-
Články
Top novinky
Reklama- Vzdělávání
- Časopisy
Top články
Nové číslo
- Témata
Top novinky
Reklama- Videa
- Podcasty
Nové podcasty
Reklama- Kariéra
Doporučené pozice
Reklama- Praxe
Top novinky
ReklamaEvent Rates, Hospital Utilization, and Costs Associated with Major Complications of Diabetes: A Multicountry Comparative Analysis
Background:
Diabetes imposes a substantial burden globally in terms of premature mortality, morbidity, and health care costs. Estimates of economic outcomes associated with diabetes are essential inputs to policy analyses aimed at prevention and treatment of diabetes. Our objective was to estimate and compare event rates, hospital utilization, and costs associated with major diabetes-related complications in high-, middle-, and low-income countries.Methods and Findings:
Incidence and history of diabetes-related complications, hospital admissions, and length of stay were recorded in 11,140 patients with type 2 diabetes participating in the Action in Diabetes and Vascular Disease (ADVANCE) study (mean age at entry 66 y). The probability of hospital utilization and number of days in hospital for major events associated with coronary disease, cerebrovascular disease, congestive heart failure, peripheral vascular disease, and nephropathy were estimated for three regions (Asia, Eastern Europe, and Established Market Economies) using multiple regression analysis. The resulting estimates of days spent in hospital were multiplied by regional estimates of the costs per hospital bed-day from the World Health Organization to compute annual acute and long-term costs associated with the different types of complications. To assist, comparability, costs are reported in international dollars (Int$), which represent a hypothetical currency that allows for the same quantities of goods or services to be purchased regardless of country, standardized on purchasing power in the United States. A cost calculator accompanying this paper enables the estimation of costs for individual countries and translation of these costs into local currency units. The probability of attending a hospital following an event was highest for heart failure (93%–96% across regions) and lowest for nephropathy (15%–26%). The average numbers of days in hospital given at least one admission were greatest for stroke (17–32 d across region) and heart failure (16–31 d) and lowest for nephropathy (12–23 d). Considering regional differences, probabilities of hospitalization were lowest in Asia and highest in Established Market Economies; on the other hand, lengths of stay were highest in Asia and lowest in Established Market Economies. Overall estimated annual hospital costs for patients with none of the specified events or event histories ranged from Int$76 in Asia to Int$296 in Established Market Economies. All complications included in this analysis led to significant increases in hospital costs; coronary events, cerebrovascular events, and heart failure were the most costly, at more than Int$1,800, Int$3,000, and Int$4,000 in Asia, Eastern Europe, and Established Market Economies, respectively.Conclusions:
Major complications of diabetes significantly increase hospital use and costs across various settings and are likely to impose a high economic burden on health care systems.
: Please see later in the article for the Editors' Summary
Published in the journal: . PLoS Med 7(2): e32767. doi:10.1371/journal.pmed.1000236
Category: Research Article
doi: https://doi.org/10.1371/journal.pmed.1000236Summary
Background:
Diabetes imposes a substantial burden globally in terms of premature mortality, morbidity, and health care costs. Estimates of economic outcomes associated with diabetes are essential inputs to policy analyses aimed at prevention and treatment of diabetes. Our objective was to estimate and compare event rates, hospital utilization, and costs associated with major diabetes-related complications in high-, middle-, and low-income countries.Methods and Findings:
Incidence and history of diabetes-related complications, hospital admissions, and length of stay were recorded in 11,140 patients with type 2 diabetes participating in the Action in Diabetes and Vascular Disease (ADVANCE) study (mean age at entry 66 y). The probability of hospital utilization and number of days in hospital for major events associated with coronary disease, cerebrovascular disease, congestive heart failure, peripheral vascular disease, and nephropathy were estimated for three regions (Asia, Eastern Europe, and Established Market Economies) using multiple regression analysis. The resulting estimates of days spent in hospital were multiplied by regional estimates of the costs per hospital bed-day from the World Health Organization to compute annual acute and long-term costs associated with the different types of complications. To assist, comparability, costs are reported in international dollars (Int$), which represent a hypothetical currency that allows for the same quantities of goods or services to be purchased regardless of country, standardized on purchasing power in the United States. A cost calculator accompanying this paper enables the estimation of costs for individual countries and translation of these costs into local currency units. The probability of attending a hospital following an event was highest for heart failure (93%–96% across regions) and lowest for nephropathy (15%–26%). The average numbers of days in hospital given at least one admission were greatest for stroke (17–32 d across region) and heart failure (16–31 d) and lowest for nephropathy (12–23 d). Considering regional differences, probabilities of hospitalization were lowest in Asia and highest in Established Market Economies; on the other hand, lengths of stay were highest in Asia and lowest in Established Market Economies. Overall estimated annual hospital costs for patients with none of the specified events or event histories ranged from Int$76 in Asia to Int$296 in Established Market Economies. All complications included in this analysis led to significant increases in hospital costs; coronary events, cerebrovascular events, and heart failure were the most costly, at more than Int$1,800, Int$3,000, and Int$4,000 in Asia, Eastern Europe, and Established Market Economies, respectively.Conclusions:
Major complications of diabetes significantly increase hospital use and costs across various settings and are likely to impose a high economic burden on health care systems.
: Please see later in the article for the Editors' SummaryIntroduction
The prevalence of diabetes worldwide was estimated to be 2.8% in 2000 and projected to rise to 4.4% by 2030, with more than three-quarters of people with diabetes living in developing countries [1]. Diabetes imposes a considerable burden in terms of premature mortality, morbidity, and health care costs. Life expectancy for people with diabetes has been estimated to be up to 10 y shorter than for people without diabetes [2]–[4]. Likewise diabetes imposes substantial demands on health care systems, as medical expenditures for people with diabetes are up to three times greater than for those without diabetes, largely because of macrovascular complications [5]–[7].
Currently there is a paucity of information on the direct medical costs associated with treating diabetes in low - and middle-income countries [8]. For example, lacking microlevel data, a recent estimate of the global health care costs of treating diabetes was based on country-level information regarding total health care spending, the prevalence of diabetes, and ratios of the costs of care for people with and without diabetes [9]. Although such an approach provides estimates of the overall resources devoted to the treatment of diabetes, it provides no indication of how different types of complications contribute to health care costs.
Health care resources devoted to people with diabetes may differ across countries because of a wide variety of factors including different rates of complications and the case fatality associated with events, as well as patterns of treatment such as the frequency and length of hospital episodes. Estimates of the resource use associated with treating different types of events associated with diabetes are essential inputs to projections of the economic burden of diabetes. These inputs are also needed in economic evaluations of interventions for prevention or treatment of diabetes, in order to quantify costs that may be averted owing to lower rates of complications.
The purpose of this study was to estimate acute and long-term resource use associated with five major complications of diabetes, on the basis of patient-level information from the Action in Diabetes and Vascular Disease (ADVANCE) study [10], a multinational clinical trial that included over 11,000 participants from 20 countries. Focusing on three groups of countries defined by geography and level of economic development, we examined variation in rates of major complications and used regression models to estimate the short-term and long-term hospital use associated with these events. Combining these estimates with estimated hospital bed-day costs from the World Health Organization's (WHO) CHOICE project [11], we estimated the total annual hospital costs associated with major complications among patients with diabetes in different regions.
Methods
Study Population
All patients included in this analysis were participants in the ADVANCE (Action in Diabetes and Vascular Disease: Preterax and Diamicron MR Controlled Evaluation) study. ADVANCE was a randomised 2×2 factorial trial in 11,140 normotensive patients with type 2 diabetes comparing (i) gliclazide MR-based intensive glucose control regimen, or regular, guideline-based glucose control therapy in patients with type 2 diabetes, and (ii) routine blood pressure lowering based on a perindopril-indapamide combination or matching placebo [12]. The gliclazide MR-based intensive blood glucose control regimen aimed to reduce haemoglobin A1C to 6.5% or lower (compared with haemoglobin A1C targets of 7%–8% suggested by most regional guidelines) [10]. As the focus of the current study was on variation in hospital use associated with major complications, rather than on the outcomes associated with particular therapies, the analysis was based on all participants in the study. ADVANCE is registered with ClinicalTrials.gov, number NCT00145925.
Patients were eligible for the trial if they had been diagnosed with type 2 diabetes mellitus at the age of 30 y or older, were aged 55 y or older at entry to the study, and had a history of major macrovascular disease or at least one other risk factor for macrovascular disease. The eligibility criteria were intentionally designed to enroll a broad cross-section of high-risk patients [12]. In this study countries are grouped into three regions. The countries (with numbers of randomized patients in parentheses) in each region are: Asia (4,136) comprising China (3,293), India (471), Malaysia (236), and the Philippines (136); Eastern Europe (2,142) comprising the Czech Republic (209), Estonia (155), Hungary (434), Lithuania (118), Poland (604), Russia (164), and Slovakia (458); and Established Market Economies (4,862) comprising Australia (978), Canada (436), France (196), Germany (327), Ireland (442), Italy (21), The Netherlands (507), New Zealand (630), and the United Kingdom (1,325). These regions are compatible with the World Bank's geographic regions, as Asia comprises countries from the World Bank's South Asia and East Asia and Pacific regions and Eastern Europe comprises countries from the World Bank's Europe and Central Asia region.
Identification of Complications and Hospitalizations
Five prespecified endpoints from the study were used in the analysis: (i) major coronary events; (ii) major cerebrovascular events; (iii) heart failure; (iv) peripheral vascular events; and (v) new or worsening nephropathy. Outcomes were coded according to the 10th Revision of the International Classification of Diseases. Information on hospitalization (including admission for less than one day) was collected from all patients during the trial at their regular clinic visits or at the time of death, if relevant [10].
Statistical Methods
The cumulative incidence of events was plotted by region, and standard log-rank methods without adjustment for covariates were used to test for significant differences across regions. Annual estimates of the probability of admission to the hospital and the total number of days spent in hospital were calculated using regression models for longitudinal (panel) data [13]–[15]. For this analysis, hospital use was separated into two periods: (i) use during the year in which the complication occurs, and (ii) use in all subsequent years. Indicator variables were defined for each of the five types of complications, and distinguishing these two different periods. Other variables in the models included current age, sex, and region. We included an indicator variable for having more than one type of event in the same year to enable multiple complications to have a combined impact on hospital use or length of stay that differed from the sum of the individual effects. We also included indicator variables for mortality to capture different patterns of resource use near the time of death. Separate mortality variables were defined for each region and for three categories of events based on preliminary analyses indicating similar effects for the specific complications comprising each category: (i) coronary events or heart failure; (ii) cerebrovascular events; and (iii) all other deaths. Finally, we included indicator variables for study years (i.e., years since randomization) to allow for time-varying effects that were not captured in the other model covariates.
Two separate regression equations were estimated to model health care use. In both models, each individual contributes multiple observations, and the statistical models account for correlation between these observations. First, a logistic regression was used to model the annual probability of having at least one hospitalization, including random effects at the patient level. Second, a negative binomial regression was used to model counts of the total number of days spent in hospital within a year, given at least one hospital admission. The negative binomial regression was estimated using a generalized estimating equation approach with a log link [16]. As a preliminary analysis provided strong evidence of overdispersion in these data (p<0.0001 on a likelihood ratio test), the negative binomial model was used in preference to Poisson estimation. Similar two-part modeling approaches are commonly used in estimating cost and utilization functions for many types of health care [17], as these approaches enable explicit modeling of the decision to seek care, separate from the intensity of utilization.
Methods for Estimating Total Expected Hospital Use and Associated Costs
The expected annual number of days spent in hospital, given a particular event or event history, was computed by multiplying the estimated probability of hospitalization (calculated using the logistic regression equation) by the estimated annual number of days for those hospitalized (calculated using the negative binomial regression equation). The proportional contributions of each type of complication and multiple complications during the follow-up period were estimated and reported by region.
In order to compute estimated costs, we combined the regional estimates of expected hospital use in this study with estimated hospital bed-day costs made available by WHO's CHOICE project (www.who.int/choice). The methodology for estimating these bed-day costs has been described in detail elsewhere [11]. In brief, cross-country regression models were applied to a dataset compiled from secondary literature and unpublished reports on cost analyses in hospitals and health centres in 49 countries, between 1973 and 2000, totaling 2,173 country-years of observations. Cost data were adjusted for inflation using gross domestic product (GDP) deflator series and adjusted for currency differences using purchasing-power–parity exchange rates. Cost functions were estimated using ordinary least squares regression, relating the natural log of costs per hospital bed-day to the natural log of GDP per capita, the natural log of the hospital occupancy rate, and indicator variables for hospital level (primary, secondary, or tertiary), hospital type (public or private), and the inclusion of drug or food costs. For the present study we computed region-specific bed-day costs by applying the published coefficients from the WHO-CHOICE regression model [11] to estimates of 2008 GDP per capita from the World Bank (computed as regional averages reflecting the distribution across countries in the study population). We assumed a tertiary-level, public not-for-profit hospital, and included food but not drug costs. As a sensitivity analyses we also computed estimates for secondary-level hospitals.
Total costs were calculated as the product of the estimated probability of hospitalization, the estimated number of hospital days given admission, and the estimated hospital per diem cost. To account for uncertainty in these estimates we recomputed the results with 1,000 bootstrapped regression coefficient estimates for each of the three components. All costs are presented in 2008 international dollars (Int$), which represent a hypothetical currency that allows for the same quantities of goods or services to be purchased regardless of country, standardized on purchasing power in the US. While the main analyses in this paper report estimates at the regional level, we also present examples of calculations for selected countries. Costs for all countries involved in the ADVANCE study are readily available using a cost calculator provided as a supplement to this paper (Dataset S1). The cost calculator reports costs in international dollars as well as in local currency units, and also enables calculation of costs under various alternative assumptions, for example about hospital level.
All statistical analyses were undertaken using STATA 10.1 and the cost calculator is implemented as an Excel spreadsheet.
Results
Some regional differences were observed in the baseline characteristics of the population (Table 1). Compared with participants from Established Market Economies participants in the other regions were younger and more likely to be female. Blood pressure was substantially higher among Eastern European patients, who had a mean blood pressure at entry of 150/85 mm Hg. Body mass index was on average significantly lower among Asian patients.
Tab. 1. Characteristics of study participants at baseline. 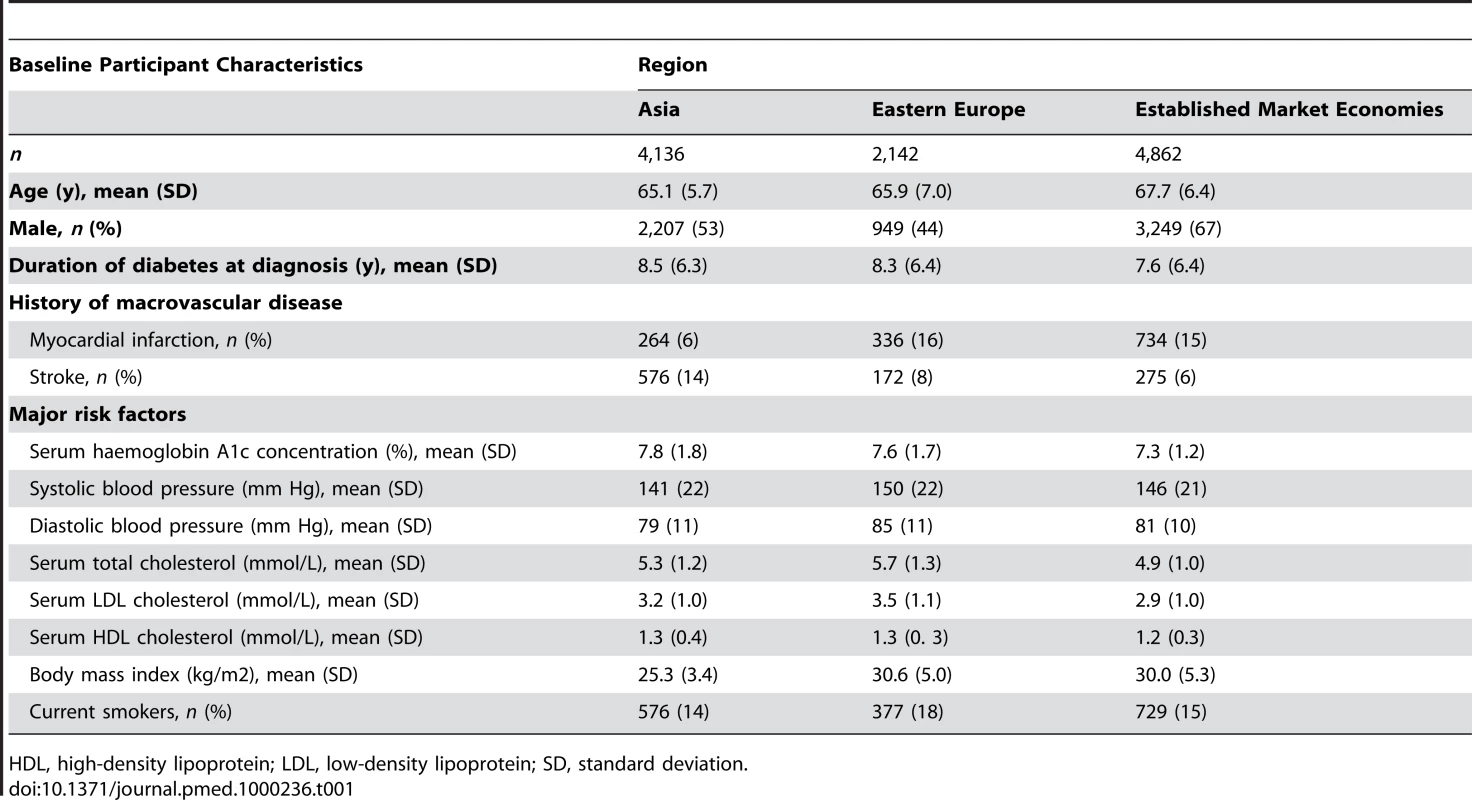
HDL, high-density lipoprotein; LDL, low-density lipoprotein; SD, standard deviation. A total of 10,955 hospitalizations were recorded during the study follow-up (median duration of follow-up was 5.0 y). The average numbers (standard deviation [SD]) of hospitalizations per participant during the trial by region were: Asia 0.7 (1.2); Eastern Europe 0.9 (1.6); Established Market Economies 1.3 (1.9). Significant differences across regions were observed in the cumulative incidence of the five types of complications and all-cause mortality (Figure 1). Compared with patients from Established Market Economies those in Eastern Europe had significantly higher incidence of cerebrovascular events (Figure 1B), heart failure (Figure 1C), and peripheral vascular disease (Figure 1D). In Asia the incidence of coronary events (Figure 1A) and peripheral vascular disease was significantly lower, whereas the incidence of stroke and nephropathy (Figure 1E) was significantly higher.
Fig. 1. Cumulative incidence of major complications and all-cause mortality in the ADVANCE study, by region. 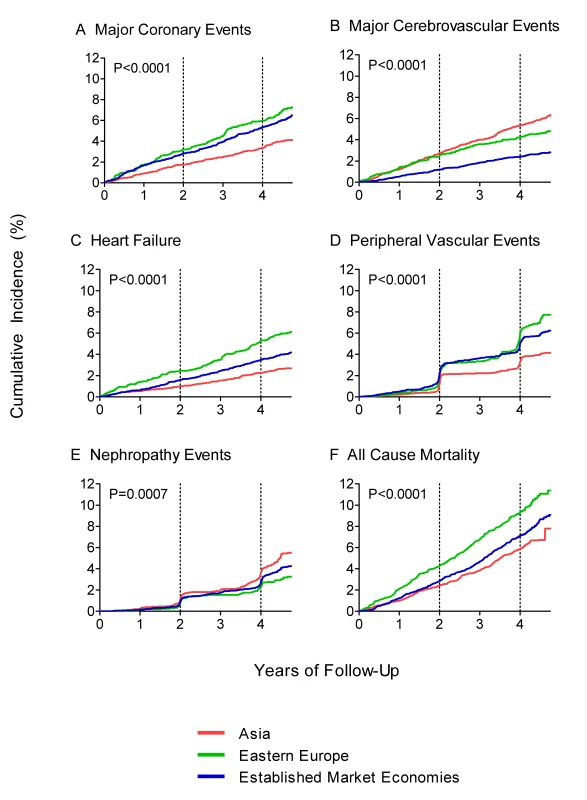
(A–E) Major complications. (F) All-cause mortality. The two-part regression results are reported in Table 2. These results may be used to predict hospital utilization among patients of a particular age and living in a particular region, in a year in which the patient either experiences a specific first complication or has a history of past complications. The regional predictions of complication-specific hospital use are reported in Table 3 for nonfatal complications. The first section reports probabilities of hospitalization following each type of complication. Overall, probabilities of hospitalization were highest for heart failure (93%–96% across regions); probabilities of hospitalization for coronary and cerebrovascular events were slightly lower. The lowest probabilities occurred for nephropathy (15%–26% across regions). Comparable probabilities for fatal events are available in Dataset S1. For coronary events and heart failure, fatal events were associated with lower probabilities of admission in all regions, presumably owing to acute fatality occurring before reaching hospital. Probabilities of admission were similar between fatal and nonfatal stroke events, while other types of complications were associated with greater probabilities of hospital use preceding fatal events. Across regions, probabilities of having at least one hospital admission were highest in Established Market Economies and lowest in Asia.
Tab. 2. Regression results for probability of hospitalization and expected number of hospital bed-days given at least one hospitalization. 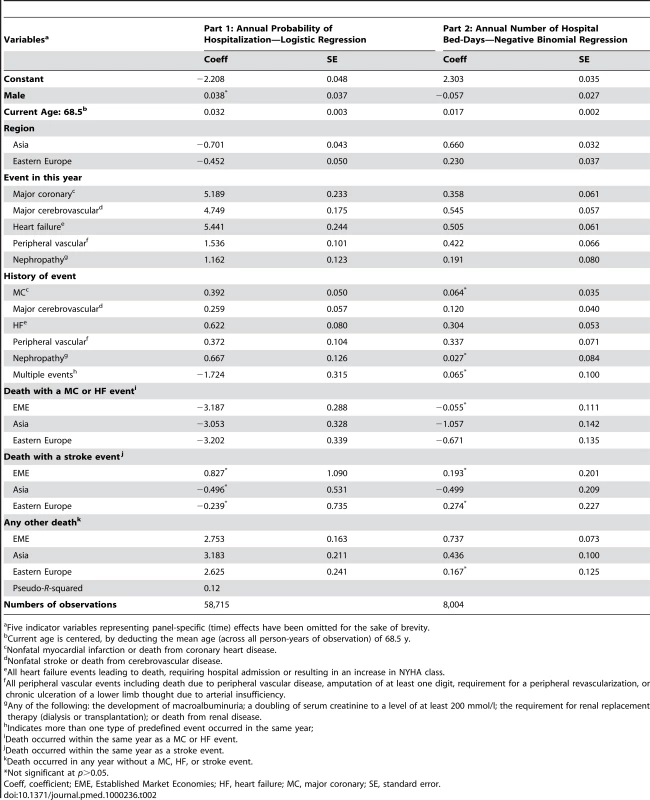
Five indicator variables representing panel-specific (time) effects have been omitted for the sake of brevity. Tab. 3. Estimated yearly probabilities of hospitalization and estimated numbers of bed-days per year given at least one hospitalization, by region. 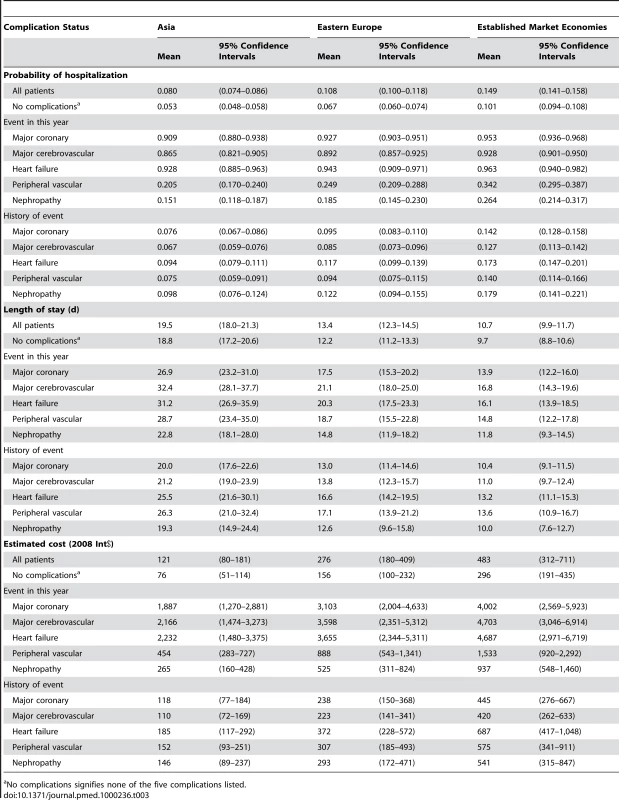
No complications signifies none of the five complications listed. The second section in Table 3 shows average numbers of inpatient bed-days per year given at least one hospitalization in that year. Numbers of days spent in hospital were greatest for stroke (17–32 across regions) and heart failure (16–31) and smallest for nephropathy (12–23). Again the estimated models also enable calculation of comparable figures for fatal complications (Dataset S1). Fatal coronary events and heart failure had shorter predicted lengths of stay in all regions; differences between fatal and nonfatal stroke varied by region; and length of stay increased in all regions for all other events and for those without complications. The overall comparison of length of stay across regions has the opposite pattern than that for hospitalization probabilities, with average length of stay in the absence of any of the specified complications in this study at nearly 19 d for Asia compared to 12 d in Eastern Europe and 10 d in Established Market Economies.
The final section in Table 3 reports estimated regional costs associated with the different types of complications, on the basis of the estimated numbers of total bed-days from ADVANCE, combined with WHO-CHOICE estimates of hospital per diem costs. Overall estimated annual hospital costs for patients with none of the specified events or event histories ranged from Int$76 in Asia to Int$296 in Established Market Economies. All complications included in this analysis led to significant increases in hospital costs. Coronary events, cerebrovascular events, and heart failure were the most costly, at more than Int$1,800, Int$3,000, and Int$4,000 in Asia, Eastern Europe, and Established Market Economies, respectively. Patients with a history of complications continued to have higher hospital use and costs in subsequent years relative to those without any history of complications. In a sensitivity analysis assuming that costs were incurred in secondary-level rather than tertiary-level hospitals, we found that costs were approximately 30% lower than those reported in the main analysis.
Although Table 3 presents regional estimates it is also possible to estimate country-specific costs by applying WHO-CHOICE hospital per diem estimates derived from national GDP per capita. For example, using this approach the estimated annual costs associated with nonfatal coronary events were Int$1,871 (95% confidence interval 1,260–2,857) for China, Int$2,655 (1,734–3,975) for Russia, and Int$3,947 (2,535–5,842) for the UK. The provided cost calculator (Dataset S1) enables estimation of hospital use and costs for any country in the ADVANCE study, assuming any specified hospital level, and expressed in either international dollars or local currency units.
Figure 2 shows the contributions from each type of specified complication to overall hospital use by region during the 5-y follow-up of the study. The complications identified in this study contributed the highest proportion of hospital use in Eastern Europe (approximately two-thirds), primarily due to the higher incidence of macrovascular events such as heart failure. In Asia these five complications contributed 60% to overall hospital use, with about half of the use associated with cerebrovascular events.
Fig. 2. Contributions of specific complications to total hospital use during the ADVANCE study, by region. 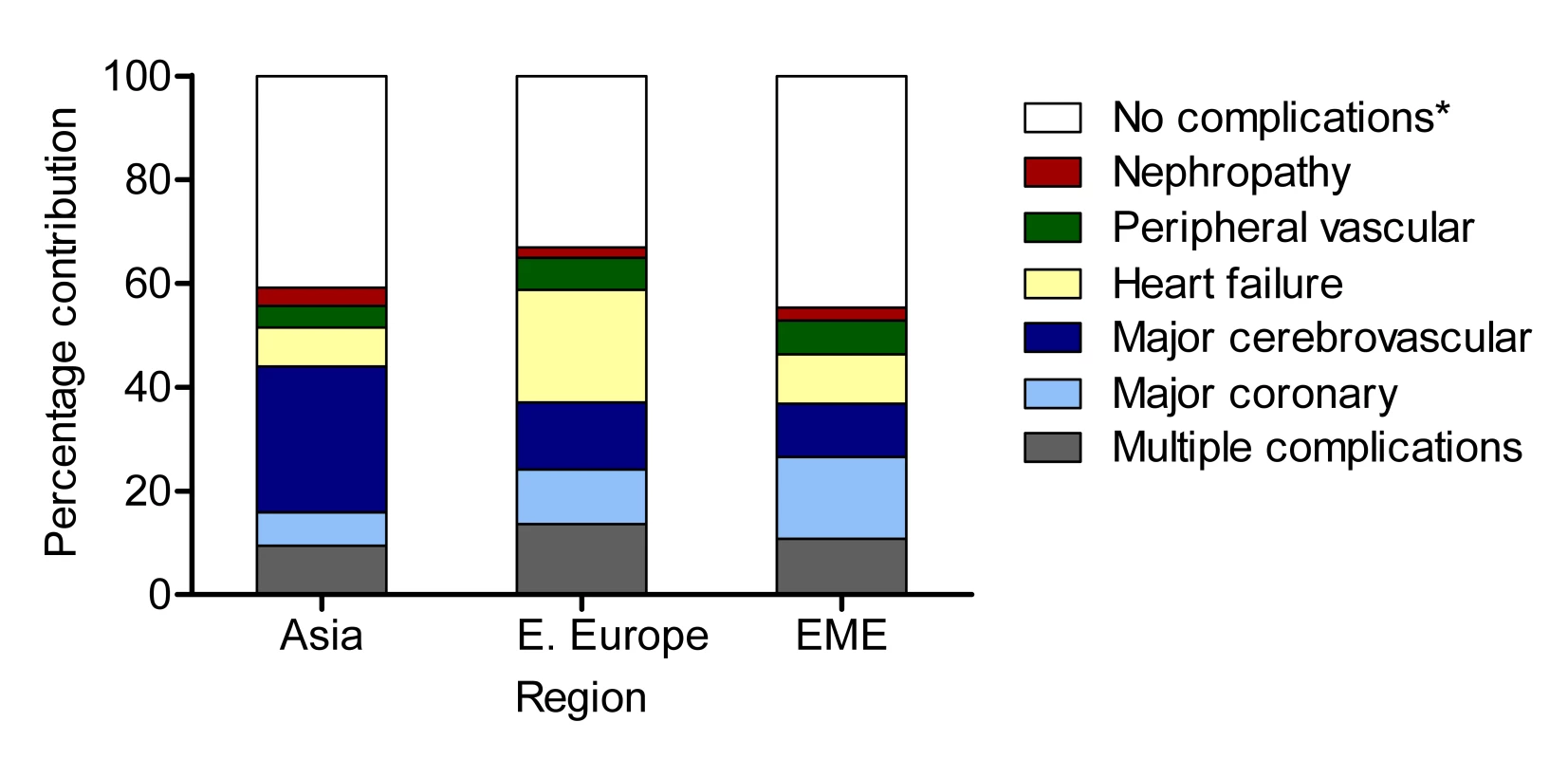
“No complications” signifies none of the five complications listed. EME, Established Market Economies. Discussion
In this study we have reported results from analyses of a large patient-level dataset collected in 20 countries (including seven countries in Eastern Europe and four in Asia) to obtain empirical estimates of the hospital use and indicative costs associated with a set of major complications that occur commonly in people with diabetes. There were significant differences in both the incidence of these complications and in patterns of hospital use across regions. Overall, patients in Asia and Eastern Europe had higher incidence of some events (e.g., stroke) than patients in Established Market Economies, lower rates of hospitalization, and longer lengths of stay. Specific complications varied markedly in their contributions to hospital use across regions. For example in Asia around 30% of days spent in hospital by people with diabetes could be attributed to stroke, whereas heart failure was more important in Eastern Europe. In both of these regions, major complications contributed a greater proportion of the hospital use recorded during the study than in Established Market Economies.
In addition to estimating hospital use directly from the ADVANCE data, we have also reported on estimated costs associated with this use, applying the hospital per diem costing methodology developed by WHO's CHOICE project. These cost estimates are intended to quantify hospital resource use associated with these events and not simply the cost of the admission for the event. Costs are reported in this paper using international dollars, as this approach facilitates comparability across regions by capturing differences in purchasing power for both traded and nontraded goods [18]. The models presented here can also be used to calculate estimates of hospital costs for patients in any of the 20 countries involved in the ADVANCE study, and for various combinations of complications based on the reported regression equations. To facilitate use of these models we have developed a simple spreadsheet-based tool that can be used to calculate hospital costs for all countries involved in ADVANCE (Dataset S1). It is also possible to refine costing estimates using supplementary costing information when available, such as hospital per diem costs by specialty in a specific country. The modular approach presented in this paper—with separate components for estimating probabilities of admission, length of stay, and bed-day costs—allows for flexibility in substituting estimates derived from other available sources for any of the three components.
An important motivation behind this analysis has been to develop a set of hospital cost estimates for major complications in patients with diabetes in Asian and Eastern European countries. To put our estimates into some perspective, recent estimates reported by WHO indicate an average annual per capita health expenditure of Int$216 for China and Int$698 for Russia [19]. Our results indicate that the annual hospital costs for people with diabetes experiencing major macrovascular complications such as coronary or cerebrovascular events are between four and ten times these average per capita expenditures. When interpreting these results it is important to note that this study has focused on hospital inpatient use and costs. Reports from developed countries have consistently observed that costs of inpatient care represent around half or more of the total health costs for people with diabetes [20]–[24], and this pattern of resource use is also reflected in more recent studies in developing countries [25],[26]. However, complications of diabetes can demand resources from other elements in the health system as well (e.g., increased use of outpatient services), and the fraction of all costs relating to hospital inpatient stays may vary across regions. Quantifying resource use and associated costs for the other health system elements should be a focus for future work, as the rising prevalence of diabetes globally is likely to require considerable additional health care resources to treat these and other major complications of diabetes.
Another important use of the information provided in this study is to provide essential inputs to economic evaluations. Cost-effectiveness analyses of interventions to manage diabetes conducted in developed countries often show that a significant proportion of the implementation costs are offset by savings in future treatment costs because of lower rates of complications [27],[28]. There is a need to undertake comparable studies of cost-effectiveness of alternative interventions for the treatment and prevention of diabetes in different regions (particularly in low - and middle-income countries). Our results can inform such analyses by providing estimates of the hospital resource use for countries in Asia and Eastern Europe. In this regard it will be useful to undertake a reexamination of the limited existing economic evaluations of diabetes that have been conducted in these regions, which have not accounted for regional differences in the incidence of complications [29], or have been confined to intermediate outcomes such as costs per case of diabetes prevented [30].
How do these results compare with previous studies reporting resource use and costs for major complications of diabetes? In regard to developed countries, the average lengths of stay for diabetic patients having macrovascular events in the UK are similar to previous estimates [31]. Our estimated annual costs for cerebrovascular events and heart failure also appear to be comparable with these previous estimates, but prior estimates of the cost of coronary heart disease events are around 50% higher than those reported here [31]. These cost differences for coronary heart disease are mostly likely due to higher costs associated with the specialty cardiology care of around £400 per day in the earlier study [31], compared with the WHO-CHOICE estimate of Int$302 used in this study. The reporting of the probability of hospitalization and average annual length of stay for each complication facilitates the calculation of additional estimates where other information on hospital bed-day costs is available. In terms of other comparisons, the hospital costs reported here for several macrovascular events appear to be of similar magnitude to a recent Chinese hospital-based cross-sectional study [26], but other studies have reported a wide variation in these costs [29]. For many other countries such as Russia we can find no published estimates available.
This study involves patients recruited by 215 centres in the ADVANCE study who were seen regularly in clinics over an average period of 5 y as part of a wider clinical trial. Although having prospectively collected information on the complications of a large group of patients is a key strength, it should also be noted that elements of the trial design and entry criteria may limit the applicability of the results to a broader patient population. Caution is therefore warranted in generalizing from the trial to all diabetic patients. Because the ADVANCE study intervention involved use of pharmacological therapies, we expect that absolute rates of complications in the trial may differ from those in general practice; on the other hand, because the trial protocol did not specify how patients with major complications would be treated in hospital, we expect that the frequency and intensity of hospital utilization in the trial will be more robust and generalizable to routine practice. While it would be useful to undertake prospective costing studies outside of clinical trials, the infrastructure costs associated with recruitment and follow-up of large cohorts of people with diabetes are likely to be important barriers to this form of data collection in many countries. Given persistent gaps in the evidence base on the economics of diabetes outcomes in low - and middle-income countries, this study provides critical information on patterns of hospital resource use and costs in settings where there have been no previous longitudinal studies.
To summarise, we expect that the estimates reported here will help inform the evaluation of therapies aimed at preventing diabetes-related complications, as they provide explicit quantification of the potential to avert future health care costs through successful secondary prevention. These results are required for decision makers who need to anticipate future health care costs for people with diabetes, or who wish to examine the cost-effectiveness of interventions aimed at reducing the rates of complications. Health care providers, policy makers, and health service researchers require timely information on the expected health and economic consequences of diabetes. Understanding the relative burden associated with different complications will provide critical evidence for health care decisions characterized by significant complexity and persistent uncertainty, particularly in settings constrained by severely limited resources.
Supporting Information
Zdroje
1. WildS
RoglicG
GreenA
SicreeR
KingH
2004 Global prevalence of diabetes: estimates for the year 2000 and projections for 2030. Diabetes Care 27 1047 1053
2. GuK
CowieCC
HarrisMI
1998 Mortality in adults with and without diabetes in a national cohort of the U. S. population, 1971–1993. Diabetes Care 21 1138 1145
3. RoperNA
BilousRW
KellyWF
UnwinNC
ConnollyVM
2001 Excess mortality in a population with diabetes and the impact of material deprivation: longitudinal, population based study. BMJ 322 1389 1393
4. NarayanKM
BoyleJP
ThompsonTJ
SorensenSW
WilliamsonDF
2003 Lifetime risk for diabetes mellitus in the United States. JAMA 290 1884 1890
5. SelbyJV
RayGT
ZhangD
ColbyCJ
1997 Excess costs of medical care for patients with diabetes in a managed care population. Diabetes Care 20 1396 1402
6. RamachandranA
RamachandranS
SnehalathaC
AugustineC
MurugesanN
2007 Increasing expenditure on health care incurred by diabetic subjects in a developing country: a study from India. Diabetes Care 30 252 256
7. RubinR
AltmanWM
MendelsonDN
1994 Health care expenditures for people with diabetes mellitus, 1992. J Clin Endocrinol Metab 78 809A 809F
8. NarayanKM
ZhangP
KanayaAM
WilliamsDE
EngelgauMM
2006 Diabetes: The pandemic and potential solutions. Disease control priorities in developing countries. 2nd edition. New York Oxford University Press 591 604
9. International Diabetes Federation 2006 Diabetes atlas. 3rd Edition. Brussels International Diabetes Federation
10. PatelA
MacMahonS
ChalmersJ
NealB
BillotL
W
2008 Intensive blood glucose control and vascular outcomes in patients with type 2 diabetes. N Engl J Med 358 2560 2572
11. AdamT
EvansDB
MurrayCJL
2003 Econometric estimation of country–specific hospital costs. Cost Eff Resour Alloc 1 3
12. ADVANCE Management Committee 2001 Study rationale and design of ADVANCE: action in diabetes and vascular disease—preterax and diamicron MR controlled evaluation. Diabetologia 44 1118 1120
13. WooldridgeJM
2001 Econometric analysis of cross section and panel data. Boston: MIT Press.
14. DigglePJ
HeagertyPJ
LiangK-Y
ZegerSL
2002 Analysis of longitudinal data. 2nd Edition. Oxford Oxford University Press
15. Rabe-HeskethS
SkrondalA
2005 Multilevel and longitudinal modeling using stata. College Station (Pennsylvania) Stata Press
16. Liang KY ZegerSL
1986 Longitudinal data analysis using generalized linear models Biometrika 73 13 22
17. JonesAM
2000 Health econometrics.
CulyerAJ
NewhouseJP
Handbook of health economics. Edition 1, volume 1, chapter 6 Amsterdam Elsevier 265 344
18. World Health Organization 2003 Making choices in health: WHO guide to cost-effectiveness analysis. Geneva World Health Organization
19. World Health Organization 2009 World health statistics 2009. Geneva World Health Organization
20. RubinRJ
AltmanWM
MendelsonDN
1994 Health expenditures for people with diabetes mellitus, 1992. J Clin Endocrinol Metab 78 809A 809F
21. HenrikssonF
AgardhC-D
BerneC
BolinderJ
LönnqvistF
2000 Direct medical costs for patients with type 2 diabetes in Sweden. J Intern Med 248 387 396
22. JönssonB
2002 Revealing the cost of Type II diabetes in Europe. Diabetologia 45 S5 S12
23. HoganP
DallT
NikolovP
American Diabetes Association 2003 Economic costs of diabetes in the U.S. in 2002. Diabetes Care 26 917 932
24. American Diabetes Association 2008 Economic costs of diabetes in the U.S. in 2007. Diabetes Care 31 596 615
25. RayappaPH
RajuKNM
KapurA
BjorkS
SylvestC
KumarDMD
1999 The impact of socio-economic factors on diabetes care. Int J Diab Dev Countries 19 7 19
26. WangW
FuCW
PanCY
ChenW
ZhanS
2009 How do type 2 diabetes mellitus-related chronic complications impact direct medical cost in four major cities of urban China? Value Health 12 923 929
27. ClarkePM
GrayAM
BriggsA
StevensRJ
MatthewsDR
HolmanRR
2005 Cost-utility analyses of intensive blood glucose and tight blood pressure control in type 2 diabetes (UKPDS 72). Diabetologia 48 868 877
28. HermanWH
HoergerTJ
BrandleM
HicksK
SorensenS
2005 Diabetes Prevention Program Research Group. The cost-effectiveness of lifestyle modification or metformin in preventing type 2 diabetes in adults with impaired glucose tolerance. Ann Intern Med 142 323 332
29. XieX
VondelingH
2008 Metformin cost-utility analysis of intensive blood glucose control with metformin versus usual care in overweight type 2 diabetes mellitus patients in Beijing, P.R. China. Value Health 11 S23 S32
30. RamachandranA
SnehalathaC
YamunaA
MaryS
ZhangP
2007 Cost-effectiveness of the interventions in the primary prevention of diabetes among Asian Indians: within-trial results of the Indian Diabetes Prevention Programme (IDPP). Diabetes Care 30 2548 2552
31. ClarkeP
GrayA
LegoodR
BriggsA
HolmanR
2003 The impact of diabetes-related complications on healthcare costs: results from the United Kingdom Prospective Diabetes Study (UKPDS Study No. 65). Diabet Med 20 442 450
Štítky
Interní lékařství
Článek vyšel v časopisePLOS Medicine
Nejčtenější tento týden
2010 Číslo 2- Berberin: přírodní hypolipidemikum se slibnými výsledky
- Léčba bolesti u seniorů
- Příznivý vliv Armolipidu Plus na hladinu cholesterolu a zánětlivé parametry u pacientů s chronickým subklinickým zánětem
- Jak postupovat při výběru betablokátoru − doporučení z kardiologické praxe
- Červená fermentovaná rýže účinně snižuje hladinu LDL cholesterolu jako vhodná alternativa ke statinové terapii
-
Všechny články tohoto čísla
- Effectiveness of Non-nucleoside Reverse-Transcriptase Inhibitor-Based Antiretroviral Therapy in Women Previously Exposed to a Single Intrapartum Dose of Nevirapine: A Multi-country, Prospective Cohort Study
- The Global Research Neglect of Unassisted Smoking Cessation: Causes and Consequences
- Adolescent HIV—Cause for Concern in Southern Africa
- Impact of Antiretroviral Therapy on Incidence of Pregnancy among HIV-Infected Women in Sub-Saharan Africa: A Cohort Study
- Automated Detection of Infectious Disease Outbreaks in Hospitals: A Retrospective Cohort Study
- Event Rates, Hospital Utilization, and Costs Associated with Major Complications of Diabetes: A Multicountry Comparative Analysis
- Pretreatment CD4 Cell Slope and Progression to AIDS or Death in HIV-Infected Patients Initiating Antiretroviral Therapy—The CASCADE Collaboration: A Collaboration of 23 Cohort Studies
- Can Broader Diffusion of Value-Based Insurance Design Increase Benefits from US Health Care without Increasing Costs? Evidence from a Computer Simulation Model
- Causes of Acute Hospitalization in Adolescence: Burden and Spectrum of HIV-Related Morbidity in a Country with an Early-Onset and Severe HIV Epidemic: A Prospective Survey
- Developing Global Maps of the Dominant Vectors of Human Malaria
- Guidance for Developers of Health Research Reporting Guidelines
- Packages of Care for Attention-Deficit Hyperactivity Disorder in Low- and Middle-Income Countries
- A New Policy on Tobacco Papers
- Ghostwriting at Elite Academic Medical Centers in the United States
- Measuring hsCRP—An Important Part of a Comprehensive Risk Profile or a Clinically Redundant Practice?
- PLOS Medicine
- Archiv čísel
- Aktuální číslo
- Informace o časopisu
Nejčtenější v tomto čísle- Packages of Care for Attention-Deficit Hyperactivity Disorder in Low- and Middle-Income Countries
- Measuring hsCRP—An Important Part of a Comprehensive Risk Profile or a Clinically Redundant Practice?
- Developing Global Maps of the Dominant Vectors of Human Malaria
- Guidance for Developers of Health Research Reporting Guidelines
Kurzy
Zvyšte si kvalifikaci online z pohodlí domova
Současné možnosti léčby obezity
nový kurzAutoři: MUDr. Martin Hrubý
Všechny kurzyPřihlášení#ADS_BOTTOM_SCRIPTS#Zapomenuté hesloZadejte e-mailovou adresu, se kterou jste vytvářel(a) účet, budou Vám na ni zaslány informace k nastavení nového hesla.
- Vzdělávání



