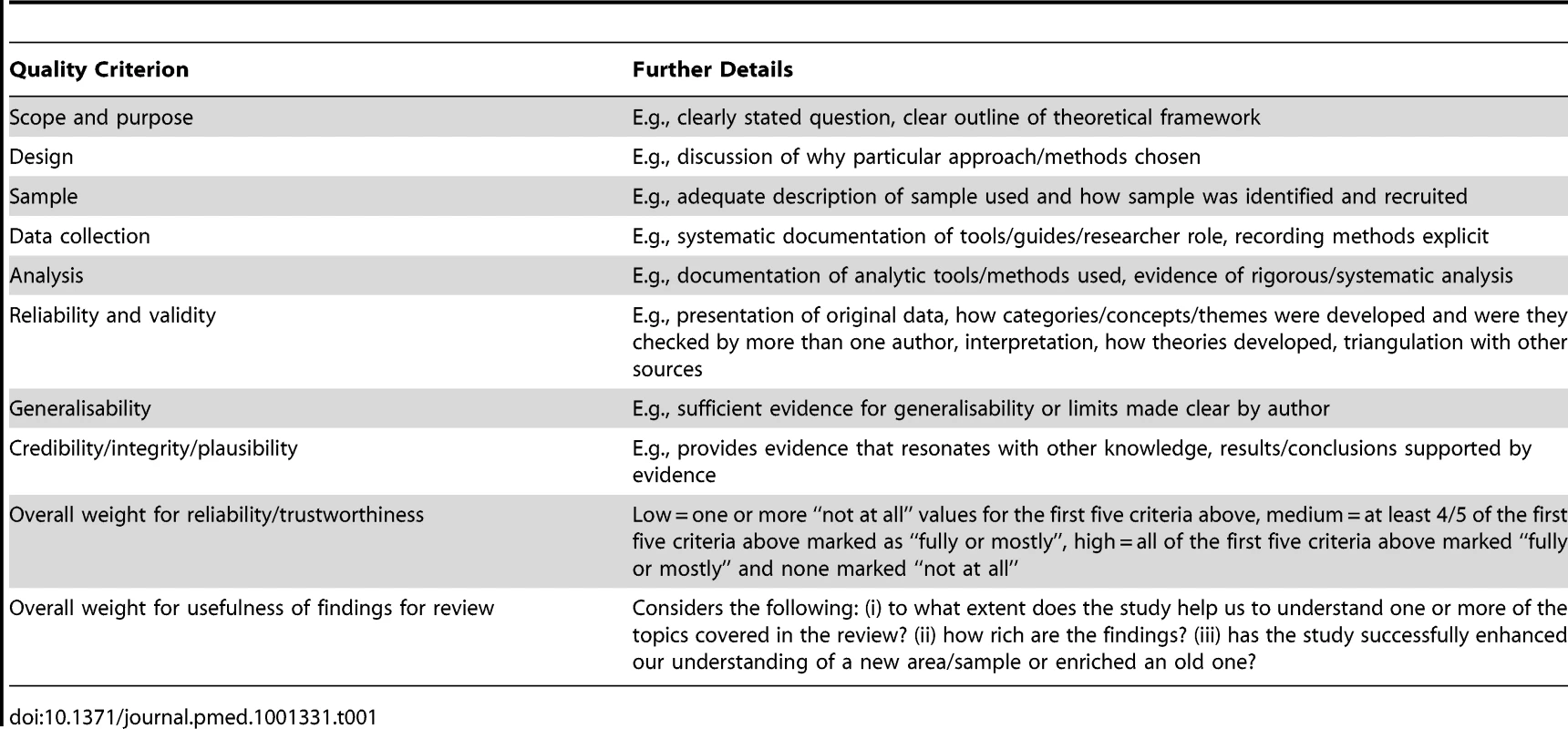
Analysis
We synthesised our study findings using thematic analysis. This process, which involves identifying prominent or recurring themes, has previously been used to successfully synthesise a large number of studies [25], and draws on existing literature around the synthesis of qualitative research [26]–[29]. Defining what counts as “data” in qualitative research is not straightforward [29]. We took the approach suggested by Thomas and Harden [29] and took “data” to be not just that in the form of quotations but all of the text labelled as “results” or “findings” in study reports.
Studies judged to have met the inclusion criteria were independently reviewed and coded by two reviewers by hand. They applied open codes to text, identified themes, and documented supporting evidence in the form of quotes. From this, a list of initial codes and themes was created. These codes were then inserted into qualitative analysis software (NVivo), and PDFs of all included studies were imported for further analysis. The use of such software can facilitate the development of themes and allow reviewers to examine the contribution made to their findings by individual studies or groups of studies [29]. Analysis in NVivo involved examination of concepts for similarities and differences, refinement of descriptive themes, verification that data was a “good fit” for the themes, and development of analytic themes. We then undertook a final process of verification using the 28 studies that had scored high for both reliability and usefulness.
Ethical Approval
Ethical approval was not required for this work.
Results
Description of Studies
In all, 126 papers met our inclusion criteria. Of those, 102 were classified as primary studies [30]–[131], and a further 24 as associated papers [132]–[155]. The links between primary and associated papers can be seen in Table S1. An overview of the selection process can be seen in Figure 1.
Fig. 1. Flow chart of study selection process. 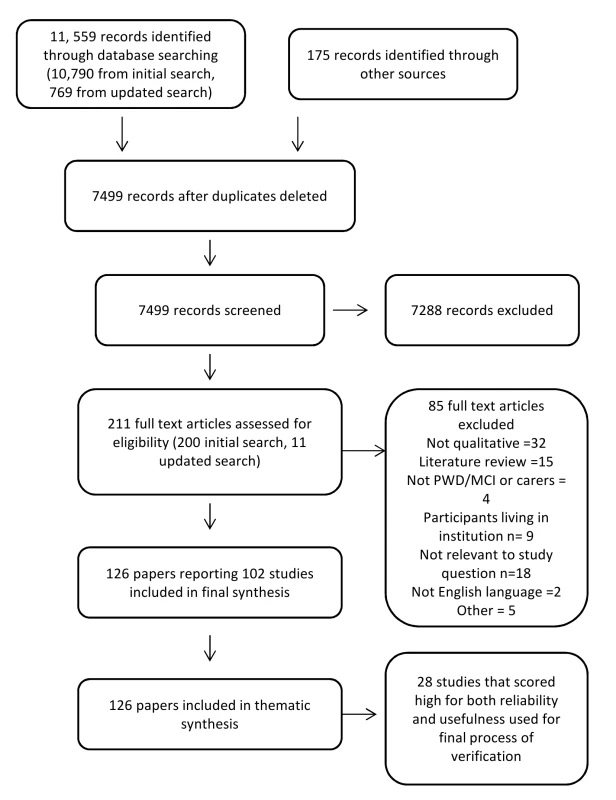
PWD, person with dementia. Studies included a total of 3,095 participants: 1,145 individuals with dementia or MCI and 1,950 informal carers. We found studies conducted in 14 different countries, although the majority (76%) were from the UK or North America. Study characteristics are summarised in Table 2, with details of individual studies provided in Table S1. Participants were community-dwelling, the majority lived with a carer, and they were predominantly white. However, 16 studies [32],[42],[66],[67],[70],[72],[74],[85],[86],[88],[92],[98]–[100],[118],[122] either focused on the views and experiences of black and minority ethnic groups in the UK and North America or compared the views of different ethnic groups.
Tab. 2. Overview of study characteristics. 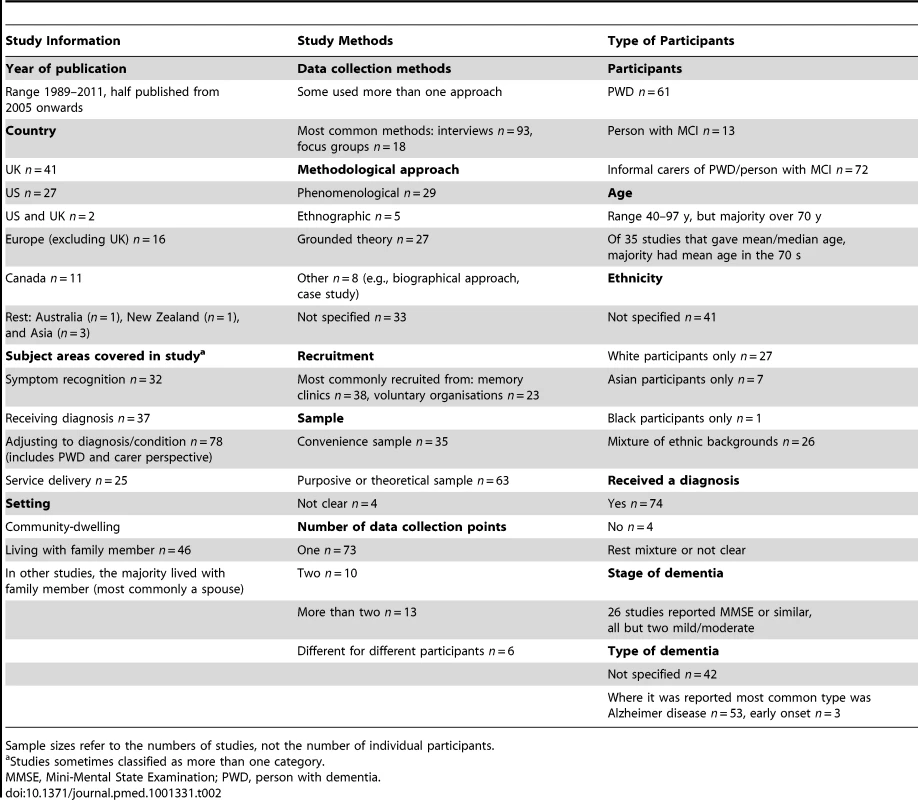
Sample sizes refer to the numbers of studies, not the number of individual participants. Study Quality
Overall, 32% of the studies scored high for reliability, 32% medium, and 35% low, and 57% scored high, 30% medium, and 13% low for usefulness; 27% scored high for both reliability and usefulness. A summary of individual quality assessment scores can be found in Table S1 and of overall quality assessment domains in Figure 2.
Fig. 2. Summary of quality assessment domains. 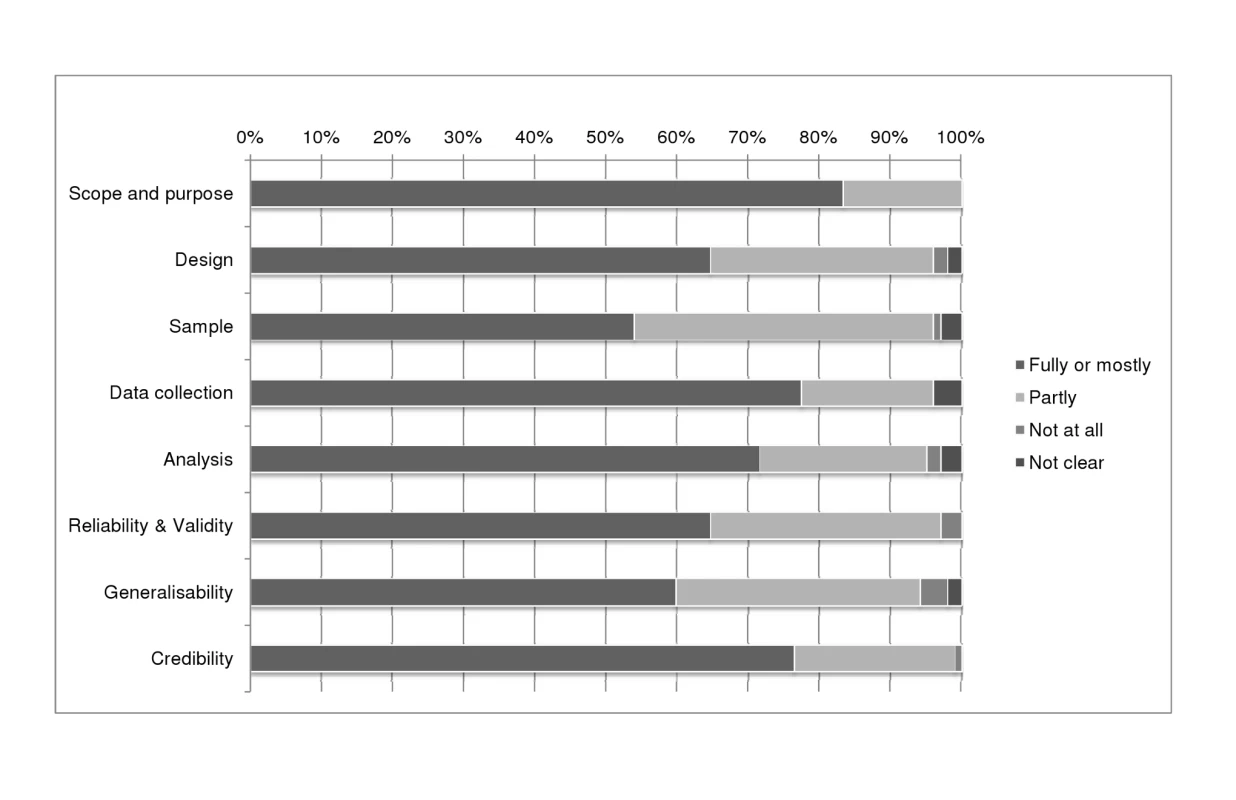
This figure shows review authors' judgements about each quality domain presented as percentages across all included studies. Findings from the Thematic Analysis
We identified three overarching thematic categories as being central to the process of receiving and adapting to a diagnosis of dementia: (1) pathways through diagnosis (including barriers and facilitators of earlier diagnosis, and the challenge of the diagnosis to identity, roles, and relationships); (2) conflicts that need to be resolved to accommodate the diagnosis (including the acceptability or otherwise of support, autonomy versus safety, the need to focus on today or tomorrow, and the usefulness or harmfulness of knowledge); and (3) living with dementia (including practical strategies to minimise the impact of dementia, and the support that professionals and agencies can give) (see Figure 3). The evidence to support these themes can be seen in Table S2.
Fig. 3. Themes and subthemes. 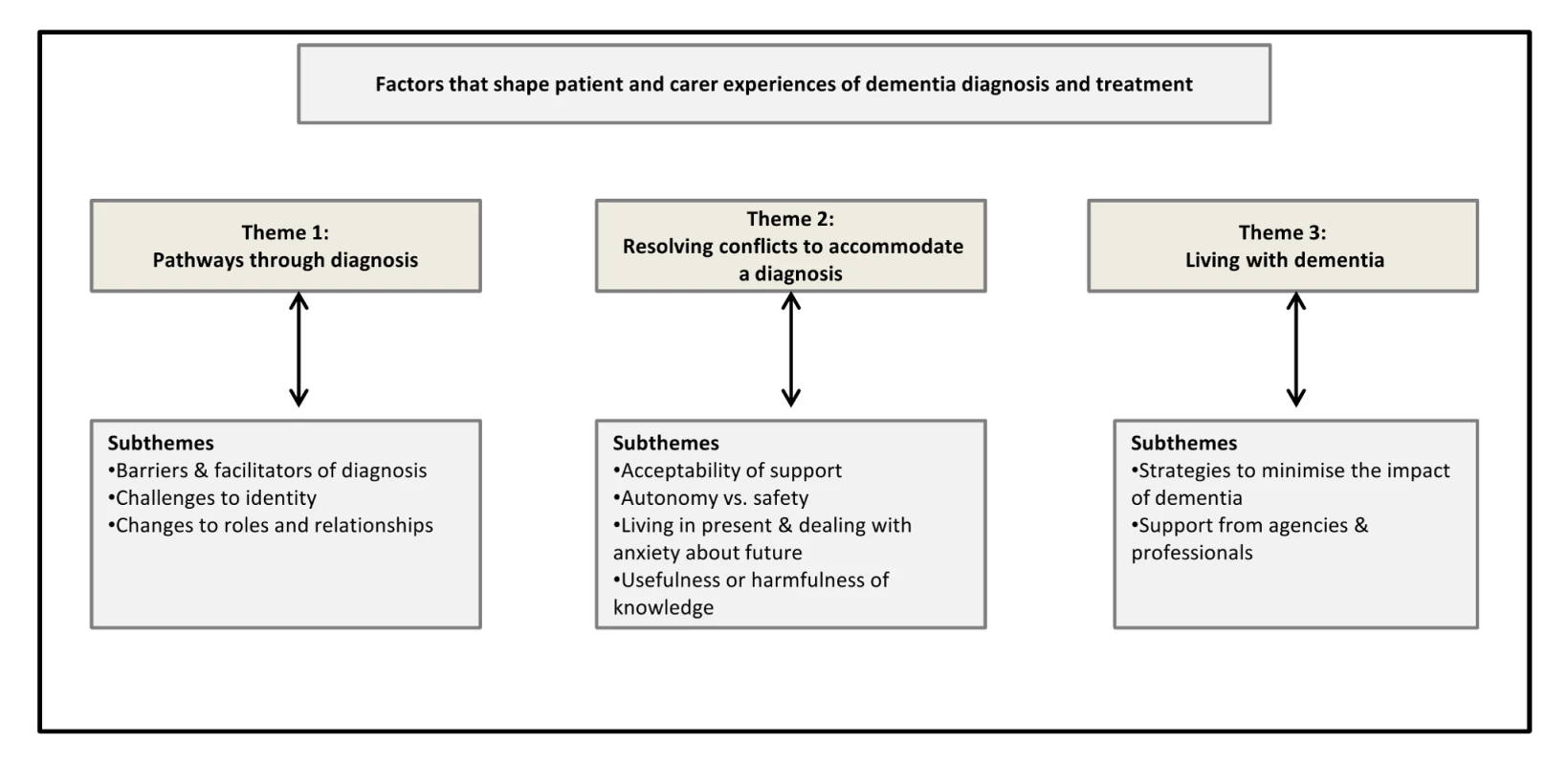
This figure shows the three overarching themes and the related subthemes that emerged from our analysis. The themes apply both to the individuals with dementia and to their family carer/s, and are not necessarily sequential but are interlinked and reflect ongoing processes of adjustment that can occur from the moment symptoms of dementia appear. Quotes supporting each theme are presented in Table S3. Each thematic category is discussed in more detail below. Supporting citations in the text are representative rather than comprehensive.
Theme 1: Pathways through Diagnosis
Barriers to early diagnosis
Among our sample, persistent barriers to early diagnosis were stigma, the normalisation of symptoms, and a lack of awareness about the signs and symptoms of dementia. It often took a trigger event or tipping point such as a hospitalisation or bereavement [34],[37],[40],[42],[51],[53],[92],[114],[118],[138] before people sought help. Family members often recognised something was wrong before the person with dementia did, and were frequently instrumental in obtaining a diagnosis [32],[40],[41],[45],[54],[72],[88],[115],[129]. There was evidence of greater stigma among minority ethnic populations and evidence that they were less likely to recognise symptoms of dementia as an illness than white individuals, and more likely to ascribe these symptoms to the ageing process [32],[86],[118],[119]. In addition, symptoms of dementia were sometimes given cultural or religious explanations [118]. As many studies did not provide detailed demographic information, it was unclear whether level of education or socioeconomic status impacted on awareness of dementia and help-seeking behaviour. Studies suggest that in some cases doctors are slow to recognise symptoms or reluctant to give a diagnosis [38],[39],[68],[74],[88],[92],[124], and that even when people have been referred to memory services the process may be slow, with long periods of waiting [93],[152].
Impact of diagnosis
Regardless of culture and context, we found many similarities in individual's experiences of becoming a person with dementia. Dementia had an enormous impact on identity [72],[91],[121], leading to feelings of loss, anger, uncertainty, and frustration. [33],[37],[50],[53],[58]–[61],[77],[79],[109]. People with dementia struggled to preserve aspects of their former self and were often supported in this by family carers, who focused on remaining abilities rather than drawing attention to mistakes [109],[144]. Dementia also had a significant impact on roles and relationships, both within the family and in wider social networks. A desire to preserve a pre-dementia identity sometimes led to people being reluctant to disclose their diagnosis to family or wider social networks [52],[53],[109], which could lead to social isolation [53],[62],[105]. Despite this, some studies suggested that eventually both the individuals with dementia and their carers reached a state of acceptance [36],[45],[88],[91].
Unsurprisingly, our analysis revealed that dementia had a significant impact on both the individuals with dementia and their families. Spouses had to adjust to increasingly unequal relationships [30],[54],[63],[64],[97],[104],[114],[123],[125], and communication between the couple was often affected. However, studies looking at the experiences of couples often found an emphasis on working together as a team, with a high degree of mutuality [39],[50],[88],[91],[110],[134]. It was clear that there was often significant strain on carers [39],[42],[44],[56],[109],[119],[123],[127], which often impacted adversely on their own health [43],[44],[61],[78],[117].
For some individuals, receiving a diagnosis was the beginning of the adjustment process, but for others, who had been experiencing symptoms for some time, considerable adjustment had already preceded the diagnosis. Although diagnosis was often traumatic [38],[50],[51],[62],[152], the validation of suspicions could come as a relief [45],[93],[129]. There was also a proportion of individuals with dementia and carers who continued to consider memory loss insignificant even after diagnosis [51],[93],[119].
Theme 2: Resolving Conflicts to Accommodate a Diagnosis
Among our sample, beliefs about, and perceptions of, dementia varied considerably, with meanings attached to a diagnosis being shaped by the individual's current situation, by past experiences, and by exposure to others with dementia. For example, families that included a member with professional experience of dementia or who had a relative with dementia were more likely to completely acknowledge a diagnosis than those who had had no previous exposure to dementia [84]. Adjusting to a diagnosis is a complex process, and a number of ambiguities and polarised findings emerged from our analysis (see Box 2). These ambiguities represent conflicts that may need to be resolved in order to accommodate a diagnosis.
Box 2. Polarised Findings
-
Reactions to, and readiness for, a diagnosis may vary between individuals and between the individuals with dementia and their family/carers.
-
Individuals with dementia and their families/carers may struggle to preserve a pre-dementia identity whilst also adapting to a diagnosis and assimilating the disease into a new identity.
-
Carers may be torn between protecting the person with dementia and promoting their independence.
-
Individuals with dementia and their carers may focus on the present whilst also experiencing anxiety about the future.
-
There can be a tension between a desire to maintain social contacts and strategies to minimise or normalise the impact of dementia.
-
Information may be empowering for some people, but others may reject new knowledge and resist a diagnosis.
-
Peer support is often beneficial but can have a negative impact by showing what the future may hold.
Studies identified the potential conflict that could arise as people strove to preserve identity and autonomy in the face of increasing symptoms. This sometimes led to an apparent unawareness of or a resistance to acknowledge a diagnosis [37]. Study authors did not, however, interpret this simply as denial but rather as a self-maintaining strategy [136] or a deliberate choice to be seen as an agent rather than an object [90]. This was reflected in individual's attitudes towards information, and there was evidence that some people with dementia and their carers actively sought information [89],[90], whereas others rejected new knowledge. However, understanding of, and attitudes towards, dementia were not fixed, and evolved throughout the disease trajectory.
Theme 3: Living with Dementia
This theme relates to the strategies that individuals with dementia and their families adopted to deal with the impact of dementia on their lives, and also to the support they required from professionals and agencies. The adoption of strategies to manage the disease, minimise losses, reduce social isolation, and maintain normalcy was common [50],[58],[69],[90],[134]. This included practical strategies such as using reminders or prompts, social strategies such as relying on family support, and emotional strategies such as using humour or finding meaningful activity.
Supporting People with Dementia and Their Carers
The general practitioner or family physician was generally the first point of contact for people with dementia and their carers [43],[93] and had an important role to play in facilitating service access [43],[74]. However, in our sample, experiences were mixed, with some participants reporting a delay in referral to memory services and others reporting confidentiality obstacles, with doctors reluctant to talk to carers about their family member with dementia [74],[88],[106],[124]. Attending memory clinics could be shocking or frightening [51],[75],[94], and receiving a diagnosis could lead to increased tension as someone negotiated a new identity as a person with dementia [37].
There was a clear need for greater support after diagnosis [78], including advice [61],[129], social and psychological support [61],[125], access to community care [43],[93], and respite [127]. There was evidence that valuable support was provided by voluntary organisations such as the Alzheimer's Society [93],[106],[114], although signposting to these needed to be improved [61]. Information provision was seen as key in many studies, but it was clear that better knowledge sharing at point of diagnosis was not always the solution [152]. The information needs of patients varied over time, and information provision needed to be ongoing, with flexibility in timing and format [93],[106].
Amongst people with Alzheimer disease and their family carers, there was variation in perceptions of the benefits of acetylcholinesterase inhibitors, with some studies reporting that medication gave people hope [48],[71],[97],[111],[121],[152], one study reporting that patients and their carers felt that the benefits were not clear but they were “worth a try” [71], and two studies reporting that patients felt medication had little to offer them [62],[106]. Studies suggested that there was now an increasing expectation that medication would be available [93], that attitudes towards medication got less positive over time [49], and that drug treatment was often initiated by the carer [71].
Amongst our sample it was clear that many people found peer support valuable [37],[38],[72],[93],[129],[131]. However, for others there could be negative consequences, as the inclusion of people at different stages in the dementia trajectory could make people aware of what the future held for them [37]. The timing of referral to community-based support groups may be key [43],[78],[106], and such decisions are likely to be facilitated by continuous therapeutic relationships between individuals with dementia and the practitioners involved in their care.
Discussion
We found 102 studies exploring the experiences of community-dwelling individuals with dementia or MCI, and their family carers, of diagnosis, treatment, and the transition to becoming a person with dementia. What emerged from our analysis was the complexity and variety of responses to becoming a person with dementia, and how this makes diagnosing and supporting this group particularly challenging. There were many commonalities, but beliefs and experiences were context-specific and could be polarised. For example, willingness or readiness to receive a diagnosis varied, and there was evidence that it was often a carer rather than the person with memory problems who initiated a diagnosis. Carers were also often torn between protecting the person with dementia and promoting his or her independence. Moreover, it was clear that individuals with dementia and their family and friends were simultaneously struggling to preserve a pre-dementia self whilst at the same time accommodating the diagnosis and assimilating the disease into a new identity.
We used systematic and rigorous methods for reviewing qualitative literature. However, there are a number of methodological issues that could affect the validity of our findings. Qualitative studies are challenging to identify using standard search techniques [156],[157], and despite our efforts to identify all available studies, we cannot exclude the possibility that some were missed. Moreover, excluding studies reported in languages other than English may have introduced bias. However, we used a comprehensive search strategy, including extensive lateral searching to minimise missing studies, we included studies from 14 different countries, and we are confident that we have reached thematic saturation.
We did not exclude studies from our review on the basis of quality, but we did attempt to “weight” studies by using only those that scored high for both reliability and usefulness in a final process of verification of our themes. However, this approach may be contentious, as there is no consensus on what constitutes a “good” quality qualitative study, nor well-established methods for weighting qualitative studies [22],[158]. That said, our quality assessment procedures were thorough, and the process of reaching inter-reviewer agreement maximised robustness.
Although not all studies provided demographic information, analysis of the characteristics of participants in the studies included in the systematic review suggested that there was a skew towards more affluent, educated participants, most of whom were white. Whilst qualitative research does not generally set out to be representative, it is appropriate to consider the transferability of findings. It is, therefore, a concern that much of the research in this area has been carried out on those populations more easily accessible to researchers. Such populations may have different attitudes to information provision and be more accustomed to self-advocacy [37]. Moreover, although more than 40% of studies did not specify what type of dementia participants had, where this information was given, it was clear that the majority had Alzheimer disease. The experiences of individuals with Alzheimer disease and their carers may not be directly transferable to people with other types of dementia.
The themes in the review relating to coping strategies, the impact of dementia on quality of life and relationships, and experiences of care were similar to those from other reviews [17],[18]. It has been suggested that dementia is not necessarily a source of dreadful suffering [18],[19], and, indeed, among our sample we found evidence that many people adopted positive mindsets and appeared to successfully incorporate dementia into their lives. Nevertheless, it was clear that dementia has a significant impact on people's lives and relationships and is a major threat to identity. Moreover, the progressive nature of the disease means that the process is cyclical and requires constant adjustment. This review highlights how priorities and views change over time, and the need for services to be organised to address that process. Previous reviews [8],[19] have found that people with dementia and their carers are generally in favour of disclosure, and this is supported by this review. However, it is clear that a tension exists between the self-maintaining strategies people employ to minimise the impact of dementia on their lives and sense of self, and the acceptance of a diagnosis and all its implications [136].
Implications for Practice
Our review suggests that key needs for people with dementia and their carers include the early provision of information about financial aids and entitlements, the opportunity to talk to supportive professionals, signposting to appropriate statutory and voluntary services, and specialist support. Support needs to be ongoing, flexible, and sensitive to the needs of different groups, such as those with early onset dementia [38] or minority ethnic groups [118]; it needs to take into account the needs for continuity of care [33]; and it needs to manage care needs and safety whilst being aware of the person's sense of identity and dignity [125]. In the UK it has been suggested that specialist dementia advisors might provide such support [159]. Indeed, it is clear from the literature that the needs of people with dementia and their carers are complex and varied, and those making decisions about the timing and delivery of services need appropriate expertise and training. A further consideration relates to the availability of appropriate resources. It is possible that publicity around early diagnosis, such as the UK government campaign to raise public awareness of the early signs of dementia, may be raising expectations of services in the earlier stages of the illness [93]. This has implications for service delivery, as it may lead to the diversion of resources away from those with more advanced dementia.
Implications for Research
This review provides a comprehensive account of studies reporting the experiences of community-dwelling individuals with dementia and their carers on receiving a diagnosis and becoming a person with dementia. Indeed, there is now a substantial body of qualitative research on the transition to becoming a person with dementia. However, such research has largely been carried out in community-based populations that are easily accessible to researchers. Less is known about the oldest old, those who do not access services, or those have comorbid health conditions. Our review excluded individuals living in long-term care, and further research may be needed to explore issues around diagnosis for people living in residential homes. Although we included experiences of post-diagnosis support and treatment, the focus of our review was on the earlier stages of dementia, and we did not address issues such as behavioural problems or the transition to long-term care. Furthermore, many studies provided little or no demographic data, and it was difficult to assess the impact of factors such as type of dementia, level of education, or other socioeconomic factors on patient and carer experiences. Future qualitative studies should consider including greater detail about the characteristics of participants so that transferability can be better assessed.
Conclusions
It is often suggested that the voice of the person with dementia is not present in research. We found this not to be the case in qualitative research studies. There is now a substantial body of qualitative evidence relating to the experiences of community-dwelling individuals with cognitive impairment and their family carers, particularly in relation to the transition to becoming a person with dementia. This review provides a comprehensive account of how people accommodate and adapt to a diagnosis of dementia that could be useful to professionals working with individuals with dementia. The synthesis focuses attention on three aspects of the diagnostic transition: the challenge the diagnosis poses to identity and role, the conflicts that may need to be resolved to accommodate the diagnosis, and the practical management strategies that can assist individuals with dementia and their families. The next steps to ensure patient benefit should involve the development and evaluation of interventions, particularly those relating to post-diagnosis support.
Supporting Information
Zdroje
1. Alzheimer's Disease International (2009) World alzheimer report 2009. London: Alzheimer's Disease International. Available: http://www.alz.co.uk/research/files/WorldAlzheimerReport.pdf. Accessed 18 September 2012.
2. Alzheimer's Disease International (2010) World alzheimer report 2010: the global economic impact of dementia. London: Alzheimer's Disease International. Available: http://www.alz.co.uk/research/files/WorldAlzheimerReport2010.pdf. Accessed 18 September 2012.
3. IliffeS, BooroffA, GallivanS, GoldenbergE, MorganP, et al. (1990) Screening for cognitive impairment in the elderly using the mini-mental state examination. Br J Gen Pract 40 : 277–279.
4. BoustaniM, PetersonB, HansonL, HarrisR, LohrKN (2003) Screening for dementia in primary care: a summary of the evidence for the U.S. Preventive Services Task Force. Ann Intern Med 138 : 927–937.
5. BanerjeeS, ChanJ (2008) Organisation of old age psychiatric services. Psychiatry 7 : 49–54.
6. UK National Audit Office (2010) Improving dementia services in England—an interim report. London: UK National Audit Office.
7. RaitG, WaltersK, BottomleyC, PetersenI, IliffeS, et al. (2010) Survival of people with clinical diagnosis of dementia in primary care: cohort study. BMJ 341: c3584.
8. BamfordC, LamontS, EcclesM, RobinsonL, MayC, et al. (2004) Disclosing a diagnosis of dementia: a systematic review. Int J Geriatr Psychiatry 19 : 151–169.
9. IliffeS, ManthorpeJ, EdenA (2003) Sooner or later? Issues in the early diagnosis of dementia in general practice: a qualitative study. Fam Pract 20 : 376–381.
10. UK National Institute for Health and Clinical Excellence, Social Care Institute for Excellence (2006) Dementia: supporting people with dementia and their carers. NICE clinical guidance 42. Available: http://www.nice.org.uk/nicemedia/pdf/CG042NICEGuideline.pdf. Accessed 26 August 2012.
11. UK National Audit Office (2007) Improving services and support for people with dementia. London: UK National Audit Office.
12. UK Department of Health (2010) Quality outcomes for people with dementia: building on the work of the national dementia strategy. London: UK Department of Health.
13. BanerjeeS, WillisR, MatthewsD, ContellF, ChanJ, et al. (2007) Improving the quality of care for mild to moderate dementia: an evaluation of the Croydon Memory Service Model. Int J Geriatr Psychiatry 22 : 782–788.
14. MittelmanMS, RothDL, ClayOJ, HaleyWE (2007) Preserving health of Alzheimer caregivers: impact of a spouse caregiver intervention. Am J Geriatr Psychiatry 15 : 780–789.
15. Lingard J, Milne A (2004) First Signs—celebrating the achievements of the Dementia Advice and Support Service: a project for people in the early stages of dementia. London: Mental Health Foundation.
16. Dixon-WoodsM, FitzpatrickR (2001) Qualitative research in systematic reviews. Has established a place for itself. BMJ 323 : 765–766.
17. SteemanE, de CasterleBD, GodderisJ, GrypdonckM (2006) Living with early-stage dementia: a review of qualitative studies. J Adv Nurs 54 : 722–738.
18. De BoerME, HertoghC, DroesRM, RiphagenII, JonkerC, et al. (2007) Suffering from dementia-the patient's perspective: a review of the literature. Int Psychogeriatr 19 : 1021–1039.
19. RobinsonL, GemskiA, AbleyC, BondJ, KeadyJ, et al. (2011) The transition to dementia—individual and family experiences of receiving a diagnosis: a review. Int Psychogeriatr 23 : 1026–1043.
20. LecouturierJ, BamfordC, HughesJC, FrancisJJ, FoyR, et al. (2008) Appropriate disclosure of a diagnosis of dementia: identifying the key behaviours of ‘best practice’. BMC Health Serv Res 8 : 95.
21. GreenhalghT, PeacockR (2005) Effectiveness and efficiency of search methods in systematic reviews of complex evidence: audit of primary sources. BMJ 331 : 1064–1065.
22. Spencer L, Ritchie J, Lewis J, Dillon L (2003) Quality in qualitative evaluation: a framework for assessing research evidence. London: UK Government Chief Social Researcher's Office. Available: http://www.uea.ac.uk/edu/phdhkedu/acadpapers/qualityframework.pdf. Accessed 18 September 2012.
23. BunnF, DickinsonA, Barnett-PageE, HortonK (2008) A systematic review of older people's perceptions of facilitators and barriers to participation in falls prevention interventions. Ageing Soc 28 : 449–472.
24. PocockM, TrivediD, WillsW, BunnF, MagnussonJ (2010) Parental perceptions regarding healthy behaviours for preventing overweight and obesity in young children: a systematic review of qualitative studies. Obes Rev 11 : 338–353.
25. MarstonC, KingE (2006) Factors that shape young people's sexual behaviour: a systematic review. Lancet 368 : 1581–1586.
26. CampbellR, PoundP, PopeC, BrittenN, PillR, et al. (2003) Evaluating meta-ethnography: a synthesis of qualitative research on lay experiences of diabetes and diabetes care. Soc Sci Med 56 : 671–684.
27. BrittenN, CampbellR, PopeC, DonovanJ, MorganM, et al. (2002) Using meta ethnography to synthesise qualitative research: a worked example. J Health Serv Res Policy 7 : 209–215.
28. MarstonC (2004) Gendered communication among young people in Mexico: implications for sexual health interventions. Soc Sci Med 59 : 445–456.
29. ThomasJ, HardenA (2008) Methods for the thematic synthesis of qualitative research in systematic reviews. BMC Med Res Methodol 8 : 45.
30. AdamsKB (2006) The transition to caregiving: the experience of family members embarking on the dementia caregiving career. J Gerontol Soc Work 47 : 3–29.
31. AdamsT (1994) The emotional experience of caregivers to relatives who are chronically confused—implications for community mental health nursing. Int J Nurs Stud 31 : 545–553.
32. AdamsonJ (2001) Awareness and understanding of dementia in African/Caribbean and South Asian families. Health Soc Care Community 9 : 391–396.
33. BamfordC, BruceE (2000) Defining the outcomes of community care: the perspectives of older people with dementia and their carers. Ageing Soc 20 : 543–570.
34. BanninghLJW, Vernooij-DassenM, RikkertMO, TeunisseJP (2008) Mild cognitive impairment: coping with an uncertain label. Int J Geriatr Psychiatry 23 : 148–154.
35. BeardRL (2004) In their voices: identity preservation and experiences of Alzheimer's disease. J Aging Stud 18 : 415–428.
36. BeardRL, FettermanDJ, WuB, BryantL (2009) The two voices of Alzheimer's: attitudes toward brain health by diagnosed individuals and support persons. Gerontologist 49: S40–S49.
37. BeardRL, FoxPJ (2008) Resisting social disenfranchisement: negotiating collective identities and everyday life with memory loss. Soc Sci Med 66 : 1509–1520.
38. BeattieA, Daker-WhiteG, GilliardJ, MeansR (2004) ‘How can they tell?’ A qualitative study of the views of younger people about their dementia and dementia care services. Health Soc Care Community 12 : 359–368.
39. BenbowSM, OngYL, BlackS, GarnerJ (2009) Narratives in a users' and carers' group: meanings and impact. Int Psychogeriatr 21 : 33–39.
40. BliesznerR, RobertoKA, WilcoxKL, BarhamEJ, WinstonBL (2007) Dimensions of ambiguous loss in couples coping with mild cognitive impairment. Fam Relat 56 : 196–209.
41. BoiseL, MorganDL, KayeJ, CamicioliR (1999) Delays in the diagnosis of dementia: perspectives of family caregivers. Am J Alzheimers Dis Other Demen 14 : 20.
42. BowesA, WilkinsonH (2003) ‘We didn't know it would get that bad’: South Asian experiences of dementia and the service response. Health Soc Care Community 11 : 387–396.
43. BruceDG, PatersonA (2000) Barriers to community support for the dementia carer: a qualitative study. Int J Geriatr Psychiatry 15 : 451–457.
44. ButcherHK, HolkupPA, BuckwalterKC (2001) The experience of caring for a family member with Alzheimer's disease. West J Nurs Res 23 : 33–55.
45. ByszewskiAM, MolnarFJ, AminzadehF, EisnerM, GardeziF, et al. (2007) Dementia diagnosis disclosure: a study of patient and caregiver perspectives. Alzheimer Dis Assoc Disord 21 : 107–114.
46. CahillS, BegleyE, TopoP, SaarikalleK, MacijauskieneJ, et al. (2004) ‘I know where this is going and I know it won't go back’: hearing the individual's voice in dementia quality of life assessments. Dementia 3 : 313–330.
47. CahillSM, GibbM, BruceI, HeadonM, DruryM (2008) ‘I was worried coming in because I don't really know why it was arranged’: the subjective experience of new patients and their primary caregivers attending a memory clinic. Dementia 7 : 175–189.
48. ClareL (2002) Developing awareness about awareness in early-stage dementia: the role of psychosocial factors. Dementia 1 : 295–312.
49. ClareL, RothI, PrattR (2005) Perceptions of change over time in early-stage Alzheimer's disease: implications for understanding awareness and coping style. Dementia 4 : 487–520.
50. ClareL, ShakespeareP (2004) Negotiating the impact of forgetting: dimensions of resistance in task-oriented conversations between people with early-stage dementia and their partners. Dementia 3 : 211–232.
51. CornerL, BondJ (2006) The impact of the label of mild cognitive impairment on the individual's sense of self. Philos Psychiatr Psychol 13 : 3–12.
52. CotrellV, LeinL (1992) Awareness and denial in the Alzheimer's disease victim. J Gerontol Soc Work 19 : 115–132.
53. DebS, HareM, PriorL (2007) Symptoms of dementia among adults with Down's syndrome: a qualitative study. J Intellect Disabil Res 51 : 726–739.
54. DerksenE, Vernooij-DassenM, GillissenF, Olde RikkertM, ScheltensP (2006) Impact of diagnostic disclosure in dementia on patients and carers: qualitative case series analysis. Aging Ment Health 10 : 525–531.
55. DugganS, BlackmanT, MartyrA, Van SchaikP (2008) The impact of early dementia on outdoor life: a ‘shrinking world’? Dementia 7 : 191–205.
56. DugglebyW, WilliamsA, WrightK, BollingerS (2009) Renewing everyday hope: the hope experience of family caregivers of persons with dementia. Issues Ment Health Nurs 30 : 514–521.
57. FrankL, LloydA, FlynnJA, KleinmanL, MatzaLS, et al. (2006) Impact of cognitive impairment on mild dementia patients and mild cognitive impairment patients and their informants. Int Psychogeriatr 18 : 151–162.
58. GilliesBA (2000) A memory like clockwork: accounts of living through dementia. Aging Ment Health 4 : 366–374.
59. GilmourH, GibsonF, CampbellJ (2003) Living alone with dementia: a case study approach to understanding risk. Dementia 2 : 403–420.
60. GilmourJA, HuntingtonAD (2005) Finding the balance: living with memory loss. Int J Nurs Pract 11 : 118–124.
61. HainD, TouhyTA, EngströmG (2010) What matters most to carers of people with mild to moderate dementia as evidence for transforming care. Alzheimers Care Today 11 : 162.
62. HarmanG, ClareL (2006) Illness representations and lived experience in early-stage dementia. Qual Health Res 16 : 484–502.
63. HarrisPB, KeadyJ (2004) Living with early onset dementia: exploring the experience and developing evidence-based guidelines for practice. Alzheimers Care Today 5 : 111–122.
64. HarrisPB, SterinGJ (1999) Insider's perspective: defining and preserving the self of dementia. J Ment Health Aging 5 : 241–256.
65. HellströmI, NolanM, LundhU (2005) Awareness context theory and the dynamics of dementia. Dementia 4 : 269.
66. HintonL, FranzC, FriendJ (2004) Pathways to dementia diagnosis: evidence for cross-ethnic differences. Alzheimer Dis Assoc Disord 18 : 134–144.
67. HintonWL, LevkoffS (1999) Constructing Alzheimer's: narratives of lost identities, confusion and loneliness in old age. Cult Med Psychiatry 23 : 453–475.
68. HolstG, HallbergIR (2003) Exploring the meaning of everyday life, for those suffering from dementia. Am J Alzheimers Dis Other Demen 18 : 359–365.
69. HoworthP, SaperJ (2003) The dimensions of insight in people with dementia. Aging Ment Health 7 : 113–123.
70. HulkoW (2009) From ‘not a big deal’ to ‘hellish’: experiences of older people with dementia. J Aging Stud 23 : 131–144.
71. HutchingsD, VanoliA, McKeithI, BrothertonS, McNameeP, et al. (2010) Good days and bad days: the lived experience and perceived impact of treatment with cholinesterase inhibitors for Alzheimer's disease in the United Kingdom. Dementia 9 : 409–425.
72. HutchinsonSA, Leger-KrallS, WilsonHS (1997) Early probable Alzheimer's disease and awareness context theory. Soc Sci Med 45 : 1399–1409.
73. JanssonW, NordbergG, GrafströmM (2001) Patterns of elderly spousal caregiving in dementia care: an observational study. J Adv Nurs 34 : 804–812.
74. Jutlla K, Moreland N (2007 March) Twice a child III: the experience of Asian carers of older people with dementia in Wolverhampton. London: Dementia UK.
75. KatsunoT (2005) Dementia from the inside: how people with early-stage dementia evaluate their quality of life. Ageing Soc 25 : 197–214.
76. Keady J, Gilliard J (1999) The early experience of Alzheimer's disease: implications for partnership and practice. In: Adams T, Clarke CL, editors. Dementia care: developing partnerships in practice. London: Bailliere Tindall. pp. 227–256.
77. KoppelOSB, DallosR (2007) The development of memory difficulties: a journey into the unknown. Dementia 6 : 193–213.
78. LaakkonenML, RaivioMM, Eloniemi-SulkavaU, SaarenheimoM, PietiläM, et al. (2008) How do elderly spouse care givers of people with Alzheimer disease experience the disclosure of dementia diagnosis and subsequent care? J Med Ethics 34 : 427–430.
79. LangdonSA, EagleA, WarnerJ (2007) Making sense of dementia in the social world: a qualitative study. Soc Sci Med 64 : 989–1000.
80. DavisLL, GillissCL, Deshefy-LonghiT, ChestnuttDH, MolloyM (2011) The nature and scope of stressful spousal caregiving relationships. J Fam Nurs 17 : 224–240.
81. de WittL, PloegJ, BlackM (2010) Living alone with dementia: an interpretive phenomenological study with older women. J Adv Nurs 66 : 1698–1707.
82. LeungKK, FinlayJ, SilviusJL, KoehnS, McClearyL, et al. (2011) Pathways to diagnosis: exploring the experiences of problem recognition and obtaining a dementia diagnosis among Anglo-Canadians. Health Soc Care Community 19 : 372–381.
83. KuoLM, ShyuYI (2010) Process of ambivalent normalisation: experience of family caregivers of elders with mild cognitive impairment in Taiwan. J Clin Nurs 19 : 3477–3484.
84. RobertoKA, BliesznerR, McCannBR, McPhersonMC (2011) Family triad perceptions of mild cognitive impairment. J Gerontol B Psychol Sci Soc Sci 66 : 756–768.
85. LawrenceV, MurrayJ, SamsiK, BanerjeeS (2008) Attitudes and support needs of Black Caribbean, south Asian and White British carers of people with dementia in the UK. Br J Psychiatry 193 : 240–246.
86. LawrenceV, SamsiK, BanerjeeS, MorganC, MurrayJ (2010) Threat to valued elements of life: the experience of dementia across three ethnic groups. Gerontologist 51 : 39–50.
87. LinglerJH, NightingaleMC, ErlenJA, KaneAL, ReynoldsCF3rd, et al. (2006) Making sense of mild cognitive impairment: a qualitative exploration of the patient's experience. Gerontologist 46 : 791–800.
88. LivingstonG, LeaveyG, ManelaM, LivingstonD, RaitG, et al. (2010) Making decisions for people with dementia who lack capacity: qualitative study of family carers in UK. BMJ 341: c4184.
89. LuYF, HaaseJE (2009) Experience and perspectives of caregivers of spouse with mild cognitive impairment. Curr Alzheimer Res 6 : 384–391.
90. MacQuarrieCR (2005) Experiences in early stage Alzheimer's disease: understanding the paradox of acceptance and denial. Aging Ment Health 9 : 430–441.
91. MacRaeH (2010) Managing identity while living with Alzheimer's disease. Qual Health Res 20 : 293–305.
92. MahoneyDF, CloutterbuckJ, NearyS, ZhanL (2005) African American, Chinese, and Latino family caregivers' impressions of the onset and diagnosis of dementia: cross-cultural similarities and differences. Gerontologist 45 : 783–792.
93. Manthorpe J, Samsi K, Campbell S, Abley C, Keady J, et al.. (2011) The transition from cognitive impairment to dementia: older people's experiences. Southampton: NIHR Service Delivery and Organisation Programme.
94. MasonE, ClareL, PistrangN (2005) Processes and experiences of mutual support in professionally-led support groups for people with early-stage dementia. Dementia 4 : 79–112.
95. MenneHL, KinneyJM, MorhardtDJ (2002) ‘Trying to continue to do as much as they can do’: theoretical insights regarding continuity and meaning making in the face of dementia. Dementia 1 : 367–382.
96. MokE, LaiCK, WongFL, WanP (2007) Living with early-stage dementia: the perspective of older Chinese people. J Adv Nurs 59 : 591–600.
97. Moniz-CookE, ManthorpeJ, CarrI, GibsonG, Vernooij-DassenM (2006) Facing the future: a qualitative study of older people referred to a memory clinic prior to assessment and diagnosis. Dementia 5 : 375.
98. Moreland N (2001) Twice a child: dementia care for African-Caribbean and Asian older people in Wolverhampton. London: Dementia UK.
99. Moreland N (2003) Twice a child II: service development for dementia care for African-Caribbean and Asian older people in Wolverhampton. London: Dementia UK.
100. MukadamN, CooperC, BasitB, LivingstonG (2011) Why do ethnic elders present later to UK dementia services? A qualitative study. Int Psychogeriatr 23 : 1070–1077.
101. MurrayJ, SchneiderJ, BanerjeeS, MannA (1999) EUROCARE: a cross-national study of co-resident spouse carers for people with Alzheimer's disease: II—a qualitative analysis of the experience of caregiving. Int J Geriatr Psychiatry 14 : 662–667.
102. NeufeldA, HarrisonMJ (2003) Unfulfilled expectations and negative interactions: nonsupport in the relationships of women caregivers. J Adv Nurs 41 : 323–331.
103. NygardL, BorellL (1998) A life-world of altering meaning: expressions of the illness experience of dementia in everyday life over 3 years. Occup Ther J Res 18 : 109–136.
104. O'ConnorDL (1999) Living with a memory-impaired spouse: (re)cognizing the experience. Can J Aging 18 : 211–235.
105. OstwaldSK, DugglebyW, HepburnKW (2002) The stress of dementia: view from the inside. Am J Alzheimers Dis Other Demen 17 : 303–312.
106. PearceA, ClareL, PistrangN (2002) Managing sense of self: coping in the early stages of Alzheimer's disease. Dementia 1 : 173.
107. PerryJ, O'ConnorD (2002) Preserving personhood: (re)membering the spouse with dementia. Fam Relat 51 : 55–62.
108. PhinneyA (1998) Living with dementia: from the patient's perspective. J Gerontol Nurs 24 : 8–16.
109. PhinneyA (2006) Family strategies for supporting involvement in meaningful activity by persons with dementia. J Fam Nurs 12 : 80–101.
110. PollittPA, O'ConnorDW, AndersonI (1989) Mild dementia: perceptions and problems. Ageing Soc 9 : 261–275.
111. PostSG, StuckeyJC, WhitehousePJ, OllertonS, DurkinC, et al. (2001) A focus group on cognition-enhancing medications in Alzheimer disease: disparities between professionals and consumers. Alzheimer Dis Assoc Disord 15 : 80.
112. PrattR, WilkinsonH (2003) A psychosocial model of understanding the experience of receiving a diagnosis of dementia. Dementia 2 : 181.
113. PrestonL, MarshallA, BucksRS (2007) Investigating the ways that older people cope with dementia: a qualitative study. Aging Ment Health 11 : 131–143.
114. QuinnC, ClareL, PearceA, van DijkhuizenM (2008) The experience of providing care in the early stages of dementia: an interpretative phenomenological analysis. Aging Ment Health 12 : 769–778.
115. RobinsonL, ClareL, EvansK (2005) Making sense of dementia and adjusting to loss: psychological reactions to a diagnosis of dementia in couples. Aging Ment Health 9 : 337–347.
116. RobinsonP, EkmanSL, MeleisAI, WinbladB, WahlundLO (1997) Suffering in silence: the experience of early memory loss. Health Care Later Life 2 : 107–120.
117. SamuelssonAM, AnnerstedtL, ElmståhlS, SamuelssonSM, GrafströmM (2001) Burden of responsibility experienced by family caregivers of elderly dementia sufferers. Scand J Caring Sci 15 : 25–33.
118. Seabrooke V, Milne A (2004) Culture and care in dementia: a study of the Asian community in north west Kent. London: The Mental Health Foundation.
119. ShajiKS, SmithaK, LalKP, PrinceMJ (2003) Caregivers of people with Alzheimer's disease: a qualitative study from the Indian 10/66 Dementia Research Network. Int J Geriatr Psychiatry 18 : 1–6.
120. SmithAP, BeattieBL (2001) Disclosing a diagnosis of Alzheimer's disease: patient and family experiences. Can J Neurol Sci 28(Suppl 1): S67–S71.
121. SteemanE, GodderisJ, GrypdonckM, De BalN, Dierckx de CasterleB (2007) Living with dementia from the perspective of older people: is it a positive story? Aging Ment Health 11 : 119–130.
122. SterrittPF, PokornyME (1998) African-American caregiving for a relative with Alzheimer's disease. Geriatr Nurs 19 : 127–124, 127-128, 133-124.
123. SvanstromR, DahlbergK (2004) Living with dementia yields a heteronomous and lost existence. West J Nurs Res 26 : 671–687.
124. TeelCS, CarsonP (2003) Family experiences in the journey through dementia diagnosis and care. J Fam Nurs 9 : 38.
125. TodresL, GalvinK (2006) Caring for a partner with Alzheimer's disease: intimacy, loss and the life that is possible. Int J Qual Stud Health Well-being 1 : 50–61.
126. Van DijkhuizenM, ClareL, PearceA (2006) Striving for connection: appraisal and coping among women with early-stage Alzheimer's disease. Dementia 5 : 73.
127. VelloneE, SansoniJ, CohenMZ (2002) The experience of Italians caring for family members with Alzheimer's disease. J Nurs Scholarsh 34 : 323–329.
128. WatkinsR, ChestonR, JonesK, GilliardJ (2006) ‘Coming out’ with Alzheimer's disease: changes in awareness during a psychotherapy group for people with dementia. Aging Ment Health 10 : 166–176.
129. WerezakL, StewartN (2002) Learning to live with early dementia. Can J Nurs Res 34 : 67–85.
130. WestiusA, AnderssonL, KallenbergK (2009) View of life in persons with dementia. Dementia 8 : 481–500.
131. WolversonEL, ClarkeC, Moniz-CookE (2010) Remaining hopeful in early-stage dementia: a qualitative study. Aging Ment Health 14 : 450–460.
132. AminzadehF, ByszewskiA, MolnarFJ, EisnerM (2007) Emotional impact of dementia diagnosis: exploring persons with dementia and caregivers' perspectives. Aging Ment Health 11 : 281–290.
133. BliesznerR, RobertoKA (2010) Care partner responses to the onset of mild cognitive impairment. Gerontologist 50 : 11–22.
134. ClareL (2002) We'll fight it as long as we can: coping with the onset of Alzheimer s disease. Aging Ment Health 6 : 139–148.
135. ClareL (2003) ‘I'm still me’: living with the onset of dementia. J Dement Care 11 : 32–35.
136. ClareL (2003) Managing threats to self: awareness in early stage Alzheimer's disease. Soc Sci Med 57 : 1017–1029.
137. CloutterbuckJ, MahoneyDF (2003) African American dementia caregivers: the duality of respect. Dementia 2 : 221.
138. ConnellCM, BoiseL, StuckeyJC, HolmesSB, HudsonML (2004) Attitudes toward the diagnosis and disclosure of dementia among family caregivers and primary care physicians. Gerontologist 44 : 500–507.
139. DerksenE, Vernooij-DassenM, GillissenF, Olde-RikkertM, ScheltensP (2005) The impact of diagnostic disclosure in dementia: a qualitative case analysis. Int Psychogeriatr 17 : 319–326.
140. FoxK, HintonWL, LevkoffS (1999) Take up the caregiver's burden: stories of care for urban African American elders with dementia. Cult Med Psychiatry 23 : 501–529.
141. GalvinK, TodresL, RichardsonM (2005) The intimate mediator: a carer's experience of Alzheimer's. Scand J Caring Sci 19 : 2–11.
142. HarrisPB, KeadyJ (2009) Selfhood in younger onset dementia: transitions and testimonies. Aging Ment Health 13 : 437–444.
143. HellstromI, NolanM, LundhU (2005) ‘We do things together’: a case study of ‘couplehood’ in dementia. Dementia 4 : 7.
144. HellströmI, NolanM, LundhU (2007) Sustaining ‘couplehood’. Dementia 6 : 383.
145. HicksMH, LamMS (1999) Decision-making within the social course of dementia: accounts by Chinese-American caregivers. Cult Med Psychiatry 23 : 415–452.
146. JolleyD, MorelandN, ReadK, KaurH, JutllaK, et al. (2009) The ‘Twice a Child’ projects: learning about dementia and related disorders within the black and minority ethnic population of an English city and improving relevant services. Ethn Inequal Health Soc Care 2 : 4–9.
147. NearySR, MahoneyDF (2005) Dementia caregiving: the experiences of Hispanic/Latino caregivers. J Transcult Nurs 16 : 163–170.
148. OrtizA, SimmonsJ, HintonWL (1999) Locations of remorse and homelands of resilience: notes on grief and sense of loss of place of Latino and Irish-American caregivers of demented elders. Cult Med Psychiatry 23 : 477–500.
149. PhinneyA (2002) Fluctuating awareness and the breakdown of the illness narrative in dementia. Dementia 1 : 329–344.
150. PhinneyA, ChaudhuryH, O'ConnorDL (2007) Doing as much as I can do: the meaning of activity for people with dementia. Aging Ment Health 11 : 384–393.
151. PhinneyA, CheslaCA (2003) The lived body in dementia. J Aging Stud 17 : 283–299.
152. Pratt R, Wilkinson H (2001) ‘Tell me the truth’: the effect of being told the diagnosis of dementia from the perspective of the person with dementia. London: The Mental Health Foundation.
153. RobinsonP, EkmanSL, WahlundLO (1998) Unsettled, uncertain and striving to understand: toward an understanding of the situation of persons with suspected dementia. Int J Aging Hum Dev 47 : 143–161.
154. Vernooij-DassenM, DerksenE, ScheltensP, Moniz-CookE (2006) Receiving a diagnosis of dementia: the experience over time. Dementia 5 : 397.
155. De WittL, PloegJ, BlackM (2009) Living on the threshold: the spatial experience of living alone with dementia. Dementia 8 : 263–291.
156. BarrosoJ, GollopCJ, SandelowskiM, MeynellJ, PearcePF, et al. (2003) The challenges of searching for and retrieving qualitative studies. West J Nurs Res 25 : 153–178.
157. WongSS, WilczynskiNL, HaynesRB (2004) Developing optimal search strategies for detecting clinically relevant qualitative studies in MEDLINE. Stud Health Technol Inform 107 : 311–316.
158. Dixon-WoodsM, ShawRL, AgarwalS, SmithJA (2004) The problem of appraising qualitative research. Qual Saf Health Care 13 : 223–225.
159. UK Department of Health (2009) Living well with dementia—the National Dementia Strategy Joint commissioning framework for dementia. London: UK Department of Health.
Štítky
Interní lékařství
Článek vyšel v časopisePLOS Medicine
Nejčtenější tento týden
2012 Číslo 10- Berberin: přírodní hypolipidemikum se slibnými výsledky
- Příznivý vliv Armolipidu Plus na hladinu cholesterolu a zánětlivé parametry u pacientů s chronickým subklinickým zánětem
- Léčba bolesti u seniorů
- Jak postupovat při výběru betablokátoru − doporučení z kardiologické praxe
- Červená fermentovaná rýže účinně snižuje hladinu LDL cholesterolu jako vhodná alternativa ke statinové terapii
-
Všechny články tohoto čísla
- The Double Burden of Obesity and Malnutrition in a Protracted Emergency Setting: A Cross-Sectional Study of Western Sahara Refugees
- PRISMA-Equity 2012 Extension: Reporting Guidelines for Systematic Reviews with a Focus on Health Equity
- Human Rights Research and Ethics Review: Protecting Individuals or Protecting the State?
- Serious and Life-Threatening Pregnancy-Related Infections: Opportunities to Reduce the Global Burden
- Donor Funding for Newborn Survival: An Analysis of Donor-Reported Data, 2002–2010
- The Potential Impact of Pre-Exposure Prophylaxis for HIV Prevention among Men Who Have Sex with Men and Transwomen in Lima, Peru: A Mathematical Modelling Study
- Removing the Age Restrictions for Rotavirus Vaccination: A Benefit-Risk Modeling Analysis
- Where There Is No Paramedic: The Sachigo Lake Wilderness Emergency Response Education Initiative
- Associations between Mode of HIV Testing and Consent, Confidentiality, and Referral: A Comparative Analysis in Four African Countries
- Strengthening Medical Product Regulation in Low- and Middle-Income Countries
- Bringing Clarity to the Reporting of Health Equity
- Developing a National Mental Health Policy: A Case Study from Uganda
- Psychosocial Factors That Shape Patient and Carer Experiences of Dementia Diagnosis and Treatment: A Systematic Review of Qualitative Studies
- Research Conducted Using Data Obtained through Online Communities: Ethical Implications of Methodological Limitations
- Genetic Predictors of Response to Serotonergic and Noradrenergic Antidepressants in Major Depressive Disorder: A Genome-Wide Analysis of Individual-Level Data and a Meta-Analysis
- Risk of Cardiovascular Disease and Total Mortality in Adults with Type 1 Diabetes: Scottish Registry Linkage Study
- PLOS Medicine
- Archiv čísel
- Aktuální číslo
- Informace o časopisu
Nejčtenější v tomto čísle- Human Rights Research and Ethics Review: Protecting Individuals or Protecting the State?
- The Potential Impact of Pre-Exposure Prophylaxis for HIV Prevention among Men Who Have Sex with Men and Transwomen in Lima, Peru: A Mathematical Modelling Study
- Psychosocial Factors That Shape Patient and Carer Experiences of Dementia Diagnosis and Treatment: A Systematic Review of Qualitative Studies
- Genetic Predictors of Response to Serotonergic and Noradrenergic Antidepressants in Major Depressive Disorder: A Genome-Wide Analysis of Individual-Level Data and a Meta-Analysis
Kurzy
Zvyšte si kvalifikaci online z pohodlí domova
Současné možnosti léčby obezity
nový kurzAutoři: MUDr. Martin Hrubý
Všechny kurzyPřihlášení#ADS_BOTTOM_SCRIPTS#Zapomenuté hesloZadejte e-mailovou adresu, se kterou jste vytvářel(a) účet, budou Vám na ni zaslány informace k nastavení nového hesla.
- Vzdělávání



