-
Články
Top novinky
Reklama- Vzdělávání
- Časopisy
Top články
Nové číslo
- Témata
Top novinky
Reklama- Videa
- Podcasty
Nové podcasty
Reklama- Kariéra
Doporučené pozice
Reklama- Praxe
Top novinky
ReklamaDefining Research to Improve Health Systems
article has not abstract
Published in the journal: . PLoS Med 7(11): e32767. doi:10.1371/journal.pmed.1001000
Category: Policy Forum
doi: https://doi.org/10.1371/journal.pmed.1001000Summary
article has not abstract
Summary Points
-
Research has an important role to play in strengthening health systems to improve system performance and public health impact.
-
The multiple definitions of operational research, implementation research, and health systems research creates confusion and negatively affects the credibility and progress of the research.
-
The aim of this paper is to present working definitions of operational research, implementation research, and health systems research to provide greater clarity for non-specialists, scientists, policymakers, and donors working to strengthen health systems.
Introduction
A major obstacle to achieving the health-related Millennium Development Goals (MDGs) is the weakness of the health systems in many low - and middle-income countries, and their struggle to effectively provide health care to populations in need [1],[2]. Several global health initiatives have been created over the last decade to support the delivery of available interventions for priority health problems, and in recent years there have been some major new initiatives to support health system strengthening [1],[3],[4]. These developments have been accompanied by a growing recognition of the role of research in improving health systems and health care delivery. The ministerial summit on health research that was held in Mexico in 2004 concluded that research has a crucial part to play in strengthening health systems and in improving the equitable distribution of quality health services for populations in need, and the summit called for greater support for such research [5]. Since then, the number of research initiatives on health systems in low - and middle-income countries has increased substantially [6],[7]. This is a positive development that we would like to see expanded and accelerated to build up evidence-based knowledge to improve the effectiveness of health systems. Unfortunately, these initiatives have also led to growing confusion about what type of research is involved and at whom that research is targeted. The fact that the various research initiatives originate from different research backgrounds (biomedicine, social sciences, organization of services, health economics, etc.) has led to an inconsistent use of terminology to describe the research. Multiple definitions of operational research, implementation research, and health systems research have been proposed in recent years [2],[6]–[18], and many of these define the scope of their research very broadly, resulting in considerable overlap between definitions. Operational research and implementation research are sometimes used interchangeably in the literature, or are classified as health systems research [10]–[12],[17].
So does this matter?
We believe it does, because the resulting confusion may create duplications and inefficiencies both in the funding for different research efforts and among those seeking to understand and use the evidence. It indicates a lack of shared conceptual clarity among scientists and decision-makers about the scope, nature, methodologies, and issues to be addressed by the research involved [6]. This makes efforts to retrieve relevant evidence on particular topics even more complex than it already is, negatively affecting the credibility of the research itself.
The aim of this paper is to present working definitions of operational research, implementation research, and health systems research in the context of research to strengthen health systems, with the intention of providing greater clarity and consistency for non-specialists, scientists, policymakers, and donors.
As a starting point, the three research areas described here refer to research domains that differ at their core in the type of research questions they address, in how they are organized, and in how they interface with the health system. Below, we briefly describe the proposed three domains, indicate where they differ and overlap, how they complement each other, and how they could more effectively interact for greater impact of the overall research effort. We hope that, in this year with an unprecedented focus on research to strengthen health systems with the First Global Symposium on Health Systems Research this paper will contribute to greater clarity and more efficient approaches to fulfil the overall objective of strengthening health systems to improve population health [19].
Defining the Research Domains
Building on the numerous definitions that exist in the literature under the overall umbrella of research to improve health systems, three domains of research can be defined using their primary characteristics: the focus of the research, the users of the research outputs, and the utility of the research outputs (see Figure 1 and Table 1).
Fig. 1. Research to improve health systems. 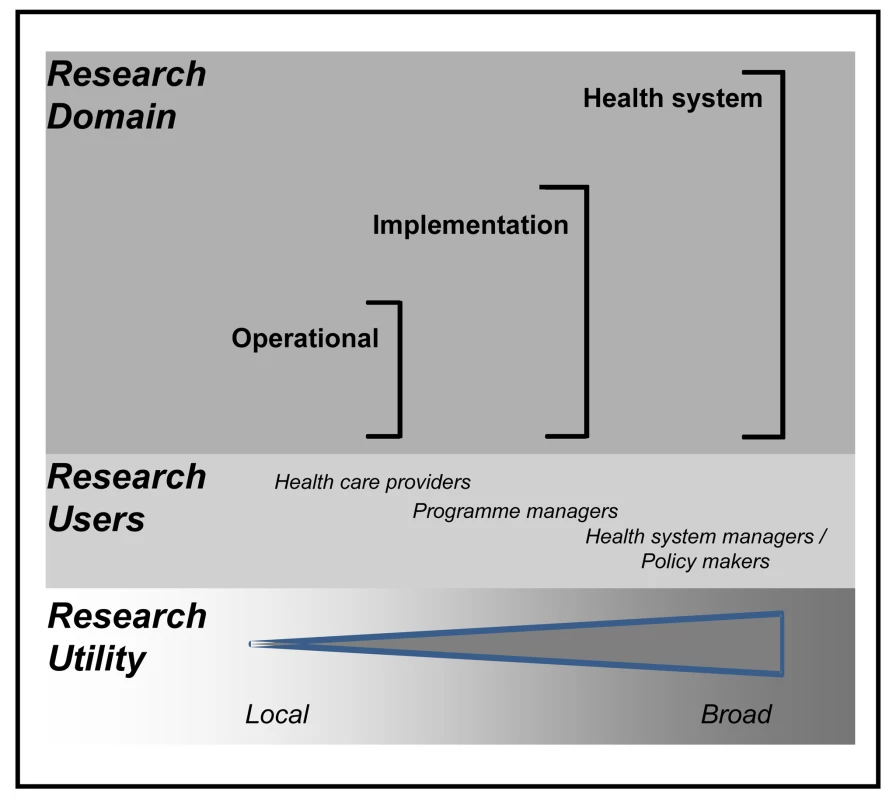
Tab. 1. Defining research to improve health systems. 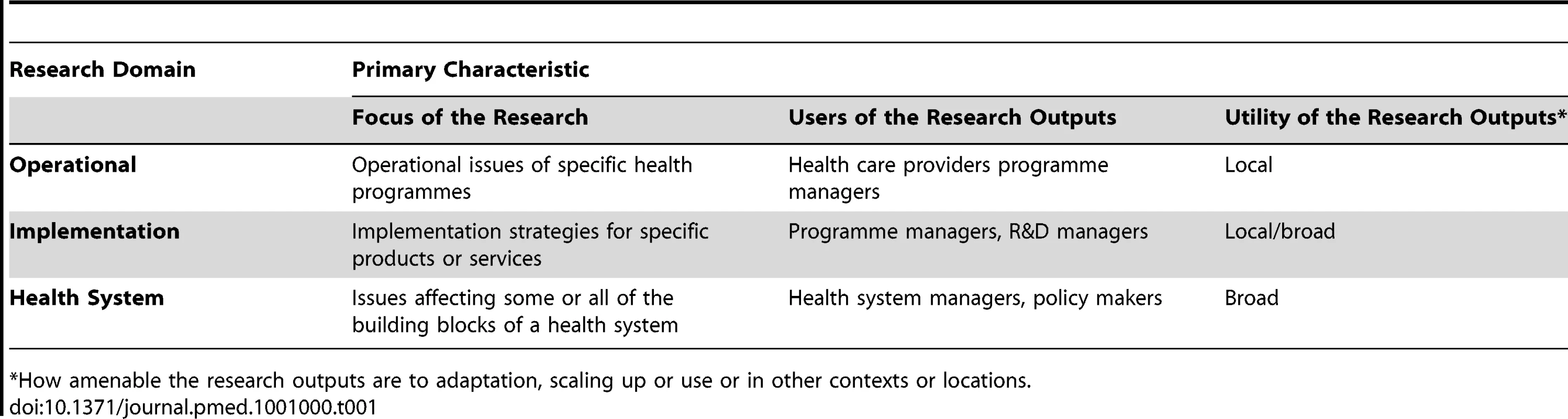
*How amenable the research outputs are to adaptation, scaling up or use or in other contexts or locations. The focus of the research within a health system [20] is explained more fully in the following sections.
The users of the research outputs (published results, findings, methodologies, etc.) fall broadly into three groups with operational research being predominantly, but not exclusively, of use to health care providers; implementation research predominantly of use to managers of programmes scaling up an intervention; and research on the health system as a whole (or one of its building blocks) of most use to those who manage or need to make policy for the health system.
In another characteristic, the importance of how amenable the research is to adaptation and use in other contexts or locations—also varies across the three domains. We define this characteristic as the utility of the research, where utility describes the fact, character, or quality of something being useful or serviceable [21]. While it is well established that all research to support health systems is context-specific, careful consideration of study design and reporting of context-specific factors generally improve the application of this research to other settings. This can be achieved in varying degrees of success across the three domains. For example, operational research tends to address a local problem, taking into account the particular context in which it occurs. Therefore, the research utility of the outputs would not be readily applicable to other settings without careful and considerable adaptation.
As it moves through implementation research and onto health systems research, the utility of the research tends to be broader and have increasingly common points of comparison with other contexts. Therefore, it is not uncommon to be able to generate lessons from this type of research that are applicable to other settings within the country or even for other countries. So, using research utility as defined here, operational research generates research outputs that are generally local in their utility, and health systems research has a primary characteristic of generally being more amenable to adaptation and application in other contexts, i.e., a broad utility. Again the degree of utility is wholly dependent on the use of an appropriate study design or protocol that takes into consideration of contextual factors.
In subsequent sections we will elaborate on these definitions using case studies and examples to illustrate them.
1. Research Domain: Operational
Operational research aims to develop solutions to current operational problems of specific health programmes or specific service delivery components of the health system, e.g., a health district or a hospital. Table 2 gives some selected examples of research questions that illustrate the local nature of the type of problems that this research addresses. These are problems that confront a local disease control programme, health district, or health clinic during the execution of its routine operations, and for which practically useful answers or solutions are urgently needed to allow operations to proceed more effectively. This research is characterized by a strong problem-solving focus and an urgency to find solutions. Its demand-driven nature and close association with health care delivery and routine health care operations ensure operational relevance of the research activities and rapid uptake and local utilization of research findings. The operational problems are often identified through routine monitoring and evaluation activities for which this research, where it exists, can be an important complement that allows a health programme to explore new ideas and experiment with potentially more effective approaches to its operations.
Tab. 2. Examples of research questions for the three research domains. 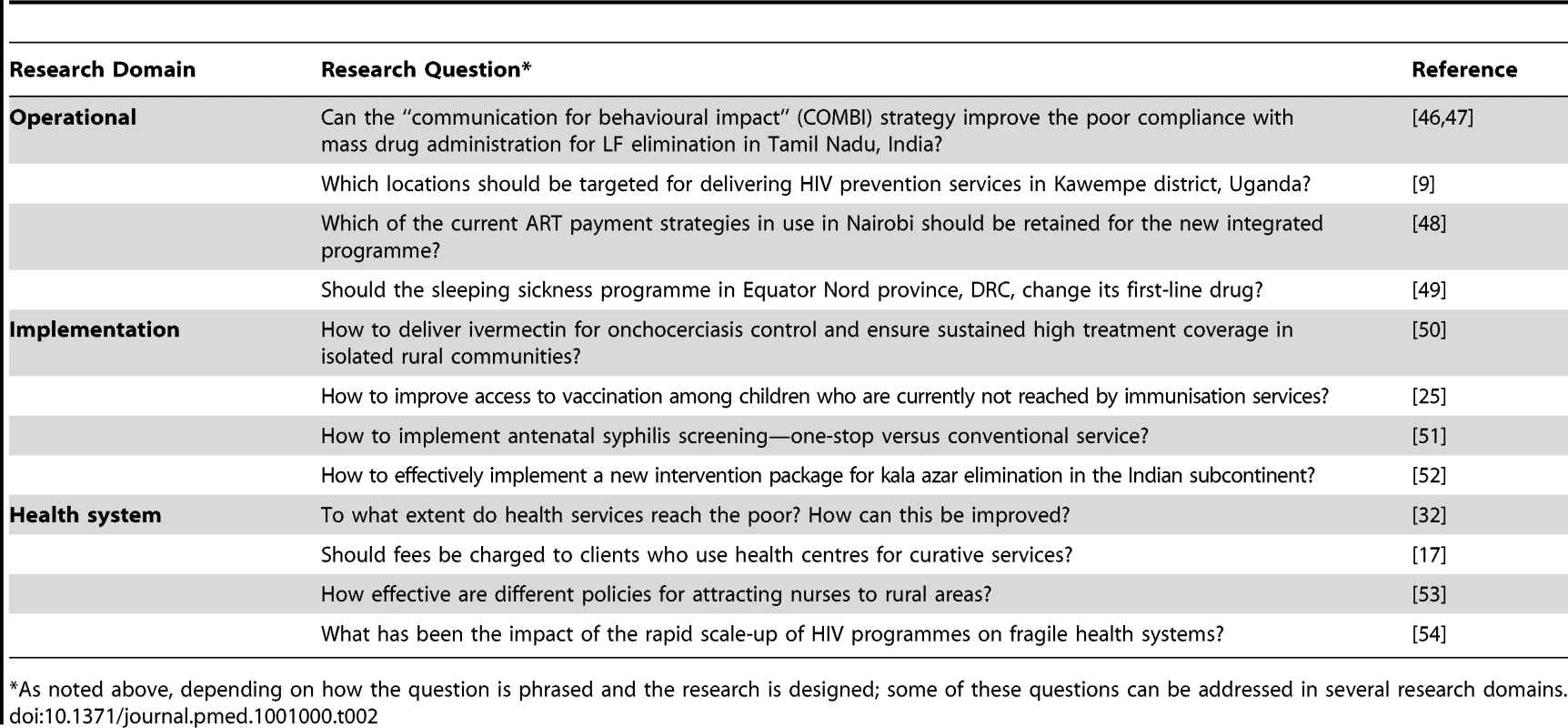
*As noted above, depending on how the question is phrased and the research is designed; some of these questions can be addressed in several research domains. A wide range of study designs and research methods are used, ranging from descriptive and analytical studies to operational experiments and the use of mathematical modelling. The research often starts with exploratory studies to better define the problem and its determinants, and to identify potential solutions that can subsequently be tested under operational conditions. The research requires the involvement of, and is usually executed by, health staff who have the necessary research experience and/or by scientists from collaborating local research institutions. In their definition of operational research, Zachariah et al. [8] stress the local, programme-based focus of research that “can enhance the quality, effectiveness or coverage of programs in which the research is being done.” Similarly, WHO refers to research “for programme decision making to achieve a specific outcome” [22]; and the Global Fund refers to research that “provides decision-makers with information to enable them to improve the performance of their programs” [9]. Hence, the results of this research tend to have a local utility and, because of its design, are not generally amenable for adaptation and use in other settings. This in no way devalues the research, and useful lessons—such as methodological approaches—could be applied elsewhere if reported. However, operational research is still not commonly undertaken, and many of the lessons that could be learnt remain unpublished.
Many health programmes and health system managers do not see operational research as a priority, and it is sometimes perceived as a waste of time and resources, distracting from the need for operational action on the basis of “common sense” [23]. Such attitudes tend to soften with exposure to properly executed operational research that delivers practical results, but quality operational research does not come easily, given the general lack of research capacity and research funding at the operational level. Several global health initiatives offer additional funding for operational research but most of these funds are not taken up at country and programme level because of the lack of appreciation for this type of research and insufficient local research capacity [10].
2. Research Domain: Implementation
Implementation research aims to develop strategies for available or new health interventions in order to improve access to, and the use of, these interventions by the populations in need. Table 2 provides some examples of this type of research for which the starting point is the availability of an intervention or intervention package that has been proven efficacious in previous research, but for which major questions remain as to how to scale up the intervention and ensure effective integration within the health system. This research is characterized by a focus on the need for innovative approaches and/or ensuring the effectiveness of implemented interventions. Examples may include mass treatment with ivermectin for onchocerciasis or the introduction of new evidence-based birth practices for isolated communities where there are no formal health services or maternity clinics. This research often addresses implementation of newly developed products, such as a pharmaceutical, medical device, or vaccine, where this research represents the last phase of the product development pipeline. However, in this definition implementation research also covers such interventions as service delivery approaches, behavioural interventions, or understanding the impact of a payment mechanism.
Many promising health interventions have had only limited impact on the burden of disease in low - and middle-income countries because of implementation problems that were not identified, researched, and addressed. For example, research on the impact of insecticide-treated nets to reduce malaria was stopped too soon: phase IV effectiveness trials were not followed up by implementation research, and 15 years later the utilization of nets is still low in Africa. Hence, it is critical to include research on implementation as an extension of the development phase or R&D pipeline when testing a new intervention.
The examples of implementation research above tend to be developed as focused studies with clear research questions. Multicentre and multicountry studies are often used, as these help clarify which findings are location-specific and which are more generalisable. Large-scale implementation studies often have two phases. The first phase consists of descriptive, formative research to better understand the major implementation challenges and to design potential implementation strategies. This is often followed by a second phase, in which the most promising implementation strategies are tested and compared in large-scale experimental studies in settings at the appropriate level of the health system [24],[25]. Social science research methods are extensively used (including qualitative research methods for stakeholder analysis and process evaluation) as well as methods for determining the cost of implementation strategies at different levels of the formal and informal health system.
Implementation research is usually undertaken by multidisciplinary research groups drawn from many countries, including those where the study is located. There is often a network of such groups, supported by international research institutions and expertise as required. The necessary local research capacity in behavioural sciences, health economics, and epidemiology is still inadequate in many low-income countries, and building such research capacity remains a top priority [7],[14]. Where adequate research capacity does exist, it is often isolated, and special efforts may be needed to identify and involve such groups in research initiatives.
With regard to existing definitions, Sanders et al. refer to “research to promote the uptake and successful implementation of evidence-based interventions and policies” [12], and Allottey et al. to “evidence that informs effective, sustained and embedded adoption of interventions by health systems and communities” [13]. The Special Programme for Research and Training in Tropical Diseases (TDR) defines implementation research as “research to significantly improve access to efficacious interventions by developing practical solutions to common implementation problems” [14]. As these definitions indicate, implementation research is intervention-specific, but in contrast to operational research, it is often designed with the intention of creating outputs that can be applicable beyond the local environment in which the research is done.
The relevance of implementation research is increasingly being recognized, and several convincing examples in recent years have demonstrated the effectiveness of this type of research in enabling implementation and scale-up of priority health interventions [26],[27]. However, compared to the corresponding investment in R&D, implementation research is receiving only limited financial support; it will be important to correct this imbalance.
3. Research Domain: Health System
Health systems research addresses health system and policy questions that are not disease-specific but concern systems problems that have repercussions on the performance of the health system as a whole. It addresses a wide range of questions, from health financing, governance, and policy to problems with structuring, planning, management, human resources, service delivery, referral, and quality of care in the public and private sector. Table 2 gives a few examples of research questions that illustrate the nature of the research involved (e.g., studies on the effectiveness of different policies for attracting nurses to rural areas). Health systems issues are often highly context-specific, and many case studies try to elucidate a certain health system challenge within its specific environment.
However, with appropriate study design and planning, health systems research can not only answer policy questions relevant to the specific health system in which the research is undertaken, but can generate valuable lessons that are more amenable to adaptation and adoption in other settings. This is particularly true when a systems perspective is used, i.e., by considering all the positive and negative effects of a particular system-level intervention, this research can provide a robust and accurate understanding of health systems challenges and their potential solutions, thereby improving the utility of the findings in other settings [28]. This systems approach, in combination with stakeholder engagement, also informs the definition of priority research questions to address health systems challenges.
Health systems research by necessity is highly multidisciplinary, with a strong emphasis on social sciences, economics, and anthropological investigations, for example on community perceptions of health care. Much ongoing research consists of descriptive, comparative, and evaluation studies and secondary analytical research. Although experimental studies are less common, partly because of operational and ethical challenges in experimenting at the health system level, they can be very informative and provide convincing evidence on the benefit of innovations in health system efficiency and health impact [29]. Most research is undertaken through collaboration between academic institutions, with a major role being played by a few institutions with special expertise in health systems research or in one of its research disciplines (e.g., health economics and policy analysis). Health planners and decision-makers may contribute to defining the research questions, but are otherwise not much involved in undertaking the research itself [6].
The research in this domain falls under the general definition by the Alliance for Health Policy and Systems Research (HPSR) as: “The production of new knowledge to improve how societies organize themselves to achieve health goals.” The Alliance for HPSR further clarifies that “the prime focus of health policy and systems research is not a specific disease or service, but rather the health system as a whole. However, health systems research sometimes adopts a disease or service specific focus” (http://www.who.int/alliance-hpsr/en/ [17]). More specifically, it can address any or all of the six building blocks of health systems identified by the WHO [20]: service delivery, information and evidence, medical products and technologies, health workforce, health financing, and leadership and governance. In doing so, it should explicitly acknowledge the importance of the continuous interactions between the different building blocks of the health systems and the different sectors (including non-health sectors) involved, as well as all the other characteristics of complex health systems [28]. Another definition offered by Varkevisser et al. [30] refers to health systems research as “research that enhances the efficiency and effectiveness of the health system.”
Research on health systems addresses a huge research area that has only been marginally covered to date [6]. Because of the multitude of system challenges and their complex multidimensional environment, research prioritization is essential and some recent priority-setting initiatives are seen as being timely [20],[31]–[33]. Due to the relative scarcity of research capacity to undertake this type of research, efforts to improve the design, robustness, and applicability of the evidence generated in one setting to another would be highly desirable. Systems thinking methods and approaches can offer tremendous help and guidance on this [28]. By using a systematic, comprehensive way of examining the design and evaluation of potential health systems interventions, and ensuring involvement and ownership of all stakeholders involved, the utility and pay back from the evidence generated from this research greatly increases.
Related Research Areas and Research Terms
There are a number of related research areas that may overlap with the above research domains but are out of the scope of this paper. Some of them are briefly described here. First, monitoring and evaluation aims to track the progress of a health intervention and to determine whether it is having its intended impact. As a routine operational activity, it is usually not regarded as research by itself, although its findings are instrumental for identifying priority problems for research. However, the term evaluation can sometimes refer to the more formal evaluation designs such as process, economic, or impact evaluations, or can be used separately to answer questions related to the three research domains described in this paper [34].
Intervention science—the development of new and improved health interventions—is another important area of research that may considerably overlap with implementation research [35],[36]. This science is mainly concerned with biomedical research, where the early stages of intervention development are often far removed from the field. However, as the development phase is nearing its completion, evaluation of the intervention effectiveness is usually done under real-life conditions [37]. Hence, towards the end of the development process, intervention development and implementation research tend to closely overlap.
Some terms are very similar to those used to describe the three research domains but have been used in different ways in the literature. Operations research usually refers to the use of mathematical optimization methods for operational decision making, but this is sometimes also called operational research [34],[35],[38].
Implementation science has been defined as the study of methods to promote the systematic uptake of research findings into routine clinical practice [39], and as such is complementary to knowledge translation (another term with its own diversity of definitions!) [40]–[42].
Implementation science has also been said to be similar to translational research or defined as ‘research that identifies barriers to proven interventions and that facilitates the creation of strategies to overcome them’ and in this sense implementation science is equal to implementation research as described above [15],[43],[44].
The term health services research suggests research that focuses on the service component of the health system, but it is often defined more broadly and used interchangeably with health systems research [17],[45].
Conclusion
Definitions are meant to clarify. But if too many different definitions for the same terms abound, so much confusion results that they become an obstacle to progress. Our aim here is not to establish which of these definitions are correct or to launch an intense debate about definitions that would distract from the need to support the research itself and the use of research results to improve health. Instead, we seek to provide a simple framework that is easily understood by both experts in the field and the managers, policy makers, and donors working to improve health systems and deliver better health care. We have tried to map the three main research domains, the research targets, and the users, and to highlight the importance of context and study design in the subsequent utility of the research findings.
Research on operational problems, on implementation strategies, and on health system challenges all involve multidisciplinary research that tends to use the same type of quantitative and qualitative research methods. But these three research domains differ in the type of research questions they address, in the way they are designed, and in their expected outcomes. Operational research and implementation research are action-oriented, respond to operational problems or implementation challenges, and work towards developing targeted solutions. Research on health system challenges addresses more complex, systems problems and is geared towards improving the understanding of what works for whom and under what circumstances. It provides guidance on what might work better within the system as a whole.
The three research domains are not mutually exclusive, and there are large overlapping areas. Research on operational problems is about local problem solving, but not all the problems it addresses are truly local. Many occur in a similar manner in multiple locations and may represent implementation problems for specific interventions that might be efficiently tackled by implementation research, or are representative of a systems problem that could be effectively addressed through health systems research. New implementation strategies are often designed to overcome specific health system failures, e.g., how to improve access to vaccination among children who are currently not reached by immunization services or home treatment for malaria in communities where formal health systems are not able to effectively provide such treatment. In such situations, implementation research develops innovative solutions that are in effect improvements of the health system and that could be regarded as health systems research, especially when these innovations affect more than just a single intervention. Such overlap between the three research domains provides opportunities for cross-fertilization that should lead to greater consideration by operational and implementation researchers of the wider system implications of their research. Accordingly, this should encourage the expansion of study designs and an appreciation of the feasibility of experimentation with different health system solutions.
We hope the above helps clarify what research to improve health systems is seeking to achieve. In essence it is quite simple: it involves operational research on operational problems, implementation research on implementation strategies for available interventions, and research on health system challenges as the main focus of health systems research. To improve health care delivery to poor populations, all of these research domains are very much needed.
Zdroje
1. FryattRMillsANordstromA 2010 Financing of health systems to achieve the health Millennium Development Goals in low-income countries. Lancet 375 419 426
2. MadonTHofmanKJKupferLGlassRI 2007 Public health implementation science. Science 318 1728 1729
3. SambBEvansTDybulMAtunRMoattiJP 2009 An assessment of interactions between global health initiatives and country health systems. Lancet 373 2137 2169
4. TravisPBennettSHainesAPangTBhuttaZ 2004 Overcoming health-systems constraints to achieve the Millennium Development Goals. Lancet 364 900 906
5. World Health Organization 2005 Report from the Ministerial Summit on Health Research 2004, Mexico City, Mexico Geneva World Health Organization
6. BennettSAdamTZarowskyCTangcharoensathienVRansonK 2008 From Mexico to Mali: progress in health policy and systems research. Lancet 372 1571 1578
7. World Health Organization 2009 Scaling up research and learning for health systems: now is the time. Report of a High Level Task Force Geneva World Health Organization
8. ZachariahRHarriesADIshikawaNRiederHLBissellK 2009 Operational research in low-income countries: what, why, and how? Lancet Infect Dis 11 711 717
9. The Global Fund and World Health Organization 2007 Guide to operational research in programmes supported by the Global Fund Geneva The Global Fund
10. World Health Organization and the Global Fund 2008 Framework for Operations and Implementation Research in Health and Disease Control Programmes Geneva World Health Organization
11. HorstickOSommerfeldJKroegerARidleyR 2010 Operational research in low-income countries. Lancet Infect Dis 10 369 370
12. SandersDHainesA 2006 Implementation research is needed to achieve international health goals. PLoS Med 3 e186
13. AlloteyPReidpathDDGhalibHPagnoniFSkellyWC 2008 Efficacious, effective, and embedded interventions: implementation research in infectious disease control. BMC Public Health 8 343
14. UNICEF/UNDP/World Bank/WHO Special Programme for Research and Training in Tropical Diseases 2003 Implementation Research in TDR: conceptual and operational framework Geneva World Health Organization. Report No.: TDR/IDE/SP/03.1
15. EcclesMPArmstrongDBakerRClearyKDaviesH 2009 An implementation research agenda. Implement Sci 4 18
16. BhattacharyyaOReevesSZwarensteinM 2009 What is implementation research: rationale, concepts and practice. Research on Social Work Practice 19 491 502
17. Alliance for Health Policy and Systems Research 2007 What is health policy and systems research and why does it matter? Geneva World Health Organization
18. MillsAGilsonLHansonKPalmerNLagardeM 2008 What do we mean by rigorous health-systems research? Lancet 372 1527 1529
19. World Health Organization and partners 2010 The First Global Symposium on Health Systems Research (HSR) - Science to Accelerate Universal Health Coverage, Montreux, November 2010. Available: http://www.hsr-symposium.org/. Accessed 10 September 2010
20. World Health Organization 2007 Everybody's business: strengthening health systems to improve health outcomes. WHO's framework for action Geneva World Health Organization
21. 1989 The Oxford English Dictionary Second Edition
22. World Health Organization, Department of Reproductive Health and Research 2003 Expanding capacity for operations research in reproductive health Geneva World Health Organization Report No.: WHO/RHR/02.18
23. ZachariahRFordNDraguezBYunOReidT 2010 Conducting operational research within a non governmental organization: the example of Medecins Sans Frontieres. Internat Health 2 1 8
24. CDI Study Group 2010 Community-directed interventions for priority health problems in Africa: results of a multicountry study. Bull World Health Organ 88 509 518
25. World Health Organization 2009 Meeting of the Strategic Advisory Group of Experts on Immunization, October 2009 – conclusions and recommendations. Wkly Epidemiol Rec 84 517 532
26. PagnoniF 2009 Malaria treatment: no place like home. Trends Parasitol 25 3 115 119
27. RemmeJHF 2004 Research for control: the example of onchocerciasis. Trop Med Int Health 9 243 254
28. de SavignyDAdamT 2009 Systems thinking for health systems strengthening Geneva World Health Organization, Alliance for Health Policy and Systems Research
29. De SavignyDKasaleHMbuyaCReidG 2008 Fixing health systems. 2nd ed Ottawa International Development Research Centre
30. VarkevisserCMPathmanathanIA.T.B 2003 Designing and conducting health systems research projects: Proposal development and fieldwork Ottawa International Development Research Centre
31. Task Force on Heath Systems Research 2004 Informed choices for attaining the Millennium Development Goals: towards an international cooperative agenda for health-systems research. Lancet 364 997 1003
32. RansonKLawTJBennettS 2010 Establishing health systems financing research priorities in developing countries using a participatory methodology. Soc Sci Med 70 1933 1942
33. RansonMKChopraMAtkinsSDal PozMRBennettS 2010 Priorities for research into human resources for health in low - and middle-income countries. Bull World Health Organ 88 435 443
34. LastJM 2001 A dictionary of epidemiology; fourth edition Oxford Oxford University Press
35. CraigPDieppePMacintyreSMichieSNazarethI 2008 Developing and evaluating complex interventions: the new Medical Research Council guidance. BMJ 337 a1655
36. RemmeJHBlasEChitsuloLDesjeuxPMEngersHDKanyokTP 2002 Strategic emphases for tropical diseases research: a TDR perspective. Trends Parasitol 18 421 426
37. EdejerTTBaltussenRAdamTHutubessyRAcharyaA 2003 WHO guide to cost-effectiveness analysis Geneva World Health Organization
38. GuiasuS 2009 Probabilistic models in operations research New York Nova Science Publishers
39. EcclesMPMittmanBS 2006 Welcome to Implementation Science. Implement Sci 1 1 3
40. McKibbonKALokkerCWilczynskiNLCiliskaDDobbinsM 2010 A cross-sectional study of the number and frequency of terms used to refer to knowledge translation in a buddy of health literature in 2006: a Tower of Babel? Implement Sci 5 1 11
41. WallinL 2009 Knowledge translation and implementation research in nursing. Int J Nurs Stud 46 576 587
42. WalkerAEGrimshawJJohnstonMPittsNSteenN 2003 PRIME–PRocess modelling in ImpleMEntation research: selecting a theoretical basis for interventions to change clinical practice. BMC Health Serv Res 3 22
43. WoolfSH 2008 The meaning of translational research and why it matters. JAMA 299 211 213
44. GrayJ 2010 Global health experts seek to transform programs through implementation science. Global Health Matters 9 10 12
45. LohrKNSteinwachsDM 2002 Health services research: an evolving definition of the field. Health Serv Res 37 7 9
46. RamaiahKDDasPKAppavooNCRamuKAugustinDJ 2000 A programme to eliminate lymphatic filariasis in Tamil Nadu state, India: compliance with annual single-dose DEC mass treatment and some related operational aspects. Trop Med Int Health 5 842 847
47. RamaiahKDVijay KumarKNHoseinEKrishnamoorthyPAugustinDJ 2006 A campaign of “communication for behavioural impact” to improve mass drug administrations against lymphatic filariasis: structure, implementation and impact on people's knowledge and treatment coverage. Ann Trop Med Parasitol 100 345 361
48. ZachariahRVan EngelgemIMassaquoiMKochollaLManziM 2008 Payment for antiretroviral drugs is associated with a higher rate of patients lost to follow-up than those offered free-of-charge therapy in Nairobi, Kenya. Trans R Soc Trop Med Hyg 102 288 293
49. RobaysJNyamowalaGSeseCBetu Ku Mesu KandeVLutumbaP 2008 High failure rates of melarsoprol for sleeping sickness, Democratic Republic of Congo. Emerg Infect Dis 14 966 967
50. UNICEF/UNDP/World Bank/WHO Special Programme for Research and Training in Tropical Diseases 1996 Community-directed treatment with ivermectin: report of a multi-country study Geneva World Health Organization Report No.: TDR/AFT/RP/96.1
51. MunkhuuBLiabsuetrakulTChongsuvivatwongVMcNeilEJanchivR 2009 One-stop service for antenatal syphilis screening and prevention of congenital syphilis in Ulaanbaatar, Mongolia: a cluster randomized trial. Sex Transm Dis 36 714 720
52. MondalDSinghSPKumarNJoshiASundarS 2009 Visceral leishmaniasis elimination programme in India, Bangladesh, and Nepal: reshaping the case finding/case management strategy. PLoS Negl Trop Dis 3 e355 doi:10.1371/journal.pntd.0000355
53. BlaauwDErasmusEPagaiyaNTangcharoensatheinVMulleiKMudhuneS 2010 Policy interventions that attract nurses to rural areas: a multicountry discrete choice experiment. Bull World Health Organ 88 350 356
54. RabkinMEl-SadrWMDe CockKM 2009 The impact of HIV scale-up on health systems: A priority research agenda. J Acquir Immune Defic Syndr 52 Suppl 1 S6 11
Štítky
Interní lékařství
Článek Water Supply and HealthČlánek Sanitation and Health
Článek vyšel v časopisePLOS Medicine
Nejčtenější tento týden
2010 Číslo 11- Berberin: přírodní hypolipidemikum se slibnými výsledky
- Léčba bolesti u seniorů
- Příznivý vliv Armolipidu Plus na hladinu cholesterolu a zánětlivé parametry u pacientů s chronickým subklinickým zánětem
- Červená fermentovaná rýže účinně snižuje hladinu LDL cholesterolu jako vhodná alternativa ke statinové terapii
- Jak postupovat při výběru betablokátoru − doporučení z kardiologické praxe
-
Všechny články tohoto čísla
- Why Do Evaluations of eHealth Programs Fail? An Alternative Set of Guiding Principles
- Strategies for Increasing Recruitment to Randomised Controlled Trials: Systematic Review
- Water Supply and Health
- Prescription Medicines and the Risk of Road Traffic Crashes: A French Registry-Based Study
- Air Pollution and the Microvasculature: A Cross-Sectional Assessment of In Vivo Retinal Images in the Population-Based Multi-Ethnic Study of Atherosclerosis (MESA)
- Can We Count on Global Health Estimates?
- Production and Analysis of Health Indicators: The Role of Academia
- WHO and Global Health Monitoring: The Way Forward
- Global Health Estimates: Stronger Collaboration Needed with Low- and Middle-Income Countries
- Sanitation and Health
- Combining Domestic and Foreign Investment to Expand Tuberculosis Control in China
- Colorectal Cancer Screening for Average-Risk North Americans: An Economic Evaluation
- Efficacy of Oseltamivir-Zanamivir Combination Compared to Each Monotherapy for Seasonal Influenza: A Randomized Placebo-Controlled Trial
- Road Trauma in Teenage Male Youth with Childhood Disruptive Behavior Disorders: A Population Based Analysis
- A Call for Responsible Estimation of Global Health
- Hygiene, Sanitation, and Water: What Needs to Be Done?
- Defining Research to Improve Health Systems
- Which Path to Universal Health Coverage? Perspectives on the World Health Report 2010
- Doctors and Drug Companies: Still Cozy after All These Years
- Hygiene, Sanitation, and Water: Forgotten Foundations of Health
- The Imperfect World of Global Health Estimates
- PLOS Medicine
- Archiv čísel
- Aktuální číslo
- Informace o časopisu
Nejčtenější v tomto čísle- Efficacy of Oseltamivir-Zanamivir Combination Compared to Each Monotherapy for Seasonal Influenza: A Randomized Placebo-Controlled Trial
- Doctors and Drug Companies: Still Cozy after All These Years
- Strategies for Increasing Recruitment to Randomised Controlled Trials: Systematic Review
- Prescription Medicines and the Risk of Road Traffic Crashes: A French Registry-Based Study
Kurzy
Zvyšte si kvalifikaci online z pohodlí domova
Současné možnosti léčby obezity
nový kurzAutoři: MUDr. Martin Hrubý
Všechny kurzyPřihlášení#ADS_BOTTOM_SCRIPTS#Zapomenuté hesloZadejte e-mailovou adresu, se kterou jste vytvářel(a) účet, budou Vám na ni zaslány informace k nastavení nového hesla.
- Vzdělávání



