-
Články
Top novinky
Reklama- Vzdělávání
- Časopisy
Top články
Nové číslo
- Témata
Top novinky
Reklama- Videa
- Podcasty
Nové podcasty
Reklama- Kariéra
Doporučené pozice
Reklama- Praxe
Top novinky
ReklamaCardiac Complications in Patients with Community-Acquired Pneumonia: A Systematic Review and Meta-Analysis of Observational Studies
Background:
Community-acquired pneumonia (CAP) is a leading cause of morbidity and mortality. CAP can trigger acute cardiac events. We sought to determine the incidence of major cardiac complications in CAP patients to characterize the magnitude of this problem.Methods and Findings:
Two investigators searched MEDLINE, Scopus, and EMBASE for observational studies of immunocompetent adults with clinical and radiological evidence of CAP that reported any of the following: overall cardiac complications, incident heart failure, acute coronary syndromes (ACS), or incident cardiac arrhythmias occurring within 30 days of CAP diagnosis. At a minimum, studies had to establish enrolment procedures and inclusion and exclusion criteria, enrol their patients sequentially, and report the incidence of cardiac complications as a function of their entire cohorts. Studies with focus on nosocomial or health care–associated pneumonia were not included. Review of 2,176 citations yielded 25 articles that met eligibility and minimum quality criteria. Seventeen articles (68%) reported cohorts of CAP inpatients. In this group, the pooled incidence rates for overall cardiac complications (six cohorts, 2,119 patients), incident heart failure (eights cohorts, 4,215 patients), acute coronary syndromes (six cohorts, 2,657 patients), and incident cardiac arrhythmias (six cohorts, 2,596 patients), were 17.7% (confidence interval [CI] 13.9–22.2), 14.1% (9.3–20.6), 5.3% (3.2–8.6), and 4.7% (2.4–8.9), respectively. One article reported cardiac complications in CAP outpatients, four in low-risk (not severely ill) inpatients, and three in high-risk inpatients. The incidences for all outcomes except overall cardiac complications were lower in the two former groups and higher in the latter. One additional study reported on CAP outpatients and low-risk inpatients without discriminating between these groups. Twelve studies (48%) asserted the evaluation of cardiac complications in their methods but only six (24%) provided a definition for them. Only three studies, all examining ACS, carried out risk factor analysis for these events. No study analyzed the association between cardiac complications and other medical complications or their impact on other CAP outcomes.Conclusions:
Major cardiac complications occur in a substantial proportion of patients with CAP. Physicians and patients need to appreciate the significance of this association for timely recognition and management of these events. Strategies aimed at preventing pneumonia (i.e., influenza and pneumococcal vaccination) in high-risk populations need to be optimized. Further research is needed to understand the mechanisms underlying this association, measure the impact of cardiac complications on other CAP outcomes, identify those patients with CAP at high risk of developing cardiac complications, and design strategies to prevent their occurrence in this population.
: Please see later in the article for the Editors' Summary
Published in the journal: . PLoS Med 8(6): e32767. doi:10.1371/journal.pmed.1001048
Category: Research Article
doi: https://doi.org/10.1371/journal.pmed.1001048Summary
Background:
Community-acquired pneumonia (CAP) is a leading cause of morbidity and mortality. CAP can trigger acute cardiac events. We sought to determine the incidence of major cardiac complications in CAP patients to characterize the magnitude of this problem.Methods and Findings:
Two investigators searched MEDLINE, Scopus, and EMBASE for observational studies of immunocompetent adults with clinical and radiological evidence of CAP that reported any of the following: overall cardiac complications, incident heart failure, acute coronary syndromes (ACS), or incident cardiac arrhythmias occurring within 30 days of CAP diagnosis. At a minimum, studies had to establish enrolment procedures and inclusion and exclusion criteria, enrol their patients sequentially, and report the incidence of cardiac complications as a function of their entire cohorts. Studies with focus on nosocomial or health care–associated pneumonia were not included. Review of 2,176 citations yielded 25 articles that met eligibility and minimum quality criteria. Seventeen articles (68%) reported cohorts of CAP inpatients. In this group, the pooled incidence rates for overall cardiac complications (six cohorts, 2,119 patients), incident heart failure (eights cohorts, 4,215 patients), acute coronary syndromes (six cohorts, 2,657 patients), and incident cardiac arrhythmias (six cohorts, 2,596 patients), were 17.7% (confidence interval [CI] 13.9–22.2), 14.1% (9.3–20.6), 5.3% (3.2–8.6), and 4.7% (2.4–8.9), respectively. One article reported cardiac complications in CAP outpatients, four in low-risk (not severely ill) inpatients, and three in high-risk inpatients. The incidences for all outcomes except overall cardiac complications were lower in the two former groups and higher in the latter. One additional study reported on CAP outpatients and low-risk inpatients without discriminating between these groups. Twelve studies (48%) asserted the evaluation of cardiac complications in their methods but only six (24%) provided a definition for them. Only three studies, all examining ACS, carried out risk factor analysis for these events. No study analyzed the association between cardiac complications and other medical complications or their impact on other CAP outcomes.Conclusions:
Major cardiac complications occur in a substantial proportion of patients with CAP. Physicians and patients need to appreciate the significance of this association for timely recognition and management of these events. Strategies aimed at preventing pneumonia (i.e., influenza and pneumococcal vaccination) in high-risk populations need to be optimized. Further research is needed to understand the mechanisms underlying this association, measure the impact of cardiac complications on other CAP outcomes, identify those patients with CAP at high risk of developing cardiac complications, and design strategies to prevent their occurrence in this population.
: Please see later in the article for the Editors' SummaryIntroduction
Community-acquired pneumonia (CAP) is a common and deadly condition. In the United States alone, it is estimated that each year CAP affects 5–6 million people, results in about 1.1 million hospital admissions, and causes the death of over 60,000 Americans, representing the most frequent cause of infectious disease–related mortality and, along with influenza, the overall eighth leading cause of death in this country [1],[2].
CAP occurs more frequently in the middle aged and the elderly, a population that is also at the highest risk for cardiac diseases [3],[4]. Not surprisingly, more than half of elderly patients who present to the hospital with CAP in the United States have preexisting chronic cardiac conditions, and as the population continues to age, this association will become more important [3],[5].
Acute infections, including CAP, can affect the cardiovascular system in various ways and have been recognized as precipitants of acute cardiac events [6]–[8]. Although the possibility of major cardiac complications occurring in a considerable proportion of CAP patients is very plausible, systematic data on the magnitude of this problem are remarkably scant [9]. Given the burden of CAP in North America and other western societies [1],[2], a careful characterization of the risk of cardiac complications in patients with this infection can have important implications for health policy-making and direct patient care. This systematic review examines the literature published on cardiac complications in patients with CAP in an attempt to characterize the nature and significance of this association, and to identify areas in this field that require further investigation.
Methods
The PRISMA checklist is provided in Text S1.
Search Strategy
Our systematic search strategy was developed to capture all articles of prognosis of CAP in which cardiac complications had been reported and is presented in Text S2. We included articles reporting in English, French, or Spanish languages. We searched the following databases: MEDLINE (from 1950 to June 13, 2010), Scopus (from 1960 to June 13, 2010), and EMBASE (from 1980 to June 13, 2010). Reference lists of selected papers were also screened for additional articles of interest.
Outcomes
Our outcomes consisted of the incidence of cardiac complications as a combined endpoint, incident (new or worsening) heart failure, acute coronary syndromes (ACS; acute myocardial infarction or unstable angina), and incident cardiac arrhythmias within 30 d of CAP diagnosis.
Eligibility Criteria
To ensure that the literature reviewed dealt with CAP rather than other conditions, we included only studies in which the definition of CAP was supported by radiographic evidence of acute airspace disease (new or progressing infiltrate within 48 h of presentation), and clinical signs or symptoms of pulmonary infection. Only observational studies reporting the occurrence of any of the cardiac complications of interest in their results or stating the evaluation of these outcomes in their methods were considered. At a minimum, studies had to establish enrolment procedures and inclusion and exclusion criteria in their methodological section, enrol their patients sequentially, and report the incidence of cardiac complications as a function of their entire cohorts.
We excluded studies with focus on nosocomial or health care–associated pneumonia, case series (defined as studies with ≤25 participants), articles without original data, antibiotic efficacy trials (because they are usually restricted to highly selected patients), and articles dealing primarily with pediatric patients or patients infected with the human immunodeficiency virus. We also excluded studies in which the inception time of their cohorts was beyond 48 h from the diagnosis of pneumonia.
Selection of Studies
All titles and abstracts of the citations identified by our literature search were independently screened by two investigators (VFC-M and KNS). Relevant articles were reviewed in their entirety. Each investigator made a recommendation for inclusion or exclusion of single articles and if discordant, a third investigator solved the discrepancy (GR). When two or more articles had overlap of their populations and reported on the same cardiac outcomes, only the most inclusive article was considered.
Data Extraction, Synthesis, and Analyses
We systematically collected data on the incidence of the cardiac complications of interest, the characteristics of the populations studied, and several aspects of the study setting and methodological design (Table S1). We contacted (by e-mail) the corresponding authors of those papers that offered no details of the methodology followed for the ascertainment of the cardiac complications of interest, and asked them to provide us with copies of the study protocols (or similar) in which this information would be available. Given the aim of our analyses, we focused on how rigorously the evaluation of medical and/or cardiac complications was established in the methodological considerations of these studies as an indicator of their risk of bias in the ascertainment and reporting of these outcomes and their quality relevant to our work. Publication bias was assessed by preparing a funnel plot for the outcome of overall cardiac complications.
Pooled incidence rates of cardiac complications were calculated separately for studies dealing with outpatients, inpatients as a whole, low-risk inpatients (e.g., inpatients with no indication for hospital admission, low-risk pneumonia severity index categories, not requiring admission to intensive care units, etc.), and high-risk inpatients (i.e., patients admitted to intensive care units). We took this approach to prevent heterogeneity in our estimates since these categories represent distinct populations of CAP patients. We performed prespecified subgroup analyses for studies of CAP inpatients by characteristics of their study setting and design, quality indicators of potential bias (see above), and attributes of their populations. Because of the limited number of studies available, these analyses are presented in a descriptive format only. Pooled event rates and their confidence intervals (CIs) were estimated using a random effects model weighted by the inverse variance. When only one study was available, the Agresti-Coull method was used. All analyses were conducted in comprehensive meta-analysis version 2.2.
Results
Our search strategy yielded 2,176 articles for review. A flow summary of the selection process is provided in Figure 1. Table 1 presents a summarized description of the 25 ultimately selected articles [10]–[34]. Two studies had overlapping study populations [30],[34], but since the smaller study reported on each of the four cardiac complications of interest [30], while the larger one reported only data on ACS [34], we kept both but considered only the latter for analyses related to ACS. One article reported on outpatients and inpatients as separate groups [19], and for purposes of comparative and pooled analyses, each group was treated as a distinct study. Table S1 provides the most detailed information on the setting, methodology, population, and findings of the included studies.
Fig. 1. PRISMA flow diagram: selection process. 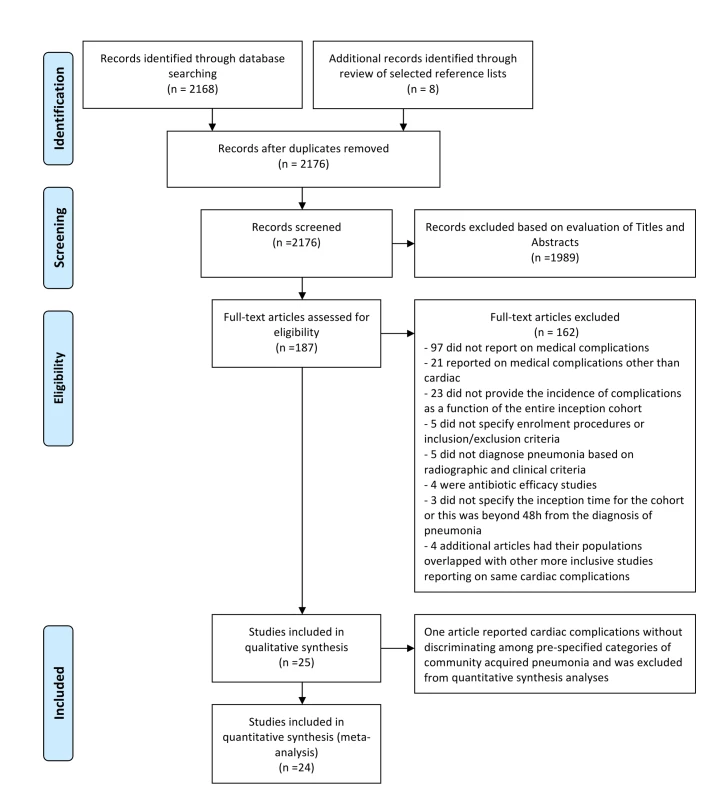
Tab. 1. Studies of cardiac complications in patients with CAP. 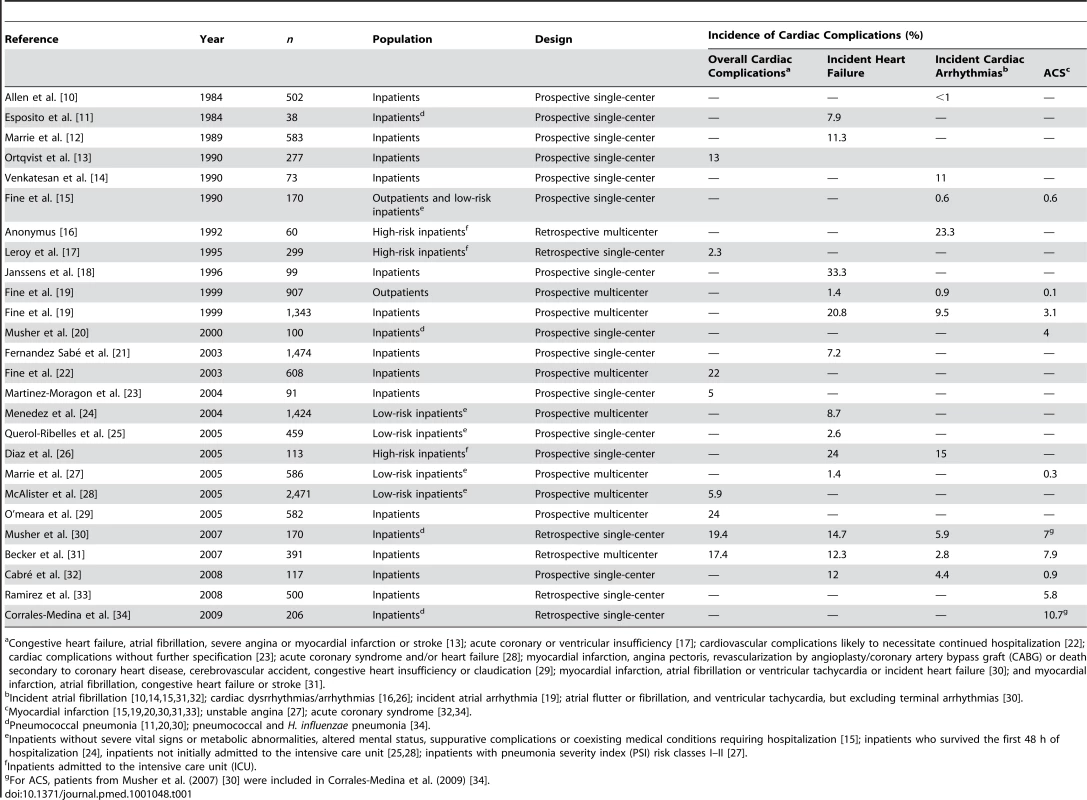
Congestive heart failure, atrial fibrillation, severe angina or myocardial infarction or stroke [13]; acute coronary or ventricular insufficiency [17]; cardiovascular complications likely to necessitate continued hospitalization [22]; cardiac complications without further specification [23]; acute coronary syndrome and/or heart failure [28]; myocardial infarction, angina pectoris, revascularization by angioplasty/coronary artery bypass graft (CABG) or death secondary to coronary heart disease, cerebrovascular accident, congestive heart insufficiency or claudication [29]; myocardial infarction, atrial fibrillation or ventricular tachycardia or incident heart failure [30]; and myocardial infarction, atrial fibrillation, congestive heart failure or stroke [31]. Assessment of Quality and Risk of Bias
The evaluation of medical and cardiac complications was documented in the methodological considerations of 68% (17 cohorts, n = 12,068) and 48% (12 cohorts, n = 9,344) of the 25 studies, respectively; whereas definitions of the cardiac complications of interest were available for 24% (six cohorts, n = 4,125) of them (Table S1). Table 2 provides the stratification of the articles by these quality elements for each of the cardiac complications of interest. The definitions used for the ascertainment of cardiac complications in the studies for which this information was available is provided in Table S2. Due to the low number of studies, a visual inspection of our funnel plot for overall cardiac complications did not allow for a meaningful assessment of publication bias (Figure S1).
Tab. 2. Studies of cardiac complications in patients with CAP: Methodological considerations for the ascertainment of medical and cardiac complications. 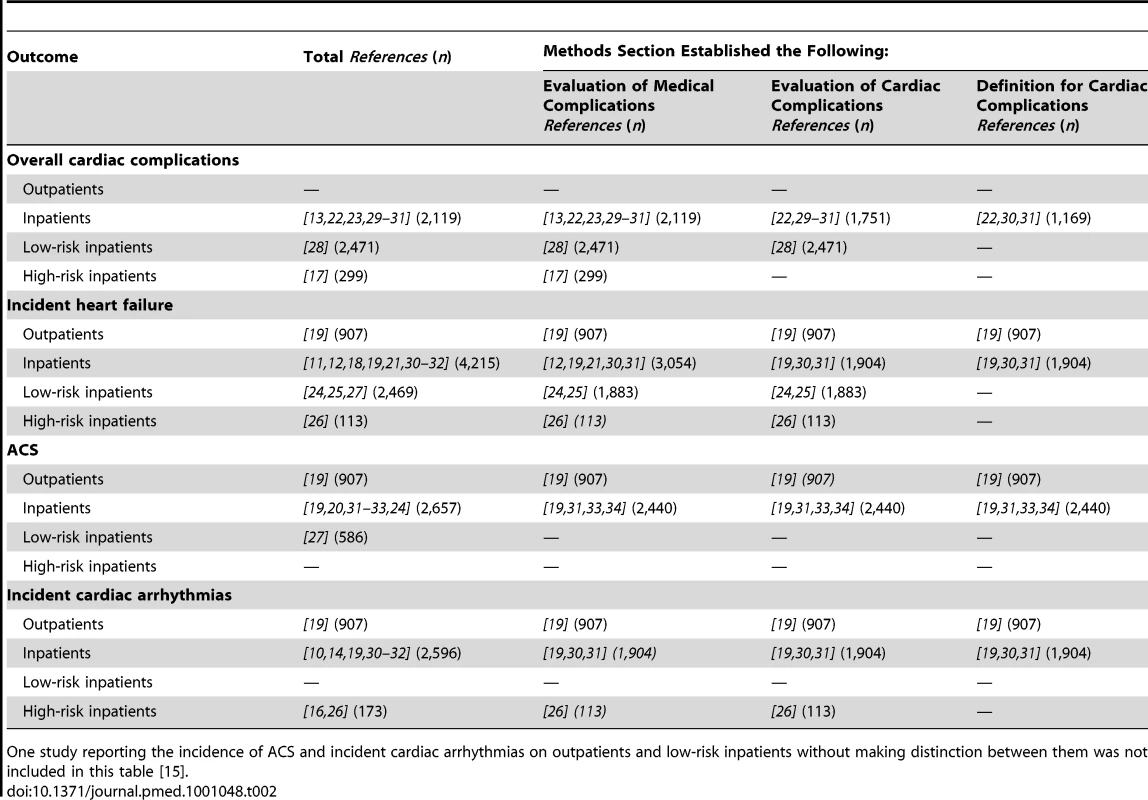
One study reporting the incidence of ACS and incident cardiac arrhythmias on outpatients and low-risk inpatients without making distinction between them was not included in this table [15]. Overall Cardiac Complications
Six studies focused on CAP inpatients [13],[22],[23],[29]–[31], one on low-risk inpatients [28], and one on high-risk inpatients [17]; with pooled incidence rates of 17.7% (CI 13.9–22.2) 5.9% (5.0–6.9), and 2.3% (1.0–4.9) for each of these groups, respectively (Figure 2).
Fig. 2. Pooled rates of the incidence of cardiac complications in patients with CAP. 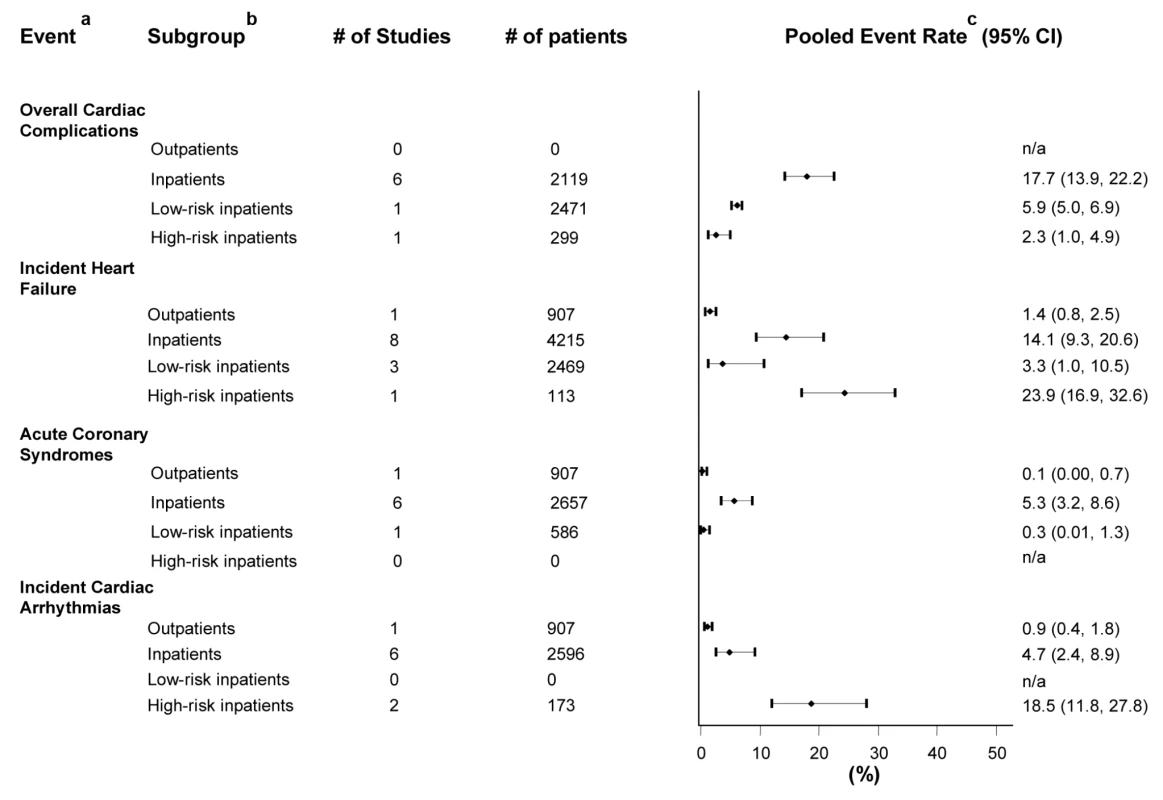
One study reporting the incidence of ACS and incident cardiac arrhythmias on outpatients and low-risk inpatients without making distinction between them was not included in the calculations of pooled rates [15]. aFor definitions refer to Table 1. bLow-risk inpatients included studies of inpatients with no indication for hospital admission, pneumonia severity index (PSI) risk-classes I–II, not initially admitted to intensive care units or who survived the first 48 h of hospitalization. High-risk inpatients included patients admitted to intensive care units. cWhen only one study was available, the reported rate represents the study event rate. Incident Heart Failure
One study reported on outpatients [19], eight on inpatients [11],[12],[18],[19],[21],[30]–[32], three on low-risk inpatients [24],[25],[27] and one on high-risk inpatients [26]. The pooled incidence rates for each of these groups were 1.4% (0.8–2.5), 14.1% (9.3–20.6), 3.3% (1.0–10.5), and 23.9% (16.9–32.6), respectively (Figure 2).
Acute Coronary Syndromes
Five studies reported only on myocardial infarction [15],[19],[20],[31],[33], one on unstable angina [27], and two on ACS in general [32],[34]. One study reported on outpatients and low-risk inpatients without making distinction between them and was not accounted for in the calculations of pooled rates [15]. One study focused on outpatients [19], six on inpatients [19],[20],[31]–[34], and one on low-risk inpatients [27], with pooled incidence rates of 0.1% (0.0–0.7), 5.3% (3.2–8.6), and 0.3% (0.01–1.3), respectively (Figure 2).
Incident Cardiac Arrhythmias
Five studies reported solely on atrial fibrillation [10],[14],[15],[31],[32], one study on all atrial arrhythmias [19], two on cardiac arrhythmias in general [16],[26], and one on atrial fibrillation (88% of the cases) and ventricular arrhythmias (excluding terminal arrhythmias) [30]. One study reporting on outpatients and low-risk inpatients without making distinction between them was not included in the calculations of pooled rates [15]. One study evaluated outpatients [19], six studied inpatients [10],[14],[19],[30]–[32], and two focused on high-risk inpatients [16],[26]; giving pooled incidence rates of 0.9% (0.4–1.8), 4.7% (2.4–8.9), and 18.5% (11.8–27.8), respectively (Figure 2).
Subgroup Analyses
Tables 3 and 4 describe the results of prespecified subgroup analyses of studies on CAP inpatients by characteristics of their setting, methodology, and population. Incident cardiac arrhythmias and incident heart failure were more common in papers published before 2000 and those coming from Europe. Overall cardiac complications and ACS, on the other hand, were more frequent in studies published between 2000 and 2005, and after 2005, respectively, and in papers coming from North America. All cardiac complications but ACS were more common in studies of prospective multicenter design. Additionally, all cardiac complications tended to occur more frequently in studies in which the evaluation of these events was stated in their methodological considerations or a definition for their ascertainment was available.
Tab. 3. Studies of cardiac complications in inpatients with CAP: Subgroup analysis by study setting and design. 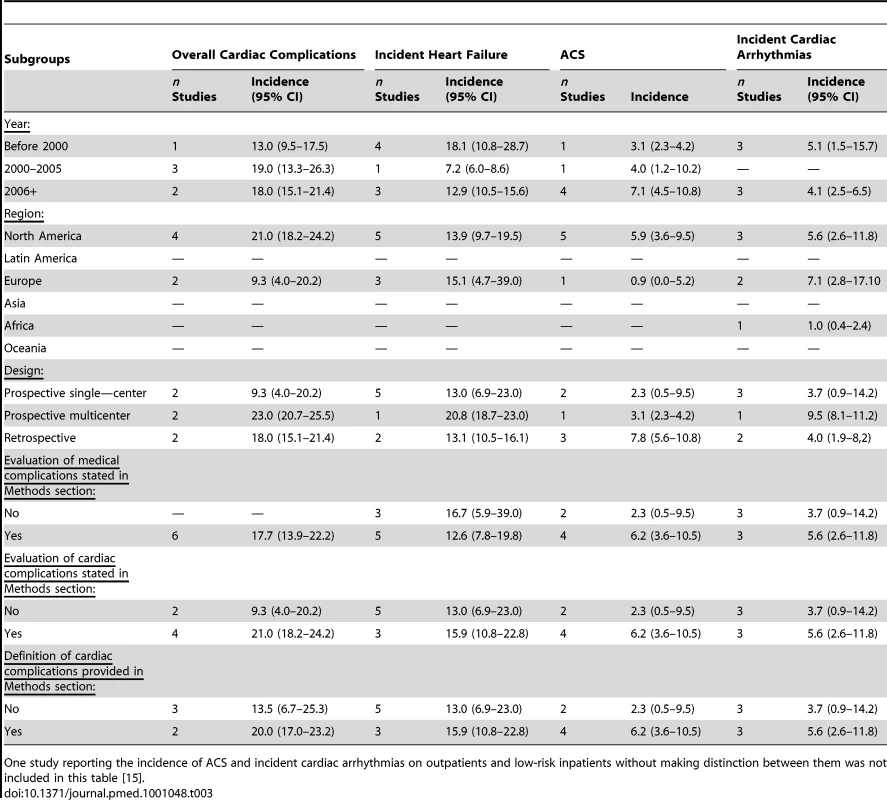
One study reporting the incidence of ACS and incident cardiac arrhythmias on outpatients and low-risk inpatients without making distinction between them was not included in this table [15]. Tab. 4. Studies of cardiac complications in inpatients with CAP: subgroup analysis by baseline characteristics of the population. 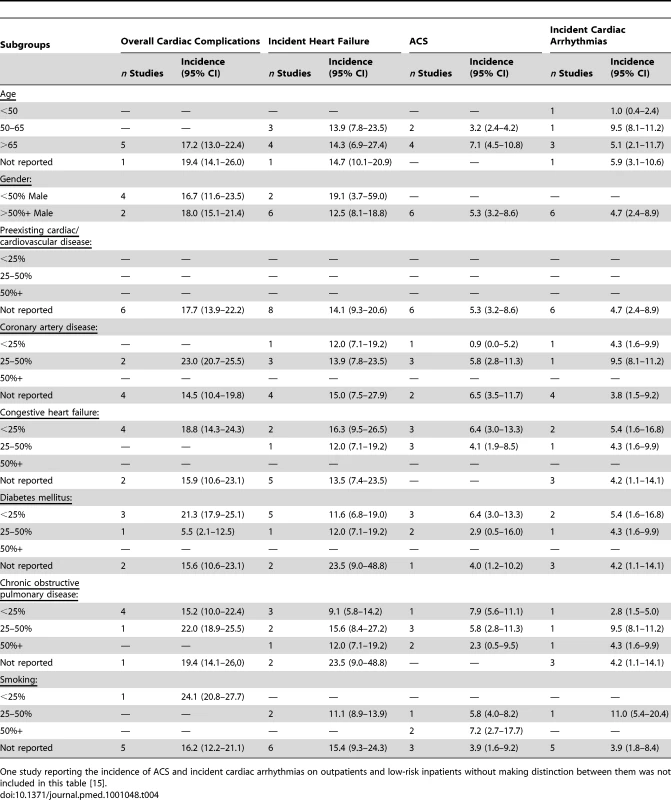
One study reporting the incidence of ACS and incident cardiac arrhythmias on outpatients and low-risk inpatients without making distinction between them was not included in this table [15]. Incident heart failure, incident cardiac arrhythmias, and ACS tended to be more common in studies with older populations and higher rates of preexisting coronary artery disease, but not in those with higher prevalence of preexisting congestive heart failure. Studies of predominantly female populations had higher incidences of incident heart failure, whereas the opposite was observed for overall cardiac complications. Rates of all cardiac complications but incident heart failure were lower in studies of patients with higher prevalence of diabetes mellitus. While overall cardiac complications, incident heart failure and incident cardiac arrhythmias were more common in studies with higher prevalence of chronic obstructive pulmonary disease, the opposite was observed for ACS. Finally, ACS occurred more commonly in studies of patients with higher rates of smoking.
Risk Factors and Impact of Cardiac Complications on CAP Outcomes
Only three studies [31],[33],[34], all dealing with CAP and ACS, attempted to analyze risk factors for the occurrence of cardiac complications. Possible risk factors identified included older age, preexisting congestive heart failure [34], severity of pneumonia [33], and the use of insulin by glucose sliding scales in hospitalized patients [31]. No study analyzed the association of cardiac complications with the development of other medical complications (i.e., acute renal failure, respiratory failure, shock, etc.), or the impact of these events on other CAP outcomes (i.e., mortality).
Discussion
Our main finding is that major cardiac complications occur in a significant proportion of patients with CAP, especially in those requiring hospitalization for this infection. The pooled incidence rates of overall cardiac complications, incident heart failure, ACS, and incident arrhythmias in hospitalized patients with CAP were 17.7%, 14.1%, 5.3%, and 4.7%, respectively. Given the burden of CAP in North America and other western societies [1],[2], these pooled findings have important implications. Firstly, clinicians need to realize the significance of this association for appropriate clinical alertness and to better inform CAP patients about the risk of cardiac complications once the diagnosis of pneumonia is made. Secondly, physicians and health officials need to increase efforts to optimize the rates of influenza and pneumococcal vaccination among the elderly and those with chronic cardiac conditions to reduce the incidence of CAP in these high-risk populations. Thirdly, attention needs to be directed to the potential impact of cardiac complications in the mortality and cost associated with CAP. Finally, the research community needs to urgently direct more efforts to the study of this area.
Our results expand on the findings of Fine et al. [9], who in the only previous systematic review on this topic reported four CAP cohorts (232 patients total) with a pooled incidence of heart failure of 8.6%. Our study not only confirms that incident heart failure is common in the course of CAP but suggests that its occurrence in patients hospitalized with this infection may be much higher than previously realized, and that ACS and cardiac arrhythmias are also remarkably frequent in this population.
Incident heart failure can be precipitated by CAP by several mechanisms [7],[30]. Acute inflammation can not only depress myocardial function, as it is well described in septic states [35],[36], but it can also increase large artery stiffness and the pulse wave reflections from peripheral middle-sized and small arteries that return to the heart in late systole, increasing left ventricular afterload and raising oxygen consumption [37]. Hypoxemia associated with CAP can raise pulmonary arterial pressure and right ventricular afterload while impairing myocardial oxygen delivery [7]. Tachycardia, common in acute infections, increases myocardial oxygen needs but shortens the diastolic period in which coronary perfusion occurs [38]–[40]. The net result of these effects is a shift in the metabolic supply/demand ratio of the myocardium and further impairment of its function. These changes are presumed to be of greater significance in patients with preexisting cardiac disease. In addition, incident heart failure in CAP can result from myocardial inflammation (myocarditis), a complication well described in patients with pneumonia mainly of viral origin, and that could have been underrepresented in previous investigations because of a lack of adequate noninvasive techniques for its identification (i.e., cardiac magnetic resonance imaging) [41]. Finally, we realize that acute renal impairment, common in hospitalized CAP patients [19], can also play a role in this setting [42].
Acute infections, including CAP, can also trigger the occurrence of ACS, and clinical studies have shown a significant temporal increase in the risk of ACS soon after the development of respiratory infections [34],[43],[44]. Surges of biomechanical stress, as a result of increased sympathetic activity and other hemodynamic changes (i.e. alterations of the circulatory volume and the systemic and coronary vascular tone), can prompt plaque rupture [7]. Acute infections can also promote plaque disruption by increasing intraplaque inflammatory activity [7]. In this setting, thrombus formation over a disrupted coronary plaque—a key step in the development of ACS—would be favoured by infection-induced prothrombotic changes in the blood and endothelium [7]. In addition, preexisting coronary artery disease that doesn't produce myocardial ischemia under baseline conditions can result in significant ischemia in the face of increased metabolic demands associated with CAP (i.e., demand ischemia; see above).
Most of the cardiac arrhythmias reported in the reviewed studies represented atrial tachyarrhythmias, particularly atrial fibrillation. Abnormalities in the cardiac conduction system in the setting of acute pneumonia have been recognized since the early 20th century and consistently confirmed thereafter [45],[46]. More recently, a study of more than 800,000 patients admitted to the hospital with atrial fibrillation as a secondary condition found that in patients 65 y of age or older, the second leading primary diagnosis was pneumonia (7%), after only congestive heart failure (13%), and before acute myocardial infarction (6%) [8].
While incident heart failure, ACS, and cardiac arrhythmias constitute distinct clinical entities, they share many pathophysiological bases and risk factors, and the occurrence of one of them can as well trigger the development of the others. While only one study in our review clearly documented the frequent concomitant occurrence of more than one cardiac complication in CAP patients [30], we think that this scenario is likely to be rather common.
Our study highlights several shortcomings of the medical literature on this area, which might influence our interpretations. Only a small proportion of studies primarily focused on cardiac outcomes and very few provided a definition for them, raising concerns for potential bias in the ascertainment and/or reporting of these events in those studies that did not. This is relevant especially for incident heart failure and ACS since their manifestations can overlap with those of CAP and other associated conditions (i.e., lung injury). Nevertheless, the few studies that provided clear definitions for the cardiac complications of interest consistently reported substantial incidences of these outcomes, providing reassurance for the validity of our findings. Only three studies of CAP and ACS looked at possible risk factors for the occurrence of these events but their analyses were largely underpowered and limited [31],[33],[34]. While it seems intuitive to think that the presence of preexisting cardiac conditions should have an important effect on the risk of cardiac complications in patients with CAP, further research will be needed to delineate their significance in this setting. As well, the association of cardiac complications with the development of other medical complications (i.e., acute renal failure, respiratory failure, shock, etc.), or the impact of these events in other CAP outcomes (i.e., mortality) is yet to be established. Finally, little is known about the timing of these complications, and only one study suggested that ACS in CAP patients tend to occur within few days after hospital admission [34].
Our work has limitations beyond the methodological shortcomings of the individual analyzed studies. We cannot rule out potential publication bias against studies that found no significant occurrences of cardiac complications. Additionally, we can only assume that the diagnostic evaluations in individual studies were performed in a uniform manner and the ascertainment of cardiac events was correct. The small number of studies dealing with CAP populations other than inpatients as a whole prevents us from drawing firm conclusions on the incidence of cardiac complications in these groups; and the finding of a counter-intuitively lower incidence of overall cardiac complications in high-risk CAP inpatients could be explained by this factor. The implied differences in the management of inpatients and outpatients may have led to the under-reporting of cardiac events in studies dealing with the latter group. Although studies of cardiac complications in CAP inpatients were the most common in our review, their number was still underpowered for performing adequate analyses (i.e., meta-regression) of factors that could account for the heterogeneity in their findings, and any appreciable difference observed in our subgroup analyses should be viewed in this context. Our review was limited to cardiac complications occurring within 30 d from presentation with CAP because it is assumed that the influence of the infection on patients' comorbid conditions is maximal during this time [47]; however, it is plausible that this influence can go beyond this period as it has been suggested by recent studies [44],[48]. Likewise, many of the mechanisms implicated in the development of cardiac complications in patients with CAP could account for similar occurrences in other infectious and noninfectious acute inflammatory states [7]. In fact, evidence suggests that acute infections of the urinary and gastrointestinal tract are also associated with increased risk of ACS in the short term [7],[44],[49]. However, exploring the magnitude of these associations was beyond the scope of our review.
Our findings highlight the urgent need for prospective, well-designed, and adequately powered studies of cardiac complications in patients with CAP. Investigations should focus on identifying risk factors for the occurrence of cardiac complications in this population and developing strategies to identify those CAP patients at high risk for developing these events. These strategies may include clinical scoring systems, biomarker-based approaches, noninvasive cardiac imaging, or a combination of these. Studies are also needed to characterize the impact of cardiac complications on the mortality and resource utilization associated with CAP. Careful mechanistic studies of the pathophysiology of cardiac complications in the course of CAP and the role of preexisting heart disease in their development should serve for the appropriate design of interventions aimed at preventing their occurrence in high-risk groups. As an example, discriminating between acute plaque rupture versus demand ischemia as the factor driving the occurrence of ACS in this population will have important and obvious therapeutic implications. Such interventions will need to be tested in randomized clinical trials. The ultimate goal will be to improve the outcomes of patients with CAP and to decrease the burden that this disease imposes on our health care systems through recognition of risk, prevention, and intervention on acute cardiac complications.
Supporting Information
Zdroje
1. RautMScheinJModySGrantRBensonC 2009 Estimating the economic impact of a half-day reduction in length of hospital stay among patients with community-acquired pneumonia in the US. Curr Med Res Opin 25 2151 2157
2. FileTMJrMarrieTJ 2010 Burden of community-acquired pneumonia in North American adults. Postgrad Med 122 130 141
3. FryAMShayDKHolmanRCCurnsATAndersonLJ 2005 Trends in hospitalizations for pneumonia among persons aged 65 years or older in the United States, 1988–2002. JAMA 294 2712 2719
4. Lloyd-JonesDAdamsRJBrownTMCarnethonMDaiS 2010 Heart disease and stroke statistics–2010 update: a report from the American Heart Association. Circulation 121 e46 e215
5. United States Census Bureau 2008 National Population Projections Washington (D.C.) U.S. Census Bureau
6. KhandAUGemmellIRankinACClelandJG 2001 Clinical events leading to the progression of heart failure: insights from a national database of hospital discharges. Eur Heart J 22 153 164
7. Corrales-MedinaVFMadjidMMusherDM 2010 Role of acute infection in triggering acute coronary syndromes. Lancet Infect Dis 10 83 92
8. WattigneyWAMensahGACroftJB 2003 Increasing trends in hospitalization for atrial fibrillation in the United States, 1985 through 1999: implications for primary prevention. Circulation 108 711 716
9. FineMJSmithMACarsonCAMuthaSSSankeySS 1996 Prognosis and outcomes of patients with community-acquired pneumonia. A meta-analysis. JAMA 275 134 141
10. AllenSC 1984 Lobar pneumonia in Northern Zambia: clinical study of 502 adult patients. Thorax 39 612 616
11. EspositoAL 1984 Community-acquired bacteremic pneumococcal pneumonia. Effect of age on manifestations and outcome. Arch Intern Med 144 945 948
12. MarrieTJDurantHYatesL 1989 Community-acquired pneumonia requiring hospitalization: 5-year prospective study. Rev Infect Dis 11 586 599
13. OrtqvistAHedlundJGrillnerLJalonenEKallingsI 1990 Aetiology, outcome and prognostic factors in community-acquired pneumonia requiring hospitalization. Eur Respir J 3 1105 1113
14. VenkatesanPGladmanJMacfarlaneJTBarerDBermanP 1990 A hospital study of community acquired pneumonia in the elderly. Thorax 45 254 258
15. FineMJSmithDNSingerDE 1990 Hospitalization decision in patients with community-acquired pneumonia: a prospective cohort study. Am J Med 89 713 721
16. 1992 The aetiology, management and outcome of severe community-acquired pneumonia on the intensive care unit. The British Thoracic Society Research Committee and The Public Health Laboratory Service. Respir Med 86 7 13
17. LeroyOSantreCBeuscartCGeorgesHGueryB 1995 A five-year study of severe community-acquired pneumonia with emphasis on prognosis in patients admitted to an intensive care unit. Intensive Care Med 21 24 31
18. JanssensJPGautheyLHerrmannFTkatchLMichelJP 1996 Community-acquired pneumonia in older patients. J Am Geriatr Soc 44 539 544
19. FineMJStoneRASingerDEColeyCMMarrieTJ 1999 Processes and outcomes of care for patients with community-acquired pneumonia: results from the Pneumonia Patient Outcomes Research Team (PORT) cohort study. Arch Intern Med 159 970 980
20. MusherDMAlexandrakiIGravissEAYanbeiyNEidA 2000 Bacteremic and nonbacteremic pneumococcal pneumonia. A prospective study. Medicine (Baltimore) 79 210 221
21. Fernandez-SabeNCarratalaJRosonBDorcaJVerdaguerR 2003 Community-acquired pneumonia in very elderly patients: causative organisms, clinical characteristics, and outcomes. Medicine (Baltimore) 82 159 169
22. FineMJStoneRALaveJRHoughLJObroskyDS 2003 Implementation of an evidence-based guideline to reduce duration of intravenous antibiotic therapy and length of stay for patients hospitalized with community-acquired pneumonia: a randomized controlled trial. Am J Med 115 343 351
23. Martinez-MoragonEGarcia FerrerLSerra SanchisBFernandez FabrellasEGomez BeldaA 2004 [Community-acquired pneumonia among the elderly: differences between patients living at home and in nursing homes]. Arch Bronconeumol 40 547 552
24. MenendezRTorresAZalacainRAspaJMartin VillasclarasJJ 2004 Risk factors of treatment failure in community acquired pneumonia: implications for disease outcome. Thorax 59 960 965
25. Querol-RibellesJMTeniasJMQuerol-BorrasJMLabradorTNietoA 2005 Levofloxacin versus ceftriaxone plus clarithromycin in the treatment of adults with community-acquired pneumonia requiring hospitalization. Int J Antimicrob Agents 25 75 83
26. DiazAAlvarezMCallejasCRossoRSchnettlerK 2005 [Clinical picture and prognostic factors for severe community-acquired pneumonia in adults admitted to the intensive care unit]. Arch Bronconeumol 41 20 26
27. MarrieTJHuangJQ 2005 Low-risk patients admitted with community-acquired pneumonia. Am J Med 118 1357 1363
28. McAlisterFAMajumdarSRBlitzSRoweBHRomneyJ 2005 The relation between hyperglycemia and outcomes in 2,471 patients admitted to the hospital with community-acquired pneumonia. Diabetes Care 28 810 815
29. O'MearaESWhiteMSiscovickDSLylesMFKullerLH 2005 Hospitalization for pneumonia in the Cardiovascular Health Study: incidence, mortality, and influence on longer-term survival. J Am Geriatr Soc 53 1108 1116
30. MusherDMRuedaAMKakaASMaparaSM 2007 The association between pneumococcal pneumonia and acute cardiac events. Clin Infect Dis 45 158 165
31. BeckerTMoldoveanuACukiermanTGersteinHC 2007 Clinical outcomes associated with the use of subcutaneous insulin-by-glucose sliding scales to manage hyperglycemia in hospitalized patients with pneumonia. Diabetes Res Clin Pract 78 392 397
32. CabreMSerra-PratMForceLPalomeraEPallaresR 2008 Functional status as a risk factor for mortality in very elderly patients with pneumonia. Med Clin (Barc) 131 167 170
33. RamirezJAlibertiSMirsaeidiMPeyraniPFilardoG 2008 Acute myocardial infarction in hospitalized patients with community-acquired pneumonia. Clin Infect Dis 47 182 187
34. Corrales-MedinaVFSerpaJRuedaAMGiordanoTPBozkurtB 2009 Acute bacterial pneumonia is associated with the occurrence of acute coronary syndromes. Medicine (Baltimore) 88 154 159
35. MaederMFehrTRickliHAmmannP 2006 Sepsis-associated myocardial dysfunction: diagnostic and prognostic impact of cardiac troponins and natriuretic peptides. Chest 129 1349 1366
36. SuffrediniAFFrommREParkerMMBrennerMKovacsJA 1989 The cardiovascular response of normal humans to the administration of endotoxin. N Engl J Med 321 280 287
37. ChirinosJASegersP 2010 Noninvasive evaluation of left ventricular afterload: part 2: arterial pressure-flow and pressure-volume relations in humans. Hypertension 56 563 570
38. FerroGDuilioCSpinelliLLiucciGAMazzaF 1995 Relation between diastolic perfusion time and coronary artery stenosis during stress-induced myocardial ischemia. Circulation 92 342 347
39. SarnoffSJBraunwaldEWelchGHJrCaseRBStainsbyWN 1958 Hemodynamic determinants of oxygen consumption of the heart with special reference to the tension-time index. Am J Physiol 192 148 156
40. MerkusDKajiyaFVinkHVergroesenIDankelmanJ 1999 Prolonged diastolic time fraction protects myocardial perfusion when coronary blood flow is reduced. Circulation 100 75 81
41. MavrogeniSManoussakisMN 2010 Myocarditis as a complication of influenza A (H1N1): evaluation using cardiovascular magnetic resonance imaging. Hellenic J Cardiol 51 379 380
42. BockJSGottliebSS 2010 Cardiorenal syndrome: new perspectives. Circulation 121 2592 2600
43. ClaytonTCThompsonMMeadeTW 2008 Recent respiratory infection and risk of cardiovascular disease: case-control study through a general practice database. Eur Heart J 29 96 103
44. SmeethLThomasSLHallAJHubbardRFarringtonP 2004 Risk of myocardial infarction and stroke after acute infection or vaccination. N Engl J Med 351 2611 2618
45. DegraffACTravellJGYagerJA 1931 An electrocardiographic study of the heart in lobar pneumonia. J Clin Invest 10 633 651
46. MorganrothJDimarcoJPAnzuetoANiedermanMSChoudhriS 2005 A randomized trial comparing the cardiac rhythm safety of moxifloxacin vs levofloxacin in elderly patients hospitalized with community-acquired pneumonia. Chest 128 3398 3406
47. MusherDM 2008 Clinical and microbiological end points in the treatment of pneumonia. Clin Infect Dis 47 Suppl 3 S207 209
48. YendeSD'AngeloGKellumJAWeissfeldLFineJ 2008 Inflammatory markers at hospital discharge predict subsequent mortality after pneumonia and sepsis. Am J Respir Crit Care Med 177 1242 1247
49. BaylinAHernandez-DiazSSilesXKabagambeEKCamposH 2007 Triggers of nonfatal myocardial infarction in Costa Rica: heavy physical exertion, sexual activity, and infection. Ann Epidemiol 17 112 118
Štítky
Interní lékařství
Článek vyšel v časopisePLOS Medicine
Nejčtenější tento týden
2011 Číslo 6- Berberin: přírodní hypolipidemikum se slibnými výsledky
- Léčba bolesti u seniorů
- Příznivý vliv Armolipidu Plus na hladinu cholesterolu a zánětlivé parametry u pacientů s chronickým subklinickým zánětem
- Červená fermentovaná rýže účinně snižuje hladinu LDL cholesterolu jako vhodná alternativa ke statinové terapii
- Jak postupovat při výběru betablokátoru − doporučení z kardiologické praxe
-
Všechny články tohoto čísla
- The First Model-Based Geostatistical Map of Anaemia
- The Dynamics of Health and Return Migration
- Life Course Trajectories of Systolic Blood Pressure Using Longitudinal Data from Eight UK Cohorts
- Evaluation of Coseasonality of Influenza and Invasive Pneumococcal Disease: Results from Prospective Surveillance
- Energy Density, Portion Size, and Eating Occasions: Contributions to Increased Energy Intake in the United States, 1977–2006
- Scaling Up Global Health Interventions: A Proposed Framework for Success
- The Effect of Highly Active Antiretroviral Therapy on the Survival of HIV-Infected Children in a Resource-Deprived Setting: A Cohort Study
- Cardiac Complications in Patients with Community-Acquired Pneumonia: A Systematic Review and Meta-Analysis of Observational Studies
- Epidemiological Characteristics of 2009 (H1N1) Pandemic Influenza Based on Paired Sera from a Longitudinal Community Cohort Study
- Mapping the Risk of Anaemia in Preschool-Age Children: The Contribution of Malnutrition, Malaria, and Helminth Infections in West Africa
- More and Better Information to Tackle HIV Epidemics: Towards Improved HIV Incidence Assays
- Human Trafficking: The Shameful Face of Migration
- Global Protection and the Health Impact of Migration Interception
- Migration and "Low-Skilled" Workers in Destination Countries
- The Effect of Handwashing at Recommended Times with Water Alone and With Soap on Child Diarrhea in Rural Bangladesh: An Observational Study
- PLOS Medicine
- Archiv čísel
- Aktuální číslo
- Informace o časopisu
Nejčtenější v tomto čísle- Migration and "Low-Skilled" Workers in Destination Countries
- Mapping the Risk of Anaemia in Preschool-Age Children: The Contribution of Malnutrition, Malaria, and Helminth Infections in West Africa
- More and Better Information to Tackle HIV Epidemics: Towards Improved HIV Incidence Assays
- Energy Density, Portion Size, and Eating Occasions: Contributions to Increased Energy Intake in the United States, 1977–2006
Kurzy
Zvyšte si kvalifikaci online z pohodlí domova
Současné možnosti léčby obezity
nový kurzAutoři: MUDr. Martin Hrubý
Všechny kurzyPřihlášení#ADS_BOTTOM_SCRIPTS#Zapomenuté hesloZadejte e-mailovou adresu, se kterou jste vytvářel(a) účet, budou Vám na ni zaslány informace k nastavení nového hesla.
- Vzdělávání



